Abstract
Pacemakers respond to the physical activity of patients by increasing the heart rate to compensate for the increased demand. They sense the physical activity of the patient with the help of different types of sensors that work with different mechanisms. In this case, we are presenting a 74-year-old male who was experiencing intermittent chest pain and palpitations. Following interrogation, he was found to have atrial paced tachycardias due to a tracking of the atrial tachycardia.
Keywords: pacemaker mediated tachycardia, inappropriate rate responsiveness, sensor defect, tachycardia, minute ventilation sensor defect, pacemaker driven tachycardia
Introduction
A pacemaker is a type of cardiac implantable electronic device that can generate electrical impulses. They can be temporary or permanent. The main indications for pacemaker placement are symptomatic bradycardia from the sinus node or AV node, second or third-degree heart block, long QT syndrome, recurrent syncope, etc. [1]. The pacemaker can be single chamber, dual chamber, and biventricular. Mode of pacemaker is specified by coding in which the first letter stands for the area being paced, the second letter for the area being sensed, the third letter states response of pacemaker, the fourth letter is for presence or absence of rate modulation, and the fifth letter specifies location or absence of multisite pacing [2].
Case presentation
A 74-year-old male presented with intermittent chest pain. Chest pain was dull, substernal, and non-radiating. The pain started while walking and was relieved with rest. It was associated with shortness of breath, palpitations, and dizziness without syncope. He denied orthopnea, paroxysmal nocturnal dyspnea, cough, and leg swelling. He had a history of atrial fibrillation status post cardioversion and ablation, coronary artery disease, diabetes mellitus, hypertension, carotid artery stenosis status post endarterectomy, and sick sinus syndrome status post pacemaker implantation.
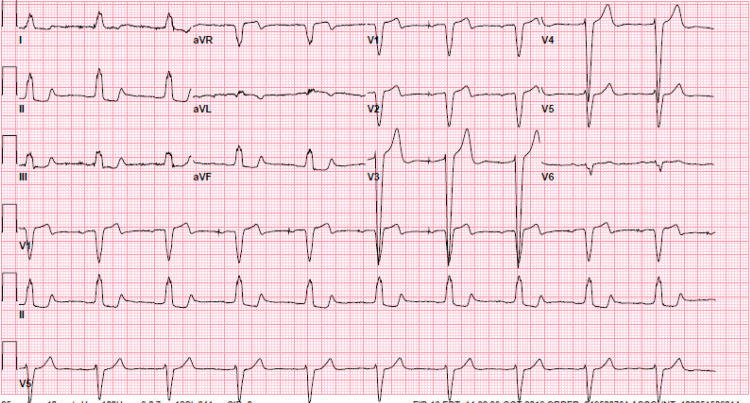
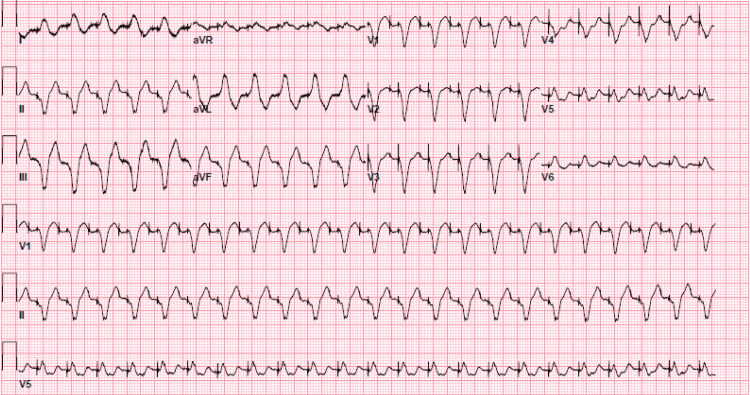
A physical exam revealed a heart rate of 74 beats per minute, a temperature of 37 degrees Celsius, a respiratory rate of 16 per minute, and oxygen saturation of 97% on room air. The cardiovascular exam was unremarkable. Initial EKG was pertinent for sinus rhythm with first-degree atrioventricular (AV) block and left bundle branch block as shown in Figure 1. He was admitted to the cardiac care unit. Telemetry showed multiple events with dual-paced tachycardia to 140 beats per minute. He began to have chest pain when tachycardic. EKG at that time showed dual-paced tachycardia with a rate of 139 as shown in Figure 2. The initial laboratory workup was unremarkable as shown in Table 1.
Table 1. Initial laboratory work-up.
| Test | Results | Reference Range |
| White Blood Count (WBC) | 6.5 | 4.5-11.00 k/uL |
| Hemoglobin | 13 | 13.6-16.3 g/dL |
| Platelet | 244 | 150-450 k/uL |
| Sodium | 139 | 135-145 meq/L |
| Potassium | 4.2 | 3.5-5.2 mmol/L |
| Chloride | 111 | 96-108 mmol/L |
| Phosphorus | 3.6 | 2.4-4.7 mg/dL |
| Magnesium | 2.1 | 1.5-2.5 mg/dL |
| Creatinine | 0.68 | 0.5-1.1 mg/dL |
| Blood Urea Nitrogen | 16 | 6-23 mg/dL |
| Brain Natriuretic Peptide (BNP) | 156 | 0.0-100 pg/mL |
| Troponin | <0.010 | <0.031 mg/dL |
| Aspartate aminotransferase | 26 | 1-35 U/L |
| Alanine aminotransferase | 28 | 1-45 U/L |
| Alkaline phosphatase | 56 | 38-126 U/L |
Figure 1. Initial EKG showing sinus rhythm with first degree AV block and left bundle branch block.
Figure 2. Electrocardiogram (EKG) showing atrial-paced tachycardia with rate of 139 beats/minute.
Device interrogation was done and it showed atrial-paced tachycardia and multiple short paroxysms of atrial-paced tachycardia due to tracking of atrial tachycardia. There was no evidence of atrial fibrillation on device interrogation. The device was reprogrammed from DDDR (dual, dual, dual, rate-responsive) mode to DDI (dual, dual, Inhibition) mode. Rate adaptiveness was turned off. The minute ventilation sensor was deactivated and the device was reprogrammed for a motion-based accelerometer only. Beta-blocker dose was increased as tolerated. On telemetry after changing the settings, he didn’t get any episodes of atrial tachycardia. Coronary angiography was done given the nature of the chest pain which was found to have non-obstructive mild two-vessel coronary artery disease. Chest X-ray showed the intact placement of pacemaker leads without any fracture of the leads shown in Figure 3. On outpatient follow-up, the patient didn't have these episodes and remained in sinus rhythm for four months. Atrial fibrillation came back after that which was treated with a second ablation following which he remained in sinus rhythm.
Figure 3. Chest X-ray showing dual-chamber pacemaker with intact leads.
Discussion
Pacemakers have two types of sensors to adjust the heart rate according to the physical activity of the patient. The first one is the activity sensor which is a piezoelectric accelerometer that responds to the acceleration/motion and produces the electric charge in proportion to acceleration. The change in voltage is used to estimate the physical activity based on the algorithms. The second type of sensor is the minute ventilation sensor. These sensors can measure the impedance of the thoracic cavity. During the respiratory cycle, impedance changes due to the change in air content of the thoracic cavity. This change in impedance helps these sensors to estimate the respiratory rate and minute ventilation further and pacemaker changes the rate of heart pacing based on activity sensing by these sensors [3].
Current literature states that dual-sensing has a more physiological response to physical activity and patients have a better quality of living rather than each one of the single sensors [4-5]. Some patients with an accelerometer as the only sensor of physical activity complain of fatigue during the exercise as heart rate does not increase as needed. There is an ongoing study for comparing the accelerometer and minute ventilation sensors.
Pacemaker-mediated tachycardia (PMT) could be due to multiple mechanisms like tracking of sinus tachycardia or atrial arrhythmias, tracking of electromagnetic devices, and endless loop tachycardia due to a reentrant circuit, etc. Endless loop tachycardia is the most common mechanism of pacemaker-mediated tachycardia. The usual symptoms of PMT are chest pain, palpitations, syncope, or rarely heart failure symptoms. Temporary treatment can be done by placing the magnet on the pacemaker pocket but definitive management requires reprogramming of the device [6-7].
Sensor-mediated tachycardia can be due to false sensing by minute ventilation sensors resulting in a false estimation of minute ventilation due to a few reasons. The concurrent use of other monitoring devices like cardiac monitoring equipment, electrocardiograph equipment, external defibrillators, and respiratory monitoring equipment can lead to incorrect interpretation as elevated minute ventilation by minute ventilation sensor and lead to pacemaker-induced tachycardia [8-9]. Electrocautery can also lead to false estimation of minute ventilation by the sensors and lead to tachycardia [10-11]. Sensor-mediated tachycardia can also be due to tracking the atrial tachycardia or arrhythmias [6-7].
Patients admitted to an inpatient unit for cardiac monitoring should have the rate-responsive mode turned off. In our case, patient symptoms improved after turning off the minute ventilation sensor. His intermittent chest pain, palpitations, and dizziness were most likely due to atrial-paced tachycardia.
Conclusions
Pacemaker-mediated tachycardia due to tracking of atrial rate by a sensor is an uncommon mechanism. Atrial ectopy is common after ablation in patients with atrial fibrillation. In this case, tachycardia resolved after reprogramming the device and increasing the dose of beta blocker to suppress the atrial ectopy. Although atrial tachycardia while on telemetry could be due to interference, tracking atrial ectopy would explain the symptoms of this patient in the field. Chest pain of the patient is likely related to increased demand during tachycardia.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Puette JA, Malek R, Ellison MB. StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. Pacemaker. [PubMed] [Google Scholar]
- 2.The revised NASPE/BPEG generic code for antibradycardia, adaptive-rate, and multisite pacing. Bernstein AD, Daubert JC, Fletcher RD, et al. Pacing Clin Electrophysiol. 2002;25:260–264. doi: 10.1046/j.1460-9592.2002.00260.x. [DOI] [PubMed] [Google Scholar]
- 3.Device sensing: sensors and algorithms for pacemakers and implantable cardioverter defibrillators. Kaszala K, Ellenbogen KA. Circulation. 2010;122:1328–1340. doi: 10.1161/CIRCULATIONAHA.109.919704. [DOI] [PubMed] [Google Scholar]
- 4.Assessment of adaptive rate response provided by accelerometer, minute ventilation and dual sensor compared with normal sinus rhythm during exercise: a self-controlled study in chronotropically competent subjects. Cao Y, Zhang Y, Su Y, Bai J, Wang W, Ge J. Chin Med J (Engl) 2015;128:25–31. doi: 10.4103/0366-6999.147798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Influence of DDD rate response pacing with integrated double sensors on physical efficiency and quality of life. Pilat E, Mlynarski R, Wlodyka A, Kargul W. Europace. 2008;10:1189–1194. doi: 10.1093/europace/eun212. [DOI] [PubMed] [Google Scholar]
- 6.Pacemaker-mediated arrhythmias. Alasti M, Machado C, Rangasamy K, et al. J Arrhythm. 2018;34:485–492. doi: 10.1002/joa3.12098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abu-haniyeh A, Hajouli S. StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. Pacemaker mediated tachycardia. [PubMed] [Google Scholar]
- 8.Pacemaker-driven tachycardia induced by electrocardiograph monitoring in the recovery room. Hu R, Cowie DA. Anaesth Intensive Care. 2006;34:266–268. doi: 10.1177/0310057X0603400221. [DOI] [PubMed] [Google Scholar]
- 9.Monitoring equipment induced tachycardia in patients with minute ventilation rate-responsive pacemakers. Southorn PA, Kamath GS, Vasdev GM, Hayes DL. Br J Anaesth. 2000;84:508–509. doi: 10.1093/oxfordjournals.bja.a013480. [DOI] [PubMed] [Google Scholar]
- 10.Electrocautery-induced pacemaker tachycardia: why does this error continue? Rozner MA, Nishman RJ. Anesthesiology. 2002;96:773–774. doi: 10.1097/00000542-200203000-00045. [DOI] [PubMed] [Google Scholar]
- 11.Upper rate pacing after radiofrequency catheter ablation in a minute ventilation rate adaptive DDD pacemaker. van Gelder BM, Bracke FA, el Gamal MI. Pacing Clin Electrophysiol. 1994;17:1437–1440. doi: 10.1111/j.1540-8159.1994.tb02464.x. [DOI] [PubMed] [Google Scholar]