Abstract
Currently, the debate surrounding the regulation of e-cigarettes focuses mainly on the size of e-cigarettes’ potentially beneficial effects (i.e., adult cessation) versus their unwarranted effects (i.e., initiation among tobacco-naïve adolescents). Therefore, we investigated the relative scale of e-cigarette use transitions in the United States. We reported cross-sectional weighted prevalence estimates of past-month e-cigarette use by ever cigarette use from Waves 1–4 of the Population Assessment of Tobacco and Health study (2013–2018) among youth (12–17 years) and adults (≥18 years). We also examined past-month e-cigarette mono and dual transitions related to cigarette smoking and reported the longitudinal weighted prevalence across waves. Among youth new e-cigarette users, the proportion of never-cigarette smokers increased from 24.1% in Wave 1 (n= 418) to 51.4% in Wave 4 (n=310) (p<0.0001 for trend). Of youth e-cigarette mono-users in Wave 1 (n= 151), 15.2% transitioned to cigarette mono-use and 8.2%, dual-use at Wave 2 or 3 or 4, compared to 60.2%, no tobacco use and 16.4%, e-cigarette mono-use. Among young adult dual-users (18–24 years; n=684), 22.6% transitioned to no tobacco use, 60.1% continued cigarette use, 11.4% dual use, and 5.9% e-cigarette mono-use. Among adult dual-users ≥25 years old (n=1560), 13.6% transitioned to no tobacco use, 71.3% cigarette mono-use, 9.0% dual-use, and 6.1% e-cigarette mono-use. Transition to cigarette mono-use and continued dual-use were common among adult past-month e-cigarette users, while e-cigarette uptake was common among youth never-cigarette smokers. These findings contrast with data from other countries showing limited evidence of e-cigarette initiation among youth never cigarette smokers. Both e-cigarette and cigarette use should be addressed in youth and adults, given the potential for dual use in both populations.
Keywords: Cigarettes, Dual use, E-cigarettes, Harm reduction, Longitudinal
Introduction
E-cigarettes (electronic nicotine delivery systems, ENDS) use among youth in the United States (US) has intensified the debate about their contribution to reducing harm from tobacco and concerns about their role in smoking initiation (National Academies of Sciences, 2018; US Department of Health and Human Services, 2016). Documented reports of e-cigarette use differ across studies depending on the age group. E-cigarettes have been the commonly reported tobacco product utilized among youth in the US since 2014, with 19.6% of high school students reporting current e-cigarette use in 2020 (Wang et al., 2020) compared to 4.6% and 5% who reported current cigarette or cigar use (Gentzke et al., 2020). Additionally, e-cigarette sales increased by 122.2% from 2014 to 2020 (Ali et al., 2020). Likewise, among adults, the current use of e-cigarettes ranges from 1.4% to 6.8% across several studies (Chou et al., 2017; Coleman et al., 2017; Delnevo et al., 2016; Kasza et al., 2017; McMillen et al., 2015; Parker & Villanti, 2019; Phillips et al., 2017; Villarroel et al., 2020).
A central premise of e-cigarette harm reduction is that should their use continue to increase; they will reduce smoking harms in populations by enabling cessation and reducing the smoking frequency of combustible cigarettes. From this perspective, e-cigarette’s potential for tobacco control promises reductions in the global burden of disease caused by smoking (Abrams et al., 2018; Hajek et al., 2014; McNeill A et al., 2015; Warner & Mendez, 2018). On the other hand, the increased popularity of e-cigarettes and their potential to lead to cigarette smoking raise concerns about their role in expanding nicotine addiction among young people and subsequent perpetuation of the tobacco epidemic (Chapman et al., 2018; Glantz & Bareham, 2018; Soneji et al., 2017).
The debate of the impact of e-cigarettes in populations has often been marred by inferring causal or population effects from cross-sectional, ecological studies or data obtained from limited samples or short follow-ups (Barrington-Trimis et al., 2015; Chapman et al., 2018; Dutra & Glantz, 2014). The 2018 report on e-cigarettes by the National Academies of Science, Engineering and Medicine emphasized that because the e-cigarette phenomenon is relatively recent, “majority of studies … lack sufficient duration of follow-up to study the naturalistic cigarette smoking progression sequence” (National Academies of Sciences, 2018). Accordingly, what has been missing is a real-world look at the totality of potentially positive/negative transitions of e-cigarette use in the US, based on representative longitudinal data.
In 2011, the National Institutes of Health (NIH) and Food and Drug Administration (FDA) commenced the Population Assessment of Tobacco and Health (PATH) cohort study, as the first extensive research effort since Congress gave FDA the authority to regulate tobacco products in 2009 (US Department of Health and Human Services, 2020; Hyland et al., 2017). Studies from PATH Waves 1 and 2 started answering some questions about e-cigarette transition during one year among US adults (Coleman et al., 2018; Verplaetse et al., 2018). These studies showed mixed results about e-cigarettes’ value for adult cigarette smokers’ cessation. For example, prior research found that the majority of adult dual-users in Wave 1 (87.8%) continued dual-use or cigarette-only smoking at one-year follow-up, compared to 12.1% who quit cigarette smoking (7.0%) or maintained e-cigarette use only (5.1%) (Coleman et al., 2018). Furthermore, in a systematic review and meta-analysis of observational and clinical studies, the authors found that e-cigarette use was associated with lower odds of cigarette smoking cessation among those who use(d) e-cigarettes compared to those who did not use e-cigarettes (Kalkhoran and Glantz 2016). However, the authors noted that the review’s conclusions were not sensitive to the design of the included studies; or whether cigarette smokers were interested in quitting. In contrast, a Cochrane review showed that using an e-cigarette with nicotine increased smoking cessation compared to e-cigarettes without nicotine or nicotine replacement therapy with moderate-certainty evidence. However, the included studies were randomized clinical trials and limited by imprecision (Hartmann-Boyce et al., 2021).
Although prior studies have been conducted on e-cigarettes and cigarettes, most have been conducted using mainly cross-sectional study designs (Mirbolouk et al., 2018); with the evolving e-cigarette marketplace, there is a need to assess changing use patterns among a nationally representative group of youth and adult e-cigarette users. This current study considers four waves from the PATH study for youth and adults to provide a comparative overview of the real-world evolution of e-cigarette use with cigarette smoking in the US between 2013–2018. Currently, the debate surrounding the regulation of e-cigarettes focuses mainly on the size of e-cigarettes’ potentially beneficial effects (i.e., adult cessation) vs. their unwarranted effects (i.e., initiation among tobacco-naïve adolescents) (Abrams et al., 2018). Therefore, we aimed to examine the following outcomes based on the relative scale of potentially positive/negative transitions of e-cigarettes in the US, including for youth 1) trends in continued never-cigarette smoking among e-cigarette users; 2) transition from e-cigarette mono-use to cigarette smoking; and for adults 3) transition of dual (e-cigarette/cigarette) use to e-cigarette mono or no tobacco use (quitting). A comprehensive picture of e-cigarette use with respect to cigarette use may support the development of multiple prevention strategies that will help interrupt pathways to reduce e-cigarette and cigarette use in the general population.
Methods
Study sample
We used data from the public use files of Waves 1 (2013–2014), 2 (2014–2015), 3 (2015–2016), and 4 (2016–2018) of the PATH study (US Department of Health and Human Services, 2020. Detailed methodology for the PATH has been previously described (Hyland et al., 2017). Briefly, the PATH is a nationally representative sample of civilian, non-institutionalized US youth and adults that examines tobacco use and its effect on health. Youth (12–17 years) and adults (≥18 years) were surveyed separately using audio computer-assisted self-interview. The survey included a stratified address-based sample of households that oversampled young adults aged 18–24 years, tobacco users, and African Americans in the adult cohort. The household screener response rate was 54% and the youth survey response rates were 78.4%, 87.3%, 83.3% and 79.5% for Waves 1–4, respectively. The survey response rates for the adult Waves 1–4 data were 74.0%, 83.2%, 78.4% and 73.5%, respectively. The Westat Institutional Review Board provided approval for the PATH study. Participants aged ≥18 years provided informed consent, and youth participants provided assent while their parent/legal guardian provided consent. Survey responses were weighted to adjust for nonresponse, varying selection probabilities, and oversampling to reflect national estimates. Our analysis focused on cross-sectional trends in continued never-cigarette smoking among e-cigarette users, as well as transitions among youth and adults who reported past-month (past 30-day) use of e-cigarettes, alone (mono-use) or in combination with cigarettes (dual-use) at Wave 1 (W1) and had complete follow-up information at Wave 2 (W2) or 3 (W3) or 4 (W4). The Institutional Review Board of the University reviewed this current study and deemed it exempt.
Study measures
Tobacco use
Past-month e-cigarette use was derived from answers to questions; “ever used an e-cigarette” and respondents who answered “yes” were asked; “used an e-cigarette at least once in the past 30 days” for both youth and adults at each wave (Chaffee et al., 2018; Dai et al., 2018; Kasza et al., 2017). This definition was applied to past-month cigarette smoking. Ever cigarette smoking was assessed from the question; “(n)ever smoked a cigarette, even one or two puffs” for youth and adults (Chaffee et al., 2018). Those who responded “Yes” were classified as ever users, and those who responded “No” as never users. Because e-cigarette/cigarette use is one of the most common and important combinations for the regulatory implications of e-cigarettes (Kasza et al., 2017), dual-use was derived from responses of ≥1 or more days to past-month e-cigarette and cigarette use as “Yes”, while 0 was classified as “No”. We used the broadened definition for e-cigarettes from W3. The question on e-cigarette use was expanded to include other ENDS (i.e., e-cigarettes, e-cigars, e-hookahs, e-pipes, hookah pens, personal vaporizers, and vape pens), with past-month use implying the use of any ENDS (US Department of Health and Human Services, 2020). To avoid confusion and have consistent terminology, we used the term e-cigarettes and pointed to the possible effect of the change in e-cigarette question from W3 on our analysis in the limitations.
Transitions
All transitions are for past-month tobacco use. The change in e-cigarette use status across the waves was considered for e-cigarette mono- and dual-use (Coleman et al., 2018). For past-month e-cigarette mono-users at W1, we considered the following transitions from W1 to W2 or W3 or W4; 1) transition to dual-use, 2) continuing e-cigarette mono-use, 3) transition to cigarette mono-use, 4) transition to no use of any tobacco/nicotine (considered an indicator of quitting). For past-month dual-users at W1, we considered the following transitions from W1 to W2 or W3 or W4; 1) continuing dual-use, 2) transition to e-cigarette mono-use, 3) transition cigarette mono-use, 4) transition to no use of any tobacco/nicotine. No use of any tobacco/nicotine at W2 or W3 or W4 was defined as participants reporting no past-month use of e-cigarettes and cigarettes, as well as other tobacco products (OTPs).
Statistical analyses
We reported cross-sectional weighted prevalence estimates for participants with complete data for past-month e-cigarette use and cigarette smoking in the overall population in the four waves for youth and adults separately. We summarized age-group distributions of past-month e-cigarette use for youth and adults by ever-cigarette smoking. Furthermore, we conducted descriptive statistics by calculating prevalence estimates for e-cigarette mono- and dual-use among youth and adults identified from W1 and assessed change in their use status at W2 or W3 or W4 in the longitudinal analysis (Coleman et al., 2018).
We used the individual replicate cross-sectional weights provided by the PATH study for the four waves to obtain the prevalence estimates. For the longitudinal analysis, we used the all-waves replicate weight for W4. The replicate weights provide unbiased variance estimates to account for nonresponse, varying selection probabilities, and oversampling to reflect national demographics (US Department of Health and Human Services, 2020). Weighted percentages were reported with corresponding 95% confidence intervals (CI). Pearson chi-square tests were used to evaluate differences in proportions between ever- and never-cigarette smoking by e-cigarette use. We tested the linear trend for the proportions of overall past-month e-cigarette use, and e-cigarette use by ever- and never-cigarette smoking against the general population of the PATH study and across the four waves using the chi-square test for trends.
Youth identified from W1 and aged up into the adult data at W2 or W3, or W4 were included only in the youth transition analysis. We conducted a supplemental analysis for the transitions of never- and past-month cigarette users who had reported no use of e-cigarettes at W1 among youth and adults (Online Resource 1). The analytic sample included participants who provided complete data for the e-cigarette and cigarette use across the waves. Data analyses were performed between 2018 and 2020, using STATA 14 and 16.0 (StataCorp LP, College Station, TX).
Results
Overall e-cigarette prevalence and trends among youth and adults
The overall prevalence of past-month e-cigarette use among 13559 youth in W1 was 3.1% (95% CI: 2.8–3.5), increasing to 3.6% (95% CI: 3.2–4.1) in W2 among 12059 youth, 4.1% (95% CI: 3.7–4.7) in W3 among 11546 youth and 4.3% (95% CI: 3.9–4.8) in W4 among 14431 youth (p<0.0001 for trend) (Table 1). Among 32225 US adults in W1, overall prevalence of past-month e-cigarette use was 6.7% (95% CI: 6.4–7.0), becoming 6.3% (95% CI: 5.9–6.6) in W2 among 27460 adults, 7.0% (95% CI: 6.7–7.3) in W3 among 27860 adults and 6.2% (95% CI: 6.0–6.5) in W4 among 33170 adults (p=0.0001 for trend) (Table 2).
Table 1:
Prevalence of past-month e-cigarette use among US youth (12–17 years) by cigarette smoking history: PATH study 2013–2018
| Past-month E-cigarette use | Ever Cigarette use n (%, 95% CI) |
Never Cigarette use n (%, 95% CI) |
Total n (%, 95% CI) |
|---|---|---|---|
| Wave 1; 2013–2014 (N=13,559) | |||
| Yes, n (%, 95% CI) | 321 (2.4, 2.1–2.7) a,b | 97 (0.8, 0.6–0.9) c,d | 418 (3.1, 2.8–3.5) e |
| Age, n (%, 95% CI) | |||
| 15–17 | 271 (78.1, 72.8–82.5) | 71 (21.9, 17.5–27.2) | 342 (100.0) |
| Wave 2; 2014–2015 (N=12,059) | |||
| Yes, n (%, 95% CI) | 273 (2.3, 2.0–2.7) | 141 (1.3, 1.1–1.6) | 414 (3.6, 3.2–4.1) |
| Age, n (%, 95% CI) | |||
| 15–17 | 220 (65.2, 60.0–70.3) | 106 (34.8, 29.7–40.3) | 326 (100.0) |
| Wave 3; 2015–2016 (N=11,546) | |||
| Yes, n (%, 95% CI) | 273 (2.5, 2.2–3.0) | 176 (1.6, 1.3–1.9) | 449 (4.1, 3.7–4.7) |
| Age, n (%, 95% CI) | |||
| 15–17 | 223 (63.6, 57.3–69.5) | 137 (36.4, 30.5–42.7) | 360 (100.0) |
| Wave 4; 2016–2018 (N=14,431) | |||
| Yes, n (%, 95% CI) | 331 (2.4, 2.1–2.7) | 258 (1.9, 1.7–2.2) | 589 (4.3, 3.9–4.8) |
| Age, n (%, 95% CI) | |||
| 15–17 | 281 (57.7, 52.4–62.9) | 204 (42.3, 37.1–47.6) | 485 (100.0) |
Abbreviations: CI, confidence interval; PATH, Population Assessment of Tobacco and Health Study; US, United States; n, unweighted sample; %, weighted percentages rounded up to 1 decimal place.
Indicates significant (p<0.05) difference between ever and never cigarette smoking among e-cigarette users at each wave.
Indicates significant (p<0.05) linear trend for the comparison across Waves 1–4 for the proportion of overall e-cigarette ever cigarette users among past-month e-cigarette users.
Indicates significant (p<0.05) linear trend for the comparison across Waves 1–4 for the proportion of overall e-cigarette never cigarette users in general population.
Indicates significant (p<0.05) linear trend for the comparison across Waves 1–4 for the proportion of overall never cigarette use among past-month e-cigarette users.
Indicates significant (p<0.05) linear trend for the comparison across Waves 1–4 for the proportion of overall past month e-cigarette use in general population.
Indicates significant (p<0.05) difference between age-groups for ever and never cigarette smoking among e-cigarette users at Wave 1 only.
Table 2:
Prevalence of past-month e-cigarette use among US adults (≥18 years) by cigarette smoking history: PATH study, 2013–2018
| Past-month E-cigarette use | Ever Cigarette use n (%, 95% CI) |
Never Cigarette use n (%, 95% CI) |
Total n (%, 95% CI) |
|---|---|---|---|
| Wave 1; 2013–2014 (N=32,225) | |||
| Yes, n (%, 95% CI) | 4308 (6.5, 6.2–6.8) a, b | 119 (0.2, 0.1–0.2) c, d | 4427 (6.7, 6.4–7.0) e |
| Age, n (%, 95% CI) | |||
| 25+ | 2888 (99.1, 98.6–99.4) | 25 (0.9, 0.6–1.4) | 2913 (100.0) |
| Wave 2; 2014–2015 (N=27,460) | |||
| Yes, n (%, 95% CI) | 3262 (6.1, 5.8–6.5) | 117 (0.2, 0.1–0.2) | 3379 (6.3, 5.9–6.6) |
| Age, n (%, 95% CI) | |||
| 25+ | 2191 (99.6, 99.1–99.8) | 8 (0.4, 0.2–1.0) | 2199 (100.0) |
| Wave 3; 2015–2016 (N=27,860) | |||
| Yes, n (%, 95% CI) | 3478 (6.5, 6.3–6.9) | 298 (0.5, 0.4–0.5) | 3776 (7.0, 6.7–7.3) |
| Age, n (%, 95% CI) | |||
| 25+ | 2131 (98.2, 97.1–98.9) | 30 (1.8, 1.1–2.9) | 2161 (100.0) |
| Wave 4; 2016–2018 (N=33,170) | |||
| Yes, n (%,95% CI) | 3662 (5.8, 5.6–5.1) | 360 (0.4, 0.4–0.5) | 4022 (6.2, 6.0–6.5) |
| 25+ | 2190 (98.0, 97.0–98.7) | 34 (2.0, 1.3–3.0) | 2224 (100.0) |
Abbreviation: CI, confidence interval; PATH, Population Assessment of Tobacco and Health Study; US, United States; n, unweighted sample, %, weighted percentages rounded up to 1 decimal place.
Indicates significant (p<0.05) difference between ever and never cigarette smoking among e-cigarette users at each wave.
Indicates significant (p<0.05) linear trend for the comparison across Waves 1–4 for the proportion of overall e-cigarette ever cigarette users among past-month e-cigarette users.
Indicates significant (p<0.05) linear trend for the comparison across Waves 1–4 for the proportion of overall e-cigarette never cigarette users in general population.
Indicates significant (p<0.05) linear trend for the comparison across Waves 1–4 for the proportion of overall never cigarette use among past-month e-cigarette users.
Indicates significant (p<0.05) linear trend for the comparison across Waves 1–4 for the proportion of overall past month e-cigarette use in general population.
Indicates significant (p<0.05) difference between age-groups for ever and never cigarette smoking among e-cigarette users at each wave.
Trends in proportions of youth never-cigarette smokers among new past-month e-cigarette users
In W1, 24.1% (95% CI: 20.1–28.6) of past-month e-cigarette users were never-cigarette smokers, increasing to 35.8% (95% CI: 31.1–40.7) in W2, 38.2% (95% CI: 32.8–43.9) in W3 and 44.3% (95% CI: 39.8–48.9) in W4 (p<0.0001 for trend; data not shown). The proportion of never-cigarette smokers among new past-month e-cigarette users (i.e., new e-cigarette users in the past 30 days in the subsequent waves) rose from 24.1% in W1 to 51.4% in W4 (p<0.0001 for trends; Figure 1: Panel A).
Figure 1.
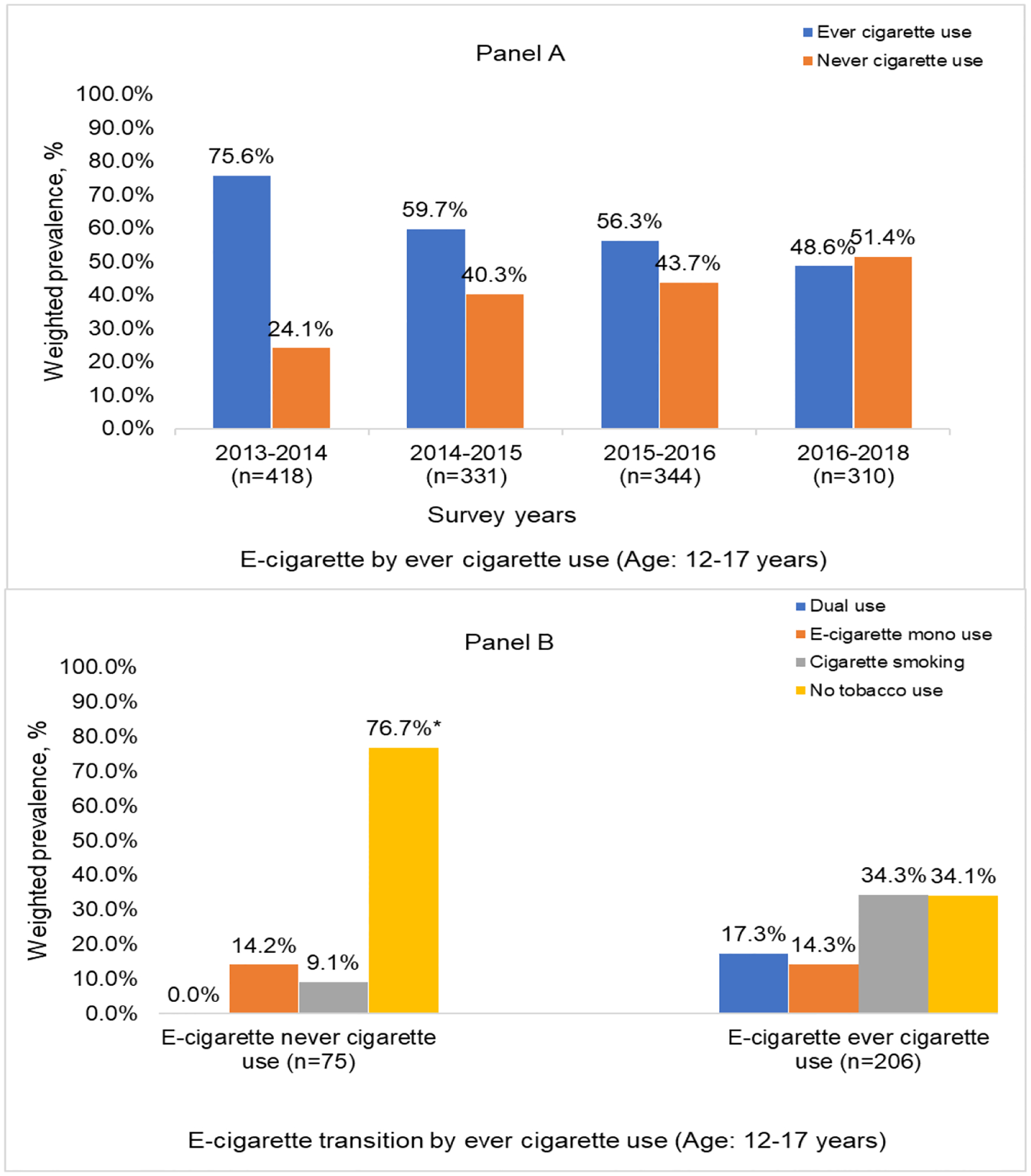
Panel A: Changes in never-cigarette smoking status among new past-month e-cigarette users (12–17 years): PATH study, 2013–2018
Panel B: Transitions of past-month e-cigarette use among youth (12–17 years) according to never vs. ever cigarette smoking: PATH study, 2013–2018
*p<0.001 for difference between transition categories at Wave 2/3/4 among e-cigarette never cigarette users and e-cigarette ever cigarette users
Prevalence of e-cigarette transitions among youth
For e-cigarette mono-users in W1 (n=151), 15.2% transitioned to cigarette smoking and 8.2% to dual-use at W2 or W3 or W4, compared to 60.2% reporting no tobacco use, or 16.4% reporting e-cigarette mono-use at W2 or W3 or W4 (p<0.0001; Table 3). This trend differed according to ever-cigarette smoking, where among e-cigarette never-cigarette smokers in W1, 9.1% transitioned to past-month cigarette smoking (9.1% cigarette, 0% dual-use) at W2 or W3 or W4, compared to 51.6% transitioning to past-month cigarette smoking (34.3% cigarette, 17.3% dual-use) among e-cigarette, ever-cigarette smokers (p<0.0001; Figure 1: Panel B). Among youth dual-users in W1 (n=129), 61.2% maintained cigarette smoking or dual-use at W2 or W3 or W4 (Table 3).
Table 3:
Transition of past-month e-cigarette use among the US population (≥12 years): PATH study, 2013–2018
| Wave 2/3/4 | ||||
|---|---|---|---|---|
| Wave 1 | ||||
| E-cigarette dual n (%, 95% CI) |
E-cigarette mono n (%, 95% CI) |
Cigarette mono n (%, 95% CI) |
No tobacco n (%, 95% CI) |
|
| 12–17 years | ||||
| Total (n=280) |
32
(12.5, 8.7–17.8) |
33
(13.9, 9.9–19.2) |
82
(27.5, 21.9–33.9) |
133
(46.1, 40.4–51.8)* |
| E-cigarette dual use (n=129) | 20 (18.1, 11.0–28.4) |
13 (10.7, 6.0–18.4) |
60 (43.1, 32.6–54.2) |
36 (28.1, 19.8–38.2) |
| E-cigarette mono use (n=151) | 12 (8.2, 5.6–14.3) |
20 (16.4, 10.6–24.4) |
22 (15.2, 10.0–22.5) |
97 (60.2, 51.9–68.0) |
| 18–24 years | ||||
| Total (n=923) |
88
(9.6, 7.8–12.0) |
74 (9.0, 7.1–11.3) |
470
(49.4, 45.6–53.2) |
291
(32.0, 28.7–35.4)* |
| E-cigarette dual use (n=684) | 74 (11.4, 9.0–14.5) |
35 (5.9, 4.3–8.1) |
425 (60.1, 55.4–64.5) |
150 (22.6, 19.3–26.3) |
| E-cigarette mono use (n=239) | 14 (4.8, 2.6–8.5) |
39 (17.6, 12.7–23.8) |
45 (19.3, 14.2–25.8) |
141 (58.3, 49.6–66.5) |
| ≥25 years | ||||
| Total (n=1900) |
153
(7.8, 6.6–9.2) |
202
(11.0, 9.3–12.9) |
1175
(60.9, 58.0–63.9) |
370
(20.3, 18.1–22.6)* |
| E-cigarette dual use (n=1560) | 142 (9.0, 7.5–10.7) |
89 (6.1, 4.7–7.9) |
1127 (71.3, 68.1–74.4) |
202 (13.6, 11.5–16.1) |
| E-cigarette mono use (n=340) | 11 (2.6, 1.5–4.5) |
113 (32.7, 27.8–38.1) |
48 (14.7, 10.8–19.6) |
168 (50.0, 44.6–55.3) |
Abbreviations: PATH, Population Assessment of Tobacco and Health; US, United States; %, weighted percentage; 95% CI, 95% confidence interval.
Note: Frequencies are unweighted; weighted % are row %.
Bold face indicates differences between groups (e-cigarette dual use, e-cigarette mono use, cigarette mono use and no tobacco use) were significant at p <0.0001.
Trends in proportions of adult never-cigarette smokers among new past-month e-cigarette users
In W1, 2.3% (95% CI; 1.9–2.9) of adult past-month e-cigarette users were never-cigarette smokers, increasing to 2.8% (95% CI: 2.3–3.5) in W2, 6.5% (95% CI: 5.7–7.5) in W3 and 6.7% (95% CI: 5.8–7.6) in W4 (p<0.0001 for trend; data not shown). The proportion of never-cigarette users among new past-month e-cigarette users aged 18–24 years rose from 6.7% in W1 to 22.4% in W4 (p<0.0001 for trend; Figure 2: Panel A). Among adults aged ≥25 years, the proportion of never-cigarette users increased from 0.9% in W1 to 3.7% in W4 (p<0.0001 for trend; Figure 2: Panel B).
Figure 2.
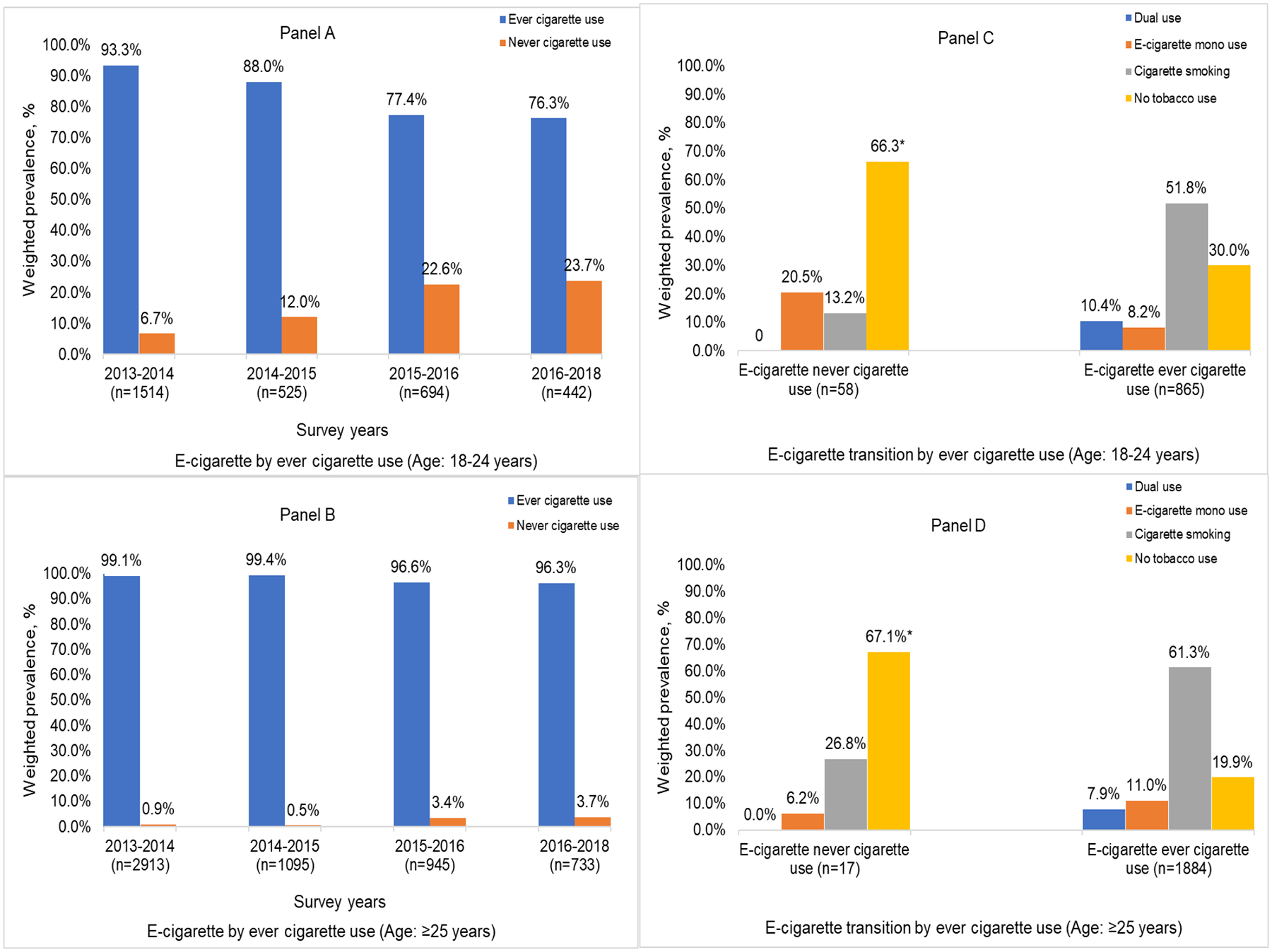
Panel A: Changes in never-cigarette smoking status among new past-month e-cigarette users (18–24 years): PATH study, 2013–2018
Panel B: Changes in never-cigarette smoking status among new past-month e-cigarette users (≥25 years): PATH study, 2013–2018
Panel C: Transitions of past-month e-cigarette use among youth (18–24 years) according to never vs. ever cigarette smoking: PATH study, 2013–2018
Panel D: Transitions of past-month e-cigarette use among youth (≥25 years) according to never vs. ever cigarette smoking: PATH study, 2013–2018
*p<0.001 for difference between transition categories at Wave 2/3/4 among e-cigarette never cigarette users and e-cigarette ever cigarette users
Prevalence of e-cigarette transitions among adults
For adult dual-users aged 18–24 years in W1 (n=684), 60.1% were cigarette mono-users in W2 or W3 or W4, and 11.4% continued as dual-users (Table 3). Among those aged ≥25 years (n=1560), 71.3% were cigarette mono-users, and 9.0%, dual-users. For adult e-cigarette mono-users aged 18–24 years at W1 (n=239), 58.3% reported no use of any tobacco at W2 or W3 or W4, compared to 36.9% who continued with e-cigarettes (17.6%) or progressed to cigarette smoking (19.3%). This trend differed according to ever-cigarette smoking, where among e-cigarette users aged 18–24 years who were never-cigarette smokers in W1, 13.2% transitioned to past-month cigarette smoking at W2 or W3 or W4, compared to 72.2% transitioning to past-month cigarette smoking (51.8% cigarette-, 10.4% dual-use) among e-cigarette, ever-cigarette smokers (p<0.0001; Figure 2: Panel C).
Among e-cigarette mono users aged ≥25 years (n=340), 50.0% reported no use of any tobacco at W2 or W3 or W4, compared to 47.4% who continued with e-cigarettes (32.7%) or progressed to cigarette smoking (14.7%) (Table 3). This trend differed according to ever-cigarette smoking, where among e-cigarette users aged ≥25 years who were never-cigarette smokers in W1, 26.8% transitioned to past-month cigarette smoking at W2 or W3 or W4, compared to 69.2% transitioning to past-month cigarette smoking (61.3% cigarette-, 7.9% dual-use) among e-cigarette, ever-cigarette smokers (p=0.0002; Figure 2: Panel D).
Discussion
Our analysis provides a comprehensive perspective of the evolution of e-cigarette use with cigarette use among youth and adults in the US between 2013–2018. Overall, e-cigarette use increased among youth, but not adults, and younger e-cigarette users were more likely to be never- than ever-cigarette smokers. Adult e-cigarette users, by contrast, were mainly cigarette smokers. Looking at e-cigarette transition to cigarette smoking in youth showed that one in 4 e-cigarette users who were never-cigarette smokers in W1 transitioned to cigarette smoking (i.e., dual- and cigarette mono-use) at W2 or W3 or W4. E-cigarette transitions in adults aged 18–24 years showed that among past-month dual-users in W1, 22.6% reported no past-month use of any tobacco. In contrast, 60.1% continued as cigarette and 11.4% as dual-users at W2 or W3 or W4. For adults aged ≥25 years, among dual-users in W1, 13.6% reported no past-month use of any tobacco, while 71.3% continued as cigarette users and 9.0% as dual-users at W2 or W3 or W4. Our estimates of e-cigarette prevalence among youth in the PATH study were generally lower than those from school-based national surveys of youth such as the National Youth Tobacco Survey. These findings are comparable with literature that explain the differences in the mode of survey administration may account for the differences in prevalence because surveys administered in a school-based environment tend to overestimate tobacco use behaviors due to peer influences. In contrast, youth from home-based surveys may underestimate tobacco use behaviors due to fear of their parents/legal guardians.
Trends of never-cigarette use among youth e-cigarette users
One of the main criteria to judge e-cigarettes’ potential for harm reduction is their utility in helping adult smokers quit without causing substantial initiation and addiction among young never-cigarette smokers (Maziak, 2014). As the evidence of young e-cigarette smokers being at greater risk of progressing to cigarette smoking accumulates (Berry et al., 2019; East et al., 2018; Osibogun et al., 2020; Soneji et al., 2017), questions about youth initiation are acquiring much importance. Our analysis offers a perspective of young e-cigarette users’ profiles in the US, where they are more likely to have never smoked cigarettes. As Figure 1: Panel A shows, the proportion of never-cigarette smokers among young e-cigarette users more than doubled from W1 to W4 (24.1% to 51.4%). This finding contrasts with data from other countries showing limited evidence of e-cigarette initiation among youth never-cigarette smokers (ASH factsheet, 2014). Thus, in the US, e-cigarettes are increasingly attracting adolescents who have never used cigarettes, who are most vulnerable to nicotine’s effect on their developing brain (Barrington-Trimis & Leventhal, 2018; National Academies of Sciences, 2018), and may be subject to the consequences of lifelong nicotine addiction (US Department of Health and Human Services, 2012).
E-cigarette transitions among youth
E-cigarettes’ potential to lead to cigarette smoking is another outcome for judging their unwanted effects as a means of harm reduction, especially in youth (Chapman, 2013; Chapman et al., 2018). Our analysis assessed such potential by looking at the transition of e-cigarette mono-use among youth across the waves. This analysis showed that for every three adolescent e-cigarette mono-users in W1 who reported no past-month use of any tobacco in W2 or W3 or W4, there was one who became a cigarette- or dual-user. This may not provide a firm answer to the debate on whether young e-cigarette users are predisposed to tobacco/nicotine experimentation rather than being at an increased risk of smoking because of their e-cigarette use (Barrington-Trimis et al., 2016; Etter, 2018; Primack et al., 2015). Of particular interest for such debate is the evolution of e-cigarette users who have never tried cigarettes since this can represent e-cigarettes’ potential in the real world to recruit youth to cigarette smoking. Our analysis showed that among adolescents who had never used cigarettes, about one in 4 past-month e-cigarette-only users ended up being past-month cigarette smokers (including dual use), signaling the likelihood of e-cigarettes’ potential to lead to cigarette smoking. However, one may argue that the use of e-cigarettes in youth may be short-lived experimentation in response to a novel product, changes in how e-cigarettes are marketed, and how the product’s evolution may influence its use over time.
Dual-use transitions among adults
E-cigarettes’ potential to aid smoking cessation at the population level has focused mostly on whether dual-use in adults is a transitional stage towards cigarette quitting or an emerging tobacco use pattern (Rahman et al., 2015). By looking at the totality of the dual-use transitions between 2013–2018, our analysis shows that for every two adults aged 18–24 years who reported no past-month use of any tobacco, about five were cigarette users, and one continued with dual use. Among adults aged ≥25 years, for every two who reported no past-month use of any tobacco, about eight were cigarette users, and one continuing with dual-use. While smoking cessation methods used in real-world conditions have varying short- and long-term effectiveness, claims of e-cigarettes’ superiority in such settings is repeatedly made (Benmarhnia et al., 2018; Bullen et al., 2013; Caponnetto et al., 2013; Tseng et al., 2016). Benmarhnia et al.’s analysis of transitions between W1 and W2 in the PATH showed that 5.6% of e-cigarette users at W1 were persistently abstinent from all tobacco products at W2 (Benmarhnia et al., 2018). This is compared to rates of 6.1% for nicotine replacement therapy, 10.2% for varenicline, 10.3% for bupropion and 12.5% for no aid used (Benmarhnia et al., 2018). In contrast, one study of young adult non-daily smokers indicated that more frequent use of ENDS six months before entry into the study predicted more frequent cigarette use over the next year (Doran et al., 2017). Likewise, a more recent study conducted among 3578 previous year smokers from the PATH cohort (2017–2019) found that using e-cigarettes for cessation did not improve successful quitting or relapse in this population (Chen et al., 2022).
Implications
According to e-cigarettes as harm reduction, hardcore smokers who cannot quit otherwise may benefit from switching entirely to e-cigarettes or quitting all tobacco products with the help of e-cigarettes (Abrams et al., 2018). Some well-conducted clinical trials support a beneficial role for e-cigarettes in helping smokers quit in a clinical cessation setting (Hajek et al., 2019; Hartmann-Boyce et al., 2021). However, this potential needs to be balanced with evidence from population and real-world studies showing that, if anything, e-cigarettes can impede cessation and lead to dual-use. Also, because of heavy marketing, false claims of safety, and the use of flavors, e-cigarettes are recruiting many young people who have never used tobacco/nicotine into life-long nicotine addiction (Vogel et al., 2019; Vogel et al., 2018). Based on a unique population-based longitudinal data of tobacco use in the US, our study emphasizes the real-world negative potential of e-cigarettes on young people. Accordingly, while we continue to assess the effectiveness of e-cigarette use for cessation among adult cigarette smokers within clinical settings, population-wide marketing, false safety claims, and the targeting of youth are legitimate targets for regulation and policy to limit the negative aspects of e-cigarette promotion documented already in a plethora of studies in the US and elsewhere (Jenssen & Boykan, 2019; Klein et al., 2016; Sapru et al., 2020).
Limitations
Our study’s main limitation is between waves; changes were made to the PATH study questionnaire. Specifically, we used the expanded definition on questions about using any ENDS from W3. However, this is unlikely to have affected our analysis as we focused on the transitions of e-cigarette users at W1 in subsequent waves. The expanded definition of e-cigarettes in W3 and W4 will not affect our outcomes classification since we started with e-cigarette users at W1. Second, our analysis focused on e-cigarette/cigarette interaction without entertaining OTP combinations in the US (Kasza et al., 2017). This is the primary interaction shaping the discourse about e-cigarettes’ potential to affect cigarette smoking morbidity and mortality (National Academies of Sciences, 2018). Third, past-month e-cigarette/cigarette use may not indicate regular tobacco use, especially among youth, as research shows that youth who used e-cigarettes in the past month are mostly infrequent users (Warner, 2015). However, using any tobacco/nicotine may be detrimental to youth, and it is necessary to see how youth transition with e-cigarettes. Future research should examine transitions to regular tobacco use patterns, which may be crucial to understanding overall transition patterns. Fourth, our analysis did not capture the influence of the rapid-changing e-cigarette marketplace landscape. E-cigarette use may likely have increased in the PATH cohort following data collection for 2016–2018, following the proliferation of newer products such as Juul e-cigarettes. Finally, we considered transitions in past-month use across the four waves, which may not represent prolonged use patterns.
Conclusions
The comprehensive picture from four waves of the PATH study about e-cigarette/cigarette use evolution among youth and adults poses a concern for balancing e-cigarettes’ positive/negative potentials. In young and adult e-cigarette users, we see continued cigarette use, dual-use, and transition to cigarette smoking and potentially spreading nicotine addiction among young never-smokers, rather than quitting among adult smokers. While our assessment does not imply a direct measurement of harm differentials between these e-cigarette transitions, it provides much of what the policy and regulatory debate around e-cigarettes have focused on; their relative scale in a real-world population setting. For e-cigarettes to yield the desired public health gains by serving as alternatives to cigarettes, it should aid quitting rather than encourage the dual-use of e-cigarettes and cigarettes. Also, it should not aid tobacco/nicotine initiation among non-users. For policymakers, appropriate e-cigarette use may be potentially effective in smoking cessation for adult smokers. However, e-cigarette use in adolescents may lead to smoking initiation and regular cigarette smoking (Barrington-Trimis et al., 2016; Osibogun et al., 2020); therefore, the sale of e-cigarettes to minors should be prohibited. The new minimum age of 21 years for purchasing tobacco products may help limit access to e-cigarettes among minors in the US (Liber et al., 2020). Because there is a documented history of targeting vulnerable groups, especially youth and young adults, by the tobacco industry, regulations to restrict e-cigarette use in the general population are warranted. These findings indicate that both prevention and cessation efforts are needed for both youth and adults and that both e-cigarette and cigarette use should be addressed, given the potential for dual use. Targeted communications that emphasize the concerns of youth e-cigarette use and separately the potential benefits of e-cigarettes for adult smokers should be developed by government agencies and health organizations. Accordingly, the imbalance in the scale of potentially positive/negative transitions related to e-cigarettes in the US needs to be considered when planning regulatory actions for e-cigarettes.
Supplementary Material
Funding:
Olatokunbo Osibogun was supported by the NIDA T32DA043449 grant at the time of this study. Zoran Bursac is supported by FIU-Research Center in Minority Institution (grant U54MD012393-01). Wasim Maziak is supported by NIH (grants R01-DA035160, R01-TW010654, R01-DA042477) and the NIDA T32DA043449 grant. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to disclose that are relevat to the content of this article.
Ethics approval: The Florida International University Institutional Review Board deemed this study exempt.
Data Availability:
The data from the Population Assessment of Tobacco and Health Data is publicly available from the Inter-university Consortium for Political and Social Research at https://doi.org/10.3886/ICPSR36498.v11.
References
- Abrams DB, Glasser AM, Pearson JL, Villanti AC, Collins LK, & Niaura RS (2018). Harm Minimization and Tobacco Control: Reframing Societal Views of Nicotine Use to Rapidly Save Lives. Annu Rev Public Health, 39, 193–213. 10.1146/annurev-publhealth-040617-013849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali FRM, Diaz MC, Vallone D, Tynan MA, Cordova J, Seaman EL, Trivers KF, Schillo BA, Talley B, & King BA (2020). E-cigarette Unit Sales, by Product and Flavor Type - United States, 2014–2020. MMWR Morb Mortal Wkly Rep, 69(37), 1313–1318. 10.15585/mmwr.mm6937e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrington-Trimis JL, Berhane K, Unger JB, Cruz TB, Huh J, Leventhal AM, Urman R, Wang K, Howland S, Gilreath TD, Chou CP, Pentz MA, & McConnell R (2015). Psychosocial Factors Associated With Adolescent Electronic Cigarette and Cigarette Use. Pediatrics, 136(2), 308–317. 10.1542/peds.2015-0639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrington-Trimis JL, & Leventhal AM (2018). Adolescents’ Use of “Pod Mod” E-Cigarettes - Urgent Concerns. N Engl J Med, 379(12), 1099–1102. 10.1056/NEJMp1805758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrington-Trimis JL, Urman R, Berhane K, Unger JB, Cruz TB, Pentz MA, Samet JM, Leventhal AM, & McConnell R (2016). E-Cigarettes and Future Cigarette Use. Pediatrics, 138(1). 10.1542/peds.2016-0379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benmarhnia T, Pierce JP, Leas E, White MM, Strong DR, Noble ML, & Trinidad DR (2018). Can e-Cigarettes and Pharmaceutical Aids Increase Smoking Cessation and Reduce Cigarette Consumption? Findings from a Nationally Representative Cohort of American Smokers. Am J Epidemiol. 10.1093/aje/kwy129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry KM, Fetterman JL, Benjamin EJ, Bhatnagar A, Barrington-Trimis JL, Leventhal AM, & Stokes A (2019). Association of Electronic Cigarette Use With Subsequent Initiation of Tobacco Cigarettes in US Youths. JAMA Netw Open, 2(2), e187794. 10.1001/jamanetworkopen.2018.7794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bullen C, Howe C, Laugesen M, McRobbie H, Parag V, Williman J, & Walker N (2013). Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet, 382(9905), 1629–1637. 10.1016/S0140-6736(13)61842-5 [DOI] [PubMed] [Google Scholar]
- Caponnetto P, Campagna D, Cibella F, Morjaria JB, Caruso M, Russo C, & Polosa R (2013). EffiCiency and Safety of an eLectronic cigAreTte (ECLAT) as tobacco cigarettes substitute: a prospective 12-month randomized control design study. PLoS One, 8(6), e66317. 10.1371/journal.pone.0066317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaffee BW, Watkins SL, & Glantz SA (2018). Electronic Cigarette Use and Progression From Experimentation to Established Smoking. Pediatrics, 141(4). 10.1542/peds.2017-3594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman S (2013). Should electronic cigarettes be as freely available as tobacco cigarettes? No. BMJ, 346, f3840. https://www.ncbi.nlm.nih.gov/pubmed/23771038 [DOI] [PubMed] [Google Scholar]
- Chapman S, Bareham D, & Maziak W (2018). The Gateway Effect of e-cigarettes; Reflections on main Criticisms. Nicotine Tob Res. 10.1093/ntr/nty067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R, Pierce JP, Leas EC, Benmarhnia T, Strong DR, White MM, Stone M, Trinidad DR, McMenamin SB, & Messer K (2022). Effectiveness of e-cigarettes as aids for smoking cessation: evidence from the PATH Study cohort, 2017–2019. Tob Control. 10.1136/tobaccocontrol-2021-056901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou SP, Saha TD, Zhang H, Ruan WJ, Huang B, Grant BF, Blanco C, & Compton W (2017). Prevalence, correlates, comorbidity and treatment of electronic nicotine delivery system use in the United States. Drug Alcohol Depend, 178, 296–301. 10.1016/j.drugalcdep.2017.05.026 [DOI] [PubMed] [Google Scholar]
- Coleman B, Rostron B, Johnson SE, Persoskie A, Pearson J, Stanton C, Choi K, Anic G, Goniewicz ML, Cummings KM, Kasza KA, Silveira ML, Delnevo C, Niaura R, Abrams DB, Kimmel HL, Borek N, Compton WM, & Hyland A (2018). Transitions in electronic cigarette use among adults in the Population Assessment of Tobacco and Health (PATH) Study, Waves 1 and 2 (2013–2015). Tob Control. 10.1136/tobaccocontrol-2017-054174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman BN, Rostron B, Johnson SE, Ambrose BK, Pearson J, Stanton CA, Wang B, Delnevo C, Bansal-Travers M, Kimmel HL, Goniewicz ML, Niaura R, Abrams D, Conway KP, Borek N, Compton WM, & Hyland A (2017). Electronic cigarette use among US adults in the Population Assessment of Tobacco and Health (PATH) Study, 2013–2014. Tob Control, 26(e2), e117–e126. 10.1136/tobaccocontrol-2016-053462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai H, Catley D, Richter KP, Goggin K, & Ellerbeck EF (2018). Electronic Cigarettes and Future Marijuana Use: A Longitudinal Study. Pediatrics, 141(5). 10.1542/peds.2017-3787 [DOI] [PubMed] [Google Scholar]
- Delnevo CD, Giovenco DP, Steinberg MB, Villanti AC, Pearson JL, Niaura RS, & Abrams DB (2016). Patterns of Electronic Cigarette Use Among Adults in the United States. Nicotine Tob Res, 18(5), 715–719. 10.1093/ntr/ntv237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doran N, Brikmanis K, Petersen A, Delucchi K, Al-Delaimy WK, Luczak S, Myers M, & Strong D (2017). Does e-cigarette use predict cigarette escalation? A longitudinal study of young adult non-daily smokers. Prev Med, 100, 279–284. 10.1016/j.ypmed.2017.03.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutra LM, & Glantz SA (2014). Electronic cigarettes and conventional cigarette use among U.S. adolescents: a cross-sectional study. JAMA Pediatr, 168(7), 610–617. 10.1001/jamapediatrics.2013.5488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- East K, Hitchman SC, Bakolis I, Williams S, Cheeseman H, Arnott D, & McNeill A (2018). The Association Between Smoking and Electronic Cigarette Use in a Cohort of Young People. J Adolesc Health, 62(5), 539–547. 10.1016/j.jadohealth.2017.11.301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etter JF (2018). Gateway effects and electronic cigarettes. Addiction, 113(10), 1776–1783. 10.1111/add.13924 [DOI] [PubMed] [Google Scholar]
- Gentzke AS, Wang TW, Jamal A, Park-Lee E, Ren CF, Cullen KA, & Neff L (2020). Tobacco Product Use Among Middle and High School Students - United States, 2020. Mmwr-Morbidity and Mortality Weekly Report, 69(50), 1881–1888. <Go to ISI>://WOS:000600946300001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glantz SA, & Bareham DW (2018). E-Cigarettes: Use, Effects on Smoking, Risks, and Policy Implications. Annu Rev Public Health, 39, 215–235. 10.1146/annurev-publhealth-040617-013757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajek P, Etter JF, Benowitz N, Eissenberg T, & McRobbie H (2014). Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit. Addiction, 109(11), 1801–1810. 10.1111/add.12659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, Li J, Parrott S, Sasieni P, Dawkins L, Ross L, Goniewicz M, Wu Q, & McRobbie HJ (2019). A Randomized Trial of E-Cigarettes versus Nicotine-Replacement Therapy. N Engl J Med, 380(7), 629–637. 10.1056/NEJMoa1808779 [DOI] [PubMed] [Google Scholar]
- Hartmann-Boyce J, McRobbie H, Lindson N, Bullen C, Begh R, Theodoulou A, Notley C, Rigotti NA, Turner T, Butler AR, Fanshawe TR, & Hajek P (2021). Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev, 4, CD010216. 10.1002/14651858.CD010216.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland A, Ambrose BK, Conway KP, Borek N, Lambert E, Carusi C, Taylor K, Crosse S, Fong GT, Cummings KM, Abrams D, Pierce JP, Sargent J, Messer K, Bansal-Travers M, Niaura R, Vallone D, Hammond D, Hilmi N, Kwan J, Piesse A, Kalton G, Lohr S, Pharris-Ciurej N, Castleman V, Green VR, Tessman G, Kaufman A, Lawrence C, van Bemmel DM, Kimmel HL, Blount B, Yang L, O’Brien B, Tworek C, Alberding D, Hull LC, Cheng YC, Maklan D, Backinger CL, & Compton WM (2017). Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tob Control, 26(4), 371–378. 10.1136/tobaccocontrol-2016-052934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenssen BP, & Boykan R (2019). Electronic Cigarettes and Youth in the United States: A Call to Action (at the Local, National and Global Levels). Children (Basel), 6(2). 10.3390/children6020030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasza KA, Ambrose BK, Conway KP, Borek N, Taylor K, Goniewicz ML, Cummings KM, Sharma E, Pearson JL, Green VR, Kaufman AR, Bansal-Travers M, Travers MJ, Kwan J, Tworek C, Cheng Y-C, Yang L, Pharris-Ciurej N, van Bemmel DM, Backinger CL, Compton WM, & Hyland AJ (2017). Tobacco-Product Use by Adults and Youths in the United States in 2013 and 2014. New England Journal of Medicine, 376(4), 342–353 %U http://www.nejm.org/doi/310.1056/NEJMsa1607538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein EG, Berman M, Hemmerich N, Carlson C, Htut S, & Slater M (2016). Online E-cigarette Marketing Claims: A Systematic Content and Legal Analysis. Tob Regul Sci, 2(3), 252–262. 10.18001/TRS.2.3.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liber AC, Xue Z, Cahn Z, Drope J, & Stoklosa M (2020). Tobacco 21 adoption decreased sales of cigarette brands purchased by young people: a translation of population health survey data to gain insight into market data for policy analysis. Tob Control. 10.1136/tobaccocontrol-2020-055932 [DOI] [PubMed] [Google Scholar]
- Maziak W (2014). Harm reduction at the crossroads: the case of e-cigarettes. Am J Prev Med, 47(4), 505–507. 10.1016/j.amepre.2014.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMillen RC, Gottlieb MA, Shaefer RM, Winickoff JP, & Klein JD (2015). Trends in Electronic Cigarette Use Among U.S. Adults: Use is Increasing in Both Smokers and Nonsmokers. Nicotine Tob Res, 17(10), 1195–1202. 10.1093/ntr/ntu213 [DOI] [PubMed] [Google Scholar]
- McNeill A, Brose LS, Calder R, Hitchman SC, Hajek P, & McRobbie H (2015). E-cigarettes: an evidence update. A report commissioned by Public Health England. [DOI] [PubMed]
- Mirbolouk M, Charkhchi P, Kianoush S, Uddin SMI, Orimoloye OA, Jaber R, Bhatnagar A, Benjamin EJ, Hall ME, DeFilippis AP, Maziak W, Nasir K, & Blaha MJ (2018). Prevalence and Distribution of E-Cigarette Use Among U.S. Adults: Behavioral Risk Factor Surveillance System, 2016. Annals of Internal Medicine, 169(7), 429 %U http://annals.org/article.aspx?doi=410.7326/M7317-3440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering and Medicine. Public health consequences of e-cigarette. Washington, DC: National Academies Press, 2018. Available at 10.17226/24952. Accessed October 2018. [DOI] [Google Scholar]
- Osibogun O, Bursac Z, & Maziak W (2020). E-Cigarette Use and Regular Cigarette Smoking Among Youth: Population Assessment of Tobacco and Health Study (2013–2016). Am J Prev Med, 58(5), 657–665. 10.1016/j.amepre.2020.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker MA, & Villanti AC (2019). Patterns and Frequency of Current e-Cigarette Use in United States Adults. Subst Use Misuse, 54(12), 2075–2081. 10.1080/10826084.2019.1626433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips E, Wang TW, Husten CG, Corey CG, Apelberg BJ, Jamal A, Homa DM, & King BA (2017). Tobacco Product Use Among Adults - United States, 2015. Mmwr-Morbidity and Mortality Weekly Report, 66(44), 1209–1215. 10.15585/mmwr.mm6644a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack BA, Soneji S, Stoolmiller M, Fine MJ, & Sargent JD (2015). Progression to Traditional Cigarette Smoking After Electronic Cigarette Use Among US Adolescents and Young Adults. JAMA Pediatr, 169(11), 1018–1023. 10.1001/jamapediatrics.2015.1742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman MA, Hann N, Wilson A, Mnatzaganian G, & Worrall-Carter L (2015). E-cigarettes and smoking cessation: evidence from a systematic review and meta-analysis. PLoS One, 10(3), e0122544. 10.1371/journal.pone.0122544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sapru S, Vardhan M, Li Q, Guo Y, Li X, & Saxena D (2020). E-cigarettes use in the United States: reasons for use, perceptions, and effects on health. BMC Public Health, 20(1), 1518. 10.1186/s12889-020-09572-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soneji S, Barrington-Trimis JL, Wills TA, Leventhal AM, Unger JB, Gibson LA, Yang J, Primack BA, Andrews JA, Miech RA, Spindle TR, Dick DM, Eissenberg T, Hornik RC, Dang R, & Sargent JD (2017). Association Between Initial Use of e-Cigarettes and Subsequent Cigarette Smoking Among Adolescents and Young Adults: A Systematic Review and Meta-analysis. JAMA Pediatr, 171(8), 788–797. 10.1001/jamapediatrics.2017.1488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tseng TY, Ostroff JS, Campo A, Gerard M, Kirchner T, Rotrosen J, & Shelley D (2016). A Randomized Trial Comparing the Effect of Nicotine Versus Placebo Electronic Cigarettes on Smoking Reduction Among Young Adult Smokers. Nicotine Tob Res, 18(10), 1937–1943. 10.1093/ntr/ntw017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. National Institutes of Health. National Institute on Drug Abuse, and United States Department of Health and Human Services. Food and Drug Administration. Center for Tobacco Products. Population Assessment of Tobacco and Health (PATH) Study [United States] Public-Use Files. Inter-university Consortium for Political and Social Research; [distributor], 2020-October-21. 10.3886/ICPSR36498.v11 [DOI] [Google Scholar]
- US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. (2016). E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General. Available at https://e-cigarettes.surgeongeneral.gov/documents/2016_sgr_full_report_non-508.pdf. Accessed October 2018
- US Department of Health and Human Services. Preventing tobacco use among youth and young adults: A report of the surgeon general. Atlanta, GA: USDHHS, US centers for disease control and prevention, national center for chronic disease prevention and health promotion, office on smoking and health. 2012 [Google Scholar]
- Action on Smoking and Health (2014). Use of electronic cigarettes in Great Britain. https://www.grea.ch/sites/default/files/e-cig_in_great_britain.pdf. Accessed October 2018
- Verplaetse TL, Moore KE, Pittman BP, Roberts W, Oberleitner LM, Peltier MR, Hacker R, Cosgrove KP, & McKee SA (2018). Intersection of e-cigarette use and gender on transitions in cigarette smoking status: Findings across waves 1 and 2 of the Population Assessment of Tobacco and Health (PATH) study. Nicotine Tob Res. 10.1093/ntr/nty187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarroel MA, Cha AE, & Vahratian A (2020). Electronic Cigarette Use Among U.S. Adults, 2018. NCHS Data Brief(365), 1–8. https://www.ncbi.nlm.nih.gov/pubmed/32487293 [PubMed] [Google Scholar]
- Vogel EA, Prochaska JJ, Ramo DE, Andres J, & Rubinstein ML (2019). Adolescents’ E-Cigarette Use: Increases in Frequency, Dependence, and Nicotine Exposure Over 12 Months. J Adolesc Health, 64(6), 770–775. 10.1016/j.jadohealth.2019.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel EA, Ramo DE, & Rubinstein ML (2018). Prevalence and correlates of adolescents’ e-cigarette use frequency and dependence. Drug Alcohol Depend, 188, 109–112. 10.1016/j.drugalcdep.2018.03.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang TW, Neff LJ, Park-Lee E, Ren C, Cullen KA, & King BA (2020). E-cigarette Use Among Middle and High School Students - United States, 2020. MMWR Morb Mortal Wkly Rep, 69(37), 1310–1312. 10.15585/mmwr.mm6937e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner KE (2015). The remarkable decrease in cigarette smoking by American youth: Further evidence. Prev Med Rep, 2, 259–261. 10.1016/j.pmedr.2015.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner KE, & Mendez D (2018). E-cigarettes: Comparing the Possible Risks of Increasing Smoking Initiation with the Potential Benefits of Increasing Smoking Cessation. Nicotine Tob Res. 10.1093/ntr/nty062 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data from the Population Assessment of Tobacco and Health Data is publicly available from the Inter-university Consortium for Political and Social Research at https://doi.org/10.3886/ICPSR36498.v11.


