Abstract
Background:
Few population-based studies have examined incidence and mortality of cancers of the biliary tract, including intrahepatic bile duct, extrahepatic bile duct, ampulla of Vater, and overlapping or other lesion of the biliary tract in one study.
Methods:
To further the understanding of recent rates of biliary tract cancers, we used population-based data, to examine incidence and mortality during 2013–2017. We examined how rates varied by sex, age, race/ethnicity, U.S. census region, and stage at diagnosis.
Results:
Intrahepatic bile duct was the most common biliary tract cancer with an incidence rate of 1.49 per 100,000 persons. Cancer incidence rates per 100,000 persons were 0.96 for extrahepatic bile duct, 0.45 for ampulla of Vater, and 0.24 for overlapping or other lesion of the biliary tract. Cancer death rates per 100,000 persons were 1.66 for intrahepatic bile duct and 0.45 for other biliary tract. Intrahepatic bile duct incidence and death rates were higher among males than females, higher among Hispanic and Asian and Pacific Islander persons compared to non-Hispanic Whites, and higher in the Northeast and in urban counties.
Conclusion:
This report provides national estimates of these rare biliary tract cancers.
Impact:
Key interventions targeted to high-risk populations may help reduce incidence and mortality of cancers of the biliary tract by improving primary prevention through strategies to reduce tobacco and alcohol use, control overweight and obesity, and promote hepatitis B vaccination and use of syringe service programs meant to curb the transmission of infectious diseases such as viral hepatitis.
Keywords: rare cancers, epidemiology, cancer surveillance
Introduction
Cancer of the biliary tract arises from the biliary epithelium of the small ducts in the periphery of the liver (intrahepatic) and the main ducts of the hilum (extrahepatic).1 Extrahepatic biliary tract cancers include the ampulla of Vater, overlapping lesion of the biliary tract, and “biliary tract, Not Otherwise Specified (NOS),” in addition to the gallbladder and pancreatic biliary ducts.1 These cancers are all rare and are often diagnosed at late stage disease with poor prognosis.2
Risk factors for cancers of the biliary tract vary by anatomic site, and differences in incidence and death rates may be observed.3 Known risk factors for intrahepatic and extrahepatic bile duct cancer include primary sclerosing cholangitis and inflammatory bowel disease.4 Primary sclerosing cholangitis (PSC) is an autoimmune disease that results in structuring of extrahepatic and/or intrahepatic bile ducts.5 Some studies have identified obesity, diabetes, heavy alcohol use, and smoking as risk factors for intrahepatic and extrahepatic bile duct cancer as well.6 Hepatitis B virus (HBV) and/or hepatitis C virus (HCV) infection, cirrhosis of the liver, and duodenal and gastric ulcers have also been associated with bile duct cancer.6
Gallbladder cancer is a rare, lethal cancer and is the most common type of biliary tract malignancy.7 In the United States, women have higher incidence and death rates of gallbladder cancer than men.8 Risk factors for gallbladder cancer include a personal or family history of gallstones, obesity, chronic infection and inflammation in the gallbladder, and ill-defined genetic variants.2 While many liver cancer cases are related to HBV and HCV infections, other behaviors and conditions that increase the risk of developing liver cancer include obesity, tobacco use, excessive alcohol use, diabetes, and nonalcoholic fatty liver diseases, including nonalcoholic steatohepatitis.9,10
As previous studies have noted, studies often examine specific biliary tract cancer types, such as only gallbladder cancer, intrahepatic bile duct cancer combined with liver cancer, or examined biliary tract cancers with all anatomic sites combined.3,11 Therefore, calculations of incidence rates for cancers of the biliary tract do not always present rates for each site individually.12 To further the understanding of recent rates of biliary tract cancer, we used data from the U.S. Cancer Statistics (USCS), covering the entire U.S. population, to examine incidence and mortality during 2013–2017. We examined how site-specific rates varied by sex, age, race/ethnicity, U.S. Census region, and stage of disease at diagnosis.
Methods
Data Sources
Cancer Incidence Data.
Population-based incidence data are from the USCS, which combines Centers for Disease Control and Prevention’s (CDC’s) National Program of Cancer Registries (NPCR) and National Cancer Institute’s (NCI) Surveillance, Epidemiology, and End Results Program (SEER) datasets.13 This combined dataset includes cancer incidence data from central cancer registries reporting to NPCR or SEER from all states and the District of Columbia. Data about all new diagnoses of cancer from patient records at medical facilities such as hospitals, physicians’ offices, therapeutic radiation facilities, freestanding surgical centers, and pathology laboratories are reported to central cancer registries, which collate these data and use state vital records to collect information about any cancer deaths that were not reported as cases. Incidence data met USCS publication criteria, covering 100% of the U.S. population during 2013–2017.13
We selected all malignant cases of biliary tract cancer defined using International Classification of Diseases for Oncology, Third Edition (ICD-O-3) diagnosed during 2013–2017.14 We selected topography codes C22.1 for intrahepatic cancers, C24.0 for extrahepatic cancers including distal bile duct and perihilar bile ducts, C24.1 for ampulla of Vater cancer, and combined C24.8 (overlapping) and C24.9 (NOS) for overlapping and other lesions of biliary tract. Liver cancers with ICD-O-3 topography code C22.0 and histology codes 8160, 8161, 8180 were included as intrahepatic cancers as they are believed to be intrahepatic in origin.15 Klatskin tumors with ICD-O-3 topography code C22.0 and histology code 8162 were classified as extrahepatic cancers.15 Incidence data on liver cancer (C22.0 excluding histology codes 8160, 8161, 8180) and gallbladder cancer (C23.9) were examined as supplemental data as they are often grouped as being a part of the biliary tract.3
Mortality Data.
Mortality data during 2013–2017 are from CDC’s National Center for Health Statistics’ National Vital Statistics System.16 Although more recent mortality data are available, we used data collected from 2013–2017 to be consistent with the most recent incidence data available. The International Classification of Diseases and Related Health Problem 10th Revision was used to define deaths codes attributed to intrahepatic bile duct cancer (C22.1), other biliary tract cancers (C24), liver cancer (C22.0), and gallbladder cancer (C23).17
Population.
Age-specific analyses used these grouped categories: 0–49, 50–59, 60–69, 70–79, and ≥ 80 years. Youngest age group consisted of individuals aged 0–49 years due to small case counts.
Race and ethnicity.
Race and Hispanic ethnicity data were collected separately and combined in this analysis. To be compatible with available annual population estimates used a denominators for the rates, we used standard methods to categorize race into 4 groups (White, Black, American Indian/Alaska Native, and Asian or Pacific Islander).18 Cases with unknown race were included in the “All Races” category but were not inlcuded as separate category because population estimate is not available for unknown race. Then we combined race and ethnicity information for five racial/ethnic groups: non-Hispanic White, non-Hispanic Black, non-Hispanic American Indian/Alaska Native, non-Hispanic Asian/Pacific Islander, and Hispanic including all races.
Region.
States were grouped into four regions defined by the U.S. Census Bureau: Northeast, Midwest, South, and West.19
Rural-urban status.
The U.S. Department of Agriculture Economic Research Service 2013 vintage rural-urban continuum classification scheme was used to categorize county of residence at diagnosis as metropolitan (rural-urban continuum codes 1–3) or nonmetropolitan (rural-urban continuum codes 4–9).20
Stage of disease at diagnosis.
Stage was classified using SEER Summary Stage 2000 for diagnosis years 2001–2003 and 2016–2017, Derived SEER Summary Stage 2000 for diagnosis years 2004–2014, and either SEER Summary Stage 2000 or Derived SEER Summary Stage 2000 for diagnosis year 2015.21 Even though different staging schema were used during the study time period, rules and staging criteria were the same characterizing cancers as localized, regional, distant, or unknown stage. Analyses by stage excluded cases that were diagnosed only by death certificate or autopsy (4.7% of cases).
Statistical Methods
Incidence and mortality rates.
We calculated overall average annual age-adjusted incidence rates (IR) and mortality rates (MR) using SEER*Stat 8.3.6.22 Average annual rates for 2013–2017 per 100,000 persons were age adjusted by the direct method to the 2000 U.S. standard population.23 Corresponding 95% confidence intervals (CIs) were calculated, using the Tiwari method, as modified gamma intervals.24 To determine differences between subgroups, incidence and mortality rate ratios (IRR and MRR, respectively) were calculated; rates were considered statistically different if the 95% CIs of the rate ratios excluded one.25 Rates and rate ratios were calculated by sex, age group, race/ethnicity, geographic region, and stage. Statistical differences were not calculated for stage.
Results
Incidence
During 2013–2017, there were 28,343 intrahepatic bile duct cancer cases, 18,075 extrahepatic bile duct cancer cases, 10,382 ampulla of Vater cancer cases, and 4,540 cancers of overlapping and other lesions of the biliary tract (Table 1) reported in the United States. Intrahepatic bile duct was the most common site for biliary tract cancers with an incidence rate of 1.49 per 100,000 persons. Incidence rate of extrahepatic bile duct cancer was 0.96 per 100,000 persons. Cancers of the ampulla of Vater and overlapping and other lesions of the biliary tract were rare with an incidence rate of 0.45 and 0.24 per 100,000 persons, respectively. Compared to females, males had higher incidence of intrahepatic bile duct cancer (IR =1.69 per 100,000; IRR 1.27, 95% CI 1.24–1.30), extrahepatic bile duct cancer (IR =1.19 per 100,000; IRR 1.50, 95% CI 1.45–1.55), ampulla of Vater cancer (IR = 0.70 per 100,00; IRR 1.56, 95% CI 1.50–1.62), and cancer of overlapping and other lesions of the biliary tract (IR = 0.26 per 100,000; IRR 1.18, 95% CI 1.11–1.26).
Table 1.
Average age-adjusted incidence ratesa in cancer of the biliary tract, gallbladder, and liver by sex, age, race/ethnicity, and region- United Statesb 2013–2017
| Intrahepatic Bile Duct | Extrahepatic Bile Duct | Ampulla of Vater | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | n | IR (95% CI) | IRR (95% CI) | n | IR (95% CI) | IRR (95% CI) | n | IR (95% CI) | IRR (95% CI) |
|
| |||||||||
| Total | 28,343 | 1.49 (1.47–1.51) | 18,075 | 0.96 (0.95–0.98) | 10,382 | 0.45 (0.44–0.46) | |||
| Sex | |||||||||
| Female | 13,598 | 1.33 (1.31–1.35) | 1.00 (referent) | 8,131 | 0.78 (0.76–0.80) | 1.00 (referent) | 4,556 | 0.45 (0.43–0.46) | 1.00 (referent) |
| Male | 14,745 | 1.69 (1.66–1.72) | 1.27 (1.24–1.30)f | 9,944 | 1.19 (1.17–1.22) | 1.50 (1.45–1.55)f | 5,826 | 0.70 (0.68–0.71) | 1.56 (1.50–1.62)f |
| Race-ethnicity | |||||||||
| White, non-Hispanic | 20,823 | 1.47 (1.45–1.49) | 1.00 (referent) | 12,953 | 0.91 (0.89–0.92) | 1.00 (referent) | 7,287 | 0.51 (0.50–0.53) | 1.00 (referent) |
| Black, non-Hispanic | 2,660 | 1.36 (1.31–1.41) | 0.93 (0.89–0.97)f | 1,770 | 0.96 (0.92–1.01) | 1.06 (1.01–1.12)f | 993 | 0.53 (0.49–0.56) | 1.03 (0.96–1.10) |
| American Indian/Alaska Native, non-Hispanic | 171 | 1.40 (1.19–1.63) | 0.95 (0.81–1.11) | 126 | 1.07 (0.88–1.28) | 1.18 (0.97–1.42) | 66 | 0.58 (0.45–075) | 1.14 (0.87–1.46) |
| Asian or Pacific Islander, non-Hispanic | 1,497 | 1.69 (1.65–1.78) | 1.15 (1.09–1.21)f | 1,140 | 1.35 (1.27–1.43) | 1.49 (1.40–1.59)f | 653 | 0.74 (0.68–0.80) | 1.43 (1.32–1.56)f |
| Hispanic | 3,057 | 1.72 (1.65–1.78) | 1.17 (1.12–1.22)f | 1,995 | 1.20 (1.15–1.26) | 1.33 (1.26–1.39)f | 1,323 | 0.76 (0.72–0.81) | 1.49 (1.40–1.58)f |
| Age (yrs) | |||||||||
| 0–49 | 2,042 | 0.21 (0.20–0.21) | 1.00 (referent) | 865 | 0.09 (0.08–0.09) | 1.00 (referent) | 680 | 0.07 (0.06–0.07) | 1.00 (referent) |
| 50–59 | 4,927 | 2.18 (2.11–2.24) | 10.60 (10.06–11.17)f | 2,340 | 1.03 (0.99–1.08) | 11.93 (11.03–12.92)f | 1,624 | 0.73 (0.69–0.76) | 10.56 (9.64–11.57)f |
| 60–69 | 8,826 | 5.08 (4.97–5.18) | 24.73 (23.57–25.97)f | 4,751 | 2.74 (2.66–2.81) | 31.55 (29.33–33.97)f | 2,776 | 1.60 (1.54–1.66) | 23.27 (21.39–25.35)f |
| 70–79 | 7,637 | 7.81 (7.63–7.99) | 38.06 (36.23–39.99)f | 5,287 | 5.44 (5.29–5.59) | 62.73 (58.35–67.51)f | 2,962 | 3.04 (2.93–3.16) | 44.33 (40.76–48.27)f |
| ≥80 | 4,911 | 8.17 (7.94–8.40) | 39.80 (37.78–41.94)f | 4,832 | 7.97 (7.75–8.20) | 91.95 (85.49–98.99)f | 2,340 | 3.90 (3.75–4.07) | 56.85 (52.15–62.03)f |
| Region | |||||||||
| Northeast | 5,991 | 1.71 (1.66–1.75) | 1.00 (referent) | 3,828 | 1.09 (1.06–1.13) | 1.00 (referent) | 2,065 | 0.59 (0.57–0.62) | 1.00 (referent) |
| South | 6,422 | 1.57 (1.53–1.61) | 0.92 (0.89–0.95)f | 3,820 | 0.93 (0.90–0.96) | 0.85 (0.82–0.89)f | 2,275 | 0.56 (0.54–0.58) | 0.95 (0.89–1.01) |
| Midwest | 10,249 | 1.44 (1.41–1.47) | 0.84 (0.82–0.87)f | 6,202 | 0.88 (0.86–0.91) | 0.81 (0.78–0.84)f | 3,615 | 0.52 (0.50–0.54) | 0.88 (0.83–0.93)f |
| West | 5,681 | 1.34 (1.30–1.38) | 0.79 (0.76–0.81)f | 4,225 | 1.02 (0.98–1.05) | 0.93 (0.89–0.97)f | 2,427 | 0.59 (0.56–0.61) | 0.99 (0.93–1.05) |
| Rural/urban | |||||||||
| Urban | 24,060 | 1.55 (1.53–1.57) | 1.00 (referent) | 15,277 | 1.00 (0.99–1.02) | 1.00 (referent) | 8,783 | 0.58 (0.57–0.59) | 1.00 (referent) |
| Rural | 4,277 | 1.43 (1.39–1.47) | 0.92 (0.89–0.95)f | 2,796 | 0.92 (0.89–0.96) | 0.92 (0.88–0.96)f | 1,597 | 0.54 (0.51–0.56) | 0.93 (0.88–0.98)f |
|
| |||||||||
| Overlapping and other lesions of biliary tract | Gallbladder | Liver | |||||||
| Characteristic | n | IR (95% CI) | IRR (95% CI) | n | IR (95% CI) | IRR (95% CI) | n | IR (95% CI) | IRR (95% CI) |
|
| |||||||||
| Total | 4,540 | 0.24 (0.23–0.25) | 20,709 | 1.11 (1.09–1.12) | 140,364 | 7.06 (7.02–7.10) | |||
| Sex | |||||||||
| Female | 2,313 | 0.22 (0.21–0.23) | 1.00 (referent) | 13,976 | 1.35 (1.33–1.38) | 1.00 (referent) | 34,588 | 3.32 (3.28–3.36) | 1.00 (referent) |
| Male | 2,227 | 0.26 (0.25–0.27) | 1.18 (1.11–1.26)f | 6,733 | 0.81 (0.79–0.83) | 0.60 (0.58–0.62)f | 105,776 | 11.33 (11.26–11.40) | 3.41 (3.37–3.45)f |
| Race-ethnicity | |||||||||
| White, non-Hispanic | 3,244 | 0.23 (0.22–0.24) | 1.00 (referent) | 12,830 | 0.90 (0.88–0.91) | 1.00 (referent) | 84,375 | 5.71 (5.67–5.75) | 1.00 (referent) |
| Black, non-Hispanic | 476 | 0.26 (0.24–0.28) | 1.14 (1.03–1.26)f | 3,232 | 1.75 (1.68–1.81) | 1.94 (1.87–2.02)f | 21,223 | 9.71 (9.57–9.84) | 1.70 (1.67–1.73)f |
| American Indian/Alaska Native, non-Hispanic | 46 | 0.42 (0.31–0.47) | 1.87 (1.34–2.53)f | 204 | 1.82 (1.56–2.09) | 2.02 (1.74–2.33)f | 1,748 | 13.01 (12.37–13.66) | 2.28 (2.17–2.39)f |
| Asian or Pacific Islander, non-Hispanic | 193 | 0.23 (0.20–0.27) | 1.02 (0.87–1.18) | 1,066 | 1.23 (1.15–1.31) | 1.37 (1.28–1.46)f | 9,984 | 10.99 (10.77–11.21) | 1.92 (1.88–1.96)f |
| Hispanic | 552 | 0.32 (0.30–0.35) | 1.43 (1.30–1.57)f | 3,248 | 1.89 (1.82–1.96) | 2.10 (2.02–2.19)f | 22,285 | 11.86 (11.70–12.03) | 2.08 (2.05–2.11)f |
| Age (yrs) | |||||||||
| 0–49 | 217 | 0.02 (0.02–0.02) | 1.00 (referent) | 1,119 | 0.11 (0.11–0.12) | 1.00 (referent) | 7,673 | 0.75 (0.74–0.77) | 1.00 (referent) |
| 50–59 | 663 | 0.29 (0.27–0.32) | 13.62 (11.66–15.97)f | 2,921 | 1.30 (1.25–1.35) | 11.54 (10.76–12.38)f | 34,394 | 15.01 (14.85–15.17) | 19.89 (19.40–20.39)f |
| 60–69 | 1,133 | 0.65 (0.61–0.69) | 30.19 (26.08–35.09)f | 5,428 | 3.13 (3.04–3.21) | 27.82 (26.07–29.70)f | 54,103 | 30.97 (30.71–31.23) | 41.04 (40.07–42.04)f |
| 70–79 | 1,288 | 1.33 (1.26–1.40) | 61.50 (53.20–71.39)f | 6,074 | 6.25 (6.09–6.41) | 55.61 (52.16–59.34)f | 28,057 | 28.59 (28.26–28.93) | 37.89 (36.94–38.87)f |
| ≥80 | 1,239 | 2.03 (1.91–2.14) | 93.87 (81.16–109.01)f | 5,167 | 8.55 (8.31–8.78) | 76.04 (71.25–81.21)f | 16,137 | 27.04 (26.63–27.47) | 35.84 (34.88–36.84)f |
| Region | |||||||||
| Northeast | 854 | 0.24 (0.23–0.26) | 1.00 (referent) | 4,394 | 1.26 (1.22–1.30) | 1.00 (referent) | 24,682 | 6.76 (6.67–6.84) | 1.00 (referent) |
| South | 954 | 0.23 (0.22–0.25) | 0.96 (0.87–1.06) | 4,477 | 1.10 (1.07–1.13) | 0.87 (0.84–0.91)f | 24,725 | 5.74 (5.67–5.81) | 0.85 (0.83–0.87)f |
| Midwest | 1,679 | 0.24 (0.23–0.25) | 0.98 (0.90–1.07) | 7,216 | 1.03 (1.00–1.05) | 0.82 (0.79–0.85)f | 56,281 | 7.54 (7.48–7.61) | 1.12 (1.10–1.13)f |
| West | 1,053 | 0.25 (0.24–0.27) | 1.05 (0.95–1.15) | 4,622 | 1.12 (1.08–1.15) | 0.89 (0.85–0.93)f | 34,676 | 7.80 (7.72–7.88) | 1.15 (1.14–1.17)f |
| Rural/urban | |||||||||
| Urban | 3,836 | 0.25 (0.24–0.26) | 1.00 (referent) | 17,659 | 1.16 (1.14–1.18) | 1.00 (referent) | 120,140 | 7.40 (7.35–7.44) | 1.00 (referent) |
| Rural | 702 | 0.24 (0.22–0.25) | 0.94 (0.86–1.02) | 3,042 | 1.01 (0.98–1.05) | 0.87 (0.84–0.91)f | 20,177 | 6.49 (6.39–6.58) | 0.88 (0.86–0.89)f |
Abbreviations: IR = incidence rate; IRR = incidence rate ratio; CI = confidence interval.
Per 100,000 standard population; overall rates were age-adjusted to the 2000 U.S. standard population.
Cancer incidence data were compiled from cancer registries that meet the data quality criteria for all invasive cancer sites combined, representing 100% of the U.S. population during 2013–2017.
Categories may not add to total because of rounding and because unknown values were excluded.
Racial and ethnic groups are mutually exclusive. Hispanic persons can be any race. Rates are not presented as a separate category for those with unknown or other race or unknown ethnicity.
The U.S. Department of Agriculture Economic Research Service 2013 vintage rural-urban continuum codes were used to categorize county residence at time of cancer diagnosis as urban (codes 1–3) or rural (codes 4–9) (https://www.ers.usda.gov/data-products/rural-urban-continuum-codes).
Significant at P<0.05.
Hispanic (IR=1.72 per 100,000 persons) and non-Hispanic Asian/Pacific Islander persons(IR=1.69 per 100,000 persons) had the highest incidence of intrahepatic bile duct cancer, about 15%−17% higher than among non-Hispanic White. Compared to non-Hispanic White persons (IR=1.47 per 100,000 persons), non-Hispanic Asian/Pacific Islander persons had higher incidence rate of extrahepatic bile duct cancer (1.35 per 100,000 persons).
Individuals aged 80 years or older had the highest incidence of intrahepatic bile duct cancer (8.17 per 100,000), extrahepatic bile duct cancer (7.97 per 100,000), ampulla of Vater cancer (3.90 per 100,000), and cancer of overlapping and other lesions of the biliary tract (2.03 per 100,000 persons). Individuals living in rural areas had lower incidence of intrahepatic bile duct cancer (1.43 per 100,000), extrahepatic bile duct cancer (0.92 per 100,000), and ampulla of Vater cancer (0.54 per 100,000) compared to individuals living in urban areas (1.55, 1.00, and 0.58 per 100,000, respectively).
During 2013–2017 there were 20,709 cases of gallbladder cancer and 140,364 cases of liver cancer. The incidence rate of gallbladder cancer was 1.11 per 100,000 persons. The incidence rate of liver cancer was 7.06 per 100,000 persons.
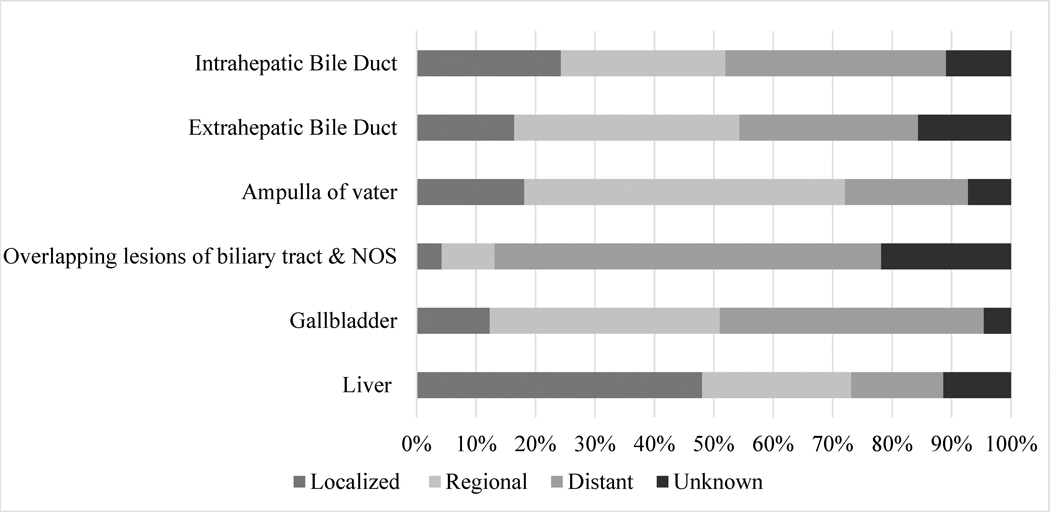
Stage
Stage at diagnosis varied for each cancer site. (Figure 1). Most cases of overlapping and other lesions of biliary tract (65.0%) were diagnosed at distant stage. For cancers of the extrahepatic bile duct and ampulla of Vater, 37.9% and 53.9% of cases were diagnosed at a regional stage, respectively. For intrahepatic bile duct cancer, 27.7% of cases were diagnosed at regional stage and 37.1% were diagnosed at distant stage. For gallbladder cancer 38.7% of cases were diagnosed at regional stage and 44.4% were diagnosed at distant stage. For liver cancer 48,1% of cases were diagnosed at localized stage and 25.2% were diagnosed at regional stage.
Figure 1. Stage of diagnosisa for cancers of the biliary tract, gallbladder, and liverb- United Statesc 2013–2017.
The figure is a bar graph that shows percentage of cases diagnosed at each stage of diagnosis for cases of intrahepatic bile duct cancer, extrahepatic bile duct cancer, ampulla of vater cancer, overlapping lesions of the biliary tract & NOS cancer, gallbladder cancer and liver caner during 2013–2017.
aStage was classified using SEER Summary Stage 2000 for diagnosis years 2001–2003 and 2016–2017, Derived SEER Summary Stage 2000 for diagnosis years 2004–2014, and either SEER Summary Stage 2000 or Derived SEER Summary Stage 2000 for diagnosis year 2015.
b Cancers diagnosed by death certificate or autopsy report were excluded.
cStage of diagnosis data were compiled from cancer registries that meet the data quality criteria for all invasive cancer sites combined, representing 100% of the U.S. population during 2013–2017.
Mortality
During 2013–2017, there were 31,391 deaths attributed to intrahepatic bile duct cancer and 8,390 deaths attributed to other biliary tract cancers (Table 2). Compared to females (MR = 1.49 per 100,000 for intrahepatic bile duct cancer deaths and 0.45 per 100,000 for other biliary tract cancer deaths), death rates were higher among males for intrahepatic bile duct cancer (1.88 per 100,000; MRR 1.26, 95% CI 1.23–1.29) and other biliary tract cancer (0.51 per 100,000; MRR 1.28, 95% CI 1.22–1.33).
Table 2.
Average annual mortality ratesa in cancer of the biliary tract, gallbladder, and liver by sex, age, race/ethnicity, and region- United Statesb 2013–2017
| Intrahepatic Bile Duct | Other Bile Duct | |||||
|---|---|---|---|---|---|---|
| Characteristic | n | IR (95% CI) | IRR (95% CI) | n | IR (95% CI) | IRR (95% CI) |
|
| ||||||
| Total | 31,391 | 1.66 (1.65–1.68) | 8,390 | 0.45 (0.44–0.46) | ||
| Sex | ||||||
| Female | 15,454 | 1.49 (1.47–1.52) | 1.00 (referent) | 4,218 | 0.40 (0.39–0.41) | 1.00 (referent) |
| Male | 15,937 | 1.88 (1.85–1.91) | 1.26 (1.23–1.29)f | 4,172 | 0.51 (0.49 −0.53) | 1.28 (1.22–1.33)f |
| Race-ethnicity | ||||||
| White, non-Hispanic | 23,169 | 1.62 (1.60–1.65) | 1.00 (referent) | 6,392 | 0.44 (0.43–0.45) | 1.00 (referent) |
| Black, non-Hispanic | 3,054 | 1.62 (1.56–1.68) | 1.00 (0.96–1.04) | 773 | 0.43 (0.40–0.46) | 0.97 (0.90–1.05) |
| American Indian/Alaska Native, non-Hispanic | 203 | 1.75 (1.51–2.02) | 1.08 (0.93–1.25) | 42 | 0.38 (0.27–0.52) | 0.87 (0.62–1.19) |
| Asian or Pacific Islander, non-Hispanic | 1,782 | 2.08 (1.98–2.18) | 1.28 (1.22–1.34)f | 403 | 0.48 (0.44–0.53) | 1.09 (0.98–1.21) |
| Hispanic | 3,118 | 1.85 (1.78–1.91) | 1.14 (1.09–1.18)f | 767 | 0.47 (0.43–0.50) | 1.06 (0.98–1.14) |
| Age (yrs) | ||||||
| 0–49 | 1,718 | 0.17 (0.16–0.18) | 1.00 (referent) | 300 | 0.03 (0.03–0.03) | 1.00 (referent) |
| 50–59 | 4,619 | 2.05 (1.99–2.11) | 11.83 (11.19–12.52) | 858 | 0.38 (0.35–0.40) | 12.48 (10.92–14.29)f |
| 60–69 | 8,855 | 5.10 (4.99 – 5.20) | 29.47 (27.98–31.06) | 1,947 | 1.12 (1.07–1.17) | 37.10 (32.83–42.06)f |
| 70–79 | 8,847 | 9.09 (8.90–9.28) | 52.56 (49.89–55.39) | 2,383 | 2.46 (2.36–2.56) | 81.41 (72.15–92.15)f |
| ≥80 | 7,352 | 12.15 (11.87–12.43) | 70.25 (66.64–74.10) | 2,902 | 4.72 (4.55 −4.89) | 156.24 (138.64–176.63)f |
| Region | ||||||
| Northeast | 6,453 | 1.84 (1.79–1.88) | 1.00 (referent) | 1,573 | 0.44 (0.42–0.46) | 1.00 (referent) |
| South | 7,231 | 1.76 (1.72–1.80) | 0.96 (0.93–0.99)f | 1,957 | 0.48 (0.46–0.50) | 1.08 (1.01–1.16)f |
| Midwest | 10,290 | 1.50 (1.48–1.53) | 0.82 (0.79–0.85)f | 2,961 | 0.44 (0.42–0.46) | 1.00 (0.94–1.06) |
| West | 7,183 | 1.72 (1.68–1.76) | 0.93 (0.90–0.97)f | 1,815 | 0.44 (0.42–0.46) | 1.00 (0.93–1.07) |
| Rural/urban | ||||||
| Urban | 26,691 | 1.70 (1.68–1.72) | 1.00 (referent) | 6,921 | 0.44 (0.43–0.46) | 1.00 (referent) |
| Rural | 4,700 | 1.49 (1.44–1.53) | 0.87 (0.85–0.90)f | 1,469 | 0.46 (0.44–0.48) | 1.03 (0.98–1.10) |
|
| ||||||
| Gallbladder | Liver | |||||
| Characteristic | n | IR (95% CI) | IRR (95% CI) | n | IR (95% CI) | IRR (95% CI) |
|
| ||||||
| Total | 10,932 | 0.58 (0.57–0.60) | 96,772 | 4.92 (4.89–4.95) | ||
| Sex | ||||||
| Female | 7,362 | 0.71 (0.69–0.72) | 1.00 (referent) | 26,285 | 2.49 (2.46–2.52) | 1.00 (referent) |
| Male | 3,563 | 0.44 (0.42–0.45) | 0.62 (0.59–0.64)f | 70,487 | 7.75 (7.69–7.81) | 3.11 (3.07–3.16)f |
| Race-ethnicity | ||||||
| White, non-Hispanic | 7,183 | 0.50 (0.49–0.51) | 1.00 (referent) | 61,443 | 0.51 (0.50–0.52) | |
| Black, non-Hispanic | 1,586 | 0.88 (0.84–0.93) | 1.77 (1.67–1.87)f | 14,656 | 0.90 (0.85–0.95) | 1.69 (1.66–1.72)f |
| American Indian/Alaska Native, non-Hispanic | 105 | 0.99 (0.80–1.21) | 1.99 (1.61–2.42)f | 974 | 1.09 (0.881.32) | 1.87 (1.75–2.00)f |
| Asian or Pacific Islander, non-Hispanic | 585 | 0.70 (0.64–0.76) | 1.39 (1.27–1.52)f | 6,235 | 0.68 (0.63–0.75) | 1.72 (1.67–1.76)f |
| Hispanic | 1,443 | 0.88 (0.83–0.92) | 1.75 (1.65–1.86)f | 13,098 | 0.90 (0.85–0.95) | 1.80 (1.76–1.84)f |
| Age (yrs) | ||||||
| 0–49 | 424 | 0.04 (0.04–0.05) | 1.00 (referent) | 3,439 | 0.34 (0.33–0.35) | 1.00 (referent) |
| 50–59 | 1,242 | 0.55 (0.52–0.58) | 12.93 (11.57–14.48)f | 19,612 | 8.52 (8.40–8.64) | 25.05 (24.15–25.98)f |
| 60–69 | 2,656 | 1.53 (1.47–1.59) | 35.79 (32.29–39.76)f | 33,973 | 19.46 (19.25–19.67) | 57.21 (55.23–59.27)f |
| 70–79 | 3,200 | 3.30 (3.19–3.41) | 77.13 (69.66–85.59)f | 21,817 | 22.37 (22.07–22.67) | 65.66 (63.43–68.20)f |
| ≥80 | 3,403 | 5.59 (5.40–5.78) | 130.75 (118.13 – 145.04)f | 17,931 | 29.70 (29.26–30.14) | 87.31 (84.16–90.59)f |
| Region | ||||||
| Northeast | 2,222 | 0.63 (0.60–0.66) | 1.00 (referent) | 15,459 | 4.23 (4.17–4.30) | 1.00 (referent) |
| South | 2,430 | 0.60 (0.57–0.62) | 0.95 (0.89–1.00) | 17,716 | 4.15 (4.08–4.21) | 0.98 (0.96–1.00) |
| Midwest | 3,701 | 0.55 (0.53–0.57) | 0.87 (0.82–0.92)f | 38,748 | 5.44 (5.39–5.50) | 1.29 (1.26–1.31)f |
| West | 2,445 | 0.59 (0.57–0.62) | 0.94 (0.88–0.99)f | 23,438 | 5.36 (5.29–5.43) | 1.27 (1.24–1.29)f |
| Rural/urban | ||||||
| Urban | 9,170 | 0.59 (0.58–0.60) | 1.00 (referent) | 81,283 | 4.96 (4.92–4.99) | 1.00 (referent) |
| Rural | 1,755 | 0.55 (0.53–0.58) | 0.94 (0.89–0.99)f | 15,489 | 4.75 (4.67–4.82) | 0.96 (0.94–0.97)f |
Abbreviations: MR = mortality rate; MRR = mortality rate ratio; CI = confidence interval.
Per 100,000 standard population; overall rates were age-adjusted to the 2000 U.S. standard population.
bData are from CDC’s National Center for Health Statistics National Vital Statistics System.
Categories may not add to total because of rounding and because unknown values were excluded.
Racial and ethnic groups are mutually exclusive. Hispanic persons can be any race. Rates are not presented as a separate category for those with unknown or other race or unknown ethnicity.
The U.S. Department of Agriculture Economic Research Service 2013 vintage rural-urban continuum codes were used to categorize county residence at time of cancer death as urban (codes 1–3) or rural (codes 4–9) (https://www.ers.usda.gov/data-products/rural-urban-continuum-codes). Mortality data for rural-urban status were available for grouped years 2012–2016.
Significant at P<0.05
Compared to non-Hispanic whites (MR = 1.62 per 100,000), death rates for intrahepatic bile duct cancer were higher among non-Hispanic Asian/Pacific Islanders (2.08 per 100,000; MRR 1.28, 95% CI 1.22–1.34) and Hispanics (1.85 per 100,000; MRR 1.14, 95% CI 1.09–1.18).
By age, individuals aged 80 years or older had the highest death rate of other biliary tract cancers (4.72 per 100,000; MRR 156.24, 95% CI 138.64–176.63) compared to individuals younger than 50 years of age (MR = 0.03 per 100,000).
By U.S. Census region, individuals who lived in the South at the time of diagnosis had the lowest rate of intrahepatic bile duct cancer deaths (1.50 per 100,000; MRR 0.82, 95% CI 0.79–0.85) compared to individuals living in the Northeast (MR = 1.84 per 100,000). Individuals living in the Midwest (1.76 per 100,000; MRR 0.96, 95% CI 0.93–0.99) and West (1.72 per 100,000; MRR 0.93, 95% CI 0.90–0.97) also had a lower death rate compared to individuals living in the Northeast. Individuals living in the Midwest had a higher death rate of other biliary tract cancers (0.48 per 100,000; MRR 1.08, 95% CI 1.01–1.16) compared to individuals living in the Northeast (MR=0.44 per 100,000).
During 2013–2017 there were 10,932 deaths attributed to gallbladder cancer and 96,712 deaths attributed to liver cancer. Death rate of gallbladder cancer was 0.58 per 100,000 persons. Death rate of liver cancer was 4.92 per 100,000 persons.
Discussion
Using national data, this study found differences in incidence and mortality rates for cancers of the biliary tract by sex, race/ethnicity, age, and U.S. Census region. This study also found that 68.1% of cancer cases of the biliary tract were diagnosed at a late stage (regional and distant), when treatment is less effective.
Higher incidence rates of intrahepatic bile duct cancer, extrahepatic bile duct cancer, and ampulla of Vater cancer were observed among Hispanics (all races) and non-Hispanic Asian/Pacific Islander persons, and a higher incidence rate of overlapping and other lesions of biliary tract was observed among American Indian/Alaska Native persons. This is consistent with previous studies that found higher rates for each anatomic site among American Indian/Alaska Native, Asian/Pacific Islander, and Hispanic persons.12 Etiologic research on cancers of the biliary tract suggests that risk factors vary by anatomic site.3 As previously mentioned, obesity, diabetes, heavy alcohol use, and smoking have been identified as risk factors for biliary tract cancers.6 Further epidemiologic studies that examine risk factors by race/ethnic groups of cancers of the biliary tract may help explain observed differences in incidence rates.
In this study, the number of deaths attributed to intrahepatic bile duct cancer were higher than the number of reported incident cases of intrahepatic bile duct cancer. A review of SEER cases found that the primary site for more than a third (38%) of cholangioarcinomas was coded to liver rather than to intrahepatic bile duct; the authors suggest that if site of origin cannot be determined during abstraction of cholangioarcinomas cases, that it be assigned to intrahepatic bile duct.11 For common cancer sites, there is good agreement (≥95%) between the cancer site reported as the underlying cause of death and the cancer site recorded in the population-based cancer registry, but less agreement for some less common sites, such as biliary tract cancers.26
Primary sclerosing cholangitis (PSC) is defined as chronic inflammation of the biliary duct that ultimately results in fibrosis and structuring (narrowing of duct) of the intrahepatic and/or extrahepatic bile ducts.27 Cholangiocarcinoma cases occurring in individuals with PSC is found synchronously with the diagnosis of PSC in 20–30% of individuals and within 1 year in 50%.28 Individuals with PSC also have increased incidence of gallstones, cholecystitis, gallbladder polyps, and gallbladder cancer.29 There is not consensus for an evidence-based guideline for cholangiocarcinoma surveillance of individuals diagnosed with PSC.30 However, one study suggests that surveillance for bile duct cancers in individuals with PSC may lead to improved outcomes.29 A study examining individuals with PSC in a surveillance program found those who were diagnosed with hepatobiliary cancer and in the program had an earlier stage of cancer diagnosis, a lower 5-year risk of a cancer-related adverse event (32% vs 75%), and significantly higher overall survival at 5 years (68% vs 20%) compared to patients that were not in the surveillance program.31
Smoking, alcohol, and obesity have been associated as risk factors for intrahepatic and extrahepatic bile duct cancer.6 Tobacco-related cancers could be prevented by reducing tobacco use through sustained, comprehensive, evidence-based tobacco prevention and control interventions.32 Alcohol-control policies and alcohol screening and brief intervention may reduce the prevalence of heavy and binge drinking.33 Community strategies and clinical interventions may help prevent and control overweight and obesity and may reduce the risk of cancer.34
There are several strategies for liver cancer prevention that also may be beneficial for the prevention of other biliary tract cancers. The hepatitis B vaccine is recommended for all infants at birth, children and adolescents younger than 19 years of age who have not yet been vaccinated, and adults who may be at an increased risk of hepatitis B including those requesting protection without acknowledgement of a specific risk factor. Adults at increased risk for HBV infection include those with travel to certain countries, work exposure to blood, high-risk sexual behavior, injection drug use, living situations that may increase exposure to HBV infection, and certain medical conditions.35,36 Although there is no hepatitis C vaccine, there is a cure, and CDC now recommends universal hepatitis C virus screening for all U.S adults and all pregnant women during every pregnancy, except in settings where the prevalence of HCV infection is <0.1%.37
Since 1998, CDC’s National Comprehensive Cancer Control Program (NCCCP) has provided funding, guidance, and technical assistance that state, territorial, and tribal programs use to design and implement comprehensive cancer control (CCC) plans.38 An Institute of Medicine report in 2010 described several barriers to hepatitis B and hepatitis C prevention and control efforts, including a lack of knowledge and awareness among health care providers, populations at high risk, and the public.39 Additionally, a recent CDC Vital Signs reported that the annual rate of reported acute hepatitis C tripled from 2009 to 2018, highlighting the need to improve viral hepatitis prevention in the United States.40 Since 2015, the NCCCP has been engaged in implementing key liver cancer primary prevention and early detection and screening strategies around the promotion of vaccination and screening for viral hepatitis to prevent liver cancer in high risk populations. The United States Preventive Services Task Force recommends screening for hepatitis B virus (HBV) infection in adolescents and adults at increased risk for infection.41
Although this paper did not assess temporal differences in rates during the 5-year period, a previous study examining incidence trends during 1999–2013 of cancers of the biliary tract found that incidence of intrahepatic and extrahepatic cancer increased among all adults incidence of ampulla of Vater cancer increased among younger adults (18–44 years of age).3The opioid crisis has increased the number of people who inject drugs in the United States and has thereby contributed to the increased risk of HCV transmission observed over the past decade.40 The opioid crisis in addition to nonalcoholic fatty liver disease, including nonalcoholic steatohepatitis, as an emerging cause of liver failure, may be contributing factors to the increases in liver cancer observed in the United States.9,42 Key interventions targeted to high-risk populations may help reduce prevalence of potential risk factors by improving knowledge and awareness of risk factors and improving prevention through hepatitis B vaccination, use of syringe service programs, and testing and treatment for hepatitis C meant to curb the transmission of viral hepatitis.
The findings of this study are subject to three limitations. First, delays in cancer reporting might contribute to an underestimate of recently reported incidence rates. Second, analyses may be biased if race or ethnicity were misclassified. Reporting of race and ethnicity uses data from medical records and death certificates, which might be inaccurate in some cases. Methods are used to verify that this race ethnicity data are as accurate as possible. Third, classification of cases and deaths coded to intrahepatic bile duct and liver cancer should be interpreted with caution. A study by Polednak et al. suggested that some deaths in the liver-biliary tract could be miscoded; they found that only 82% of people reported to have died from liver cancer were confirmed to have a primary liver cancer diagnosis (potential over-reporting) and some with a liver cancer diagnosis were coded as dying from another cause (potential under-reporting). This study also suggested that deaths for intrahepatic bile duct cancers tended to be overreported.43
This report provides national estimates of rare biliary tract cancers, which are often diagnosed at late stage. Key interventions targeted to high-risk populations might help reduce incidence and mortality of cancers of the biliary tract by improving prevention of viral hepatitis through hepatitis B vaccination, use of syringe service programs, and testing and treatment of hepatitis C. Evidence-based prevention programs for tobacco and alcohol use, and community and clinical interventions for obesity may also be beneficial.
Acknowledgements
We gratefully acknowledge the contributions of the state and regional cancer registry staff and health department personnel for their work in collecting the data used in this study.
This research was supported in part by an appointment (TD Ellington) to the Research Participation Program at CDC administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and CDC.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Disclosure of Potential Conflict of Interest
No potential conflicts of interest were disclosed.
Division of Cancer Prevention and Control, National Center for Chronic Disease Prevention and Health Promotion, CDC
Division of Viral Hepatitis, National Center of HIV/AIDS, Viral Hepatitis, STD and TB Prevention, CDC
References
- 1.Bridgewater JA, Goodman KA, Kalyan A, Mulcahy MF. Biliary Tract Cancer: Epidemiology, Radiotherapy, and Molecular Profiling. Am Soc Clin Oncol Educ Book. 2016;35:e194–e203. doi: 10.1200/EDBK_160831 [DOI] [PubMed] [Google Scholar]
- 2.Marcano-Bonilla L, Mohamed EA, Mounajjed T, Roberts LR. Biliary tract cancers: epidemiology, molecular pathogenesis and genetic risk associations. Chin Clin Oncol. 2016;5(5):61. doi: 10.21037/cco.2016.10.09 [DOI] [PubMed] [Google Scholar]
- 3.Van Dyke AL, Shiels MS, Jones GS, et al. Biliary tract cancer incidence and trends in the United States by demographic group, 1999–2013. Cancer. 2019;125(9):1489–1498. doi: 10.1002/cncr.31942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chapman RW. Risk factors for biliary tract carcinogenesis. Ann Oncol. 1999;10 Suppl 4:308–11 [PubMed] [Google Scholar]
- 5.Tyson GL, El-Serag HB. Risk factors for cholangiocarcinoma. Hepatology. 2011;54(1):173–184. doi: 10.1002/hep.24351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petrick JL, Yang B, Altekruse SF, et al. Risk factors for intrahepatic and extrahepatic cholangiocarcinoma in the United States: A population-based study in SEER-Medicare. PLoS One. 2017;12(10):e0186643. Published 2017 Oct 19. doi: 10.1371/journal.pone.0186643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmidt MA, Marcano-Bonilla L, Roberts LR. Gallbladder cancer: epidemiology and genetic risk associations. Chin Clin Oncol. 2019;8(4):31. doi: 10.21037/cco.2019.08.13 [DOI] [PubMed] [Google Scholar]
- 8.Henley SJ, Weir HK, Jim MA, Watson M, Richardson LC. Gallbladder Cancer Incidence and Mortality, United States 1999–2011. Cancer Epidemiol Biomarkers Prev. 2015;24(9):1319–1326. doi: 10.1158/1055-9965.EPI-15-0199 [DOI] [PubMed] [Google Scholar]
- 9.Massoud O, Charlton M. Nonalcoholic Fatty Liver Disease/Nonalcoholic Steatohepatitis and Hepatocellular Carcinoma. Clin Liver Dis. 2018. Feb;22(1):201–211. doi: 10.1016/j.cld.2017.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Islami F, Goding Sauer A, Miller KD, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018;68:31–54. doi: 10.3322/caac.21440 [DOI] [PubMed] [Google Scholar]
- 11.Altekruse SF, Devesa SS, Dickie LA, McGlynn KA, Kleiner DE. Histological classification of liver and intrahepatic bile duct cancers in SEER registries. J Registry Manag. 2011. Winter;38(4):201–5. [PMC free article] [PubMed] [Google Scholar]
- 12.Castro, Felipe A et al. “Biliary tract cancer incidence in the United States-Demographic and temporal variations by anatomic site.” International journal of cancer vol. 133,7 (2013): 1664–71. doi: 10.1002/ijc.28161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Technical Notes, based on 2019 submission data (1999–2017): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; www.cdc.gov/uscs, released in June 2020. [Google Scholar]
- 14.World Health Organization. International classification of diseases for oncology, third edition, first revision. Geneva: World Health Organization; 2014. [Google Scholar]
- 15.Welzel TM, McGlynn KA, Hsing AW, O’Brien TR, Pfeiffer RM. Impact of classification of hilar cholangiocarcinomas (Klatskin tumors) on the incidence of intra- and extrahepatic cholangiocarcinoma in the United States. J Natl Cancer Inst. 2006; 98: 873–875. [DOI] [PubMed] [Google Scholar]
- 16.National Center for Health Statistics. National Vital Statistics System: Mortality Data. Atlanta, GA: US Department of Health and Human Services, CDC; 2019 [Google Scholar]
- 17.World Health Organization. International statistical classification of diseases and related health problems, tenth revision: World Health Organization; 2015. [PubMed] [Google Scholar]
- 18.CDC. Race recode for USCS. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. 2020. https://www.cdc.gov/cancer/uscs/public-use/dictionary/race-recode-USCS.htm. [Google Scholar]
- 19.U.S. Census Bureau Regions and Divisions with state FIPS codes. [Google Scholar]
- 20.The U.S. Department of Agriculture Economic Research Service. 2013. [Google Scholar]
- 21.Ruhl JL, Callaghan C, Hurlbut A, Ries LAG, Adamo P, Dickie L, Schussler N (eds.) Summary Stage 2018: Codes and Coding Instructions, National Cancer Institute, Bethesda, MD, 2020. [Google Scholar]
- 22.National Cancer Institute. SEER*Stat software. Bethesda, MD: National Cancer Institute, Surveillance Research Program; 2018. [Google Scholar]
- 23.Anderson R & Rosenberg H. Age standardization of death rates: implementation of the year 2000 standard. Natl Vital Stat Rep 1998;47:1–16. [PubMed] [Google Scholar]
- 24.Tiwari RC, Clegg LX, Zou Z. Efficient interval estimation for age-adjusted cancer rates. Statistical Methods in Medical Research 2006;15:547–569. [DOI] [PubMed] [Google Scholar]
- 25.Fay MP. Approximate confidence intervals for rate ratios from directly standardized rates with sparse data. Communications in Statistics: Theory and Methods 2007;28(9):2141–2160. [Google Scholar]
- 26.German RR, Fink AK, Heron M, et al. The accuracy of cancer mortality statistics based on death certificates in the United States. Cancer Epidemiol. 2011;35(2):126–131. doi: 10.1016/j.canep.2010.09.005 [DOI] [PubMed] [Google Scholar]
- 27.Eaton JE, Talwalkar JA, Lazaridis KN, et al. Pathogenesis of primary sclerosing cholangitis and advances in diagnosis and management. Gastroenterology 2013;145:521–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fevery J, Verslype C, Lai G, Aerts R, Van Steenbergen W. Incidence, diagnosis, and therapy of cholangiocarcinoma in patients with primary sclerosing cholangitis. Dig Dis Sci. 2007;52(11):3123–3135. doi: 10.1007/s10620-006-9681-4 [DOI] [PubMed] [Google Scholar]
- 29.Fung BM, Lindor KD, Tabibian JH. Cancer risk in primary sclerosing cholangitis: Epidemiology, prevention, and surveillance strategies. World J Gastroenterol. 2019;25(6):659–671. doi: 10.3748/wjg.v25.i6.659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hilscher MB, Tabibian JH, Carey EJ, Gostout CJ, Lindor KD. Dominant strictures in primary sclerosing cholangitis: A multicenter survey of clinical definitions and practices. Hepatol Commun. 2018;2:836–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kipp BR, Stadheim LM, Halling SA, Pochron NL, Harmsen S, Nagorney DM, Sebo TJ, Therneau TM, Gores GJ, de Groen PC, Baron TH, Levy MJ, Halling KC, Roberts LR. A comparison of routine cytology and fluorescence in situ hybridization for the detection of malignant bile duct strictures. Am J Gastroenterol. 2004;99:1675–1681. [DOI] [PubMed] [Google Scholar]
- 32.Holford TR, Meza R, Warner KE, et al. Tobacco control and the reduction in smoking-related premature deaths in the United States, 1964–2012. JAMA 2014;311:164–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alattas M, Ross CS, Henehan ER, Naimi TS. Alcohol policies and alcohol-attributable cancer mortality in U.S. States, Chemico-Biological Interactions (2019). DOI: 10.1016/j.cbi.2019.108885 [DOI] [PubMed] [Google Scholar]
- 34.Steele CB, Thomas CC, Henley SJ, et al. Vital Signs: Trends in Incidence of Cancers Associated with Overweight and Obesity - United States, 2005–2014. MMWR Morb Mortal Wkly Rep. 2017;66(39):1052–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Healthcare Quality Promotion (DHQP), 2020. https://www.cdc.gov/vaccinesafety/vaccines/hepatitis-b-vaccine.html
- 36.Schillie S, Vellozzi C, Reingold A, et al. Prevention of Hepatitis B Virus Infection in the United States: Recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm Rep 2018;67(No. RR-1):1–31. DOI: 10.15585/mmwr.rr6701a1externalicon [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults — United States, 2020. MMWR Recomm Rep 2020;69(No. RR-2):1–17. DOI: 10.15585/mmwr.rr6902a1externalicon. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. Division of Cancer Prevention and Control, Centers for Disease Control and Prevention. https://www.cdc.gov/cancer/ncccp/index.htm
- 39.Committee on the Prevention and Control of Viral Hepatitis Infection, Institute of Medicine. Hepatitis and liver cancer: a national strategy for prevention and control of hepatitis B and C. Colvin HM, Mitchell AE, eds. Washington (DC): National Academies Press; 2010. [PubMed] [Google Scholar]
- 40.Ryerson AB, Schillie S, Barker LK, Kupronis BA, Wester C. Vital Signs: Newly Reported Acute and Chronic Hepatitis C Cases ― United States, 2009–2018. MMWR Morb Mortal Wkly Rep 2020;69:399–404. DOI: 10.15585/mmwr.mm6914a2externalicon. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.US Preventive Services Task Force, Krist AH, Davidson KW, Mangione CM, Barry MJ, Cabana M, Caughey AB, Donahue K, Doubeni CA, Epling JW Jr, Kubik M, Ogedegbe G, Owens DK, Pbert L, Silverstein M, Simon MA, Tseng CW, Wong JB. Screening for Hepatitis B Virus Infection in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2020. Dec 15;324(23):2415–2422. doi: 10.1001/jama.2020.22980. [DOI] [PubMed] [Google Scholar]
- 42.National Academies of Sciences, Engineering, and Medicine. 2017. A National Strategy for the Elimination of Hepatitis B and C: Phase Two Report. Washington, DC: The National Academies Press. doi: 10.17226/24731. [DOI] [PubMed] [Google Scholar]
- 43.Polednak AP. Using cancer registries to assess the accuracy of primary liver or intrahepatic bile duct cancer as the underlying cause of death, 1999–2010. J Registry Manag. 2013;40(4):168–175. [PubMed] [Google Scholar]