Abstract
Background
SARS‐CoV‐2 infection in the age group of 0–17 years contributes to approximately 22% of all laboratory‐confirmed SARS‐CoV‐2 infections. Fortunately, this age group has a lower death rate (0.5 per 100 000) that accounts for only 4% of the total deaths due to COVID‐19. Despite the low mortality rate in the pediatric population, children of minority groups represented 78% of the deaths highlighting the existing disparities in access to health care.
Methods
With the emergence of the more contagious COVID‐19 variants and the relatively slow pace of vaccination among the pediatric population, it is possible to see more cases of significant lung injury and potential for transplantation for the younger age group.
Results
To our knowledge, our patient is the youngest to have undergone lung transplantation for SARS‐CoV‐2.
Conclusion
The case presented unique challenges, particularly in relation to timing for listing and psychosocial support for parents who were his decision makers.
Keywords: COVID‐19, lung transplantation, pediatric
Abbreviations
- VV‐ECMO
veno‐venous extra‐corporeal membrane oxygenation
1. INTRODUCTION
SARS‐CoV‐2 infection in the age group of 0–17 years contributes to approximately 22% of all laboratory‐confirmed SARS‐CoV‐2 infections. 1 Fortunately, this age group has a lower death rate (0.5 per 100 000) that accounts for 4% of the total deaths due to COVID‐19. 1 Despite the low mortality rate in pediatric population, children of minority groups represented 78% of the deaths highlighting the existing disparities in access to health care. 2 With the emergence of the more contagious COVID‐19 variants and relatively slow pace of vaccination among the pediatric population, cases of irreversible lung injury and need for transplantation will remain. To our knowledge, our patient is the youngest to have undergone lung transplantation for SARS‐CoV‐2. The case presented unique challenges, particularly in relation to timing for listing and psychosocial support for parents who were his decision makers.
2. CASE REPORT
A 16‐year‐old Hispanic male patient with history of asthma was diagnosed with COVID‐19 pneumonia in late September 2020. He weighed 164 lbs and was 183 cm tall. The patient was infected with COVID‐19 prior to the availability of vaccination for his age group. He was treated at another hospital with remdesivir, dexamethasone, and empiric antibiotics. Despite supportive care, his condition progressed to requiring mechanical ventilation and ultimately veno‐venous extracorporeal membrane oxygenation (VV‐ECMO). His clinical course was notable for hemoptysis and recurrent bilateral pneumothoraces, requiring chest tube placement. During the next 2 weeks, he was extubated and re‐intubated again but never required a tracheostomy as he was awake throughout, requiring minimal sedation. He was transferred to our facility 1 month later for further management and evaluation for lung transplantation. His ECMO cannula was changed to left subclavian vein (Medtronic 27 Fr) cannula to enable ambulation and was extubated to high flow nasal cannula.
CT thorax was notable for areas of ground‐glass opacification, cystic dilatation, and pulmonary fibrosis (Figure 1). A second course of high‐dose methylprednisolone failed to reverse lung injury, and there was no indication of clinical improvement (refractory oxygen needs and inability to wean off ECMO support). Daily targeted physical therapy improved his conditioning, initially from bed to chair, and finally to being able to ambulate for 50 ft consistently. Throughout this phase, the medical team maintained constant communication with his parents (who made decisions for him), who were vacillating from the decision to assess for transplantation in anticipation of natural recovery. Even as the parents opted to wait for his recovery during the initial period, they were equally skeptical of a protracted stay on ECMO due to risk for complications. Of particular concern for the parents was the modest median 5‐year survival for lung transplant recipients and the significant lifestyle limitations he may experience at his young age. The medical team had to ensure that the parents had a comprehensive understanding of the process before consenting to transplantation. In particular, psychosocial factors including medication adherence were assessed meticulously given the young age of the patient. Following multiple rounds of discussions with family, an expedited pretransplant evaluation was performed and no obvious contra‐indications were identified. He was ultimately listed for bilateral lung transplantation 66 days after being on ECMO. During the period he was listed, his parents required constant reassurance. After 49 days of being listed, he successfully underwent bilateral lung transplantation. The donor was an 18‐year‐old male, DBD (donation after brain death). SARS‐CoV‐2 was ruled out for the donor from both nasopharyngeal swab and bronchial alveolar lavage specimens. A conventional clamshell exposure was used for the surgery. Intraoperatively, we encountered several adhesions mostly limited to the hilum, but hemostasis was achieved without difficulty. The pneumonectomy and implantation proceeded in the standard fashion. The explants demonstrated evidence of lung injury with congestion and areas of cystic dilatation (Figure 2). The ECMO support was decannulated on first postoperative day and he was extubated subsequently. The patient was discharged home 3 weeks after lung transplantation in stable condition.
FIGURE 1.
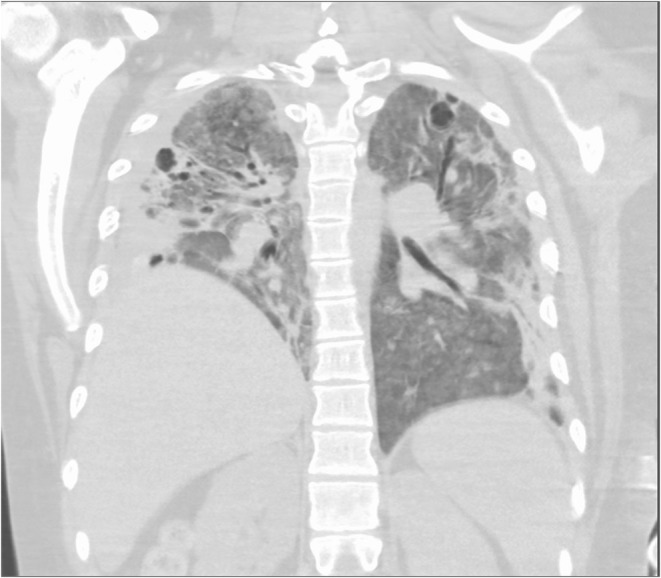
CT thorax obtained 90 days after the initial diagnosis‐demonstrating bilateral diffuse ground‐glass opacification with areas of cystic dilatation, atelectasis, and early fibrosis
FIGURE 2.
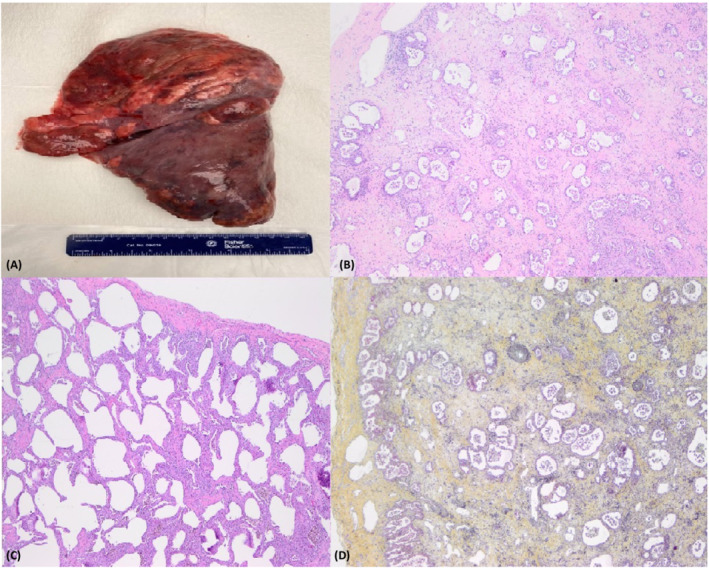
(A) Gross image of the right lung with congestion, subpleural cystic dilatation involving upper lobe, likely secondary to barotrauma. (B) Histopathology (H & E ×10) demonstrating diffuse interstitial expansion with proliferation of fibroblasts, myofibroblasts, and occasional lymphocytes with reactive type 2 pneumocyte hyperplasia a focal non‐specific pattern of lung injury. (C) Diffuse interstitial expansion with lymphocyte predominant inflammatory infiltrate (H&E ×10). (D) Foci of Interstitial expansion with predominance of mature collagenous fibrosis (Movat pentachrome staining)
3. DISCUSSION
In children above the age of 11, pediatric lung transplantation is most commonly performed for children with cystic fibrosis, followed by idiopathic pulmonary hypertension. 3 In this age group, encountering patients with COVID‐19 who require lung transplantation remains a rare possibility, due to the relatively indolent course of illness in children. Pediatric lung transplantation presents distinct challenges compared with the adults‐ due to considerations with size matching and the evolving immune system in children; and also the psychosocial factors associated with decision‐making by parents despite the unique considerations of pediatric lung transplantation, the median survival is 5.7 years, which is comparable with adults. 3 In reality, the medical management prior to transplantation in our patient did not differ significantly from the adults who require an expedited transplantation. As in other patients transplanted for COVID‐19, we monitored the patient for signs of irreversibility such as lack of change in clinical variables (degree of oxygen support, arterial blood gases, ability to wean from extracorporeal support, and imaging signs of pulmonary fibrosis). In our patient, who was anthropometrically similar to an adult, finding a donor did not prove to be a significant challenge.
Intraoperative findings of dense hilar and pleural adhesions were similar to previously reported cases. 4 The histopathology findings of explanted lungs were notable for diffuse interstitial expansion with proliferation of fibroblasts, myofibroblasts, and occasional lymphocytes with reactive type 2 pneumocyte hyperplasia a focal non‐specific pattern of lung injury. There was evidence of mature collagenous fibrosis. The pathology findings in the lung are identical to previously reported cases where diffuse interstitial fibrosis dominates the pattern with other non‐specific findings. 5
A unique aspect to be considered in performing an expedited lung transplantation in the pediatric age group is the psychosocial impact of such a definitive therapy. There were perceptible challenges to decision making specifically in relation to the decision and timing of listing. The medical team was diligent about repeatedly ensuring that the patient and his parents had a comprehensive understanding of his clinical condition and the intricacies of lung transplantation. Furthermore, the psychosocial impact of transplantation in adolescence, including risk of non‐adherence and ensuing complications was carefully evaluated at every phase. 6 The appropriate timing of listing was equally arduous given that the concern of performing a definitive procedure like lung transplantation in a young patient had to be counterbalanced against the risks of losing the window for lung transplantation (in anticipation of recovery) due to complications of being on prolonged extracorporeal support. The complications of prolonged extracorporeal support are not trivial and include hemorrhage, thrombosis, sepsis, multi‐organ failure, limb ischemia, and limb loss. 7 , 8 Even though it was compelling to monitor and hope for natural recovery, the irreversible nature of his lung injury, in addition to young age, long term ECMO dependence and deconditioning, necessitated lung transplantation as the curative treatment. The parents required considerable reassurance over a period of time regarding the appropriateness and timing of decision to list for transplantation.
In performing expedited lung transplantation for the pediatric age group, ensuring proper understanding of pros and cons of transplantation as well as proactive engagement of the parents in informed decision making is critical. Based on our experience, the medical management and operative difficulties are similar to that of adults.
AUTHOR CONTRIBUTIONS
All authors contributed equally to the writing and review of this manuscript. Dr. Ramineni provided the histopathology images.
CONFLICT OF INTEREST
The authors do not have any conflict of interest to declare pertaining to this manuscript.
Kumar A, Li GW, Segraves JM, et al. Pediatric lung transplantation for COVID‐19: Unique clinical and psychosocial barriers. Pediatric Transplantation. 2022;00:e14351. doi: 10.1111/petr.14351
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
REFERENCES
- 1. CDC COVID‐19 trends [Internet]. Accessed November 16, 2021. https://www.cdc.gov/coronavirus/2019‐ncov/cases‐updates/burden.html
- 2. Bixler [Internet]. Accessed September 15, 2020. https://www.cdc.gov/mmwr/volumes/69/wr/mm6937e4.htm?s_cid=mm6937e4_w
- 3. Hayes D Jr, Cherikh WS, Chambers DC, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: twenty‐second pediatric lung and heart‐lung transplantation report‐2019; focus theme: donor and recipient size match. J Heart Lung Transplant. 2019;38(10):1015‐1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bharat A, Machuca TN, Querrey M, et al. Early outcomes after lung transplantation for severe COVID‐19: a series of the first consecutive cases from four countries. Lancet Respir Med. 2021;9(5):487‐497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Aesif SW, Bribriesco AC, Yadav R, et al. Pulmonary pathology of COVID‐19 following 8 weeks to 4 months of severe disease: a report of three cases, including one with bilateral lung transplantation. Am J Clin Pathol. 2021;155(4):506‐514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Simons LE, McCormick ML, Mee LL, Blount RL. Parent and patient perspectives on barriers to medication adherence in adolescent transplant recipients. Pediatr Transplant. 2009;13(3):338‐347. [DOI] [PubMed] [Google Scholar]
- 7. Bemtgen X, Zotzmann V, Benk C, et al. Thrombotic circuit complications during venovenous extracorporeal membrane oxygenation in COVID‐19. J Thromb Thrombolysis. 2021;51(2):301‐307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Popugaev KA, Bakharev SA, Kiselev KV, et al. Clinical and pathophysiologic aspects of ECMO‐associated hemorrhagic complications. PLoS One. 2020;15(10):e0240117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.


