Abstract
Purpose
This study aimed to determine the effects of a circuit exercise program on the physical fitness parameters of children with atypical autism spectrum condition (ASC) and typically developing (TD) children.
Method
Fourteen (14) boys with atypical autism (mean age: 10.07 ± 0.25 years; weight: 24.97 ± 0.64 kg; height: 126.79 ± 1.33 cm) and 14 typically developing boys (mean age: 10.07 ± 0.30 years; weight: 26.97 ± 0.55 kg; height: 126.50 ± 0.62 cm) participated in the study. The children were divided into four groups using a random coin toss: Autism Exercise Group (AEG), Autism Control Group (ACG), Typically Developing Exercise Group (TDEG), and Typically Developing Control Group (TDCG). Testing parameters from the Bruininks-Oseretsky test of gross motor proficiency (BOT-2) included running speed and agility, balance, bilateral coordination, and the standing long jump. Handgrip strength (both sides), reaction times (visual and auditory), and flexibility tests were also performed. The exercise program consisted of three 60-minute sessions per week for 12 weeks, using the most-to-least prompting method.
Findings
Significant improvements were observed for AEG in running speed and agility, balance, standing long jump, reaction times, handgrip strength, and flexibility (p < 0.05). For TDEG, only the standing long jump scores failed to significantly improve (p < .05). Comparing AEG and TDEG pre- and post-test results, the former showed 30% greater development with respect to balance, standing long jump, auditory reaction time, and handgrip strength (p < 0.05).
Conclusion
Based on the significant improvements in physical fitness parameters of AEG, we recommend that children with ASC start sports training immediately when diagnosed with autism and participate in structured physical activities with their peers.
Keywords: autism, BOT-2, exercise, physical fitness
Introduction
Autism spectrum condition (ASC) is a neurodevelopmental condition characterized by differences in social communication and interaction, typically also involving repetitive behaviors and restricted interests. Furthermore, ASC is often accompanied by unusual sensory experiences affecting single or multiple modalities and diminished motor skills such as poor hand-eye coordination and unstable balance (Casassus et al. 2019, Intaitė et al. 2019, Lipinski et al. 2019, Gowen and Hamilton 2013, American Psychiatric Association (DSM-V) 2013, Simmons et al. 2009, Green et al. 2009, Ozonoff et al. 2008). Atypical autism is often described as a subthreshold diagnosis, presenting with some symptoms of autism but insufficient to meet criteria for a diagnosis of childhood autism (or autistic disorder). Alternatively, atypical autism can be diagnosed when there is a late onset of symptomatology. Atypical autism (as defined by ICD-10) is seen as being equivalent to the DSM-IV-TR diagnostic category of pervasive developmental disorder not otherwise specified (PDD NOS). DSM-5 does not have a separate diagnostic category for PDD NOS. In accordance with DSM IV; children with atypical autism are the children who display rigid, stereotypic behaviors that show limitations in mutual social interaction, verbal and non-verbal communication (American Psychiatric Association [APA] 2000).
ASC and motor development
Compared to typically developing (TD) children, children with ASC experience problems related to balance, postural stability, walking, joint flexibility, and speed of movement (Casassus et al. 2019, Carrigan and Allez 2017, Lipinski et al. 2019, Jansiewics 2006, Minshew et al. 2004). In addition to restricted and repetitive behaviors, ASC is also characterized by a pronounced preference for environmental certainty. Individuals with ASC may present with differences when it relates to emotional and cognitive processing functions that are necessary for decision making (Sahuquillo-Leal et al. 2020, García-Blanco et al. 2017a, García-Blanco et al. 2017b). In children with ASC, problems with both fine and gross motor skills are observed to varying degrees. In this context, the results of prior studies (Piek and Dyck 2004, Beversdorf et al. 2001) indicated that children with ASC are less willing to perform certain movements than children who do not have ASC.
The study of Green et al. (2009) included 101 children with ASC, and its reported that 79% of the participants had movement disorders, with such difficult motor skills restricting their physical activity. Pan (2008) compared physical activity levels of primary school students with ASC (n = 23) to those of typically developing students (n = 23) in their study, and the results suggested very low activity levels for the children with ASC. The implementation of exercise programs supporting basic movement skills is a vital component in the education of children with ASC. In particular, Eichstaedt and Lavay (1992) stated that instructing children with ASC in basic movement skills contributes significantly to these children's understanding of their own bodies as well as their environment they live in. In this context, Tekin-İftar and Kırcaali-İftar (2006) suggested most-to-least prompting that is one of the most effective methods to teach movement to individuals with intellectual disorders and those with ASC. While children with ASC may appear physically similar to typically developing children, the results of prior case reports (Jansiewics 2006, Minshew et al. 2004, Yılmaz et al. 2004, Srinivasan et al. 2014, Pan 2008). Hence, this study was planned considering how children with TD and ASC would respond to a similar exercise program. In this context, the current study aims to determine the effects of a 12-week structured circuit exercise program on the physical fitness levels parameters of children with ASC and TD children.
Method
Participants
There are no official statistics regarding the prevalence of autism in Turkey. According to data from the Centers for Disease Control and Prevention (CDC) of the United States Department of Health and Human Services and the Autism and Developmental Disabilities Monitoring (ADDM) Network, the prevalence of ASC in 8-year-old children is approximately 1.7%, or 1 in 59 (Baio et al. 2018). Additionally, CDC studies conducted in Asia, Europe, and North America have reported an average prevalence of ASC between 1% and 2% (ADDM Community Report on Autism 2018). In the present study, aprevalence of 1% was used to calculate the sample size, resulting in a minimum sample size of 15 with a significance level of 0.05, z = 1.96, and sampling error (d) = 0.05. A value of p = 0.01 was accepted as the level of statistical significance, thus q = 0.99. Children who were diagnosed with atypical autism according to DSM-IV criteria by specialist doctors working in the pediatric psychiatry department of the state hospital were participated in this study. The participants were subsequently re-evaluated according to the DSM-5 diagnostic criteria mentioned in previous section, and all of them meet the whole criteria. The study participants included boys with atypical ASC (n = 14) and TD children (n = 14). They were divided into four groups by means of a random coin toss (Suresh 2011, Clark and Westerberg 2009), designated as follows: Autism Exercise Group (AEG; n = 7), Autism Control Group (ACG; n = 7), Typically Developing Exercise Group (TDEG; n = 7), and Typically Developing Control Group (TDCG; n = 7). The mean ages of the children with ASC and TD children in this study were 10.07 0.25 and 10.07 0.30 years, respectively. The results of Baio et al. (2018) study demonstrated stated that ASC is usually more common in boys than in girls by a factor of approximately 5. The participants in this study were exclusively boys as we were unable to find a sufficient number of girls with atypical autism to participate. The participants were turkish/caucasion. Ethical approval was obtained from the Cukurova University Faculty of Medicine Ethical Committee for Non-Interventional Clinical Researches (decision number 11, serial number 15). Consent forms were signed by the families of the children who agreed to participate in the study voluntarily.
Inclusion and exclusion criteria for children with ASC and typically developing children participating in this study
The children with ASC who participated in this study all received medical treatment for their condition, attended special education or rehabilitation centers, were able to follow instructions, and possessed both motor imitation skills and bathroom skills. Exclusion criteria included having engaged in regular physical activity before the start of the study, physical disabilities, or other health problems. These facts were established by interviewing special education teachers working in the schools attended by the participants, child development specialists, and the families of the participants. The TD children involved in this study did not regularly participate in athletic activities and had no physical disabilities or health problems.
Environment and materials used in exercise program
The exercise program was carried out in an indoor sports hall with a rubber floor. Performance measurements were conducted in a performance measurement lab equipped with appropriate heating, lighting, and sound insulation. A balance beam, balance blocks, step platform, slalom sticks, referee's whistle, hand lamp, meter stick, sphygmometer, and chronometer were used to take measurements during exercise sessions.
The researchers and trainers
The study was conducted by eight people, including a researcher and seven trainers with knowledge of autism and expertise in preparing individual training programs for children with ASC. All of the exercises for children with ASC were carried out in the form of one-on-one teaching. Only children in the exercise groups participated in the exercise program, which lasted a total of twelve weeks.
The physical tests
The Bruininks-Oseretsky (BOT-2) test was developed to measure the motor functions of children with normal and common developmental disorders between the ages of four and twenty-one (Fransen et al. 2014). The entire test consists of eight subtests and a total of 53 items. Of the subtests, four measure gross motor skills, one measures both fine and gross motor skills, and three measure fine motor skills. The BOT-2 test is a revised version of the first version developed in 1978 by Bruininks-Oseretsky. In this study, six subtests belonging to the BOT-2 rough engine test were used. Participants were worn shoes during the subtests of BOT-2. The motor proficiency levels of the students have been determined with the BOT-2 (Bruininks and Bruininks 2005). The validity and reliability study of BOT-2 in Turkey has been carried out by Mülazımoglu Balli (2006). BOT-2 was administered twice, once before the start of the basic training program (pre-test) and once after the program finishes (post-test). Since BOT2 has not yet been conducted on Turkish children, the analyzes were made on point scores. According to the results of scientific research, it is recommended to use points of point instead of norm values to observe this improvement, even if the improvement in the motor skill level of children is minimal (Mülazımoğlu-Ballı and Gürsoy 2012, Najafabadi et al. 2018, Mülazımoğlu-Ballı and Gürsoy 2012, Bruininks and Bruininks 2005, Yanardag et al. 2009, Günal and Bumin 2007, Yılmaz et al. 2004, Işık and Zorba 2020, Mülazımoglu Balli 2006). The BOT2 test, which is applied to children with normal development, is stated to have high validity and reliability coefficient in terms of content and structure (Bruininks and Bruininks 2005). It has been reported that BOT-2, performed on children aged 8–11 years with normal development, is a valid and reliable test in terms of motor skills (Jírovec et al. 2019). Besides, Dewey and Cantell stated that children with autism use the BOT-2 test to determine their motor development and that the BOT2 test has a high validity and reliability coefficient (r = 0.86) in terms of content and structure (Dewey et al. 2007).
Subtests used in the BOT-2 test battery
Running speed and agility.
Standing on the dominant foot on the balance (I) beam (eyes open).
Standing in the ‘foot thumb-heel contact’ position on the balance (II) beam (eyes open).
Coordination (I): Simultaneous foot and toe-tapping in the same direction.
Coordination (II): Simultaneous foot and toe-tapping in different directions.
Standing Long Jump (Bruininks and Bruininks, 2005).
Prior to starting the tests, the dominant foot and hand preferences of the children were determined. Foot preferences were identified following three repetitions of kicking a ball on the ground with one of their feet. To determine their dominant hands, the children were asked to take and throw tennis balls in a basket three times in a row.
Other tests
The sit and reach flexibility test, handgrip strength test (measured using a Takei Hand Grip Dynamometer), and visual and auditory reaction time measurement tests (using the Newtest 1000 reaction device) were also performed. Time measurements were recorded to a precision of 0.01 s (Tamer 2000, Saygın et al. 2005, Özmerdivenli et al. 2004).
The instructional method used for children with ASC and TD children
The most-to-least prompting method was employed to instruct the children with ASC participating in the exercise program (Tekin-İftar and Kırcaali-İftar 2006, Yanardag 2007). The children with ASC were provided with skill instruction and controlling prompts by the trainers so that the exercises were performed simultaneously. Based on the assumption that TD children exhibit normal developmental characteristics while engaging in exercise, they started with the ‘model prompts and verbal prompts’ step, the second step of the most-to-least prompting teaching method. After the children had performed the movement correctly, we continued to the next step of the prompt technique.
Exercise program stages
Determining the given stimulus for children with ASC: The target stimulus enabling the individual to respond is a question or explanation, employed to elicit a reaction or response from the individual (Kirkendall et al. 1987). Verbal instructions (come, go, stop, climb on, land on, walk, jump, keep, leave, sit, etc.) for movement skills were established in order to prompt reactions from the children with ASC.
Determining how to react to the behaviors of the children with ASC: Constant reinforcement was employed by the trainers to elicit the correct reactions before and after prompts (Tekin-İftar and Kırcaali-İftar 2006, Schloss et al. 2001).
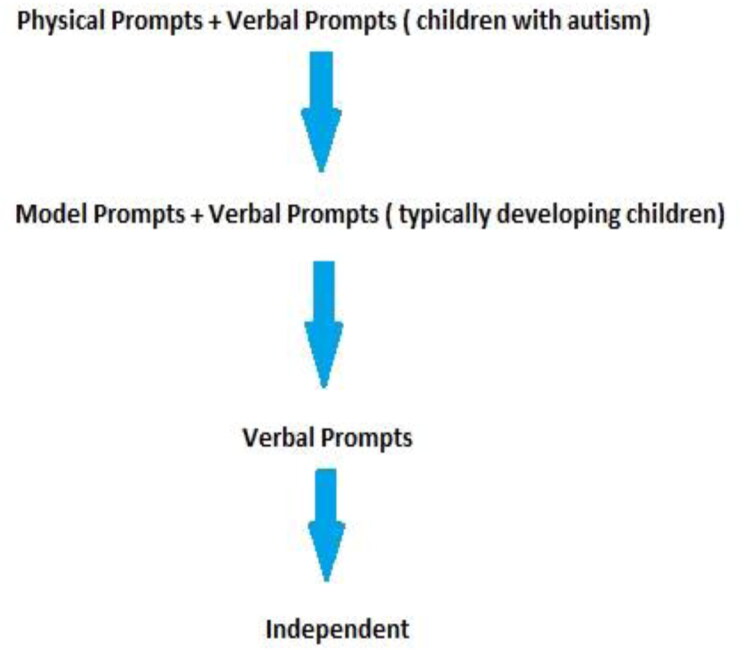
The order of the controlling prompts is shown in Figure 1.
Figure 1.
Order of the application of controlling prompts (Tekin-İftar and Kırcaali-İftar 2006).
12-Week structured circuit exercise program
A four-part circuit exercise program was implemented for the exercise groups. The format and contents of the program can be seen in Table 1.
Table 1.
The content of 12-week structured circular training program applied to AEG and TDECG.
| Weeks | The numbers of repetition and set | Warm-up | Main period | Cool-down |
|---|---|---|---|---|
| 1–4 weeks | 3 set x 3 rep. | 15min | 40min | 5min |
| 5–8 weeks | 3 set x 6 rep. | |||
| 9–12 weeks |
3 set x 9 rep. |
|
|
|
| Including of main period | ||||
| ||||
| Warm-up (15min): walking (It was used in the 100-120 bpm for warm-up heart rate) (10min), stretching exercises (5 min) Cool-down (5min): Stretching exercises (5min) | ||||
Trained with weights accounting for 5% of body weight (Muratlı 1997).
Exercise program and implementation
Children in the exercise group exercised sixty minutes per day, three days a week for twelve weeks. In exercise program and practice, there was a rest day between sessions. Work was done on day mondays, wednesdays and fridays. Repetitions were only performed after the children had completed the required sets for all the stations, starting again with the first (balance) station. The children’s heart rates were measured before and after completion of the exercise session. During each exercise session, resting was permitted for 1–2 min between stations since the intensity of exercise between the first (balance) station and the third (strength) station (strength station) was low, with pulses below 90–100 beats per minute. Resting enabled the participants to concentrate and maintain their motivational levels. At the end of the fourth station, double the resting time was allowed because the heart rates exceeded 90–100 beats per minute following the fourth (jumping) station. After resting, the participants resumed exercising, beginning again at the first station until all repetitions were completed.
The maximum number of repetitions of leaps was determined for each child for 30 s. During the study, 50% of the maximum number of jumps was run at the repetition count. That is 8 repetitions were performed on a child who made 16 jumps in 30 s. Meanwhile, the instructor made the jumps together. The tasks performed in the circuit session program; Walking on a standard balance beam (length 400, height 15, width 10 cm). Walking on balance wedges (12 pieces, height 10, width 10 cm) lined up side by side. Jumping over obstacles (12, obstacle height 10 cm in the first week, increased every week to 25 cm in the last week) by jumping with two feet. Jumping up and down on the aerobic step board with two feet (length 96, width 34.6, height 15 cm). Pulling rope using both hands (length 10 m, thickness 50 mm). Visual reaction exercises (flashlight emitting white light was used). Auditory reaction exercises (low-pitched referee whistle was used). The first four weeks of the exercise session involved 3 sets x 3 repetitions for each exercise, increasing to 3 sets x 6 repetitions for weeks 5–8 and then to 3 sets x 9 repetitions for the final four weeks.
Data analysis
In general, the distribution of a sample significantly affects the sample size necessary for a robust statistical analysis. As a sample size gets larger, the data tend to conform to a normal probability distribution, whereas small sample sizes frequently exhibit non-normal distribution (Krithikadatta 2014). We employed the SPSS 15.0 package program to statistically evaluate the data. A nonparametric test was performed as test scores did not show normal distribution based on the results of the Kolmogorov-Smirnov normality test and the Mann-Whitney U test. For comparisons, a significance level of p < 0.05 was chosen.
Results
The mean age, weight, and height of the children with ASC (n = 14) were 10.07 ± 0.25 years, 24.97 ± 0.64 kg and 126.79 ± 1.33 cm, respectively (Table 2). For the typically developing children TDC (n = 14), the mean age, weight, and height were 10.07 ± 0.30 years, 26.26 ± 0.55 kg, and 126.50 ± 0.62 cm, respectively. There were no significant differences between the two groups in terms of these parameters (p > 0.05 for all) (Table 3).
Table 2.
Demographic characteristics of the participants.
| ASC (n = 14) |
TDC (n = 14) |
Mann-Whitney U Test |
||||
|---|---|---|---|---|---|---|
| Demographic characteristics | std | std | z | p | ||
| Age (year) | 10.07 | 0.25 | 10.07 | 0.30 | −0.27 | .79 |
| Body weight (kg) | 24.97 | 0.64 | 26.26 | 0.55 | −1.49 | .14 |
| Height (cm) | 126.79 | 1.33 | 126.50 | 0.62 | −1.35 | .18 |
Table 3.
Comparison of differences between pre- and post-test values for AEG vs. ACG and TDEG vs. TDCG.
| The applied tests | AEG Pre-post-test difference (n = 7) | ACG Pre-post-test difference (n = 7) | Mann-Whitney U Test |
TDEG Pre-post-test difference (n = 7) | TDCG Pre-post-test difference (n = 7) | Mann-Whitney U Test |
|||
|---|---|---|---|---|---|---|---|---|---|
| Mean Rank | Mean Rank | Z | p | Mean Rank | Mean Rank | Z | p | ||
| Running speed and agility (sec) | 11.00 | 4.00 | −3.22 | 0.001 ** | 10.43 | 4.57 | −2.71 | 0.007 * | |
| Balance (sec) | Balance –I | 10.64 | 4.36 | −2.97 | 0.003 ** | 7.50 | 7.50 | 0.00 | 0.999 |
| Balance –II | 10.93 | 4.07 | −3.28 | 0.001 ** | 9.64 | 5.36 | −2.74 | 0.032 * | |
| Bilateral coordination | Coordination –I | 9.00 | 6.00 | −1.88 | 0.060 | 7.93 | 7.07 | −0.54 | 0.593 |
| Coordination –II | 9.07 | 5.93 | −1.66 | 0.096 | 8.57 | 6.43 | −1.21 | 0.227 | |
| Strength (cm) | Standing long jump | 10.93 | 4.07 | −3.24 | 0.001 ** | 7.50 | 7.50 | 0.00 | 0.999 |
| Reaction time (ms) | Right hand visual | 4.00 | 11.00 | −3.13 | 0.002 ** | 4.00 | 11.00 | −3.13 | 0.002 ** |
| Left hand visual | 4.29 | 10.71 | −2.88 | 0.004 ** | 4.00 | 11.00 | −3.15 | 0.002 ** | |
| Right hand audial | 4.00 | 11.00 | −3.14 | 0.002 ** | 4.00 | 11.00 | −3.13 | 0.002 ** | |
| Left hand audial | 4.00 | 11.00 | −3.15 | 0.002 ** | 4.00 | 11.00 | −3.14 | 0.002 ** | |
| Hand strength (kg) | Hand grip strength (right) | 11.00 | 4.00 | −3.14 | 0.002 ** | 11.00 | 4.00 | −3.16 | 0.002 ** |
| Hand grip strength (left) | 10.29 | 4.71 | −2.50 | 0.013 * | 9.93 | 5.07 | −2.29 | 0.028 * | |
| Flexibility (cm) | Sit and Reach Test | 10.93 | 4.07 | −3.09 | 0.002 ** | 11.00 | 4.00 | −3.21 | 0.001 ** |
p < 0.05.
p < 0.01.
Statistical analysis of the pre- and post-test physical fitness levels for AEG and ACG revealed significant differences in favor of AEG in terms of running speed and agility, balance I-II, standing long jump, right- and left-hand visual and auditory reactions, grip strength (both hands), and flexibility tests (p < 0.05). There were no significant differences with regard to the bilateral coordination tests (p > 0 .05).
For TDEG and TDCG, significant differences in favor of TDEG were observed in running speed and agility, balance II, right- and left-hand visual and auditory reactions, handgrip strength (both hands), and flexibility tests (p < 0.05). No significant differences were found with respect to bilateral coordination and the standing long jump (p > 0.05) (Table 4).
Table 4.
Comparison of pre- and post-test results for AEG and TDEG.
| The applied tests | AEG Pre-post-test difference (n = 7) | TDEG Pre-post-test difference (n = 7) | Mann-Whitney U Test |
||
|---|---|---|---|---|---|
| Mean Rank | Mean Rank | Z | p | ||
| Running speed and agility (sec) | 8.43 | 6.57 | −0.88 | 0.381 | |
| Balance (sec) | Balance –I | 10.50 | 4.50 | −3.02 | 0.003 ** |
| Balance –II | 10.64 | 4.36 | −3.00 | 0.003 ** | |
| Bilateral coordination | Coordination –I | 8.79 | 6.21 | −1.36 | 0.174 |
| Coordination –II | 7.93 | 7.07 | −0.42 | 0.674 | |
| Strength (cm) | Standing long jump | 11.00 | 4.00 | −3.39 | 0.001 ** |
| Reaction time (ms) | Right hand visual | 6.93 | 8.07 | −0.51 | 0.609 |
| Left hand visual | 7.29 | 7.71 | −0.19 | 0.848 | |
| Right hand audial | 4.43 | 10.57 | −2.75 | 0.006 ** | |
| Left hand audial | 4.29 | 10.71 | −2.88 | 0.004 ** | |
| Hand strength (kg) | Handgrip strength (right) | 10.71 | 4.29 | −2.89 | 0.004 ** |
| Handgrip strength (left) | 9.36 | 5.64 | −1.67 | 0.096 | |
| Flexibility (cm) | Sit and Reach Test | 8.57 | 6.43 | −0.99 | 0.326 |
p < 0.05.
p < 0.01.
Comparing the pre- and post-test differences in physical fitness for AEG and TDEG, we observed significant differences in favor of AEG in balance I-II, standing long jump, right- and left-hand auditory reactions, and right-hand grip strength tests (p < 0.05). There were no significant differences in running speed and agility, bilateral coordination I-II, right- and left-hand visual reactions, left-hand grip strength, and flexibility tests, however (p > 0.05).
Discussion
It has been reported that physical exercise contributes to effect on body mass indexes (BMI), motor coordination, dynamic balance, muscle strength, and academic achievement positively (Ferreira et al. 2018). Looking at the content of these effective exercise programs; It is stated that it was made 50–60% of the maximal heart rate is 8–36 weeks, 2–3 sessions per week and 20–40 min each session (Srinivasan et al. 2014). Stavrou et al. (2018) applied 3 sessions a week for 12 weeks to a child with a high-function ASC and an exercise program for 40–45 min of balance, personal awareness, group games, visual-motor coordination activities, movement, time, space and orientation games. At the end of 12 weeks, it was found that the child's behavior, skills and communication improved. However, in the literature, there is no study in which children with Autism Spectrum Status (ASC) and Typically Developing Children were taken and evaluated together with an inclusive physical activity program. Only in the study of Ferreira et al. (2018) 55 ASC and their peers (their peers with typical development) were given exercise programs by volunteer trainers. In the other study, the Inclusive Physical Activity Program, an exercise program including basic movement skills (object control, balance, locomotor skill), physical and perceptual motor skills, was applied 2 days a week for 3 months, 45 min a day. However, during the evaluation, it was found that only 55 individuals with ASC were followed up (Nalbant 2018). For this reason, this study aimed to determine the effects of a 12-week circuit exercise program on various physical fitness parameters of children with autism spectrum condition (ASC) and typically developing (TD) children.
The results of our study indicate that children with ASC may have experience more difficulties and problems in terms of strength, balance, postural stability, walking, joint flexibility, and running speed and agility compared with TD children. Therefore, they may have score lower than TD children in visual-motor and upper extremity coordination speed skills. The similar results were also reported in the prior studies; for example Green et al. (2009), Jansiewics (2006), Minshew et al. (2004), Pan (2008), Todd and Reid (2006), and Günal and Bumin (2007). The results of McCoy and Morgan (2020) study reported that adolescents with ASC participate in physical activity less frequently and are more likely to be overweight or obese compared to their normally developing peers. Pan (2008) compared the physical activity levels of primary school students with ASC and TD children during the school period, and the results of their study demonstrated that children with ASC engaged in very low levels of physical activity.
As a result of the twelve-week circuit exercise program implemented in our study, statistical analysis of the pre-post-test differences of AEG and ACG revealed significant differences in favor of AEG in running speed and agility, balance I-II, standing long jump, right-left hand visual and auditory reactions, right-left handgrip strength, and flexibility, while there was no significant difference in bilateral coordination results (p > 0.05). Kern et al. (2013) the study examined handgrip strength in participants diagnosed with an autism spectrum condition (ASC) as compared with neurotypical children. Thirty-three children, aged 2–17 years, with an ASD and 33 gender-, race-, and age-matched neurotypical controls were tested using a handgrip dynamometer. The handgrip strength in participants with an ASC was significantly (p < 0.0001) lower than the neurotypical controls. The mean handgrip strength was 39.4 ± 17.7 kg in children with ASC and 65.1 ± 26.7 kg in controls. The results support the hypothesis that children with an ASC have significantly poorer handgrip strength as compared with neurotypical children. The results of prior studies (Fragala-Pinkham et al. 2005, Yılmaz et al. 2004, Yanardag 2007, Magnusson et al. 2012, Srinivasan et al. 2014, Sowa and Meulenbroek 2012) suggested that different exercise programs undertaken by children with ASC resulting in a positive increase in balance, standing long jump, and running speed and agility. Also, the results of the Battaglia et al. (2019) study indicated that water sports generally have positive effects on the motor and social skills of individuals with atypical development.
As a result of the exercise program carried out in our study, positive increases were observed in a number of parameters related to gross motor skills in the AEG children, a finding supported by the literature. Because of this, we can confidently state that directing all children, especially those with ASC, to participate in exercise programs at an when diagnosed with autism, should be started immediately will contribute positively to their motor development. Our study found that the AEG children showed an improvement in balance parameters following their participation in the exercise program. However, Yanardag (2007) conducted a study with eight boys with ASC aged 5–7 participating in a 12-week exercise program consisting of three 40-minute sessions per week, and its results indicated that neither the pool nor the land group (both n = 4) showed a statistically significant difference in their balance parameters at the end of 12 weeks. It may be explained by the low mean age of the children (5–7 ages) and/or the shorter exercise time of only 40 minutes in study of Yanardag. Rad et al. (2012) examined the results of 20 children (n: 10 control, n: 10 experiments) with ASC, an average of 9 years old, who participated in an 8-week SPARK exercise program consisting of 45-minute sessions three times a week. SPARK the program included aerobic dance, running games, jumping rope and nine different sports. The Bruininks-Oseretsky Test of Motor Proficiency (BOTMP) was used to evaluates motor skills. At the end of 8 weeks, the results of their study demonstrated that the static balance and standing long jump parameters of the exercise group were significantly improved in comparison with those of the control group. However, there were no significant differences in bilateral coordination or running speed and agility. In our study, no statistically significant difference was found between the post-study developmental differences of both ASC and TD children participating in the exercise program. Rad et al. similar results were seen in their study. The bilateral coordination results were consistent with those of our study. The absence of a significant difference in running speed and agility may be due to the fact that the exercise program was limited to a period of only eight weeks. Based on the results of our study and similar studies cited above, the duration of an exercise program implemented with the goal of improving running speed and agility in children with ASC should be 10 weeks at minimum. In our study, no significant difference was observed between the pre-and post-test results for bilateral coordination in the AEG children. Bilateral coordination is defined as the ability to coordinate both sides of the body simultaneously in a controlled and organized manner. The development of bilateral coordination begins in the early stages of life and forms the basis for further motor development (Karambe et al. 2017). A study by Kaur et al. (2013) included fourteen typically developing children aged 4–7 and an 11-year-old high-functioning boy diagnosed with ASC. A robot imitation exercise program involving karate and dance actions was created for them to follow 30 min per day twice a week for four weeks. At the end of the study, the results demonstrated an improvement in the participants’ bilateral coordination. Bilateral coordination may vary up among individuals up to the age of six, developing significantly between the ages of seven and ten. As stated in the study of Rafie et al. (2016), bilateral coordination and response speed are considered complex perceptual-motor skills, which develop later than other skills. Najafabadi et al. (2018) investigated the effects of a 12-week SPARK exercise program, consisting of three 40-minute sessions per week, on the social and motor skills of 28 children with ASC between the ages of five and twelve. The program included aerobic dance, running games, jumping rope and nine different sports. The Bruininks-Oseretsky Test of Motor Proficiency (BOTMP) was used to evaluates motor skills. At the end of the exercise program, the results of their study indicated bilateral coordination and static and dynamic balance of the exercise group had significantly improved, consistent with the results of our study. Examining the SPARK program in more detail reveals that the activities engaged in were high intensity, of sufficiently long duration, and involving complex physical movements. We believe that the reason for the improvement in bilateral coordination results may be due to the variety of activities and the complex movements required to perform them. In our study, only rope pulling was used to assess bilateral coordination. In line with these findings, we recommend using exercise programs consisting of more complex motor movements for the development of bilateral coordination in children with ASC. In a study conducted by Yanardag (2007), eight boys with ASC aged 5–7 years old participated in an exercise program for 12 weeks, with three 40-minutes sessions per week. The boys were divided into two groups, one doing exercises in a pool (n = 4) and the other doing exercises on land (n = 4). At the end of 12 weeks, the results of the demonstrated that the changes in bilateral coordination results for both groups were non-significant similar to our findings.
In our study, the exercise program was found to positively affect the reaction time of AEG children. Reaction time is defined as the time between the start of a stimulus and that of motor behavior. In individuals with autism, reaction times are an important parameter for rapid motor response during physical activity (Baisch et al. 2017). The results of Wainwright-Sharp and Bryson (1993) study indicated that while children with ASC have been observed to respond to long-term stimuli in a manner similar to typically developing children, they show a decreased response to short-term stimuli compared to TD children. The exercise program implemented in the present study positively affected the reaction times of children with ASC to short-term stimuli. We can thus conclude that exercise programs engaged in regularly and over the long-term have a positive effect on reaction times.
Our exercise program also improved the handgrip strength and flexibility parameters of the AEG children. The results of prior studies (Fragala-Pinkham et al. 2005, Yılmaz et al. 2004, Rad et al. 2012, Yanardag et al. 2009) demonstrated that handgrip strength and flexibility parameters increased after children with ASC had engaged in an exercise program. In the limited studies on handgrip strength, diminished manual dexterity has been linked to not only poor handgrip strength but also delays in fine motor development in children with neurological motor problems. Alaniz et al. (2015) and Li-Tsang (2003) indicated that the finger and handgrip strength of individuals with ASC perform vital roles in pen control, handwriting legibility, and the ability to perform fine motor movements independently. Based on the results of our study, we can confidently state that the improvement in the handgrip strength of children with ASC can positively affect their academic and fine motor skills. In our study, we observed significant improvement in the flexibility parameters of the AEG children following exercise. The definition of flexibility relates to the extent to which a movement can be performed at the maximal joint range of motion (Shivalingaiah et al. 2016). Magnusson et al. (2012) studied six children with ASC who participated in a sixteen-session exercise program, completed in either 8 or 12 weeks, and the results of their study demonstrated that upon completion of the program the children’s flexibility had improved, although the difference was not statistically significant. Our study involved a total of 36 as opposed to only 16 exercise sessions, leading us to conclude that short-term exercise programs are not likely to have a significant positive effect on the development of flexibility in children with ASC. In a study by Pan (2011) involving15 twins with ASC (exercise = 7, control = 8) and fifteen typically developing twins (exercise = 7, control = 8), those in the exercise groups exercised in water twice a week for 14 weeks. At the end of this period, the results of Pan (2011) study showed an increase in flexibility was observed for the children with ASC in the exercise group, consistent with the results of our study.
As a result of the 12-week circuit exercise program implemented in our study, statistical analysis of the pre- and post-test physical fitness for TDEG and TDCG revealed significant differences in favor of TDEG in terms of running speed and agility, balance II, right- and left-hand visual and auditory reactions, right- and left-handgrip strength, and flexibility. No statistically significant difference was found, however, with respect to bilateral coordination (p > 0.05). Several studies on typically developing children who participated in exercise programs have reported significant differences comparing pre-and post-test values for sound and light reaction times, running speed and agility, and balance parameters (Kien and Chiodo 2003, Diallo et al. 2001, Ölçücü et al. 2011, Şirinkan 2011, Özmerdivenli 2004). In our study, the differences between TDEG pre-and post-test values for balance I and the standing long jump were not statistically significant because the children had already received maximum scores in centimeters and seconds for the pre-test based on the point scoring system used in BOT-2. Although the post-test values actually increased in terms of seconds and centimeters, the resulting differences were not statistically significant since the total point scores remained the same. Studies on the physical responses to exercise of typically developing children have found significant differences in handgrip strength and flexibility following participation in an exercise program (Ölçücü et al. 2011, Şirinkan 2011, Saygın et al. 2005, Şahin et al. 2012). Katie et al. (2003) reported a significant difference in handgrip strength in favor of those participating in regular physical education in comparison to children whose only structured physical activity in primary school consists of table tennis. Based on the results of our study as well as the findings of other studies, we believe that directing all children into physical education programs at an early age will contribute positively to their motor development and overall quality of life. Following the conclusion of the 12-week circuit exercise program in our study, statistical analysis of the differences of pre- and post-test physical fitness parameters for AEG and TDEG showed significant increases in favor of AEG in balance I-II, the standing long jump, right-and left-hand auditory reactions, and right-hand grip strength tests (p < 0.05). There were no significant differences in left-hand grip strength, flexibility, running speed and agility, coordination I-II, or right- and left-hand visual reaction tests (p > 0.05). Pan (2008) compared the physical activity levels of primary school students with ASC and typically developing children during the school year, and results suggested very low levels of physical activity for children with ASC. Individuals with ASC experience numerous challenges engaging in regular physical activity due to their difficulties in self-control, generalization, and planning, their typically low levels of motivation, and poor motor functions. In addition, they may, depending on the severity of their ASC condition, exhibit significant differences in gross and/or fine motor skills, and thus may prefer to abstain from participating in group games that require such skills. The results of Beversdorf et al. (2001) study demonstrated children with ASD may have sedentary lifestyles. This situation presents some problems when assessing the motor skills and physical fitness parameters of children with ASC. The most striking result obtained in our study was the observation that the difference in motor skills development in children with ASC following the exercise program was 30% (according to the difference of the total point scores of the pre and post test) higher than in TD children. In contrast, even when not engaging in structured exercise programs, typically developing children tend to be much more active than children with ASC, taking part in group play as part of their normal everyday lives, resulting in motor development levels superior to those of children with ASC. Therefore, the 30% greater development in motor skills that we observed in children with ASC as compared to TD children can easily be explained by the fact that children with ASC did stem from not leading an active life before. For this reason, it is of critical importance for individuals with ASC to engage in regular exercise, even at low intensity. The results of the prior studies (Yılmaz et al. 2004, Eichstaedt and Lavay 1992, Cornish and McManus 1996, Darıca et al. 2000, Lee and Vargo 2017) also stated the focus should be on basic motor skills, developmental activities that will lead to increased physical activity, sports, and individual play in exercise programs since children with ASC possess poor motor skills. The results of the Hamm and Yun (2019) study indicated that individuals with ASC can be used physical activity as a tool to improve their health-related quality of life. Kozlowski et al. (2020) in their work, demonstrated that a high-intensity exercise program is feasible, safe, and well-tolerated, and may yield significant physical improvements for children with ASC without ID. Gehricke et al. (2020) compared the physical activity levels of individuals with ASC aged 6–11 and 12–17. The results of their study indicated that adolescent males with ASC in the latter age group generally exhibited low levels of physical activity, which may negatively affect future health conditions, leading to higher obesity and other health problems. In similar context, the results of the Woodman et al. (2018) demonstrated that young students with ASC participated in exercises accompanied by especially slow music to combat obesity and by fast music to defend against other health problems. Based on the results of our study, we emphasize that directing children with ASC and TD children to participate in regular physical activity will positively affect their motor development skills as well as their overall health.
Conclusion
The data of our study obtained for AEG showed positive developments in running speed and agility, balance, the standing long jump, reaction times, handgrip strength, and flexibility tests. Statistical analysis of the differences between pre-test and post-test values for TDEG and AEG revealed significant differences in favor of AEG in balance I-II, the standing long jump, auditory hand reactions, hand grip strength tests. The AEG children showed approximately 30% more development overall compared to TDEG. Considering the positive effects of physical activity on children with ASC, it is a responsibility that parents, caregivers, and rehabilitation centers should take seriously. As the participants in the present study consisted only of boys, a similar study involving girls may be carried out in the future.
Consequently, we can emphasize that guiding both children with ASC and typically developing children to begin exercise programs and age-appropriate sports at an early stage will positively affect their development.
As with the majority of studies, the design of the current study is subject to limitation. The cognitive abilities of the participants were not measured which may have an impact on physical performance, motor skill performance, and physical activity in children with ASD. Conducting a similar study that measures ASC cognitive skills is planning as a future study.
Acknowledgements
The authors would like to express their sincere gratitude to the specialists at Ağrı Provincial State Hospital and to all the participants, along with their families, for their willingness to take part in this study. Also, the authors are very grateful to the reviewers and editor for their valuable comments which have substantially improved this paper.
Disclosure statement
The authors declare that they have no conflicts of interest.
References
- ADDM Community Report on Autism, 2018. Centers for Disease Control and Prevention. Available at: <http://www.cdc.gov/ncbddd/autism/addm-community-report/documents/addm-community-report-2018-h.pdf>.[ accessed 10 Sseptember, 2020].
- Alaniz, M. L., Galit, E., Necesito, C. I. and Rosario, E. R.. 2015. Hand strength, handwriting, and functional skills in children with autism. American Journal of Occupational Therapy, 69, 6904220030p1. 10.5014/ajot.2015.016022, [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (DSM-V) , 2013. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association [APA], 2000. The diagnostic and statistical manual of mental disorders. 4th ed. text revision (DSM‐IV‐TR). Washington, DC: American Psychiatric Pub. [Google Scholar]
- Baio, J., Wiggins, L., Christensen, D. L., Maenner, M. J., Daniels, J., Warren, Z., Kurzius-Spencer, M., Zahorodny, W., Robinson Rosenberg, C., White, T., Durkin, M. S., Imm, P., Nikolaou, L., Yeargin-Allsopp, M., Lee, L. C., Harrington, R., Lopez, M., Fitzgerald, R. T., Hewitt, A., Pettygrove, S., Constantino, J. N., Vehorn, A., Shenouda, J., Hall-Lande, J., Van Naarden Braun, K. and Dowling, N. F. 2018. Prevalence of autism spectrum disorder among children aged 8 years- autism and developmental disabilities monitoring network, 11 sites, United States, 2014. Morbidity and Mortality Weekly Report. Surveillance Summaries, 67, 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baisch, B., Cai, S., Li, Z. and Pinheiro, V.. 2017. Reaction time of children with and without autistic spectrum disorders. Open Journal of Medical Psychology, 06, 166–178. [Google Scholar]
- Battaglia, G., Agrò, G., Cataldo, P., Palma, A. and Alesi, M.. 2019. Influence of a specific aquatic program on social and gross motor skills in adolescents with autism spectrum disorders: Three case reports. Journal of Functional Morphology and Kinesiology, 4(2), 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beversdorf, D. Q., Anderson, J. M., Manning, S. E., Anderson, S. L., Nordgren, R. E., Felopulos, G. J. and Bauman, M. L.. 2001. Brief report: Macrographia in high-functioning adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 31, 97–101. [DOI] [PubMed] [Google Scholar]
- Bruininks, R. H. and Bruininks, B. D.. 2005. Bruininks-Oseretsky test of motor proficiency. 2nd ed. Minneapolis, MN: NCS Pearson. [Google Scholar]
- Carrigan, N. and Allez, K.. 2017. Cognitive behaviour therapy for post-traumatic stress disorder in a person with an autism spectrum condition and intellectual disability: A case study. Journal of Applied Research in Intellectual Disabilities, 30, 326–335. [DOI] [PubMed] [Google Scholar]
- Casassus, M., Poliakoff, E., Gowen, E., Poole, D. and Jones, L. A.. 2019. Time perception and autistic spectrum condition: A systematic review. Autism Research, 12, 1440–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark, M. P. A. and Westerberg, B.. 2009. How random is the toss of a coin? Canadian Medical Association Journal, 181, E306–E308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornish, K. M. and McManus, I. C.. 1996. Hand preference and hand skill in children with autism. Journal of Autism and Developmental Disorders, 26, 597–609. [DOI] [PubMed] [Google Scholar]
- Darıca, N., Gümüşçü, Ş. and Pişkin, Ü . 2000. Autism and autistic children, Volume 129. İstanbul: Özgür Yayınları. [Google Scholar]
- Dewey, D., Cantell, M. and Crawford, S. G.. 2007. Motor and gestural performance in children with autism spectrum disorders, developmental coordination disorder, and/or attention deficit hyperactivity disorder. Journal of the International Neuropsychological Society, 13, 246–256. [DOI] [PubMed] [Google Scholar]
- Diallo, O., Dore, E., Duche, P. and Van Praagh, E. 2001. Effects of plyometric training followed by a reduced training programme on physical performance in prepubescent soccer players. Journal of Sports Medicine and Physical Fitness, 41, 342–348. [PubMed] [Google Scholar]
- Eichstaedt, C. B. and Lavay, B. W.. 1992. Physical activity for individuals with mental retardation. Illinois: Human Kinetics Books, p. 463. [Google Scholar]
- Ferreira, J. P., Andrade Toscano, C. V., Rodrigues, A. M., Furtado, G. E., Barros, M. G., Wanderley, R. S. and Carvalho, H. M.. 2018. Effects of a physical exercise program (PEP-Aut) on autistic children's stereotyped behavior, metabolic and physical activity profiles, physical fitness, and health-related quality of life: A study protocol. Frontiers in Public Health, 6, 47. 10.3389/fpubh.2018.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fragala-Pinkham, M. A., Haley, S. M., Rabin, J. and Kharasch, V. S.. 2005. A fitness program for children with disabilities. Physical Therapy, 85, 1182–1200. [PubMed] [Google Scholar]
- Fransen, J., D'Hondt, E., Bourgois, J., Vaeyens, R., Philippaerts, R. M. and Lenoir, M.. 2014. Motor competence assessment in children: Convergent and discriminant validity between the BOT-2 Short Form and KTK testing batteries. Research in Developmental Disabilities, 35, 1375–1383. [DOI] [PubMed] [Google Scholar]
- García-Blanco, A. C., Yáñez, N., Vázquez, M. A., Marcos, I. and Perea, M.. 2017. a. Modulation of attention by socio-emotional scenes in children with autism spectrum disorder. Research in Autism Spectrum Disorders, 33, 39–46. [Google Scholar]
- García-Blanco, A. C., López-Soler, C., Vento, M., García-Blanco, M. C., Gago, B. and Perea, M.. 2017. b. Communication deficits and avoidance of angry faces in children with autism spectrum disorder. Research in Developmental Disabilities, 62, 218–226. [DOI] [PubMed] [Google Scholar]
- Gehricke, J.-G., Chan, J., Farmer, J. G., Fenning, R. M., Steinberg-Epstein, R., Misra, M., Parker, R. A. and Neumeyer, A. M.. 2020. Physical activity rates in children and adolescents with autism spectrum disorder compared to the general population. Research in Autism Spectrum Disorders, 70, 101490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gowen, E. and Hamilton, A.. 2013. Motor abilities in autism: A review using a computational context. Journal of Autism and Developmental Disorders, 43, 323–344. [DOI] [PubMed] [Google Scholar]
- Green, D., Charman, T., Pickles, A., Chandler, S., Loucas, T., Simonoff, E. and Baird, G.. 2009. Impairment in movement skills of children with autistic spectrum disorders. Developmental Medicine and Child Neurology, 51, 311–316. [DOI] [PubMed] [Google Scholar]
- Günal, A. and Bumin, G.. 2007. An investigation of motor performance in autistic children. Turkish Journal of Physiotherapy and Rehabilitation, 18, 179–186. [Google Scholar]
- Hamm, J. and Yun, J.. 2019. Influence of physical activity on the health-related quality of life of young adults with and without autism spectrum disorder. Disability and Rehabilitation, 41, 763–767. [DOI] [PubMed] [Google Scholar]
- Intaitė, M., Georgescu, A. L., Noreika, V., von Saldern, M. A., Vogeley, K. and Falter-Wagner, C. M.. 2019. Adults with autism spectrum condition have atypical perception of ambiguous figures when bottom-up and top-down interactions are incongruous. Autism: The International Journal of Research and Practice, 23, 1133–1142. [DOI] [PubMed] [Google Scholar]
- Işık, M. and Zorba, E.. 2020. The effects of hemsball on the motor proficiency of students with intellectual disabilities. International Journal of Developmental Disabilities, 66, 104–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansiewics, E. M. 2006. Motor signs distinguish children with high functioning autism and Asperger's syndrome from controls. Journal of Autism and Developmental Disorders, 36, 613–621. [DOI] [PubMed] [Google Scholar]
- Jírovec, J., Musálek, M. and Mess, F.. 2019. Test of motor proficiency second edition (BOT-2): compatibility of the complete and Short Form and its usefulness for middle-age school children. Frontiers in Pediatrics, 7, 153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karambe, P., Dhote, S. N. and Palekar, T. J.. 2017. Assessment of bilateral coordination using Bruininks-Oseretsky test of motor proficiency, 2nd edition (bot-2), in 5 to 15 years school going children. International Journal of Physiotherapy and Research, 5, 2026–2030. doi: 10.16965/ijpr.129. [DOI] [Google Scholar]
- Katie, M. M., Brad, S. M., Joanne, K., Linda, D. V. and Terence, J. W. 2003. Contribution of timetabled physical education to total physical activity in primary school children. Cross Sectional Study, BMJ, 13, 327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur, M., Gifford, T., Marsh, K. L. and Bhat, A.. 2013. Effect of robot–child interactions on bilateral coordination skills of typically developing children and a child with autism spectrum disorder: A preliminary study. Journal of Motor Learning and Development, 1, 31–37. [Google Scholar]
- Kern, J. K., Geier, D. A., Adams, J. B., Troutman, M. R., Davis, G. A., King, P. G. and Geier, M. R. 2013. Handgrip strength in autism spectrum disorder compared with controls. The Journal of Strength & Conditioning Research, 27, 2277–2281. [DOI] [PubMed] [Google Scholar]
- Kien, C. L. and Chiodo, A. R.. 2003. Physical activity in middle school-aged children participating in a school-based recreation program. Archives of Pediatrics & Adolescent Medicine, 157, 811–815. [DOI] [PubMed] [Google Scholar]
- Kirkendall, R. D., Gruber J. J. and Johnson, R. E. 1987. Measurement and evaluation for physical educators. Champaign, IL: Human Kinetics Publishers Inc., p. 553. [Google Scholar]
- Kozlowski, K. F., Lopata, C., Donnelly, J. P., Thomeer, M. L., Rodgers, J. D. and Seymour, C. 2020. Feasibility and associated physical performance outcomes of a high-intensity exercise program for children with autism. Research Quarterly for Exercise and Sport, 1–12.doi: 10.1080/02701367.2020.1726272 [DOI] [PubMed]
- Krithikadatta, J. 2014. Normal distribution. Journal of Conservative Dentistry, 17, 96–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, J. and Vargo, K. K.. 2017. Physical activity into socialization: A movement-based social skills program for children with autism spectrum disorder. Journal of Physical Education, Recreation and Dance, 88, 7–13. [Google Scholar]
- Lipinski, S., Blanke, E. S., Suenkel, U. and Dziobek, I.. 2019. Outpatient psychotherapy for adults with high-functioning autism spectrum condition: Utilization, treatment satisfaction, and preferred modifications. Journal of Autism and Developmental Disorders, 49, 1154–1168. [DOI] [PubMed] [Google Scholar]
- Li-Tsang, C. W. P. 2003. The hand function of children with and without neurological motor disorders. The British Journal of Development Disabilities, 49, 99–110. [Google Scholar]
- Magnusson, J. E., Cobham, C. and McLeod, R. 2012. Beneficial effects of clinical exercise rehabilitation for children and adolescents with autism spectrum disorder. Journal of Exercise Physiology, 15, 71–79. [Google Scholar]
- McCoy, S. M. and Morgan, K.. 2020. Obesity, physical activity, and sedentary behaviors in adolescents with autism spectrum disorder compared with typically developing peers. Autism, 24, 387–399. [DOI] [PubMed] [Google Scholar]
- Minshew, N. J., Sung, K., Jones, B. L. and Furman, J. M.. 2004. Underdevelopment of the postural control system in autism. Neurology, 63, 2056–2061. [DOI] [PubMed] [Google Scholar]
- Mülazımoglu Balli, Ö. 2006. The study of validity and reliability of Bruininks-Oseretsky motor proficiency test and the effects of gymnastics education program on motor development of five-six–years–old children. PhD Thesis. Ankara University, Ankara. [Google Scholar]
- Mülazımoğlu-Ballı, Ö. and Gürsoy, F.. 2012. The study of validity and reliability of Bruininks-Oseretsky motor proficiency test for five-six– year–old Turkish children. Hacettepe Journal of Sport Sciences, 23, 104–118. [Google Scholar]
- Muratlı, S. 1997. Child and sport. 1st ed. Ankara: Kültür Matbaası, pp. 135–167. [Google Scholar]
- Najafabadi, M. G., Sheikh, M., Hemayattalab, R., Memari, A.-H., Aderyani, M. R. and Hafizi, S.. 2018. The effect of SPARK on social and motor skills of children with autism. Pediatrics & Neonatology, 59, 481–487. [DOI] [PubMed] [Google Scholar]
- Nalbant, S. 2018. Effects of participation in inclusive physical activity on social skills of individuals with autism spectrum disorder. Journal of Education and Training Studies, 6, 255–261. [Google Scholar]
- Ölçücü, B., Cenikli, A., Kaldırımcı, M. and Bostancı, Ö . 2011. The effects of movement training with and without ball on physical fitness of tennis playing children. Journal of Sports and Performance Researches, 2(1), 32–40. [Google Scholar]
- Özmerdivenli, R., Öztürk, A. and Karacabey, K. 2004. The comparison of reaction times sedantery subjects and sportsman and the effect of exercise on some physiological parameters. Doğu Anadolu Bölgesi Araştırmalar, 2(2), 81–86. [Google Scholar]
- Ozonoff, S., Young, G. S., Goldring, S., Greiss-Hess, L., Herrera, A. M., Steele, J., Macari, S., Hepburn, S. and Rogers, S. J.. 2008. Gross motor development, movement abnormalities, and early identification of autism. Journal of Autism and Developmental Disorders, 38, 644–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan, C. Y. 2008. Objectively measured physical activity between children with autism spectrum disorders and children without disabilities during inclusive recess settings in Taiwan. Journal of Autism and Developmental Disorders, 38, 1292–1301. [DOI] [PubMed] [Google Scholar]
- Pan, C. Y. 2011. The efficacy of an aquatic program on physical fitness and aquatic skills in children with and without autism spectrum disorders. Research in Autism Spectrum Disorders, 5, 657–665. [Google Scholar]
- Piek, J. P. and Dyck, M. J.. 2004. Sensory-motor deficits in children with developmental coordination disorder, attention deficit hyperactivity disorder and autistic disorder. Human Movement Science, 23, 475–488. [DOI] [PubMed] [Google Scholar]
- Rad, L. S., Rafiee, F. and Fahimi, S. H. 2012. The effect of selected physical exercises on gross motor skills of autistic children. International Journal of Sport Studies, 2, 50–57. [Google Scholar]
- Rafie, F., Ghasemi, A., Jam, A. Z. and Jalali S. 2016. Effect of exercise intervention on the perceptual-motor skills in adolescents with autism. The Journal of Sports Medicine and Physical Fitness, 57, 53–59. [DOI] [PubMed] [Google Scholar]
- Sahuquillo-Leal, R., Ghosn, F., Moreno-Giménez, A., Almansa, B., Serrano-Lozano, E., Ferrín, M. and García-Blanco, A. 2020. Jumping to conclusions in autism: Integration of contextual information and confidence in decision-making processes. European Child and Adolescent Psychiatry, 29(7),959–968. [DOI] [PubMed] [Google Scholar]
- Saygın, Ö., Polat, Y. and Karacabey, K. 2005. The effects of movement training, applied to children on their physical fitness parameters. Fırat University Medical Journal of Health Sciences, 19, 205–212. [Google Scholar]
- Schloss, P. J., Smith, M. A. and Schloss, C. A. 2001. Instructional methods for secondary students with learning and behavior problems. Boston, MA: Allyn and Bacon. [Google Scholar]
- Shivalingaiah, J., Vernekar, S., Naik, A. and Gowdar, S.. 2016. Effect of training on agility, flexibility, its correlation, and also its correlation with skin fold thickness and body mass index among runners. National Journal of Physiology, Pharmacy and Pharmacology, 6, 505–509. [Google Scholar]
- Simmons, D. R., Robertson, A. E., McKay, L. S., Toal, E., McAleer, P. and Pollick, F. E.. 2009. Vision in autism spectrum disorders. Vision Research, 49, 2705–2739. [DOI] [PubMed] [Google Scholar]
- Sowa, M. and Meulenbroek, R.. 2012. Effects of physical exercise on autism spectrum disorders: A meta-analysis. Research in Autism Spectrum Disorders, 6, 46–57. [Google Scholar]
- Srinivasan, S. M., Pescatello, L. S. and Bhat, A. N.. 2014. Current perspectives on physical activity and exercise recommendations for children and adolescents with autism spectrum disorders. Physical Therapy, 94, 875–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Şahin, M., Saraç, H., Çoban, O. and Çoşkuner, Z. 2012. An Investigation of the Effects of Taekwondo Training on the Motor Development Levels of Children. Journal of Sports and Performance Researches, 5(1), 5–14. [Google Scholar]
- Şirinkan, A. 2011. Study of physical suitability of football school students in 7-12 age group with tests of eurofit (the example of the city of Erzurum). e-Journal of New World Sciences Academy, 6(3), 178–184. [Google Scholar]
- Stavrou, K., Tsimaras, V., Alevriadou, A. and Gregoriadis, A.. 2018. The effect of an exercise program on communication and behavior of a child with autism spectrum disorder. Pedagogics, Psychology, Medical-Biological Problems of Physical Training and Sports, 22, 99–106. [Google Scholar]
- Suresh, K. P. 2011. An overview of randomization techniques: An unbiased assessment of outcome in clinical research. Journal of Human Reproductive Sciences, 4, 8–11. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Tamer, K. 2000. Measurement and evaluation of physical performance in sport. Ankara: Bağırgan Publications. [Google Scholar]
- Tekin-İftar, E. and Kırcaali-İftar, G.. 2006. Errorless teaching methods in special education. 3rd ed. Ankara: Nobel Yayın Dağıtım, p. 96. [Google Scholar]
- Todd, T. and Reid, G.. 2006. Increasing physical activity in individuals with autism. Focus on Autism and Other Developmental Disabilities, 21, 167–176. [Google Scholar]
- Wainwright-Sharp, J. A. and Bryson, S. E.. 1993. Visual orienting deficits in high-functioning people with autism. Journal of Autism and Developmental Disorders, 23, 1–13. [DOI] [PubMed] [Google Scholar]
- Woodman, A., Breviglia, E., Mori, Y., Golden, R., Maina, J. and Wisniewski, H.. 2018. The effect of music on exercise intensity among children with autism spectrum disorder: A pilot study. Journal of Clinical Medicine, 7, 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanardag, M. 2007. Effects of the different exercise training on motor performance and stereotypical behaviors of children with autism. Ph.D. dissertation. Hacettepe University. [Google Scholar]
- Yanardağ, M., Ergun, N. and Yılmaz, İ . 2009. The effect of adapted exercise education on physical fitness in children with autism. Turkish Journal of Physiotherapy and Rehabilitation, 1, 25–31. [Google Scholar]
- Yılmaz, İ., Yanardağ, M., Birkan, B. and Bumin, G. 2004. Effects of swimming training on physical fitness and water orientation in autism. Pediatrics International, 46, 624–626. [DOI] [PubMed] [Google Scholar]