To the Editor,
There has been an unprecedented rise in Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). While the predominant features of the disease are fever, cough, shortness of breath, and eventually respiratory failure, multiorgan system involvement is not an uncommon feature of the disease. A multitude of neurological manifestations including ischemic stroke, intracranial hemorrhages, and central nervous system (CNS) vasculitis have been reported.[1]
A 10-year-old boy presented with a 5-day history of declining sensorium and fever. The patient was a diagnosed case of COVID-19 by detection of SARS-CoV-2 viral nucleic acid in a nasopharyngeal swab specimen using real-time reverse-transcription polymerase chain reaction assay (RT-PCR) 20 days back. The respiratory symptoms at the time of neurological deterioration were minimal. Chest radiograph and computed tomography of thorax revealed features of resolving pneumonia. The lumbar puncture was limited due to the traumatic tap. Coagulation profile was abnormal with a platelet count of 48. 48 thousand/mm3, prothrombin time 39.9 s (reference 13.5 s), and International Normalized Ratio 3.09 (normal range: 0.90–1.10). Laboratory analysis reveals raised serum ferritin (329 ng/mL, normal range: 7.0–140.0 ng/mL) and C-reactive protein levels (94 mg/L, normal range <6 mg/L). Interleukin-6 levels were within normal limits. D-dimer levels were also raised (1.4 μg/mL, normal range <0.50 μg/mL). Contrast-enhanced magnetic resonance imaging (MRI) of the Brain revealed hypointense signal in bilateral thalami, midbrain, pons, and left superior cerebellar peduncle on T1 and T2 weighted images with T2 hypointense rim [Figure 1]. No diffusion restriction or contrast enhancement was seen [Figure 2]. Multiple other small similar lesions were seen in bilateral cerebral and cerebellar hemispheres. There were susceptibility changes within these areas signifying hemorrhage. MR angiography revealed the irregular outline of the cavernous segment of bilateral internal cerebral and left middle cerebral arteries. MR venography was normal. On day two of admission, the patient developed hypotension with respiratory distress. Inotropes were started and the patient was kept on mechanical ventilation. Unfortunately, the patient did not survive.
Figure 1.
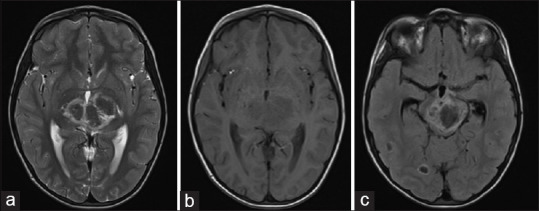
Axial T2 (a), T1 (b) weighted MRI images of the brain show hypointense area involving bilateral thalami with a hyperintense rim on T2 weighted images. Axial FLAIR image (c) shows a hypointense area in the midbrain with a hyperintense rim. Few other similar characteristic lesions are seen in the right temporal and occipital lobe
Figure 2.
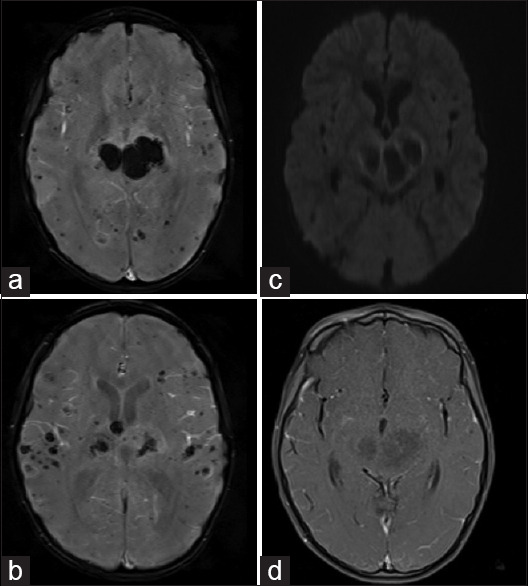
Susceptibility weighted images (a, b) show hypointense signals in bilateral thalami and bilateral cerebral parenchyma suggestive of hemorrhagic areas. No restriction on the diffusion-weighted image (c) or contrast enhancement is seen on post-contrast T1 weighted image (d)
Acute hemorrhagic necrotizing encephalopathy (AHNE) is a rare entity, reported in cases of viral infections, particularly influenza. The first case of COVID-19 associated AHNE was reported by Poyiadji et al.[2] in a 58-year-old female patient. Subsequently, similar cases were reported from various parts of the world with more emphasis on clinical features and pathophysiological mechanisms of neurological affliction.[3,4] The first case of COVID-19 related AHNE in India was reported in a 35-year-old male patient by Kumar et al.[5] Presenting features can range from headache, meningism, altered sensorium to coma, and persisting/progressive encephalopathy. There are various proposed mechanisms of neurological involvement in COVID-19. There is evidence of direct entry of the virus through the ACE-2 receptor, either through the blood-brain barrier or neuronal transport.[6,7] Indirect mechanisms like hypercoagulable state from systemic inflammation, intra-cranial cytokine storm, post-infection immune-mediated responses, endothelial damage due to direct viral invasion resulting in microangiopathy are also hypothesized.[8,9] Of most notable interest is the hypothesis of intracranial cytokine storm which results in the breakdown of the blood-brain barrier without any evidence of direct viral invasion or postinfective demyelination. The opening CSF pressure and protein may be elevated. Most of the cases reported negative SARS-CoV-2 PCR of the CSF samples. The most characteristic imaging findings include symmetric, multifocal T2/FLAIR hyperintense in cerebral white matter, brain stem, and cerebellum with areas of hemorrhage within. In most of the cases, there is bilateral thalamic involvement,[10] as in typical cases of AHNE. Contrast-enhanced images may show a ring of enhancement. Although outcome data are limited, early detection and prompt treatment may useful. High-dose corticosteroids, immune-modulators, and plasmapheresis are available treatment options and can lead to recovery in the early stages.
To conclude, AHNE should be considered in COVID-19 patients with severe encephalopathy. Awareness about this entity will lead to a better understanding of the pathophysiological mechanism, associations, and risk factors resulting in better patient care.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sachdev K, Agrawal S, Ish P, Gupta N, Raheja K. Neurological manifestations of COVID-19: A brief review. Indian J Med Res. 2020;152:41–7. doi: 10.4103/ijmr.IJMR_1395_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Poyiadji N, Shahin G, Noujaim D, Stone M, Patel S, Griffith B. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: Imaging features. Radiology. 2020;296:119–20. doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dixon L, Varley J, Gontsarova A, Mallon D, Tona F, Muir D, et al. COVID-19-related acute necrotizing encephalopathy with brain stem involvement in a patient with aplastic anemia. Neurol Neuroimmunol Neuroinflamm. 2020;7:e789. doi: 10.1212/NXI.0000000000000789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Virhammar J, Kumlien E, Fällmar D, Frithiof R, Jackmann S, Sköld MK, et al. Acute necrotizing encephalopathy with SARS-CoV-2 RNA confirmed in cerebrospinal fluid. Neurology. 2020;95:445–9. doi: 10.1212/WNL.0000000000010250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar N, Kumar S, Kumar A, Pati BK, Kumar A, Singh C, et al. Acute necrotizing encephalitis as a probable association of COVID-19. Indian J Crit Care Med. 2020;24:991–4. doi: 10.5005/jp-journals-10071-23636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 virus targeting the CNS: Tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. 2020;11:995–8. doi: 10.1021/acschemneuro.0c00122. [DOI] [PubMed] [Google Scholar]
- 7.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–80.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ, et al. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–4. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DosSantos MF, Devalle S, Aran V, Capra D, Roque NR, de Mattos Coelho-Aguiar J, et al. Neuromechanisms of SARS-CoV-2: A review. Front Neuroanat. 2020;14:37. doi: 10.3389/fnana.2020.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong AM, Simon EM, Zimmerman RA, Wang HS, Toh CH, Ng SH. Acute necrotizing encephalopathy of childhood: Correlation of MR findings and clinical outcome. AJNR Am J Neuroradiol. 2006;27:1919–23. [PMC free article] [PubMed] [Google Scholar]


