Abstract
Background:
There is sparse literature demonstrating the relationship between lower limb pediatric idiopathic rotational malalignment (IRM) and patient-reported outcomes measurement information system (PROMIS) scores. Our goal is to determine and quantify the amount that IRM deformities, as measured with the 3D gait analysis, affect childrens’ pain interference, mobility, and peer relationship PROMIS domains. Secondary outcomes include investigating the potential relationships between IRM and various subgroups (Pediatric Outcomes Data Collection Instrument (PODCI), gender, Body Mass Index (BMI), femur Versus tibia). We also examine whether the PROMIS domains correlate with PODCI in this population.
Methods:
This study was a retrospective cohort, single institution, and consecutively recruited cases series. We identified 47 children over a 3-year period who were evaluated at the motion analysis center at our tertiary care hospital, with increased torsion of the femur or tibia. After exclusions, 25 children with IRM, documented PROMIS data and gait analysis were considered.
Results:
Femoral malrotation had a significant relationship with female gender (P=0.001) and increased BMI (P<0.001). Femoral malrotation had a correlation with PROMIS pain interference (P=0.016), whereas tibial rotation did not achieve significance (P=0.084). In the ANOVA regression analysis, there was a strong prediction of the PROMIS mobility domain when both malrotation and pain interference were present (P=0.007). There were Pearson Correlations of PROMIS and PODCI domains for Mobility Versus Sports (P=0.007) and Pain Interference Versus Comfort/Pain (P=0.004), respectively.
Conclusion:
The evident relationship between lower limb rotational malalignment and PROMIS scores signifies the likelihood for gait and pain disturbance. This in turn could show us that children are likely to be more debilitated and thus may benefit from timely correction. We aim to conduct this as a multicentre trial to confirm our findings.
Level of Evidence:
Level IV.
Key Words: torsion, lower limb, patient reported outcome measure, tibia, gait analysis, pediatric, orthopaedics
Idiopathic rotational malalignment (IRM) is a relatively common complaint that comprises 16% of new referrals to pediatric orthopaedic surgeons.1 IRM in children is a condition that is still not clearly defined, which leads to difficulty in advocating for management options.2
IRM can originate from multiple levels including the femur, tibia, and foot. The foot progression angle often improves with age but persistent femoral and tibial torsion can cause ongoing deformity. Deformity usually manifests as in-toeing or out-toeing, which is contributed by excessive inward or outward femoral torsion and/or tibial torsion. Generally, in-toeing tends to resolve with increasing skeletal maturity whereas out-toeing is a more recalcitrant condition.3
Aspects of this condition that have been studied includes kinematic outcomes after femoral or tibial osteotomies3,4 and the biomechanical implications of IRM, such as increased patellofemoral pressures associated with increased femoral anteversion and external tibial torsion.5 Although IRM in children is frequently quoted as causing pain, difficulty keeping up with peers, tripping, cosmetic concerns, and psychological effects,6 little has been studied in regards to both the functional limitations and psychological effects of rotational malalignment on children themselves.
Patient-reported outcome measures (PROMs) are increasingly important in determining the impact of a disease state on children and determining the effectiveness of treatments.7 There are numerous different outcome measures including disease-specific and general outcome measures. In 2004, the National Institute of Health attempted to create an easily interpreted general outcome measure that could be applied to multiple disease states and test various health domains called the patient-reported outcomes measurement and information system (PROMIS).8,9 Pediatric PROMIS can be administered to children from ages 5 to 17 by a parent proxy and from ages 8 to 17 by self-reporting.
Traditionally, the Pediatric Outcomes Data Collection Instrument (PODCI) has been used for pediatric PROMs in orthopaedic surgery, and is validated as being specific to musculoskeletal health in children and adolescents.10 It was developed by the Pediatric Orthopedic Society of North America and the American Academy of Orthopedic Surgeons in 1998. One limitation of PODCI is that it is time-consuming to administer. Pediatric PROMIS, in contrast, has less than half the number of questions (37 vs. 86) and may be less of a burden on participating children and caregivers.
As such, PROMIS has been increasingly utilized and studied in adult musculoskeletal populations and has been shown to outperform several legacy measures in rotator cuff disease,11 orthopaedic trauma,12 rheumatoid arthritis13, and adult spine patients.14,15 The adult PROMIS subscale correlations are mirrored in the pediatric population.16 Despite this, there is little literature studying the relationship of pediatric musculoskeletal conditions and PROMIS.17,18
The primary goal for this study was to add to the body of literature, which is sparse in this area. Specifically, our hypothesis is that IRM leads to worse PROMIS scores in the mobility, pain interference, and peer relationship domains.
Secondary goals involved identifying factors influencing PROMIS scores in patients with IRM such as gender, age, BMI, location of deformity, and direction/magnitude of deformity. We also aimed to evaluate the relationship between PROMIS scores and both static and dynamic rotational deformity as measured by 3D motion analysis. In addition, we aimed to see whether any correlation exists between PROMIS and the more traditional PODCI outcome tool.
METHODS
This was a retrospective cohort, single institution, consecutively recruited case series study. We enrolled patients who had increased torsion of the femur or tibia from a tertiary care center utilizing the motion analysis center clinical database. Patients were enrolled whether they had IRM and a concomitant gait analysis.
For our inclusion criteria, the children were part of the study whether they were between 6 and 18 years of age. They all had a gait analysis for rotational malalignment performed within the last 3 years (between November 2017 and April 2020). They needed to have successfully completed the PROMIS outcome tool.
In addition, the clinical examination needed to be consistent with rotational malalignment including one of either excessive internal femoral torsion, excessive external femoral torsion, excessive internal tibial torsion, or excessive external tibial torsion. These diagnoses were determined by the treating physician and recorded in the clinical database. The patients were excluded whether they had neurological impairment, developmental delay, or prior lower extremity surgery.
The gait analysis included a comprehensive history and physical examination, complete kinematics, video recording of the gait, and kinetic analysis if possible (no assistive device). The motion analysis was performed with a ten infrared camera VICON Motion system (Vicon, Oxford, UK) at a sampling frequency of 100 Hz utilizing 5 AMTI (Advanced Mechanical Technology, Inc., Watertown, MA, USA) force plates and VICON Software. After the collection of anthropometric data, patients had retro-reflective markers placed at several anatomic landmarks: the base of the sacrum midway between the posterior superior iliac spines, both anterior superior iliac spines, the lateral epicondylar ridge of the distal end of the femur along the flexion-extension axis of the knee, the lateral aspect of the thigh along the axis of the knee (on a ten-centimeter-long aluminum wand fastened here), the most prominent point of the lateral malleolus along the transmalleolar axis (on an aluminum wand), and the mid-foot between and slightly proximal to the second and third metatarsal heads. The children walked at their self-selected speed until at least 3 trials were performed and subsequently recorded, and the average of the 3 trials of each subject was used in the statistical analysis.
Given previous studies advocated the accuracy of 3D gait analysis measures over physical examination, we concentrated on using these parameters for rotation interpretation. This is owing to unreliable physical measurements, and poor inter-observer and intra-observer reliability of bedside examinations.19 Measures of pelvic rotation, femoral rotation, tibial rotation, foot rotation and foot progression angle were calculated and recorded during the above described gait analysis. If the patient had bilateral IRM, we utilized the side that had the more severe deformity. Although 3D Magnetic Resonance Imaging and EOS low radiation imaging have been used to aid in torsional modelling, no imaging was included for these children as it is not our standard practice. For spatial-temporal gait parameters we collected cadence, velocity, and stride length.
Outcome tools used were the PROMIS and PODCI scores. The PROMIS was completed at the time of clinical review in the surgeon’s outpatient clinic on an electronic tablet device and were performed by the patient with the parent’s aid where required. The PODCI scores were collected during the gait lab visit. In some instances, for the PODCI domains, both the patient and the parent documented separate scores.
The PROMIS domains recorded include mobility, upper extremity function, pain interference, and peer relationship. PODCI domains were upper limb, transfers, sports, comfort/pain, global, and happiness.
We investigated the relationships of torsion to PROMIS domains. The study protocol was submitted to the Institutional Review Board (IRB) and approved in 2015. The statistical analysis was performed using SPSS software (version 27.0.0). Pearson correlation coefficients were used to examine the relationship between passive range of motion, gait variables, and PODCI and PROMIS scores in addition to examining the relationship between PODCI and PROMIS scores. Multiple linear regressions were performed to examine whether rotational parameters predicted PROMIS scores. The implementation of PROMIS in the clinic began in December 2017. Because of the limited number of patients that would be available to include in this study an a priori power analysis was not performed and all patients meeting the inclusion criteria of the study were included. To avoid the risk of type I error we used Bonferroni corrections because of the presence of multiple comparisons. These were calculated by category: passive range of motion (0.05/4=0.0125), gait parameters (0.05/3=0.0167), and gait kinematics (0.05/3=0.0167).
RESULTS
From the original 47 patients, 22 were excluded because of incomplete PROMIS data (21 patients) and incomplete gait analysis data (1 patient). We had a total of 25 children with IRM after exclusions. The average age in years was 13.1±2.4, and in our group there were more males than females (15 vs. 10). There were similar numbers of both femoral and tibial torsion (12 vs. 13), and also external Versus internal torsion (13 vs. 12).
Passive clinical examination measures are presented in Table 1. There was a significant relationship between elevated BMI and both internal (r=−0.741, P=0.001) and external (r=0.591, P=0.001) femoral torsion. None of the passive clinical examination measures showed a statistically significant correlation with PROMIS scores.
TABLE 1.
Passive Examination
| Passive examination | Excessive external femoral torsion (n=7) | Excessive internal femoral torsion (n=5) | Excessive external tibial torsion (n=6) | Excessive internal tibial torsion (n=7) |
|---|---|---|---|---|
| Hip external rotation | 59±15 | 22±12 | 48±26 | 29±9 |
| Hip internal rotation | 24±16 | 73±15 | 53±19 | 64±8 |
| Foot thigh angle | 14±5 | 10±6 | 30±5 | −3±6 |
| Transmalleolar axis | 21±5 | 22±6 | 38±7 | 11±6 |
Mean and SD for each diagnosis.
Kinematic values for this cohort are presented in Table 2. Femoral malrotation during gait had a significant relationship with female gender (r=0.628, P=0.001) and elevated BMI (r=−0.739, P<0.001). No statistically significant relationship was observed between foot progression and promis peer relationship scores (r=0.395, P=0.05). Absolute femoral malrotation had a statistically significant correlation with PROMIS pain interference (r=0.467, P=0.016) (Fig. 1); however, no significant relationship was found between absolute tibial rotation and PROMIS pain interference (r=−0.346, P=0.084).
TABLE 2.
Kinematics, Spatio-Temporal Parameters, PROMIS and PODCI Domains
| Excessive external femoral torsion (n=7) | Excessive internal femoral torsion (n=5) | Excessive external tibial torsion (n=6) | Excessive internal tibial torsion (n=7) | |
|---|---|---|---|---|
| Kinematics | ||||
| Pelvis rotation (mean of stance) | 1±3 | 0±3 | −1±3 | 1±3 |
| Femoral rotation (mean of stance) | −15±8 | 15±5 | 1±7 | 1±6 |
| Tibial rotation (mean of stance) | −14±5 | −23±7 | −40±9 | −4±5 |
| Foot progression angle (mean of stance) | −23±16 | 0±6 | −33±13 | 8±6 |
| Spatio-temporal parameters | ||||
| Cadence | 97±11 | 98±9 | 94±11 | 95±10 |
| Velocity | 91±19 | 100±18 | 86±18 | 91±13 |
| Stride length | 93±14 | 102±10 | 91±15 | 96±8 |
| PROMIS domain | ||||
| PROMIS score mobility | 44±10 | 47±13 | 39±7 | 47±8 |
| PROMIS score upper extremity | 50±8 | 51±10 | 39±15 | 53±7 |
| PROMIS score pain interference | 50±10 | 44±12 | 44±8 | 41±8 |
| PROMIS score peer relationship | 46±11 | 51±5 | 43±11 | 53±10 |
| PODCI domain | ||||
| PODCI Xfers | 89±17 | 96±5 | 94±10 | 94±7 |
| PODCI sports | 65±25 | 77±27 | 63±28 | 64±16 |
| PODCI comf/pain | 57±29 | 63±27 | 70±26 | 56±34 |
| PODCI global | 76±19 | 82±17 | 78±17 | 78±15 |
| PODCI happiness | 68±31 | 92±13 | 66±27 | 64±22 |
Mean and SD for each diagnosis. A negative number means external rotation.
PODCI indicate pediatric outcomes data collection instrument; PROMIS, patient reported outcomes measurement information system.
FIGURE 1.
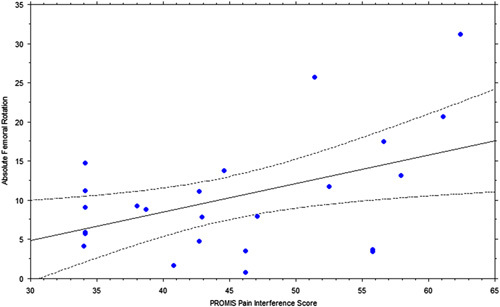
Graph of PROMIS pain interference domain (score) Versus absolute femoral rotation (degrees).
All spatio-temporal parameter measurements are shown in Table 2. Cadence did not show any correlation with PROMIS domains but was approaching statistically significant correlation with PROMIS Peer Relationship (P=0.055). Stride length was correlated with PROMIS Mobility (r=0.489, P=0.01) and PROMIS Peer Relationship (P=0.006). The velocity was correlated with PROMIS mobility (r=0.497, P=0.01) and PROMIS peer relationship (r=0.528, P=0.006).
In relation to rotation, PROMIS and PODCI scores are shown in Table 2. Neither absolute tibial nor absolute femoral rotation significantly predicted PROMIS mobility, (F=1.36, P=0.278). When PROMIS pain interference was added into the model, the 3 variables together predicted PROMIS mobility (F=5.32, P=0.007), explaining 43.2% of the variance; however, only pain interference contributed significantly to the model (t=−3.449, P=0.002).
No significant relationship was found between PROMIS mobility and PODCI transfers and mobility. There were correlations between PROMIS mobility and PODCI sports domains (r=0.519, P=0.007) (Fig. 2), and PROMIS pain interference and PODCI Comfort/Pain (r=−0.548, P=0.004) (Fig. 3).
FIGURE 2.
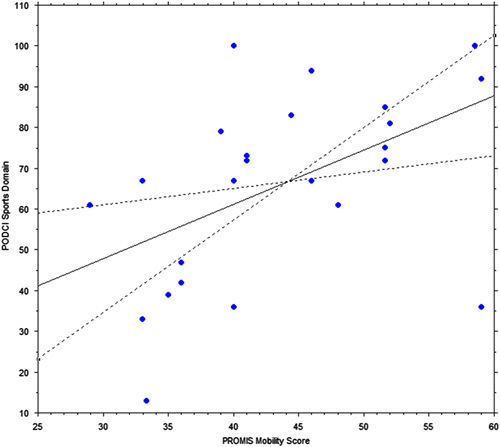
Graph of PROMIS mobility score Versus PODCI sports domain score.
FIGURE 3.
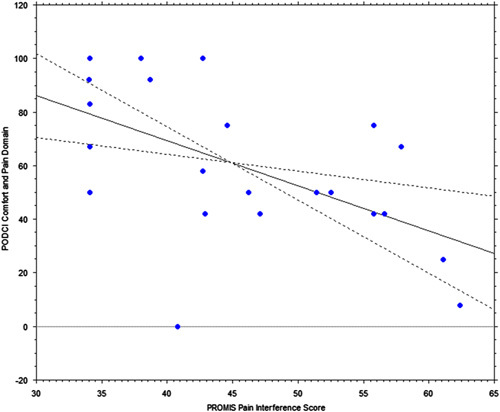
Graph of PROMIS pain interference score Versus PODCI comfort and pain domain score.
DISCUSSION
The goal of our study was to determine the relationships of femoral and tibial torsion to PROMIS domains in children. We used kinematic gait study data and PROMs to demonstrate that there are certain correlations that may be pertinent for our clinical practice.
Although we had more male patients, the higher predilection of malrotation in females is commonly noted in the literature with females generally having increased rates of femoral internal torsion.20,21 The increased prevalence of femoral external rotation in children with high BMI was again confirmed in the literature, with higher rates of femoral external rotation seen in our high BMI group (P=0.001).21
As mentioned earlier, we did not concentrate on using the passive examination measures in quantifying the rotation owing to inaccuracies as evidenced by prior research.19 This is reinforced by the fact that none of our passive measures correlated with PROMIS scores or were statistically significant.
A significant finding in our study was the strong relationship between absolute femoral malrotation and increased PROMIS pain scores (P=0.016). This is also supported by a very recent study demonstrating high pain prevalence (85%) in pediatric patients with increased internal hip rotation (P=0.002) or decreased external hip rotation (P<0.001).22 Thus, it seems that pain is directly proportional to femoral/hip malrotation. The clinical implication of this has not been clearly elucidated; however, our results show that patients with malrotation and pain had poorer PROMIS mobility scores (P=0.002). This is supported by preexisting evidence revealing that increased femoral anteversion results in poorer lower extremity function and increased fall frequency. These patients have statistically significant increase in fall frequency (P=0.02), which is especially noted during running and fast walking.23 The consequences of this are that these patients are likely more prone to injuries, especially during highly mobile sports that include running. 3D gait analysis has highlighted the notion that abnormal hip torsion may not just be a cosmetic issue as it causes alterations in all lower limb joints, thus leading to gait issues.24
It was interesting to note that the PODCI scores between both the patient and parent correlated strongly and were statistically significant in all subdomains. The literature does describe good correlation between patient and parent PODCI in lower severity diseases.25 This shows that the parents’ interpretation of the patients’ function and overall well-being is generally quite accurate.
We do acknowledge that there are limitations in our study. Our sample size is relatively small; owing to the fact this was conducted at a single institution and using strict inclusion/exclusion criteria. Malrotation at either the tibia or femur with either excessive internal and external rotation were analyzed as one cohort because of the small sample size. There may be disparities between tibial and femoral malrotation but the number is too small for statistical comparison between these groups. Also being a retrospective study, which is designed to analyze preexisting data, there is the potential for selection biases. Only participants with malrotation who underwent gait analysis as part of their evaluation were analyzed. Another limitation is that the marker placement is reliant on the physical therapist’s clinical assessment. This is particularly an issue in the overweight children in whom the body habitus can compromise optimal marker positioning. Because of these findings, we aim to do a multicenter study whilst maintaining blinding as to site, gaining a larger sample size, confirming our findings, and potentially finding further correlations.
CONCLUSION
Femoral and tibial rotation are correlated with PROMIS pain interference, indicating that more rotation results in more pain interference. In addition, femoral and tibial rotation with increased PROMIS pain interference contributes significantly to a worse PROMIS mobility score. Finally, the relationship between PROMIS and PODCI domains demonstrates the credibility of this tool in evaluating IRM and the value of appropriate management.
The evident relationship between lower limb rotational malalignment and PROMIS scores signifies the likelihood for gait and pain disturbance. This in turn could show us that children are likely to be more debilitated and thus may benefit from timely correction. We aim to conduct this as a multicenter trial to confirm our findings.
Footnotes
Contributions: J.C.: study design, data collection, data interpretation, manuscript write-up, and manuscript editing. R.H.: study design, data collection, and manuscript editing. D.B.: study conception, study design, data interpretation, and manuscript editing. E.R.: study conception, study design, data interpretation, and manuscript editing. J.P.B.: study conception, study design, data interpretation, manuscript write-up, and manuscript editing.
D.B. is consultant for Medtronic. The remaining authors have no conflict of interest to declare.
Contributor Information
Janan Chandrananth, Email: janan.chandrananth@gmail.com.
Richard Hannan, Email: rjhannan@gmail.com.
Daniel Bouton, Email: dbouton@shrinenet.org.
Ellen Raney, Email: eraney@shrinenet.org.
Susan Sienko, Email: ssienko@shrinenet.org.
Patrick Do, Email: pdo@shrinenet.org.
Jeremy P. Bauer, Email: jpbauer@shrinenet.org.
REFERENCES
- 1. Reeder B, Lyne ED, Patel DR, et al. Referral patterns to a pediatric orthopedic clinic: implications for education and practice. Pediatrics. 2004;113:e163–e167. [DOI] [PubMed] [Google Scholar]
- 2. Gruskay J, Fragomen A, Rozbruch SR. Idiopathic rotational abnormalities of the lower extremities in children and adults. JBJS Rev. 2019;7:e3. [DOI] [PubMed] [Google Scholar]
- 3. Davids JR, Davis RB, Jameson LC, et al. Surgical management of persistent intoeing gait due to increased internal tibial torsion in children. J Pediatr Orthop. 2014;34:467–473. [DOI] [PubMed] [Google Scholar]
- 4. Stevens PM, Gililland JM, Anderson LA, et al. Success of torsional correction surgery after failed surgeries for patellofemoral pain and instability. Strategies Trauma Limb Reconstr. 2014;9:5–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Passmore E, Graham HK, Pandy MG, et al. Hip- and patellofemoral-joint loading during gait are increased in children with idiopathic torsional deformities. Gait Posture. 2018;63:228–235. [DOI] [PubMed] [Google Scholar]
- 6. Naqvi G, Stohr K, Rehm A. Proximal femoral derotation osteotomy for idiopathic excessive femoral anteversion and intoeing gait. SICOT-J. 2017;3:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Marshall S, Haywood K, Fitzpatrick R. Impact of patient-reported outcome measures on routine practice: a structured review. J Eval Clin Pract. 2006;12:559–568. [DOI] [PubMed] [Google Scholar]
- 8. Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol. 2010;63:1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cella D, Yount S, Rothrock N, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care. 2007;45(5 Suppl 1):S3–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Daltroy LH, Liang MH, Fossel AH, et al. The POSNA pediatric musculoskeletal functional health questionnaire: report on reliability, validity, and sensitivity to change. J Ped Orthop. 1998;18:561–571. [DOI] [PubMed] [Google Scholar]
- 11. Beckmann JT, Hung M, Bounsanger J, et al. Psychometric evaluation of the PROMIS Physical Function Computerized Adaptive Test in comparison to the American Shoulder and Elbow Surgeons score and Simple Shoulder Test in patients with rotator cuff disease. J Shoulder Elbow Surg. 2015;24:1961–1967. [DOI] [PubMed] [Google Scholar]
- 12. Hung M, Stuart AR, Higgins TF, et al. Computerized adaptive testing using the PROMIS Physical Function Item Bank reduces test burden with less ceiling effects compared with the short musculoskeletal function assessment in orthopaedic trauma patients. J Orthop Trauma. 2014;28:439–443. [DOI] [PubMed] [Google Scholar]
- 13. Oude Voshaar MA, Ten Klooster PM, Glas CA, et al. Validity and measurement precision of the PROMIS physical function item bank and a content validity-driven 20-item short form in rheumatoid arthritis compared with traditional measures. Rheumatology. 2015;54:2221–2229. [DOI] [PubMed] [Google Scholar]
- 14. Brodke DS, Goz V, Voss MW, et al. PROMIS PF CAT outperforms the ODI and SF-36 physical function domain in spine patients. Spine. 2017;42:921–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hung M, Hon SD, Franklin JD, et al. Psychometric properties of the PROMIS physical function item bank in patients with spinal disorders. Spine. 2014;39:158–163. [DOI] [PubMed] [Google Scholar]
- 16. Makhni E, Meldau J, Blanchett J, et al. Correlation of PROMIS physical function, pain interference, and depression in pediatric and adolescent patients in the ambulatory sports medicine clinic. Orthop J Sports Med. 2019;7:2325967119851100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mulcahey M, Haley S, Slavin M, et al. Ability of PROMIS pediatric measures to detect change in children with cerebral palsy undergoing musculoskeletal surgery. J Pediatr Orthop. 2016;36:749–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kratz A, Slavin M, Mulcahey M, et al. An examination of the PROMIS pediatric instruments to assess mobility in children with cerebral palsy. Qual Life Res. 2013;22:2865–2876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Westberry DE, Wack LI, Davis RB, et al. Femoral anteversion assessment: Comparison of physical examination, gait analysis, and EOS biplanar radiography. Gait Posture. 2018;62:285–290. [DOI] [PubMed] [Google Scholar]
- 20. Shultz S, Nguyen A, Schmitz R. Differences in lower extremity anatomical and postural characteristics in males and females between maturation groups. J Orthop Sports Phys Ther. 2008;38:137–149. [DOI] [PubMed] [Google Scholar]
- 21. Sass P, Hassan G. Lower extremity abnormalities in children. Am Fam Physician. 2003;68:461–468. [PubMed] [Google Scholar]
- 22. Mackay J, Thomason P, Sangeux M, et al. The impact of symptomatic femoral neck anteversion and tibial torsion on gait, function and participation in children and adolescents. Gait Posture. 2021;86:144–149. [DOI] [PubMed] [Google Scholar]
- 23. Leblebci G, Akalan E, Apti A, et al. Increased femoral anteversion-related biomechanical abnormalities: lower extremity function, falling frequencies, and fatigue. Gait Posture. 2019;70:336–340. [DOI] [PubMed] [Google Scholar]
- 24. Alexander N, Studer K, Lengnick H, et al. The impact of increased femoral antetorsion on gait deviations in healthy adolescents. J Biomech. 2019;86:167–174. [DOI] [PubMed] [Google Scholar]
- 25. Misterska E, Kaminiarczyk-Pyzałka D, Adamczak K, et al. Mental health and adjustment to juvenile idiopathic arthritis: Level of agreement between parent and adolescent reports according to Strengths and Difficulties Questionnaire and Adolescent Outcomes Questionnaire. PLoS ONE. 2017;12:e0173768. [DOI] [PMC free article] [PubMed] [Google Scholar]


