Abstract
Objective
This study aimed to assess the association of BMI with inpatient care cost, duration, and acute complications among patients hospitalized for COVID‐19 at 273 US hospitals.
Methods
Children (aged 2–17 years) and adults (aged ≥18 years) hospitalized for COVID‐19 during March 2020–July 2021 and with measured BMI in a large electronic administrative health care database were included. Generalized linear models were used to assess the association of BMI categories with the cost and duration of inpatient care.
Results
Among 108,986 adults and 409 children hospitalized for COVID‐19, obesity prevalence was 53.4% and 45.0%, respectively. Among adults, overweight and obesity were associated with higher cost of care, and obesity was associated with longer hospital stays. Children with severe obesity had higher cost of care but not significantly longer hospital stays, compared with those with healthy weight. Children with severe obesity were 3.7 times (95% CI: 1.4–9.5) as likely to have invasive mechanical ventilation and 62% more likely to have an acute complication (95% CI: 39%–90%), compared with children with healthy weight.
Conclusions
These findings show that patients with a high BMI experience significant health care burden during inpatient COVID‐19 care.
Study Importance.
What is already known?
Overweight and obesity are risk factors for severe COVID‐19 illness among adults and children.
Many health care databases lack information about the cost of care or define obesity using the International Classification of Diseases, Tenth Revision, Clinical Modification codes that underreport obesity status.
Little is known about the cost and duration of hospitalizations for COVID‐19 among children with overweight and obesity.
What does this study add?
Among adults, overweight and obesity were associated with higher cost, and obesity was associated with longer duration of inpatient care.
Children with severe obesity had higher cost of care but not significantly longer hospital stays, compared with those with healthy weight.
Children with severe obesity had higher risk of invasive mechanical ventilation and acute complications compared with children with healthy weight.
How might these results change the direction of research or the focus of clinical practice?
The increased cost of inpatient care associated with high BMI, combined with the high prevalence of overweight and obesity in the United States, suggests a significant health care burden of high BMI among children and adults with COVID‐19.
These estimates could be used in combination with trial‐based estimates of averted COVID‐19 hospitalizations to assess the benefits to the US health care system of vaccination among patients with overweight and obesity.
INTRODUCTION
Overweight and obesity together affect more than 70% of US adults [1] and 35% of US children [2] and are risk factors for severe COVID‐19 [3, 4]. However, information on the association of body mass index (BMI) with duration and cost of inpatient care for COVID‐19 is limited. Recent studies that have reported cost estimates of COVID‐19 care did not use measured height and weight and instead relied on the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD‐10‐CM) codes that underreport obesity [5, 6]. Additionally, information on how BMI status is associated with the duration and cost of inpatient care among pediatric patients with COVID‐19 is very limited. This study assesses the health care burden of unhealthy BMI during COVID‐19 treatment by estimating the association between BMI and per patient cost and duration of inpatient care among adults and children hospitalized for COVID‐19 at 273 US hospitals.
METHODS
Premier Healthcare Database Special COVID‐19 Release (PHD‐SR; release date: 09/24/2021) is a large all‐payer US administrative database [7]. Among 847 geographically dispersed US hospitals in this database, 273 reporting patient height and weight information were selected for this study.
Cohort selection
The sample included hospitalized children (aged 2–17 years) and adults (aged ≥18 years) with measured height and weight and a primary diagnosis of COVID‐19. A COVID‐19 diagnosis was defined as having an ICD‐10‐CM code of U07.1 (COVID‐19, virus identified) during April 1, 2020 to July 31, 2021, or B97.29 (other coronavirus as the cause of diseases classified elsewhere; recommended before April 2020 release of U07.1) during March 1, 2020 to April 30, 2020. Patients whose sex was not recorded (n = 2 [0.001%]) and those with zero costs (n = 399 [0.27%]) were excluded from the study (Supporting Information Figure S1).
Outcomes and covariates
The main outcome variables were the 1) estimated cost and 2) duration of inpatient care. Both outcomes were obtained from all hospitalizations with a primary COVID‐19 discharge diagnosis code for each patient in PHD‐SR. We used costs that passed all validity checks, including financial reconciliation in PHD‐SR; otherwise, costs were calculated using reported charges multiplied by estimated hospital‐specific cost‐to‐charge ratios (Supporting Information Figure S2). Costs and charges reported by hospitals are facility fees, inclusive of salaries, but excluding professional fees for services billed to patients by independent physicians. Costs from 2021 were converted to 2020 dollars using the Personal Consumption Expenditures: Health Care Index [8].
We assessed additional outcome variables that might contribute to the differences in cost of COVID‐19 care, such as presence of invasive mechanical ventilation (defined using patient billing records) and acute complications of COVID‐19 (defined using ICD‐10‐CM codes) [9]. These were obtained from all hospitalizations with COVID‐19 for each patient.
BMI was calculated using heights and weights measured during the health care encounter closest to the patient's first hospitalization for COVID‐19 in the database. BMI among adults was categorized as underweight (<18.5 kg/m2), healthy weight (18.5–24.9 kg/m2 [reference]), overweight (25–29.9 kg/m2), and obesity (four categories: 30–34.9, 35–39.9, 40–44.9, and ≥45 kg/m2) [10]. Severe obesity is typically defined as BMI ≥ 40 kg/m2. BMI status among children was defined using the Centers for Disease Control and Prevention (CDC) BMI‐for‐age percentiles as underweight (<5th percentile), healthy weight (≥5th to <85th percentile [reference]), overweight (≥85th to <95th percentile), moderate obesity (≥95th percentile to <120% of the 95th percentile), and severe obesity (≥120% of the 95th percentile) [11].
Patient and hospital characteristics (sex, age, race and ethnicity, payer type, and US Census region and urbanicity of hospital) were obtained from patient medical records at first COVID‐19 hospitalization in PHD‐SR. Underlying medical conditions were captured by ICD‐10‐CM diagnosis codes from inpatient or outpatient medical records from January 2019 through a patient's first inpatient encounter with COVID‐19. Conditions included in the analysis were those defined by the CDC as risk factors for severe COVID‐19 illness [12], and they differed for children and adults.
Statistical analysis
Model 1 estimated the cost of inpatient care per patient using a generalized linear model (GLM) with log link function and Gamma distribution. Model 2 estimated the duration of inpatient care using a GLM model with log link function and Poisson distribution. Further, we estimated the association between BMI status and additional outcome variables that could be potential drivers of cost: (a) risk of invasive mechanical ventilation (logit model), (b) risk of acute complications (logit model), (c) the number of acute complications of COVID‐19 (GLM with Poisson distribution and log link function), and (d) risk of top three most frequent acute complications (logit model). Each model was estimated separately among adults and children.
All models included the following covariates: BMI category (reference: healthy weight), age group, sex, race and ethnicity, payer type, hospital urbanicity, hospital US Census region, and admission month via a linear and quadratic term (to account for potential nonlinear unobservable changes in the severity of illness over the course of the pandemic).
Models did not adjust for other underlying medical conditions known to be risk factors for COVID‐19 [12] because many represent intermediate variables on a causal pathway from exposure (i.e., BMI) to outcome. A supplemental analysis adjusting for these conditions was performed.
Analyses were conducted using R 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria or https://www.R-project.org/) and Stata 15.1 (StataCorp LLC, College Station, Texas).
RESULTS
The study population included 108,986 adults and 409 children hospitalized for COVID‐19 (Table 1). Most patients were non‐Hispanic White individuals (adults: 58,240 [53.4%]; children: 141 [34.5%]) admitted to urban hospitals (adults: 89,803 [82.4%]; children: 373 [91.2%]) and hospitals in the South US Census region (adults: 75,587, 69.4%; children: 334, 81.7%). Adults and children spent, on average, 8 and 5.2 days in the hospital (median: 5 and 3 days), respectively, with average costs of $20,155 and $18,697 (median: $12,023 and $9,902). Most patients (93.1% of adults and 96.6% of children) had one hospitalization for COVID‐19, and the rest had two or more hospitalizations.
TABLE 1.
Patient characteristics—Premier Healthcare Database Special COVID‐19 Release, United States, March 2020–July 2021
| Patients aged ≥18 years | Patients aged <18 years | ||||
|---|---|---|---|---|---|
| Characteristic | All | Primary COVID‐19 | Characteristic a | All | Primary COVID‐19 |
| Total, n (%) | 1,993,375 (100.0) | 108,986 (100.0) | Total, n (%) | 28,855 (100.0) | 409 (100.0) |
| Sex, n (%) | Sex, n (%) | ||||
| Female | 1,167,512 (58.6) | 53,088 (48.7) | Female | 16,550 (57.4) | 191 (46.7) |
| Male | 825,863 (41.4) | 55,898 (51.3) | Male | 12,305 (42.6) | 218 (53.3) |
| Age (y) | Age (y) | ||||
| 18–24 | 117,850 (5.9) | 1,190 (1.1) | 2–4 | 4,276 (14.8) | 78 (19.1) |
| 25–39 | 401,268 (20.1) | 8,379 (7.7) | 5–11 | 7,256 (25.1) | 107 (26.2) |
| 40–49 | 174,596 (8.8) | 12,043 (11.1) | 12–17 | 17,323 (60.0) | 224 (54.8) |
| 50–64 | 446,792 (22.4) | 32,258 (29.6) | |||
| 65–74 | 380,821 (19.1) | 24,418 (22.4) | |||
| 75+ | 472,048 (23.7) | 30,698 (28.2) | |||
| Median (IQR) | 60 (38–74) | 65 (53–76) | Median (IQR) | 13 (7–16) | 13 (6–16) |
| Race and ethnicity, n (%) | Race and ethnicity, n (%) | ||||
| Hispanic or Latino | 195,138 (9.8) | 15,559 (14.3) | Hispanic or Latino | 5,725 (19.8) | 103 (25.2) |
| Non‐Hispanic White | 1,191,863 (59.8) | 58,240 (53.4) | Non‐Hispanic White | 11,670 (40.4) | 141 (34.5) |
| Non‐Hispanic Black | 265,707 (13.3) | 18,181 (16.7) | Non‐Hispanic Black | 5,396 (18.7) | 100 (24.4) |
| Non‐Hispanic Asian | 44,481 (2.2) | 2,036 (1.9) | Non‐Hispanic Asian | 558 (1.9) | 12 (2.9) |
| Non‐Hispanic other b | 50,235 (2.5) | 2,606 (2.4) | Non‐Hispanic otherb | 995 (3.4) | 12 (2.9) |
| Unknown | 245,951 (12.3) | 12,364 (11.3) | Unknown | 4,511 (15.6) | 41 (10.0) |
| Payer type, n (%) | Payer type, n (%) | ||||
| Commercial | 548,473 (27.5) | 30,608 (28.1) | Commercial | 10,127 (35.1) | 133 (32.5) |
| Medicare | 927,030 (46.5) | 58,576 (53.7) | Medicaid | 16,608 (57.6) | 243 (59.4) |
| Medicaid | 339,952 (17.1) | 9,745 (8.9) | Other | 2,120 (7.4) | 33 (8.1) |
| Charity/indigent/self‐pay | 99,404 (5.0) | 2,963 (2.7) | |||
| Other | 78,516 (3.9) | 7,094 (6.5) | |||
| Urbanicity, n (%) | Urbanicity, n (%) | ||||
| Rural | 311,674 (15.6) | 19,183 (17.6) | Rural | 4,478 (15.5) | 36 (8.8) |
| Urban | 1,681,701 (84.4) | 89,803 (82.4) | Urban | 24,377 (84.5) | 373 (91.2) |
| US Census region, n (%) | US Census region, n (%) | ||||
| Midwest | 400,351 (20.1) | 18,895 (17.3) | Midwest and West | 5,895 (20.4) | 41 (10.0) |
| Northeast | 276,348 (13.9) | 13,184 (12.1) | Northeast | 3,466 (12.0) | 34 (8.3) |
| South | 1,266,639 (63.5) | 75,587 (69.4) | South | 19,494 (67.6) | 334 (81.7) |
| West | 50,037 (2.5) | 1,320 (1.2) | |||
| BMI (kg/m2), n (%) | BMI (BMI‐for‐age percentile), n (%) | ||||
| <18.5 (underweight) | 59,941 (3.0) | 2,136 (2.0) | <5th (underweight) | 1,973 (6.8) | 20 (4.9) |
| 18.5–24.9 (healthy weight) | 465,459 (23.4) | 18,743 (17.2) | ≥5th to <85th (healthy weight) | 13,932 (48.3) | 151 (36.9) |
| 25–29.9 (overweight) | 572,920 (28.7) | 29,918 (27.5) | ≥85th to <95th (overweight) | 5,047 (17.5) | 54 (13.2) |
| ≥30 (obesity) | 895,055 (44.9) | 58,189 (53.4) | ≥95th (obesity) | 7,903 (27.4) | 184 (45.0) |
| 30–34.9 | 427,439 (21.4) | 25,425 (23.3) | ≥120% of the 95th percentile (severe obesity) | 3,266 (11.3) | 123 (30.1) |
| 35–39.9 | 239,471 (12.0) | 15,531 (14.3) | |||
| 40–44.9 (severe obesity) | 119,369 (6.0) | 8,334 (7.6) | |||
| ≥45 (severe obesity) | 108,776 (5.5) | 8,899 (8.2) | |||
| Presence of acute complications c , n (%) | 105,070 (96.4) | Presence of acute complications c , n (%) | 290 (70.9) | ||
| Severity indicator, n (%) | Severity indicator, n (%) | ||||
| No ICU/IMV/death | 54,052 (49.6) | No ICU/IMV/death | 245 (59.9) | ||
| ICU | 52,779 (48.4) | ICU | 163 (39.9) | ||
| IMV | 11,568 (10.6) | IMV | 25 (6.1) | ||
| Death | 10,056 (9.2) | Death | <5 | ||
| Number of hospitalizations, n (%) | Number of hospitalizations, n (%) | ||||
| 1 | 101,510 (93.1) | 1 | 395 (96.6) | ||
| ≥2 hospitalizations | 7,476 (6.9) | ≥2 hospitalizations | 14 (3.4) | ||
| Duration of inpatient care (d) per patient, mean; median (IQR) | 8; 5 (3–10) | Duration of inpatient care (d) per patient, mean; median (IQR) | 5.2; 3 (2–6) | ||
| Inpatient cost ($) per patient, mean; median (IQR) | 20,155; 12,023 (6,961–21,782) | Inpatient cost ($) per patient, mean; median (IQR) | 18,697; 9,902 (4,518–18,252) | ||
Note: Patients were included if they had a primary diagnosis of COVID‐19, defined as ICD‐10‐CM code of U07.1 (COVID‐19, virus identified) during April 1, 2020–July 31, 2021 or B97.29 (other coronavirus as the cause of diseases classified elsewhere; recommended before April 2020 release of U07.1) during March 1, 2020–April 30, 2020.
Abbreviations: COPD, chronic obstructive pulmonary disease; ICU, intensive care unit; IMV, invasive mechanical ventilation.
Some cells were combined or suppressed for cell sizes <10.
The non‐Hispanic others include American Indians or Alaska Natives and Native Hawaiians or other Pacific Islanders.
Acute complications: respiratory (acute respiratory distress syndrome, pneumothorax, respiratory failure, chronic obstructive pulmonary disease exacerbation, pneumonia, asthma exacerbation), cardiovascular (cardiogenic shock, congestive heart failure, acute myocardial infarction or unstable angina, hypertensive crisis, myocarditis), hematologic (deep vein thrombosis, disseminated intravascular coagulation, pulmonary embolism), neurologic (intracranial hemorrhage, cerebral ischemia/infarction), endocrine (diabetic ketoacidosis), renal (dialysis initiation, acute kidney injury), and other (bacteremia, pressure ulcer, sepsis, acute hepatitis/liver failure).
Among adults, obesity prevalence was 53.4% (Table 1), with the highest prevalence among patients aged 25 to 39 years (71.8%), those commercially insured (65.6%), and Non‐Hispanic Black individuals (62%) (Supporting Information Table S1). Among children, obesity prevalence was 45.0% (Table 1), with the highest prevalence among those aged 12 to 17 years (55.4%), Hispanic individuals (51.5%), and those on Medicaid (48.1%).
Among adults, overweight and obesity were associated with higher cost of inpatient care, and obesity was associated with longer duration of inpatient care (Figure 1). Costs ranged from 6% or $1,131 (95% confidence interval [CI]: $629–$1,634) higher among adults with BMI of 25 to 29.9 to 34% or $6,108 (95% CI: $5,110–$7,105) higher among adults with BMI ≥ 45, compared with those with healthy weight (BMI 18.5–24.9). Duration of inpatient care ranged from 3% or 0.24 days (95% CI: 0.06–0.41) longer among patients with BMI of 30 to 34.9 to 13% or 1.03 days (95% CI: 0.79–1.27) longer among patients with BMI ≥ 45, compared with those with healthy weight. After controlling for other underlying medical conditions, we found weaker but consistently significant associations between BMI status and these outcomes (Supporting Information Figure S3). Specifically, costs ranged from 5% or $875 (95% CI: $458–$1,291) more among adults with BMI of 25 to 29.9 to 24% or $4,495 (95% CI: $3,634–$5,355) more among adults with BMI ≥ 45. Duration of inpatient care was significantly associated with high BMI categories, ranging from 3% or 0.20 days (95% CI: 0.01–0.38) longer among those with BMI of 35 to 39.9 to 9% or 0.71 days (95% CI: 0.47–0.95) longer among those with BMI of ≥45, compared with those with healthy weight.
FIGURE 1.
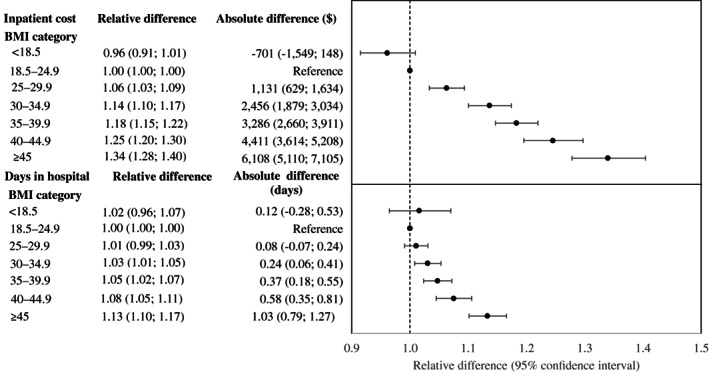
Difference in cost and duration of inpatient care among patients aged ≥18 years with a primary diagnosis of COVID‐19, by BMI category—PHD‐SR, United States, March 2020–July 2021. Each panel contains the results of a single generalized linear model, adjusted for BMI category, age, sex, race and ethnicity, payer type, hospital urbanicity, hospital US Census region, and admission month. Model 1 (upper panel) used the cost of inpatient care ($) per patient as the outcome and was a generalized linear model with log link function and Gamma distribution. Model 2 (lower panel) used the duration of inpatient care (days in hospital) per patient as the outcome and was a generalized linear model with log link function and Poisson distribution. Absolute difference represents the difference in the expected outcome (cost or duration of inpatient care) among patients in each BMI category (compared to healthy weight). Relative difference represents the ratio in the expected outcome (cost or duration of inpatient care) among patients in each BMI category (compared to healthy weight). Data in PHD‐SR, formerly known as the PHD COVID‐19 Database, are released every 2 weeks; release date September 24, 2021. PHD‐SR, Premier Healthcare Database Special COVID‐19 Release
Adults with overweight and obesity had higher risk of invasive mechanical ventilation: the risk increased monotonically from 1.22 times as high (95% CI: 1.14–1.31) among patients with BMI of 25 to 29.9 to 2.31 times as high (95% CI: 2.11–2.53) among patients with BMI ≥45, compared with those with healthy weight (Table 2). They were also more likely to have an acute complication: from 2% (95% CI: 2%–3%) more among patients with BMI of 25 to 29.9 to 6% (95% CI: 5%–6%) more among patients with BMI ≥45, compared with those with healthy weight. Overweight and obesity were associated with a 4% to 10% higher risk of pneumonia, an 8% to 30% higher risk of respiratory failure, and an 8% to 42% higher risk of acute kidney injury, increasing monotonically with higher BMI category (Table 3).
TABLE 2.
Risk of IMV, risk of acute complications, a and the number of acute complications by BMI category among adults and children hospitalized for COVID‐19—PHD‐SR, b United States, March 2020–July 2021
| Covariate b | Risk of IMV | Risk of acute complications | Number of acute complications | |
|---|---|---|---|---|
| Relative risk | Relative risk | Relative difference | Absolute difference | |
| BMI category, children | ||||
| Underweight | 3.08 (1.39–6.83) c | 1.23 (0.93–1.63) | 1.44 (0.98–2.11) | 0.34 (−0.07–0.75) |
| Healthy weight | Reference | Reference | Reference | Reference |
| Overweight | 0.52 (0.15–1.82) | 1.15 (0.90–1.49) | 1.56 (1.06–2.30) c | 0.43 (−0.03–0.89) |
| Moderate obesity | 2.01 (0.85–4.76) | 1.27 (1.00–1.63) | 1.37 (1.12–1.68) c | 0.28 (0.06–0.51) c |
| Severe obesity | 3.69 (1.44–9.48) c | 1.62 (1.39–1.90) c | 1.91 (1.59–2.30) c | 0.70 (0.45–0.95) c |
| BMI category, adults (kg/m2) | ||||
| <18.5 | 0.89 (0.76–1.04) | 0.99 (0.98–1.01) | 1.00 (0.98–1.03) | 0.01 (−0.05–0.07) |
| 18.5–24.9 | Reference | Reference | Reference | Reference |
| 25–29.9 | 1.22 (1.14–1.31) c | 1.02 (1.02–1.03) c | 1.01 (1.00–1.03) | 0.03 (0.00–0.06) |
| 30–34.9 | 1.50 (1.40–1.60) c | 1.04 (1.03–1.04) c | 1.05 (1.04–1.07) c | 0.12 (0.09–0.15) c |
| 35–39.9 | 1.67 (1.56–1.78) c | 1.04 (1.04–1.05) c | 1.08 (1.07–1.10) c | 0.19 (0.16–0.23) c |
| 40–44.9 | 1.87 (1.73–2.02) c | 1.05 (1.04–1.06) c | 1.13 (1.11–1.15) c | 0.31 (0.27–0.35) c |
| ≥45 | 2.31 (2.11–2.53) c | 1.06 (1.05–1.06) c | 1.19 (1.17–1.22) c | 0.46 (0.42–0.50) c |
Abbreviations: ARDS, acute respiratory distress syndrome; IMV, invasive mechanical ventilation; PHD‐SR, Premier Healthcare Database Special COVID‐19 Release; –, negative sign or to.
Acute complications: respiratory (included acute respiratory distress syndrome, pneumothorax, respiratory failure, chronic obstructive pulmonary disease exacerbation, pneumonia, asthma exacerbation), cardiovascular (cardiogenic shock, congestive heart failure, acute myocardial infarction or unstable angina, hypertensive crisis, myocarditis), hematologic (deep vein thrombosis, disseminated intravascular coagulation, pulmonary embolism), neurologic (intracranial hemorrhage, cerebral ischemia/infarction), endocrine (diabetic ketoacidosis), renal (dialysis initiation, acute kidney injury), and other (bacteremia, pressure ulcer, sepsis, acute hepatitis/liver failure).
Each column contains the results of a single model, with the outcome variables that could be potential drivers of cost: (a) risk of IMV (logit model), (b) risk of acute complications (logit model), and (c) the number of acute complications of COVID‐19 (generalized linear model with Poisson distribution and log link function). Models are adjusted for BMI category, age, sex, race and ethnicity, payer type, hospital urbanicity, hospital US Census region, and admission month. Absolute difference represents the difference in the expected outcome (cost or duration of inpatient care) among patients in each BMI category (compared with healthy weight). Relative difference represents the ratio in the expected outcome (cost or duration of inpatient care) among patients in each BMI category (compared with healthy weight).
p < 0.05.
TABLE 3.
Risk of the most frequent acute complications a by BMI category among adults and children hospitalized for COVID‐19—PHD‐SR, b United States, March 2020–July 2021
| Covariate | Relative risk b | ||
|---|---|---|---|
| Pneumonia | Respiratory failure | Acute kidney injury | |
| BMI category, children | |||
| Underweight | 1.82 (1.15–2.88) c | 2.07 (1.00–4.32) | 2.72 (0.78–9.51) |
| Healthy weight | Reference | Reference | Reference |
| Overweight | 1.48 (1.14–1.93) c | 1.17 (0.46–2.97) | 2.33 (0.77–7.10) |
| Obesity | 1.39 (0.93–2.07) | 1.76 (1.20–2.58) c | 2.79 (1.23–6.32) c |
| Severe obesity | 2.43 (2.01–2.94) c | 2.76 (1.79–4.25) c | 2.64 (1.26–5.55) c |
| BMI category, adults (kg/m2) | |||
| <18.5 | 0.95 (0.93–0.97) c | 0.99 (0.95–1.03) | 0.95 (0.89–1.01) |
| 18.5–24.9 | Reference | Reference | Reference |
| 25–29.9 | 1.04 (1.03–1.05) c | 1.08 (1.06–1.10) c | 1.08 (1.05–1.12) c |
| 30–34.9 | 1.06 (1.06–1.07) c | 1.13 (1.11–1.15) c | 1.17 (1.13–1.21) c |
| 35–39.9 | 1.08 (1.07–1.08) c | 1.18 (1.15–1.20) c | 1.26 (1.22–1.31) c |
| 40–44.9 | 1.09 (1.08–1.10) c | 1.22 (1.20–1.25) c | 1.34 (1.29–1.40) c |
| ≥45 | 1.10 (1.09–1.11) c | 1.30 (1.27–1.33) c | 1.42 (1.36–1.49) c |
Abbreviations: PHD‐SR, Premier Healthcare Database Special COVID‐19 Release.
The most frequent acute complications among children were as follows: pneumonia (n = 184 [45.0%]), respiratory failure (n = 108 [26.4%]), and acute kidney injury (n = 29 [7.1%]). The most frequent acute complications among adults were also pneumonia (n = 96,751 [88.8%]), respiratory failure (n = 68,443 [62.8%]), and acute kidney injury (n = 28,756 [26.4%]).
Each column contains the results of a single model, with the outcome variables representing the risk of top three most frequent acute complications (logit model). Models are adjusted for BMI category, age, sex, race and ethnicity, payer type, hospital urbanicity, hospital US Census region, and admission month. Absolute difference represents the difference in the expected outcome (cost or duration of inpatient care) among patients in each BMI category (compared with healthy weight). Relative difference represents the ratio in the expected outcome (cost or duration of inpatient care) among patients in each BMI category (compared with healthy weight).
p < 0.05.
Children with severe obesity had a 53% or $7,660 (95% CI: $1,721–$13,600) higher cost of care but not significantly longer stays, compared with those with healthy weight (Figure 2). Children with underweight had a 69% or $9,970 (95% CI: $3,127–$16,813) higher cost of care compared with those with healthy weight. However, when controlling for underlying medical conditions, underweight was no longer associated with higher cost, but severe obesity was associated with a 32% or $5,135 (95% CI: $1519–$8750) higher cost compared with those with healthy weight (Supporting Information Figure S4).
FIGURE 2.
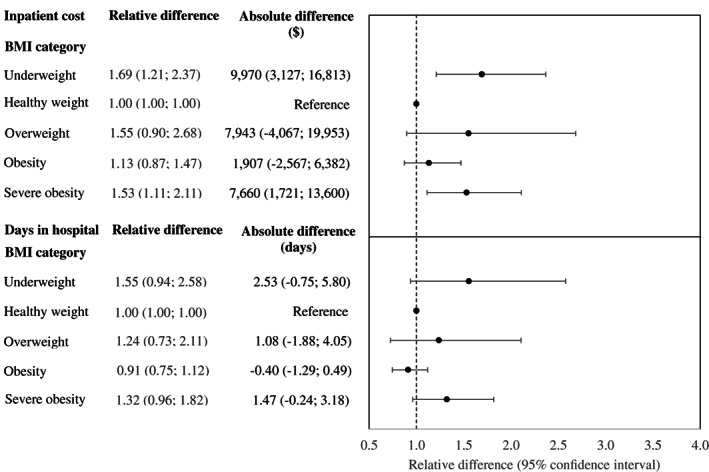
Difference in cost and duration of inpatient care among patients aged <18 years with a primary diagnosis of COVID‐19, by BMI category—PHD‐SR, United States, March 2020–July 2021. Each panel contains the results of a single generalized linear model, adjusted for BMI category, age, sex, race and ethnicity, payer type, hospital urbanicity, hospital US Census region, and admission month. Model 1 (upper panel) used the cost of inpatient care ($) per patient as the outcome and was a generalized linear model with log link function and Gamma distribution. Model 2 (lower panel) used the duration of inpatient care (days in hospital) per patient as the outcome and was a generalized linear model with log link function and Poisson distribution. Absolute difference represents the difference in the expected outcome (cost or duration of inpatient care) among patients in each BMI category (compared with healthy weight). Relative difference represents the ratio in the expected outcome (cost or duration of inpatient care) among patients in each BMI category (compared with healthy weight). Data in PHD‐SR, formerly known as the PHD COVID‐19 Database, are released every 2 weeks; release date: September 24, 2021. PHD‐SR, Premier Healthcare Database Special COVID‐19 Release
Children with severe obesity were 3.69 times (95% CI: 1.44–9.48) as likely to have invasive mechanical ventilation and 1.62 times more likely to have an acute complication (95% CI: 1.39–1.90) compared with children with healthy weight (Table 2). Children with severe obesity were 2.43 times as likely to have pneumonia, 2.76 times as likely to have respiratory failure, and 2.64 times as likely to have acute kidney injury as children with healthy weight (Table 3). Children with underweight were 3.08 (95% CI: 1.39‐6.83) times more likely to have invasive mechanical ventilation and 1.82 (95% CI: 1.15‐2.88) times as likely to have pneumonia compared with children with healthy weight.
DISCUSSION
The prevalence of obesity among both adults and children with COVID‐19 in our study population (53.4% and 45.0%, respectively) was higher than among all hospitalized patients in PHD‐SR during 2020 to 2021 (44.9% and 27.4%, respectively), as well as among all Americans in 2019 (42.4% and 19.3%, respectively) [13, 14]. The excess prevalence of obesity among patients with COVID‐19 was particularly pronounced among children, who are generally healthier than adults and for whom obesity might be the primary underlying medical condition that increases their risk for serious COVID‐19 illness.
These results highlight the need to support patients in access to appropriate prevention and management strategies (e.g., social determinants of health, community supports, counseling, therapeutics, behavior management programs) for achieving or maintaining a healthy BMI. This might be especially important for populations disproportionately affected by obesity. In particular, Hispanic or Latino adults and non‐Hispanic Black adults as well as persons from low‐income households have higher prevalence of obesity and are more likely than other populations to have severe COVID‐19 illness [15].
In this study, we show that high BMI is associated with higher cost of inpatient care among both adults and children hospitalized with COVID‐19. Among adults, the cost of inpatient care increased monotonically with BMI, with the highest cost borne by patients with BMI ≥ 45. Adipose tissue is metabolically active, and high levels of excess weight are associated with chronic inflammation [4] and impaired lung function [16]. This cost difference could partially be attributed to differences in length of hospital stay, as well as the higher risk of acute complications and need for more intensive management of COVID‐19 (invasive mechanical ventilation), all of which were shown to be important drivers of cost [17]. The same study reported that hospitalizations ending in death were more costly than other COVID‐19‐related hospitalizations, other than those involving mechanical ventilation. Given that obesity is associated with higher risk of death from COVID‐19 [3], the cost differential for patients with higher BMI may be mediated in part by their increased risk of in‐hospital death, despite presumably shorter lengths of stay for hospitalizations ending in death [17].
Among children, the cost of inpatient care was higher for those with severe obesity. Severe obesity is associated with higher risk of impaired lung function [16], chronic inflammation [4], and chronic diseases during childhood, such as nonalcoholic fatty liver disease [18], prediabetes [19], and depression [20], all of which might increase the intensity of care required for COVID‐19. Although no significant difference was found in length of hospital stays, children with severe obesity were more likely to have invasive mechanical ventilation and acute complications. Underweight status was also associated with higher cost, but that association was not significant when underlying medical conditions were controlled for.
These results may also be relevant in light of possible indirect impacts of the pandemic on adiposity among children and adults. Prior research showed that children experienced higher weight gain during the first phase of the pandemic, compared with before the pandemic [21]. At the same time, evidence on adult weight gain has been mixed [22, 23, 24].
This study has at least eight limitations. First, we studied hospitalized patients; therefore, these estimates might differ from the risk among all adults or children with COVID‐19. Second, 26% of patients had missing height information, weight information, or both. However, results using multiple imputation for missing BMI were consistent with the primary findings (results not shown). Third, the misclassification of COVID‐19, underlying medical conditions, and acute complications of COVID‐19 is possible because conditions were determined solely by ICD‐10‐CM codes, which were not confirmed by chart review (e.g., laboratory tests) [25]. Fourth, the BMI categories of some older adults could be misclassified because of complex interactions between height loss and sarcopenia, a condition characterized by loss of skeletal muscle mass and function [26]. Fifth, costs in PHD‐SR data represent only facility or institutional fees and exclude noninstitutional professional fees, meaning that our estimated hospitalization costs are underestimated [27]. A previous study found that including professional fees increased total payments per hospitalization by 26.4% for commercially insured hospitalizations and by 17.7% for Medicaid hospitalizations above facility‐only payments [27]. Sixth, the costs in this study represent the resource costs incurred by hospitals in providing inpatient services. These estimates should not be confused with expenditures incurred by health plans or patients, information about which was not available in the PHD‐SR data. Seventh, PHD‐SR represents a convenience sample of health care facilities, limiting generalizability of results to the US population. Finally, the sample of children hospitalized for COVID‐19 with measured BMI was quite small, which may have affected the significance levels of the estimates.
The results of this study can be used to inform future assessments of costs, burdens, and resources related to COVID‐19 among persons with overweight and obesity. For example, these estimates could be used in combination with trial‐based estimates of averted COVID‐19 hospitalizations to assess the benefits to the US health care system of vaccination among patients with overweight and obesity. The results could also be used to assess the additional resources required to treat COVID‐19 patients with overweight and obesity. Finally, these estimates could be used to assess the COVID‐19 costs averted if overweight and obesity were prevented or treated effectively.
These findings highlight the importance of strategies that promote and support a healthy BMI, including increased access to good nutrition and safe places to be physically active. Public health strategies to prevent COVID‐19 remain important, along with a high uptake of vaccine among eligible adults and youth with higher BMI and their close contacts.
CONFLICT OF INTEREST
The authors declared no conflict of interest.
Supporting information
Appendix S1 Supporting Information
Kompaniyets L, Goodman AB, Wiltz JL, et al. Inpatient care cost, duration, and acute complications associated with BMI in children and adults hospitalized for COVID‐19. Obesity (Silver Spring). 2022;30(10):2055‐2063. doi: 10.1002/oby.23522
REFERENCES
- 1. Centers for Disease Control and Prevention . Obesity and overweight. Updated April 20, 2022. Accessed November 22, 2021. https://www.cdc.gov/nchs/fastats/obesity-overweight.htm
- 2. Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. Health E‐Stats. National Center for Health Statistics Health; 2020.
- 3. Kompaniyets L, Goodman AB, Belay B, et al. Body mass index and risk for COVID‐19‐related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death ‐ United States, March‐December 2020. Morb Mortal Wkly Rep. 2021;70:355‐361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Popkin BM, Du S, Green WD, et al. Individuals with obesity and COVID‐19: a global perspective on the epidemiology and biological relationships. Obes Rev. 2020;21:e13128. doi: 10.1111/obr.13128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Di Fusco M, Shea KM, Lin J, et al. Health outcomes and economic burden of hospitalized COVID‐19 patients in the United States. J Med Econ. 2021;24:308‐317. [DOI] [PubMed] [Google Scholar]
- 6. Martin BJ, Chen G, Graham M, Quan H. Coding of obesity in administrative hospital discharge abstract data: accuracy and impact for future research studies. BMC Health Serv Res. 2014;14:70. doi: 10.1186/1472-6963-14-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. PINC AI Applied Sciences, PINC AI Healthcare Data ‐ Special Release: COVID‐19. Published October 2021. Accessed February 8, 2021, Last Accessed May, 2022. http://offers.premierinc.com/rs/381-NBB-525/images/PHD_COVID-19_White_Paper.pdf
- 8. Dunn A, Grosse SD, Zuvekas SH. Adjusting health expenditures for inflation: a review of measures for health services research in the United States. Health Serv Res. 2018;53:175‐196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cates J, Lucero‐Obusan C, Dahl RM, et al. Risk for in‐hospital complications associated with COVID‐19 and influenza ‐ Veterans Health Administration, United States, October 1, 2018–May 31, 2020. Morb Mortal Wkly Rep. 2020;69:1528‐1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tartof SY, Qian L, Hong V, et al. Obesity and mortality among patients diagnosed with COVID‐19: results from an integrated health care organization. Ann Intern Med. 2020;173:773‐781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Centers for Disease Control and Prevention . About child & teen BMI. Updated March 17, 2021. Accessed January 4, 2022. https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html
- 12. Centers for Disease Control and Prevention . Science brief: evidence used to update the list of underlying medical conditions associated with higher risk for severe COVID‐19. Updated June 15, 2021. Accessed April 26, 2021. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/evidence-table.html [PubMed]
- 13. Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017‐2018. NCHS Data Brief, no. 360. National Center for Health Statistics; 2020. [PubMed] [Google Scholar]
- 14. Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2017–2018. Health E‐Stats. National Center for Health Statistics; 2020.
- 15. Centers for Disease Control and Prevention . Obesity, race/ethnicity, and COVID‐19. Updated May 20, 2021. Accessed November 22, 2021. https://www.cdc.gov/obesity/data/obesity-and-covid-19.html
- 16. Dixon AE, Peters U. The effect of obesity on lung function. Expert Rev Respir Med. 2018;12:755‐767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shrestha SS, Kompaniyets L, Grosse SD, et al. Estimation of coronavirus disease 2019 hospitalization costs from a large electronic administrative discharge database, March 2020–July 2021. Open Forum Infect Dis. 2021;8:ofab561. doi: 10.1093/ofid/ofab561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Africa JA, Newton KP, Schwimmer JB. Lifestyle interventions including nutrition, exercise, and supplements for nonalcoholic fatty liver disease in children. Dig Dis Sci. 2016;61:1375‐1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Boone‐Heinonen J, Sacks RM, Takemoto EE, et al. Prenatal development and adolescent obesity: two distinct pathways to diabetes in adulthood. Child Obes. 2018;14:173‐181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Morrison KM, Shin S, Tarnopolsky M, Taylor VH. Association of depression & health related quality of life with body composition in children and youth with obesity. J Affect Disord. 2015;172:18‐23. [DOI] [PubMed] [Google Scholar]
- 21. Lange SJ, Kompaniyets L, Freedman DS, et al. Longitudinal trends in body mass index before and during the COVID‐19 pandemic among persons aged 2‐19 years ‐ United States, 2018‐2020. Morb Mortal Wkly Rep. 2021;70:1278‐1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mazidii M, Leeming E, Merino J, et al. Diet and lifestyle behaviour disruption related to the pandemic was varied and bidirectional among US and UK adults participating in the ZOE COVID Study. Nat Food. 2021;2:957‐969. [DOI] [PubMed] [Google Scholar]
- 23. Lin AL, Vittinghoff E, Olgin JE, Pletcher MJ, Marcus GM. Body weight changes during pandemic‐related shelter‐in‐place in a longitudinal cohort study. JAMA Netw Open. 2021;4:e212536. doi: 10.1001/jamanetworkopen.2021.2536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Restrepo BJ. Obesity prevalence among US adults during the COVID‐19 pandemic. Am J Prev Med. 2022;63:102‐106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Quan H, Li B, Saunders LD, et al. Assessing validity of ICD‐9‐CM and ICD‐10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res. 2008;43:1424‐1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wagenaar CA, Dekker LH, Navis GJ. Prevalence of sarcopenic obesity and sarcopenic overweight in the general population: the lifelines cohort study. Clin Nutr. 2021;40:4422‐4429. [DOI] [PubMed] [Google Scholar]
- 27. Peterson C, Xu L, Florence C, Grosse SD, Annest JL. Professional fee ratios for US hospital discharge data. Med Care. 2015;53:840‐849. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Supporting Information


