Abstract
We have been experiencing multiple waves of the coronavirus disease 2019 (COVID-19) pandemic. With these unprecedented waves, we have entered into an era of ‘new normal’. This pandemic has enforced us to rethink the very basics of childhood learning: Habits, health etiquette, and hygiene. Rehabilitation has immense importance during this pandemic considering a few aspects. Multidisciplinary COVID-19 rehabilitation clinics are essential to address the demand. The equitable distribution of COVID-19 rehabilitation services for differently-abled individuals during the pandemic is an important aspect. Rehabilitation needs identification and further studies on various rehabilitation interventions are among the key unmet future research needs.
Keywords: COVID-19, Long COVID-19, Post-COVID-19 syndrome, Rehabilitation, SARS-CoV-2, Long haulers
Core Tip: The coronavirus disease 2019 (COVID-19) pandemic has impacted negatively on multiple systems of our body, among them the pulmonary system is the most pronounced. The cardiac, nervous, and musculoskeletal systems are also involved. Post-COVID-19 especially post-intensive care unit or post mechanical ventilation and long-COVID-19 can cause significant functional loss and disability. Rehabilitation has an immense role to bring back the achievable functional status of COVID-19 patients. Multidisciplinary COVID-19 rehabilitation clinics are essential to address the demand. The equitable distribution of COVID-19 rehabilitation services for differently-abled individuals during the pandemic is an important aspect. Rehabilitation needs identification and further studies on various rehabilitation interventions are among the key unmet future research needs.
INTRODUCTION
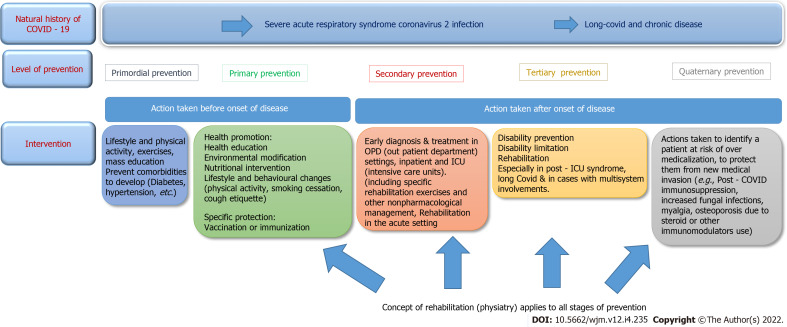
We have been experiencing multiple waves of the coronavirus disease 2019 (COVID-19) pandemic. With these unprecedented waves, we have entered into an era of ‘new normal’. This pandemic has enforced us to rethink the very basics of childhood learning: Habits, health etiquette, and hygiene. It taught us the importance of each stage of prevention: Primordial, primary (mask, sanitization, social distancing, and vaccine), secondary (treatment, critical care, and rehabilitation in acute care), tertiary (disability limitation and rehabilitation), and quaternary (prevent treatment side-effects) (Figure 1). On the other hand, it became a tragedy for people who lost their near and dear ones and those who lost their financial support/job. When we say rehabilitation, it must be emphasized that we should consider the person as a whole rather than the disease. Rehabilitation is defined as “a set of interventions designed to optimize functioning and reduce disability in individuals with health conditions in interaction with their environment”.
Figure 1.
Rehabilitation perspective of the coronavirus disease 2019. COVID-19: Coronavirus disease 2019; ICU: Intensive care unit.
Coronaviruses are single-stranded RNA viruses that cause respiratory, gastrointestinal, and neurological diseases. The first coronavirus - severe acute respiratory syndrome coronavirus (SARS-CoV) - was thought to originate in Foshan, China and resulted in the SARS-CoV pandemic (2002-2003). The second coronavirus caused Middle East respiratory syndrome, which originated from the Arabian Peninsula in 2012. SARS-CoV-2 started in Wuhan, Hubei Province, China in December 2019. On January 12, 2020, the World Health Organization (WHO) named it novel coronavirus (2019-nCoV) and officially named it ‘COVID-19’ on February 11 2020, and finally the International Committee on Taxonomy of Viruses officially designated the virus as SARS-CoV-2. On January 20, 2020 human-to-human transmission was confirmed. On 11 March 2020, WHO declared it as a ‘pandemic’. On March 18, 2020, the WHO and partners launched the Solidarity trial, an international clinical trial aimed ‘to generate robust data from around the world to find the most effective treatments for COVID-19’.
Till now, globally more than 298 million confirmed cases (in India: > 35 million) and 5.4 million (in India: > 0.4 million) deaths have been recorded.
Causative agent
COVID-19 is caused by SARS-CoV-2. SARS-CoV-2 is enveloped and spherical shaped (120 nm), having a positive-sense single-stranded RNA genome[1]. It belongs to the subfamily Orthocoronavirinae (family: Coronavirdiae; order: Nidovirales) and is classified as a beta-coronavirus [lineage B]. The name corona came from a crown-like appearance under an electron microscope (‘coronam’ is the Latin word for ‘crown’) due to the presence of spike glycoproteins on its envelope. The spike glycoprotein of SARS-CoV-2 binds to angiotensin-converting enzyme 2 (ACE2) in humans for cellular entry. Till now, five variants of concern have been identified: Alpha (B.1.1.7); Beta (B.1.351); Gamma (P.1); Delta (B.1.617.2); Omicron (B.1.1.529).
Bat [horseshoe bats (Rhinolophus spp)] is the probable natural host and pangolins are considered an intermediate host[1].
Incubation period
2-14 d (mostly 5 d).
Mode of transmission
Primarily by respiratory droplets but airborne transmission is also implicated especially following aerosol-generating procedures. Fomite transmission also has been well characterized.
Clinical features
Fever (83%-99%), cough (59%-82%), and fatigue (44%-70%) are the frequent symptoms but anorexia (40%-84%), shortness of breath (31%-40%), myalgia (11%-35%), and diarrhoea (2%-38.1%) are also seen. Loss of smell (anosmia) or loss of taste (ageusia) is also reported in many cases. Most of the cases are having mild symptoms, and people with comorbidities and older age groups are particularly prone to develop severe disease.
Clinical severity
The WHO classified COVID-19 as mild, moderate (pneumonia), severe (severe pneumonia), and critical (acute respiratory distress syndrome, sepsis, and septic shock).
Pathophysiology
After entry into the cell, this virus causes diffuse alveolar damage in the lungs. Excessive immune reaction to the virus, causing cytokine storm, is mainly responsible for the clinical severity of COVID-19. The predominant mechanisms of acute COVID-19 include the following: Direct viral toxicity; endothelial and microvascular damage; dysregulated immune system; hypercoagulability; and maladaptation of the ACE2 pathway.
Investigation
Confirmation is done by real-time polymerase chain reaction using the upper and lower respiratory tract samples. Faecal specimens at times can be used as a sample. SARS-CoV-2 antibody testing is not recommended for diagnosis. Lymphopenia is a cardinal feature. Chest X-ray shows bilateral infiltrates, and high resolution computed tomography (HRCT) scan of the thorax shows ground-glass appearance as the most common finding.
COVID-19 confirmed case definition (WHO)
A person with laboratory confirmation of COVID-19 infection is regarded as a COVID-19 confirmed case.
According to ICD 11, the code for the confirmed diagnosis of COVID-19 is RA01.0 and for the clinical diagnosis (suspected or probable) of COVID-19 is RA01.1; the code for post-COVID-19 condition is RA02.
LONG COVID
The Centres for Disease Control and Prevention defined ‘post-COVID conditions’ as “a wide range of new, returning, or ongoing health problems that people can experience four or more weeks after first being infected with the virus that causes COVID-19”[2]. It is called long COVID/long-haul COVID/post-acute COVID-19. Common long COVID-19 symptoms are fatigue, arthralgia, breathlessness, cough, loss of smell, chest pain, palpitation, anxiety/depression and sleep disturbances, difficulty in concentration, etc.
In the National Institute for Health and Clinical Excellence guidelines, two definitions of post-acute COVID-19 are given: (1) Ongoing symptomatic COVID-19 for persons who still have symptoms between 4 and 12 wk after the onset of acute symptoms; and (2) Individuals who still have symptoms for more than 12 wk after the onset of acute symptoms. A full blood count, liver and kidney function tests, a C-reactive protein test, and an exercise tolerance test (level of breathlessness, O2 saturation, and heart rate) are recommended. A chest X-ray also should be advised to all patients by 12 wk after acute infection in cases of persistent respiratory symptoms[3].
Basic mechanisms leading to post-acute COVID-19 include: (1) Virus-related pathophysiologic changes; (2) Immunologic alterations and inflammatory changes in response to the acute infection; and (3) Post-critical illness sequelae. Post-intensive care syndrome is multifactorial and probably due to microvascular ischemia, immobility, and metabolic changes during critical illness. A rehabilitation physician should be well aware of this basic pathophysiology of each aspect of COVID-19 in order to address the rehabilitation need aptly and to implement rehabilitation programs accordingly.
ROLE OF REHABILITATION MEDICINE & INTERNATIONAL CLASSIFICATION OF FUNCTIONING, DISABILITY, AND HEALTH IN COVID-19
Rehabilitation has immense importance during this pandemic considering a few aspects. From the perspectives of type of patient population, there would be different rehabilitation needs for people with COVID-19/post-COVID with no comorbidities/disabilities and those with COVID-19/post-COVID with comorbidities/disabilities. On the other hand, from the perspective of COVID-19 severity, the rehabilitation needs would be different for mild, moderate, and severe/intensive care unit (ICU) admitted patients or in patients with post-intensive care syndrome. Furthermore, at an individual level, a patient may have multiple body-system involvements, in that case, rehabilitation needs would be according to the involvement and impairments. Considering the duration of the disease rehabilitation program would differ, goal setting would change (e.g., acute, subacute, and chronic/post-COVID) accordingly.
At each stage, a basic outline of rehabilitation has to be followed in this sequence: Proper history and physical examination focusing on functional status, a list of problems according to International Classification of Functioning, Disability and Health (ICF) data set (body functions and structure suggesting impairments, activity limitations, participation restriction, and related environmental and personal factors), addressing each problem (management plan: Short- and long-term feasible and realistic goal setting after discussion with the patient, care-giver/partner/family), and trying to achieve each goal, encourage and make support groups to aid in better compliance in the rehabilitation program, to avoid drop-outs, and to strengthen mental health.
Impairments
Multiple system impairments occur like impaired lung function (the viral respiratory syndrome and/or pneumonia, pulmonary fibrosis, pulmonary embolism, damage to respiratory muscles, immobility, and atrophy), physical deconditioning and weakness (due to polyneuromyopathy, inflammatory storm to the muscles, and drugs such as steroids), metabolic changes (e.g., hyperglycemia and malnutrition), immobility and atrophy, impaired communication, impaired swallow (post mechanical ventilation and others), delirium and cognitive impairments, anxiety depression and difficulty in managing activities of daily living (ADLs), pressure injuries, incontinence, polyneuropathy, and other disorders of the peripheral nervous system. Speech-language therapists, physiotherapists, and occupational therapists are needed in such cases.
Rehabilitation starts from acute care setting, then it includes inpatient rehabilitation, outpatient settings, telerehabilitation, and home-based and community-based setting[4].
EVIDENCE-BASED REHABILITATION
We are at the very primary stage to garner evidence for COVID-19. This is the reason why we are continuously modifying and updating guidelines and evidence-based medicine[5]. Studies with stronger evidence on the efficacy of interventions and long-term monitoring are lacking.
Self-management (hospitalized and non-hospitalized)
Objective: The objective is to increase functional independence of patients. Patients with COVID-19 should be educated on self-management regarding breathlessness and gradual activity resumption[6].
Long-COVID: Post-COVID-19 symptoms are seen in > 60% of patients infected by SARS-CoV-2. Fatigue and dyspnoea were the most common post-COVID-19 symptoms, particularly 60 and ≥ 90 d after[7]. Individualized rehabilitation programs from subacute to long-term should be provided according to patient needs. The prescription and provision of rehabilitation programs should be guided by persistent symptoms and functional limitations. Post-COVID-19 impairments like fatigue, weakness, and cognitive impairment, can impact the performance of ADLs. Providing ADL training, considering home modifications (such as grab bars in the shower and toilet, and handrails along stairs), and the provision of an assistive product (such as a mobility aid, shower chair, and over-toilet frame), as needed, are important.
Persons with COVID-19 needs supervised patient-tailored programmes that are flexible enough to adapt for patients. It should be guided by baseline oxygen needs at rest and during exercise.
Persons with physical deconditioning and weakness should start with exercises that help in recovery of daily functioning, start with active range of motion exercises, and when tolerated, proceed with progressive muscle strengthening, typically offered with resistance training.
For individuals having difficulties in memory, concentration, and problem solving, education should be provided, and advice on strategies to reduce stress and anxiety should be given. Cognitive restorative rehabilitation along with cognitive exercises like memory exercises, puzzles, games, and reading and compensation tools like prompts (e.g., lists and notes) and breaking down activities are advised.
For patients with anxiety, depression, and post-traumatic stress disorder, basic mental health and psychosocial support by appropriately trained health or non-health workers should be provided.
For pain, a multidisciplinary approach for pain management is followed according to the biopsychosocial model.
For a successful rehabilitation, a multidisciplinary team approach is essential where a rehabilitation physician (physiatrist) works in collaboration with a group of physicians from multiple specialties (critical care experts, pulmonologists, neurologists, cardiologists, rheumatologists, etc.), nursing professionals, pharmacists, occupational therapists, physiotherapists, social workers, mental health experts, community workers, and other health care professionals
SYSTEMIC INVOLVEMENT OF COVID-19 AND THEIR SPECIFIC REHABILITATION APPROACHES
Pulmonary rehabilitation
Pulmonary rehabilitation improves functional capacity and quality of life in persons recovering from SARS-CoV-2 infection[8].
Diffuse alveolar damage, pulmonary vascular microthrombosis, and macrothrombosis, and immunological damage are responsible for pulmonary sequelae and lung fibrosis.
Pulmonary involvement is complicated with pneumonia, pulmonary embolisms, pulmonary fibrosis, and prolonged ventilation induced respiratory muscle weakness.
Based on a level 3 study, it is suggested that a large proportion of patients still present with dyspnoea at 3 wk of hospital discharge and that PaO2/FiO2 ratio and BMI at admission to the Emergency Department are the strongest independent predictors of persistent respiratory impairment and the need for follow-up in these patients[9].
Patients can try relieving breathlessness using a number of positions including standing with back support, forward lean sitting, and forward lean standing.
Because of risk of infection, lung function test using spirometers is not recommended in patients in the first 6-8 wk with COVID-19; later it can be done to test lung function when patients get non-infectious.
Increasing ventilation
Active cycle of breathing techniques (ACBTs) can be used. Sitting up in bed or chair or standing with support positions to improve ventilation can be adopted as it allows increased thoracic expansion.
Airway clearance
Airway clearance is advised when airway obstruction by sputum is suspected, as these are droplet generating techniques.
In most patients, ACBTs may be used for airway clearance. It includes deep breathing with thoracic expansion and then exhaling with a huff. Huffing is forced expiration with an open mouth (vibration frequency < 17 Hz). Huffing helps to move sputum from small airways to larger airways. A sequence of deep breaths (× 3) then 1-2 huffs and a cough can be used to clear sputum.
Bubble PEP (positive expiratory pressure) can also be used and combined with a huffing and cough sequence to help clear sputum.
Breathlessness education
It is important to learn self-management. The following self-management practices may be adopted.
Staying calm: Breathlessness leads to anxiety which may make it worse.
Using positions: There are several positions (high side-lying and forward lean sitting) that can be adopted that offer support to the body to make breathing easier.
Using breathing techniques: Different breathing techniques may be adopted in different situations. Deep breathing and paced breathing techniques are helpful. Pursed lip breathing helps to empty the lungs and can be helpful to remain calm and when doing a moderate level of activity.
Pursed lip breathing: The patient relaxes his/her shoulder and neck muscles, inhales through the nose for two counts (inhale, one, two, do not take deep breath, only normal breath), ‘purses’ or puckers his/her lips as if he/she is going to whistle, then lastly exhales slowly through pursed lip counting to four (exhale, one, two, three, four).
Square box breathing: The patient closes his/her eyes and inhales via the nose (count up to 4), holds the air inside (count up to 4), exhales slowly (count up to 4), and finally holds for count 4.
Patients should start at lower intensities, especially during the first 6 wk following acute illness.
Respiratory muscle training can improve effortless breathing. Inspiratory muscle training (IMT) can be facilitated via loading of inspiration, by using a breathing device (threshold IMT or power breathe). Expiratory muscle training is also helpful.
Patients should start with low-intensity exercises (≤ 3 METs or equivalent or Borg dyspnea score ≤ 3; duration: 10-15 min for first 3-4 sessions; frequency: 1-2 times/d, 3-4 times/wk) and increase slowly by 30 s to 1 min each time. Over time progression of exercises can be increased up to a Borg score of 4-5 and duration to 30-45 min for 2-3 sessions. Frequency and intensity should be individualized. Pulse oximeter is used to monitor oxygen saturation. Stop physical activities or exercises when a patient's saturation drops more than 5%-10% during exercise. Warm-up and cool-down exercises are recommended. Exercises in the home environment along with maintaining an exercise logbook are recommended[10].
At 12 wk post-discharge, all COVID-19 patients are recommended to be assessed clinically along with an evaluation with chest X-ray, for rehabilitation needs, pulmonary function tests, 6-min walking tests, sputum sampling, and echocardiogram according to clinical judgment. In cases of persistent dyspnea, high-resolution computed tomography of the chest at 6 and 12 mo is also recommended.
Cardiac rehabilitation
According to initial assessment, cardiology consultation should be taken, and further investigations are advised like blood panel, ECG, 24 h ECG, echocardiogram, cardiopulmonary exercise testing, and/or cardiac magnetic resonance imaging.
A 3-6 mo period of complete rest, based on clinical severity and duration of illness, left ventricular function at onset, and extent of inflammation on CMR, is required for patients returning to high-level sport or physically demanding occupation following myocarditis. Training and sport may resume following myocarditis, if left ventricular systolic function and serum biomarkers of myocardial injury are normal and if relevant arrhythmias are ruled out on 24 h ECG monitoring and exercise testing. Periodic assessment is needed in the first 2 years[11].
Abstinence from competitive sports or aerobic activity for 3-6 mo is recommended for competitive athletes with post-COVID cardiovascular complications and it should be until resolution of myocardial inflammation revealed by cardiac magnetic resonance imaging or troponin normalization. Serial clinical and imaging evaluation at 4-12 wk with electrocardiogram and echocardiogram may be done in those with cardiovascular complications.
Rheumatological rehabilitation (arthralgia, arthritis, and myalgia)
Early COVID-19 studies have indicated that over a quarter of mechanically ventilated patients continue to experience ICU acquired weakness at discharge from hospital[12], while half of all hospitalized patients continued to experience fatigue at 60 d post onset[13]. Physical difficulties were reported, including strength, balance, pain, exercise tolerance, and fatigue. Medical Research Council score, handgrip test, Berg balance score, and time up and go test are important assessment measures. SPO2 during exercises and exercise tolerance test (step test or sit to stand test) should be done. Early mobilization (should begin in ICU and critical care setting if tolerable and feasible; bed mobility, bed exercises, etc.), education on fatigue and breathlessness, and functional mobility are to be focused. Energy conservation techniques should be considered, such as simplifying tasks, spacing activities throughout the day, and resting before and after activities. The patient should resume his/her everyday activities and exercise slowly, gradually increasing time and exertion levels, and avoid strengthening exercises until myalgia resolves. For immobile patients with profound weakness, the daily use of neuromuscular electrical stimulation is considered to address inactivity-induced atrophies in lower-limb muscles. Biceps curl, knee strengthening, squats, heel raisers, wall push up, sit-to-stand, etc. are strengthening exercises. The patient should start the exercise in low-moderate intensity and then gradually increase accordingly. In the initial 6 wk after discharge or illness, it is recommended to keep shortness of breath or fatigue below 4/10 on the Borg scale. Clinical signs of desaturation should be monitored using a pulse oximeter when possible. Exercise must be individually prescribed with specifying training parameters regarding frequency, intensity, duration, and type and exercises must be done in a safe environment. Walking, jogging, cycling, step-ups, and marching on the spot may be undertaken if no contraindications exist.
Post-mechanical ventilation patients or those in tracheostomy may develop speech or voice issues. Assessment of any changes in voice quality and articulation problems is needed. Even in intubated patients if conscious, means of communication like notepad, communication board, etc. should be provided. The use of communication boards, communication devices, computers, and smartphone apps is encouraged to augment communication. Using voice is practiced gently through singing, reading aloud, and conversation. The patient should stay hydrated and sip water throughout the day. Optimal oral hygiene is practiced to minimize the risk of infection and maximize healing of the vocal structures. Patients with a tracheostomy may be fitted with a speech valve, which enables speaking without the use of the vocal folds, a trained physician is needed to manage these things and associated caregiver education.
Post-COVID patients may also develop steroid-induced myopathy.
Neurorehabilitation like COVID-induced spinal cord injury, post-COVID stroke, and neuropathy
Hemorrhagic stroke, hypoxic-anoxic damage, posterior reversible encephalopathy syndrome, and acute disseminated myelitis are reported in post-COVID cases.
Stroke patients developing COVID-19 have a worse prognosis, with an over nine-fold increase in mortality and a higher probability of requiring rehabilitation[14].
Regarding the natural history of COVID-19, the case series concerning four severe COVID-19 patients with HO in the hips and shoulders after 30-40 d of hospital admission suggests that the global inflammation associated to COVID-19 might play a role in the pathophysiology of HO, and enhances the need for early monitoring of joint mobility and careful mobilization of patients in the acute phase.
Cognitive domains that may be affected after severe or critical illness with COVID-19 include (but are not limited to) basic functions such as attention, concentration, and memory, higher-order functions such as problem solving, decision making, and judgement, and language such as verbal and semantic memory. Nervous system involvement is due to hypoxic encephalopathy, neuroinflammation, direct viral invasion, and sepsis associated encephalopathy.
Cognitive activities: Puzzles, word and number games, memory exercises, and reading may help improve cognitive function. COVID-19 patients with cognitive function impairment should start with activities that are challenging but achievable and increase the difficulty as able. This is important for keeping the patient motivated. These patients should participate in daily activities. Compensation strategies (prompts: Lists, notes, and alerts, such as phone alarms, can be useful for patients with impaired memory, breaking down activities into individual steps can help prevent the patient from feeling overwhelmed, and relaxation exercises, including meditation, can help alleviate the stress that may be caused by and exacerbate cognitive impairment) should be followed.
Olfactory Training and Visual Stimulation Assisted by a web application for patients with persistent olfactory dysfunction after COVID-19 showed significant improvement after 28 d[15].
Olfactory training like repeated and deliberate sniffing for 20 s each of a set of odorants (commonly lemon, rose, cloves, and eucalyptus) should be conducted at least two times a day for at least 3 mo. Studies have shown improvement in olfaction in postinfectious cases after olfactory training[16]. Intranasal vitamin A and systemic omega-3 may serve as adjuvant therapies[17].
Gastrointestinal system involvement
Diarrhoea, vomiting, and nausea are common in COVID. In cases of persistent gastrointestinal issues, nutritional assessment and micronutrient blood panel may be warranted. Decreased appetite and weight loss sometimes may occur, which also needs attention. A liver function test should be advised as hepatic dysfunction is common in severe COVID-19 cases. COVID-19 has the potential to alter gut microbiome.
Renal system involvement
Acute kidney injury tends to occur in 5% of all cases and 20%-31% of critical cases. Acute tubular necrosis is a common finding along with COVID-19 associated nephropathy. A kidney function test is advised as acute kidney injury has been encountered in many severe COVID-19 cases. Renal involvement is due to sepsis, septic shock, immunoinflammatory reactions, and drug-induced or post-steroid therapy. Patients with renal dysfunction may need a changed or individualized exercise regime and hydration advice.
Haematological system involvement
Lymphopenia, anemia, and leucopenia are common and at times thrombocytopenia can occur. Patients with COVID-19 are susceptible to pulmonary embolism and venous thromboembolism. Before starting any exercises regime, a complete hemogram should be done, and in clinically suspicious cases of thromboembolism, specific investigations are warranted.
Endocrine system involvement
Due to COVID-19 itself or after steroid therapy, hyperglycemia may occur. Post COVID-19 diabetic ketoacidosis and subacute thyroiditis with clinical thyrotoxicosis have been reported. Periodic assessment is needed in such cases.
Other system involvement
Swallowing challenges associated with COVID-19 may result from intubation induced damage in the mucous membrane of the oral cavity, nasal cavities, and/or pharynx, weakening of the swallowing mechanism, diminished swallowing reflexes and muscle tone associated with inflammation, polyneuropathy, and side-effects of medications, cognitive impairment affecting safe swallowing, ventilation induced changes in viscosity of saliva, mouth breathing, medication, or dehydration.
Rehabilitation exercises addressing each of the cardiopulmonary, neurological, vestibular, musculoskeletal, and mental/cognitive systems are recommended in a phased manner (beginning, building, and being phase). In the beginning phase, deep breathing (3 min), eye nodding, bed rolling, head nods, rocking on knees, etc. (3 min) can be tried. Subsequently, the patients can engage in crossbody patterns such as crawling, seating, or standing cross-crawl touches, marching, or walking (1 min). These can be followed by strength building by ‘yawn to smile’, biceps curls, shoulder press, heel raise, wall push-up, and mini-squats (1-3 min). Endurance building by 5-45 min walk can be done in a gradually increasing manner in all phases[18].
DISABILITY INCLUSIVE
Since the beginning of 2022, India has been facing the third wave of this pandemic. Considering the huge population and people with low socioeconomic status, rehabilitation of COVID-19 in the Indian setting can be an ideal example of other developing countries. In the Indian scenario, people with different abilities face different sorts of barriers during the pandemic. Moreover, globally people with disabilities (15% of the global population) have been affected negatively by the COVID-19 pandemic. The risk of death from COVID-19 (January 24-November 30, 2020) in England was (men: 3.1 times greater; female: 3.5 times greater) greater in people with disabilities than in those without disabilities[19]. As usual, ICU patients had more disabilities than ward patients [20]. A person with long COVID-19 will have a disability if his/her condition or any of its symptoms is causing physical or mental impairment that hinders one or more major life activities[21]. People with disabilities are susceptible to COVID-19. In India, Rights of Persons with Disabilities Act, 2016 (Section 8) guarantees the equal protection and safety for people with disabilities in such situations.
SPECIAL CLINICS AND COMMUNITY-BASED REHABILITATION
In the Indian setting, post-COVID rehabilitation clinics (adult and pediatric) are the key need currently like in the United States[22]. Community-based rehabilitation would be effective in the Indian setting to cater rehabilitation services. Falvey et al[23] showed how community-based therapists can help during pandemics. During the pandemic, the community health workers contribute to the COVID-19 response; it includes screening, referrals, arranging support for home care, staffing community-based isolation centres, and being involved in surveillance, contact tracing, service delivery to people with disabilities, home visit, outreach activities, and campaigns[24].
CONCLUSION
“Rehabilitation is an essential health service and crucial for achieving universal health coverage” (Rehabilitation 2030 initiative). Needless to say, globally rehabilitation for people with COVID-19 and post-COVID-19 syndrome is the key unmet need. We would like to conclude this chapter with some recent advances which can further the rehabilitation process, especially artificial intelligence (AI) and telerehabilitation. A patient-centric individualized AI system for home-based rehabilitation is beneficial[25,26]. AI can be useful to make early detection of long-COVID symptoms. Hassanien et al[27] showed machine learning to better understand and predict the reaction of patients to the disease and the possibilities that they may have for recovery. Furthermore, the TERECO trial showed the effectiveness of telerehabilitation in COVID-19 survivors[28]. Werneke et al[29] showed the importance of telerehabilitation during pandemic times in outpatient rehabilitation settings. Telemonitoring is generally recommended 1-4 times in the first-month post-discharge. Follow-up recommendation is based on the Barthel Index score: level 1 (0-39, dependent, weekly telemonitoring), level 2 (40-79, partially dependent, biweekly telemonitoring), and level 3 (80-100, independent, monthly telemonitoring). In this ultra-modern era with cutting-edge technology, at the end of the chapter we would like to emphasize that prevention against the development of disease or disability is far easier and more economical than the disease itself. All you need to do is to practice basic personal hygiene, a healthy active lifestyle, and comprehensive rehabilitation to prevent disease, disability, and death. Finally, rehabilitation need identification is an important step to evaluate long COVID-19 patients so that we can recognize them early to prevent disability[30].
Take-home message
What are the issues that individuals need to be supported in rehabilitation: Rehabilitation needs should be identified according to the ICF.
Currently, studies are going on to find out rehabilitation needs in these patients. However, physicians have to identify needs by focusing each body system and emphasizing on patient’s functional aspects.
Early rehabilitation intervention even when patient is in ICU is of utmost importance apart from post-discharge rehabilitation.
How should these requirements be met: Proper rehabilitation facilities and infrastructures as mentioned in Rehabilitation Initiative 2030 (World Health Organization) should be provided.
A multidisciplinary post-COVID rehabilitation clinic at tertiary hospitals, as well as outdoor and indoor COVID-19 rehabilitation facility, is required.
Future research: Observational studies are needed to find out post-COVID rehabilitation need in able-bodied individuals and also in differently-abled individuals.
Future trials are required to find out the effectiveness of specific interventions to improve functional status of people with long COVID.
Footnotes
Conflict-of-interest statement: All authors declare that they have no conflict of interest.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: February 27, 2022
First decision: April 13, 2022
Article in press: July 11, 2022
Specialty type: Medical laboratory technology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ait Addi R, Morocco; Ustun G, Turkey S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Wang LL
Contributor Information
Raktim Swarnakar, Department of Physical Medicine and Rehabilitation, All India Institute of Medical Sciences, New Delhi 110029, Delhi, India. raktimswarnakar@hotmail.com.
Shiv Lal Yadav, Department of Physical Medicine and Rehabilitation, All India Institute of Medical Sciences, New Delhi 110029, Delhi, India.
References
- 1.Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. 2021;19:141–154. doi: 10.1038/s41579-020-00459-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC Healthcare Workers [Internet] Centers for disease control and prevention. [cited 20 April 2022]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-COVID-conditions.html .
- 3.NICE COVID19 rapid guideline managing the long-term effects of COVID19 2020. [cited 20 April 2022]. Available from: https://www.nice.org.uk/guidance/ng188/resources/COVID19-rapid-guideline-managing-the-longterm-effects-of-COVID19-pdf-51035515742 .
- 4.Agostini F, Mangone M, Ruiu P, Paolucci T, Santilli V, Bernetti A. Rehabilitation setting during and after Covid-19: An overview on recommendations. J Rehabil Med. 2021;53:jrm00141. doi: 10.2340/16501977-2776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Negrini F, de Sire A, Andrenelli E, Lazzarini SG, Patrini M, Ceravolo MG International Multiprofessional Steering Committee of Cochrane Rehabilitation REH-COVER action. Rehabilitation and COVID-19: a rapid living systematic review 2020 by Cochrane Rehabilitation Field. Update as of October 31st, 2020. Eur J Phys Rehabil Med. 2021;57:166–170. doi: 10.23736/S1973-9087.20.06723-4. [DOI] [PubMed] [Google Scholar]
- 6.WHO Rehabilitation and COVID-19. [cited 20 April 2022]. Available from: https://www.who.int/teams/noncommunicable-diseases/COVID-19/rehabilitation .
- 7.Fernández-de-Las-Peñas C, Palacios-Ceña D, Gómez-Mayordomo V, Florencio LL, Cuadrado ML, Plaza-Manzano G, Navarro-Santana M. Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: A systematic review and meta-analysis. Eur J Intern Med. 2021;92:55–70. doi: 10.1016/j.ejim.2021.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reina-Gutiérrez S, Torres-Costoso A, Martínez-Vizcaíno V, Núñez de Arenas-Arroyo S, Fernández-Rodríguez R, Pozuelo-Carrascosa DP. Effectiveness of Pulmonary Rehabilitation in Interstitial Lung Disease, Including Coronavirus Diseases: A Systematic Review and Meta-analysis. Arch Phys Med Rehabil. 2021;102:1989–1997.e3. doi: 10.1016/j.apmr.2021.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Lorenzo R, Conte C, Lanzani C, Benedetti F, Roveri L, Mazza MG, Brioni E, Giacalone G, Canti V, Sofia V, D'Amico M, Di Napoli D, Ambrosio A, Scarpellini P, Castagna A, Landoni G, Zangrillo A, Bosi E, Tresoldi M, Ciceri F, Rovere-Querini P. Residual clinical damage after COVID-19: A retrospective and prospective observational cohort study. PLoS One. 2020;15:e0239570. doi: 10.1371/journal.pone.0239570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang TJ, Chau B, Lui M, Lam GT, Lin N, Humbert S. Physical Medicine and Rehabilitation and Pulmonary Rehabilitation for COVID-19. Am J Phys Med Rehabil. 2020;99:769–774. doi: 10.1097/PHM.0000000000001505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barker-Davies RM, O'Sullivan O, Senaratne KPP, Baker P, Cranley M, Dharm-Datta S, Ellis H, Goodall D, Gough M, Lewis S, Norman J, Papadopoulou T, Roscoe D, Sherwood D, Turner P, Walker T, Mistlin A, Phillip R, Nicol AM, Bennett AN, Bahadur S. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med. 2020;54:949–959. doi: 10.1136/bjsports-2020-102596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van Aerde N, Van den Berghe G, Wilmer A, Gosselink R, Hermans G COVID-19 Consortium. Intensive care unit acquired muscle weakness in COVID-19 patients. Intensive Care Med. 2020;46:2083–2085. doi: 10.1007/s00134-020-06244-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carfì A, Bernabei R, Landi F Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020;324:603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bekelis K, Missios S, Ahmad J, Labropoulos N, Schirmer CM, Calnan DR, Skinner J, MacKenzie TA. Ischemic Stroke Occurs Less Frequently in Patients With COVID-19: A Multicenter Cross-Sectional Study. Stroke. 2020;51:3570–3576. doi: 10.1161/STROKEAHA.120.031217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Denis F, Septans AL, Periers L, Maillard JM, Legoff F, Gurden H, Moriniere S. Olfactory Training and Visual Stimulation Assisted by a Web Application for Patients With Persistent Olfactory Dysfunction After SARS-CoV-2 Infection: Observational Study. J Med Internet Res. 2021;23:e29583. doi: 10.2196/29583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whitcroft KL, Hummel T. Clinical Diagnosis and Current Management Strategies for Olfactory Dysfunction: A Review. JAMA Otolaryngol Head Neck Surg. 2019;145:846–853. doi: 10.1001/jamaoto.2019.1728. [DOI] [PubMed] [Google Scholar]
- 17.Whitcroft KL, Hummel T. Olfactory Dysfunction in COVID-19: Diagnosis and Management. JAMA. 2020;323:2512–2514. doi: 10.1001/jama.2020.8391. [DOI] [PubMed] [Google Scholar]
- 18.Hopkins Medicine. Bouncing Back From COVID-19. [cited 20 April 2022]. Available from: https://www.hopkinsmedicine.org/physical_medicine_rehabilitation/coronavirus-rehabilitation/_files/impact-of-COVID-patient-recovery.pdf .
- 19.Office for National Statistics. Updated estimates of coronavirus (COVID-19) related deaths by disability status January to 20 November 2020. Office for National Statistics, London. [cited 20 April 2022]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coronavirusCOVID19relateddeathsbydisabilitystatusenglandandwales/24januaryto20november2020 .
- 20.Leite VF, Rampim DB, Jorge VC, de Lima MDCC, Cezarino LG, da Rocha CN, Esper RB Prevent Senior COVID-19 Rehabilitation Study. Persistent Symptoms and Disability After COVID-19 Hospitalization: Data From a Comprehensive Telerehabilitation Program. Arch Phys Med Rehabil. 2021;102:1308–1316. doi: 10.1016/j.apmr.2021.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.U.S. Department of Health and Human Services Guidance on “Long COVID” as a Disability Under the ADA, Section 504, and Section 1557. [cited 20 April 2022]. Available from: https://www.hhs.gov/civil-rights/for-providers/civil-rights-COVID19/guidance-long-COVID-disability/index.html#footnote10_0ac8mdc .
- 22.Steere HK, Polich G, Silver JK, Hameed F, Gellhorn AC, Borg-Stein J, Schneider JC. Ambulatory Rehabilitation of Patients Hospitalized with SARS CoV-2 Infections: Early Pandemic Experience in New York City and Boston. PM R. 2021;13:81–86. doi: 10.1002/pmrj.12506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Falvey JR, Krafft C, Kornetti D. The Essential Role of Home- and Community-Based Physical Therapists During the COVID-19 Pandemic. Phys Ther. 2020;100:1058–1061. doi: 10.1093/ptj/pzaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.WHO Community-based health care, including outreach and campaigns, in the context of the COVID-19 pandemic. [cited 20 April 2022]. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-Comm_health_care-2020.1 .
- 25.Vourganas I, Stankovic V, Stankovic L. Individualised Responsible Artificial Intelligence for Home-Based Rehabilitation. Sensors (Basel) 2020;21 doi: 10.3390/s21010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Akbari A, Haghverd F, Behbahani S. Robotic Home-Based Rehabilitation Systems Design: From a Literature Review to a Conceptual Framework for Community-Based Remote Therapy During COVID-19 Pandemic. Front Robot AI. 2021;8:612331. doi: 10.3389/frobt.2021.612331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hassanien AE, Salam A, Darwish A. Artificial intelligence approach to pre- dict the COVID-19 patient’s recovery. [cited 20 April 2022]. Available from: https://easychair.org/publications/preprint/4bf1 .
- 28.Li J, Xia W, Zhan C, Liu S, Yin Z, Wang J, Chong Y, Zheng C, Fang X, Cheng W, Reinhardt JD. A telerehabilitation programme in post-discharge COVID-19 patients (TERECO): a randomised controlled trial. Thorax. 2022;77:697–706. doi: 10.1136/thoraxjnl-2021-217382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Werneke MW, Deutscher D, Grigsby D, Tucker CA, Mioduski JE, Hayes D. Telerehabilitation During the COVID-19 Pandemic in Outpatient Rehabilitation Settings: A Descriptive Study. Phys Ther. 2021;101 doi: 10.1093/ptj/pzab110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Swarnakar R, Yadav SL, Srikumar V, Soni KD, Aggrawal R, Trikha A. ReCOVer study: A Cross-sectional Observational Study to Identify the Rehabilitation Need in Post-discharge COVID-19 Survivors [Protocol]. [cited 20 April 2022]. Available from: https://www.medrxiv.org/content/10.1101/2021.04.19.21255750v1.full .