Abstract
Background
The potential for work to be a risk factor for coronavirus disease 2019 (COVID‐19) was recognized early in the pandemic based on the likelihood of work‐related differences in exposures to COVID‐19 in different occupations. Due to intense demands of the pandemic, implementation of recommendations to collect information on occupation in relation to COVID‐19 has been uneven across the United States. The objective of this study was to investigate COVID‐19 test positivity by occupation.
Methods
We analyzed data collected from September 8 to November 30, 2020, by the Delphi Group at Carnegie Mellon University US COVID‐19 Trends and Impact Survey, offered daily to a random sample of US‐based Facebook users aged 18 years or older, who were invited via a banner in their news feed. Our focus was ever testing positive for COVID‐19 in respondents working outside the home for pay in the past 4 weeks.
Results
The major occupational groups of “Production", "Building and grounds cleaning and maintenance,” “Construction and extraction,” “Healthcare support,” and “Food preparation and serving” had the five highest test positivity percentages (16.7%–14.4%). Highest detailed occupational categories (28.6%–19.1%) were “Massage therapist,” “Food processing worker,” “Bailiff, correctional officer, or jailer,” “Funeral service worker,” “First‐line supervisor of production and operating workers,” and “Nursing assistant or psychiatric aide.” Differences in test positivity by occupation remained after adjustment for age, gender, and pre‐existing medical conditions.
Conclusion
Information on differences in test positivity by occupation can aid targeting of messaging for vaccination and testing and mitigation strategies for the current and future respiratory infection epidemics and pandemics. These results, obtained before availability of COVID‐19 vaccines, can form a basis for comparison to evaluate impacts of vaccination and subsequent emergence of viral variants.
Keywords: COVID‐19, detailed occupation, major occupation, test positivity
1. INTRODUCTION
The potential for work to be a risk factor for coronavirus disease 2019 (COVID‐19) was recognized early in the pandemic based on the likelihood of work‐related differences in exposures to COVID‐19 in different occupations. To better understand and mitigate risk, the Occupational Health Surveillance Subcommittee of the Council of State and Territorial Epidemiologists issued “Recommended interim guidance for collecting employment information about COVID‐19 cases” on April 22, 2020. 1 The document recommended collecting at least the main occupation and industry in the last 14 days for each COVID‐19 case. Government agencies provided similar recommendations. For example, the National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention (CDC) posted a science blog, entitled “Collecting occupation and industry data in public health surveillance systems for COVID‐19.” 2 This blog emphasized that “collecting information about the jobs of all workers with COVID‐19 would help the public health community identify work‐related outbreaks and evaluate risks among various groups of workers.” Also, online CDC guidance includes the recommendation to collect occupation and workplace for employed cases as relevant risk factors for COVID‐19. 3
Due to intense demands of the pandemic, including demands to collect other types of COVID‐19 surveillance data, implementation of these recommendations has been uneven across the United States. However, some jurisdictions have collected occupational information from COVID‐19 cases. For example, researchers used data from 10,850 Washington state COVID‐19 cases up to June 16, 2020. 4 The five major occupational groups with the highest prevalence estimates (in descending order) were “Farming, fishing, and forestry,” “Personal care and service,” “Healthcare practitioners and technical,” “Healthcare support,” and “Building and grounds cleaning and maintenance.”
NIOSH developed a COVID‐19 research agenda to address occupational health research gaps in the context of the ongoing response which was published in March 2021. Goal 3.1 of this study agenda is to “track and characterize SARS‐CoV‐2 infections in US workers by industry and occupation groups in a systematic and representative way so that reliable estimates of infection can be generated.” 5 Given the uneven collection of industry and occupation data by public health surveillance systems, we took the opportunity to analyze data from the Delphi Group at Carnegie Mellon University (CMU) US COVID‐19 Trends and Impact Survey, in partnership with Facebook (Delphi US CTIS) on COVID‐19 test results in relation to occupation for the entire country. The Delphi Group has the goal of developing the theory and practice of epidemic tracking and forecasting. Since April 2020, in collaboration with Facebook and a consortium of universities and public health officials, the Delphi Group has conducted the CTIS to monitor the spread and impact of the COVID‐19 pandemic in the United States. This survey is offered daily to a random sample of US‐based Facebook users aged 18 years or older, who are invited via a banner in their news feed. 6 , 7
This current report focuses on the following objectives related to the pandemic in the fall of 2020 before COVID‐19 vaccines were available and before widespread circulation of subsequent variants of SARS‐CoV‐2: (1) to investigate test positivity estimates from the start of the spread of the SARS‐CoV‐2 virus in the United States up to the end of November 2020 by major and detailed occupational groups; (2) to investigate odds of ever having a positive COVID‐19 test for major occupational groups after adjusting for gender, age, and pre‐existing conditions.
2. METHODS
2.1. Study population
Data consisted of participant responses from September 8 to November 30, 2020, to the Delphi US CTIS. 6 , 7 Since the analyses focused on reports of ever testing positive for COVID‐19, the results pertain to cumulative test positivity from the start of the pandemic to the end of November 2020. Delphi US CTIS was launched in April 2020, but questions on occupation were added in September 2020. Briefly, each day, Facebook invites a random sample of its active users 18 years or older via a banner in their Facebook Feed. If invitees agree to take the survey, they are routed to the Qualtrics web‐based survey platform hosted by the Delphi Group at CMU. The survey has changed over time but has included questions on demographics, symptoms, pre‐existing medical conditions, COVID‐19 testing, social distancing, vaccination, vaccine hesitancy, schooling, mental health, economic security, and occupation. The Delphi Group at CMU makes deidentified data available to academic researchers, including survey weights provided by Facebook. 7 Facebook does not receive survey responses to weight the data. Instead, a unique random ID is created by Facebook when the invitations are sent out. The survey responses are linked to these IDs. The Delphi Group sends Facebook lists of IDs of participants in the survey to use in creating weights. Details of the weighting methods used by Facebook are given in the “User guide for the COVID‐19 trends and impact survey weights” on Delphi's Epidata API COVID‐19 Trends and Impact Survey website. 7 In summary, Facebook generates survey weights to adjust for nonresponse error and noncoverage error. First, inverse propensity score weighting is used to adjust for nonresponse error and make the sample more representative of the sampling frame of Facebook users in the United States. Nonresponse is modeled using internal Facebook data such as age and gender and geographical variables to improve geographic representation, as well as other attributes which Facebook does not describe in detail but believe correlate to demographics to which Facebook does not have access. To correct for noncoverage, post‐stratification weights are generated to improve representation of the general US adult population. Post‐stratification over state, age, and gender is carried out using benchmarks obtained from the Current Population Survey 2018 March Supplement with the nonresponse weights as inputs. The final weights for each participant in the sample for each day denote the number of adults in the general population represented by each participant.
2.2. Description of variables
Questions used in the current analyses addressed age, gender, pre‐existing medical conditions, self‐reported COVID‐19 testing (testing type not specified) and test results, work status in the past 4 weeks, whether the work was from home or away from home, and occupation.
2.2.1. Gender
Gender was coded as male, female, and other (nonbinary, prefer to self‐describe, prefer not to answer).
2.2.2. Pre‐existing medical conditions
Participants were asked if they were ever diagnosed with specific health conditions (asthma, autoimmune disorder, cancer, chronic obstructive pulmonary disease, diabetes type 1, diabetes type 2, heart disease, high blood pressure, kidney disease, and weakened/compromised immune system).
2.2.3. Ever tested for COVID‐19
Participants were asked if they had ever been tested for COVID‐19. There were no questions on what type of test was used.
2.2.4. Ever tested positive for COVID‐19
Participants were coded as ever testing positive if they indicated they had ever been tested and reported testing positive. Answers of “I don't know” were coded as “No.”
2.2.5. Work questions
There were two questions on work. (1) In the past 4 weeks, did you do any kind of work for pay? (2) Was any of your work for pay in the last 4 weeks outside your home?
2.2.6. Occupation
Participants who had worked in the past 4 weeks were asked “Please select the occupational group that best fits the main kind of work you were doing in the last 4 weeks.”
There were 15 major occupational groups listed here and “other.” If “other” was chosen, the participant was asked “Please select the occupational group that best fits the main kind of work you were doing in the last 4 weeks” and could select from an additional eight major occupational groups as well as a 9th choice of “any other occupational group.” Thus, there were a total of 23 named major occupational groups, plus the “any other” category. Participants who selected one of the 15 major occupational groups were then asked, “Please select that job type that best fits the main kind of work you were doing in the last 4 weeks.” There were from 4 to 11 more detailed occupations listed for these 15 major occupational groups for a total of 118 detailed occupations. The choices for occupations at the first of the two levels are based on 23 major occupational groups in the US Bureau of Labor Statistics 2018 Standard Occupational Classification (SOC) system, and at the second level on more detailed occupational categories within 15 of the major occupational groups. 8 The more detailed occupational categories were based on individual 2018 SOC minor and broad occupational groups and detailed occupations and combinations of these groupings.
2.3. Statistical methods
Individual‐level data were housed and analyzed at the collaborating University. All analyses on individual‐level data were conducted in R version 3.6+ using the survey and GDAtools packages. Some analyses on summary data were conducted using JMP version 15.1.0. We present unweighted results for counts and weighted results for percentages. The 95% confidence interval (95% CI) for percentages was calculated using a maximum likelihood‐based CI interval. 9 In the descriptive tables, entries with missing data on variables in a row or a column of the table were omitted (in both the weighted percentage and the count reported). This led to different denominators across the cells in these tables. Multivariable logistic regression was conducted to better understand the odds of participants working outside the home ever testing positive for COVID‐19 in relation to major occupation group, with adjustment for gender, age, and pre‐existing conditions. Each of the pre‐existing conditions was entered into the multivariable model as a Yes/No variable, thus respondents without a particular pre‐existing condition were the reference group for that particular pre‐existing condition. Due to the use of survey weights, quasi‐binomial logistic models were run that adjusted the variance for weighting.
3. RESULTS
There were 2,965,370 responses by adults ≥18 years to the survey from September 8 to November 30, 2020. Of these participants, 1,433,840 reported working for pay in the past 4 weeks. Among the working participants, 991,619 reported working outside the home. The major occupational groups of “Computer and mathematical” and “Business and financial operations” had the lowest prevalence for working outside the home of 28% and 40%, respectively (Supporting Information: Figure S1), while 91% to 93% of respondents in the five major occupational groups of “Building and grounds cleaning and maintenance,” “Protective service,” “Construction and extraction,” “Installation, maintenance, and repair,” and “Transportation and material moving” reported working outside the home (Supporting Information: Figure S1). Over the major occupational groups, COVID‐19 test positivity showed a trend to increase with percentage of participants working outside the home (Supporting Information: Figure S1). The Pearson correlation between the percent of an occupational group working outside the home and ever test positivity was 0.76 (p < 0.01).
Demographics of the working participants indicate that the group that had worked outside the home in the past 4 weeks had a higher percentage of males (51.1% vs. 44.3%) but were similar in age distribution and in prevalence of pre‐existing conditions compared to those working from home. The most prevalent pre‐existing conditions were high blood pressure, asthma, and type 2 diabetes (Supporting Information: Table S1). Of participants who had worked in the past 4 weeks, 40.4% reported ever being tested for COVID‐19, and 12.8% of those tested reported a positive test result. For those working from home, these values were 37.4% tested and 11.3% positive, while for those working outside the home these values were 41.4% tested and 13.2% positive. In participants working outside the home, test positivity was lower in those 65 years or older, and highest for those with pre‐existing Type 1 diabetes, Type 2 diabetes, or kidney disease (Table 1).
Table 1.
Percent of 991,619 respondents (from September 8 through November 30, 2020) working outside the home ever tested for COVID‐19 and test positivity, by gender, age, and pre‐existing conditions
| Ever tested for COVID‐19 | COVID‐19 test positivity | |||
|---|---|---|---|---|
| Category | N | Weighted % (95% CI) | N | Weighted% (95% CI) |
| Working outside the home | 410,800 | 41.4 (41.3, 41.6) | 51,073 | 13.2 (13.0, 13.3) |
| Gender | ||||
| Male | 137,800 | 37.9 (37.7, 38.1) | 17,046 | 13.2 (12.9, 13.4) |
| Female | 264,152 | 45.5 (45.4, 45.7) | 32,707 | 13.0 (12.9, 13.2) |
| Other | 8654 | 39.0 (38.2, 39.2) | 1294 | 16.4 (15.2, 17.6) |
| Age (years) | ||||
| 18–44 | 198,244 | 42.9 (42.7, 43.1) | 25,097 | 13.3 (13.1, 13.5) |
| 45–64 | 176,668 | 40.1 (39.9, 40.3) | 22,278 | 13.4 (13.2, 13.6) |
| 65 or older | 35,619 | 38.1 (37.7, 38.5) | 3674 | 11.1 (10.7, 11.5) |
| Pre‐existing conditions | ||||
| Cancer | 17,114 | 46.2 (45.6, 46.8) | 2067 | 14.3 (13.6, 15.0) |
| Heart disease | 16,701 | 44.9 (44.3, 45.5) | 2306 | 15.7 (15.0, 16.5) |
| High blood pressure | 110,176 | 42.4 (42.1, 42.6) | 14,421 | 13.9 (13.6, 14.2) |
| Asthma | 68,973 | 46.7 (46.3, 47.0) | 8153 | 12.7 (12.3, 13.0) |
| Chronic lung disease such as COPD or emphysema | 11,257 | 46.1 (45.3, 46.9) | 1,520 | 16.4 (15.5, 17.4) |
| Kidney disease | 6957 | 46.9 (45.8, 47.9) | 1165 | 20.4 (19.2, 21.8) |
| Autoimmune disorder like rheumatoid arthritis or Crohn's disease | 28,930 | 48.6 (48.1, 49.1) | 3452 | 13.6 (13.1, 14,2) |
| Type 1 diabetes | 4949 | 44.9 (43.7, 46.1) | 1090 | 25.6 (23.9, 27.2) |
| Type 2 diabetes | 36,736 | 44.4 (44.0, 44.8) | 5705 | 16.9 (16.4, 17.4) |
| Weakened or compromised immune system | 24,779 | 52.1 (51.5, 52.7) | 3177 | 14.3 (13.7, 14.8) |
| None of the above pre‐existing conditions | 205,180 | 39.5 (39.4, 39.7) | 25,776 | 13.3 (13.1, 13.5) |
Note: Actual participant numbers given but weights were applied to obtain adjusted percentages. The denominators for COVID‐19 test positivity are the number of respondents ever tested for COVID‐19.
Abbreviations: COPD, chronic obstructive pulmonary disease; COVID‐19, coronavirus disease 2019; 95% CI, 95% confidence interval.
The percent ever tested for respondents working outside the home ranged from 28.2% for “Farming, fishing, and forestry” to 57.3% for “Healthcare practitioners and technicians” (Table 2), with a median value of 40.3% for the 23 major occupational groups. For the 23 major occupational groups, the Pearson correlation between percent of respondents ever tested and test positivity was −0.21 and was not statistically significant (p = 0.328).
Table 2.
Prevalence of ever been tested for COVID‐19 and test positivity by major occupational groups for participants (from September 8 through November 30, 2020) working outside the home in the last 4 weeks
| SOC code | Major occupational group | Respondents | Ever tested | COVID‐19 test positivity | ||
|---|---|---|---|---|---|---|
| N | N | Weighted % (95% CI) | N | Weighted % (95% CI) | ||
| 51‐0000 | Production | 38,219 | 13,445 | 35.6 (35.0, 36.3) | 2143 | 16.7 (15.8, 17.6) |
| 37‐0000 | Building and grounds cleaning and maintenance | 21,846 | 7593 | 34.9 (34.0, 35.7 | 1053 | 15.5 (14.3, 16.3) |
| 47‐0000 | Construction and extraction | 22,063 | 7378 | 34.0 (33.2, 34.8) | 1056 | 15.0 (13.9, 16.1) |
| 31‐0000 | Healthcare support | 53,326 | 28,998 | 56.0 (55.4, 56.5) | 4136 | 14.9 (14.3, 15.4) |
| 35‐0000 | Food preparation and serving related | 50,179 | 20,121 | 40.8 (40.1, 41.3) | 2801 | 14.4 (13.7, 15.1) |
| 45‐0000 | Farming, fishing, and forestry | 7673 | 2137 | 28.2 926.9, 29.6) | 281 | 14.3 (12.4, 16.4) |
| 33‐0000 | Protective service | 15,230 | 7343 | 49.3 (48.2, 50.3) | 1030 | 14.2 (13.1, 15.2) |
| 29‐0000 | Healthcare practitioners and technicians | 112,385 | 64,066 | 57.3 (56.9, 57.7) | 8574 | 14.0 (13.6, 14.3) |
| 49‐0000 | Installation, maintenance, and repair | 31,787 | 101,03 | 32.0 (31.4, 32.7) | 1321 | 14.0 (13.1, 14.9) |
| 41‐0000 | Sales and related | 97,821 | 34,392 | 36.0 (35.5, 36.4) | 4408 | 13.5 (13.0, 14.0) |
| 53‐0000 | Transportation and material moving | 41,933 | 13,608 | 32.5 (31.9, 33.0) | 1794 | 13.5 (12.8, 14.2) |
| 21‐0000 | Community and social service | 43,613 | 20,950 | 49.3 (48.7, 49.9) | 2405 | 12.4 (11.8, 13.1) |
| 39‐0000 | Personal care and service | 23,339 | 9359 | 41.4 (40.6, 42.2) | 1108 | 12.1 (11.2, 13.0) |
| 43‐0000 | Office and administrative support | 106,916 | 41,628 | 40.3 (40.0, 40.7) | 4871 | 12.0 (11.6, 12.5) |
| 13‐0000 | Business and financial operations | 18,512 | 6964 | 38.9 (38.0, 39.9) | 771 | 11.8 (10.7, 12.8) |
| 11‐0000 | Management | 31,348 | 12,423 | 39.8 (39.1, 40.3) | 1377 | 11.6 (10.9, 12.3) |
| 25‐0000 | Education, training, and library | 101,803 | 43,072 | 43.6 (43.2, 44.0) | 4369 | 10.8 (10.3, 11.2) |
| 23‐0000 | Legal | 12,632 | 5657 | 45.8 (44.7, 46.9) | 540 | 10.4 (9.3, 11.5) |
| 17‐0000 | Architecture and engineering | 11,405 | 4067 | 36.4 (35.3, 37.6) | 385 | 10.0 (8.8, 11.2) |
| 55‐0000 | Military | 5631 | 2502 | 46.2 (44.3, 48.1) | 238 | 10.0 (8.3, 11.9) |
| 15‐0000 | Computer and mathematical | 12,694 | 4576 | 37.2 (36.1, 38.3) | 385 | 8.5 (7.5, 9.6) |
| 27‐0000 | Arts, design, entertainment, sports, and media | 24,017 | 10,287 | 45.1 (44.2, 46.0) | 836 | 8.3 (7.6, 9.0) |
| 19‐0000 | Life, physical, and social science | 8296 | 3839 | 47.7 (46.3, 49.2) | 237 | 6.1 (5.2, 7.0) |
| Any other occupational group | 94,776 | 34,820 | 37.3 (36.8, 37.7) | 4659 | 14.5 (14.0, 15.0) | |
| No answer to major occupational group | 4175 | 1472 | 35.6 (33.7, 37.5) | 295 | 22.1 (19.2, 25.1) | |
| Total | 991,619 | 410,800 | 41.4 (41.3, 41.6) | 51,073 | 13.2 (13.0, 13.3) | |
Note: Actual participant numbers given but weights were applied to obtain adjusted percentages. The denominators for COVID‐19 test positivity are the number of respondents ever tested for COVID‐19.
Abbreviations: COVID‐19, coronavirus disease 2019; SOC, Standard Occupational Classification; 95% CI, 95% confidence interval.
The three major occupational groups with the highest test positivity were “Production” (16.7%), “Building and grounds cleaning and maintenance” (15.5%), and “Construction and extraction” (15.0%). “Healthcare support” and “Healthcare practitioners and technicians” were the 4th and 8th highest with test positivity of 14.9% and 14.0% respectively. The three occupational groups with the lowest test positivity were “Life, physical, and social science” (6.1%), “Arts, design, entertainment, sports, and media” (8.3%), and “Computer and mathematical” (8.5%).
A multivariable logistic model of ever tested positive for COVID‐19 in participants working outside the home in the past 4 weeks in relation to major occupational group was adjusted for gender, age, and pre‐existing conditions (Supporting Information: Table S2). The older age groups had a statistically lower odds for a positive test than the 18–44 age group, with the 45–65 age group having an odds ratio (OR) of 0.96 (95% CI: 0.93, 0.98) and the over 65 group having an OR of 0.72 (95% CI: 0.69, 0.76). Statistically significant increases in the odds of a positive test were found for Type 1 diabetes (OR: 1.98, 95% CI: 1.83, 2.16), Type 2 diabetes (OR: 1.35, 95% CI: 1.30, 1.40), and kidney disease (OR: 1.35, 95% CI: 1.25, 1.45). Decreases in the odds of a positive test were found for asthma (OR: 0.91, 95% CI: 0.87, 0.94) and autoimmune disorders like rheumatoid arthritis or Crohn's disease (OR: 0.95, 95% CI: 0.91, 0.99). After adjusting for sex, age, and pre‐existing conditions, there were differences between occupations on testing positive for COVID‐19. “Office and administrative support” was used as the reference group as it was a large group that had a test positivity percent near the middle of the range for the 23 major occupational groups (Table 2). Eleven occupational groups had an increased odds of testing positive with the three highest being “Production” (OR: 1.45, 95% CI: 1.34, 1.56), “Building and grounds cleaning and maintenance” (OR: 1.34, 95% CI: 1.21, 1.48), and “Construction and extraction” (OR: 1.28, 95% CI: 1.16, 1.41). There were seven occupational groups with a lower odds of testing positive compared to “Office and administrative support,” with the three with the largest decreased odds of ever testing positive being “Life, physical, and social science” (OR: 0.48, 95% CI: 0.40, 0.56), “Arts, design, entertainment, sports, and media” (OR: 0.66, 95% CI: 0.60, 0.73), and “Computer and mathematical” (OR: 0.68, 95% CI: 0.59, 0.78).
3.1. Detailed occupational categories
There were 784,477 respondents who reported working outside the home in the 15 major occupational groups with follow‐up details on detailed occupational categories. Of the 118 detailed occupational categories, five had fewer than 10 participants reporting ever testing positive, leaving 113 that were ranked by ever testing positivity. The first and third quartile of test positivity was 11.9% and 15.1%, respectively. The distribution of these 113 detailed occupational categories for test positivity within their major occupational groups ordered left to right by increasing value of test positivity for the overall major occupational group is shown in Figure 1. The range of test positivity within the 15 major occupational groups differed considerably from a minimum of 1.7 percentage points for “Sales and related,” to a maximum of 20 percentage points for “Healthcare support,” with a median value of 4.9 percentage points for the 15 major occupational categories. Major occupational groups having detailed occupational categories in both the upper and the lower quartiles of test positivity included “Personal care and service,” “Healthcare practitioners and technicians,” “Installation, maintenance, and repair,” “Protective service,” “Food preparation and serving related,” and “Healthcare support.”
Figure 1.
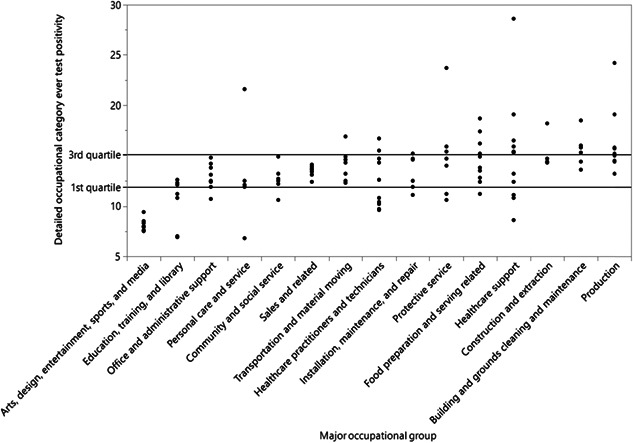
For respondents working outside the home, the figure shows the distribution of 113 detailed occupational categories for ever test positivity within their major occupational groups ordered left to right by increasing value of the overall major occupational group test positivity. Reference lines on the graph are at the first quartile (11.9%) and the third quartile (15.1%) of detailed occupational categories test positivity percentages.
The 28 detailed occupational categories in the upper quartile of COVID‐19 test positivity (from 28.6% to 15.2%) were in 10 of the 15 major occupations, but 22/28 (78.6%) of them were in the five major occupational groups of “Healthcare support,” “Production,” “Protective services,” “Food preparation and serving related,” and “Building and grounds cleaning and maintenance” (Table 3). The 29 detailed occupational categories in the lowest quartile of COVID‐19 test positivity and full details of the test positivity for detailed occupational categories within the 15 major occupational groups are given in Supporting Information: Tables S3 and S4.
Table 3.
Twenty‐eight detailed occupational categories in the upper quartile of ever testing positive for COVID‐19 out of 113 categories in 15 major occupational groups for participants (from September 8 through November 30, 2020) working outside the home in the last 4 weeks
| Major occupational group | Detailed occupational category | Ever tested N | Test positivity N, weighted % (95% CI) | |
|---|---|---|---|---|
| Healthcare support | Massage therapist | 89 | 20 | 28.6 (17.9, 41.2) |
| Production | Food processing worker | 1102 | 244 | 24.2 (20.8, 27.9) |
| Protective service | Bailiff, correctional officer, or jailer | 587 | 131 | 23.7 (18.6, 29.3) |
| Personal care and service | Funeral service worker | 55 | 13 | 21.6 (11.1, 35.4) |
| Production | First‐line supervisor of production and operating workers | 2338 | 382 | 19.1 (16.3, 22.1) |
| Healthcare support | Nursing assistant or psychiatric aide | 4326 | 811 | 19.1 (17.6, 20.7) |
| Food preparation and serving related | Bartender | 1711 | 297 | 18.7 (15.5, 22.2) |
| Building and grounds cleaning and maintenance | Maid or housekeeping cleaner | 1029 | 160 | 18.5 (15.5, 21.7) |
| Construction and extraction | Any extraction worker in oil, gas, mining, or quarrying | 1001 | 164 | 18.2 (15.2, 21.4) |
| Food preparation and serving related | Dishwasher | 366 | 57 | 17.4 (12.2, 23.5) |
| Transportation and material moving | Rail transportation worker (including railway, subway, and streetcar operator) | 347 | 65 | 16.9 (12.9, 21.5) |
| Healthcare practitioners and technicians | Licensed practical or licensed vocational nurse | 6550 | 1086 | 16.7 (15.6, 17.8) |
| Healthcare support | Occupational therapy or physical therapist assistant or aide | 382 | 64 | 16.5 (12.5, 21.1) |
| Food preparation and serving related | Waiter or waitress | 3070 | 459 | 16.2 (14.3, 18.1) |
| Building and grounds cleaning and maintenance | Grounds maintenance worker | 1089 | 132 | 16.0 (12.7, 19.6) |
| Protective service | Detective or criminal investigator | 593 | 55 | 15.9 (11.9, 20.5) |
| Healthcare support | Medical assistant | 1954 | 288 | 15.9 (13.6, 18.5) |
| Building and grounds cleaning and maintenance | Any other building and grounds cleaning or maintenance worker | 2070 | 289 | 15.8 (13.4, 18.2) |
| Production | Any other production worker | 4912 | 754 | 15.8 (14.5, 17.2) |
| Production | Any other textile, apparel, or furnishings worker | 284 | 44 | 15.7 (10.7, 21.9) |
| Healthcare practitioners and technicians | Any health technologist or technician (including hospital laboratory scientist and pharmacy technician) | 13,145 | 1919 | 15.5 (14.5, 16.5) |
| Healthcare support | Home health or personal care aide (including in‐home caregivers) | 5212 | 744 | 15.4 (14.0, 16.8) |
| Protective service | Police or sheriff officer | 1341 | 188 | 15.4 (13.1, 17.9) |
| Healthcare support | Dental assistant | 346 | 51 | 15.3 (10.5, 21.1) |
| Building and grounds cleaning and maintenance | First‐line supervisor of housekeeping or janitorial workers | 799 | 119 | 15.3 (12.4, 18.5) |
| Installation, maintenance, and repair | First‐line supervisor of mechanics, installers, or repairers | 1179 | 166 | 15.2 (12.8, 17.8) |
| Food preparation and serving related | Host or hostess at a restaurant, lounge, or coffee shop | 718 | 94 | 15.2 (11.7, 19.2) |
| Production | Printing worker | 401 | 63 | 15.2 (11.4, 19.5) |
Note: Actual participant numbers given but weights applied to obtain adjusted percentages. The denominators for COVID‐19 test positivity are the number of respondents ever tested for COVID‐19.
Abbreviations: COVID‐19, coronavirus disease 2019; 95% CI, 95% confidence interval.
4. DISCUSSION
This study is novel in that it presents an account of COVID‐19 test positivity across the United States by major occupation groups and detailed occupational categories. Since the Delphi US CTIS survey asked if respondents had ever tested positive for COVID‐19, the test positivity estimates are from the start of the spread of the SARS‐CoV‐2 virus in the United States up to the end of November 2020, during a period when COVID‐19 vaccines were not yet available in the United States. We focused on respondents who had worked outside the home since these workers have a higher risk for exposure and transmission of the SARS‐CoV‐2 virus. 10 , 11 , 12 Indeed the current analysis indicated that across the major occupational groups, COVID‐19 test positivity showed a trend to increase with percentage of participants working outside the home.
Higher test positivity was found in a number of detailed occupations within “Healthcare support,” “Production,” “Protective services,” “Food preparation and serving related,” and “Building and grounds cleaning and maintenance.” Many of these occupations require working in close physical proximity indoors or outdoors, 13 interacting with the public, 14 or have high proportions of Black or Hispanic workers who have experienced a higher risk of COVID‐19 and severe illness. 13
The current results on higher COVID‐19 test positivity for workers in healthcare, production, protective services, and construction are consistent with a number of previously published findings such as COVID‐19 occurrence in healthcare workers, 15 , 16 and COVID‐19 outbreaks in meat and poultry processing workers, 17 jail/prison/correctional facility staff, 18 and construction workers. 19 Of note, the current analysis test positivity of 10.0% for the Military, which was one of the five lowest of the 23 major occupational groups, was quite similar to the reported 10.4% test positivity for 2020 for all active components of the US military. 20
In a study reporting on COVID‐19 associated hospitalizations among healthcare personnel using data from 13 states from March through May 2020, nurses and nursing assistants accounted for 36.3% of hospitalized personnel. 21 Although there was no information on hospitalization for COVID‐19 in the current study using the Delphi US CTIS data, the test positivity percentages for COVID‐19 up to the end of November 2020 for nurses and nursing assistants were among the highest for healthcare personnel. A recent study of COVID‐19 test positivity using surveillance data from the California severe acute respiratory syndrome coronavirus 2 and respiratory virus sentinel surveillance system from sentinel outpatient testing sites in 10 counties throughout California, found that several occupational groups with high proportions of essential workers showed some evidence of higher test‐positivity. 22 These higher‐risk occupations were consistent with mortality data on workers in California. 23 Furthermore, they were consistent with findings from the current study for workers across the United States. Also, in agreement with the current study findings, the California investigators found that pre‐existing diabetes was associated with increased test positivity and asthma was associated with a decrease in test positivity. This protective effect of asthma on COVID‐19 test positivity has also been reported by researchers in Israel who studied test positivity in over 37,000 members of a nationwide health maintenance organization. 24 It is not fully understood why asthma seems to have a protective effect on COVID‐19 infection and severe disease. One possible mechanism is the reduction of angiotensin‐converting enzyme‐2, the host cell entry receptor for SARS‐CoV‐2 in people with asthma. 25 In the current study older workers had lower test positivity. It is possible that older workers were aware of their risk for severe disease and made efforts to avoid exposure both at work and outside of work. A nationwide cross‐sectional survey of 5203 adults in the United States in April and May of 2020 included questions on COVID‐19 testing and test positivity. In a multivariable logistic model on reporting a positive COVID‐19 test, the odds of testing positive declined with age. The authors hypothesized that healthier older people may have been more likely to participate, and younger participants may have been more likely to congregate in social settings, increasing the chances of exposure to SARS‐CoV‐2. 26
This study has several limitations. First, even after weighting the data, the respondents may not have represented the general US population. For example, a recent publication reported that Delphi US CTIS participants were more likely to have greater than a high school education and to be female than the general US population based on results from the US Census Bureau's American Community Survey. 6 Participation bias might lead to inaccurate population estimates, but such bias might have less effect when making comparison among different subgroups of survey respondents. Second, using test positivity cannot be interpreted as population prevalence. Respondents not reporting being tested may have not been infected or been infected and not tested. Furthermore, workers in different occupations may have had different access to testing over time. Some occupations, for example, healthcare, had screening testing programs which included asymptomatic or unexposed workers which may have led to lower positivity rates. Although there were differences in percent tested among the occupational groups, the correlation between the percent tested and the percent positive was low. Despite limitations, COVID‐19 test positivity rates have been extensively used in the United States by the CDC and other public health authorities to help understand the spread of the disease in communities and aid in targeting mitigation activities. Furthermore, in the discussion, we showed that our findings are consistent with those of other studies that have used different metrics to define occupational risk of COVID‐19. Third, COVID‐19 testing, and test results were self‐reported, and there were no details on what type of test was used which could lead to misclassification. Nevertheless, Delphi US CTIS estimates of state‐specific rates of the proportion of adults reporting that they have ever had a positive test for COVID‐19 were consistent with estimates from the US Census Bureau and CDC. 6 Fourth, occupation may have been misclassified or left missing if respondents did not recognize their occupation in the categories listed which could contribute to random error or information bias. Fifth, respondents were asked about occupation in the past 4 weeks. Some might have had different occupations or not have been working at the time of positive tests obtained earlier. Another possibility is that some respondents were working at the time of a positive COVID‐19 test but not working in the last 4 weeks. These scenarios could contribute to random error or information bias. Lastly, Facebook may send another invitation to the same eligible person 30 days or longer after the last invitation, but participants who take part more than once cannot be identified. Data checks conducted by Facebook indicated that the month‐to‐month re‐engagement in September through November 2020 was approximately 6%–8% and thus reported CIs for test positivity rates should be a little wider.
5. CONCLUSION
Among respondents working outside the home in this large survey from across the United States, there were substantial differences in COVID‐19 test positivity both between and within the 23 major occupational groups over‐and‐above differences due to working from home. Differences in test positivity by occupation reported in the current study were not influenced by COVID‐19 vaccination rate differences by occupation, but would have been influenced by transmission at work, as well as by a number of other factors such as community transmission levels, personal and social factors that affect the risk, and nonpharmaceutical mitigation strategies used both at work and in situations outside of work. 27 , 28
Information on trends in infection risk for detailed occupations and for major occupational groups can help target messaging and future studies on specific working or social conditions contributing to risk of infection and lead to improved mitigation strategies. This is important for both the current COVID‐19 pandemic and for preparedness for any future infectious epidemics or pandemics.
CONFLICTS OF INTEREST
The authors declare that there are no conflicts of interest.
DISCLOSURE BY AJIM EDITOR OF RECORD
John Meyer declares that he has no conflict of interest in the review and publication decision regarding this article.
AUTHOR CONTRIBUTIONS
Jean M. Cox‐Ganser, Paul K. Henneberger, and Caroline P. Groth made substantial contributions to the concept and design of the study. Caroline P. Groth and Garret Guthrie conducted data management. Jean M. Cox‐Ganser and Caroline P. Groth planned and directed the statistical analyses. Caroline P. Groth and Garret Guthrie implemented most statistical analyses. Jean M. Cox‐Ganser, Paul K. Henneberger, and David N. Weissman contributed to interpretation of results. Jean M. Cox‐Ganser drafted the manuscript. All authors provided critical review of the manuscript and approved the final version that was submitted for publication.
ETHICS APPROVAL
This study project was approved by the WVU Institutional Review Board as exempt secondary use of data, and by the CDC Human Research Protections Office as research that involves deidentified data.
DISCLAIMER
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
Supporting information
Supporting information.
ACKNOWLEDGMENTS
This study is based on survey results from Carnegie Mellon University's Delphi Group. The authors thank the adult Facebook users in the United States who completed the Delphi Group COVID‐19 Trends and Impact Survey. The authors' only sources of funding support for this study were their institutional salaries.
Cox‐Ganser JM, Henneberger PK, Weissman DN, Guthrie G, Groth CP. COVID‐19 test positivity by occupation using the Delphi US COVID‐19 trends and impact survey, September–November 2020. Am J Ind Med. 2022;65:721‐730. 10.1002/ajim.23410
DATA AVAILABILITY STATEMENT
Data subject to Data Use Agreements which do not allow sharing of individual‐level data.
REFERENCES
- 1. Council of State and Territorial Epidemiologists . Recommended interim guidance for collecting employment information about COVID‐19 cases. Accessed January 25, 2022. https://cdn.ymaws.com/www.cste.org/resource/resmgr/publications/Guidance_collecting_io_covid.pdf
- 2. Luckhaupt S, Burrer S, de Perio M, Sweeney MH. Collecting occupation and industry data in public health surveillance systems for COVID‐19. NIOSH Science Blog, Centers for Disease Control and Prevention. Accessed January 25, 2022. https://blogs.cdc.gov/niosh-science-blog/2020/06/11/covid-surveillance/ [Google Scholar]
- 3. CDC Guidance . Key information to collect during a case interview. Updated October 21, 2020. Accessed January 25, 2022. https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/keyinfo.html
- 4. Zhang M. Estimation of differential occupational risk of COVID‐19 by comparing risk factors with case data by occupational group. Am J Ind Med. 2021;64:39‐47. 10.1002/ajim.23199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. National Institute for Occupational Safety and Health : NIOSH Disaster Science Responder Research Program COVID‐19 Research Agenda. DHHS (NIOSH) Publication No. 2021‐113. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. 10.26616/NIOSHPUB2021113externalicon [DOI]
- 6. Salomon JA, Reinhart A, Bilinski A, et al. The US COVID‐19 trends and impact survey: continuous real‐time measurement of COVID‐19 symptoms, risks, protective behaviors, testing, and vaccination. Proc Natl Acad Sci USA. 2021;118(51):e2111454118. 10.1073/pnas.2111454118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Delphi's Epidata API COVID‐19 trends and impact survey . Accessed June 7, 2022. https://cmu-delphi.github.io/delphi-epidata/symptom-survey/
- 8. US_BLS . 2018 standard occupational classification system. United States Bureau of Labor Statistics. Accessed January 25, 2022. https://www.bls.gov/soc/2018/major_groups.htm
- 9. Rao JNK, Scott AJ. On chi‐squared tests for multiway contingency tables with cell proportions estimated from survey data. Ann Stat. 1984;12(1):46‐60. [Google Scholar]
- 10. Castillo RC, Staguhn ED, Weston‐Farber E. The effect of state‐level stay‐at‐home orders on COVID‐19 infection rates. Am J Infect Control. 2020;48(8):958‐960. 10.1016/j.ajic.2020.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Baker MG. Nonrelocatable occupations at increased risk during pandemics: United States, 2018. Am J Public Health. 2020;110:1126‐1132. 10.2105/AJPH.2020.305738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Baker MG. Occupational health surveillance as a tool for COVID‐19 prevention. Am J Public Health. 2021;111(6):999‐1001. 10.2105/AJPH.2021.306269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cox‐Ganser JM, Henneberger PK. Occupations by proximity and indoor/outdoor work: relevance to COVID‐19 in all workers and Black/Hispanic workers. Am J Prev Med. 2021;60(5):621‐628. 10.1016/j.amepre.2020.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Goldman N, Pebley AR, Lee K, Andrasfay T, Pratt B. Racial and ethnic differentials in COVID‐19‐related job exposures by occupational standing in the US. PLoS One. 2021;16(9):e0256085. 10.1371/journal.pone.0256085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chou R, Dana T, Buckley DI, Selph S, Fu R, Totten AM. Epidemiology of and risk factors for coronavirus infection in health care workers: a living rapid review. Ann Intern Med. 2020;173(2):120‐136. 10.7326/M20-1632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Baker JM, Nelson KN, Overton E, et al. Quantification of occupational and community risk factors for SARSCoV‐2 seropositivity among health care workers in a large U.S. health care system. Ann Intern Med. 2021;174(5):649‐654. 10.7326/M20-7145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Waltenburg MA, Victoroff T, Rose CE, et al. Update: COVID‐19 among workers in meat and poultry processing facilities―United States, April–May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:887‐892. 10.15585/mmwr.mm6927e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lewis NM, Salmanson AP, Price A, et al. Community‐associated outbreak of COVID‐19 in a correctional facility—Utah, September 2020‐January 2021. MMWR. 2021;70(13):467‐472. 10.15585/mmwr.mm7013a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bushman D, Sekaran J, Jeffery N, et al. Coronavirus disease 2019 (COVID‐19) outbreaks at 2 construction sites‐New York City, October‐November 2020. Clin Infect Dis. 2021;73(suppl 1):S81‐S83. 10.1093/cid/ciab312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Young JM, Stahlman SL, Clausen SS, Bova ML, Mancuso JD. Racial and ethnic disparities in COVID‐19 infection and hospitalization in the active component US military. Am J Public Health. 2021;111:2194‐2220. 10.2105/AJPH.2021.306527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kambhampati AK, O'Halloran AC, Whitaker M, et al. COVID‐19–Associated hospitalizations among health care personnel—COVID‐NET, 13 states, March 1–May 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1576‐1583. 10.15585/mmwr.mm6943e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cooksey GLS, Morales C, Linde L, et al. Severe acute respiratory syndrome coronavirus 2 and respiratory virus sentinel surveillance, California, USA, May 10, 2020‐June 12, 2021. Emerg Infect Dis. 2022;28(1):9‐19. 10.3201/eid2801.211682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chen YH, Glymour M, Riley A, et al. Excess mortality associated with the COVID‐19 pandemic among Californians 18‐65 years of age, by occupational sector and occupation: March through November 2020. PLoS One. 2021;16(6):e0252454. 10.1371/journal.pone.0252454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Green I, Merzon E, Vinker S, Golan‐Cohen A, Magen E. COVID‐19 susceptibility in bronchial asthma. J Allergy Clin Immunol Pract. 2021;9:684‐692.e1. 10.1016/j.jaip.2020.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bonser LR, Eckalbar WL, Rodriguez L, et al. The type 2 asthma mediator IL‐13 inhibits severe acute respiratory syndrome coronavirus 2 infection of bronchial epithelium. Am J Respir Cell Mol Biol. 2022;66:391‐401. 10.1165/rcmb.2021-0364OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Morlock R, Morlock A, Downen M, Shah SN. COVID‐19 prevalence and predictors in United States adults during peak stay‐at‐home orders. PLoS One. 2021;16(1):e0245586. 10.1371/journal.pone.0245586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Leso V, Fontana L, Iavicoli I. Susceptibility to coronavirus (COVID‐19) in occupational settings: the complex interplay between individual and workplace factors. Int J Environ Res Public Health. 2021;18:1030. 10.3390/ijerph18031030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Burdorf A, Porru F, Rugulies R. The COVID‐19 pandemic: one year later – an occupational perspective. Scand J Work Environ Health. 2021;47(4):245‐247. 10.5271/sjweh.3956 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
Data subject to Data Use Agreements which do not allow sharing of individual‐level data.


