Abstract
Transgender women of color are disproportionately impacted by HIV, poor health outcomes, and transgender-related discrimination (TD). We tested the Model of Gender Affirmation (GA) to identify intervention-amenable targets to enhance viral suppression (VS) using data from 858 transgender women of color living with HIV (49% Latina, 42% Black; 36% virally suppressed) in a serial mediation model. Global fit statistics demonstrated good model fit; statistically significant (p ≤ 0.05) direct pathways were between TD and GA, GA and healthcare empowerment (HCE), and HCE and VS. Significant indirect pathways were from TD to VS via GA and HCE (p = 0.036) and GA to VS via HCE (p = 0.028). Gender affirmation and healthcare empowerment significantly and fully mediated the total effect of transgender-related discrimination on viral suppression. These data provide empirical evidence for the Model of Gender Affirmation. Interventions that boost gender affirmation and healthcare empowerment may improve viral suppression among transgender women of color living with HIV.
Keywords: Transgender, HIV, Gender affirmation, Healthcare empowerment, Viral suppression
Introduction
Globally, transgender women are disproportionately impacted by HIV and transgender women living with HIV are less likely to be virally suppressed than other HIV-impacted groups [1]. Transgender women of color have also been shown to experience higher rates of violence, harassment, and discrimination than other subgroups of transgender people in the United States in virtually every aspect of life, such as employment, housing, and healthcare settings [2]. The association between discrimination and poor health outcomes has been documented but little is known about potential targets for intervention on this association. For example, experiences of discrimination among transgender people have been found to be correlated with higher rates of depression and post-traumatic stress disorder, both of which have been linked to lower rates of HIV medication adherence and negative health outcomes among people living with HIV [3–5]. Among transgender people, access to hormone therapy [6] and peer support [7] may buffer the effect of discrimination and stigma on health outcomes. The associations between social and medical gender affirmation with improved mental health outcomes have been documented but to date there is no quantitative data that explores how gender affirmation may mediate the relationship between discrimination and/or stigma and poor HIV-related health outcomes [5].
The Model of Gender Affirmation is a transgender-specific conceptual framework developed to examine the role of gender affirmation in risk-taking, self-care, and healthcare-seeking behavior among transgender women [8]. Gender affirmation has been defined as “an interpersonal, interactive process whereby a person receives social recognition and support for their gender identity and expression” [8] and can also include medical and legal processes related to gender transition [9, 10]. Other terms that have been used to describe this concept include ‘gender validation’ [11] and ‘transgender identity affirmation’ [12]. The Model of Gender Affirmation was developed to explore gender affirmation-related dimensions of health disparities experienced by transgender people and to identify potential avenues for intervention upon the relationship between transgender-related discrimination and negative health outcomes [8].
The Model of Gender Affirmation proposes that unmet need for gender affirmation in transgender persons can result in identity threat, which is the psychological threat to one’s sense of self that results from experiencing devaluation of one’s social group [13]. Transgender women whose needs for gender affirmation are not being met through social and medical pathways may attempt to reduce identity threat by seeking affirmation in contexts that pose risks and undermine health-seeking behaviors (e.g. risky sex, injection silicone). The model hypothesizes that if identity threat can be reduced by meeting transgender people’s needs for gender affirmation through health-promoting means such as social support and gender-affirming medical care, health outcomes will improve. Preliminary support for the Model of Gender Affirmation demonstrates how meeting transgender women’s needs for gender affirmation may decrease risk behavior and increase self-care [8, 14, 15].
Given the complexities of multiple and unique barriers to engagement in HIV care experienced by transgender women living with HIV, the Model of Gender Affirmation was recently adapted to further inform intervention development by integrating the concept of healthcare empowerment (HCE) [16–18]. The HCE model enables the organization, investigation, and intervention upon factors that contribute to optimal health outcomes and posits that vulnerable populations will experience improved health outcomes when they are informed, committed, collaborative, and engaged in their healthcare, and when they are able to tolerate uncertainty of future health outcomes. Studies have provided support for the HCE framework in explaining antiretroviral treatment (ART) uptake, adherence, and resulting viral suppression among non-transgender people living with HIV [16, 18–20]. The integration of the Model of Gender Affirmation with the Healthcare Empowerment Model results in a powerful and innovative conceptual framework for exploring intervention-amenable factors that affect health outcomes from a perspective that is grounded in the unique cultural context of transgender women living with HIV.
The purpose of this paper is to present support for the construct of gender affirmation in the context of HIV-related health outcomes, with a particular emphasis on evaluating whether the adapted Model of Gender Affirmation fits the data from a large sample of transgender women of color living with HIV.
Methods
In 2012, the Health Resources and Services Administration, Special Projects of National Significance, funded the initiative Enhancing Engagement and Retention in Quality HIV Care for Transgender Women of Color. Nine demonstration projects (four at community sites and five at clinical sites) in four urban centers (New York, Los Angeles, San Francisco Bay Area, and Chicago) were selected to develop and implement innovative interventions to engage and retain transgender women of color living with HIV in quality HIV care. An additional organization was funded to provide technical assistance to the demonstration projects and perform a multisite evaluation of the nine interventions. Details regarding the initiative and the interventions have been previously published [21].
The demonstration sites designed their own recruitment strategies to reach and enroll participants into their interventions. These strategies included community outreach, networking, word-of-mouth, publicity materials, and referrals from clinics and other service providers. To be eligible, one had to be 16 years or older, assigned male sex at birth, identify as transgender or female, diagnosed with HIV, and be fluent in English or Spanish. Enrolled individuals provided informed consent before participating in the study.
Before receiving the intervention, the participants visited the study site and took a self-administered baseline survey in REDCap [22] in the language of their choosing, either English or Spanish. As needed, sites had the option to have an interviewer administer the survey. The survey inquired about participants’ HIV care, health-related behaviors, and barriers and facilitators to care and is the source of the data for the present analyses. To compensate for their time and willingness to take the survey, participants received incentives that varied between $25 and $50 across sites. The study was approved by the local Institutional Review Board at each of the demonstration sites as well as at the evaluation center.
Measures
Participants reported several demographic characteristics including age, race and ethnicity, and education.
Healthcare empowerment was measured using the 4-item ICCE (informed, committed, collaborative, engaged) subscale of the Healthcare Empowerment Inventory [16]. The Likert-type response options ranged from 1 (strongly disagree) to 5 (strongly agree) with higher scores indicating greater healthcare empowerment. Sample item: ‘I try to get my healthcare providers to listen to my preferences for my treatment’; Cronbach alpha: 0.95.
Access to gender affirmation in healthcare was measured among participants who reported having ever received HIV primary care (see Online Appendix A). It was calculated as the mean score of 12 items developed for this purpose. The Likert-type response options range from 1 (least gender-affirming HIV care) to 5 (most gender-affirming HIV care) with higher scale scores indicating more gender-affirming HIV care. Sample item ‘During your last HIV medical appointment, how welcoming was your medical care provider’s waiting room for trans women?’ with response options ranging from 1 (not welcoming at all) to 5 (extremely welcoming); Cronbach alpha: 0.88.
Need for gender affirmation was measured by a 5-item measure developed specifically to measure this construct (see Appendix B). The items utilize Likert-type response options ranging from 1 (lowest need) to 5 (highest need). Higher mean scores indicate a greater need for gender affirmation. Sample item: ‘How important is it to you that strangers call you “she” when talking about you?’ with response options 1 (not at all important) to 5 (extremely important); Cronbach alpha: 0.95.
Satisfaction with gender affirmation was measured using 5 items developed specifically to measure this construct (see Online Appendix B). The items utilize Likert-type response options ranging from 1 (lowest satisfaction) to 5 (highest satisfaction). Higher mean scores indicate greater satisfaction with gender affirmation. Sample item: ‘How satisfied are you with your current level of femininity?’ with response options 1 (not at all satisfied) to 5 (extremely satisfied); Cronbach alpha: 0.87.
Experiences of transgender-related discrimination in the previous 6 months were recorded using five items—discrimination from doctor or healthcare professional, denial of job, denial of health insurance, denial of housing opportunity and denial of bed in a homeless shelter [23]. The response options ranged from 0 (never) to 4 (many times). The response to each item was dichotomized into 0 (never) and 1 (at least once) mirroring the strategy used by the authors of the items. Sample item: ‘How many times in the last 6 months have you lost housing or been denied a housing opportunity because you are transgender?’ These five items were used to measure the latent construct of transgender-related discrimination in the structural model.
Participants were categorized as being virally suppressed if their viral load had been tested in the previous 6 months and they self-reported having an undetectable viral load at the last test (using survey item: What is the result of your most recent viral load test? Response options: detectable, undetectable). Thus, viral suppression was a binary variable (1: virally suppressed; 0: not virally suppressed).
Data Analysis
We studied the missing data patterns in the variables of interest, as participants were allowed to decline to answer questions and some participants did not complete their survey. We found that 35 participants had not responded to any of the items that measured transgender-related discrimination, gender affirmation, and healthcare empowerment. These participants were dropped from the analyses. Descriptive statistics for the sample were then generated using SAS V9.4 software [24]. All further analyses were performed in Mplus 8 [25]. We then used structural equation modeling (SEM) to test the direct as well as indirect effects of transgender-related discrimination, gender affirmation and healthcare empowerment on viral suppression (Fig. 1). Transgender-related discrimination was modeled as a latent variable measured by the five binary items described in “Measures” section above. The latent variable gender affirmation was measured by: need for gender affirmation, satisfaction with gender affirmation, and access to gender affirmation in healthcare. Based on previous findings in literature, sociodemographic characteristics of age, race/ethnicity and education were also included in the hypothesized model.
Fig. 1.
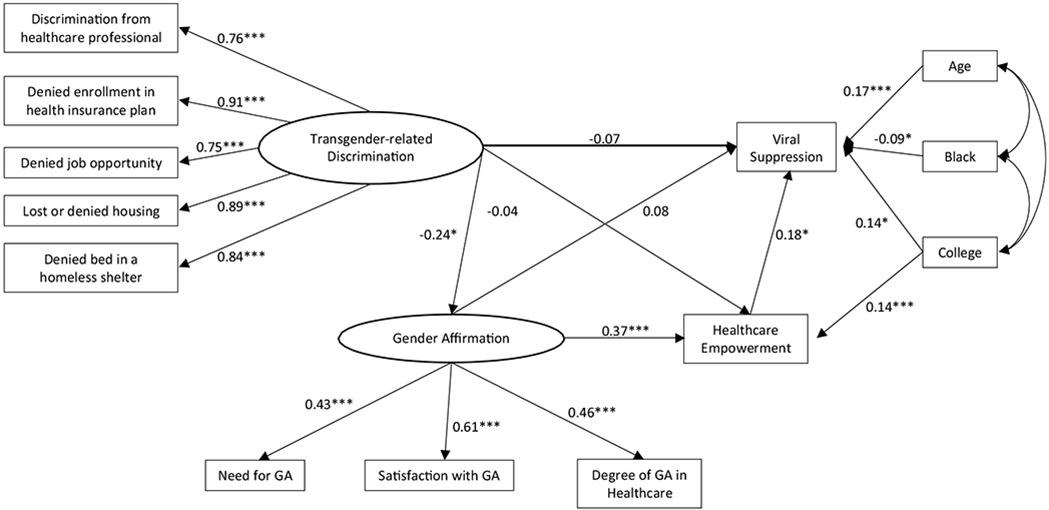
Structural equation model for transgender women of color living with HIV, depicting paths and standardized estimates among transgender-related discrimination, gender affirmation, healthcare empowerment and viral suppression (N = 823). The coefficients on the arrows from ‘transgender-related discrimination’ to each form of discrimination, and from ‘gender affirmation’ to its constituents, are the standardized factor loadings of each item on to the latent factor. *p < 0.05, ***p < 0.001 for coefficients
We used multiple imputation to create 50 complete datasets to handle the missing data, assumed to be missing-at-random (MAR). The SEM was fit using the two-stage process [26]. In the first stage, the measurement model was fit to ensure satisfactory measurement of the constructs. This was done by evaluating the relationship between each latent factor and its constituent observed variables, the correlations among the constructs and the overall model fit. In the second stage, the full hypothesized structural model was tested with an emphasis on the direct and indirect paths between constructs and the model fit. Diagonally weighted least squares estimation suitable for binary and ordinal data was used due to the presence of categorical variables (Mplus estimator WLSMV) [27]. In both stages, for both the latent factors, their measurement scale was determined by fixing the first constituent observed variable’s factor loading to 1.00. We report both unstandardized regression coefficients (B) and standardized regression coefficients (β) for each effect. At each stage, exact model-data fit was evaluated by the Chi square test of exact fit. Because the Chi square test is sensitive to trivial departures from perfect model-data fit [28], the approximate model fit was assessed using Bentler’s [29] Comparative Fit Index (CFI), the root mean square error of approximation (RMSEA), and the weighted root mean square residual (WRMR). The model is said to fit the data on an approximate basis if two of the following three conditions are met: CFI ≥ 0.95, RMSEA < 0.06, and WRMR < 1.00 [30, 31].
Results
Between December 2013 and August 2016, the nine demonstration sites recruited a total of 858 transgender women of color living with HIV. After removing 35 individuals’ data (see “Data Analysis” section above) from the total sample, the current analysis dataset consisted of 823 women. The average age was 37 years (Table 1). Approximately half (49%) were Hispanic/Latina, 42% were Black and 8% reported their race–ethnicity as one of American Indian/Alaska native, Asian/Pacific Islander or multi-racial. Less than a quarter of the sample (22%) indicated some college education and three quarters reported annual incomes less than the Federal Poverty Level ($11,490). Sources of transgender-related discrimination varied; 131 participants (16%) reported being denied health insurance and 302 participants (37%) reported being denied a job.
Table 1.
Descriptive characteristics of participants (N = 823)
| Demographic characteristics | ||
| Age [in years; mean (SD)] | 37.4 | (10.8) |
|
| ||
| n | (%) | |
|
| ||
| Race–ethnicity | ||
| Hispanic, Latina or of Spanish origin | 406 | (49) |
| Black, non-Hispanic | 349 | (42) |
| Other, non-Hispanic | 68 | (8) |
| Education: at least some college or higher | 183 | (22) |
| Study measures | ||
| Viral suppression | 303 | (37) |
| Experiences of discrimination in past 6 months | ||
| Discrimination from doctor or healthcare professional | 191 | (23) |
| Denied enrollment in health insurance plan | 131 | (16) |
| Denied a job opportunity | 302 | (37) |
| Lost or denied housing | 232 | (28) |
| Denied bed in a homeless shelter | 190 | (23) |
|
| ||
| Mean | Std Dev | |
|
| ||
| Need for gender affirmation | 3.98 | (1.2) |
| Satisfaction with gender affirmation | 3.45 | (1.1) |
| Degree of gender affirmation in healthcare | 3.75 | (0.8) |
| Healthcare empowerment | 3.87 | (1.1) |
Measurement Model
In the measurement model, all factor loadings between the latent factors and their observed variables were significant at p < 0.001. Transgender-related discrimination was negatively correlated with gender affirmation, healthcare empowerment and viral suppression (Table 2). Viral suppression, gender affirmation and healthcare empowerment were positively correlated with each other. All factor intercorrelations were significant (p < 0.01), except between transgender-related discrimination and viral suppression (p = 0.064). The measurement model fit the data satisfactorily: χ2(60) = 190.10; CFI = 0.95, RMSEA = 0.05; WRMR = 1.38.
Table 2.
Correlation matrix of measurement model latent factors and viral suppression
| Measure | 1. Discrimination | 2. Gender affirmation | 3. Health care empowerment | 4. Viral suppression |
|---|---|---|---|---|
| 1. Discrimination | 1.00 | |||
| 2. Gender affirmation | −0.24*** | 1.00 | ||
| 3. Health care empowerment | −0.12** | 0.39*** | 1.00 | |
| 4. Viral suppression | −0.09 | 0.17** | 0.25*** | 1.00 |
N = 823. Correlations were generated in Mplus 8 (Mplus estimator WLSMV)
p < 0.01;
p < 0.001
Structural Model
The structural model with the estimated standardized path coefficients is illustrated in Fig. 1. The results presented are those averaged over the 50 imputed datasets. The estimates and standard errors for each measurement and structural path is shown in Table 3. Significant positive direct effects were observed from gender affirmation to healthcare empowerment and healthcare empowerment to viral suppression. A significant negative direct effect was observed from transgender-related discrimination to gender affirmation. The only three non-significant direct effects in the structural model were from transgender-related discrimination to healthcare empowerment and viral suppression and from gender affirmation to viral suppression. With regards to the sociodemographic control variables, while age and education demonstrated significant positive direct effects on viral suppression, being Black showed a significant negative direct effect. The total indirect effect from discrimination to viral suppression was significant (B = − 0.06, p = 0.03, β = − 0.04). The specific indirect effect from discrimination to viral suppression via gender affirmation and healthcare empowerment was significant (B = − 0.02, p = 0.02, β = − 0.02), whereas the specific indirect effects from discrimination to viral suppression via gender affirmation (B = − 0.03, p = 0.27, β = − 0.02) and from discrimination to viral suppression via healthcare empowerment were both non-significant (B = − 0.009, p = 0.42, β = − 0.007). The indirect effect from gender affirmation to viral suppression via healthcare empowerment was also significant (B = 0.13, p = 0.003, β = 0.07). Therefore, in the present hypothesized model, while the variability in viral suppression (R-square = 0.13) can be explained by the direct influence of healthcare empowerment, it can also be explained by gender affirmation via healthcare empowerment and by transgender-related discrimination via gender affirmation and healthcare empowerment together. In fact, gender affirmation in combination with healthcare empowerment significantly and fully mediated the total effect of transgender-related discrimination on viral suppression. The model fit the data well: χ2(57) = 160.76; RMSEA = 0.047, CFI = 0.958, WRMR = 1.307.
Table 3.
Unstandardized estimates, standard errors, and standardized estimates for structural equation model of experiences of transgender discrimination, gender affirmation, healthcare empowerment and viral suppression (N = 823)
| Outcome variable | Explanatory variable | B | S.E. | β |
|---|---|---|---|---|
| Measurement coefficients | ||||
| D1. Discrimination from doctor or healthcare professional | Discrimination | 1.000 | – | 0.762 |
| D2. Denied enrollment in health insurance plan | Discrimination | 1.188*** | 0.062 | 0.905 |
| D3. Denied job opportunity | Discrimination | 0.985*** | 0.055 | 0.750 |
| D4. Lost or denied housing | Discrimination | 1.163*** | 0.057 | 0.885 |
| D5. Denied bed in a homeless shelter | Discrimination | 1.101*** | 0.056 | 0.839 |
| GA1. Need for gender affirmation | Gender Affirmation | 1.000 | – | 0.430 |
| GA2. Satisfaction with gender affirmation | Gender Affirmation | 1.250*** | 0.186 | 0.614 |
| GA3. Degree of gender affirmation in healthcare | Gender Affirmation | 0.731*** | 0.152 | 0.455 |
| Structural coefficients—direct effects | ||||
| Gender affirmation | Discrimination | −0.162* | 0.047 | −0.239 |
| Healthcare empowerment | Discrimination | −0.054 | 0.067 | −0.037 |
| Healthcare empowerment | Gender affirmation | 0.81*** | 0.140 | 0.372 |
| Viral suppression | Gender affirmation | 0.169 | 0.148 | 0.084 |
| Viral suppression | Discrimination | −0.088 | 0.073 | −0.065 |
| Healthcare empowerment | Education | 0.379*** | 0.099 | 0.140 |
| Viral suppression | Healthcare empowerment | 0.164* | 0.048 | 0.179 |
| Viral suppression | Age | 0.016*** | 0.004 | 0.165 |
| Viral suppression | Black | −0.187* | 0.094 | −0.089 |
| Viral suppression | Education | 0.353* | 0.106 | 0.142 |
| Structural coefficients—indirect effects | ||||
| Total indirect: D → VS | −0.058* | 0.026 | −0.043 | |
| Specific indirect | ||||
| D → GA → HCE → VS | −0.022* | 0.010 | −0.016 | |
| D → GA → VS | −0.027 | 0.025 | −0.020 | |
| D → HCE → VS | −0.009 | 0.011 | −0.007 | |
| Total and specific indirect: GA → HCE → VS | 0.133* | 0.045 | 0.066 | |
Estimates and associated statistics were generated in Mplus 8 (Mplus estimator WLSMV) based on 50 imputed datasets
D discrimination, GA gender affirmation, HCE healthcare empowerment, VS viral suppression, B unstandardized regression coefficient, SE standard error of B, β standardized regression coefficient
p < 0.05;
p < 0.001
Discussion
Our findings provide support for an adapted Model of Gender Affirmation with a large sample of transgender women of color in the US living with HIV. We found that gender affirmation in combination with healthcare empowerment significantly and fully mediated the total effect of transgender-related discrimination on viral suppression; that is, the negative association between transgender-related discrimination and viral suppression can be explained by the direct influence of gender affirmation and healthcare empowerment. Thus, when participants reported experiencing transgender-related discrimination, viral suppression was more likely to be achieved when higher levels of gender affirmation and healthcare empowerment were also reported.
When the Model of Gender Affirmation was first proposed, it was conceptualized as having two distinct dimensions—need for gender affirmation and access to gender affirmation—which were hypothesized to vary independently. In the final model presented here, gender affirmation was measured by a latent variable with three observed indicators—need for gender affirmation, satisfaction with gender affirmation, and access to transgender-competent care. All three variables were positively associated with one another. In contrast to previous research, we found support for the hypothesis that experiences of discrimination are negatively associated with healthcare empowerment. This finding may be attributable to the larger sample size we attained compared to previous studies that did not detect this association [32].
It has been extensively documented that discrimination in healthcare settings is a major barrier to achieving and maintaining viral suppression among transgender women [23, 33]. In addition, our model provides evidence that discrimination from other sources such as employment, health insurance and housing also impact viral suppression. The pervasive discrimination that transgender women experience regularly, and from multiple sources, creates intersecting structural barriers that result in persistent health disparities. From a clinical perspective, our findings suggest that gender-affirming and empowering care from a knowledgeable and culturally competent provider is important to interrupt this association between transgender-related discrimination and negative health outcomes.
Gender affirmation on its own did not lead directly to viral suppression indicating that the context of empowerment within healthcare is important for affirmation to result in improved HIV-related health outcomes. The impact of lack of empowerment within healthcare on health outcomes may be difficult to overcome even in the context of gender affirmation. Social and behavioral interventions designed to increase access to gender affirmation and healthcare empowerment may improve rates of viral suppression among transgender women of color living with HIV.
Strengths of this study include the use of data from a large national study of transgender women of color living with HIV in which recruitment occurred at both clinical and non-clinical urban sites. However, enrollment was limited to transgender women of color by design and the sample was predominantly low-income; therefore, findings cannot be directly generalized to transgender women from rural areas, those who are White, or those have a higher socioeconomic status. Because this study utilized a convenience sample and cross-sectional analyses, no causal inferences can be drawn. Further, this study used measures of gender affirmation that have not yet been validated; future research will seek to validate these scales.
These data provide empirical evidence to support the Model of Gender Affirmation, which lays the conceptual foundation for intervention development to improve health outcomes among transgender women of color living with HIV. Gender affirmation and healthcare empowerment are important components of any health promotion intervention that seeks to improve health outcomes among transgender women living with HIV.
Supplementary Material
Acknowledgements
This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number U90HA24973 in the amount of $536,244 awarded to the University of California at San Francisco. No percentage of this project was financed with non-governmental sources. This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government. We would also like to thank our participants and the survey administration staff at each of the demonstration sites. Dr. Johnson’s contribution to this manuscript was supported by NIDA K24DA037034.
Footnotes
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s10461-019-02544-2) contains supplementary material, which is available to authorized users.
References
- 1.Baral SD, et al. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13(3):214–22. [DOI] [PubMed] [Google Scholar]
- 2.James SE, et al. The report of the 2015 US transgender survey. Washington, DC: National Center for Transgender Equality; 2016. [Google Scholar]
- 3.Reisner SL, et al. Discriminatory experiences associated with posttraumatic stress disorder symptoms among transgender adults. J Couns Psychol. 2016;63(5):509–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilson EC, et al. The impact of discrimination on the mental health of trans*female youth and the protective effect of parental support. AIDS Behav. 2016. 10.1007/s10461-016-1409-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.White Hughto JM, Reisner SL, Pachankis JE. Transgender stigma and health: a critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med. 2015;147:222–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colton Meier SL, et al. The effects of hormonal gender affirmation treatment on mental health in female-to-male transsexuals. J Gay Lesbian Mental Health. 2011;15(3):281–99. [Google Scholar]
- 7.Bockting WO, et al. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health. 2013. 10.2105/AJPH.2013.301241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sevelius J Gender affirmation: a framework for conceptualizing risk behavior among transgender women of color. Sex Roles. 2013;68(11–12):675–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nuttbrock L, et al. Gender identity affirmation among male-to-female transgender persons: a life course analysis across types of relationships and cultural/lifestyle factors. Sex Relatsh Therapy. 2009;24(2):108–25. 10.1080/14681990902926764. [DOI] [Google Scholar]
- 10.Bockting W, et al. Adult development and quality of life of transgender and gender nonconforming people. Curr Opin Endocrinol Diabetes Obes. 2016;23(2):188–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nemoto T, et al. Social context of HIV risk behaviors among male-to-female transgenders of color. AIDS Care. 2004;16:724–35. [DOI] [PubMed] [Google Scholar]
- 12.Nuttbrock L, Rosenblum A, Blumenstein R. Transgender identity affirmation and mental health. Int J Transgenderism, 2002;6(4). [Google Scholar]
- 13.Major B, O’Brien L. The social psychology of stigma. Annu Rev Psychol. 2005;56:393–421. [DOI] [PubMed] [Google Scholar]
- 14.Sevelius J, Johnson M. Preliminary support for transgender-specific predictors of uptake and adherence to ART and viral load among HIV+ transgender women. In: 8th international conference on HIV treatment and prevention adherence. International Association of Providers in AIDS Care; 2013. [Google Scholar]
- 15.Sevelius J, Johnson M. A qualitative investigation of barriers to treatment initiation and engagement among transgender women living with HIV. In: 8th international conference on HIV treatment and prevention adherence. Miami Beach: International Association of Providers in AIDS Care; 2013. [Google Scholar]
- 16.Johnson MO, et al. Advances in the conceptualization and measurement of health care empowerment: development and validation of the health care empowerment inventory. PLoS ONE. 2012;7(9):e45692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson MO. The shifting landscape of health care: toward a model of health care empowerment. Am J Public Health. 2011;101(2):265–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson MO, et al. Preliminary support for the construct of health care empowerment in the context of treatment for human immunodeficiency virus. Patient Prefer Adher. 2012;6:395–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilson TE, et al. Healthcare empowerment and HIV viral control: mediating roles of adherence and retention in care. Am J Prev Med. 2018;54(6):756–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van den Berg JJ, et al. Using path analysis to evaluate the healthcare empowerment model among persons living with HIV for antiretroviral therapy adherence. AIDS Patient Care STDs. 2016;30(11):497–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rebchook G, et al. The transgender women of color initiative: implementing and evaluating innovative interventions to enhance engagement and retention in HIV care. Am J Public Health. 2017;107(2):224–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harris PA, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bradford J, et al. Experiences of transgender-related discrimination and implications for health: results from the Virginia Transgender Health Initiative Study. Am J Public Health. 2013;103(10):1820–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.SAS Institute. SAS on-line doc version 9.0. Cary: SAS Institute Inc.; 2002. [Google Scholar]
- 25.Muthén LK, Muthén BO. MPlus software. Muthén & Muthén: Los Angeles; 1998-2017. [Google Scholar]
- 26.Anderson JC, Gerbing DW. Structural equation modeling in practice: a review and recommended two-step approach. Psychol Bull. 1988;103(3):411. [Google Scholar]
- 27.Flora DB, Curran PJ. An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychol Methods. 2004;9(4):466–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bollen KA, Long JS. Introduction. Testing structural equation models. Newbury Park: Sage Publications; 1993. p. 1–9. [Google Scholar]
- 29.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107(2):238. [DOI] [PubMed] [Google Scholar]
- 30.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model: Multidiscip J. 1999;6(1):1–55. [Google Scholar]
- 31.Yu CY. Evaluating cutoff criteria of model fit indices for latent variable models with binary and continuous outcomes, in [Doctoral Dissertation]. Los Angeles: University of California; 2002. [Google Scholar]
- 32.Johnson M, et al. Preliminary support for the construct of health care empowerment in the context of treatment for human immunodeficiency virus. Patient Prefer Adher. 2012;6(1):395–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Safer JD, et al. Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016;23(2):168–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


