Abstract
Aims
The aim of this study was to report patient and clinical outcomes following robotic-assisted total knee arthroplasty (RA-TKA) at multiple institutions with a minimum two-year follow-up.
Methods
This was a multicentre registry study from October 2016 to June 2021 that included 861 primary RA-TKA patients who completed at least one pre- and postoperative patient-reported outcome measure (PROM) questionnaire, including Forgotten Joint Score (FJS), Knee Injury and Osteoarthritis Outcomes Score for Joint Replacement (KOOS JR), and pain out of 100 points. The mean age was 67 years (35 to 86), 452 were male (53%), mean BMI was 31.5 kg/m2 (19 to 58), and 553 (64%) cemented and 308 (36%) cementless implants.
Results
There were significant improvements in PROMs over time between preoperative, one- to two-year, and > two-year follow-up, with a mean FJS of 17.5 (SD 18.2), 70.2 (SD 27.8), and 76.7 (SD 25.8; p < 0.001); mean KOOS JR of 51.6 (SD 11.5), 85.1 (SD 13.8), and 87.9 (SD 13.0; p < 0.001); and mean pain scores of 65.7 (SD 20.4), 13.0 (SD 19.1), and 11.3 (SD 19.9; p < 0.001), respectively. There were eight superficial infections (0.9%) and four revisions (0.5%).
Conclusion
RA-TKA demonstrated consistent clinical results across multiple institutions with excellent PROMs that continued to improve over time. With the ability to achieve target alignment in the coronal, axial, and sagittal planes and provide intraoperative real-time data to obtain balanced gaps, RA-TKA demonstrated excellent clinical outcomes and PROMs in this patient population.
Cite this article: Bone Jt Open 2022;3(7):589–595.
Keywords: Robotics, Total knee arthroplasty, Total knee replacement, Patient reported outcomes, Patient-reported outcome measures, patient-reported outcome measures (PROMs), primary total knee arthroplasty, total knee arthroplasties (TKAs), Forgotten Joint Score (FJS), KOOS JR, pain scores, Knee Injury and Osteoarthritis Outcomes Score, Robotic-assisted total knee arthroplasty, Joint Replacement, clinical outcomes
Introduction
Over the past decade, there has been a significant increase in total knee arthroplasties (TKAs) being performed, and is projected to increase further to 3.5 million procedures in the USA by 2030. 1 However, it has been reported that approximately 19% to 25% of patients are dissatisfied with using manual jig-based instruments for their primary TKA. 2,3 Possible reasons for dissatisfaction include component malalignment and instability, as even 3° malalignment has been reported to result in pain and instability. 4
Robotic-assisted total knee arthroplasty (RA-TKA) was introduced to reduce the variability and inaccuracy in flexion and extension gap balancing achieved with conventional jig-based manual instruments. 5 RA-TKA provides real-time 3D intraoperative information on implant position and limb alignment in the coronal, sagittal, and axial planes in degrees and gap information within millimetres, which allows surgeons to confirm the target alignment and desired gap measurements that may improve clinical outcomes and patient satisfaction through accurate bone cuts and improved soft-tissue balance. 6,7
Early outcomes after RA-TKA have shown decreased pain, improved patient satisfaction, and improved early functional recovery compared to manual or conventional TKA. 6,8-11 However, mid- and long-term clinical and patient-reported outcome measures (PROMs) data remain sparse with relatively small sample sizes, particularly across institutions. 12 The purpose of this multicentre study was to report the clinical and PROMs results preoperatively, at one to two years, and greater than two years following primary RA-TKA in a large patient cohort and determine if the results were consistent across various sites.
Methods
A multicentre, prospective total joint registry study of RA-TKAs performed at five institutions across North America and Australia was conducted. The study was approved through each respective institutions’ institutional review boards (IRBs). Adult patients who underwent a primary RA-TKA and were followed up with between October 2016 and June 2021 at a participating institution, and completed at least one preoperative and postoperative PROM questionnaire with a minimum of two-year follow-up, were included. Exclusion criteria included age greater than 89 years, revision RA-TKA, patients with a status of current incarceration, and patients who were pregnant. Patients without a preoperative PROM result, or with less than one year of follow-up, were also excluded.
Across the five institutions, there were six surgeons included in the registry (ALM, AFC, GC, DC, RCM, MAM), with varied RA-TKA case distributions from 30% to 100% of robotic use for TKAs, with three of the six surgeons performing 100% RA-TKAs. All surgeons used the Stryker Mako SmartRobotics system (Stryker, USA) via medial parapatellar approach. Alignment techniques varied, including restricted kinematic, anatomical, and functional. Surgical variables extracted included approach type and use of cement during the procedure. All patients received the standard postoperative care at their respective institutions, with early mobilization, range of motion, and strengthening exercises during the perioperative period and evaluation for venous thromboembolism, wound complications, and other adverse events during routine follow-up at two to six weeks, three to six months, one year, and two years.
Patient characteristics and clinical and surgical information were collected and abstracted from the total joint registry. Demographic and clinical variables included patient age, sex, BMI, and laterality of the affected side. Postoperative complications were also collected, including rate of surgical site infections and revision surgeries. Minor postoperative complications were defined as any instance of erythema of the surgical site or calf, dermatitis, wound drainage, deep vein thrombosis, lower limb oedema, haematoma, and pain in or around the surgical site.
PROMs administered included the Forgotten Joint Score (FJS), 13 Knee Injury and Osteoarthritis Outcomes Score for Joint Replacement (KOOS JR), 14 and overall pain scale out of 100 points, with 100 indicating the most severe pain. The minimal clinically important difference (MCID) was determined for each PROM based on previously reported MCID values in the literature. 15-17 Patients were given these PROMs to complete prior to the operation, at one-year follow-up appointments, and after two years.
The FJS is a validated PROM assessment tool designed to detect subtle differences in patient satisfaction, focused on the patients’ ability to forget the artificial joint in everyday life. It uses a 12-item questionnaire of awareness of the artificial joint while performing various activities, scored on a five-point Likert scale. 13 The MCID for the FJS was determined to be 14 points, based on previously reported values using logistic regression modelling. 17
The KOOS JR is a validated seven-item questionnaire focusing on morning stiffness, pain with various activities, and function within the past week. It uses a four-point scale from “none” to “extreme” to determine a general picture of knee health and disability. 14 The MCID for the KOOS JR was determined to be 15 points, based on previously reported values using the anchor-based method. 16
Patients were also asked to rate their subjective pain on a scale of 0 to 100 at the preoperative, one- to two-year, and two-year follow-up visits. The MCID for the subjective pain scale was determined to be 23 points, based on previously reported values using a linear mixed model. 15
Statistical analysis
Descriptive statistics of frequencies, percentages, means, and standard deviations (SDs) were reported for all patient and surgical characteristics when appropriate. All PROMs were reported as means and SDs at preoperative, one- to two-year, and greater than two-year follow-up. Differences in outcomes across the follow-up timeframe were compared using repeated measures analysis of variance (ANOVA). The level of significance was set at a p-value of < 0.05. All statistical analyses were performed using SPSS v. 27.0 (SPSS, USA).
Results
A total of 861 patients underwent primary RA-TKA and met the inclusion criteria. Follow-up ranged from 24 months to 60 months. Patient characteristics are summarized in Table I. There were 535 patients with completed FJS results at preoperative, one to two years, and two or more years of follow-up. A significant improvement in FJS was noted by two or more years of follow-up, with mean FJS noted at 17.5 (SD 18.2) preoperatively, 70.2 (SD 27.8) at one to two years postoperatively, and 76.7 (SD 25.8) at two or more years postoperatively (p < 0.001) (Figure 1). There were 487 patients (91%) that improved in FJS over two or more years and met the MCID (Figure 2). There were no significant differences between institutions in FJS change.
Table I.
Patient characteristics.
| Variable | Value |
|---|---|
| Total, n | 861 |
| Mean age, yrs (range; SD) | 67 (35 to 86; 7.9) |
| Sex, n (%) | |
| Female | 405 (47) |
| Male | 452 (53) |
| Mean BMI, kg/m2 (range; SD) | 31.5 (19 to 58; 6.1) |
| Mean ASA (range; SD) | 2.4 (1 to 4; 0.5) |
| Mean LOS, days (range; SD) | 2.8 (1 to 11; 1.0) |
| Laterality, n (%) | |
| Right | 443 (52) |
| Left | 418 (48) |
| Cement, n (%) | |
| Cemented | 553 (64) |
| Cementless | 308 (36) |
ASA, American Society of Anesthesiologists; LOS, length of stay; SD, standard deviation.
Fig. 1.
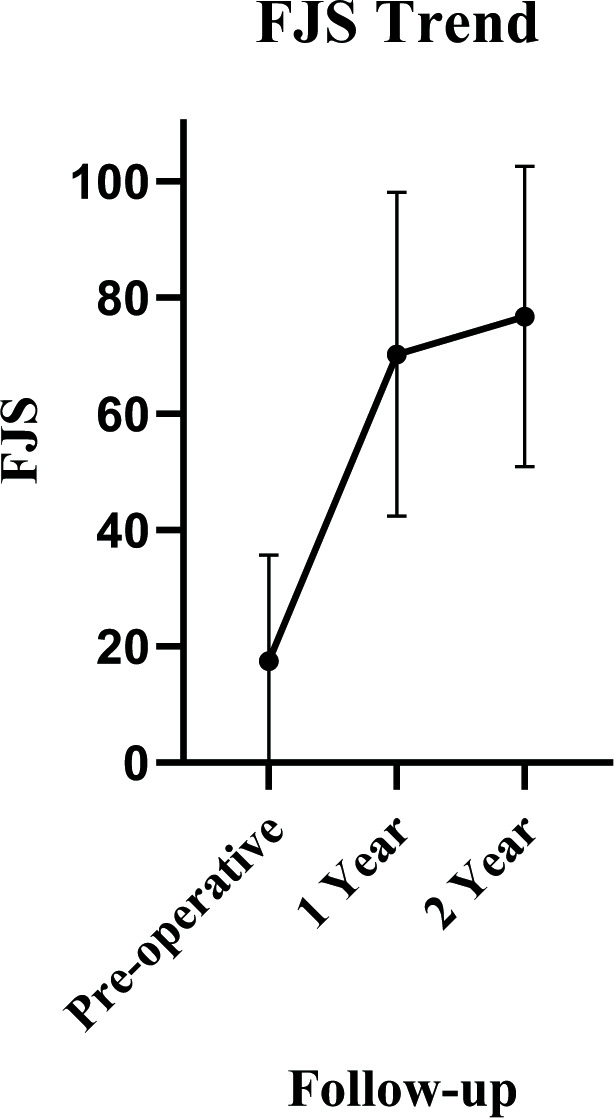
Forgotten Joint Score (FJS) over time at each follow-up timepoint. Significant improvement was noted after robotic-assisted total knee arthroplasty (p < 0.001).
Fig. 2.
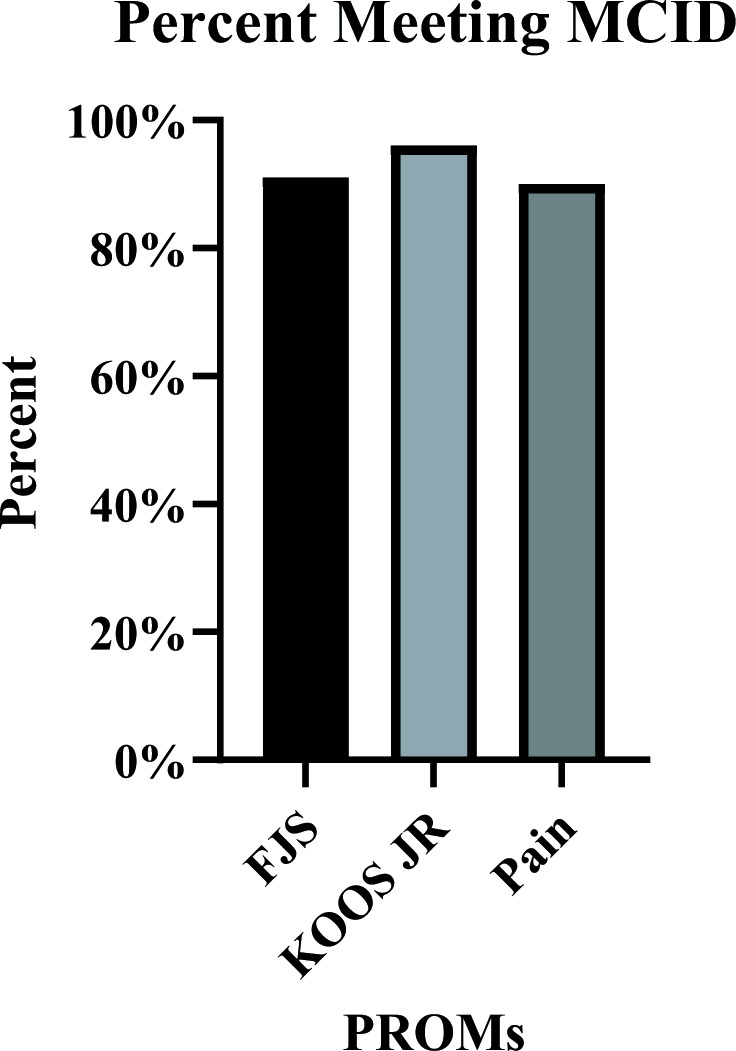
Percent of patients meeting minimal clinically important difference (MCID) by final follow-up for each patient-reported outcome. FJS, Forgotten Joint Score; KOOS JR, Knee injury and Osteoarthritis Outcome Score for Joint Replacement; PROMs, patient-reported outcome measures.
There were 448 patients with completed KOOS JR results at preoperative, one to two years, and two or more years of follow-up. A significant improvement in KOOS JR was noted by two or more years of follow-up, with mean KOOS JR noted at 51.6 (SD 11.5) preoperatively, 85.1 (SD 13.8) at one to two years postoperatively, and 87.9 (SD 13.0) at two or more years postoperatively (p < 0.001) (Figure 3). There were 431 patients (96%) who improved in KOOS JR over two or more years and met the MCID. There were no significant differences between institutions in KOOS JR change.
Fig. 3.
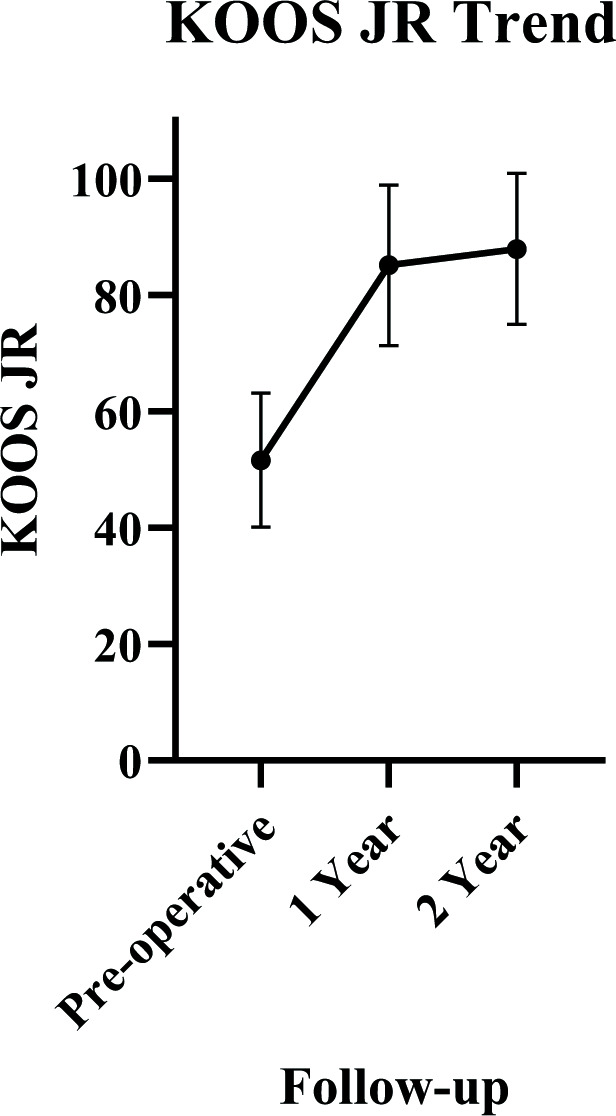
Knee injury and Osteoarthritis Outcome Score for Joint Replacement (KOOS JR) over time at each follow-up timepoint. Significant improvement was noted after robotic-assisted total knee arthroplasty (p < 0.001).
There were 485 patients who had reported their pain levels on a 100-point scale at all visits. A significant improvement in subject pain scale was also noted by two or more years of follow-up, with mean pain score of 65.7 (SD 20.4) preoperatively, 13.0 (SD 19.1) at one to two years postoperatively, and 11.3 (SD 19.9) at two are more years postoperatively (p < 0.001) (Figure 4). There were 438 (90%) patients who improved in subjective pain scale over two or more years and met the MCID. There were no significant differences between institutions in pain scale change.
Fig. 4.
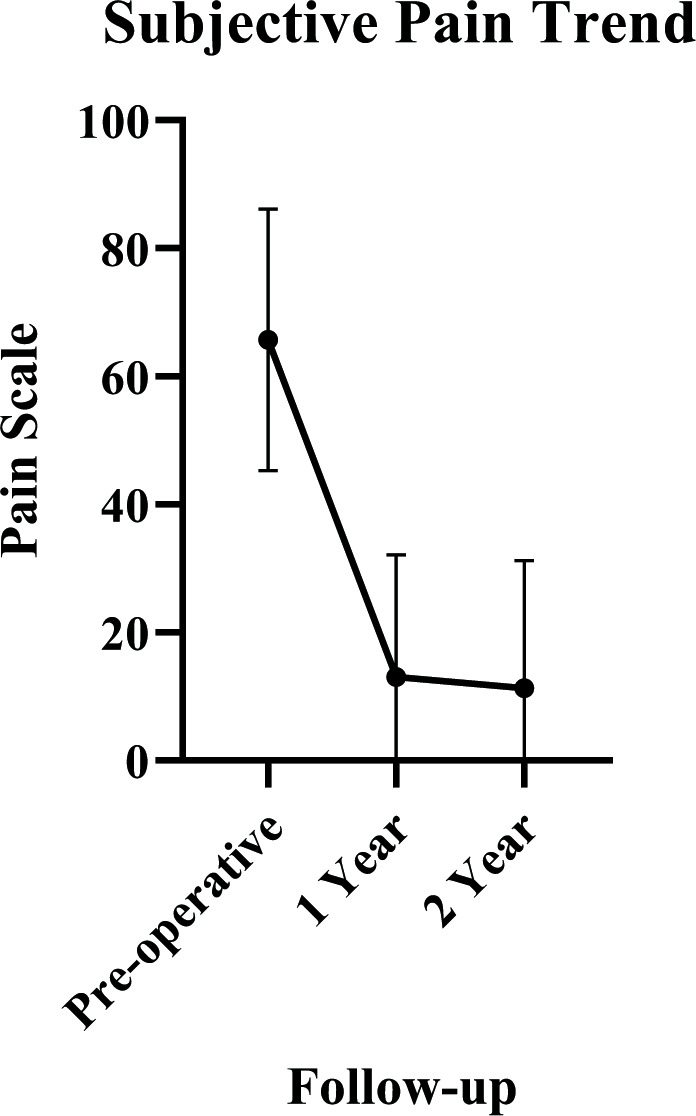
Subjective pain scale over time at each follow-up timepoint. Significant improvement was noted after robotic-assisted total knee arthroplasty (p < 0.001).
Few major complications were noted in this cohort. Eight patients (0.9%) had postoperative superficial surgical site infections treated with antibiotics. Four patients (0.5%) underwent revision arthroplasty, two patients (0.2%) for instability and two patients (0.2%) for deep periprosthetic joint infection, ranging from four months to 15 months. Four other patients were treated for stiffness via arthroscopic release of adhesions (two patients) and manipulation under anaesthesia (two patients) at two, three, four, and 27 months. Minor postoperative complications were reported for 123 patients (14%) (Table II).
Table II.
Minor complications following robotic-assisted total knee arthroplasty.
| Complication | n (%) |
|---|---|
| Total | 123 (14.3) |
| Leg swelling | 52 (6.0) |
| Erythema/dermatitis | 27 (3.1) |
| Haematoma/seroma | 11 (1.3) |
| Stiffness | 10 (1.2) |
| Superficial infection | 8 (0.9) |
| Trauma | 4 (0.5) |
| Blisters/drainage | 3 (0.3) |
| Medication side effect | 3 (0.3) |
| Gastrointestinal | 2 (0.2) |
| Deep vein thrombosis | 1 (0.1) |
| Cardiac event | 1 (0.1) |
| Uncontrolled pain | 1 (0.1) |
Discussion
RA-TKA and other navigation-based systems have been implemented over the past few decades to narrow the up to 20% margin of patients who are unhappy with their conventional jig-based TKA. 2,3,12 The use of robotic-assisted surgery for primary TKA is gaining in popularity, with most large orthopaedic manufacturers having introduced their robotic systems for TKA.
Proponents of RA-TKA argue that it provides more accurate bony resection, offers valuable intraoperative data, and achieves the target implant position and limb alignment that may improve overall patient satisfaction. 4-6,8-11,18-20 Those questioning the use of RA-TKA argue that there are no long-term data, and that the cost of RA-TKA implementation is a limiting factor for many hospital systems. 5 With any new advances in medical technology, validation in the form of short-, mid-, and long-term studies must be carried out to ensure continued safety and efficacy of a novel product. Prior studies comparing patients who have undergone RA-TKA versus conventional jig-based TKA have demonstrated statistical improvements in RA-TKA PROMs from the preoperative to postoperative state. 8,11 Our study demonstrated significant improvements in PROMs from preoperative to one and two years postoperatively for FJS, KOOS JR, and pain scores. MCID for FJS, KOOS JR, and pain scores were met for 91%, 96%, and 90% of patients, respectively, with low rates of revision.
In a sample of 150 consecutive patients undergoing TKA (75 RA-TKA, 75 manual TKA) with short-term follow-up (≤ one year), Smith et al 8 found that 94% of patients chose either very satisfied or satisfied on a Likert scoring system when asked about their RA-TKA clinical outcome, compared to 82% in the manual TKA cohort (p < 0.01). Additionally, the overall average satisfaction score was higher in the RA-TKA cohort at 7.1 versus 6.4 (p < 0.05). 8 Specific questions on the Knee Society Score (KSS) 21 regarding pain at rest and function with recreational activities were also found to be statistically significant in favour of RA-TKA (p < 0.05 for both). 8 Marchand et al 11 studied 40 total patients (20 RA-TKA, 20 manual TKA) and found that six-month postoperative Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) 22 pain and WOMAC total scores were significantly better in RA-TKA patients compared to manual TKA patients (p < 0.05 for both), while six-month postoperative WOMAC physical function scores did not achieve significance (p = 0.055). 11 At three-month follow-up, Khlopas et al 23 found equal or greater improvements in nine out of ten KSS components for 150 RA-TKA patients compared to 102 manual TKA patients, but not all findings achieved statistical significance.
Not all studies have demonstrated RA-TKA PROM superiority. Samuel et al 24 performed a propensity matched cohort study of 255 manual TKA and 85 RA-TKA patients at one year postoperatively, and found statistically equivalent PROMs and increased operating time in the RA-TKA cohort (113 minutes vs 105 minutes; p < 0.001), but decreased length of stay (p < 0.001) and a higher proportion of home discharges (p < 0.001). Liow et al 25 studied 60 knees (31 RA-TKA and 29 manual TKA) and found equivalent KSS, Oxford Knee Scores (OKS), 26,27 and satisfaction rates at two years postoperatively. 36-Item Short Form Health Survey (SF-36) energy/vitality and emotional role limitation scores both achieved significance favouring RA-TKA (p < 0.05 for both). Singh et al 28 conducted a comparison of 287 TKAs with intraoperative navigation, 367 RA-TKAs, and 6,442 manual TKAs over a four-year period, and found no significant difference in FJS scores between cohorts at three months or one year. KOOS JR scores achieved significance favouring manual TKA at three months (p < 0.001), but there was no significant difference between cohorts at one year postoperatively. 28
Although our multicentre study did not directly compare RA-TKA with manual TKA, it does demonstrate statistically significant improvements in RA-TKA patients from the pre- to postoperative states across a variety of PROMs at a minimum two-year follow-up. Even though not all 861 patients had all three PROMs recorded, this is the first study of which the authors are aware that includes a large series of patients achieving statistical significance across a two-year or greater time span in a heterogeneous population of RA-TKA patients. In addition to statistically significant PROM findings, our cohort of RA-TKA patients also achieved 91% FJS MCID, 96% KOOS JR MCID, and 90% subjective pain score MCID at greater than two years. Our improvement in PROMs is consistent with prior findings and indicates that appropriately powered studies may be needed to further delineate nuances between RA-TKA and manual TKA cohorts. 8,11,23,29 Major complications among our group were comparable to prior published studies with four individuals (0.5%) undergoing revision arthroplasty (two due to periprosthetic joint infection, two due to instability). 8,25,28
This study does have limitations. Although all data were prospectively collected, the study is retrospective in nature and demonstrates variability in surgical technique and postoperative protocols across centres. Our patient population demonstrates heterogeneity in composition and each individual surgeon’s decision on a patient’s candidacy for RA-TKA. Each surgical site also introduces additional variability in terms of the choice of target limb alignment: mechanical, kinematic, or restricted-kinematic. No alignment or component criteria were implemented in the study design, since variability was considered an important factor to demonstrate reproducibility. We did not compare outcomes based on alignment technique, since a larger cohort is required to identify meaningful differences between the various alignment techniques. Both implant designs including cruciate-retaining and posterior-stabilized components were used in this study. The authors believe this breadth in alignment variability and implant design in this large group of patients undergoing RA-TKAs could be considered a strength of the study, as PROMs were consistently improved across a broad group of components and alignments, making the study results more generalizable. While not every patient had all three PROMs, this remains the largest long-term multicentre cohort reported for the PROMs measured. FJS and KOOS JR were used as they are both proven scaling systems consistently chosen across the literature to compare pre- and postoperative states. 13,14 Additionally, MCID was calculated for each of the metrics, as not all statistically significant values demonstrated clinically valuable or useful information. 17
The ability to balance the knee in both flexion and extension, and in the medial and lateral compartments, using objective real time intraoperative data along with the ability to make adjustments in implant size and position, potentially allows for a reproducible stable knee construct, despite various alignment techniques and implant designs used in this study. The consistently improved PROMs seen may be due to the alignment techniques chosen by the authors to minimize deviation from the native joint line using either restricted kinematic, anatomical, or function alignment techniques. The authors did not use neutral mechanical aligment. Further work is needed to determine the role of neutral mechanical alignment versus kinematic or functional alignment in overall clinical results including PROMs.
Component and limb alignment likely also play a factor in outcome measures. 30,31 Areas of future research include mid- and long-term result comparisons between RA-TKA and manual TKA cohorts. More research is needed in the form of prospective randomized controlled trials to determine clinical differences between robotic and conventional TKA along with various alignment concepts. Surgeons are now able to fine-tune the position of their bony cuts, implants, and gap measurements with a high level of accuracy and precision. 19,20 RA-TKA has the potential to provide surgeons and researchers with a vast amount of intraoperative data, which may be used for clinical decision-making and research by coupling it with outcome-related measures.
This study adds to the growing body of evidence that RA-TKA can achieve consistently improved PROMs. This is the first study to demonstrate improved PROMs reaching MCID in a multicentre population of RA-TKA patients with a minimum two-year follow-up, demonstrating excellent PROMs, despite variation in surgical and alignment techniques.
Take home message
- There is limited long-term evidence in the literature on outcomes following robotic-assisted total knee arthroplasty (RA-TKA) in heterogeneous multicentre populations.
- RA-TKA demonstrated consistent clinical and patient-reported outcomes with few complications across multiple institutions at a minimum of two-year follow-up, despite variation in alignment technique.
Acknowledgements
The authors acknowledge Langan Smith.
Footnotes
Author contributions: P. Y. Joo: Methodology, Project administration, Data curation, Formal analysis, Validation, Visualization, Writing – original draft, Writing – review & editing.
A. F. Chen: Conceptualization, Methodology, Supervision, Data curation, Writing – review & editing.
J. Richards: Project administration, Resources, Data curation, Writing – review & editing.
T. Y. Law: Project administration, Resources, Data curation, Writing – review & editing.
K. Taylor: Project administration, Resources, Data curation, Writing – review & editing.
K. Marchand: Project administration, Resources, Data curation, Writing – review & editing.
G. Clark: Project administration, Resources, Data curation, Writing – review & editing.
D. Collopy: Project administration, Resources, Data curation, Writing – review & editing.
R. C. Marchand: Project administration, Resources, Data curation, Writing – review & editing.
M. Roche: Project administration, Resources, Data curation, Writing – review & editing.
M. A. Mont: Project administration, Resources, Data curation, Writing – review & editing.
A. L. Malkani: Conceptualization, Methodology, Supervision, Data curation, Writing – review & editing.
Funding statement: The authors received no financial or material support for the research, authorship, and/or publication of this article.
Ethical review statement: This study was approved by the Institutional Review Board of the host institution with appropriate datasharing agreements (IRB ID: 2021P001556).
Open access funding: The authors confirm that the open access fee was self-funded.
Contributor Information
Peter Y. Joo, Email: peter.y.joo@gmail.com.
Antonia F. Chen, Email: antoniachen1@gmail.com.
Jarod Richards, Email: jarod.richards@louisville.edu.
Tsun Y. Law, Email: tsun.s.law@gmail.com.
Kelly Taylor, Email: ktaylor@orthopedicsri.com.
Kevin Marchand, Email: kmarchand970@gmail.com.
Gavin Clark, Email: gavin@hipnknee.com.au.
Dermot Collopy, Email: dermot@hipnknee.com.au.
Robert C. Marchand, Email: bmarchand@orthopedicsri.com.
Martin Roche, Email: martin@mroche.com.
Michael A. Mont, Email: mmont@lifebridgehealth.org.
Arthur L. Malkani, Email: arthur.malkani@louisville.edu.
References
- 1. Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467(10):2606–2612. 10.1007/s11999-009-0834-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63. 10.1007/s11999-009-1119-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35–43. 10.1097/01.blo.0000238825.63648.1e [DOI] [PubMed] [Google Scholar]
- 4. Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 2007;22(8):1097–1106. 10.1016/j.arth.2007.08.001 [DOI] [PubMed] [Google Scholar]
- 5. Kayani B, Haddad FS. Robotic total knee arthroplasty: clinical outcomes and directions for future research. Bone Joint Res. 2019;8(10):438–442. 10.1302/2046-3758.810.BJR-2019-0175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J. 2018;100-B(7):930–937. 10.1302/0301-620X.100B7.BJJ-2017-1449.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. van der List JP, Chawla H, Joskowicz L, Pearle AD. Current state of computer navigation and robotics in unicompartmental and total knee arthroplasty: a systematic review with meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2016;24(11):3482–3495. 10.1007/s00167-016-4305-9 [DOI] [PubMed] [Google Scholar]
- 8. Smith AF, Eccles CJ, Bhimani SJ, et al. . Improved patient satisfaction following robotic-assisted total knee arthroplasty. J Knee Surg. 2021;34(7):730–738. 10.1055/s-0039-1700837 [DOI] [PubMed] [Google Scholar]
- 9. Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res. 2013;471(1):118–126. 10.1007/s11999-012-2407-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kayani B, Tahmassebi J, Ayuob A, Konan S, Oussedik S, Haddad FS. A prospective randomized controlled trial comparing the systemic inflammatory response in conventional jig-based total knee arthroplasty versus robotic-arm assisted total knee arthroplasty. Bone Joint J. 2021;103-B(1):113–122. 10.1302/0301-620X.103B1.BJJ-2020-0602.R2 [DOI] [PubMed] [Google Scholar]
- 11. Marchand RC, Sodhi N, Khlopas A, et al. . Patient satisfaction outcomes after robotic arm-assisted total knee arthroplasty: a short-term evaluation. J Knee Surg. 2017;30(9):849–853. 10.1055/s-0037-1607450 [DOI] [PubMed] [Google Scholar]
- 12. Kayani B, Konan S, Ayuob A, Onochie E, Al-Jabri T, Haddad FS. Robotic technology in total knee arthroplasty: a systematic review. EFORT Open Rev. 2019;4(10):611–617. 10.1302/2058-5241.4.190022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Behrend H, Giesinger K, Giesinger JM, Kuster MS. The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty. 2012;27(3):430–436. 10.1016/j.arth.2011.06.035 [DOI] [PubMed] [Google Scholar]
- 14. Lyman S, Lee Y-Y, Franklin PD, Li W, Cross MB, Padgett DE. Validation of the KOOS, JR: a short-form knee arthroplasty outcomes survey. Clin Orthop Relat Res. 2016;474(6):1461–1471. 10.1007/s11999-016-4719-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Danoff JR, Goel R, Sutton R, Maltenfort MG, Austin MS. How much pain is significant? Defining the minimal clinically important difference for the visual analog scale for pain after total joint arthroplasty. J Arthroplasty. 2018;33(7S):S71–S75. 10.1016/j.arth.2018.02.029 [DOI] [PubMed] [Google Scholar]
- 16. Hung M, Bounsanga J, Voss MW, Saltzman CL. Establishing minimum clinically important difference values for the Patient-Reported Outcomes Measurement Information System Physical Function, hip disability and osteoarthritis outcome score for joint reconstruction, and knee injury and osteoarthritis outcome score for joint reconstruction in orthopaedics. World J Orthop. 2018;9(3):41–49. 10.5312/wjo.v9.i3.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ingelsrud LH, Roos EM, Terluin B, Gromov K, Husted H, Troelsen A. Minimal important change values for the Oxford Knee Score and the Forgotten Joint Score at 1 year after total knee replacement. Acta Orthop. 2018;89(5):541–547. 10.1080/17453674.2018.1480739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bell SW, Anthony I, Jones B, MacLean A, Rowe P, Blyth M. Improved accuracy of component positioning with robotic-assisted unicompartmental knee arthroplasty: data from a prospective, randomized controlled study. J Bone Joint Surg Am. 2016;98-A(8):627–635. 10.2106/JBJS.15.00664 [DOI] [PubMed] [Google Scholar]
- 19. Kayani B, Konan S, Pietrzak JRT, Haddad FS. Iatrogenic bone and soft tissue trauma in robotic-arm assisted total knee arthroplasty compared with conventional jig-based total knee arthroplasty: a prospective cohort study and validation of a new classification system. J Arthroplasty. 2018;33(8):2496–2501. 10.1016/j.arth.2018.03.042 [DOI] [PubMed] [Google Scholar]
- 20. Sires JD, Craik JD, Wilson CJ. Accuracy of bone resection in MAKO total knee robotic-assisted surgery. J Knee Surg. 2021;34(7):745–748. 10.1055/s-0039-1700570 [DOI] [PubMed] [Google Scholar]
- 21. Culliton SE, Bryant DM, MacDonald SJ, Hibbert KM, Chesworth BM. Validity and internal consistency of the New Knee Society Knee Scoring System. Clin Orthop Relat Res. 2018;476(1):77–84. 10.1007/s11999.0000000000000014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 23. Khlopas A, Sodhi N, Hozack WJ, et al. . Patient-reported functional and satisfaction outcomes after robotic-arm-assisted total knee arthroplasty: early results of a prospective multicenter investigation. J Knee Surg. 2020;33(7):685–690. 10.1055/s-0039-1684014 [DOI] [PubMed] [Google Scholar]
- 24. Samuel LT, Karnuta JM, Banerjee A, et al. . Robotic arm-assisted versus manual total knee arthroplasty: a propensity score-matched analysis. J Knee Surg. 2021. 10.1055/s-0041-1731323 [DOI] [PubMed] [Google Scholar]
- 25. Liow MHL, Goh G-H, Wong MK, Chin PL, Tay D-J, Yeo S-J. Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2942–2951. 10.1007/s00167-016-4076-3 [DOI] [PubMed] [Google Scholar]
- 26. Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80-B(1):63–69. 10.1302/0301-620x.80b1.7859 [DOI] [PubMed] [Google Scholar]
- 27. Murray DW, Fitzpatrick R, Rogers K, et al. . The use of the Oxford hip and knee scores. J Bone Joint Surg Br. 2007;89-B(8):1010–1014. 10.1302/0301-620X.89B8.19424 [DOI] [PubMed] [Google Scholar]
- 28. Singh V, Fiedler B, Simcox T, Aggarwal VK, Schwarzkopf R, Meftah M. Does the use of intraoperative technology yield superior patient outcomes following total knee arthroplasty? J Arthroplasty. 2021;36(7S):S227–S232. 10.1016/j.arth.2020.11.001 [DOI] [PubMed] [Google Scholar]
- 29. Khlopas A, Sodhi N, Sultan AA, Chughtai M, Molloy RM, Mont MA. Robotic arm-assisted total knee arthroplasty. J Arthroplasty. 2018;33(7):2002–2006. 10.1016/j.arth.2018.01.060 [DOI] [PubMed] [Google Scholar]
- 30. Kayani B, Konan S, Tahmassebi J, Oussedik S, Moriarty PD, Haddad FS. A prospective double-blinded randomised control trial comparing robotic arm-assisted functionally aligned total knee arthroplasty versus robotic arm-assisted mechanically aligned total knee arthroplasty. Trials. 2020;21(1):194. 10.1186/s13063-020-4123-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hiyama S, Takahashi T, Takeshita K. Kinematically aligned total knee arthroplasty did not show superior patient-reported outcome measures: an updated meta-analysis of randomized controlled trials with at least 2-year follow-up. J Knee Surg. 2020. 10.1055/s-0040-1716494 [DOI] [PubMed] [Google Scholar]


