Summary
Background
Health policy can be defined as an agreement and consensus on a health-related program and set of actions taken to achieve the goals expected by programs in the area of policy. Policy analysis involves a wide range of methods, techniques, and tools in a way to reach awareness of the impacts of the developed and implemented policies. Whereas policy analysis in developed countries has a long history, in developing countries, it is instead in its first developing stages. Our paper aimed to collect systematically the studies using health policy triangle framework in doing analysis in one of the health policy issues in the Eastern Mediterranean region organization.
Methods
To conduct our literature search, ISI/Web of Science, PubMed/MEDLINE, Embase, The Cochrane Library, Global Health Database, Scopus, as well as Google Scholar from 2003 up to June 2020 were systematically mined. To evaluate the methodological quality of the included studies, the Critical Appraisal Skills Program checklist was used.
Results
We selected 30 studies, conducted between 2011 and 2020. According to the findings of these studies, in the Eastern Mediterranean region, organization region, and the role of evidence-based research in policy-making has been repeatedly emphasized, but its use in health program decision-making has been limited, and health research systems in Eastern Mediterranean region organization are still under scrutiny. There is still a gap between evidence-based research in health systems and its use in policy-making.
Discussion
Based on the present systematic review, studies based on policy analysis should focus on all the elements of health policies and provide evidence to inform decisions that can strengthen health systems, improve health and improve existing inequalities.
Keywords: Health policy, Health policy triangle framework, Decision making
Background
Strengthening health systems with the aim of achieving sustainable development goals and universal health coverage requires evidence-based policy interventions [1].
Each component of the policy process plays its proper part within the health system and the country in which is implemented as a whole [2, 3]. The process of developing health policies is complex, and many actors in this field, such as government agencies, stakeholders, political parties, the mass media, researchers, and other governments, are pursuing goals in this area. They are self-sufficient and are influential in this process based on their position, goals, and impact on politics [4].
Due to the distinctive characteristics of the health system with respect to other sectors of the society, dealing with human lives, making policies to avoid unwanted effects has a special place [5]. Policy making concerning human and financial resources to deliver health care services in due time increases the importance of decisions made in this sector [1].
The World Health Organization (WHO) defines health policy as an agreement and consensus on a health-related program and set of actions taken to achieve the goals expected by programs in the area of policy [6]. Policy analysis involves a wide range of methods, techniques, and tools in a way to reach awareness of the impacts of the developed and implemented policies.
Health policy examines the laws that directly or indirectly affect health and its various aspects. Health policy can be performed through the public and private sectors [7]. The scope of health policy is broad and varied, and is likely to be gradual, fragmented, and incomplete. The health policy process evaluates and analyzes the best opportunity to identify appropriate strategies for the health sector [8].
How a policy is achieved, how it is designed, who is affected by the policy (including proponents and opponents), and what the consequences will be is the main questions that policy analysis tries to answer. The subject of policy analysis and how to carry it out is intensively discussed in many scientific and academic circles [9]. Policy analysis is a multidisciplinary process that seeks to examine the interaction between organs, ideas, and its benefits in a political process [10].
In policy analysis, researchers seek a proper understanding of the policy process and intend to examine its nature. This can provide a better understanding of the health policy process as well as very credible evidence for the problems and issues that arise in the field of health and for future decisions that need to be made [11].
To conduct a policy analysis, various theories and models are generally used [10]. Policy analysis in developed countries has a long history [12]. In developing countries, it is instead in its first developing stages [13]. The use of policy analysis models, theories, or frameworks is very important for policymakers, and they should use these analyzes to make more accurate and useful decisions [14]. In recent decades, the tendency to use theories and models of policy analysis in the health sector has increased, and many studies have been done in this regard [12].
HEALTH POLICY TRIANGLE FRAMEWORK
In 1994, Walt and Gilson introduced a framework for health policy analysis. This framework has four main domains, including context, content, process, and actors. This framework can be used as a retrospective or prospective approach to policy analysis, and a comprehensive understanding of decision-making, planning, and policy implementation can be achieved [9]. This framework allows health researchers to examine the impact of political, social, cultural, economic, and international factors. It also discusses the process in which the policy in question is formulated, then designed, implemented, and evaluated by the policymaker, and analyzes the role of different actors in relation to the policy (Fig. 1).
Fig. 1.
Health policy triangle framework.
In many countries with diverse health systems, this framework has been used to examine health-related policies and their impact on their community [9]. This framework can be used retrospectively or prospectively [15]. In addition to developed countries, the use of this framework has increased in recent years in developing countries [13]. Examining and summarizing the application of this framework in health-related policies can strengthen and implement more appropriate policies for countries [5]. The use of this framework can also provide a valuable platform for more comprehensive policy analysis [12]. Our paper aimed to collect systematically the studies using Health policy triangle framework in doing analysis in one of the health policy issues. In particular, the focus of our study is on health policy analysis studies in the Eastern Mediterranean region organization (EMRO). EMRO is one of the six regions of the WHO, having 21 members: namely, Afghanistan, Bahrain, Djibouti, Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Libya, Morocco, Palestine (West Bank and Gaza Strip), Oman, Pakistan, Qatar, Saudi Arabia, Somalia, Sudan, Syria, Tunisia, United Arab Emirates (UAE), and Yemen [16].
Methods
LITERATURE SEARCH
To conduct our literature search, ISI/Web of Science, PubMed/MEDLINE, Embase, The Cochrane Library, Global Health Database, Scopus, as well as Google Scholar from 2003 up to June 2020 were systematically mined. Also, to increase the chance of finding relevant studies, reference lists of the studies included were assessed. Specific keywords were employed using Boolean operators (AND, OR, NOT). First, a preliminary search was performed using MeSH on the PubMed/MEDLINE database, and the keywords were identified after familiarization with the literature. The following search strategy was used:
(“Policy “OR “Policy analysis” OR “Health policy” OR “Public policy” OR ”Policy process” OR Health politics” OR “Document analysis” OR” Agenda setting” OR” ”Stakeholder analysis OR “Framework” AND” Walt AND Gilson framework” OR “Health Policy Triangle Framework” OR “Policy triangle framework” OR “Walt AND Gilson’s framework”) AND (“Afghanistan “OR “Bahrain “OR “Djibouti “OR “Egypt “OR “Iran” OR “Iraq “OR “Jordan “OR “Kuwait “OR “Lebanon “OR “Libya “OR “Morocco “OR “Oman “OR “Pakistan “OR “Qatar “OR “Saudi Arabia “OR “Somalia “OR “Sudan “OR “Syrian” OR “Tunisia “OR “Emirates “OR “Yemen “OR “Eastern Mediterranean Region Organization “OR “EMRO ““OR “Middle East “ OR “developing countries”) NOT (“America” OR “USA” OR “Australia” OR “Canada” OR “UK” OR “Europe”). The search of the databases was carried out by two researchers independently. Any differences between them were resolved through discussion.
INCLUSION CRITERIA
Studies conducted in the EMRO region.
Studies that used the health policy triangle framework to analyze policy.
Studies published in English.
Studies published in journals with the peer-review system.
Studies published between 2003 up to June 2020.
Articles whose working method was acceptable.
Articles whose full text was available.
EXCLUSION CRITERIA
Studies published in Non-EMRO countries.
Studies published in Non-English language.
Studies the findings of which were not sufficient for analysis.
Theses and chapters of books.
QUALITY ASSESSMENT OF INCLUDED STUDIES
To evaluate the methodological quality of the included studies, the Critical Appraisal Skills Program (CASP) checklist was used. This checklist contains ten questions. There are three answers (Yes, No, and Unclear) to each question. For the answer Yes, score 1 and for the answer No, score 0 were considered. Based on the scores obtained, the studies were divided into three categories: good, moderate, and weak quality (1-3: poor, 4-7: moderate and 8-10: good).
DATA EXTRACTION
Two researchers independently extracted selected study data. In case of disagreement between them, one person acted as the arbitrator, and the dispute was resolved via discussion. Name of the first author, the year of publication, the country, the title of the topic of the policy, and the most important findings related to the items of the framework were extracted.
DATA ANALYSIS
Data were analyzed using deductive content analysis guided by policy triangle framework components (namely, content, context, processes, and actors). In qualitative research, deductive content analysis is similar to inductive content analysis. Deductive content analysis is applied usually has prior theoretical knowledge as the starting point and guided by a half-structured or structured analysis matrix.
Results
This study adhered to the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” (PRISMA) guidelines.
863 articles were found in the initial search. 172 articles were duplicated and, as such, were removed. The titles of 691 articles were reviewed. 572 were removed, being unrelated studies. 30 studies were finally selected based on the study criteria. Figure 2 shows the process of searching and selecting studies [17-46].
Fig. 2.
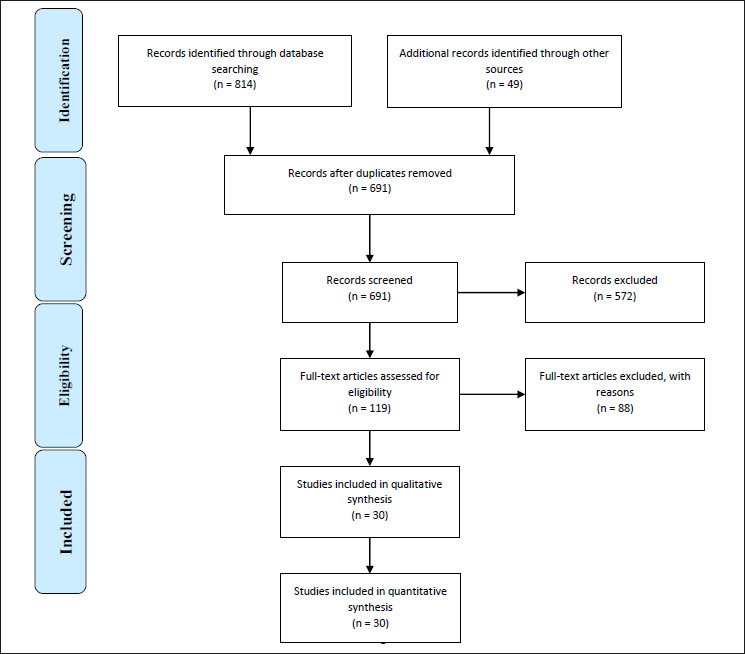
Flow-chart showing the process of study retrieval, selection and inclusion adopted in the present systematic review.
Selected studies were conducted between 2011 and 2020. Studies were conducted in Iran (16), Pakistan (4 studies), Saudi Arabia (2 studies), Lebanon (2 studies), Sudan (2 studies), Tunisia (2 studies), Egypt (1 study), Afghanistan (1 study), Syria (1 study) and Palestine (1 study). One study was conducted in four countries (Tunisia, Syria, Palestine, and Turkey). Figure 3 shows the studies according to the EMRO countries in which they have been performed.
Fig. 3.
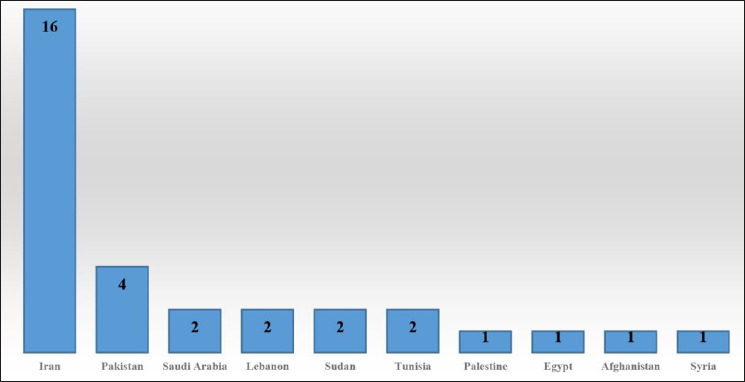
Studies included broken down according to the EMRO countries in which they have been performed.
THE METHODOLOGICAL QUALITY OF THE SELECTED STUDIES
Table I and Figure 4 show the quality of studies broken down according to the previously mentioned classification (good, moderate, and poor quality). Based on the scores obtained, 20 had good quality, 9 had moderate quality, and 1 had poor quality.
Tab. I.
Quality appraisal of the studies included in the present systematic review.
| The first author (References) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | The score of the quality | Categories |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beesley (14) | 1 | 1 | 1 | 1 | 1 | NA | 1 | 1 | 1 | 1 | 9 | Good |
| Zaidi (15) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | Good |
| Phillimore (16) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | Good |
| Seef (17) | NA | NA | NA | NA | 1 | NA | NA | 1 | 1 | 1 | 4 | Moderate |
| Zaidi (18) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | Good |
| El-Jardali (19) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | Good |
| El-Jardali (20) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | Good |
| Markazi-Moghaddam (21) | NA | 1 | NA | 1 | 1 | NA | 1 | 1 | 1 | 1 | 7 | Moderate |
| Speakman (22) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | Good |
| Awadalla (23) | 1 | NA | 0 | 0 | 1 | 1 | 1 | 0 | NA | 1 | 5 | Moderate |
| Ben Romdhane (24) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | Good |
| Faraji (25) | 1 | 1 | NA | NA | 1 | NA | 1 | 1 | NA | 1 | 6 | Moderate |
| Alharbi (26) | NA | 0 | 1 | 1 | NA | 1 | 1 | 1 | 1 | NA | 6 | Moderate |
| Goshtaei (27) | NA | 1 | 0 | 0 | 1 | 1 | 1 | NA | 1 | 1 | 6 | Moderate |
| Moshiri (28) | NA | 0 | 1 | 1 | NA | 1 | 1 | 1 | 1 | 1 | 7 | Moderate |
| Sarfraz (29) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | Good |
| Abolhassani (30) | 1 | 1 | 1 | NA | 1 | NA | 1 | 1 | 1 | 1 | 8 | Good |
| Aljumah (31) | 1 | NA | 0 | 1 | NA | 1 | 1 | NA | NA | 1 | 5 | Moderate |
| Azami-Aghdash (32) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | Good |
| Haq (33) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | Good |
| Yousefinezhad (34) | 1 | 1 | 1 | NA | 1 | 1 | 1 | 1 | 1 | 1 | 9 | Good |
| Ansari (35) | 1 | 1 | 1 | NA | 1 | NA | 1 | 1 | 1 | 1 | 8 | Good |
| Al-Ansari (36) | 1 | 0 | NA | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 6 | Moderate |
| Edalati (37) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | Good |
| Gharaee (38) | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 | Good |
| Loloei (39) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | Good |
| Mohseni (40) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | Good |
| Behzadifar (41) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | Good |
| Doshmangir (42) | 1 | 1 | NA | NA | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Good |
| Raoofi (43) | 1 | NA | NA | NA | NA | 1 | NA | 0 | 0 | 1 | 3 | Week |
Fig. 4.
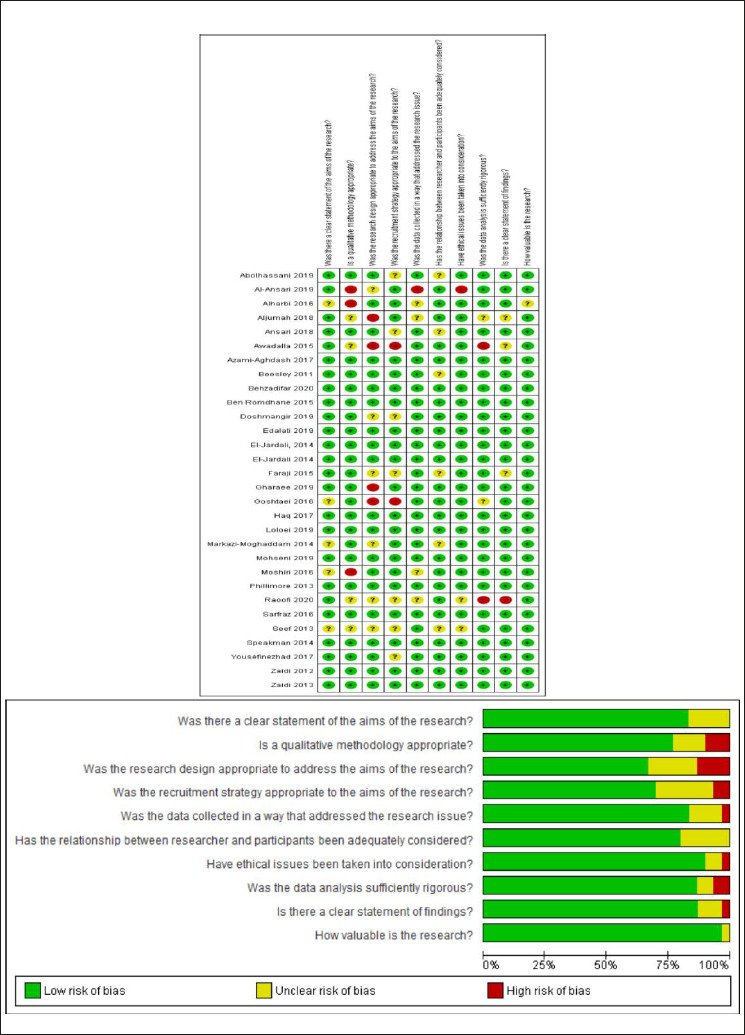
Quality assessment of the studies included in the present systematic review.
The main characteristics and findings of the selected studies are shown in Table II.
Tab. II.
Characteristics of included studies.
| First author | Year of publication | Country | Subject analyzed (title of policy) | Retrospectively or prospective | Data collection | Main finding | |||
|---|---|---|---|---|---|---|---|---|---|
| Context | Content | Process | Actors | ||||||
| Beesley (14) | 2011 | Sudan | The disrupted health sector | Retrospective | This study has been obtained by comparing and searching for documents in reputable databases and comparing them not enough information has been provided in this regard | One of the ways to help restore the functioning of the disrupted health sector is the effective and extensive participation of the international community in the form of providing technical assistance to the Ministry of Health to complete any shortcomings in specialization or experience. Creating a new health management by outsiders is also an opportunity to correct problems and introduce innovations. An example of international technical support in 2007 was the provision of technical assistance to the Sudanese Ministry of Health in the form of a manpower program | With the signing of the Comprehensive Peace Agreement in Sudan, the analysis of the situation and development plans of the health system and an improvement strategy were developed and designed and drafted by the new health officials. The World Health Organization (WHO) has launched a USAID-funded bilateral to provide full-fledged technical services to improve health care, especially in the area of human resources. The Youssid-funded capacity project to provide technical, managerial and financial support for the development and management of human resources and labor, as well as the African Medical and Research Foundation (AMREF), is the only clinical officer training school (with a track record in human resources in southern Sudan and other countries) Who were involved in developing human resource programs | Between 2005 and 2006, World Health Organization advisers supported the Sudanese Ministry of Health in conducting human resource assessments to provide the basis for a human resource development program for the Reconstruction Workforce Reconstruction Process for a Human Resource Development Program, a working group chaired by the Director of Human Resources of the Ministry of Health prepared the reference conditions for a comprehensive assessment. A multi-agency team, including three consultants, 10 data collectors and an IT specialist, coordinated with the Ministry of Health, as well as the main human resources organizations in the field of health and treatment, reviewed and collected the human resources inventory after completion. No further discussion took place after the data collection phase and after the delivery and internal rotation of the situation analysis and draft recommendations. The recommendations, the main focus of which is the proposed Human Resources Strategic Plan, were published in 2006 by the Ministry of Health | The Ministry of Health
The World Health Organization (WHO) The African Medical and Research Foundation (AMREF) Not enough information has been provided in this regard |
| Zaidi (15) | 2012 | Pakistan | NGO–government contracting for health service delivery | Retrospective | Case study data (conducted by NGOs to prevent human immunodeficiency virus HIV) using in-depth interviews, semi-structured interviews, document review and direct observation and review of national policy plans, provincial contract management, and local contract implementation | Contracts outside of preventive health services and primary health care (PHC) by providing international assistance in a number of developing countries, such as Cambodia, Guatemala, Senegal, Costa Rica, Nicaragua, Afghanistan, Pakistan, Bangladesh and India, tend to be handed over to organizations. Non-governmental organizations have contracts (non-governmental organizations) that are more important in order to provide health care services in low-income and middle-income countries.
The term non-governmental organization usually includes the non-profit sector, which aims to give these institutions better access to the deprived population and more responsiveness |
The contract for the AIDS control program, which relied on NGOs, had four distinct features: first, contracting on a large scale, including large contracts and several bidding periods, and second, emphasizing performance-based contracts and health-related goals. The general was low cost. Third, the strength of the market to attract potential contenders for the AIDS program. Although inexperienced, the public sector played a key role in managing the contracting process. The program coordinated new and energetic leadership to prevent HIV | Even after its implementation, activities were limited and lacked strategic direction. But in the early 2000s, services began to follow the international pursuit of HIV / AIDS prevention and the frustration of international donors with Pakistan’s efforts to control the search for new and daring ways to search for disease, and the government lobby was conducted with international donors at the Ministry of Finance level. This led to extensive contracting initiatives with donor budgets and an increase in the national budget allocation for HIV control from $ 2.5 million to nearly $ 10 million. It also envisages the development of a comprehensive service package (including public health measures as well as client empowerment and rehabilitative measures) in contracts that were necessary at the international level to attract HIV interventions | The Ministry of Health (MoH)
The Ministry of Finance The World Bank UK Department for International Development (DFID) United States Agency for International Development (USAID) European Commission (EC) Canadian International Development Agency (CIDA) |
| Phillimore (16) | 2013 | Tunisia, Turkey, Palestine (oPt ), and Syria | Health system challenges of cardiovascular disease and diabetes | Retrospective | Data collection of the qualitative study was done in three ways: Analysis of published and unpublished official documents on the details of the health care system of all 4 countries (Tunisia, Turkey oPt, and Syria) focusing on cardiovascular disease and diabetes, semi-structured interviews with key informants at the national and regional level in the management of these diseases have major responsibilities in the health system of countries, case studies based on fieldwork including interviews with staff, patients and care professionals as well as clinical performance observations, as well as primary and secondary level facilities and equipment And some diabetes clinics | Increasing the prevalence of diseases such as CVD and diabetes and increasing the cost of managing these diseases requires the development of new techniques for managing diseases through which patients and their care costs can be monitored and monitored.
If costs are not managed and monitored, the health care system will become “ illegible.” In Palestine: One of the problems of fragmentation of the health system, which is due to three reasons: the multiplicity of providers, the different goals and priorities of donor organizations, and the problems caused by the political separation of the West Bank and Gaza,and the Palestinian health care system relies on funding from a variety of sources, with out-of-pocket payments accounting for the largest share of the budget. In Syria, because the government’s budget for health care is unsustainable and limited, especially due to the high long-term costs of patients with NCD. In Tunisia, the health care system is budget-based and tax-based, and health care monitoring is poor. Social insurance covers a large portion of the population (more than 80%). In the private sector, the Ministry of Health’s medical guidelines for patients with non-communicable diseases are rarely followed. Expenses are out of pocket. The introduction of the family physician system (in 2006) marked a change in the system. However, prevention and treatment services in the new system have not been integrated, and there is no proper referral system, especially for infectious diseases. |
In Palestine, managing non-communicable diseases, which put the most pressure on the health system, is one of the four strategic goals of the Palestinian Ministry of National Health and other health care providers, and there are screening, diagnosis and treatment protocols for diabetes | In Palestine, the management of non-communicable diseases, which put the most pressure on the health system, is one of the four strategic goals of the Palestinian Ministry of National Health and other health care providers, and there are screening, diagnosis and treatment protocols for diabetes
In Palestine, the health system for policy making and implementation of programs in the field of these two diseases with problems such as lack of cohesion of the health system, reliance of the system on foreign donors, lack of stable information systems and lack of access to patient data and non-sharing of this information. There are differences between different parts of the health system and the lack of retention of employees, especially doctors. In this country, despite spending 64% of expenditure on health on health care, only 7% of it is spent on the prevention of public services. Although these two diseases are one of the main challenges in Syria, there is a lack of coordination and planning in different parts of the health care system. There was no systematic follow-up of weak patients to refer patients from primary to secondary care. There is no system for recording patient records, especially in rural and rural areas, and there has also been a severe shortage of skilled staff in the health system, especially outside major cities. In Tunisia, there are four frameworks and structures for NCD management, but there are no coordination, monitoring, and implementation mechanisms, and fragmentation of the system prevents coherent management of the disease. Strategic partnerships have not been strengthened, and policymakers are reluctant to see the disease as part of an economic and social development strategy, and the focus of participation is on health care, not prevention, and so inter-sectoral and conscious participation is weak. There was coordination and integration in the Turkish health system, and the structure (The new Family Health Center framework) was formed, which was inconsistent. Moreover, the Health Transformation Programme (HTP) reforms play an important role in primary care (for prevention, diagnosis and treatment) . However, the diagnosis and monitoring of non-communicable diseases has been neglected and poor, and there is no proper referral system. |
In oPt:
The Palestinian MoH The United Nations Relief and Works Agency (UNRWA) A Non-Governmental Organisation (NGO) small private sector In Syria: the government and private sectors the MoH The Ministries of Defense, Interior and Education The private sector, Private clinics, private hospitals Syria’s pharmaceutical industry In Tunisia: the MoH private sector private polyclinics In Turkey: The Ministry of Health expanding private health care sector, private hospitals The Social Security Institution (SSI), the pharmaceutical sector, professional associations and, increasingly, the media |
| Seef (17) | 2013 | Egypt | The H1N1 flu pandemic control | Retrospective | Data from the study, which looked at Egypt’s health policies to control the epidemic, were reviewed from policy documents and literature review | The 2009 flu pandemic spread internationally. The new flu virus, known as the swine flu outbreak, killed hundreds of thousands of pigs while controlling the disease (despite recommendations from health officials). This was unnecessary because the disease does not occur through contact with pigs or eating meat | H1N1 has spread around the world in a matter of weeks, infecting millions and killing more than 4,735 people. With the increasing prevalence and spread of it, the Egyptian government considered the issue as an important political issue to put the necessary measures on its agenda. The epidemic of the epidemic was a political crisis. As a new influenza virus became known as the “swine flu”, the Egyptian government set out to deal with its source and kill pigs | On March 4, 2009, the Egyptian parliament debated a law banning the breeding of pigs and their products, and lawmakers approved a request to kill all pigs in the country. The Minister of Health presented a plan to address the flu pandemic and proposed a plan for all relevant ministries, including the Ministries of Education, Transport, Environment and Agriculture. In 2009, Egypt began slaughtering about 300,000 pigs in the country. Policies were implemented through a top-down approach, with well-defined goals, the necessary political, administrative, technical, and financial resources available, the command chain established from the center to the fringes, and a system of communication and control. . But pig farmers, who were predominantly Christian, protested vehemently. International health officials say the swine flu virus, which has caused global fear, is not being transmitted by pigs and must be stopped. The World Health Organization also criticized the Egyptian government’s decision | The Ministry of Health (MoH)
The parliament No details were given about the actors |
| Zaidi (18) | 2013 | Pakistan | Nutrition Policy | Retrospective | Qualitative research data were obtained through in-depth interviews and focal group discussions with government stakeholders, donor agencies, civil society organizations (CSOs) and nutritionists, along with review of published and gray literature documents | Malnutrition in Pakistan is high and malnutrition is a chronic problem, and the most at-risk groups include pregnant and lactating women and children under the age of five. Moreover, there is no proper nutrition strategy | Interventions and policies included the establishment of Baby-Friendly Hospitals to manage malnutrition to promote newborn breastfeeding, the establishment of places in medical centers for nutrition counseling, the distribution of iron supplements and folic acid to pregnant women, and vitamin A to children. Food fortification was implemented with training and providing equipment and goods for food processing in the private sector. Pilots of targeted nutrition projects for girls’ schools (ages 6-11 years) were implemented in deprived rural areas in all provinces. The projects were funded by UN agencies, the World Food Program and international NGOs. | 770/5000
In 2008, the Food Safety Working Group and the Ministry of Food Safety were formed in Pakistan. Around the same time, a draft of Pakistan’s federal-style integrated nutrition strategy was formed with UNICEF’s support for the global Scaling Up Nutrition (SUN) movement. The release of the National Nutrition Survey NNS in early 2012, along with media advertising, raised the issue of support for researchers, the media and development partners, raising the issue of malnutrition. The provincial transfer in 2011 provided development partners with easier implementation and direct partnership with executives, and nutrition and related issues became a new public policy program led by development partners |
The Ministry of Health (MoH)
The UN agencies The World Food Program and international NGOs The Provincial Education Departments |
| El-Jardali (19) | 2014 | Lebanon | The voluntary health insurance system | Retrospective | Data collection was conducted by comprehensive and chronological media review, interviews with policymakers, stakeholders and key journalists, and review of legal documents, minutes, statistical studies, and official documents. | Out-of-pocket expenditures are very high in Lebanon (56.5%). Analysis of insurance policy Voluntarily examines how and why this policy is implemented. Public policy is a complex process. The typology of public policy consists of three aspects: distributive, regulatory and redistributive.
Distribution policies provide specific benefits or services to specific segments of the population regardless of limited resources. Regulatory policies include a direct choice as to who will be exaggerated and who will be deprived. Meanwhile, redistribution policies include large groups of citizens who benefit from or receive losses. In fact, NSSF Voluntary Insurance is a distributed policy typology. |
11 The Social insurance Law on the Establishment of the voluntary insurance branch was issued by the Council of Ministers The decree was implemented by the President of the Republic on the basis of the recommendations of the NSSF board of Directors of the Minister of Labor, consultation with the Advisory Council and the approval of the Council of Ministers. | the voluntary health insurance
policy in Lebanon was adopted by the government and adopted as a political decision to address an immediate problem, and scientific, statistical and financial evidence was not used to develop policy and implement the policy.Moreover, policy makers and other stakeholders were not involved in policy making. |
Although the Lebanese political system is democratic, the government insisted that the policy be adopted without the participation of the Ministry of Finance and the NSSF, which was not a participatory and transparent decision-making processbecause stakeholders and civil society did not participate in political discussions and decisions. |
| El-Jardali (٢٠) | 2014 | Lebanon | Nursing practice Law | Retrospective | Qualitative research data were collected using informant interviews with key stakeholders as well as a roundtable to validate the findings, identify any gaps, and obtain insights and feedback on the panels. | Lebanese nursing practice law was drafted to modernize an existing 40-year law
This draft law was made with the aim of organizing and promoting the nursing profession by upgrading and standardizing the conditions for entering the nursing profession and changing the level of nursing. |
The draft nursing practice law should be able to provide the changes required by educational programs to be promoted from a higher professional degree (TS) to a university degree (BS). | In order for this policy to be successful, there must be obstacles to implementation at the program development stage
The draft law on nursing practice was difficult to draft due to the lack of clarity in solving the problem and the lack of implementation barriers. |
The main sponsors of the Nursing Act were the Ministry of Health and the Ministry of Education. All actors agree on the need to improve nursing in Lebanon. There are many differences in how to do this. |
| Markazi-Moghaddam (21) | 2014 | Iran | Establishment of Autonomous Hospitals and the Barriers | Retrospective | In the present qualitative study, the data were obtained in two stages. In the first stage, a questionnaire with open questions was sent to all medical universities and all 54 university hospitals that were granted independence in Iran. Then, a semi-structured interview of the key respondents of the first stage was conducted and analyzed. | In some developing countries, as well as in Iran, the Ministry of Health has started the liberalization and decentralization of the public sector
In fact, autonomous hospitals are likely to be run by the university rather than their own policies and programs within the hospitals themselves. |
In 2003, when the government allowed eighty percent of government assets to be privatized or decentralized under Article 44 of the Iranian constitution, the Ministry of Health aimed to speed up service delivery, increase patient satisfaction with services across hospitals, increase productivity, and improve continuous quality. Gradually, in 2006, he moved to self-governing public university hospitals. | To implement this program, MOHME is open to all medical universities (they operate on behalf of the Ministry of Health in each province and are responsible for providing health care, university education in medical sciences, and overseeing public and private health care organizations). He ordered that at least one public hospital be declared
Therefore, 18 hospitals were finally selected and independent, but the Ministry of Health and insurance organizations did not pay for the reforms. The steps of formulating and implementing the policy were carried out separately in Iran, and therefore the major organizational reforms faced serious obstacles in the implementation and were not successful. |
The Ministry of Health (MoH)
The medical universities The insurance organization The Hospitals |
| Speakman (22) | 2014 | Afghanistan | Midwifery Education initiative
and its influence on women’s health and empowerment |
Retrospective | Qualitative data collection was performed by reviewing documents published in reputable databases and interviews with knowledgeable key individuals. Documents related to policies, institutional reports, guidelines, and media articles were obtained by searching databases and websites. | Following the political transition in Afghanistan, which paved the way for the reconstruction and improvement of the destroyed health system, maternal health became a priority due to the high mortality rate. The Community Midwifery Education Program (CME) began teaching rural midwives in 2002 and expanded nationally in 2005. | The Community Midwifery Education (CME) programme, which was initially launched as a pilot project for non-governmental organizations but became an internationally recognized program
It is currently used as a model for other countries (eg Pakistan, Ethiopia, Laos). In the CME program, the two indicators used in Afghanistan were the maternal mortality ratio (MMR) index and the number of the skilled birth attendant (SBA) that were developed to achieve the Millennium Development Goals (MDGs), which was predicted (from 2002 to 2015) to reduce MMR by 50% and in line with the goal. Second, increase the SBA from 6 percent to 50 percent. CME improves maternal care and provides an example of women’s empowerment. And it has had a wider social impact than expected. |
The Community Midwifery Education (CME) began in 2002 with rural midwifery training and continued until 2015. It expanded nationally in 2005. In the same year, the Afghan Midwives Association (AMA) was established as a professional association for midwives..HealthNet-TPO (HNTPO) presented a program with the budget of the Dutch government to complete the shortcomings of the Afghan government and inject financial resources. The CME pilot began with a Dutch government budget and Jhpiego technical support to develop a curriculum for target groups. Moreover, it improved the indicators and eventually became a well-known international program. | Afghan Ministry of Health officials
NGOs, Ministry of Public Health, Ministry of Women’s Affairs, inter-national donors (World Bank, European Commission, USAID), UN agencies Unicef, UNFPA, WHO), implementing NGOs (HealthNet-TPO, Jhpiego), and civil society organisations (AMA). Dutch INGO HealthNet-TPO (HNTPO) and other partners in the health sector. |
| Awadalla (23) | 2015 | Sudanese | Quality assurance program | Retrospective | The study was a review of documents about Sudan. Study data were conducted by searching valid sources and databases. | The use of quality improvement programs (QAP) in healthcare systems is essential
Sudan launched its National Quality Assurance Program in 2001 in the health sector. However, the obstacles facing the program have led to poor performance and inefficiency. |
The program began vertically from top to bottom, but there was no structural system for regular reporting and monitoring in Sudanese state hospitals. | There was no redistribution of financial and technical resources from the federal level to the states
Adequate information on how the program was implemented was not provided to states and hospitals, and communication between different levels was not effective. |
Physicians are influenced by both their professional power and their managerial role in implementing the program. |
| Ben Romdhane (24) | 2014 | Tunisia | Health system challenges of NCDs | Retrospective | The present qualitative study data were obtained through the analysis of official documents of hypertension, diabetes and obesity and tobacco programs, and case studies of fieldwork conducted in four clinics and semi-structured interviews with key individuals. | The challenges of the health system in non-communicable diseases in Tanzania and its analysis are highly dependent on routine social and demographic indicators, and research in this area has been in its early stages.
And this gap must be filled through policy analysis and solutions |
Integration of care program of four major groups of non-communicable diseases in primary health care, development of health care through the private sector | There was no capacity in the Tunisian Ministry of Health for an integration strategy, nor was there a platform for private sector intervention in the management of communicable diseases. | The WHO
The Ministry of Health(MoH) The emerging private sector The private polyclinics National legislators, regional councils, researchers, the pharmaceutical industry, Capitalists and the mass media |
| Faraji (25) | 2015 | Iran | Control of Diabetes | Retrospective | Searching for information sources on policies and programs for the prevention and control of diabetes in Iran since 1989 (the first program of the World Health Organization in the field of prevention and control of diabetes) were done in reputable databases | Due to the increasing prevalence of diabetes in Iran (trend analysis from 2005 to 2011) and also the possibility of increasing its prevalence in the future, it is necessary to analyze policies and programs related to the prevention and control of diabetes. | In line with the Global Diabetes Program in 1989, the National Diabetes Prevention and Control Program was piloted at 17 Iranian University of Medical Sciences for people over 30 and pregnant women between 1999 and 2001. | The Ministry of Health of Iran (MoHME), in coordination with the National Diabetes Committee (established in 1996), presented the National Diabetes Program and Patient Training Patterns to the general public with the aim of preventing and controlling diabetes. | internal stakeholders included
the national diabetes committee members, the representatives of the medical universities; Department of Endocrinology and Metabolic of Center for Non-communicable Disease Control, Center for Network Development and Health Promotion, Bureau of Population & Family Health, and Office of Community Nutrition Improvement of Ministry of Health and Medical, Office of hospital administration and Clinical Service Excellence, Endocrinology & Metabolism Research Institute of Tehran University of Medical Sciences, the chancellors and vice-chancellors of the medical universities, Iranian Society of Nephrology, the financial director of treatment deputy, the general manager of Center for Non-communicable Disease Control and the program experts at the medical universities internal stakeholders participated in the development of the diabetes program, and the main stakeholders outside the field of healthcare did not participate in the development of the program. |
| Alharbi (26) | 2016 | Saudi Arabia | Diabetes | Retrospective | Articles on diabetes and healthcare policy were searched by PubMed and Medline Database to find research sources. The sources were manually screened by the authors before entering the study. | Rapid economic development and urbanization” in Saudi Arabia, along with behavioral changes, has led to a change in lifestyle, followed by a decrease in physical activity, increased consumption of refined carbohydrates and increased obesity, as well as non-communicable diseases such as diabetes. | Saudi Arabia’s Ministry of Health has approved a ten-year national executive plan and sought to implement targeted health care methods in all areas of health care.
It is also designed to prevent, treat and rehabilitate patients and has created a network of integrated facilities with the aim of providing appropriate health standards for 20 specialized centers for the treatment of diabetics. |
In Saudi Arabia’s public health system, diabetes-related services are mainly provided by providing primary health care services in diabetes centers after initial screening. The role of the Diabetes Center is to manage care. | In Saudi Arabia, the Ministry of Health is responsible for health care, monitoring and planning policies and responsibility for health promotion, early diagnosis and treatment of the disease.
several governmental bodies, including the Ministry of Defense and Aviation (the second-largest health services provider), the Ministry of the Interior and the National Guards, also provide health care |
| Goshtaei (27) | 2016 | Iran | Nutrition policy process challenges | Retrospective | The qualitative data of the present study were obtained through semi-structured interviews with 59 policymakers, knowledgeable key stakeholders and nutrition experts at the Iranian University of Medical Sciences. | The nutrition transition is rapidly taking place in the world due to lifestyle changes, especially in developing countries. On the other hand, food shortages are due to economic factors and lack of awareness. Nutritional policies play an essential role in improving the health of society. Analyzing these policies can help design and implement interventions and programs to improve the nutritional status of the community, especially the low-income population.
In Iran, this has happened rapidly and has led to overweight and obesity. Although many nutritional policies have been developed, no systematic research has been conducted to analyze and evaluate these policies in the context of policy analysis. |
Despite the statement of the National Nutrition Policy in Iran, the absence of some senior policy makers in the preparation of the National Nutrition Policy Statement has not been signed by the President. Thus, this led to the failure of organizations to implement the National Nutrition Policy Statement
There are insufficient coordination mechanisms to address the challenges in the field of nutrition Nutritional policies are often not evidence-based interventions, and there is not enough support for nutrition policy makers. The weakness of agreement in society and the main policy in prioritizing and arranging interventions and the role and responsibilities of institutions is an issue. Nutritional studies are performed only once every 10 years, so it is difficult to analyze the status of micronutrients and identify the trend. There is often disagreement between policies at the national level and existing programs. National capacity in public health nutrition is limited, especially human resources to implement nutritional programs. Some policies clearly do not specify operational plans and work plans. The nutrition policy process is a top-down approach in Iran, and national surveys do not show enough nutritional indicators and program success. There is not enough food monitoring system in Iran. The impact of most programs and policies is not systematically assessed. Evaluating nutrition policy is expensive and time consuming. |
National nutrition policy statement policy, which was not approved by the High Council for Health and Food Safety due to a change in council officials and was not sent to organizations for implementation. However, the Minister of Health, Treatment and Medical Education signed the statement and sent it to the country’s medical universities, and the university’s presidents were required to implement it through the provincial health council. | The Ministry of Health
MoHME The High Council of Health and Food Security The Universities of Medical Sciences (UMS) |
| Moshiri (28) | 2016 | Iran | The Formation of Primary
Health Care in Rural Iran |
Retrospective | Qualitative study data that examined the process of PHC implementation as well as the status of referral system in Iran from 1982 to 1989 through semi-structured and in-depth individual interviews (with 35 participants with different roles and situations during development and They also ran PHC (as well as extensive data from you) and collected resources in libraries. | In the late 1970s and even early 1980s, many people in need of treatment went to traditional healers, and the number and distribution of primary care centers with a public budget and the number of licensed physicians, most of them working in urban areas. Life expectancy was low and infant and maternal mortality was high, and there was no coherent vaccination program, so PHC network formation was required. | Primary health care in Iran has created an effective model for the effectiveness of health and population indicators .Since its inception, Iran has had two main goals in mind: improving justice and access.
Demographic and health indicators (eg, life expectancy, Birth rate per 1000 population, Birth rate per 1000 population, Population doubling time year and etc.) after the start of the program. Improved primary health care program concluded that the provision of health care could no longer depend on the presence of a physician. He was determined to provide social services for all citizens. |
In 1980, during the meetings of the Organizational Council of the Ministry of Health (which included the Minister of Health, all Deputy Ministers and some experts), discussions and decisions were made on general issues, but the details were mainly discussed by Dr Kamel Shadpour, Cyrus Pileroudi and Ayyub Espandar wrote with great care and was ready to perform. The purposeful interaction of PHC designers with local actors before the performance stage led to the formation of an extensive and cohesive network and the participation of groups was strengthened. The implementation of the program began with determining the location of health houses and main villages and satellite villages. After preparing the program for the expansion of the required budget network, the Ministry of Health estimated the year, and then the members of the parliament added a reference line for the expansion of the PHC network by creating a budget line when approving the budget. After the implementation of health centers throughout the country, it was done in a serious and accurate way. | The Ministry of Health (MoH)
The parliament Dr. Shadpour and Dr. Pile- roudi Former UNICEF president, Mr. James P. Grant |
| Sarfraz (29) | 2016 | Pakistan | Pakistan’s Maternal, Newborn and Child Health (MNCH) Program | Retrospective | The data presented in this qualitative paper were collected over a 3-month period in 2011. To find a wide range of challenges, qualitative data were collected from program managers, midwives, and members of the local community, such as mothers, wives, and mothers-in-law. There was also a comprehensive review of policy and planning documents on the subject | The Mother, Infant and Child Health Program were launched in 2006 with the aim of improving maternal health indicators (reducing maternal mortality), especially in order to improve MDG indicators.
Moreover, trained midwives and licensed maternal health care services in rural communities. |
Under the MNCH program, the Department of Health has developed important goals for PC-1, executive strategies, operational procedures, and estimated costs.
The MNCH program consists of two parts, one of which is to strengthen the region’s health sector technically, including improving management capacity, simplifying services to provide basic and comprehensive emergency care services for women and children and EMONC infants, and integrating MNCH services at the regional level. The other part was training experienced community-based staff to provide services |
To implement the program, the Ministry of Health and the Ministry of Foreign Affairs have each pledged to pay 50 percent of the cost of the program, other international organizations through the Ministry of Health. The continuation of this program was shaky due to the lack of financial resources of the government. There is no transparency about the future management methods of program management. Given that the transfer of the Ministry of Health was imminent at the time of data collection, there were no plans for financial management and long-term sustainability. The process of monitoring and evaluating program progress has been defined but not implemented. Resource delivery was recorded to strengthen the health care system to provide care for mothers and children, but this information was not in line with the goals of the service. Local cultural values were not included in the guidelines, and the culture of patriarchy and religious values that usually existed in Pakistani society, especially in rural areas, posed challenges to the implementation of the program and prevented the program’s goals from being achieved. | The Ministry of Health (MoH) and the Department for International Development)
The USAID The UNICEF The UNFPA |
| Abolhassani (30) | 2017 | Iran | The establishment of the Drug Naming | Retrospective | The present qualitative study data were collected first (semi-structured interview with main experts, observation) and secondary (documents). | Common medical errors due to significant human and financial costs and the safety of the patient have been high on the health policy agenda.
Due to the high rate of drug errors in Iran and the warnings of the World Health Organization about the name of the drug, policymakers of the Food and Drug Organization (FDO) have addressed this issue. Structural, situational, international and cultural factors play a major role in this |
In order to reduce drug errors and increase patient safety, the Food and Drug Organization of Iran (FDO)adopted a multifaceted and integrated approach to the initial naming of drugs,
and activated the National Drug Naming Committee, which was appointed The names of the drugs should not be misleading and should not be similar to other names of drugs registered in Iran and other countries. Branded brands should not be taken from International Non proprietary Name (INNs) of worldwide acceptability INNs, and the similarity in or writing the name of the drug with other names registered in the Iranian pharmaceutical system is mandatory (the name of the drug must be at least two consecutive letters different from the names of other registered drugs). |
The National Committee for the Appointment of Medicines within the Food and Drug Organization is in charge of implementing the naming program.
The pre-committee evaluation must comply with the criteria prepared by the FDO The National Committee for the Appointment of Medicines within the Food and Drug Administration is in charge of implementing the naming program. Pre-committee evaluation must comply with the criteria developed by the FDO, which will lead to better decision-making by committee members. The committee has processes so that all drug manufacturers are required to approve the committee before registering their products. First, submit the initial submission (maximum three special names) based on FDO criteria. After evaluating the pre-committee, send it to the main committee, and if approved, according to the rules of the trademark, manufacturers can register in the General Office of Trademarks Registry (GOTR |
The Ministry of Health
Patient safety officials in the Ministry of Health and affiliated medical sciences universities, hospitals and deputies of health the Food and Drug Organization of Iran (FDO) The General Office of Trademarks Registry (GOTR) the Department of Medicines (DoM) SCOs (the Iran Medical Council) health care providers (hospitals, pharmacies, physicians, nurses) and academics in this field the syndicate of pharmaceutical manufacturers and pharmaceutical manufacturers |
| Aljumah (31) | 2017 | Saudi Arabia | Colorectal cancer | Prospective | This forward-looking study has been obtained by comparing and searching for documents in reputable databases and comparing them | Following the increase
in the incidence of colorectal cancer and due to high demand, A forward-looking and systematic analysis of Colorectal cancer (CRC) screening policy was conducted in Saudi Arabia Despite the increasing prevalence of colorectal cancer in Saudi Arabia, there is no policy to prevent and screen for colorectal cancer. |
This policy must be carried out at the national level (country-wide) of Saudi Arabia and can be used by the general public | Due to the forward-looking nature of the present study, steps will be taken to develop CRC policy in Saudi Arabia
Although this policy does not currently exist in Saudi Arabia, it is expected that the effect of its development and its subsequent implementation will be provided in the near future. |
Actors who make policies will include the following
Influential individuals, local scientific associations, international organizations, governmental and non-governmental organizations and institutions International organizations: WHO, American Gastroenterology Association, the American Cancer Society, the European Society for Medical Oncology, the Association of European Cancer Leagues, the United European Gastroenterology State or government institutions: Regional Health Directory, The Saudi Commission for Health Specialties (SCHS) is a scientific body founded by virtue of the Royal Decree in 1992 that provides licensing and privilege for all health care providers Non-state actors: Civil society organizations and charities, Saudi Cancer Society. |
| Azami-Aghdash (٣٢) | 2017 | Iran | Road Traffic Injury Prevention | Retrospective | A qualitative study was conducted as a case study. Study data were collected by three methods of semi-structural interview, published reports and review of literature and documents of the last ten years and analysis of data and policies. | In Iran, RTIs are the first cause of injury and the second cause of death
Injury prevention policies in road traffic are essential due to a large number of road traffic injuries in Iran. Due to the increase in Road Traffic Injuries (RTIs), the identification of seat belts has emerged as an effective tool for reducing injuries in accidents and the need to increase safety equipment in vehicles and its training. |
Policies that were implemented with the two topics of seat belt and explaining prevention policies in students which was done in the form of four topics: program planning, policy formulation, policy implementation, policy evaluation | The Incident Prevention Training Policy was implemented in 2007 for elementary and middle school students and aims to improve the culture of safety and social discipline among students and their parents, strengthen responsibility and self-confidence among students, and teach. Safety and traffic tips for students were familiarity with traffic violations.Also, the proposal of the law of compulsory wearing of seat belts,The traffic police issued a circular on the implementation of the executive directive by the Ministry of Interior, the Ministry of Justice, the Ministry of Industry and Mines, the Ministry of Roads and Transportation, and the approval of the executive directive by the parliament (Majlis) | Actors in Student Policy: Ministry of Education, Ministry of Culture and Islamic Guidance, Management and Planning Organization, Teachers ‘Parents’ Council, Traffic Police and in Seat Belt Policy: Ministry of Interior, Ministry of Industry and Mines, Ministry of Education, Ministry of Culture and Islamic Guidance, Ministry of Roads and Transportation, Ministry of Justice and Management and Planning Organization, and Traffic Police |
| Haq (33) | 2017 | Pakistan | Evidence-informed health policy making | Retrospective | The data of the present study were performed in three ways: Review the literature and then a counseling session with key experts and informants to explore broad areas of policy development and in-depth interviews with participants from different levels of the health system, and finally a roundtable discussion with experts to share and consolidate and analyze information and data. | Health is not a priority for administrative or political levels, but reliance on basic evidence to maintain public acceptance and efficiency in public policy as well as effective measures in fundamental interventions.
In Pakistan, various actors - local and global - are working to facilitate the development of evidence-based health policies. However, effective intervention requires knowledge of the country’s context and knowledge of the complexities of how to formulate policies in Pakistan. |
The PC-I is the initial form according to which all projects and projects required are prepared by the planning commission
And the approval of the package of necessary health services was approved as part of the health policies of the provinces But the 2001-2002 Health Policy Document was in fact a hollow document and not a policy Rather, it was a practical plan that was approved quickly over a period of days because it was merely a symbol of the government’s efforts to have a new policy that could serve as another sign of that government, but no evidence. The discourse or measurement process of the options available was not anticipated. |
In the two key periods before and after the transfer of health to the provinces, the policy-making process was formed primarily at the federal and provincial levels, but the implementation process has faced many challenges. Political decisions have taken place in an unorganized and almost aimless manner. Furthermore, there is no process for knowing the evidence. Decisions are usually delayed and few are made arbitrarily, usually by the Office of the Minister of Health. Where political leadership is strong (for example, the senior minister of Punjab province) plays an active role, but this situation is less desirable in other provinces and regions. Programs are either not approved or are implemented incompletely. The current system for data collection and management, including the health management information system and the district health information system, is only running in five of the 30 areas. | The Ministry of Health
The WHO The Provincial Experts |
| Yousefinezhadi (34) | 2017 | Iran | Hospital Accreditation Policy | Retrospective | Qualitative study data were obtained by reviewing documents related to the policy-making and accreditation process (official letters, laws, legal regulations, instructions, reports and meetings of the Ministry of Health) and face-to-face semi-structured face interviews. | Hospital accreditation is an external evaluation system aimed at assessing patient quality and safety and encouraging continuous quality improvement.
It is developed by an independent accreditation body and local professional institution to evaluate the hospital in terms of structures, processes and results (outputs/ outcome) using predefined and optimal standards. |
2157 accreditation criteria for the accreditation of 36 departments of the hospital
Two accreditation criteria were developed for accreditation of 36 hospital wards and it was taught at the university and hospital level. It was mandatory and monitored by hospital evaluators, and then Non-standard hospitals were required to address problems and improve performance over a specified period of time |
In 2012, the hospital’s appraisal system was renamed and upgraded to a hospital accreditation system, which used the department’s method to develop accreditation standards for Iranian hospitals. After reviewing the accreditation standards of some of the leading countries, such as the United States, France, and the Middle East, the accreditation standards of Iranian hospitals were implemented. The Office for the Accreditation of Healthcare Institutions (OAHI) finalized the first draft of the standards and piloted it in eight hospitals and as a result, the standards were modified using the comments receivedand after discussions and expert meetings, 2157 accreditation criteria for the accreditation of 36 departments of the hospital were placed in the accreditation program with a focus on structures and processes.
The whole process of compiling this program in six stages And it lasted three years |
The Ministry of Health
Patient safety officials in the Ministry of The Office for the Accreditation of Healthcare Institutions (OAHI) The hospitals The Universities of Medical Sciences and Health Services (UMSs) The authorities at the hospital evaluation department |
| Ansari (35) | 2018 | Iran | Palliative Care Policy | Retrospective | Data were collected through semi-structured in-depth interviews | Because cancer is the third leading cause of death in Iran and cancer patients need supportive care and pain management, providing palliative care services, the main need of health systems is to provide services to cancer patients. | The integration of palliative care and support services within health care systems should be one of the most important goals and human resources, financial resources and physical equipment (resource management) should be considered.
Political feasibility, social feasibility, and structural feasibility must also be considered |
To implement this policy, standardization of care, the participation of stakeholders and strategies and educational management are required. | The Ministry of Health
Health care providers Volunteers Governmental and non Governmental Medical، education and research centers |
| Al-Ansari (36) | 2019 | Iran | Alcohol policy in Iran | Retrospective | Search and extract resources on the websites of official organizations such as the Ministry of Health and the Ministry of Justice
Also, literature and political documents that are available to the public |
Despite restrictions on alcohol consumption in most Muslim countries, alcohol consumption has recently increased
And because of the civil ban on alcohol and the lack of enough information about alcohol policies, it is not in line with global policies |
Among the ten policy areas of the WHO that each country can choose according to the local conditions,
In this regard, Iran has developed and implemented all its policies in the framework of a comprehensive program for prevention, treatment and reduction of alcohol poisoning in 2011-2015. |
In 2006, the Supreme Leader’s General Policy on Combating Drug and Alcohol Abuse was announced and the fight against planting, production, import, export, storage and distribution of various types of drugs and alcohol consumption became illegal. Health was set up, and in the same year, the office estimated the size of the alcoholic population.
Under the Eleventh Government (2013-2017), health was a top priority, leading to a larger national health budget for treatment. The policy adopted in 2011 forced the Ministry of Health to make progress in the treatment of alcoholism and in accordance with the recommendations of the World Health Organization in response to alcohol. The overall policy was set out in broad licenses on “health” and “comprehensive health” over a 20-year perspective and in the plan of the ‘Fifth National Development Plan’in 2014, some of these general policies aimed at improving mental health, especially among students., and prevention of harm caused by drugs, psychedelics and alcohol. |
The Ministry of Health
The Ministry of Health’s Mental Health office The governmental funding institute The State Welfare Organisation of Iran decision-makers and Policy developers The Law Enforcement Force of the Islamic Republic of Iran (NAJA) The Border Guard Command Community and religious actors International agencies Researchers Industry(very little role) |
| Edalati (37) | 2019 | Iran | Nutrition labelling | Retrospective | Review relevant documents and articles and semi-structured interviews with stakeholders | Implementing a nutrition labeling strategy to promote healthy eating and fight non communicable diseases is essential. | Provide and implement accepted executive guidelines on nutrition guidelines
Forcing to label food And provide guidance on nutritional facts And nutrition guidelines on food packaging and products |
In 2014, after the introduction of the traffic light and nutrition program, the National Committee for the Development of Food Labels was formed, and after reviewing its executive instructions, it was implemented voluntarily for 2 years and then compulsorily. | Food and Drug Administration
Iran Broadcasting organization |
| Gharaee (38) | 2019 | Iran | Public-Private Partnership in Providing Primary Health Care Policy | Retrospective | Data were collected through stakeholder interviews and document analysis and analyzed through content analysis. | the public-private partnership (PPP) is one of the basic strategies for achieving (the third goal of the Sustainable Development Goals) UHC, and in Iran’s upstream documents and in many legal articles, PPP has been considered by national policymakers | The major policies that need to be designed are:
Reduce public sector ownership using private sector power Attract people’s participation Improving the efficiency of the PHC system Repair payment system Increase justice |
In implementing the policy, the issues of coordination, creating a suitable environment, necessary tenders, employing and training the required human resources, creating a referral system, and formulating the Board of Trustees of the people should be considered. | Deputy of health of ministry of health
Minister of Health University of Medical Sciences Health insurance companies University’s office for Legal Affairs Municipality Department of education Public sector employee Politicians people (households) planning and budget organization Supportive organizations Foundation, State Welfare Organization) physicians Private sector |
| Loloei (٣٩) | 2019 | Iran | Salt reduction in bread | Retrospective | In the present qualitative study, data were collected from three methods: interview (with 37 informed and key frames), observation (directly from the work of traditional and industrial bakeries, as well as traditional flour factories) and focused group discussion.(five group discussions with people were waiting in the queue of bakeries) | In Iran, the average decrease in salt consumption (which is approximately 15-10 grams per day, especially from sodium hidden in bread, cheese and fast foods) has been seriously pursued since 2009.
However, although the Supreme Council of Health and Food Security is the coordinator of organizations working in the field of public health, all government agencies involved in wheat, flour and bread are pursuing their goals and related issues. With the health of bread and the reduction of salt in this main food, there is less mutual cooperation |
Following the establishment of a specialized working group at the Ministry of Health, Treatment and Medical Education of Iran in 2013, effective and practical solutions to eliminate the use of baking soda and reduce salt content in the bread production process were presented. Moreover, industrialization of traditional bread production (changing the pattern of bread consumption), reviewing the list of permitted and used materials in the cooking industry, revising national standards and guidelines, creating a proper culture in the field of healthy consumption of bread (through the broadcasting of the Republic Broadcasting) Islamic Iran, Newspapers, Books, Educational Brochures, and Urban Advertising P. quality wheat for domestic purchases and imports of wheat, food industry to hire graduates of technical supervision and strict implementation of health on traditional bread and bakery also close to traditional industrial complexes. | Due to changes in the government and the priorities of the Ministry of Health, the results of the meetings of the specialized working group for improving the quality of bread were ineffective, and the mentioned policies and efforts made in bread production were not carried out. | The Ministry of Health
The Council of Health and Food Security The bread producers (industrial and traditional) The Bakers |
| Mohseni (40) | 2019 | Iran | Malnutrition among children under 5 years old | Retrospective | The study data were obtained by reviewing policy and state and organizational policy documents, including the Constitution of the Islamic Republic of Iran, Iran’s 20-Year Vision Plan, Fourth and Fifth Five-Year Development Plans, Comprehensive Scientific Map of Iran, a comprehensive scientific roadmap of the health system, health system reform plan, health indicators in the Islamic Republic of Iran, document of poverty reduction and targeting of subsidies, reports published by the Health and Food Security High Council, and other relevant organizations (in scientific databases and data database searches) and semi-structured face-to-face interviews. | Malnutrition is one of the leading causes of death in children under 5 years of age and is a life-threatening factor in children’s health. Despite economic development in developing countries, it is still a major health problem in these countries. | The UNICEF Global Health Program for Children is GOBI-FFF, which includes seven programs. The content of policies adopted in Iran includes two main categories in accordance with UNICEF policy: quality-based of life policies (the most important of which include nutrition promotion policies), which are the three main policies of breastfeeding, nutrition of children under 5 years and control of micro-nutritional deficiencies include iron, iodine, vitamin A and vitamin D. | In the above documents, the issues of mother and child are important and it is necessary to take care of them
Politicians are more focused on mother and child issues than on other groups. After examining the current situation and prioritizing the problems of the provinces of the country based on malnutrition and indicators were created to measure the deficiency of micronutrients, efforts were made to involve other organizations and test policies. Appropriate policies were adopted and implemented as executive guidelines. Has been notified Feedback has been received from other organizations involved in child affairs, and self-assessment of the activities of the organizations and monitoring of the implementation of the activities has been done. |
The Ministry of Health
The Ministry of Co-operation, Labor and Social Welfare The Ministry of Agriculture The Ministry of Industry, Mine and Trade The Ministry of Education The Ministry of Culture and Islamic Guidance The Ministry of Research Science andTechnology The Ministry of Interior The Islamic Consultative AssemblyThe Targeting Subsidies Organization The Welfare Organization The Planning and Budget Organization The National Standards Organization Literacy Movement The Islamic Republic of Iran Broadcasting The Imam Khomeini Relief Committee NGOs (Saman) The Iranian Children’s Nutrition Science Association The Iranian Nutrition Forum The Scientific Society of Food and Nutrition Supporter of Health The Experts The Researchers The University professors The World Health Organization UNICEF The Food and Agriculture Organization The World Food Program Office |
| Behzadifar (41) | 2019 | Iran | The hepatitis C | Retrospective | After searching and collecting the relevant documents between September 2017 and July 2018, the relevant form was prepared, then the title, content and year of publication of the policies and documents were collected. Qualitative study data were extracted using semi-structured and face-to-face interviews with participants over two different time periods. | In Iran, the general public has a negative attitude towards HCV
Therefore, in order to increase public awareness, educational activities are carried out at different levels of the health sector, especially in PHC. However, generally, they are weak and unorganized. Most HCV research activities are carried out by research centers of the Ministry of Health, which pay less attention to socio-cultural and economic dimensions. |
The Ministry of Health of Iran has developed its plans and policies for the control and management of the disease in accordance with the WHO and other relevant international organizations. Health policies and decision-makers are working to prioritize HCV. Iran’s Hepatitis Network provides many educational and therapeutic activities in this field for patients. | The formation of the National Hepatitis Committee is an essential step in the HCV decision-making process in Iran
The key members of this committee include researchers, health policy- and decision-makers, and their responsibilities are policy and planning, management, and monitoring. |
In Iran, the Ministry of Health is the most important actor in designing and supporting HCV policies that implement disease control policies, including planning, budgeting, medical, educational, and screening activities. |
| Doshmangir (42) | 2020 | Iran | Policy analysis of the Iranian Health Transformation Plan in primary healthcare | Retrospective | It was a qualitative study data were collected through document analysis, round-table discussion, and semi-structured interviews with stakeholders | Health systems reform is inevitable due to the never-ending changing nature of societal health needs Iran needed to change its health care system. After the 8-year war with Iraq, Governments focused more on health care While little attention was paid to public health and prevention. Following several amendments, Dr. Hassan Rouhani, The President of Iran put the issue of health at the center. Soon after coming to power and fulfilling its campaign promise, HTP was apparently the most important Ubud’s government social project. Focus areas include Medical care, public health and PHC, medicine Training and improvement of the medical pricing system. | The Government of Iran
launched the “Health Transformation Plan” (HTP) in May 2014, to facilitate the attainments of UHC The goals of the reforms are: 1) to increase global health Insurance coverage 2) Ensure financial support from Patients 3) Ensure fair and equitable distribution Doctors and subspecialties across the country 4) Improving hoteling and renovation in the public sector 5) Expand outpatient services in the public health sector. 6) Promote delivery (NVD) and Prevent the increase in the number of unnecessary cesarean sections 7) Improve care and financial support From patients with special needs and end-stage diseases and 8) Establishment of air ambulance services. |
Health systems reform )HTP (focused on health problems and issues, and hospitals affiliated with the Department of Health. The scheme was later extended to cover PHC
HTP focused on health problems and issues,hospitals affiliated with the Department of Health. The scheme was later extended to cover PHC Initiated PHC modification includes programs including: Developments in the proper structure of the health team, development of family functioning, service delivery and PHC services in rural areas and cities with a population of less than 20,000 and in suburban areas and cities with a population of about 20,000 to 50,000, a new integration of services including smoking cessation, nutrition improvement, prevention of traffic accidents, promotion of physical activity Prevent cancer, prevent cardiovascular disease, prevent diabetes, improve oral health Prevent mental illness and improve the health status of people with mental illness, create and Strengthen cross-sectoral collaboration, and create and modify FP and referral systems. |
the Ministry of Health and Medical Education (MoHME) The explanation was not complete |
| Azam Raoofi (43) | 2020 | Iran | COVID-19 | Retrospective | Qualitative study data were obtained from the analysis of the targeted content of documents, programs, reports of actions and documents and official news of the Ministry of Health and Iranian websites related to COVID-19, as well as China and the World Health Organization. | Following the global outbreak of the COVID-19 virus, the Iranian Ministry of Health announced on February 19 that the disease was spreading in Iran (Qom city), and as of March 5, 2020, all 31 provinces were infected. The total number of confirmed cases on April 3 was 53,183, of which 3,294 died and 17,935 were recovered
Due to unilateral US political sanctions against Iran, it has raised major concerns about the country’s health care.Iran has made great efforts to defeat this prevalence, so it is very important to learn policies to formulate appropriate policies and implement them accordingly. |
The content of Iran’s policy regarding the prevalence of corona can be divided into two categories: pre-outbreak and post-outbreak. Examination of incoming passengers from China and transfer of suspicious cases to certain hospitals, return of Iranian students residing in China and quarantining them for two weeks and allocation of special funds to provide the necessary resources, such as personnel, medicines, equipment, etc. And actions After the outbreak, it was based on the WHO six building blocks, which included Including Inter-sectoral cooperation, legislation
Obtaining a license to import equipment and medical universities with permission to recruit new personnel Service delivery for providing, equipping and operating medical centers and ambulances, and providing and equipping paraclinical centers Disinfection of public places, insurance, resource allocation, employment and human resources, informing and increasing public awareness, research, technology and information system, medicines and medical equipment. |
The COVID-19 National Committee was set up at the Iranian Ministry of Health, which needs to be strengthened
Corona’s countermeasures are a major concern for public health, which requires inter-sectoral collaboration and government agreement through various coalitions. There are several factors to consider when planning and implementing programs, Including : paying attention to the capacity of medical universities and their ability to implement programs, the need for inter-sectoral collaboration and attention to formal multidisciplinary working groups given the complexity of the issue, The need for regular negotiations between policymakers and the so-called street-level bureaucrats (SLBs) to optimize service delivery and achieve the best possible results. Paying attention to the attitudes, strategies and knowledge of frontline employees that unofficially influences policy implementation The government’s attention to the evaluation and monitoring of frontline staff and the provision of financial and non-financial incentives for stakeholders, Considering the importance of the role of political agents and other stakeholders, including the clergy, governors, mayors and Friday prayer leaders of Qom and Mashhad, member of parliamentarians MPs, as well as some experts and academics in making some decisions such as closure of holy shrines and cancellation of Friday prayers for the implementation of social distancing and pay attention to their role as mediators or political intermediaries To compromise and limit differences between coalitions to reach a collective agreement. |
The Ministry of Health
MoHME The governmental and non-governmental organizations The Universities of Medical Sciences (UMS) The MoHME various deputies (particularly Deputies for Curative Affairs, Public Health, Nursing, and Administration and Finance) The Food and Drug Organization, The Emergency Services Organization, The Iran Health Insurance Organization are the main intra- organizational actors within the MoHME, almost 200 The Medical Associations, The General Medical Council, The General Nursing Council, The Social Security Organization (and other insurance organizations), the Islamic Consultative Assembly (Parliament), The Cabinet of Ministers and Officials Planning and Budget |
Discussion
Policy analysis is a valuable process for understanding policy processes, identifying the determinants of the failures and successes of past policies, and planning for future ones [13], and is also complex due to the diverse nature of health issues [13, 47]. The present study assessed published studies related to health issues in the Eastern Mediterranean region using a Health policy triangle framework. The findings of the present study were selected from thirty extracted articles. With the exception of one study [34], all studies were retrospective. It seems that in order to evaluate the programs of the health system, it seems that in order to evaluate health system programs, it is better to pay attention to studies with prospective design and put it on the agenda, because evidence arising from these researches in improving the health systems and providing services by policymakers and researchers would be of higher quality and strength. Policy analysis can show the agility and dynamism of countries’ health systems [48, 49]. Findings of studies based on four elements of study (context - why do you need this policy -, content - what is the policy mainly about-, process - how this policy is designed and implemented - and actors - who participate and influence policy formulation and implementation) were analyzed and reported.
CONTEXT
The policy analysis process should be such as to reflect a thorough understanding of the context, decision-making, planning and implementation of policies. Because health issues go beyond health care and are influenced by psychosocial, economic and environmental factors [13, 47], health policy-making is an inherently political process, which is influenced by the social and political context, and therefore understanding and analyzing political systems can help better assess the context and why a given policy is chosen [50].
Demographic, epidemiological, educational, technological, cultural, as well as social developmental, economic and financial issues, the specific type of political regime are some of the issues that should be seen in context [51]. In the included studies, political and administrative factors, as well as economic and financial one, and social and cultural variables, personal and political interests, promotion of international standards of sectarianism, urgency and values of policymakers and media policies are the most important underlying parameters determining the success of a given health policy. Impacts on specific policies were reported. In most of the selected studies, the contextual factors of the country of the study did not have a direct impact on the choice of policy for analysis. It seems that the priority criteria for policy analysis in EMRO countries should be more transparent and the use of evidence should be increased. This could contribute to a more efficient and effective use of financial resources for policy analysis research [52]. Topics analyzed by researchers in selected studies included high prevalence or mortality rates, WHO reports, the Sustainable Development Goals (SDGs), Universal Health Coverage (UHC) achievement. Researcher evaluated also whether political decisions to solve a problem were taken based on evidence. Despite the fact that the type of political system, financing and Gross Domestic Product (GDP) per capita allocated to health programs are important elements in health policy making and can influence health policies related processes, none of the studies included in the present systematic review focused specifically on these factors and their impact on the policy in question.
The health policy triangle framework states that national, international, political, economic and social factors can influence health policies. However, based on the Leicher’s classification of these factors, some of which depend on circumstances, structural, cultural, and international factors, most of the selected studies did not pay full attention to these issues and paid less attention to their impact. These issues can be effective in creating a tendency to analyze or not analyze a policy in the health sector. One of the important points was the attention of the researchers of the selected studies to the selection of topics related to diseases and issues such as health justice, health finance, governance, use of evidence whereas other issues were less analyzed. Perhaps one of the reasons for choosing diseases for policy analysis is easier access, greater participation of people in these studies, which encourages EMRO researchers to analyze them. Of course, the nature of some issues in the health sector may make researchers less interested in analyzing them. They may be conservative and not accept the problems they need to gather information about them.
On the other hand, due to political issues such as wars and sanctions in the EMRO region and its great impact on the health sector, the influence of these issues has received less attention. Ethnic and national prejudices have not been accounted for in the analysis of health sector policies in the countries of this region. Religious tendencies in this area have not been considered in selected studies. The existence of wars in Afghanistan, Syria and Yemen and the sanctions on Iran can affect the process of policy analysis of health-related issues. Lack of full vaccination coverage, failure to achieve the Millennium Development Goals (MDGs) goals, inadequate access to health services, reduced health budgets, issues related to children, women and the elderly, immigrants and refugees problems, as well as economic-financial problems and declining incomes, can dramatically impact health funding and resources allocation, which in its turn further complicates these problems.
To analyze a policy in the health sector, one should not be utilitarian and conservative. You have to see the underlying issues. These affect the success or failure of that policy. Policy analysis is a dynamic and political process. The diversity of EMRO countries’ political systems is crucial in implementing or not implementing health sector policies. The attention and priorities of policymakers in these countries can influence the choice of a given issue for policy analysis. Unfortunately, this issue has received less attention. Researchers seem to have sought to analyze issues that are more influenced by international factors.
CONTENT
Content is the body of policy, which includes the nature and details of a policy proposal or document and is expressed through all its components, including: programs, projects, specific activities, goals, general objectives and observable goals [53, 54]. The content of the selected studies is given in Table II.
Some articles referred to the formulation of policies, guidelines, and related laws, and some referred to its communication to related organizations and some other articles described the goals of the strategies. However, some studies did not fully explain the content of the programs under study and the relevant documentation and program outputs were not explained. Some studies did not mention or were vague.
The programs referred to for framework analysis were mainly developed by the Ministry of Health of these countries. The selected studies did not document any health initiatives and related issues or programs that were felt needed and pursued by other health-related organizations. It seems that in EMRO countries, the main focus for the implementation and start of health programs is only the Ministry of Health, and due to over-reliance on this ministry, the process of programs is unipolar and still or other organizations are not sensitive in this regard or if there were no documents.
While health should be current and considered in all policies in countries. At the heart of “Health in All Policies” is the study of health determinants, which are largely controlled by policies of sectors other than those involved in health, because in the “Health in All Policies” process, addressing the social factors of health and disease can be a powerful tool for reducing health inequalities [55].
Health is highly influenced by lifestyle and environment and many health issues are simultaneously deeply affected by factors outside the traditional realm of health and healthcare. Factors such as literacy, poverty, employment and racism contribute to differences in life expectancy as well as health-related quality of life. Concerns about how to address these factors have led to a focus on “health in policies”, in which policies in the social sectors such as transport, housing, employment and agriculture can ideally focus on health and access to health contribute to equity in health [56]. Once the problems are identified, the content analysis will focus on the suggestions and goals themselves. Sources (material and political) should be mentioned in the discussion of the content of a policy. Material resources, such as equipment and money and technical and organizational resources, this type of resources means the knowledge and organizational and managerial abilities to implement the proposals. Moreover, political resources are essentially the power to implement a policy. None of the studies addressed this issue.
PROCESS
In the analysis of this section, what should be considered is to describe the process of health policies, ie policy formulation and implementation of policies and issues related to them. If Walt considers the three main aspects of the policy process to be the following: The issue of power in terms of who makes decisions and who influences them. The concept and types of policies in terms of what politics is and how it is policy-making, and the logic and rules of politics in terms of its formation as a logical process.
In some of the articles included in the present systematic review, some explained the program and its purpose, while others described the activities of care centers and decision-making committees such as the National Committee for Hepatitis and Acquired Immunodeficiency Syndrome (AIDS), etc. Some considered the reason for the programs to be due to the urgency of the issue and other than political decisions. Some studies have pointed to the implementation and structural challenges of programs and policies, the latter of which has been highlighted in these studies as one of the factors in the failure of health programs. Other reasons for the programs’ failure include internal wars and crises, weak financial and technical capacity, disputes between states, sanctions, and declining funding for national standards produced without infrastructure. It seems that one of the reasons for the failure of the programs was the lack of proper prioritization to solve the problems under study, as mentioned in the articles. Because in order to succeed in promoting health programs, it is very important to pay attention to prioritization and criteria (which must be clearly defined and understood by decision makers and stakeholders in each country) and should not be the sole responsibility of specific institutions or ministries. Therefore, in all policies, stakeholders and supporters should be considered as key factors. As shown in these studies, programs that sought advocacy were more successful because advocacy as a key strategy to achieve the goals of health promotion and Advocacy organizations play a key role in promoting justice in health, given global challenges, research and policy [57].
Also, health should be separated from political issues and levels of health governance, policies and measures should be complementary to each other because participation in health governance, policy-making and development of interventions and its implementation by sectors other than health is important and health is mainly outside. Areas and levels of health are created and attention to the creation and implementation of health in all policies strengthens the potential that other sectors have for health [58]. It should be noted that developing countries underestimate the role of education in their policies, and the budgets allocated for health education in these countries are very small and health policy makers pay very little attention to this issue. Therefore, indigenous educational projects should be designed in accordance with the context of communities, and on the other hand, executive decision-making groups should be multidisciplinary, and their roles should be clearly defined before determining program priorities, and involving groups other than Medical teams are very effective in advancing goals [44, 45, 52].
ACTORS
The WHO in its 2000 report defined health systems as “all organizations, institutions, and resources dedicated to the production of health measures,” which includes a full range of actors and health care providers, including sectors. Private, non-profit, non-governmental organizations (NGOs) as well as international donor foundations [59]. Therefore, health systems are operating at the central, regional, local, social and home levels, and all of these institutions must be considered at all levels of strengthening health systems. Actors include any institution, character, or social movement that has the ability to influence health events, and a common feature of all social actors is that they have a certain amount of power.
The most important actor mentioned in the present study was the Ministry of Health. Several articles referred to the role of domestic and foreign NGOs. NGOs play an important role in providing health services and health policies, and the importance of these organizations in providing health services in low- and middle-income countries has become increasingly important [60]. In poor countries, they are more effective and efficient than public organizations and act as agents of change in international economic, social and environmental policies. It seems that EMRO countries have not yet been able to use the effective potential of NGOs in advancing health policies, ignoring the need to strengthen government health programs and cooperate with organizations to achieve the goals set in the SDGs and improve the quality and efficiency of health care. Non-governmental support is therefore essential [61].
The involvement of NGOs with the public sector should play a key role in addressing justice issues and improving the quality of services provided, along with addressing system access and accountability issues. In these studies, the role of the private sector as actors was very small and in some studies it was not explicitly mentioned, while policymakers, who want to move health systems towards UHC must play appropriate roles to provide, identify and rely on private providers and health markets. The importance of strengthening public and private health systems has been repeatedly emphasized in various documents by various international, regional and national institutions related to health care such as WHO, USAID, Global Fund, etc. The non-governmental sector and the private sector, due to their potential and capabilities, can fill the gaps and shortcomings that exist in the public sector, so a serious partnership between them can ultimately increase accountability, equity and efficiency in the health care system. It should be noted that health care outsourced to the private sector in low- and middle-income countries (LMICs) is very widespread, even though weak, and highly heterogeneous. It seems that in EMRO member countries, the role of these two sectors, namely non-governmental organizations and the private sector as a very important player in health system policy, is very small and has led to the lack of progress in existing policies in the health sector.
LIMITATIONS
In this context, it seems that the place of the result and the cause of the failure of the programs is empty, and also there are no solutions to the problems in the research. Gilson and Rafaeli pointed out some of the gaps and weaknesses in the analysis of health policies in low- and middle-income countries mentioned in special cases [13].
Conclusion
In the EMRO region, the role of evidence-based research in policy-making has been repeatedly emphasized, but its use in health program decision-making has been limited and health research systems in the EMR are still under scrutiny. We think that they have not been able to produce needed evidence and inject it into health systems. There is still a gap between evidence-based research in health systems and its use in policy-making, as well as in the analysis of health policies in LMICs. The findings of these studies also confirm this, and therefore studies based on policy analysis should be aimed at achieving this goal because evidence-based decisions can strengthen health systems, improve health and improve existing inequalities. Also, considering that this analysis triangle has 4 specific components, studies should be selected that can be analyzed based on the four elements of this study, but some studies did not have these conditions. On the other hand, this framework should be re-examined and its components should be up-to-date and more standardized in order to enable deeper analyses.
Acknowledgements
Not applicable.
Figures and tables
Footnotes
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Funding
Not applicable.
Authors’ contributions
MB and HR designed the study. MB, SA, MM, SJE, MKG, AB, SA, SS, LD and NLB collected the data and performed the data analysis. HR, NLB, MB, SS, SJE and LD edited and revised the paper for grammar. All authors read and approved the final paper for publication.
References
- [1].Correa-de-Araujo R. Evidence-based practice in the united states: Challenges, progress, and future directions. Health Care Women Int 2016;37:2-22. https://doi.org/10.1080/07399332.2015.1102269 10.1080/07399332.2015.1102269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].van de Goor I, Hämäläinen RM, Syed A, Juel Lau C, Sandu P, Spitters H, Eklund Karlsson L, Dulf D, Valente A, Castellani T, Aro AR, REPOPA consortium . Determinants of evidence use in public health policy making: Results from a study across six EU countries. Health Policy Plan 2017;121:273-81. https://doi.org/10.1016/j.healthpol.2017.01.003 10.1016/j.healthpol.2017.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Contandriopoulos D, Benoît F, Bryant-Lukosius D, Carrier A, Carter N, Deber R, Duhoux A, Greenhalgh T, Larouche C, Leclerc BS, Levy A, Martin-Misener R, Maximova K, McGrail K, Nykiforuk C, Roos N, Schwartz R, Valente TW, Wong S, Lindquist E, Pullen C, Lardeux A, Perroux M. Structural analysis of health-relevant policy-making information exchange networks in Canada. Implement Sci 2017;12:116. https://doi.org/10.1186/s13012-017-0642-4 10.1186/s13012-017-0642-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Cheung KK, Mirzaei M, Leeder S. Health policy analysis: a tool to evaluate in policy documents the alignment between policy statements and intended outcomes. Aust Health Rev 2010;34:405-13. https://doi.org/10.1071/AH09767 10.1071/AH09767 [DOI] [PubMed] [Google Scholar]
- [5].Robert E, Rajan D, Koch K, Muggleworth Weaver A, Porignon D, Ridde V. Policy dialogue as a collaborative tool for multistakeholder health governance: a scoping study. BMJ Glob Health 2020;4(Suppl 7):e002161. https://doi.org/10.1136/bmjgh-2019-002161 10.1136/bmjgh-2019-002161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].World Health Organization. Health policy 2020 [updated 28 August 2020. Available from: https://www.who.int/topics/health_policy/en/.
- [7].Mulcahy G, Boelsen-Robinson T, Hart AC, Pesantes MA, Sameeha MJ, Phulkerd S, Alsukait RF, Thow AM. A comparative policy analysis of the adoption and implementation of sugar-sweetened beverage taxes (2016-19) in 16 countries. Health Policy Plan 2022;37:543-64. https://doi.org/10.1093/heapol/czac004 10.1093/heapol/czac004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kind J, Maeschli B, Bruggmann P. How to set the agenda for hepatitis C: a theory-driven policy analysis. Health Res Policy Syst 2022;20:20. https://doi.org/10.1186/s12961-022-00824-3 10.1186/s12961-022-00824-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Gilson L, Raphaely N. The terrain of health policy analysis in low and middle income countries: a review of published literature 1994-2007. Health Policy Plan 2008;23:294-307. https://doi.org/10.1093/heapol/czn019 10.1093/heapol/czn019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Browne J, Coffey B, Cook K, Meiklejohn S, Palermo C. A guide to policy analysis as a research method. Health Promot Int 2019;34:1032-44. https://doi.org/10.1093/heapro/day052 10.1093/heapro/day052 [DOI] [PubMed] [Google Scholar]
- [11].Walt G, Gilson L. Can frameworks inform knowledge about health policy processes? Reviewing health policy papers on agenda setting and testing them against a specific priority-setting framework. Health Policy Plan 2014;29 (Suppl 3):6-22. https://doi.org/10.1093/heapol/czu081 10.1093/heapol/czu081 [DOI] [PubMed] [Google Scholar]
- [12].Montenegro Martínez G, Carmona Montoya A, Franco-Giraldo Á. Models for public health policy analysis reported in scientific publications. Gac Sanit 2020;S0213-9111:30275-4. https://doi.org/10.1016/j.gaceta.2019.11.007 10.1016/j.gaceta.2019.11.007 [DOI] [PubMed] [Google Scholar]
- [13].Walt G, Shiffman J, Schneider H, Murray SF, Brugha R, Gilson L. ‘Doing’ health policy analysis: methodological and conceptual reflections and challenges. Health Policy Plan 2008;23:308-17. https://doi.org/10.1093/heapol/czn024 10.1093/heapol/czn024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Shiffman J, Sultana S. Generating political priority for neonatal mortality reduction in Bangladesh. Am J Public Health 2013;103:623-31. https://doi.org/10.2105/AJPH.2012.300919 10.2105/AJPH.2012.300919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].O’Brien GL, Sinnott SJ, Walshe V, Mulcahy M, Byrne S. Health policy triangle framework: Narrative review of the recent literature. Health Policy OPEN 2020;1:100016. https://doi.org/10.1016/j.hpopen.2020.100016 10.1016/j.hpopen.2020.100016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].World Health Organization. WHO’s Eastern Mediterranean Region comprises 2020 [updated 28 August 2020. Available from: http://www.emro.who.int/countries.html.
- [17].Beesley M, Cometto G, Pavignani E. From drought to deluge: how information overload saturated absorption capacity in a disrupted health sector. Health Policy Plan 2011;26:445-52. https://doi.org/10.1093/heapol/czq083 10.1093/heapol/czq083 [DOI] [PubMed] [Google Scholar]
- [18].Zaidi S, Mayhew SH, Cleland J, Green AT. Context matters in NGO-government contracting for health service delivery: a case study from Pakistan. Health Policy Plan 2012;27:570-81. https://doi.org/10.1093/heapol/czr081 10.1093/heapol/czr081 [DOI] [PubMed] [Google Scholar]
- [19].Phillimore P, Zaman S, Ahmad B, Shoaibi A, Khatib R, Khatib R, Husseini A, Fouad F, Elias M, Maziak W, Tlili F, Tinsa F, Ben Romdhane H, Kılıç B, Kalaça S, Ünal B, Critchley J. Health system challenges of cardiovascular disease and diabetes in four Eastern Mediterranean countries. Glob Public Health 2013;8:875-89. https://doi.org/10.1080/17441692.2013.830756 10.1080/17441692.2013.830756 [DOI] [PubMed] [Google Scholar]
- [20].Seef S, Jeppsson A. Is it a policy crisis or it is a health crisis? The Egyptian context--analysis of the Egyptian health policy for the H1N1 flu pandemic control. Pan Afr Med J 2013;14:59. https://doi.org/10.11604/pamj.2013.14.59.1631 10.11604/pamj.2013.14.59.1631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Zaidi S, Mohmand SK, Hayat N, Acosta AM, Bhutta ZA. Nutrition policy in the post-devolution context in Pakistan: An analysis of provincial opportunities and barriers. IDS Bull 2013;44:86-93. [Google Scholar]
- [22].El-Jardali F, Bou-Karroum L, Ataya N, El-Ghali HA, Hammoud R. A retrospective health policy analysis of the development and implementation of the voluntary health insurance system in Lebanon: learning from failure. Soc Sci Med 2014;123:45-54. https://doi.org/10.1016/j.socscimed.2014.10.044 10.1016/j.socscimed.2014.10.044 [DOI] [PubMed] [Google Scholar]
- [23].El-Jardali F, Hammoud R, Younan L, Nuwayhid HS, Abdallah N, Alameddine M, Bou-Karroum L, Salman L. The making of nursing practice law in Lebanon: a policy analysis case study. Health Res Policy Syst 2014;12:52. https://doi.org/10.1186/1478-4505-12-52 10.1186/1478-4505-12-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Markazi-Moghaddam N, Aryankhesal A, Arab M. The first stages of liberalization of public hospitals in Iran: establishment of autonomous hospitals and the barriers. Iran J Public Health 2014;43:1640-50. [PMC free article] [PubMed] [Google Scholar]
- [25].Speakman EM, Shafi A, Sondorp E, Atta N, Howard N. Development of the community midwifery education initiative and its influence on women’s health and empowerment in Afghanistan: a case study. BMC Womens Health 2014;14:111. https://doi.org/10.1186/1472-6874-14-111 10.1186/1472-6874-14-111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Awadalla H. Implementation of quality assurance program in Sudanese public hospitals: lessons learned. J Med Med Res 2015;3:7-14. [Google Scholar]
- [27].Ben Romdhane H, Tlili F, Skhiri A, Zaman S, Phillimore P. Health system challenges of NCDs in Tunisia. Int J Public Health 2015;60 (Suppl 1):S39-46. https://doi.org/10.1007/s00038-014-0616-0 10.1007/s00038-014-0616-0 [DOI] [PubMed] [Google Scholar]
- [28].Faraji O, Etemad K, Akbari Sari A, Ravaghi H. Policies and programs for prevention and control of diabetes in Iran: A document analysis. Glob J Health Sci 2015;7:187-97. https://doi.org/10.5539/gjhs.v7n6p187 10.5539/gjhs.v7n6p187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Alharbi NS, Alotaibi M, de Lusignan S. An analysis of health policies designed to control and prevent diabetes in Saudi Arabia. Glob J Health Sci 2016;8:233-41. https://doi.org/10.5539/gjhs.v8n11p233 10.5539/gjhs.v8n11p233 [DOI] [Google Scholar]
- [30].Goshtaei M, Ravaghi H, Sari AA, Abdollahi Z. Nutrition policy process challenges in Iran. Electron Physician 2016;8:1865-73. https://doi.org/10.19082/1865 10.19082/1865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Moshiri E, Rashidian A, Arab M, Khosravi A. Using an analytical framework to explain the formation of primary health care in rural Iran in the 1980s. Arch Iran Med 2016;19:16-22. [PubMed] [Google Scholar]
- [32].Sarfraz M, Hamid S. Exploring managers’ perspectives on MNCH program in Pakistan: a qualitative study. PLoS One 2016;11:e0146665. https://doi.org/10.1371/journal.pone.0146665 10.1371/journal.pone.0146665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Abolhassani N, Akbari Sari A, Rashidian A, Rastegarpanah M. The establishment of the drug naming committee to restrict look-alike medication names in Iran: a qualitative study. Int J Risk Saf Med 2017;29:69-79. https://doi.org/10.3233/JRS-170740 10.3233/JRS-170740 [DOI] [PubMed] [Google Scholar]
- [34].Aljumah AA, Aljebreen AM. Policy of screening for colorectal cancer in Saudi Arabia: a prospective analysis. Saudi J Gastroenterol 2017;23:161-8. https://doi.org/10.4103/sjg.SJG_468_16 10.4103/sjg.SJG_468_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Azami-Aghdash S, Gorji HA, Shabaninejad H, Sadeghi-Bazargani H. Policy analysis of road traffic injury prevention in Iran. Electron Physician 2017;9:3630-8. https://doi.org/10.19082/3630 10.19082/3630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Haq Z, Hafeez A, Zafar S, Ghaffar A. Dynamics of evidence-informed health policy making in Pakistan. Health Policy Plan 2017;32:1449-56. https://doi.org/10.1093/heapol/czx128 10.1093/heapol/czx128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Yousefinezhadi T, Mosadeghrad AM, Arab M, Ramezani M, Sari AA. An Analysis of hospital accreditation policy in Iran. Iran J Public Health 2017;46:1347-58. [PMC free article] [PubMed] [Google Scholar]
- [38].Ansari M, Rassouli M, Akbari ME, Abbaszadeh A, Akbarisari A. Palliative care policy analysis in Iran: a conceptual model. Indian J Palliat Care 2018;24:51-7. https://doi.org/10.4103/IJPC.IJPC_142_17. 10.4103/IJPC.IJPC_142_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Al-Ansari B, Thow AM, Mirzaie M, Day CA, Conigrave KM. Alcohol policy in Iran: policy content analysis. Int J Drug Policy 2019;S0955-3959:30210-5. https://doi.org/10.1016/j.drugpo.2019.07.032 10.1016/j.drugpo.2019.07.032 [DOI] [PubMed] [Google Scholar]
- [40].Edalati S, Omidvar N, Haghighian Roudsari A, Ghodsi D, Zargaraan A. Development and implementation of nutrition labelling in Iran: A retrospective policy analysis. Int J Health Plann Manage 2019;45:e28-e44. https://doi.org/10.1002/hpm.2924 10.1002/hpm.2924 [DOI] [PubMed] [Google Scholar]
- [41].Gharaee H, Tabrizi JS, Azami-Aghdash S, Farahbakhsh M, Karamouz M, Nosratnejad S. Analysis of public-private partnership in providing primary health care policy: an experience from Iran. J Prim Care Community Health 2019;10:2150132719881507. https://doi.org/10.1177/2150132719881507 10.1177/2150132719881507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Loloei S, Pouraram H, Majdzadeh R, Takian A, Goshtaei M, Djazayery A. Policy analysis of salt reduction in bread in Iran. AIMS Public Health 2019;6:534-45. https://doi.org/10.3934/publichealth.2019.4.534 10.3934/publichealth.2019.4.534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Mohseni M, Aryankhesal A, Kalantari N. Prevention of malnutrition among children under 5 years old in Iran: a policy analysis. PLoS One 2019;14:e0213136. https://doi.org/10.1371/journal.pone.0213136 10.1371/journal.pone.0213136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Behzadifar M, Azari S, Gorji HA, Martini M, Bragazzi NL. The hepatitis C virus in Iran: health policy, historical, ethical issues and future challenges. J Prev Med Hyg 2020;61:E109-E18. https://doi.org/10.15167/2421-4248/jpmh2020.61.1.1438 10.15167/2421-4248/jpmh2020.61.1.1438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Doshmangir Rashidian A, Kouhi F, Sergeevich Gordeev V. Setting health care services tariffs in Iran: half a century quest for a window of opportunity. Int J Equity Health 2020;19:112. https://doi.org/10.1186/s12939-020-01224-1 10.1186/s12939-020-01224-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Raoofi A, Takian A, Akbari Sari A, Olyaeemanesh A, Haghighi H, Aarabi M. COVID-19 pandemic and comparative health policy learning in Iran. Arch Iran Med 2020;23:220-34. https://doi.org/10.34172/aim.2020.02 10.34172/aim.2020.02 [DOI] [PubMed] [Google Scholar]
- [47].Embrett MG, Randall GE. Social determinants of health and health equity policy research: exploring the use, misuse, and nonuse of policy analysis theory. Soc Sci Med 2014;108:147-55. https://doi.org/10.1016/j.socscimed.2014.03.004 10.1016/j.socscimed.2014.03.004 [DOI] [PubMed] [Google Scholar]
- [48].El-Jardali F, Lavis JN, Ataya N, Jamal D. Use of health systems and policy research evidence in the health policymaking in eastern Mediterranean countries: views and practices of researchers. Implement Sci 2012;7:2. https://doi.org/10.1186/1748-5908-7-2 10.1186/1748-5908-7-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Barnish M, Tørnes M, Nelson-Horne B. How much evidence is there that political factors are related to population health outcomes? An internationally comparative systematic review. BMJ Open 2018;8:e020886. https://doi.org/10.1136/bmjopen-2017-020886 10.1136/bmjopen-2017-020886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Casey M, Rohde D, Brady AM, Fealy G, Hegarty J, Kennedy C, McNamara M, Nicholson E, O’Connell R, O’Connor L, O’Leary D, O’Reilly P, Stokes D. Developing a new health-related policy analysis tool: An action research cooperative inquiry approach. J Nurs Manag 2019;27:1233-41. https://doi.org/10.1111/jonm.12804 10.1111/jonm.12804 [DOI] [PubMed] [Google Scholar]
- [51].Frenk J. Comprehensive policy analysis for health system reform. Health Policy 1995;32:257-77. https://doi.org/10.1016/0168-8510(95)00739-f 10.1016/0168-8510(95)00739-f [DOI] [PubMed] [Google Scholar]
- [52].Gibson JL, Martin DK, Singer PA. Setting priorities in health care organizations: criteria, processes, and parameters of success. BMC Health Serv Res 2004;4:25. https://doi.org/10.1186/1472-6963-4-25 10.1186/1472-6963-4-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Walt G, Gilson L. Reforming the health sector in developing countries: the central role of policy analysis. Health Policy Plan 1994;9:353-70. https://doi.org/10.1093/heapol/9.4.353 10.1093/heapol/9.4.353 [DOI] [PubMed] [Google Scholar]
- [54].Araújo Jr JLCd, Maciel Filho R. Developing an operational framework for health policy analysis. Rev Bras de Saúde Matern Infant 2001;1:203-21. https://doi.org/10.1590/S1519-38292001000300002 10.1590/S1519-38292001000300002 [DOI] [Google Scholar]
- [55].Zaidi S, Bhutta Z, Hussain SS, Rasanathan K. Multisector governance for nutrition and early childhood development: overlapping agendas and differing progress in Pakistan. BMJ Glob Health 2018;3(Suppl 4):e000678. https://doi.org/10.1136/bmjgh-2017-000678 10.1136/bmjgh-2017-000678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Collins J, Koplan JP. Health impact assessment: a step toward health in all policies. JAMA 2009;302:315-7. https://doi.org/10.1001/jama.2009.1050 10.1001/jama.2009.1050 [DOI] [PubMed] [Google Scholar]
- [57].Carlisle S. Health promotion, advocacy and health inequalities: a conceptual framework. Health Promot Int 2000;15:369-76. https://doi.org/10.1093/heapro/15.4.369 10.1093/heapro/15.4.369 [DOI] [Google Scholar]
- [58].De Leeuw E. Engagement of sectors other than health in integrated health governance, policy, and action. Annu Rev Public Health 2017;38:329-49. https://doi.org/10.1146/annurev-publhealth-031816-044309 10.1146/annurev-publhealth-031816-044309 [DOI] [PubMed] [Google Scholar]
- [59].World Health Organization. The world health report 2000 - Health systems: improving performance 2000 [updated 9 November 2020. Available from: https://www.who.int/whr/2000/en/
- [60].Ejaz I, Shaikh BT, Rizvi N. NGOs and government partnership for health systems strengthening: a qualitative study presenting viewpoints of government, NGOs and donors in Pakistan. BMC Health Serv Res 2011;11:1-7. https://doi.org/10.1186/1472-6963-11-122 10.1186/1472-6963-11-122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Shaikh B, Kadir M, Hatcher J. Health care and Public health in South Asia. Public Health 2006;2:142-4. https://doi.org/10.1016/j.puhe.2005.08.018 10.1016/j.puhe.2005.08.018 [DOI] [PubMed] [Google Scholar]


