Abstract
Emergencies, such as natural and manmade disasters, can present an opportunity or be a detriment to preventive healthcare. While stay‐at‐home orders which some states implemented to mitigate the impact of COVID‐19 are known to reduce acute and routine care, little is known about missed preventive care. Dental care, unlike other forms of preventive care ‐ such as pediatric vaccines and well‐visits, is simpler to analyze as it is not practicable with telehealth. Using weekly foot traffic data by SafeGraph from January 2018 to June 2020, we examine the effect of stay‐at‐home orders on visits to dental offices, finding a 15.4% decline after March 2020 for states with stay‐at‐home orders. Surprisingly, we find that states which allowed dental care during the stay‐at‐home period experienced a further 7.4% decline in visits. Using Michigan Medicaid dental claims for children we find that the decline of 0.25 claims per month is driven primarily by fewer diagnostic and preventive care visits. Though some preventive visits were rescheduled, we estimate only 58% of visits missed in March and April 2020 were made up by the end of the year. These estimates quantify the short‐term declines in preventive dental care, suggesting similar declines in other preventive care.
Keywords: I120, I130, I180
1. INTRODUCTION
On March 15, 2020, as the novel coronavirus spread through US cities, The New York Times published an infographic categorizing occupations by risk of exposure to the virus. 1 The risk was evaluated as a function of physical proximity to others and the extent of exposure. Though health care professionals faced the overall greatest risk, dentists and dental hygienists topped the list as the care they provide involves not only immediate proximity to the patient, but also work in the direct path of the exhalation plume of the patient. In recognition of this risk, most states suspended elective medical procedures, including some dental care. Furthermore, starting in the first week of March, 39 states and DC imposed stay‐at‐home orders which limited individuals' ability to step outside the home. While these orders did not halt all dental care, many dentists shut their practices temporarily in order to slow the spread of the virus, protect patients and providers, and conserve personal protective equipment. Dental offices took this opportunity to reconfigure their practice to introduce protective measures such as temperature screenings, updated procedures (limited polishing, peroxide swish, etc.), greater spacing of patients, and upgraded air filtration systems.
In this study, we evaluate changes in visits to dentists' offices due to the stay‐at‐home orders imposed by some states to mitigate the spread of COVID‐19 starting in March 2020. Though many clinics reopened for limited services in these states, patients avoided dental care for fear of exposure to the virus. We also take advantage of variability in the wording of stay‐at‐home orders to examine whether language actively encouraging dental care during this period yielded the intended policy outcome.
COVID‐19 has impacted delivery of all types of health care, as medical facilities have become ground zero of spread of the virus. Early estimates show 38%–45% decline in inpatient care, based on electronic records and claims data (Bhatt et al., 2020; Garcia et al., 2020; Hartnett et al., 2020; Trinkl & Sizemore, 2020; Zhang, 2021). Less is known, however, about changes in outpatient and preventive care, as scarcity of appropriate data combined with availability of incomplete substitutes prevents adequate assessment of declines. Mast and Munoz del Rio (2020) show a 29%–36% decline in cancer screenings months after the stay‐at‐home orders were lifted. Ziedan et al. (2020) is the only study to our knowledge that evaluates all outpatient care, finding 40% decline in visits, of which 15%–16% was attributable to the state mandates. In June 2020, the Centers for Disease Control and Prevention (CDC) reported survey results for US adults showing 40.9% avoided medical care during the pandemic, of which 12.0% avoided emergency care and 31.5% avoided routine care. Even less is known about pediatric, and more specifically, pediatric preventive care. In May 2020, the CDC reported early indication of 21.5% decline in orders placed for childhood vaccines (Santoli et al. (2020)), with no more recent updates on actual vaccines administered available.
Emergency conditions, such as natural or man‐made disasters, or pandemics such as COVID‐19, can act as unique opportunities for advancement of public health priorities or, conversely, set back decades of such progress. Deryugina and Molitor (2020) show that, in an unintended consequence of the displacement due to Hurricane Katrina, Medicare beneficiaries who moved to lower mortality areas experienced lower mortality rates after the disaster. Conversely, Danagoulian and Jenkins (2021) show maternal smoking and breastfeeding declined after the Flint water contamination. As preventive care makes up the plurality of dental care, 2 it serves as an effective area for evaluation of the impact of pandemic on preventive care more generally. 3 In Healthy People 2030, the US Department of Health and Human Services identifies decade specific public health priorities guiding individuals, organizations, and communities toward better health outcomes. As part of its 355 objectives, it sets a target for preventive dental care (82.7% for low income youth) and the use of the oral health care system, more generally, (45%). 4 Disruptions in delivery of preventive care, such as those occurring during the COVID‐19 pandemic may set back gains in public health by a decade.
Dental care is not fully integrated into the health care payment and delivery system in the US. It is not included in most employer provided health insurance plans, but may be offered as a separate benefit. There are very few federal policies regulating access to dental care: The Affordable Care Act makes no mention of dental care, though the insurance exchanges may include some standalone dental plans or dental benefits incorporated in health plans. 5 While all Medicaid plans provide coverage of dental benefits for children, such coverage varies by state for adults. Medicare benefits do not include dental coverage.
As a result, there exists a significant unmet need for dental care, particularly among low‐income, elderly, and other underserved populations. Dental caries are the most common chronic disease among children, affecting about 60% of 5 to 17 year‐olds, and 25% of under 5 year‐olds. Nationally, 27% of all adults have untreated dental caries, however it is much more prevalent among adults with incomes below 100% of Federal Poverty Level (44%) and blacks (42%). 6 Among pregnant women, 30%–40% experience some periodontal disease, and only 25%–50% of those who perceive a dental problem seek care. Among older adults, a lifetime of unmet need, poor hygiene, presence of comorbidities, as well as lack of mobility combine to diminish desire and ability to seek dental care, resulting in further increases in dental caries, periodontal disease, active decay, and loss of teeth (Bersell, 2017; Blackburn et al., 2017).
While lack of dental care among children and young adults results in short‐term pain, tooth loss, difficulty eating, speech impediment, and self‐image problems, chronic periodontal problems affect overall health among adults. Poor oral hygiene has been associated with increased incidence of chronic obstructive pulmonary disease and pneumonia among people living in the community and in long‐term care facilities (Manger et al., 2017). At the same time, chronic inflammation associated with periodontal disease has been associated with chronic heart disease and stroke (Brown et al., 2011; Mustapha et al., 2007; Sen et al., 2018). Nasseh et al. (2017) also show significantly lower health care costs for patients with Type 2 diabetes who seek periodontal care.
Poor teeth affect more than health, however. As Glied and Neidell (2010) showed using variation in water fluoridation between localities, oral health results in 4% higher earnings among women, particularly among families of low socioeconomic status. In a systematic review of literature on oral health and school outcomes, Rebelo et al. (2019) find that children with one or more decayed tooth have a higher probability of poor school performance and attendance than caries‐free children.
This study contributes to the three above mentioned bodies of literature, using the COVID‐19 pandemic to evaluate changing dental care in the wake of disruptions in access to care. Furthermore, this study makes a significant contribution to causal literature on dental care. Much of the existing literature characterizes socioeconomic and clinical characteristics of dental care, but very few evaluate causal outcomes relating to policy changes. Among these, Buchmueller et al. (2016), Decker and Lipton (2015), and Choi (2011) evaluate the effectiveness of Medicaid expansion of dental coverage to adults. And Buchmueller et al. (2015) consider whether increasing payment to dentists affects access to dental care for children on Medicaid, finding modest but positive effects on willingness to accept patients.
We quantify the effect of state stay‐at‐home orders on visits to dental offices using high frequency weekly foot traffic data from cellular devices between January 2018 through June 2020. Comparing states which instituted a stay‐at‐home order in the first week of March 2020 to those which did not, we estimate a 12.3%–14.5% decline in dentist visits, largely coming from metropolitan areas. Taking advantage of differences in wording, we evaluate whether including dental care as allowable reason to leave home increased visits to dentist offices. We find no significant difference in visits with and without dental allowances.
We also explore what types of care were missed using Medicaid dental claims for children in Michigan. Comparing care before and after March 2020, we estimate a 5.6% point decline in probability of a claim, of which the largest declines are estimated in diagnostic and preventive care (4.4 pp and 4.1 pp, respectively). Comparing duration in months between preventive claims, we find 52% fewer preventive visits occurred in March and April 2020 than should have, though some of these missing visits occurred later in the year. In net, however, we estimate that by the end of the year, only 58% of preventive visits occurred compared to the same period in the year prior to the pandemic.
We proceed, next, with a description of the policies evaluated here, as well as the variability in the language which we use in our analyses. Data and Estimation Method sections follow, detailing the datasets used and the method of analysis. Results follow with a Discussion of findings and policy implications.
1.1. COVID‐19, dental care, and state policies
COVID‐19 changed the delivery of health care in multiple ways. As the virus spread, 32 states implemented moratoria on elective procedures to mitigate the risk of contagion to providers and patients. At the same time, 49 states and DC (with the notable exception of Wyoming), extended Medicaid coverage of telehealth services. Finally, 39 states and DC implemented stay‐at‐home orders limiting individual mobility outside the home. Combined, these policies sharply reduced both demand as well as supply of medical care, particularly non‐acute care which can be delayed. At the same time, some care moved into the virtual domain with telehealth.
While Verma (2020) documents the dramatic rise in telehealth visits during this period, Ziedan et al. (2020) summarizes the challenges posed when trying to identify these visits in electronic health records or claims data, as procedure codes designated for such services were relatively unused. Instead, Centers for Medicare and Medicaid Services (CMS) identified procedures codes which became telehealth eligible during the pandemic, rendering such care indistinguishable from in‐person visits.
This analysis focuses on the implementation of the stay‐at‐home orders. The first of these orders was implemented on March 19 by California, and these orders were in effect anywhere between 4 and 10 weeks. Orders remained in effect through May in most states, with a handful of states retaining the restrictions through June.
The language of the stay‐at‐home orders was not consistent across states. Some orders included a detailed description of the activities for which a person may leave home, as well as a complete list of types of businesses which are deemed essential and thus exempt from the closure requirement. Other states, such as California, remained vague, failing to specify exempt activities or businesses. One dimension along which stay‐at‐home orders differed was the list of allowable reasons to leave home. While food and medical care was consistently mentioned as valid reasons for leaving home, some states also listed dental care, whether urgent or non‐urgent, as allowable.
We take advantage of state decisions to impose these stay‐at‐home orders to evaluate its effect on dental care. We expect to see larger declines in dental visits in states with stay‐at‐home orders as restriction on movement reduces one's ability to engage in in‐person health care. We also use the variability of inclusion of dental care in some stay‐at‐home orders (“dental allowance”, henceforth) to evaluate the impact of the mention on dental visits. A priori, we would expect dental visits to be higher in states with dental allowances. Figure 1 shows states which implemented stay‐at‐home orders and those with additional dental allowance in the language. The figure also shows the timeline of the implementation of these orders.
FIGURE 1.
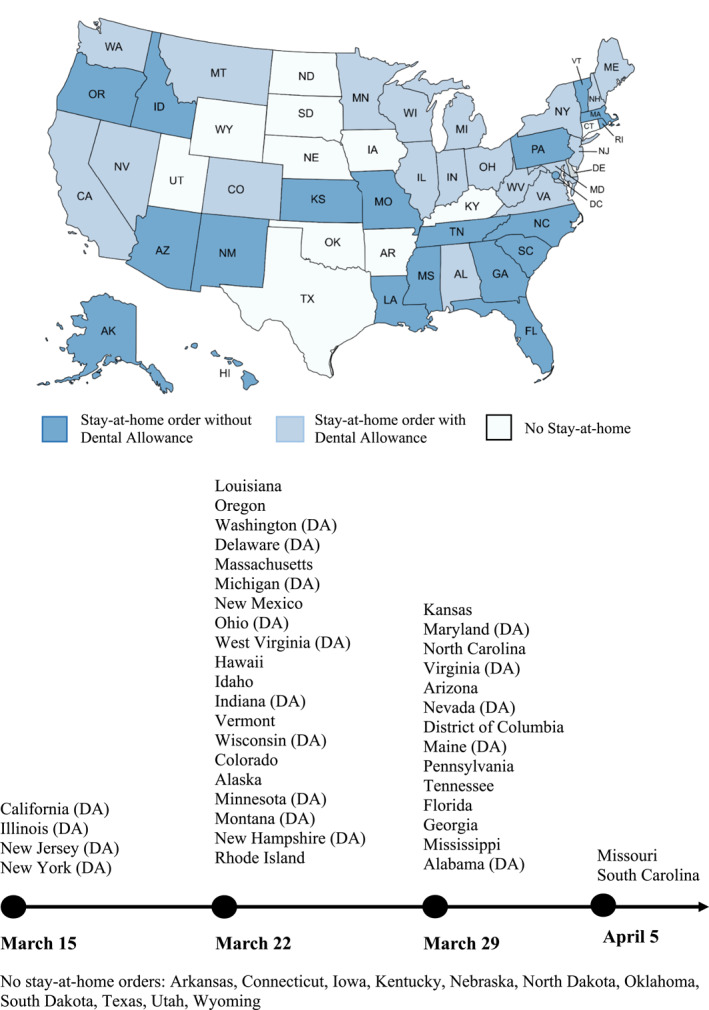
States with stay‐at‐home orders, with or without dental allowance
Dental care provides a unique opportunity to evaluate the impact of the policies bypassing many of the problems presented by other forms of health care. First, it circumvents the problem of identification of telehealth visits, as dental care is not practicable without an in‐person consultation and, as such, does not lend itself to telehealth visits. As such, we can assume that all visits to dental offices and claims occurring after March 2020 capture the totality of care, and constitute in‐person care.
Second, though dental offices may be located in larger medical office environments, they are rarely part of hospital outpatient premises. This means that we can disentangle a visit to the dental office from visits to other types of medical care. Furthermore, though all physician offices are designated by a single North American Industry Classification System (NAICS) code, dental offices have a separate code allowing for easier identification of these venues. As our analysis is based on foot‐traffic data, we are able to unambiguously identify visits to dental offices. Third, dental care was identified in many stay‐at‐home orders as an allowable reason to leave home, giving us a unique opportunity not only to evaluate the impact of the order, but also the language of the order on missed health care.
2. DATA
2.1. COVID‐19 policies
We use multiple sources for COVID‐19 policies. At the state level we use the COVID‐19 US State Policy Database (CUSP), which tracks the dates when each state implemented social safety programs and physical distancing policies in response to the pandemic (Raifman et al., 2020). We use these data to determine whether a stay‐at‐home order was issued by each state in the data. Thirty‐nine states and DC implemented a stay‐at‐home order in late March or early April 2020. At the county level, we use policy intervention data compiled from the Johns Hopkins University Center for Systems Science and Engineering COVID‐19 Dashboard (Killeen et al., 2020).
We read stay‐at‐home executive orders released by each state, as collected and organized by FINRA, 7 for inclusion of language on dental care in these orders. A state was deemed to have included dental care as an allowable exception to its stay‐at‐home order if it was mentioned as an allowable reason for leaving home or as an essential business exempt from the shutdown conditions. 20 states were recognized as having some form of a dental allowance.
We supplemented the state data with monthly local area unemployment estimates from the Bureau of Labor Statistics. We also include counts of COVID‐19 cases per week by state from the first reported cases in the week of January 20, 2020. Weekly deaths are also reported as part of a sensitivity analysis in predicting weekly visit changes.
2.2. SafeGraph
To measure visits to dentists' offices, we use data from the SafeGraph Patterns platform, which collects location data from points of interest (POIs) across the United States. The SafeGraph consists of high‐resolution cellular device data that tracks the geolocation of users of over 1000 apps, and links their movement to specific commercial establishments across space and time. The data combine information on more than 4 million POIs in the US on a daily basis. The data contain information on the POI location name, address, NAICS code, brand association, and business descriptor categories, as well as the volume of visits to each establishment. Though we are unable to track specific cellular devices across time, the data also contain lists of brands visited on the same day as the establishment.
We restrict the data to visits to dentist offices (NAICS 621210). One challenge of tracking visits to dental provider offices is that these are sometimes located in shopping malls or within other shopping venues. Though the geometry of each establishment allows for identification of adjacent businesses, to preclude confusion introduced by this co‐location and possible co‐visitation of establishments, we exclude dental offices with over 200 visits per week. This drops fewer than 1% of locations.
We aggregate the number of visits to each type of establishment at the county level and at the state level, and track them on a weekly basis. While stay‐at‐home orders constituted executive orders issued by the governor of the state, some counties enacted additional measures or more restrictive orders than the state. State orders superseded county orders where they were in conflict, with state orders setting minimum scope and county orders imposing additional restrictions. We chose to analyze the data at the weekly frequency to capture the rapidly changing nature of policy on coronavirus in the initial weeks and months after the virus was discovered.
The SafeGraph data comes with a number of limitations that are important to note. First, this data does not track every cellular device in the United States. This could lead to selection bias, as users which allow geolocation data may differ from others. To address this, SafeGraph has explored the potential sample bias by comparing volume of cellular devices tracked at state, county, and census block group level to the Census population counts at those geographies. Though SafeGraph does not collect any demographic indicators of device owners, they use the geographic representation of device homes to evaluate bias in average education, household income, and race compared to the Census. Though they show evidence of bias at every geographic unit, state and county aggregations have less bias than census block group. 8 Andersen et al. (2020) report that data engineers at SafeGraph report no significant changing in sample composition across time as individuals turn on and off tracked apps. Thus, we follow Andersen et al. (2020) and not adjust for sampling bias. Furthermore, this also motivates us to rely on state and county level analysis, as opposed to point of interest, to reduce any potential change in bias over time.
Second, the SafeGraph data is not a comprehensive count of visitors to any given location as, in addition to tracking only a sample of cellular device users, it does not track individuals without such devices. We address this limitation by looking at the change in the volume of visits throughout the period of analysis, rather than the number of visits. Furthermore, we normalize visits by using SafeGraph reported total number of devices to impute people‐per‐device weight for analyses, yielding an approximation of total visits by persons.
Third, the data allows us to know only that a visitor was within the premises of the dentist's office. We do not know if and what type of services were delivered. To the extent that the nature of visits to these establishment has not changed after March 2020, we believe the visits are an accurate proxy for care received.
2.3. Medicaid Claims
We use Medicaid dental claims for children born in Michigan between 2013 and 2015 from birth through the age of 5. In an exclusive agreement with the Michigan Department of Health and Human Services, these claims are linked to vital records for any eligible enrollees in the sample. The resulting combined dataset includes not only claims for all children within the cohort in the state, but also parental demographic characteristics (e.g., age, race, educational attainment). Furthermore, the data includes monthly eligibility confirmation, which allows us to observe not only claims, but also establish absence of claims by month by enrollee. Finally, though more than 97% of all dental claims are from managed care plans and lack payment information, we use the remaining fee‐for‐service claims to extrapolate payments to the managed care claims. 9 These data cover claims from 2013 to 2020 aggregated to the enrollee month level.
Using American Dental Association codes, we create categories of care and types of procedures. 10 We aggregate procedure codes into diagnostic (CPT D0100‐D0999), preventive (CPT D1110‐D1999), restorative (CPT D2140‐D2999), and endodontics (CPT D3110‐D3999). We also focus on specific types of procedures: oral evaluations (CPT D0120‐D0180), diagnostic imaging (CPT D0210‐D0395), tests and examinations (CPT D0414‐D0603), prophylaxis (CPT D1110‐D1120), fluoride treatment (CPT D1206‐D1208), sealant (CPT D1310‐D1354), spacers (CPT D1510‐D1999), amalgam (CPT D2140‐D2150), resin‐based composite (CPT D2330‐D2394), pulp cap (CPT D3110‐D3120), pulpotomy (CPT D3220‐D3222), endodontic therapy (CPT D3230‐D3240), extraction (CPT D7111‐D7251), emergency care (CPT D9110), sedation (CPT D9210‐D9248), consultation with a specialist (CPT D9310), inpatient treatment (CPT D9410‐D9450), and behavior management (CPT D9920).
Appendix Figure I1 plots the weekly counts of visits from SafeGraph against the weekly counts of claims in the Medicaid data at the state level (panel (a)) and the county level (panel (b)). The datasets are well‐aligned in at both state and county level, before and after March 2020.
2.4. Estimation Method
In the absence of randomly assigned stay‐at‐home treatments across a population, we take advantage of the variation in the orders to COVID‐19 between US states and counties to estimate a difference‐in‐differences (DD) specification. In the presence of conditional independence of assignment of treatment and parallel pre‐trends, the DD specification simulates an experimental setup with quasi‐random assignment of treatment and control. Thus, if these assumptions hold, we can infer a causal relationship between the stay‐at‐home orders and changing patterns in health care utilization.
Since the data used in this analysis allows for a longitudinal view of states and counties for more than 2 years prior and 4 months during the pandemic, we take advantage of the additional information of these repeated measurements to estimate a two‐way fixed effects DD model, specified as:
| (1) |
where are counts of visits for state/county, s, in week, t; the DD structure is captured by which is an interaction of indicators for time‐period starting in March 2, 2020 and states or counties which enacted policy of interest (stay‐at‐home, dental allowance). All specifications include local area unemployment in percentage terms at the state level; when dental allowance is the outcome of interest, the specifications also include the number of COVID‐19 cases at the state level and three lags thereof. These state characteristics are captured in . To account for unobservable time‐invariant state characteristics, such as weather, political leanings, public health infrastructure, and population compliance with policy, we include state or county fixed effects, . We also include week‐year fixed effects, , to remove variation attributable to economic, political, social, and health events which had a nationwide impact.
When evaluating stay‐at‐home policies, standard errors are clustered at state level for state analyses, and county level for county analysis, to account for heteroskedasticity and serial correlation at the treatment unit across time. Evaluations of the dental allowance orders include standard errors clustered at state level at both state and county level analysis as the treatment unit in both cases is the state.
To account for the measurement error inherent in the use of cellular device data, as mentioned in the previous section, as well as to account for population size differences between states, we define the outcome variable , in terms of log of visits in a given week within a state or county, as appropriate. The policies of interest are whether a state or county issued a stay‐at‐home order in March or April 2020, and whether such an order explicitly listed dental care as an allowable reason for leaving home.
2.5. Sensitivity and robustness of estimates
To test the parallel‐trends assumption needed for the causal interpretation of the DD estimate, we estimate an event study specification:
| (2) |
where the indicator for COVID‐19 period has been replaced by week‐year indicators for each time unit. The resulting analysis, as expressed in graphical format, tracks the weekly difference between states or counties which enacted the policy of interest to those that did not.
We also performed two stratification exercises. First, we separated the sample by weekend and weekday. We believe that weekend visits to dentist offices are more likely to be emergent in nature, while those during the week are more likely to be scheduled ahead and consist of routine and preventive care.
Second, we separate states according to metropolitan status of an area. In the absence of Census classification, we assign states to be more metropolitan if they have above median population density. 11 For counties, we use Census designation of metropolitan, micropolitan, and non‐metropolitan in stratifying analyses. In the first months COVID‐19 spread primarily in urban and metropolitan areas, such as Washington, New York, and Michigan, motivating more draconian measures in these states. Stay‐at‐home measures may have had a deeper impact in these states compared to those which are less metropolitan.
2.6. Mechanisms
To better understand how dental care changes during this period, we compare Medicaid claims composition for dental care among children before and after March 2020 in Michigan. We estimate a linear specification:
| (3) |
where is an outcome of medical utilization. is an indicator for all months starting in March 2020. Individual characteristics, such as child's gender, and maternal race, education, and age are represented by . As children age through the data, we capture cohort specific trends using which includes birth month and birth year fixed effects. To account for seasonal variability in use of dental services, we also include as month fixed effects and year fixed effects. Standard errors are clustered at the individual level.
As claims are aggregated to monthly sums per child, we analyze the following outcomes of interest: total claims, total payment, categories of claims (diagnostic, preventive, restorative, endodontics), and procedures by type (e.g., imaging, sealant). In the analysis, we consider both the count of claims, as well as the presence of a claim. While we report the estimates for presence of any claim, the results by count are available in Appendix D.
3. RESULTS
3.1. Google searches
Prior to reporting on the results of analysis of foot traffic data, we use Google Trends data to explore social awareness of restrictions imposed on dental care by the stay‐at‐home orders. We track searches for “dentist”, which we believe reflect individual interest in looking for dental care. 12
Google Trends reports the relative volume of searches for the given geographic area (state) and the time‐period specified (January 2018–June 2020) in the form of an index ranging from 0 to 100 at a weekly frequency. The index assigns a value of 100 to the week with the highest volume of searches and assigns values with respect to this peak volume for other weeks in the period. Weeks with searches below an unspecified level are censored to zero. To recover the relative volume of searches, we weigh the index by state population in 2018 and sum these across states according to presence of stay‐at‐home order and, separately, according to the presence of dental allowance. Finally, to account for the relative population size between states with and without stay‐at‐home orders, we compute the 3‐week moving average percent change in searches for each group.
Figure 2 presents the percent change in unadjusted weighed searches separated by presence of a stay‐at‐home order during this period (Panel a), and separated by presence of a dental allowance (Panel b). Panel (a) in the figure shows a cyclicality of searches with spikes in July, December, and January; in March 2020 searches declined in all states, whether these had stay‐at‐home orders or not. Panel (b) compares searches in states with a dental allowance to those without. In this panel, all states had enacted some form of a stay‐at‐home order which is reflected in the deep decline in searches in March 2020. While states with a dental allowance appear to lead by about a week, the decline is the same in these states than those without. The subsequent analysis will attempt to explore this trend using foot traffic data.
FIGURE 2.
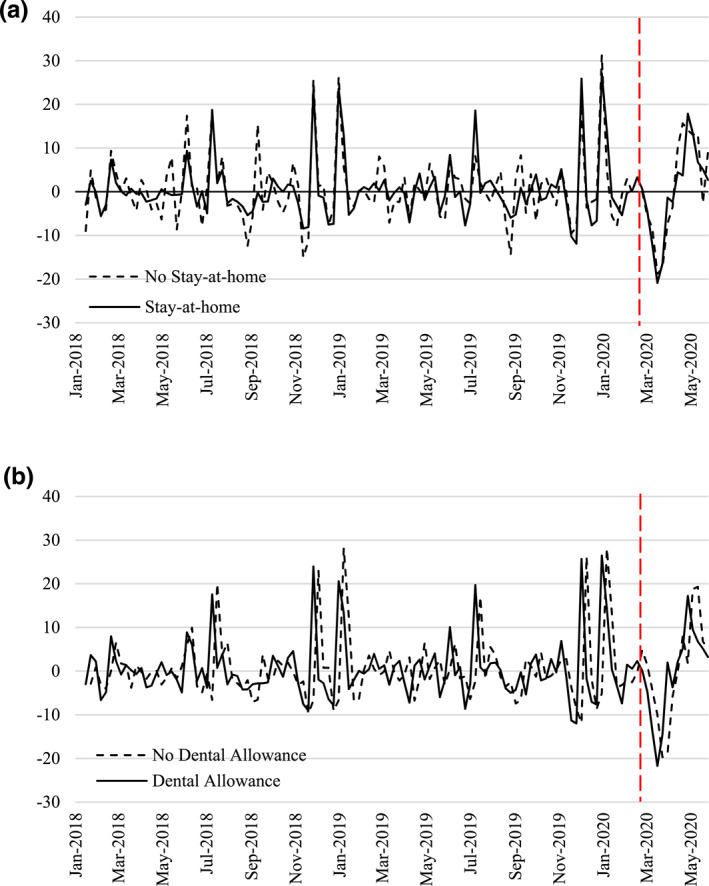
Google searches for “dentist”. (a) Stay‐at‐home versus no stay‐at‐home states. (b) Stay‐at‐home states with and without dental allowance (DA). Source: Google Trends Jan 2018–Jun 2020. Three week moving average change (in percentage) of index of search volume by state aggregated with population weights according to treatment status
3.2. State characteristics
Table 1 explores differences in dental visit volumes between states with and without a stay‐at‐home order (Panel A), and states with and without a dental allowance in their stay‐at‐home order (Panel B), before and after March 2020. Columns (1) and (2) present means before March 2020 for states with and without eventual stay‐at‐home orders, as well as differences in their means tested against the hypothesis of no difference; columns (3) and (4) present means after March 2020 with test of differences in means. States with stay‐at‐home orders are significantly different even before the pandemic: they have a higher population density and on average have a higher unemployment rate. Though these states have significantly more dental visits in total, they have fewer per capita visits and the differences are not statistically significant. States with dental allowances are smaller than other states with stay‐at‐home orders, and have fewer per capita dental visits. After March 2020, states with a stay‐at‐home order experienced a sharper rise in unemployment, parallel with a greater rise in per capita COVID‐19 cases. Though both types of states experience a decline in dental visits per capita, states with stay‐at‐home orders experience a steeper decline than those without, widening the difference from 5.2 visits to 9.06 visits per 10,000.
TABLE 1.
Characteristics of states by their stay‐at‐home status
| Before | After | ||||||
|---|---|---|---|---|---|---|---|
| (1) | (2) | (2)‐(1) | (3) | (4) | (4)‐(3) | ||
| No order | Order | Difference | No order | Order | Difference | ||
| Panel A: Stay‐at‐Home Orders | |||||||
| Unemployment | 3.33 | 3.79 | 0.46*** | 7.7 | 10.34 | 2.64*** | |
| Population density | 101.9 | 472.5 | 370.6*** | 101.9 | 472.5 | 370.6*** | |
| ln(Cases) | 8.81 | 9.43 | 0.619*** | ||||
| Dental visits | 22,614 | 28,722 | 6108 | 17,702 | 19,661 | 1959 | |
| Dental visits per capita* | 46.34 | 41.14 | −5.2 | 38.02 | 28.96 | −9.06 | |
| Panel B: Dental Allowance | |||||||
| Unemployment | 3.91 | 3.68 | −0.23*** | 9.97 | 10.72 | 0.75*** | |
| Population density | 737 | 208.1 | −528.9*** | 737 | 208.1 | −528.9*** | |
| ln(Cases) | 9.16 | 9.7 | 0.539*** | ||||
| Dental visits | 23,412 | 34,032 | 10,620 | 17,163 | 22,160 | 4997 | |
| Dental visits per capita* | 41.77 | 40.5 | −1.27 | 29.83 | 28.08 | −1.75 | |
Notes: Panel (A) compares states with stay‐at‐home orders with those without, before and after March 2020. Panel (B) compares states with dental allowance to those without, before and after March 2020. Column (1) includes means from states without and column (2) with the specified order, before the pandemic, and the difference between these in the next column with a t‐test of no significance. Column (3) and (4) include means from states without and with the specified order after the pandemic, and the difference between these in the next column with a t‐test of no significance. Per capita is per 10,000 persons.
***p < 0.01, **p < 0.05, *p < 0.10.
Source: SafeGraph Patterns 2018–2020.
For the purposes of our analysis, we assume that the stay‐at‐home policies were exogenous to the volume or use of dental services within the state. Similarly, we believe that the allowance of dental services from the stay‐at‐home restrictions are independent of its volume of utilization. However, in light of the differences between the states we are motivated to carefully account for time‐invariant state characteristics using fixed effects, as well as time‐variant state characteristics such as the monthly unemployment rate.
3.3. Main results
We present our main DD results in Table 2 for visits to dentist offices. Panel A presents results aggregated at the state level, while Panel B presents the same analysis aggregated at the county level. DD estimates are presented for all visits (columns (1) ‐(2)), weekday versus weekend (columns (3) ‐(4)), and more versus less metropolitan (columns (5) ‐(6)). While column (1) presents estimates for visits per 10,000 population, the nature of the SafeGraph data does not allow for reliable interpretation of levels, making log of visits (column (2)) our preferred specification followed through all remaining analyses. We estimate a 14.5% decline at state and 12.3% decline at county level in visits in the post‐pandemic time period. Both weekday and weekend visits decline by similar proportions, however, while less metropolitan states drive the effects at the state level (12.8%), at the county level of analysis metropolitan shows the largest magnitude of change (13.3%).
TABLE 2.
Difference‐in‐differences estimates for stay‐at‐home order at state and county level
| All | Weekday | Weekend | Metropolitan | Non‐metropolitan | ||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Visits per 10,000 pop | Log visits | Log visits | Log visits | Log visits | Log visits | |
| Panel A: State | ||||||
| Stay‐at‐Home*After | −3.606* | −0.145*** | −0.144** | −0.157*** | −0.095 | −0.128*** |
| (2.059) | (0.053) | (0.054) | (0.052) | (0.112) | (0.036) | |
| R‐squared | 0.888 | 0.993 | 0.993 | 0.992 | 0.983 | 0.994 |
| Obs. | 6681 | 6681 | 6681 | 6681 | 3275 | 3406 |
| Dependent variable mean | 40.705 | 9.607 | 9.461 | 7.577 | 10.123 | 9.111 |
| Panel B: County | ||||||
| Stay‐at‐Home*After | −0.082** | −0.123*** | −0.124*** | −0.121*** | −0.133*** | 0.015 |
| (0.037) | (0.017) | (0.017) | (0.018) | (0.026) | (0.080) | |
| R‐squared | 0.934 | 0.962 | 0.962 | 0.907 | 0.979 | 0.03 |
| Obs. | 353,575 | 353,575 | 352,109 | 321,792 | 146,990 | 125,781 |
| Dependent variable mean | 0.769 | 4.565 | 4.418 | 2.824 | 5.71 | 3.135 |
Notes: The dependent variable in (1) is the sum of weekly visits at the state (panel A) or county (panel B) level to dental offices, normalized by state or county population. The dependent variable in (2)‐(6) is the log of the sum of weekly visits at the state (panel A) or county (B) level to dental offices. Each analysis also includes indicator for after March 1, 2020, an indicator for states (or counties) that issued stay‐at‐home orders, state unemployment level, state (Panel A) and county (Panel B) fixed effects, and week‐year fixed effects. States are defined as metropolitan if they have above median population density per American Community Survey estimate for 2019. Counties are defined as metropolitan using Census Bureau definition. Standard errors are clustered at the state level in Panel A and county level in Panel B.
***p < 0.01, **p < 0.05, *p < 0.10.
Source: SafeGraph Patterns 2018–2020.
Shifting attention toward the wording of the orders, Table 3 compares visits in states that mention dental care as an allowance in stay‐at‐home orders to those that do not. The estimates show no differences at state level or county level at conventional levels of statistical significance. However, non‐metropolitan areas appear to experience 10.9% decline in visits compared to states without dental allowances, when analyzed at the county level. The lack of statistical significance in most of these results allows us to rule out positive effects of meaningful magnitude.
TABLE 3.
Difference‐in‐differences by allowance of dental visits from stay‐at‐home order
| All visits | Weekend | Weekday | Metropolitan | Non‐metropolitan | ||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Visits per 1000 pop | Log visits | Log visits | Log visits | Log visits | Log Visits | |
| Panel A: State | ||||||
| Dental Allowance*After | −0.34 | −0.022 | 0.007 | −0.027 | 0.103 | −0.073 |
| (2.188) | (0.056) | (0.052) | (0.057) | (0.095) | (0.061) | |
| R‐squared | 0.876 | 0.993 | 0.992 | 0.992 | 0.982 | 0.994 |
| Obs. | 5240 | 5240 | 5240 | 5240 | 1965 | 3275 |
| Dependent variable mean | 39.467 | 9.68 | 7.656 | 9.532 | 10.487 | 9.195 |
| Panel B: County | ||||||
| Dental Allowance*After | 0.048 | −0.066 | −0.011 | −0.076 | −0.047 | −0.109** |
| (0.076) | (0.045) | (0.040) | (0.046) | (0.050) | (0.043) | |
| R‐squared | 0.929 | 0.965 | 0.914 | 0.965 | 0.979 | 0.846 |
| Obs. | 261,258 | 261,258 | 239,591 | 260,341 | 120,571 | 81,735 |
| Dependent variable mean | 0.792 | 4.72 | 2.944 | 4.575 | 5.763 | 3.156 |
Notes: Sample restricted to states with stay‐at‐home orders. The dependent variable in (Equation 1) is the sum of weekly visits at the state (Panel A) or county (Panel B) level normalized by population and in (2)‐(6) the log of sum of visits to dental offices. Each analysis also includes indicator for after March 1, 2020, an indicator for states that included a dental allowance in their stay‐at‐home orders, state unemployment level, state (Panel A) and county (Panel B) fixed effects, and week‐year fixed effects. States are defined as metropolitan if they have above median population density per American Community Survey estimate for 2019. Counties are defined as metropolitan using Census Bureau definition. Standard errors are clustered at the state level for both Panel A and B.
***p < 0.01, **p < 0.05, *p < 0.10.
Source: SafeGraph Patterns 2018–2020.
3.4. Event study
Figure 3 show the weekly differences between states with and without a stay‐at‐home order between September 2019 and June 2020. Each point corresponds to a coefficient estimate of the adjusted difference in reference to the last week in February 2020, marked by the red dashed line. The 95% confidence intervals for the estimate are reported by bands around the estimate. Panel (a) shows a decline in dentist visits starting in the first week of February, well before the first state‐wide stay‐at‐home orders, but experiences the sharpest decline in the first week of March 2020. Visits remain low through the end of May 2020, when many of the orders were lifted, and do not regain the levels seen in February. Weekday visits (Panel (b)) drive the bulk of the overall trend, but even weekend visits (Panel (c)) experience the same sharp decline. The latter is surprising since weekend dentist visits are more likely to represent emergency dental care and, hence, are more sensitive to delays in care. Appendix Figure B1 shows the results of the event study at county level for all, weekend/weekday visits. While the estimates are more noisy, the declines are similarly significant and persistent through the stay‐at‐home period. Appendix Figure B2 presents estimates of the event study stratified by metropolitan, micropolitan, and non‐metropolitan classification of county. These results emphasize that the largest changes in visits occurred in metropolitan areas.
FIGURE 3.
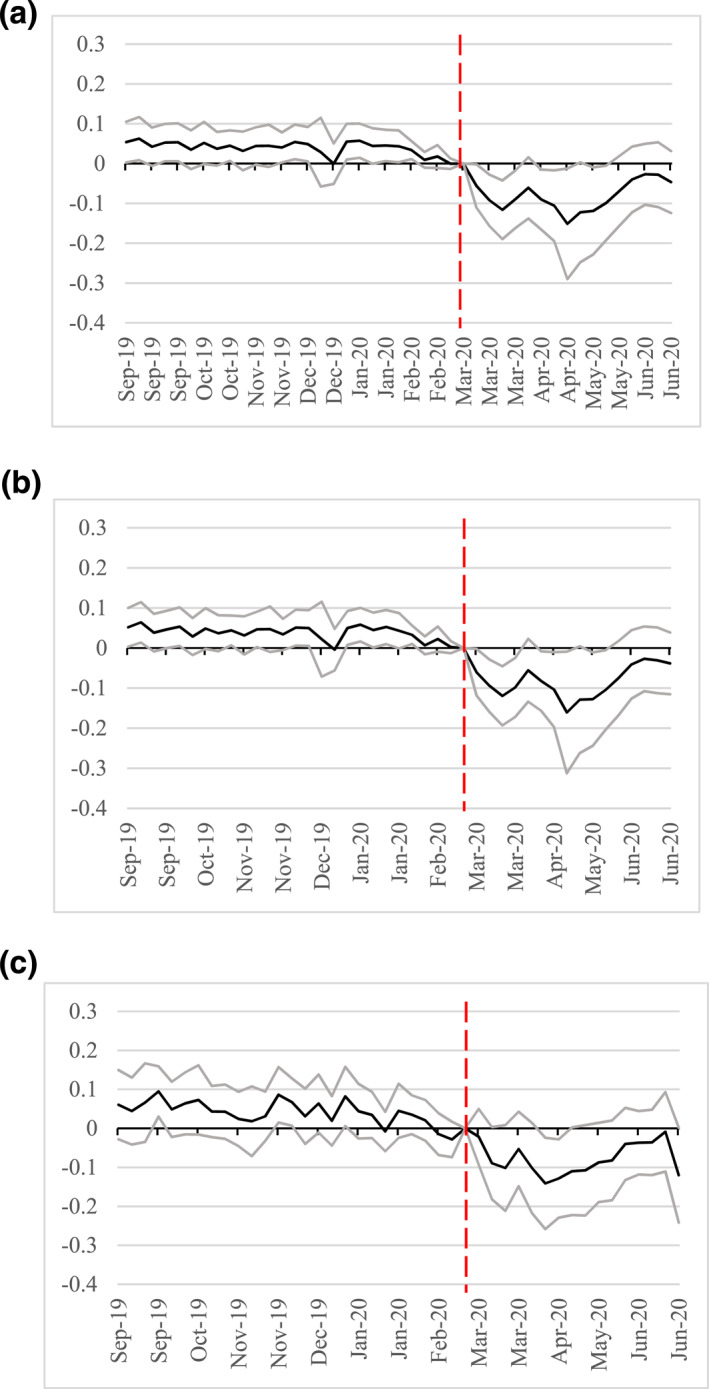
Event study of stay‐at‐home orders on dental visits. (a) All visits. (b) Weekday visits. (c) Weekend visits. The dependent variable is the log of visits to dental offices. Each point is the estimated weekly difference between states with and without a stay‐at‐home order, relative to the last week of February 2020, adjusted for state unemployment level, state fixed effects, and week‐year fixed effects. Confidence intervals, clustered at the state level, reported around point estimate. Source: SafeGraph Patterns 2018–2020.
Figure 4 shows the effect of the order with and without a dental allowance. While the DD results showed no statistically significant difference between these states, panel (a) shows that states with a dental allowance experienced an 8% decline in visits in the initial weeks, and the difference persists through the duration of these orders. While these estimates lose statistical significance at conventional levels in May, the magnitude of the effects remain consistent throughout the period. However, when stratifying the analysis between weekend and weekday, we see that these differences emerge from weekday visits exclusively, with no discernible differences in weekend utilization. County level analysis shown in Appendix Figure A5 show similar trends.
FIGURE 4.
Event study of dental allowance order on dental visits. (a) All visits. (b) Weekday visits. (c) Weekend visits. The dependent variable is the log of visits to dental offices. Each point is the estimated weekly difference between states with and without a dental allowance in their stay‐at‐home order, relative to the last week of February 2020, adjusted for state unemployment level, state fixed effects, and week‐year fixed effects. Confidence intervals, clustered at the state level, reported around point estimate. Source: SafeGraph Patterns 2018–2020.
Stratification of the dental allowance by metropolitan status of state or county shows a difference in behavior. At the state level, Appendix Figure C1 shows that states with large metropolitan areas experienced no difference in visits in the presence of a dental allowance, but recovered swiftly (and even appear to have caught up on visits at the end of May and June); states with fewer metropolitan areas, however, had an approximate 8%–16% decline when dental allowance was included in the stay‐at‐home order through all post‐period weeks. At the county level (Appendix Figures C2 and C3) the estimates show deeper declines in states with dental allowances for both metropolitan and micropolitan counties.
In all figures, we observe that while differences existed between states prior to February 2020, these differences appear to be constant across time, satisfying the parallel trends assumption. To understand these pre‐trends better, we conduct two additional analyses in Appendix L. Recognizing that the months since the first news of COVID and the imposition of stay‐at‐home orders may have involved some voluntary adjustment in visits to dental offices, we separate the pre‐period into January 2018–November 2019 and December 2019–February 2020. In panel (a) of Appendix Figure L1 the December 2019–February 2020 period is omitted and the event study selects the last week of November 2019 as the reference period. Though a visual inspection shows no evidence of a pre‐trend, the F‐test of joint significance of pre‐period is significant at 0.1% level. In panel (b) the event study is repeated using the December 2019–February 2020 pre‐period only. Here, while the visual inspection suggests some modest pre‐trend, their joint significance is rejected by an F‐test at conventional levels. We conclude that prior to the pandemic there is no consistent evidence of a pre‐trend, though there may have been some adjustment in the months leading up to the stay‐at‐home orders. 13
3.5. Dental claims
Table 4 summarizes the estimates of changing Medicaid dental claims after March 2020. Estimates are reported for claims (columns (1)‐(2)) and payment (columns (3)‐(4)) totals as well as at the extensive margins. Consistent with the foot‐traffic data, we find a 5.5% point decline in likelihood of a claim or payment, which constitutes about 0.25 visits per month per enrollee. The average monthly payment per enrollee declined by $5.7 in March.
TABLE 4.
Medicaid dental claims before and after March 2020, Michigan
| Claims | Payment | |||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| # Count | Any | $ amount | Any | |
| After Mar 2020 | −0.2500*** | −0.0559*** | −5.7845*** | −0.0559*** |
| (0.0045) | (0.0007) | (0.1994) | (0.0007) | |
| R‐squared | 0.024 | 0.034 | 0.006 | 0.033 |
| Obs. | 9,287,674 | 9,287,674 | 9,287,674 | 9,287,674 |
| Dependent variable mean | 0.2318 | 0.0587 | 5.5428 | 0.0587 |
Note: The dependent variable in (1) and (2) are the total count and any claims per month per enrollee; in (3) and (4) it is the dollar total and any payments made per month per enrollee. Each specification also includes demographic variables (gender, maternal age, race, and education), fixed effects for birth month, birth year, claim month, and claim year. Standard errors are clustered at individual level.
***p < 0.01, **p < 0.05, *p < 0.10.
Source: MDHHS Medicaid Claims, Children 0–5, 2013–2020.
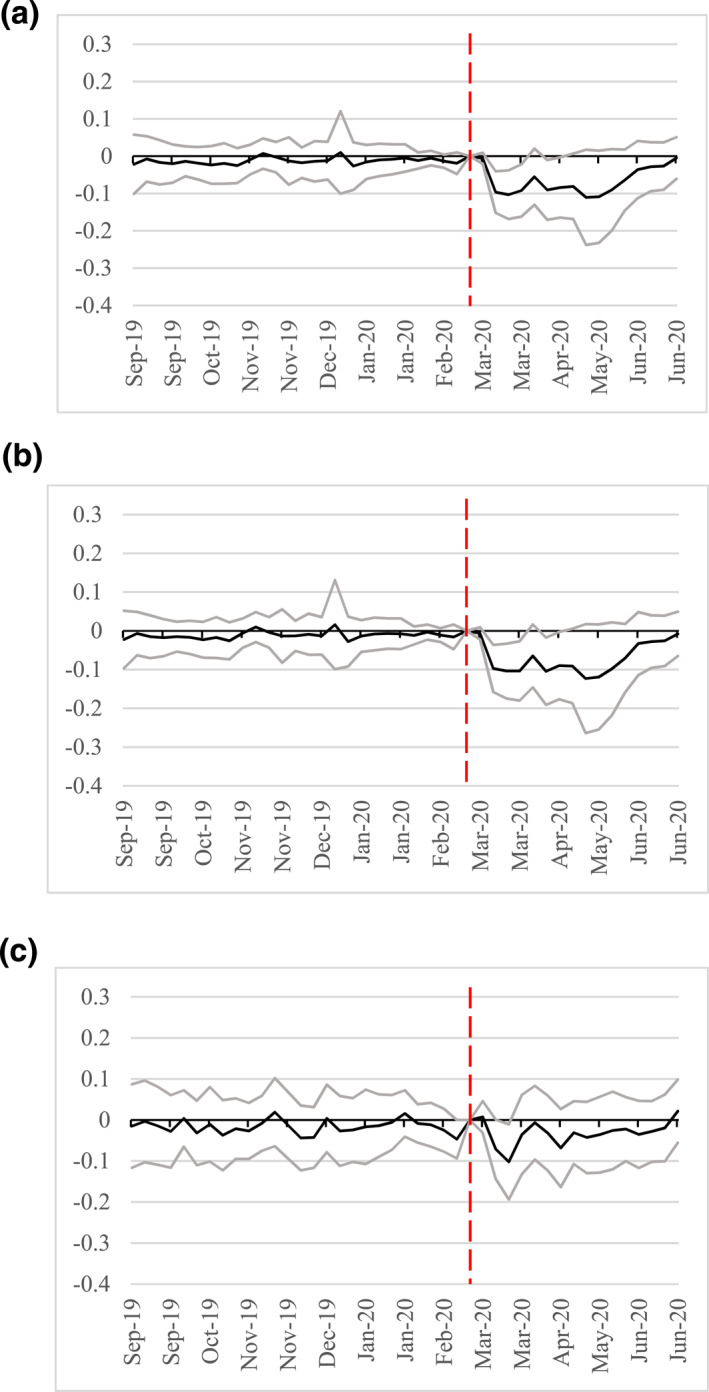
Stratifying by category of care (Panel (a)) and type of procedure (Panel (b)), Figure 5 plots the coefficient estimates for specification (3), showing claims for diagnostic and preventive care decrease by 4.4 pp and 4.1 pp respectively. Restorative care declines by 1.4 pp, while endodontic care hardly changes. Procedures show a similar pattern: prophylaxis, fluoride treatment, evaluation decrease by almost 4 pp, imaging decreases by two pp, while more acute and urgent procedures show little change. Estimates of count of claims by category and type are very similar in effect and magnitude and are shown in Appendix Figure D1.
FIGURE 5.
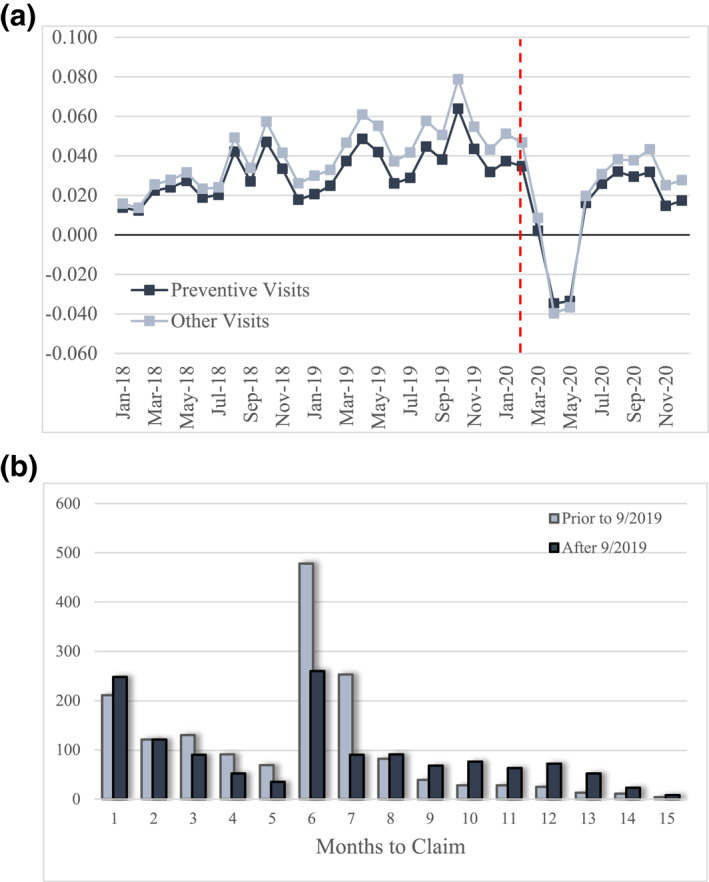
Preventive care through the pandemic. (a) Adjusted time trends for preventive and non‐preventive visits. (b) Months to claim for preventive visit. In panel (a), total number of preventive visits are adjusted for child demographic characteristics (gender and maternal age, race, and education), and birth month and birth year. Standard errors are clustered at individual level. Panel (b) shows frequency of number of months between preventive claim visits in the pre‐pandemic period (May 2018‐August 2019) in light blue, and the post‐pandemic period (September 2019‐December 2020). September 2019 was chosen as the start of the post‐pandemic period because a preventive visit in March 2020 would have followed one 6 months prior, in September 2019. Source: Michigan Department of Health and Human Services (MDHHS) Medicaid Claims, Children 0‐5yo 2013–2020.
Figure 6 examines missed preventive care in greater detail. Panel (a) shows monthly probability of a preventive care, relative to other visits, adjusted for child's demographic characteristics (gender and maternal age, education, and race) and birth year and month. The effect of the stay‐at‐home orders impact preventive care visits in two ways: first, there is a sharp and sustained decline in preventive visits between March and May; second, though preventive visits rise starting in June, their incidence does not return to pre‐pandemic seasonal trends.
FIGURE 6.
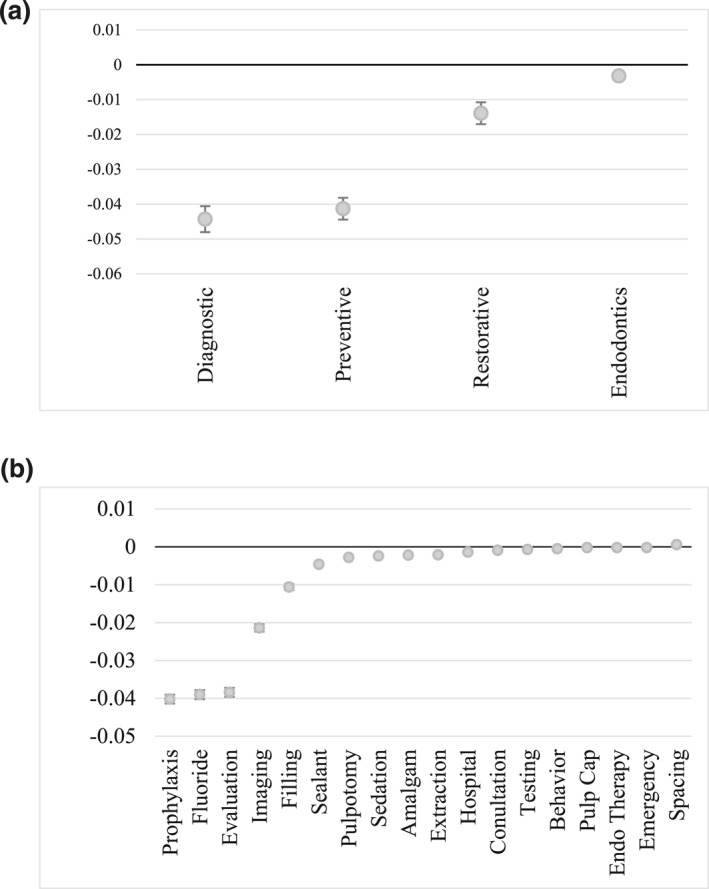
Medicaid dental claims by type. (a) Any procedure by category of care. (b) Any procedure by type of care. Each point represents the coefficient of a separate regression estimating the effect of post‐March 2020 on probability of a claim for specified procedure. The dependent variable is an indicator whether procedure was performed in the month for child. Each regression also includes demographics (gender and maternal race, age, and education), and indicators for birth month, birth year, claim month, and claim year. Standard errors are clustered at individual level, and are represented by whiskers around the coefficient estimate. Source: Michigan Department of Health and Human Services (MDHHS) Medicaid Claims, Children 0‐5yo 2013–2020.
Panel (b) depicts the distribution of time in months between preventive visits. To construct this distribution, we assumed that a preventive visit which should have occurred in March 2020 would have been a return visit for one conducted in September 2019, six months prior. Thus, the first set of on schedule preventive visits to be canceled would have been those which originated in September 2019, allowing us to set the post‐pandemic period accordingly. The light blue bars in Panel (b) show that prior to the pandemic, the modal number of months between successive preventive visits was 6 months, followed by 7 months. In the post‐pandemic period, while 6 months remains the modal months to preventive visit, the number of visits constitute a fraction of those seen in the pre‐pandemic period. Similarly, visits at 7 months were similarly very low. The difference in visits allows us to estimate that approximately 381 visits should have occurred in March and April, which were missed. Starting in May 2020, however, visits rise above the pre‐period monthly counts, suggesting that, indeed, some preventive visits were rescheduled in the months that followed. Netting the missed visits during the stay‐at‐home period against the rescheduled visits in the remainder of the year, we estimate that 158 visits, or 41.4% of missed visits, never occurred in the remaining months of the year.
3.6. Robustness analyses
We perform several robustness checks to evaluate the sensitivity of our estimates to the choice of specification.
3.7. Staggered implementation
We check the sensitivity of our estimates to the staggered implementation of the stay‐at‐home orders using the Callaway and Sant’Anna (2021) weighted difference‐in‐differences method. The results presented in Appendix Table H1 show that while the group of states which implemented the stay‐at‐home order in the second week of March 2020 experienced the largest effect (−18.7%) on visits to dental offices, states which implemented in the weeks that followed had a much smaller effect as seen in event study in Appendix Figure H1. Overall, the estimate using this method is more modest, showing a 5.2% decline for all states which implemented the stay‐at‐home order.
3.8. Policy timing
We note that while the data used in this analysis spans January 2019 to June 2020, the stay‐at‐home orders were implemented in March 2020 and lifted in most states by June 1, 2020. Appendix Table A1 splits the post period into March 2020–May 2020 and post‐May 2020. The estimates for log visits show a 15.6% decline in visits in the immediate stay‐at‐home period, and a 11.3% decline in the post‐May period compared to the pre‐period.
We also explore the importance of the ban on elective procedures as the trigger for declining dental visits. In Appendix Table F1, we report estimates for the period after the ban at both state and county level, for states with eventual stay‐at‐home orders, and those with dental allowances. We find no significant effect of the ban on procedures on dental visits at state level, though county level estimates are much more precise. This is consistent with the observation that there was some anticipation in the month of February, but the bulk of the effect occurred upon the implementation of the stay‐at‐home policies.
3.9. Dental office closures
Stay‐at‐home orders may have primarily affected the operation of dental offices, preventing patients from receiving the care they sought. To explore this, we estimate Equation (1) for the log of the count of dental offices at county level with any visits during this period. The results reported in Appendix Table E1 show a 2.4% decrease in the number in dental offices with any visits in states with stay‐at‐home order, and a 1.5% decrease in the number in states which included a dental allowance in their stay‐at‐home order.
3.10. Dental allowance
To better understand the effect of dental allowances on visits, we examine the effect of these policies on visits to physician offices in these states in Appendix Table C1. We find that dental allowances did not have any effects on visits to physician offices–both in terms of statistical significance of the estimates, but also estimated effect magnitude.
3.11. Cross‐border spillovers
Turning to the Medicaid claims, we explore the possibility that the stay‐at‐home order in Michigan may have motivated parents to take their children to dental clinics out of the state. Appendix Table D1 explores the share of out‐of‐state claims after March 2020, showing a decline of 0.47% points in any such claims. We also estimate a difference‐in‐differences estimate comparing children with to those without out‐of‐state claims after March 2020. These estimates in columns (2)‐(5) show that while all out of state claims declined by 0.23 claims after March 2020, children with out‐of‐state providers had 0.75 more claims. Surprisingly, despite this increase, the total payment for out‐of‐state use declined by $9.4 per enrollee per week during this period. To explore this more fully, Appendix Table D2 re‐estimates the difference‐in‐differences specification for children with and without out‐of‐state claims after March 2020, by type of care provided (diagnostic, preventive, restorative, or endodontic). As with the total, while out‐of‐state use declines for all categories of care, we estimate significant differential increase in diagnostic (1.4pp), preventive (3.0pp), and restorative (3.1pp) care for children with any out‐of‐state claims. Though preventive and restorative have the largest percentage point increase, the relative magnitude is greatest for restorative care which constitutes more than doubling of out‐of‐state claims compared to pre‐pandemic levels. This suggests that while children with any out‐of‐state claims were more likely to seek care during the stay‐at‐home order, these tend to be restorative dental care, rather than preventive or diagnostic.
3.12. Sample definitions
We test the sensitivity of our estimates to definition of metropolitan states, censoring of office visits, and definition of control group. Appendix Table G1 defines metropolitan states as those with population density above 75th percentile, with results consistent main estimates.
Appendix Table J1 re‐estimates the main specification without removing dental offices with more than 200 weekly visits. The magnitude of estimated effects is somewhat greater suggesting that those we present in Tables 2 and 3 are conservative.
Kentucky and Connecticut implemented closure of essential businesses, though did not impose a stay‐at‐home mandate. These states are included in the control group in the main analysis, but are excluded from the sample in Appendix Table K1. The estimated effects are greater, suggesting that the preferred estimates in Table 2 are conservative.
We also test the sensitivity of our estimates to inclusion of employees among visits to dental offices. Appendix Table M1 re‐defines visits exclusive of those lasting longer than 240 min. The estimates are consistent with our preferred specification.
3.13. Imputing population effects
To address the data limitation of device–not people–counting, we implement an imputation exercise using population and device counts by state and county. SafeGraph provides a weekly number of devices for each census block group from January 2019 to June 2020. Using this shorter panel, we compute the weekly device‐per‐capita counts at state and county level, with annual population estimates from the American Community Survey 2019. We use these weights with the raw number of visits to obtain an estimate of the total number of people who visited dentists' office (with or without devices). The estimates of the preferred specification, in Appendix Table N1, are attenuated with up to a 7.3% decline in visits over this period.
4. DISCUSSION
We estimate that visits to dentist offices declined by up to 14.5% following the stay‐at‐home orders. While we expected these orders to result in a more modest decline in urgent dental visits, weekend visits declined by 15.7%. To the extent that some of this decrease is attributable to the 2.4% decrease in the count of dental offices in operation, we estimate a net 12.1% decrease in demand for dental visits. This estimate is comparable to other estimates of outpatient care. Ziedan et al. (2020) estimate an overall 40% decline in outpatient visits starting in February 2020, of which 15%–16% they attribute to the stay‐at‐home policies.
We also find that inclusion of dental allowance in stay‐at‐home orders does not generate the intended effect. At state and county level we find no evidence of significant positive effect of the policy, and estimate a 10.9% decline in non‐metropolitan counties.
What was happening to these visits? The analysis of dental claims shows that preventive and diagnostic are the categories of care with the largest declines. Analyses of timing of dental care in the claims data suggests that approximately 41.4% of visits which were missed during the stay‐at‐home order were never caught up in the remaining months of 2020. We estimate the cumulatively, more than 110,000 visits were missed in the SafeGraph data nationally by the end of June 2020 as seen in Appendix Figure B3. As this represents a fraction of true magnitude of visits, we interpret it with due caution. We conclude, therefore, that while some missed care was delayed, a sizable share of these was, indeed, foregone care.
This finding is consistent with the nature of dental care. According to a 2018 survey conducted by the American Dental Association, 52% of those surveyed made their most recent appointment for a regular check‐up. 14 The frequency and timing of these visits is rigidly regulated by insurance design, filling up dental appointment times months in advance. Thus, it is much easier to cancel a missed appointment than to try to reschedule it. As with other types of health care, Medicaid beneficiaries are more likely to face difficulties in rescheduling such care.
These missed visits are likely to have short‐ and long‐term effects on both dental as well as overall health. First, Medicaid beneficiaries are more likely to use the emergency department for care (Hsia et al., 2014), highlighting the tenuous link with primary and preventive care in this population. The beneficiaries may not reschedule these canceled appointments, severing an already weak link with the dentist. Second, Lee et al. (2020) use Florida Medicaid dental benefit reimbursement expansion for pediatric patients to estimate that an 11.4 pp (22.5%) increase in preventive visits is correlated with a 0.3% point (73.1%) decrease in emergency department visits for caries. We estimate a 5.4% point decrease in preventive visits in Michigan and a 15.4% decrease in visits overall, nationally during the stay‐at‐home order. Thus, using these estimates, we can project an approximately 0.14–0.20% point increase in emergency department visits for dental decay in the years ahead.
The limitations of this study stem from the opportunistic nature of the data used for analyses. Using SafeGraph data allows us to see foot‐traffic in the close proximity of a dental office for tracked cellular devices. This does not represent actual care received, nor prevents erroneous attribution of visits in the vicinity of a dental clinic. However, the SafeGraph data has been used extensively to evaluate stay‐at‐home policies and social distancing during the COVID‐19 pandemic (Castaneda & Saygili, 2020; Dave et al., 2020; Elharake et al., 2021; Gao et al., 2020; Kang et al., 2020; Yan et al., 2021), utilization of health care services (Andersen et al., 2020; Cantor et al., 2020), as well as unintended social and health outcomes (Bullinger et al., 2020; Chalfin et al., 2021).
5. CONCLUSION
Our analysis shows that dental visits, and preventive dental care in particular, experienced a sharp decline in the spring of 2020, as stay‐at‐home orders discouraged unnecessary medical care. If dental care is representative of other outpatient and preventive care, such declines are justifiable as part of mitigation strategies given the scale and fatality of the COVID‐19 pandemic. However, we fail to find evidence of visits returning to pre‐pandemic levels once the orders were lifted, and our analysis of claims through the end of 2020 suggest that a sizable share of the preventive visits was never rescheduled. While declining dental care is an important predictor of future adverse health events, it is also a bellwether for other forms of preventive care which have likely seen similar magnitude of declines. Such declines in access and use of other preventive care services predict a much greater decline in public health as years of advances in screenings, maintenance, and treatment will be offset by this disruption. These results motivate an active public health initiative to regain the momentum in preventive care now and following future pandemic mitigation measures, particularly in vulnerable and underserved communities.
CONFLICT OF INTEREST
The author declares that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Supporting information
Supporting Information S1
ACKNOWLEDGMENTS
The authors gratefully acknowledge support from Dr. Phillip Levy, and the Office of the Dean of College of Liberal Arts and Sciences at Wayne State University. The authors are grateful to Dr. Allen Goodman, participants of the Health Economics Research Analysis group, the University of Michigan H2D2, Vanderbilt University Virtual VAEM Seminar Series, and Office of the Chief Economist Seminar Series of Bureau of Economic Analysis seminar participants. Thomas Wilk received support from Health Economics Research and Analysis group, Dr. Phillip Levy, and the Office of the Dean of College of Liberal Arts and Sciences at Wayne State University.
Danagoulian, S. , & Wilk, T. A. (2022). Locking out prevention: Dental care in the midst of a pandemic. Health Economics, 31(9), 1973–1992. 10.1002/hec.4558
ENDNOTES
Gamio, Lazaro “The Workers Who Face the Greatest Coronavirus Risk” The New York Times March 15, 2020. Accessed on March 25, 2021. URL: https://www.nytimes.com/interactive/2020/03/15/business/economy/coronavirus‐worker‐risk.html
ADA News “Survey: More Americans want to visit the dentist” March 1, 2018. Visited on March 25, 2021. URL: https://www.ada.org/en/publications/ada‐news/2018‐archive/march/survey‐more‐americans‐want‐to‐visit‐the‐dentist
In the context of the Grossman health capital model, preventive dental care constitutes a direct investment into future health.
Healthy People 2030 “Oral Condition” https://health.gov/healthypeople/objectives‐and‐data/browse‐objectives/health‐care/increase‐use‐oral‐health‐care‐system‐oh‐08 Accessed May 54, 2021.
Healthcare.gov “Dental Coverage in the Marketplace” Accessed 4/6/2021. https://www.healthcare.gov/coverage/dental‐coverage/
Elizabeth Hinton and Julia Paradise “Access to Dental Care in Medicaid: Spotlight on Nonelderly Adults” in Kaiser Family Foundation Issue Brief. March 17, 2016. Accessed 4/23/2021. URL: https://www.kff.org/medicaid/issue‐brief/access‐to‐dental‐care‐in‐medicaid‐spotlight‐on‐nonelderly‐adults/
Registered trademark of the Financial Industry Regulation Authority, Inc. Available at https://www.finra.org/rules‐guidance/key‐topics/covid‐19/shelter‐in‐place. Last accessed 2/25/2021.
More detail on SafeGraph analysis can be found at: https://colab.research.google.com/drive/1u15afRytJMsizySFqA2EPlXSh3KTmNTQ#sandboxMode=true&scrollTo=bqTCWW28_14k.
We attenuate managed care claims to 95% of fee‐for‐service amount to account for possible cost differences.
American Dental Association CDT‐2017 “Code on Dental Procedures and Nomenclature” Effective January 1, 2017. Accessed March 18, 2021. https://www.deltadentalco.com/uploadedFiles/ProviderFeeSchedules/DDCO_Par_Provider_Documents/CDT%202017_Code%20on%20Dental%20Proc_Nomenclature%20online.pdf
While we would prefer to use more rigorous method of classifying states according to metropolitan status designation, the Census Bureau does not provide such classification at the state level. States are defined as more metropolitan if they have above median population density per American Community Survey estimate for 2019. We check sensitivity of our findings to this definition by designated states as metropolitan if above 75th percentile in population density in Appendix Table G1.
Google Trends query data has been previously used to track social awareness. See Chalfin et al. (2019) and Agüero and Beleche (2017).
We also test pre‐trends using the pre‐trend testing method proposed by Rambachan and Roth (2022), implementing it using their proposed code. Though the results of this analysis are presented in Appendix Figure L2 and Appendix Table L1, we do not draw inference from these results as the challenges of parameter selection, model specification, coding implementation do not allow a complete understanding of the implication of these estimates.
ADA News “Survey: More Americans want to visit the dentist” March 1, 2018. Visited on March 25, 2021. URL: https://www.ada.org/en/publications/ada‐news/2018‐archive/march/survey‐more‐americans‐want‐to‐visit‐the‐dentist
DATA AVAILABILITY STATEMENT
The SafeGraph data used in most of the analysis is available by request from https://www.safegraph.com/. The Medicaid claims data is subject to data use agreement with the Michigan Department of Health and Human Services (MDHHS) and cannot be shared. These data are available upon application to MDHHS.
REFERENCES
- Agüero, J. M. , & Beleche, T. (2017). Health shocks and their long‐lasting impact on health behaviors: Evidence from the 2009 H1N1 pandemic in Mexico. Journal of Health Economics, 54, 40–55. 10.1016/j.jhealeco.2017.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen, M. , Bryan, S. , & Slusky, D. (2020). COVID‐19 surgical abortion restriction did not reduce visits to abortion clinics. National Bureau of Economic Research Working Paper Series No. 28058. 10.3386/w28058 Retrieved from http://www.nber.org/papers/w28058 [DOI] [Google Scholar]
- Bersell, C. H. (2017). Access to oral health care: A national crisis and call for reform. Journal of Dental Hygiene, 91(1), 6–14. [PubMed] [Google Scholar]
- Bhatt, A. S. , Moscone, A. , McElrath, E. E. , AnubodhVarshney, S. , Claggett, B. L. , Bhatt, D. L. , JamesJanuzzi, L. , Butler, J. , Adler, D. S. , ScottSolomon, D. , & Vaduganathan, M. (2020). Fewer hospitalizations for acute cardiovascular conditions during the COVID‐19 pandemic. Journal of the American College of Cardiology, 76(3), 280–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackburn, J. , Morrisey, M. A. , & Sen, B. (2017). Outcomes associated with early preventive dental care among medicaid‐enrolled children in Alabama. JAMA Pediatrics, 171(4), 335–341. 10.1001/jamapediatrics.2016.4514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, T. T. , Dela Cruz, E. , & Brown, S. S. (2011). The effect of dental care on cardiovascular disease outcomes: An application of instrumental variables in the presence of heterogeneity and self‐selection. Health Economics, 20(10), 1241–1256. 10.1002/hec.1667 [DOI] [PubMed] [Google Scholar]
- Buchmueller, T. , Miller, S. , & Vujicic, M. (2016). How do providers respond to changes in public health insurance coverage? Evidence from adult Medicaid dental benefits. American Economic Journal: Economic Policy, 8(4), 70–102. [Google Scholar]
- Buchmueller, T. C. , Orzol, S. , & Shore‐Sheppard, L. D. (2015). The effect of Medicaid payment rates on access to dental care among children. American Journal of Health Economics, 1(2), 194–223. [Google Scholar]
- Bullinger, L. R. , Carr, J. B. , & Packham, A. (2020). COVID‐19 and crime: Effects of stay‐at‐home orders on domestic violence. National Bureau of Economic Research Working Paper Series No. 27667. http://www.nber.org/papers/w27667. 10.3386/w27667 [DOI]
- Callaway, B. , & Sant’Anna, P. H. C. (2021). Difference‐in‐Differences with multiple time periods. Journal of Econometrics, 225(2), 200‐230. 10.1016/j.jeconom.2020.12.001 [DOI] [Google Scholar]
- Cantor, J. H. , Sood, N. , Bravata, D. , Pera, M. , & Whaley, C. M. (2020). The impact of the COVID‐19 pandemic and policy response on health care utilization: Evidence from county‐level medical claims and cellphone data. National Bureau of Economic Research Working Paper Series No. 28131. 10.3386/w28131 Retrieved from http://www.nber.org/papers/w28131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castaneda, M. A. , & Saygili, M. (2020). The effect of shelter‐in‐place orders on social distancing and the spread of the COVID‐19 pandemic: A study of Texas. Frontiers in Public Health, 8, 596607. 10.3389/fpubh.2020.596607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalfin, A. , Danagoulian, S. , & Deza, M. (2019). More sneezing, less crime? Health shocks and the market for offenses. Journal of Health Economics, 68, 102230. 10.1016/j.jhealeco.2019.102230 [DOI] [PubMed] [Google Scholar]
- Chalfin, A. , Danagoulian, S. , & Deza, M. (2021). COVID‐19 has strengthened the relationship between alcohol consumption and domestic violence. National Bureau of Economic Research Working Paper Series No. 28523. 10.3386/w28523 Retrieved from http://www.nber.org/papers/w28523 [DOI] [Google Scholar]
- Choi, M. K. (2011). The impact of Medicaid insurance coverage on dental service use. Journal of Health Economics, 30(5), 1020–1031. [DOI] [PubMed] [Google Scholar]
- Danagoulian, S. , & Jenkins, D. (2021). Rolling back the gains: Maternal stress undermines pregnancy health after Flint's water switch. Health Economics, 30(3), 564–584. [DOI] [PubMed] [Google Scholar]
- Dave, D. , Friedson, A. I. , Matsuzawa, K. , & Sabia, J. J. (2020). When Do Shelter‐in‐Place Orders Fight COVID‐19 Best? Policy Heterogeneity Across States and Adoption Time. Econ inq. 10.1111/ecin.12944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker, S. L. , & Lipton, B. J. (2015). Do Medicaid benefit expansions have teeth? The effect of Medicaid adult dental coverage on the use of dental services and oral health. Journal of Health Economics, 44, 212–225. 10.1016/j.jhealeco.2015.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deryugina, T. , & Molitor, D. (2020). Does when you die depend on where you live? Evidence from Hurricane Katrina. The American Economic Review, 110(11), 3602–3633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elharake, J. A. , Shafiq, M. , McFadden, S. M. , Malik, A. A. , & Omer, S. B. (2021). The association of COVID‐19 risk perception, county death rates, and voluntary health behaviors among U.S. Adult population. The Journal of Infectious Diseases, (4), 593–597. 10.1093/infdis/jiab131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao, S. , Rao, J. , Kang, Y. , Liang, Y. , Kruse, J. , Dopfer, D. , Sethi, A. K. , Mandujano Reyes, J. F. , Yandell, B. S. , & Patz, J. A. (2020). Association of mobile phone location data indications of travel and stay‐at‐home mandates with COVID‐19 infection rates in the US. JAMA Network Open, 3(9), e2020485. 10.1001/jamanetworkopen.2020.20485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia, S. , Albaghdadi, M. S. , Meraj, P. M. , Schmidt, C. , Garberich, R. , Jaffer, F. A. , Dixon, S. , Rade, J. J. , Tannenbaum, M. , Chambers, J. , Huang, P. P. , & Henry, T. D. (2020). Reduction in ST‐segment elevation cardiac catheterization laboratory activations in the United States during COVID‐19 pandemic. Journal of the American College of Cardiology, 75(22), 2871–2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glied, S. , & Neidell, M. (2010). The economic value of teeth. Journal of Human Resources, 45(2), 468–496. 10.3368/jhr.45.2.468 [DOI] [Google Scholar]
- Hartnett, K. P. , Kite‐Powell A., DeVies J., and , Coletta M. A., Boehmer T. K., Adjemian J., Gundlapalli A. V. 2020. "Impact of the COVID‐19 pandemic on emergency department visits — United States, January1, 2019–may 30, 2020." MMWR Morb Mortal Wkly Rep 69:699‐704. 10.15585/mmwr.mm6923e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsia, R. Y. , Nath, J. B. , & Baker, L. C. (2014). Emergency department visits by children, adolescents, and young adults in California by insurance status, 2005‐2010. JAMA, 312(15), 1587–1588. 10.1001/jama.2014.9905. PMID: 25321913; PMCID: PMC4636208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang, Y. , Gao, S. , Liang, Y. , Li, M. , Rao, J. , & Kruse, J. (2020). Multiscale dynamic human mobility flow dataset in the U.S. during the COVID‐19 epidemic. Scientific Data, 7(1), 390. 10.1038/s41597-020-00734-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killeen, B. D. , Wu, J. Y. , Shah, K. , Anna, Z. , Nikutta, P. , Tamhane, A. , Chakraborty, S. , Wei, J. , Gao, T. , & Thies, M. (2020). A county‐level dataset for informing the United States' response to COVID‐19. arXiv preprint arXiv:2004.00756.
- Lee, H. H. , Faundez, L. , Nasseh, K. , & LoSasso, A. T. (2020). Does preventive care reduce severe pediatric dental caries? Preventing Chronic Disease, 17, E136. 10.5888/pcd17.200003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manger, D. , Walshaw, M. , Fitzgerald, R. , Doughty, J. , Wanyonyi, K. L. , White, S. , & Gallagher, J. E. (2017). Evidence summary: The relationship between oral health and pulmonary disease. British Dental Journal, 222(7), 527–533. 10.1038/sj.bdj.2017.315 [DOI] [PubMed] [Google Scholar]
- Mast, C. , & A Munoz, del R. (2020). Delayed cancer screenings—A second look. Epic Health Research Network. [Google Scholar]
- Mustapha, I. Z. , Debrey, S. , Oladubu, M. , & Ugarte, R. (2007). Markers of systemic bacterial exposure in periodontal disease and cardiovascular disease risk: A systematic review and meta‐analysis. Journal of Periodontology, 78(12), 2289–2302. 10.1902/jop.2007.070140 [DOI] [PubMed] [Google Scholar]
- Nasseh, K. , Vujicic, M. , & Glick, M. (2017). The relationship between periodontal interventions and Healthcare costs and utilization. Evidence from an integrated dental, medical, and pharmacy commercial claims Database. Health Economics, 26(4), 519–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raifman, J. , Nocka, K. , Jones, D. , Bor, J. , Lipson, S. , Jay, J. , & Chan, P. (2020). COVID‐19 US state policy database. Retrieved from http://www.tinyurl.com/statepolicies
- Rambachan, A. , & Roth, J. (2022). A more credible approach to parallel trends. Unpublished Manuscript.
- Rebelo, M. A. B. , Rebelo Vieira, J. M. , Pereira, J. V. , Quadros, L. N. , & Vettore, M. V. (2019). Does oral health influence school performance and school attendance? A systematic review and meta‐analysis. International Journal of Paediatric Dentistry, 29(2), 138–148. [DOI] [PubMed] [Google Scholar]
- Sen, S. , Giamberardino, L. D. , Moss, K. , Morelli, T. , Rosamond, W. D. , Gottesman, R. F. , Beck, J. , & Offenbacher, S. (2018). Periodontal disease, regular dental care use, and incident ischemic stroke. Stroke, 49(2), 355–362. 10.1161/strokeaha.117.018990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinkl, J. , & Sizemore, O. (2020). Return to near average number of ED visits for acute MI and strokes 12 weeks post COVID‐19 emergency declaration. Epic Health Research Network, 7. [Google Scholar]
- Verma, S. (2020). Early impact of CMS expansion of Medicare telehealth during COVID‐19. Health Affairs Blog, 15, 15. [Google Scholar]
- Yan, Y. , Bayham, J. , Richter, A. , & Fenichel, E. P. (2021). Risk compensation and face mask mandates during the COVID‐19 pandemic. Scientific Reports, 11(1), 3174. 10.1038/s41598-021-82574-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, J. (2021). Hospital avoidance and unintended deaths during the COVID‐19 pandemic. American Journal of Health Economics, 7(4), 405–426. 10.1086/715158 [DOI] [Google Scholar]
- Ziedan, E. , Simon, K. , & Wing, C. (2020). Effects of state COVID‐19 closure policy on NON‐COVID‐19 health care utilization. NBER Working Papers, 27621. 10.3386/w27621 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information S1
Data Availability Statement
The SafeGraph data used in most of the analysis is available by request from https://www.safegraph.com/. The Medicaid claims data is subject to data use agreement with the Michigan Department of Health and Human Services (MDHHS) and cannot be shared. These data are available upon application to MDHHS.


