Abstract
Aims
To synthesize available data on the impact of the COVID‐19 pandemic on clinical supervision practices of healthcare workers and students in healthcare settings.
Design
A quantitative rapid review of the literature.
Data Sources
A search of MEDLINE, Embase, PsycINFO, the Cochrane Library and Scopus for English language papers published between December 2019 (initial onset of the pandemic) to March 2021.
Review methods
Using the World Health Organization and Cochrane guidelines for rapid reviews, following an identification of relevant papers and data extraction, a narrative synthesis approach was used to develop themes.
Results
Eight studies met the inclusion criteria. Four themes identified from data synthesis were nature and extent of disruptions to clinical supervision, unmet need for psychological support, supervisors also need support and unpacking telesupervision. Findings highlight the extent and nature of disruption to clinical supervision at the point of care. Further information on factors that facilitate high‐quality telesupervision have come to light.
Conclusion
The COVID‐19 pandemic has placed tremendous burden on healthcare workers compromising their own health and well‐being. It is essential to restore effective clinical supervision practices at the point of care, so as to enhance patient, healthcare worker and organizational outcomes into the post‐COVID‐19 pandemic period.
Impact
This review has provided initial evidence on the adverse impacts of the COVID‐19 pandemic on clinical supervision of healthcare workers and students at the point of care. Available evidence indicates the urgent need to restore effective and high‐quality clinical supervision practices in health settings. The review has highlighted a paucity of studies in this area, calling for further high‐quality studies.
Keywords: clinical supervision, COVID‐19 pandemic, supportive supervision
1. INTRODUCTION
The ongoing impact of the COVID‐19 pandemic continues to be felt across communities, sectors and organizations. Nowhere has this impact been more dramatic than in healthcare due to the increased burden of disease related to managing patients with COVID‐19, while also accounting for challenges to the healthcare workforce. Challenges confronting the healthcare workforce include shortages, stress, burnout and attrition (Department of Health [DoH], 2021). Many studies related to the impact of the COVID‐19 pandemic on the healthcare workforce have now shed light on the mental health challenges induced by the pandemic (Holton et al., 2021; Shanafelt et al., 2020). Two scoping reviews on the physical and mental health impacts of COVID‐19 on healthcare workers, have reported high levels of anxiety, depression, distress and insomnia (Shaukat et al., 2020; Shreffler et al., 2020). Female healthcare workers and nurses are among those that are at an increased risk of experiencing these impacts (Cabarkapa et al., 2020). It has become more important now than ever to better support the healthcare workforce as they battle the most wide‐spread health threat faced in recent times.
As the COVID‐19 pandemic has put a considerable strain on healthcare organizations' financial and human resources, timely development and implementation of new mental health and well‐being support initiatives for staff may not be possible. This makes it necessary to consider existing professional support mechanisms which can be seized to offer more support to healthcare workers in the workplace. Clinical supervision is well‐placed to do this, as there is evidence to support that high‐quality supervision practices and effective supervisors can facilitate positive outcomes for healthcare workers and organizations (Cutcliffe & McFeely, 2001; Martin, Lizarondo, et al., 2021; Martin, Tian, & Kumar, 2021; Milne & Reiser, 2020). High‐quality clinical supervision practices cannot exist in an environment where supervisors and supervisees are time poor (Ducat et al., 2016; Snowdon et al., 2019). Yet again, due to the pandemic, healthcare workers are time poor, prioritizing clinical duties over non‐clinical activities such as clinical supervision. As means of addressing these challenges, it is imperative to firstly map the nature and extent of disruptions caused by the pandemic to clinical supervision practices in healthcare settings, so that evidence‐informed enabling strategies can be implemented.
Rapid reviews are undertaken in preference to systematic reviews when information is needed quickly to inform policy and practice. As the COVID‐19 pandemic continues to impact healthcare systems globally, and put immense pressure on the healthcare workforce, there is a need for timely synthesis of current research on this topic. Therefore, this rapid review was undertaken, guided by the World Health Organization (WHO) practical guide on rapid reviews (Tricco et al., 2017); and the Cochrane interim guidance on rapid reviews (Garritty et al., 2020).
2. AIM
The aim of this rapid review was to investigate the impacts of the COVID‐19 pandemic on clinical supervision structures, processes and outcomes for healthcare workers and students in healthcare settings.
2.1. Design
The planning, conducting and reporting of this rapid review was guided by the WHO and Cochrane guidelines for rapid reviews (Garritty et al., 2020; Tricco et al., 2017). Narrative synthesis was used to synthesize available quantitative data to develop themes of information. A protocol was developed and registered on Open Science Framework (Martin, Lizarondo, et al., 2021; Martin, Tian, & Kumar, 2021). The WHO checklist for rapid reviews was used to ensure quality assurance of the review (see Supplementary Table 1).
2.2. Search methods
The following electronic databases were searched: MEDLINE; Embase; Emcare; PsycINFO; the Cochrane Library and Scopus. These databases were chosen as these are commonly used health‐centric databases and include single and multidisciplinary databases. As a means of avoiding publication bias, grey literature search was also be undertaken through online databases (ProQuest Central; ProQuest Dissertations & Theses Global; ProQuest Coronavirus Research Database), theses repository (TROVE) and an internet web engine (Google) to capture any additional publications, such as theses or dissertations and governmental or technical reports. Given the nature of a rapid review (i.e. need for a quick turnaround), the focus population of this review (i.e. healthcare workers and students) and the time of first reported human cases of COVID‐19, searches were restricted to English language, and publication date from December 2019 onwards (when COVID‐19 was first reported) (search date: March 2021). Search strategy for all databases has been included as Supplementary Table 2. Inclusion criteria were studies of healthcare workers and students from nursing, midwifery, medicine, dentistry, pharmacy and other allied professions that were receiving clinical supervision in one‐to‐one or group formats, in‐person or remotely (i.e. telesupervision) and using quantitative methods or where the quantitative data were able to be separated from mixed methods studies. The full inclusion and exclusion criteria have been provided in Table 1.
TABLE 1.
Inclusion/exclusion criteria
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Population | Healthcare workers (all levels of work experience, education and position classification) and/ or students on placement from the following disciplines:
|
|
| Intervention | All types (e.g. individual, group or peer supervision) and modes (e.g. face to face, telephone or videoconferencing) of CS (Milne, 2007) in primary, secondary and tertiary healthcare settings (e.g. hospitals and community settings) | Other forms of education and training to support/ direct/ guide healthcare workers or students on placement, such as staff training, consultancy, mentoring, coaching and operational or performance management |
| Comparator | CS in pre‐COVID times or no comparator | N/A |
| Outcome | Impact of the COVID‐19 pandemic on:
|
|
| Study design |
|
|
| Other |
|
|
2.3. Search outcomes
Following the search, all citations were imported into Endnote X9™ (The EndNote Team, 2013), and duplicates removed. Screening of titles and abstracts against the inclusion criteria was conducted using Covidence™ (Veritas Health Innovation, 2021). All citations were independently screened by two reviewers from the review team (ET and SK), with a third reviewer (PM) acting to resolve conflicts. Where titles and abstracts met the inclusion criteria, they were initially selected to be part of the review (step one). In step two, full‐text copies of eligible articles were retrieved for full examination. During this process, the full papers were examined independently by two reviewers (ET and SK) to identify if they met the inclusion criteria, with the third reviewer (PM) acting to resolve conflicts.
2.4. Methodological quality
The modified McMaster Quantitative Critical Appraisal tool (Law et al., 1998) was chosen as it is generic by design (i.e. it is not specific to individual research designs), is freely available and widely used. The tool provides a common framework for evaluating different research designs within a rapid review. The methodological quality of included studies was assessed by one reviewer (ET) and verified by another reviewer (PM). All discrepancies were resolved through mutual discussion. All studies, regardless of the results of their methodological quality, underwent data extraction and synthesis.
2.5. Data extraction
Data extraction was conducted by one reviewer (PM) and verified by another reviewer (ET) using a customized data extraction form, developed specifically for this review. The form was piloted by two reviewers (PM and ET) on three studies and subsequently refined. The categories on the form included country, setting, study participants, clinical supervision parameters (such as duration and frequency), clinical supervision structure, process and outcomes and supportive aspects of supervision. Quantitative data only were extracted from included mixed methods studies. See Supplementary Table 3 for the data extraction template.
2.6. Data synthesis
Due to the nature of the review, extracted data were synthesized narratively. Narrative synthesis is an approach to the synthesis of review findings from multiple sources in textual format providing an integrated interpretation of the topic area (Popay et al., 2006). Using the framework for narrative synthesis provided by Popay et al. (2006), a preliminary synthesis of findings from included studies was developed; similarities, differences and relationships in data across the studies were explored; and assessment of the robustness of the synthesis was undertaken by discussing findings in a wider context to test the extent to which conclusions are generalizable. Three reviewers (PM, ET and LL) were involved in the data synthesis process to ensure rigour in the synthesis process.
3. RESULTS
The database search yielded 4196 records. After removal of 973 duplicates, 3223 records underwent title and abstract screening. Subsequently, 24 articles were retrieved for full‐text review. Eight publications, which met all the inclusion parameters, were included in this review. Figure 1 (flow diagram of included studies) has further information. Two publications each were from the United Kingdom (Choi et al., 2020; Wanis et al., 2021), United States of America (Natchaba, 2020; Shklarski & Abrams, 2021) and Belgium (Kapila et al., 2020; Ulenaers et al., 2021); and one each from Australia (Bourke et al., 2021) and Italy (Zoia et al., 2020). Included studies spanned students, residents and practicing (i.e. post‐qualification) healthcare workers, from allied health (n = 3: Bourke et al., 2021; Natchaba, 2020; Shklarski & Abrams, 2021); nursing and midwifery (n = 2: Bourke et al., 2021; Ulenaers et al., 2021); dentistry (n = 1: Wanis et al., 2021) and medicine (n = 3: Bourke et al., 2021; Kapila et al., 2020; Zoia et al., 2020). Most included papers were quantitative (n = 6 cross‐sectional studies: Choi et al., 2020; Kapila et al., 2020; Natchaba, 2020; Ulenaers et al., 2021; Wanis et al., 2021; Zoia et al., 2020); and the remaining two studies (Bourke et al., 2021; Shklarski & Abrams, 2021), employed a mixed methods design. See Table 2 for further information on study characteristics.
FIGURE 1.
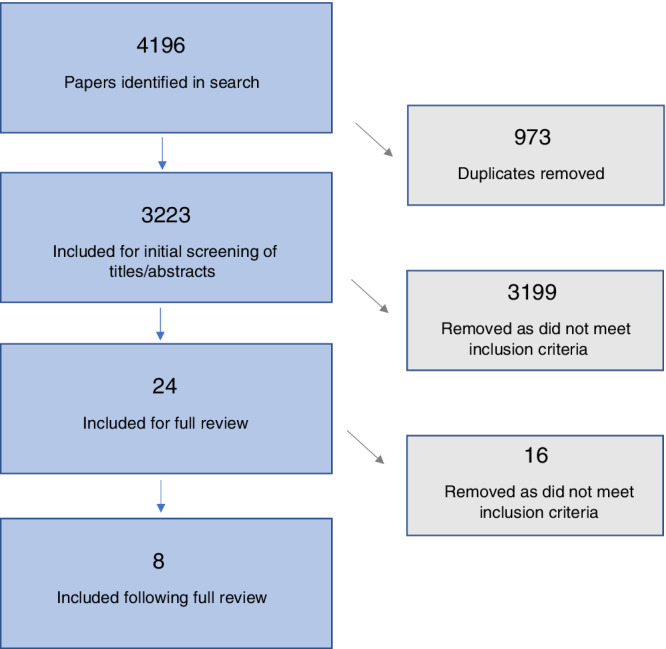
Flow diagram of included studies
TABLE 2.
Study characteristics
| No: | Author | Design | Country | Participants | Measures |
|---|---|---|---|---|---|
| 1 | Bourke et al. (2021) | Mixed methods | Australia | n = 1505 students (Nursing/midwifery/paramedicine 52%; medicine 9%, physiotherapy 8%; occupational therapy 6%, nutrition or dietetics 6%; speech pathology 4%; pharmacy 4% and 14 allied health disciplines 11%) | Online survey |
| 2 | Choi et al. (2020) | Cross‐sectional | United Kingdom | n = 440 final year students (Medicine) | Online survey |
| 3 | Kapila et al. (2020) | Cross‐sectional | Belgium, plus international participants from India, Romania, Israel and Italy | n = 86 plastic surgery residents (Medicine; 35 Belgium and 51 international participants) | Online survey |
| 4 | Natchaba (2020) | Cross‐sectional | United States | n = 68 practicing healthcare workers (Unclear, possibly social work and other allied health disciplines) | Online survey |
| 5 | Shklarski and Abrams (2021) | Mixed methods | United States | n = 76 practicing healthcare workers (social work and other professions not specified) | Online survey |
| 6 | Ulenaers et al. (2021) | Cross‐sectional | Belgium | n = 665 students (Nursing) | Online survey |
| 7 | Wanis et al. (2021) | Cross‐sectional | United Kingdom | n = 122 trainees (dental specialty) | Online survey |
| 8 | Zoia et al. (2020) | Cross‐sectional | Italy | n = 192 neurosurgery residents (Medicine) | Online survey |
3.1. Methodological quality
All included studies stated their purpose clearly, included a relevant background literature review and justification of the sample size. Two studies did not provide a detailed description of the study sample (Choi et al., 2020; Zoia et al., 2020). Only one study (Natchaba, 2020) used reliable, and four studies (Choi et al., 2020; Kapila et al., 2020; Natchaba, 2020; Ulenaers et al., 2021) used valid outcome measures. Only four studies reported results in terms of statistical significance (Bourke et al., 2021; Choi et al., 2020; Natchaba, 2020; Shklarski & Abrams, 2021). All studies except one (Kapila et al., 2020) used appropriate analysis methods. All studies reported the clinical importance of the findings and included conclusions appropriate to the study methods and results. The McMaster critical appraisal checklist is attached as Supplementary Table 4.
3.2. Impact of the COVID‐19 pandemic on clinical supervision practices
Four final themes were developed through the narrative synthesis process: nature and extent of disruptions to clinical supervision, unmet need for psychological support, supervisors also need support and unpacking telesupervision.
3.2.1. Nature and extent of disruptions to clinical supervision
All studies, except for one (Zoia et al., 2020) reported disruptions to a range of clinical supervision parameters such as frequency and duration, and reduced access to their supervisor, owing to the pandemic. Reduced access to supervisors was reported by supervisees to occur at times when they required more support, advice and reassurance. In the Australian study of 1505 pre‐registration students from several professions, one‐third of student supervisees reported that their supervisor did not have time to support them (Bourke et al., 2021). This was especially true for students on their first rural or remote placement and from an allied health profession. In a U.K. study of 440 medical students (Choi et al., 2020) a significant relationship was found between disruption to student placements and their perceived work readiness and confidence in assisting hospitals earlier. In an international study of 86 plastic surgery residents (Kapila et al., 2020), only 30% of Belgian residents and 39% of international residents surveyed reported receiving adequate supervision through the pandemic. In an U.S. study of 68 care coordinators and their supervisors (Natchaba, 2020), participants in both groups reported reduction in the frequency and duration of clinical supervision sessions. Some supervisors reported their supervision sessions moving from a fortnightly to a monthly arrangement. Supervision duration was reduced from 31 to 60 min to less than 30 min, and from more than 60 min to 31 to 60 min (Natchaba, 2020). The study of 122 dental specialty trainees also reported disruptions to planned clinical supervision sessions (Wanis et al., 2021). In contrast, in a U.S. study of 76 social workers and other healthcare workers, 76.6% of survey respondents reported no change to their clinical supervision structure and process. In this study however 82% of supervisees reported a good supervisory relationship with their supervisor, which is a well‐known facilitator of clinical supervision quality (Shklarski & Abrams, 2021). Similarly, in an Italian study of neurosurgery residents, those that were involved in the direct management of COVID‐19 patients (65.9%), reported receiving good support from supervisors most of the time. Further information about supervision parameters have not been reported by the authors of this study.
3.2.2. Unmet need for psychological support
Restorative or supportive functions of clinical supervision enable supervisors to support supervisees through critical and challenging times via facilitating reflection, debriefing and equipping with strategies to cope with stress. Although supervisees in the included studies expressed need for more support, especially for their psychological well‐being, this need remained largely unmet by supervisors. The pandemic was a time of great stress particularly for students undertaking clinical placements, which was manifested as an increased need for support and guidance and concerns for mental health. Even practicing healthcare workers experienced urgent needs to meet with their supervisors at short notice during the first wave of the pandemic given the newness of the situation (Shklarski & Abrams, 2021). A Belgian study of 665 nursing students, expressed an increased need to be heard, prepared and supported. They articulated a clear need for interactions with their supervisor (Ulenaers et al., 2021). Furthermore, participants reported gaps in the psychological support received and the inability to unwind in clinical supervision (Ulenaers et al., 2021). Similarly, in a study of dental specialty trainees, 62% reported feeling overwhelmed and anxious regarding the effects of the pandemic on their training ability and resulting career impacts long term (Wanis et al., 2021). In the Australian study, students reported reduced access to, and engagement from, their supervisors. Notably, younger students more frequently reported a decline in their well‐being, indicating an increased need for support (Bourke et al., 2021). The study of care coordinators and their supervisors highlighted that due to the COVID‐19 pandemic, lesser time was being spent in discussing about ‘self’ (i.e. supportive supervision), as managerial and administrative tasks tended to dominate the supervision sessions (Natchaba, 2020).
3.2.3. Supervisors also need support
Supervisors need support themselves to be able to better meet the supervisee's needs. Similar to supervisees, supervisors too experienced a great deal of stress induced by the COVID‐19 pandemic. A study included in this review highlights the importance of support for supervisors so that they can provide consistent support to supervisees to maintain the effectiveness of clinical supervision through challenging times such as the COVID‐19 pandemic. In this study, 70% reported that their supervisor behaved the same before and after the pandemic (Shklarski & Abrams, 2021), thereby linking consistency of supervisor behaviours to supervisee perceptions of effective supervision. Only when the supervisor is supported in their own role through times of change, they can continue to function as an effective supervisor. In another study of allied healthcare workers, where supervisors fostered a positive relationship, even a change of supervision mode from face‐to‐face to a remote format did not affect the quality of supervision (Natchaba, 2020).
3.2.4. Unpacking telesupervision
The COVID‐19 pandemic has seen a surge in the use of telesupervision due to quarantine and physical distancing requirements. Some studies included in this review have added evidence to this area. In the U.S. study of healthcare workers (Shklarski & Abrams, 2021), 88% of the participants switched to telesupervision because of the pandemic. They used Facetime, phone, Zoom or a combination of these platforms. Participants that had a positive supervisory relationship prior to switching to telesupervision, and those that had prior face‐to‐face contact, remained largely unaffected by the change of the supervision mode. Interestingly, in this study, younger participants perceived telesupervision to be less effective, when compared to their older counterparts. Supervisees in this study (Shklarski & Abrams, 2021), were also less affected by stress induced by the pandemic compared to other studies included in this review, reinforcing the value of a positive supervisory relationship and consistency in supervisor behaviours through challenging times. Interestingly, practicing healthcare workers in another study also reported that the change from face‐to‐face to telesupervision mode did not affect their supervision quality (Natchaba, 2020). Further information about this switch to telesupervision remains unknown.
4. DISCUSSION
This rapid review investigated the impacts of the COVID‐19 pandemic on clinical supervision structures, processes and outcomes for healthcare workers and students in healthcare settings. Findings indicate that the pandemic, not unexpectedly, has caused significant disruptions to clinical supervision of staff and students in healthcare settings. It highlights the need for healthcare workers to evaluate their clinical supervision arrangements to determine the nature and extent of impact, and to devise measures to re‐set effective supervision practices. Findings of this review reinforce the need to incorporate supportive components within supervision. As the pandemic has triggered several mental health concerns among healthcare workers (Holton et al., 2021; Shaukat et al., 2020; Shreffler et al., 2020), it is even more important to enhance the support provided within supervision now and into the post‐pandemic period (Martin & Snowdon, 2020). Furthermore, findings emphasize the need to provide support not only to supervisees, but also to supervisors, as the pandemic has been a stressful period for all. Finally, this review has added some further light on telesupervision, which remains an under‐investigated area within clinical supervision research.
Clinical supervision can produce positive outcomes only when the supervision provided, and supervisors are effective (Martin, Lizarondo, et al., 2021; Martin, Tian, & Kumar, 2021; Rothwell et al., 2021). Notable prerequisites for this are organizational structures and processes that can enable effective supervision, and quarantined time for supervisors and supervisees to engage in effective supervision practices (Ducat et al., 2016). There is evidence in the literature that shows that supervision sessions need to be of a certain frequency (at least monthly) and duration (at least 45 to 60 min) to be effective (Martin et al., 2014). The COVID‐19 pandemic has essentially disrupted key parameters of supervision by effecting structures and processes within healthcare and by permeating competing demands whereby healthcare workers are time pressured (Wang et al., 2021). Healthcare organizations and workers need to work together to consider clinical supervision time sacred, so that workers can receive the support they need in their roles through challenging times.
Supportive or restorative clinical supervision has been shown to enhance well‐being and reduce burnout (Milne & Reiser, 2020). Interestingly, healthcare workers were already experiencing health and well‐being concerns at work even prior to the COVID‐19 pandemic (Melnyk et al., 2018; Petrie et al., 2019; Ruitenburg et al., 2012), resulting in staff turnover, absenteeism and sickness; impacting on the quality of patient care and carrying huge financial implications to organizations internationally (Milne & Reiser, 2020). The pandemic has catapulted such pressures, placing healthcare workers at an even higher risk of mental health and well‐being issues (Holton et al., 2021; Shaukat et al., 2020; Shreffler et al., 2020). Clinical supervision can be a part of the solution to address this given its inherent supportive functions. This relies on a supervisor that has the required competencies to facilitate supportive supervision. Milne and Reiser (2020) outline six competencies of supportive supervision for the supervisor, along with 12 practical strategies. The competencies include developing supervisee's personal coping strategies and professional competencies by offering advice and guidance, encouraging supervisees to build relationships with peers and colleagues, building and strengthening the supervisory relationship, challenging thinking errors and clarifying associated feelings, providing constructive feedback and addressing interpersonal problems (Milne & Reiser, 2020; pp. 120–123). Supervisees have also been encouraged to be ready for their work by improving personal coping strategies, to be professionally able by developing competencies to better perform wok duties, and to be interpersonally effective by enhancing the supervisory relationship and boosting their social support (Milne & Reiser, 2020; pp. 145–146). Organizations, while making clinical supervision training available for workers, will need to embed elements of supportive supervision to enhance supervisor and supervisee knowledge, skills and competencies in undertaking supportive supervision (Martin, Lizarondo, et al., 2021; Martin & Snowdon, 2020; Martin, Tian, & Kumar, 2021; Milne & Reiser, 2020).
This review has shed light on factors that enable and sustain the switch from face‐to‐face to telesupervision. It is unsurprising that those with positive supervisory relationships largely remained unaffected when switching from face‐to‐face to telesupervision arrangements. This further illuminates the importance of positive supervisory relationships, adding to the already abounding evidence (Martin et al., 2014). It is noteworthy that when supervisor behaviours during the pandemic were consistent with pre‐pandemic behaviours, supervisees perceived supervision to be better, despite the switch to telesupervision (Shklarski & Abrams, 2021). This finding has implications not only for supervisors, but also healthcare organizations as supervisors (i.e. more senior staff) need support so that they can cope well during stressful times, so that supervisees (i.e. more junior staff) can receive the level of support and guidance they need. One study in this review found that supervisees preferred some online platforms like Zoom to undertake telesupervision when compared to other platforms such as Facetime. This may have been because Zoom is more frequently associated with work and Facetime with outside of work activities. While setting up telesupervision, supervisors and supervisees need to discuss and decide on the best platform or combination of platforms that they can trial using. This needs to be evaluated after a trial period to ensure it is meeting supervisee needs (Martin et al., 2018). It is noteworthy that one study (Shklarski & Abrams, 2021) found that younger supervisees perceived telesupervision as less effective, while another study (Bourke et al., 2021) noted that younger students more frequently reported a decline in their well‐being. Younger supervisees may benefit from more structure and support in clinical supervision in all modes. This area warrants further investigation.
5. LIMITATIONS
As the COVID‐19 pandemic set in only towards the end of 2019, and as conducting and publishing primary research is often time‐consuming, only a handful of primary studies were available that met inclusion criteria for this review. All studies used a cross‐sectional survey design, and most studies had methodological flaws. Most studies only collected perspectives from supervisees, using bespoke surveys without established psychometric properties. Further research is needed that uses standardized measurement tools and investigates clinical supervision impacts also from the supervisor and organizational perspectives. The resulting impact on patient care, although challenging to study, will need to be investigated. Despite the heterogeneity and opportunities for improved methodological rigour, this review provides a starting point to understand the disruptions to clinical supervision at the point of care. The review team consisting of clinical supervision practice and research experts have tapped into their knowledge of the broader clinical supervision literature to contextualize the findings of this review, to devise practical strategies that can inform policy and practice in real world settings.
6. CONCLUSION
This rapid review has provided initial evidence on the adverse impacts of the COVID‐19 pandemic on clinical supervision of healthcare workers and students at the point of care. Available evidence highlights the tremendous impact of the COVID‐19 pandemic, drastic changes to clinical supervision practices and highlights an urgent need to restore effective and high‐quality clinical supervision practices in health settings. It is essential to restore effective clinical supervision practices at the point of care, so as to enhance patient, healthcare worker and organization outcomes into the post‐COVID‐19 pandemic period. Further high‐quality studies are needed on the continued and long‐term impacts of the COVID‐19 pandemic on clinical supervision practices in healthcare settings.
AUTHOR CONTRIBUTIONS
All authors have agreed on the final version. All authors have made substantial contributions to the conception and design, acquisition of data, analysis and interpretation of data. All authors were involved in drafting the article and revising it critically for important intellectual content.
FUNDING INFORMATION
This manuscript is a part of Dr Priya Martin's postdoctoral fellowship which was funded through an Advance Queensland Industry Research Fellowship Grant and co‐funded by Darling Downs Health, Southern Queensland Rural Health, the University of Queensland Rural Clinical School and the University of South Australia.
CONFLICT OF INTEREST
No conflict of interest has been declared by the authors.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/jan.15360.
Supporting information
Supplementary Table 1
Supplementary Table 2
Supplementary Table 3
Supplementary Table 4
ACKNOWLEDGEMENT
Open access publishing facilitated by The University of Queensland, as part of the Wiley ‐ The University of Queensland agreement via the Council of Australian University Librarians.
Martin, P. , Tian, E. , Kumar, S. , & Lizarondo, L. (2022). A rapid review of the impact of COVID‐19 on clinical supervision practices of healthcare workers and students in healthcare settings. Journal of Advanced Nursing, 00, 1–9. 10.1111/jan.15360
Contributor Information
Priya Martin, Email: priya.martin@uq.edu.au, @drprimart.
Saravana Kumar, @EvidenceBytes.
Lucylynn Lizarondo, @lucylizarondo20.
DATA AVAILABILITY STATEMENT
Data can be obtained by contacting the first author via email
REFERENCES
- Bourke, L. , Hellwege, B. , Jessup, B. , Heaney, S. , Sheepway, L. , Hoang, H. , Podubinski, T. , Farthing, A. , Rasiah, R. , Fitzroy, R. , Obamiro, K. , Jatrana, S. , Argus, G. , & Knight, S. (2021). The impact of COVID‐19 on student placements facilitated by university departments of rural health. Australian Rural Health Education Network. Retrieved from https://www.arhen.org.au/wp‐content/uploads/2021/08/Impact‐of‐COVID‐19‐on‐Student‐Placements‐February‐2021.pdf
- Cabarkapa, S. , Nadjidai, S. E. , Murgier, J. , & Ng, C. H. (2020). The psychological impact of COVID‐19 and other viral epidemics on frontline healthcare workers and ways to address it: A rapid systematic review. Brain, Behavior, & Immunity ‐ Health, 8, 100144. 10.1016/j.bbih.2020.100144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi, B. , Jegatheeswaran, L. , Minocha, A. , Alhilani, M. , Nakhoul, M. , & Mutengesa, E. (2020). The impact of the COVID‐19 pandemic on final year medical students in the United Kingdom: A national survey. BMC Medical Education, 20(1), 206. 10.1186/s12909-020-02117-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutcliffe, J. , & McFeely, S. (2001). Practice nurses and their 'lived experience' of clinical supervision. British Journal of Nursing (Mark Allen Publishing), 10(5), 312–323. 10.12968/bjon.2001.10.5.5359 [DOI] [PubMed] [Google Scholar]
- Department of Health . (2021). COVID‐19 surge health workforce package. Australian Government. Retrieved from https://www.health.gov.au/initiatives‐and‐programs/covid‐19‐surge‐health‐workforce‐package
- Ducat, W. , Martin, P. , Kumar, S. , Burge, V. , & Abernathy, L. (2016). Oceans apart, yet connected: Findings from a qualitative study on professional supervision in rural and remote allied health services. The Australian Journal of Rural Health, 24(1), 29–35. 10.1111/ajr.12192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garritty, C. , Gartlehner, G. , Kamel, C. , King, V.J. , Nussbaumer‐Streit, B. , Stevens, A. , Hamel, C. , Affengruber, L. (2020). Cochrane rapid reviews. Interim Guidance from the Cochrane Rapid Reviews Methods Group. Retrieved from https://methods.cochrane.org/rapidreviews/sites/methods.cochrane.org.rapidreviews/files/public/uploads/cochrane_rr_‐_guidance‐23mar2020‐final.pdf [DOI] [PMC free article] [PubMed]
- Holton, S. , Wynter, K. , Trueman, M. , Bruce, S. , Sweeney, S. , Crowe, S. , Dabscheck, A. , Eleftheriou, P. , Booth, S. , Hitch, D. , Said, C. M. , Haines, K. J. , & Rasmussen, B. (2021). Immediate impact of the COVID‐19 pandemic on the work and personal lives of Australian hospital clinical staff. Australian Health Review, 45, 656–666. 10.1071/AH21014 [DOI] [PubMed] [Google Scholar]
- Kapila, A. K. , Schettino, M. , Farid, Y. , Ortiz, S. , & Hamdi, M. (2020). The impact of coronavirus disease 2019 on plastic surgery training: The resident perspective. Plastic and Reconstructive Surgery. Global Open, 8(7), e3054. 10.1097/GOX.0000000000003054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law, M. , Stewart, D. , Pollock, N. , Letts, L. , Bosch, J. , & Westmorland, M. (1998). Critical review form – Quantitative studies. McMaster Evidence Review Synthesis Team. Retrieved from https://healthsci.mcmaster.ca/merst
- Martin, P. , & Snowdon, D. (2020). Can clinical supervision bolster clinical skills and well‐being through challenging times? Journal of Advanced Nursing, 76(11), 2781–2782. 10.1111/jan.14483 [DOI] [PubMed] [Google Scholar]
- Martin, P. , Copley, J. , & Tyack, Z. (2014). Twelve tips for effective clinical supervision based on a narrative literature review and expert opinion. Medical Teacher, 36(3), 201–207. 10.3109/0142159X.2013.852166 [DOI] [PubMed] [Google Scholar]
- Martin, P. , Lizarondo, L. , & Kumar, S. (2018). A systematic review of the factors that influence the quality and effectiveness of telesupervision for healthcare workers. Journal of Telemedicine and Telecare, 24(4), 271–281. 10.1177/1357633X17698868 [DOI] [PubMed] [Google Scholar]
- Martin, P. , Lizarondo, L. , Kumar, S. , & Snowdon, D. (2021). Impact of clinical supervision on healthcare organisational outcomes: A mixed methods systematic review. PLoS One, 16(11), e0260156. 10.1371/journal.pone.0260156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin, P. , Tian, E.J. , & Kumar, S. (2021). Impact of the COVID‐19 pandemic on clinical supervision practices of healthcare workers and students in healthcare settings: A rapid review protocol. Open Science Framework. 10.17605/OSF.IO/CSRZ3. [DOI] [PMC free article] [PubMed]
- Melnyk, B. M. , Orsolini, L. , Tan, A. , Arslanian‐Engoren, C. , Melkus, G. D. , Dunbar‐Jacob, J. , Rice, V. H. , Millan, A. , Dunbar, S. B. , Braun, L. T. , Wilbur, J. , Chyun, D. A. , Gawlik, K. , & Lewis, L. M. (2018). A National Study Links Nurses' physical and mental health to medical errors and perceived worksite wellness. Journal of Occupational and Environmental Medicine, 60(2), 126–131. 10.1097/JOM.0000000000001198 [DOI] [PubMed] [Google Scholar]
- Milne, D. L. (2007). An empirical definition of clinical supervision. British Journal of Clinical Psychology, 46(4), 437–447. 10.1348/014466507X197415 [DOI] [PubMed] [Google Scholar]
- Milne, D. L. , & Reiser, R. P. (2020). Supportive clinical supervision. Enhancing well‐being and reducing burnout through restorative leadership. Pavilion Publishing. [Google Scholar]
- Natchaba, N . (2020). Evaluating the effectiveness of clinical supervision in the care coordination workforce (paper 455) [doctoral dissertation, St. John fisher college]. Fisher Digital Publications. Retrieved from https://fisherpub.sjfc.edu/cgi/viewcontent.cgi?article=1464&context=education_etd
- Petrie, K. , Crawford, J. , Baker, S. , Dean, K. , Robinson, J. , Veness, B. G. , Randall, J. , McGorry, P. , Christensen, H. , & Harvey, S. B. (2019). Interventions to reduce symptoms of common mental disorders and suicidal ideation in physicians: A systematic review and meta‐analysis. The Lancet. Psychiatry, 6(3), 225–234. 10.1016/S2215-0366(18)30509-1 [DOI] [PubMed] [Google Scholar]
- Popay J., Roberts H., Sowden A., Petticrew M., Arai L., Rodgers M., Britten N., Roen K., & Duffy S. (2006). Guidance on the Conduct of Narrative Synthesis in Systematic Reviews: A product from the ESRC Methods Programme. Retrieved from https://www.lancaster.ac.uk/media/lancaster‐university/content‐assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1‐April2006.pdf
- Rothwell, C. , Kehoe, A. , Farook, S. F. , & Illing, J. (2021). Enablers and barriers to effective clinical supervision in the workplace: A rapid evidence review. BMJ Open, 11(9), e052929. 10.1136/bmjopen-2021-052929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruitenburg, M. M. , Frings‐Dresen, M. H. , & Sluiter, J. K. (2012). The prevalence of common mental disorders among hospital physicians and their association with self‐reported work ability: A cross‐sectional study. BMC Health Services Research, 12, 292–298. 10.1186/1472-6963-12-292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt, T. , Ripp, J. , & Trockel, M. (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID‐19 pandemic. JAMA, 323(21), 2133–2134. 10.1001/jama.2020.5893 [DOI] [PubMed] [Google Scholar]
- Shaukat, N. , Ali, D. M. , & Razzak, J. (2020). Physical and mental health impacts of COVID‐19 on healthcare workers: A scoping review. International Journal of Emergency Medicine, 13(1), 40. 10.1186/s12245-020-00299-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shklarski, L. , & Abrams, A. (2021). Effective supervision during the COVID‐19 pandemic – The transition to remote learning. In Shklarski L. & Abrams A. (Eds.), A contemporary approach to clinical supervision (1st ed., pp. 26–48). Routledge. 10.4324/9781003180883 [DOI] [Google Scholar]
- Shreffler, J. , Petrey, J. , & Huecker, M. (2020). The impact of COVID‐19 on healthcare worker wellness: A scoping review. The Western Journal of Emergency Medicine, 21(5), 1059–1066. 10.5811/westjem.2020.7.48684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snowdon, D. A. , Sargent, M. , Williams, C. M. , Maloney, S. , Caspers, K. , & Taylor, N. F. (2019). Effective clinical supervision of allied health professionals: A mixed methods study. BMC Health Services Research, 20(1), 2. 10.1186/s12913-019-4873-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The EndNote Team . (2013). EndNote. Clarivate Analytics.
- Tricco, A.C. , Langlois, E.V. , & Straus, S.E. , editors. (2017). Rapid reviews to strengthen health policy and systems: A practical guide. World Health Organisation. Retrieved from http://apps.who.int/iris/bitstream/handle/10665/258698/9789241512763‐eng.pdf?sequence=1 [Google Scholar]
- Turnbull, C. , Grimmer‐Somers, K. , Kumar, S. , May, E. , Law, D. , & Ashworth, E. (2009). Allied, scientific and complementary health professionals: A new model for Australian allied health. Australian Health Review, 33(1), 27–37. 10.1071/AH090027 [DOI] [PubMed] [Google Scholar]
- Ulenaers, D. , Grosemans, J. , Schrooten, W. , & Bergs, J. (2021). Clinical placement experience of nursing students during the COVID‐19 pandemic: A cross‐sectional study. Nurse Education Today, 99, 104746. 10.1016/j.nedt.2021.104746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veritas Health Innovation . (2021). Covidence systematic review software, web‐based software, Melbourne, Australia. https://www.covidence.org
- Wang, H. , Zhou, X. , Jia, X. , Song, C. , Luo, X. , Zhang, H. , Wu, H. , & Ye, J. (2021). Emotional exhaustion in front‐line healthcare workers during the COVID‐19 pandemic in Wuhan, China: The effects of time pressure, social sharing and cognitive appraisal. BMC Public Health, 21(1), 829. 10.1186/s12889-021-10891-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wanis, C. , Aulakh, G. , Wilson, G. , & Moore, R. (2021). Impact of COVID‐19 on dental specialty training in the UK: The trainee perspective. Faculty Dental Journal, 12(1), 23–29. 10.1308/rcsfdj.2020.124 [DOI] [Google Scholar]
- Zoia, C. , Raffa, G. , Somma, T. , Della Pepa, G. M. , La Rocca, G. , Zoli, M. , Bongetta, D. , De Divitiis, O. , & Fontanella, M. M. (2020). COVID‐19 and neurosurgical training and education: An Italian perspective. Acta Neurochirurgica, 162(8), 1789–1794. 10.1007/s00701-020-04460-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1
Supplementary Table 2
Supplementary Table 3
Supplementary Table 4
Data Availability Statement
Data can be obtained by contacting the first author via email


