Abstract
Background:
Despite the relatively high incidence of phalangeal fractures, there is an imperfect understanding of the epidemiology and anatomical distribution of these fractures. This study describes the patient characteristics, anatomic distribution, and detailed fracture patterns of phalangeal fractures among a large adult cohort in the United States.
Methods:
A retrospective study was performed among patients with phalangeal fractures in the United States between January 2010 and January 2015. Included patients were 18 years old or older and had a diagnosis of a phalangeal fracture. A total of 2140 phalangeal fractures in 1747 patients were included, and a manual chart review was performed to collect epidemiological and radiographic information. Fractures were classified based on location and fracture pattern.
Results:
The median age at the time of injury was 45 years (interquartile range, 30–57), and 65% of patients were men. The small finger had the highest incidence of fractures (26%) followed by the ring finger (24%). Distal and proximal phalanges demonstrated the highest incidence of fractures at 39% each. The dominant hand was affected in 44% of cases. Eighteen percent of fractures were due to a work-related trauma mechanism, and the most common mechanism of injury was blunt trauma (46%).
Conclusion:
This study provides a detailed overview of the anatomic distribution and fracture patterns of phalangeal fractures in an adult US population and, thus, may aid hand surgeons treating these injuries.
Takeaways
Question: What are the anatomic distribution and epidemiology of phalangeal fractures in an American cohort?
Findings: A retrospective chart and radiographic analysis of 2140 phalangeal fractures revealed that the median age of injury was 45 years. Overall, fractures occurred more commonly in men; however, women sustained a more significant proportion at older ages. Small finger fractures had the highest incidence among the digits. The distal and proximal phalangeal fractures had the same incidence. Work-related trauma accounted for 18% of injuries.
Meaning: Understanding the epidemiology of phalangeal fractures may aid hand surgeons in treating these injuries.
INTRODUCTION
When considering both health care–related and lost productivity costs, fractures of the hand have a high economic burden compared with other orthopedic injuries, such as injuries to the skull, hip, knee, or lower limbs.1 Also, with an annual incidence of 68 per 100,000 persons, finger fractures are among the five most common presenting diagnoses of the upper extremity in American emergency departments, and account for 0.2%–3% of all patient visits to emergency departments.2,3 An optimal understanding of the epidemiological and anatomical distribution of phalangeal fractures is paramount to reducing associated health care costs and fracture risk.4
Previous studies on the anatomical distribution of hand fractures have been performed using populations from geographical regions, including China and Europe, with relatively small numbers of patients.5–9 Kremer et al8 found that phalangeal fractures were most common in the ring finger, while Weum et al7 reported that the small finger was most commonly affected. The distribution of fractures among men and women varied between studies, from Weum et al7 reporting 70% of patients to be men, up to the 90% reported by Van Oosterom et al.9 With regard to the fracture patterns within the individual phalanges, their distribution has been examined in German and Norwegian populations with sample sizes limited to 283 and 459 phalangeal fractures, respectively.5,7
However, due to these studies being relatively small and originating from a different geographic area with potentially different demographics, previous results may not be reflective of practice in the United States. Despite the relative ubiquity of phalangeal fractures treated at hospitals in the United States, there is an incomplete understanding of detailed epidemiology and the anatomical distribution of phalangeal fractures.
Therefore, the objective of this study is to provide an epidemiological overview of phalangeal fractures among US adults, with a specific focus on the anatomical distribution and fracture patterns.
MATERIALS AND METHODS
Patient Inclusion
Institutional review board approval was requested and granted under protocol number 2019P000635. This study included all patients aged 18 years or older who were diagnosed with a phalangeal fracture at one of two level I trauma centers in New England between January 1, 2010 and January 1, 2015. A total of 2507 fractures were identified in 2404 patients using Current Procedural Terminology codes that are used to indicate surgical or conservative care for digital fractures (SDC 1). (See appendix, Supplemental Digital Content 1, which displays CPT codes for surgical and conservative care of phalangeal fractures, http://links.lww.com/PRSGO/C122.) All selected patients were confirmed to also have International Classification of Diseases codes that were appropriate for phalangeal fractures. The exclusion criteria consisted of nontraumatic fracture or amputation proximal to the distal interphalangeal joint (211), no X-ray available (73), patients younger than 18 years old (39), nonphalangeal fracture (38), old fractures that refractured in the same location (5), and pregnancy (1). Three hundred sixty-seven fractures were excluded, leaving a total of 2140 phalangeal fractures and 1747 patients who met the inclusion criteria. Some smaller portions of this dataset have been analyzed in other published studies looking at specific injuries from our group. These previous studies were not epidemiologic studies and had a different research question than the current study.10–13
Explanatory and Outcome Variables
A manual chart review was performed for all patients to collect demographic and radiographic information to characterize the fracture patterns and epidemiology. These data included age, sex, hand dominance, participation in manual labor, smoking, diabetes (diagnosis of type 1 or type 2 diabetes at the time of presentation), insurance type [private, Medicare (national health insurance program based on age or health conditions), Medicaid (federal and state health insurance programs for those with limited income or resources), self-pay, other], race (Asian, Black, Hispanic, other, and White), fracture of the right or left hand, affected digit (thumb, index, middle, ring, and small), affected phalanx (proximal, middle, and distal), intraarticular or extraarticular fracture, fracture location (base, shaft, neck, head, tuft, and complex multilevel fracture), and fracture type [transverse, oblique, spiral, vertical, dorsal base, volar base, radial or ulnar base, unicondylar, bicondylar, tuft, and unclassifiable (Fig. 1; Table 1)]. Fracture locations were classified as “complex multilevel” if they extended throughout the phalanx, and the fracture patterns were classified as “unclassifiable” if no recognizable fracture pattern was present. For the base type fractures (dorsal, volar, radial, or ulnar base) in the proximal parts of the phalanges, please consider that these include fractures with various trauma mechanisms (eg, avulsion fractures, pilon fractures, and shear fractures).
Fig. 1.
A graphical representation of the fracture-type classification system. Reproduced and adapted with permission from Sarwark JF, ed. Essentials of Musculoskeletal Care, 4th ed. Rosemont, Ill.: American Academy of Orthopaedic Surgeons; 2010, p. 398.
Table 1.
Classification of Fracture Type
| Distal Phalanx |
|---|
| Tuft fracture |
| Transverse fracture |
| Oblique fracture |
| Vertical fracture |
| Base fracture only |
| Volar base, dorsal base, or radial/ulnar base fracturea |
| Proximal or middle phalanx |
| Head fracture only |
| Unicondylar or bicondylar fracture |
| Transverse fracture |
| Oblique fracture |
| Spiral fracture |
| Vertical fracture |
| Base fracture only |
| Volar base, dorsal base, or radial/ulnar base fracturea |
| Proximal, middle, or distal phalanx |
| Complex multilevel fracture → unclassifiable fracture throughout entire phalanx |
*These may include fractures with various trauma mechanisms, for example, avulsion fractures, pilon fractures, and shear fractures
The presence of dislocation (defined as dislocation of the fractured phalanx), whether the fracture was open or closed, the injury mechanism (crush, sharp, explosion, blunt trauma, and other), injury date, whether the fracture was the result of a work-related injury, and most recent date of follow-up were also collected. Fractures were classified based on the findings and interpretations of the radiologist. If the radiology report lacked the data required for classification, the radiographs were reviewed independently by an author of the study for classification.
Statistical Analysis
Normality of data was determined using the Shapiro–Wilk test. Categorical data were stated as frequencies and percentages, while continuous data were described as medians and interquartile ranges (IQRs). A univariate analysis was performed to report the demographic and fracture data.
RESULTS
Patient Characteristics
A total of 1747 patients and 2140 traumatic phalangeal fractures were identified and analyzed. The median age at the time of injury was 44.7 years (IQR, 30.3–57.4), and 65% of patients were men. The most common race was White (76%) followed by Hispanic (10%), Black (6%), other (5%), and Asian (3%). Twenty-two percent of patients were employed in manual labor, 17% of patients smoked at the time of injury, and 6% of patients had diabetes. The most common insurance was private (61%) followed by Medicare (17%), Medicaid (16%), and self-pay [6% (Table 2)].
Table 2.
Patient Characteristics
| Total (n = 1747) | |
|---|---|
| Age in years, median (IQR) | 44.7 (30.3‐57.4) |
| Male patients, n (%) | 1129 (64.6) |
| Smoking, n (%) | 292 (16.7) |
| Diabetes, n (%) | 104 (5.95) |
| Manual labor, n (%) | 377 (21.6) |
| Race, n (%) | |
| White | 1325 (75.8) |
| Hispanic | 171 (9.79) |
| Black | 112 (6.41) |
| Other | 88 (5.04) |
| Asian | 51 (2.92) |
| Insurance type, n (%) | |
| Private | 913 (61.2) |
| Medicare | 251 (16.8) |
| Medicaid | 231 (15.5) |
| Self-pay | 91 (6.10) |
| Other | 7 (0.47) |
Missing values per variable: smoking 43, diabetes 9, manual labor 221, insurance type 254.
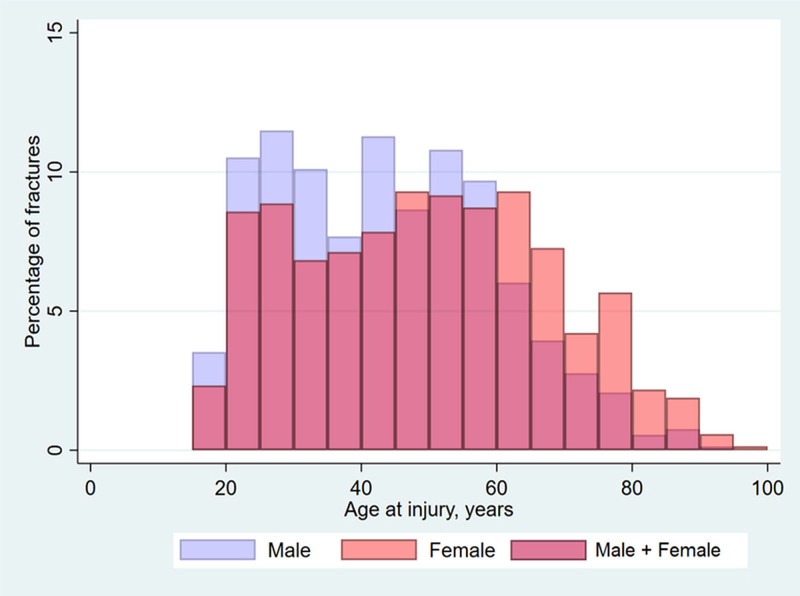
Although the majority of fractures occurred in men, the distribution of phalangeal fractures was different between sexes in different age groups, with men sustaining a greater proportion of fractures at a younger age and women sustaining a greater proportion at an older age (Fig. 2).
Fig. 2.
As demonstrated in the figure, the peak incidence of phalangeal fractures occurs at a younger age in male patients when compared with women.
Fracture Locations and Types
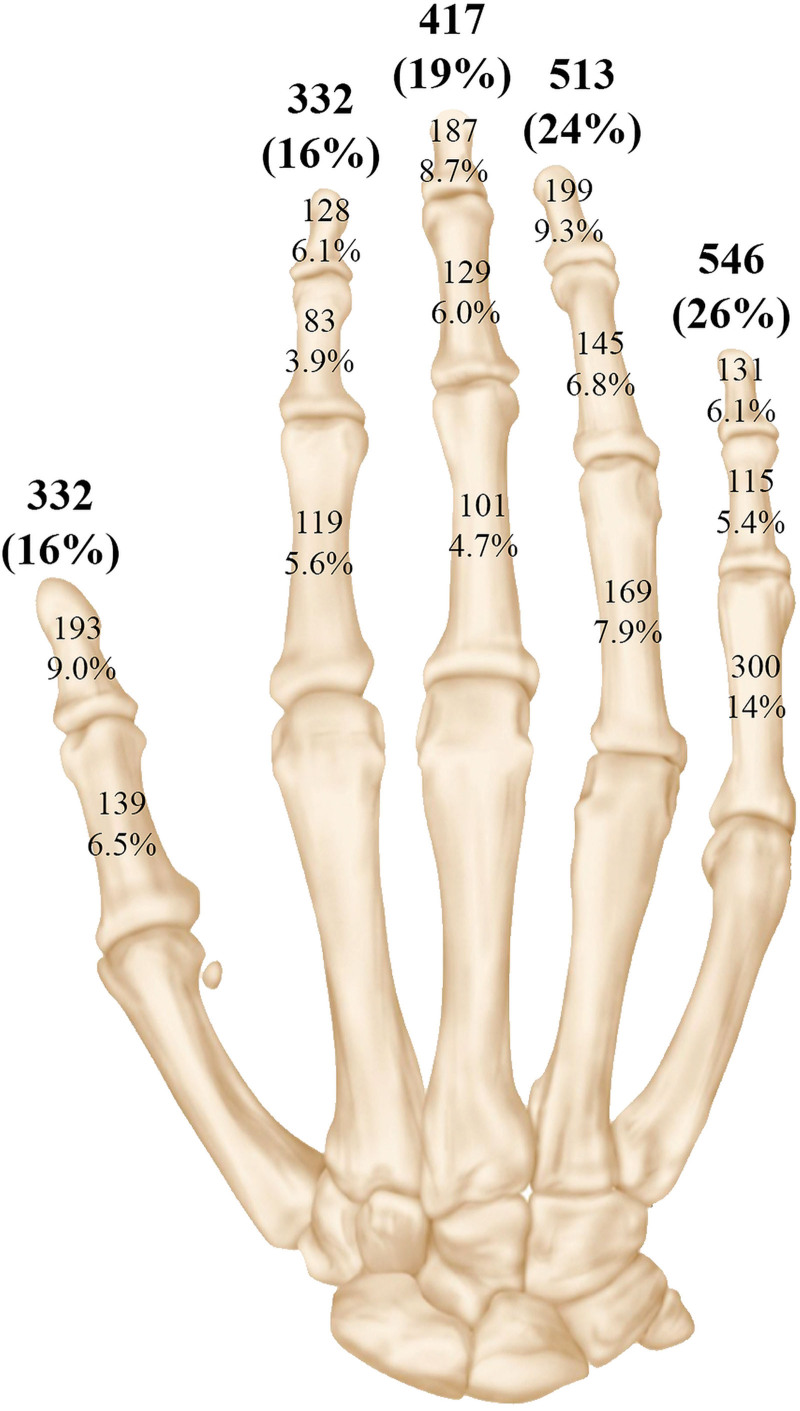
The overall incidence of phalangeal fractures varied between digits, with the small finger having the highest incidence of fractures (26%) followed by the ring finger (24%), middle finger (19%), and thumb and index finger (both 16%). The proximal and distal phalanges had the highest incidence of fractures (each 39%), followed by middle phalanges [22% (Fig. 3)].
Fig. 3.
The overall number and percentage of fractures per digit is thumb (322, 16%), index (322, 16%), middle (417, 19%), ring (513, 24%), and small (546, 26%). Reproduced and adapted with permission from Sarwark JF, ed. Essentials of Musculoskeletal Care, 4th ed. Rosemont, Ill.: American Academy of Orthopaedic Surgeons; 2010, p. 398.
The phalangeal shaft was the most common fracture location comprising 36% of the phalangeal fractures followed by the base (32%), tuft (19%), head (6%), neck (4%), and complex multilevel fractures (4%). Among the head fractures, unicondylar fractures were about three times as common as bicondylar fractures. Oblique, transverse, and tuft fractures (all 19% each after rounding) were the most common fracture types. Additionally, base fractures occurred with notable frequency, with volar and dorsal base fractures being twice as common as radial or ulnar base fractures (Table 3).
Table 3.
Types and Locations of Fractures
| Fracture Location | Fracture Type | Total, n (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Transverse | Oblique | Spiral | Vertical | Dorsal Base | Volar Base | Radial/Ulnar Base | Unicondylar | Bicondylar | Tuft | Unclassifiable | ||
| Base, n | 0 | 0 | 0 | 0 | 282 | 271 | 125 | 0 | 0 | 0 | 0 | 678 (31.7) |
| Shaft, n | 352 | 362 | 29 | 23 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 768 (35.9) |
| Neck, n | 52 | 35 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 92 (4.30) |
| Head, n | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 91 | 27 | 0 | 1 | 119 (5.56) |
| Tuft, n | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 396 | 0 | 396 (18.5) |
| Complex multilevel fracture, n | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 87 | 87 (4.07) |
| Total, n (%) | 404 (18.9) | 397 (18.6) | 31 (1.45) | 25 (1.17) | 282 (13.2) | 271 (12.7) | 125 (5.84) | 91 (4.25) | 27 (1.26) | 396 (18.5) | 91 (4.25) | 2140 (100) |
The fracture locations were stratified by phalanx (Table 4). As mentioned, fractures of the small finger were most common with a predisposition for the proximal phalanx (14%), compared with 5.4% in the middle and 6.1% in the distal phalanx, respectively. For all digits except the thumb, shaft fractures were common in the proximal phalanges with a decreasing incidence more distally. About one in 25 (4.07%) fractures were classified as complex multilevel fractures due to extensive comminution throughout the phalanx, without a clear predilection for any of the phalanges.
Table 4.
Location of Fractures within Phalanxes
| Fracture Location | Digit | Digit | Digit | Digit | Digit | Total, n (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I (Thumb) | II (Index) | III (Middle) | IV (Ring) | V (Small) | |||||||||||
| Phalanx | Phalanx | Phalanx | Phalanx | ||||||||||||
| Proximal | Distal | Proximal | Middle | Distal | Proximal | Middle | Distal | Proximal | Middle | Distal | Proximal | Middle | Distal | ||
| Base, n | 75 | 71 | 27 | 19 | 21 | 29 | 45 | 49 | 38 | 54 | 55 | 69 | 72 | 54 | 678 (31.7) |
| Shaft, n | 36 | 58 | 59 | 46 | 21 | 53 | 53 | 37 | 90 | 54 | 37 | 183 | 27 | 14 | 768 (35.9) |
| Neck, n | 5 | 0 | 14 | 5 | 0 | 4 | 17 | 0 | 12 | 14 | 0 | 17 | 4 | 0 | 92 (4.30) |
| Head, n | 20 | 0 | 15 | 6 | 0 | 6 | 10 | 0 | 16 | 16 | 0 | 24 | 6 | 0 | 119 (5.56) |
| Tuft, n | 0 | 53 | 0 | 0 | 81 | 0 | 0 | 95 | 0 | 0 | 104 | 0 | 1 | 62 | 396 (18.5) |
| Complex multilevel fracture, n | 3 | 11 | 4 | 7 | 7 | 9 | 4 | 6 | 13 | 7 | 3 | 7 | 5 | 1 | 87 (4.07) |
| Total, n (%) | 139 (6.50) | 193 (9.02) | 119 (5.56) | 83 (3.88) | 130 (6.07) | 101 (4.72) | 129 (6.03) | 187 (8.74) | 169 (7.90) | 145 (6.78) | 199 (9.30) | 300 (14.0) | 115 (5.37) | 131 (6.12) | 2140 (100) |
Fracture Characteristics
Fifty-seven percent of fractures occurred in the left hand, while 43% of fractures were in the right hand. Overall, patients sustained fractures in their dominant hand in 44% of cases and 88% of cases were in right-hand dominant patients. Twelve percent of patients presented with fractures in multiple digits, and in less than 1% of cases, patients had bilateral phalangeal fractures. For 18% of the fractures, there was a work-related trauma mechanism (Table 5).
Table 5.
Characteristics of Phalangeal Fractures and Mechanisms of Injury
| Characteristic | Frequency | Percentage |
|---|---|---|
| Laterality | ||
| Right hand | 922 | 43.1 |
| Left hand | 1218 | 56.9 |
| Both hands affected* | 8 | 0.46 |
| Dominant hand affected† | 801 | 43.8 |
| Injury characteristics | ||
| Occupation-related injury‡ | 377 | 18.3 |
| Multiple digits affected* | 216 | 12.4 |
| Open fracture | 590 | 27.6 |
| Fracture-dislocation | 88 | 4.11 |
| Intraarticular fracture | 1010 | 47.2 |
| Mechanism of injury§ | ||
| Crush | 519 | 24.6 |
| Sharp | 466 | 22.1 |
| Explosion | 21 | 0.99 |
| Blunt trauma | 970 | 45.9 |
| Other | 136 | 6.44 |
*Per-patient analysis, N = 1747.
†N = 1830.
‡N = 2063.
§N = 2112.
Twenty-eight percent of fractures were classified as open fractures, 4% were fracture dislocations, and 48% were intraarticular. The most common mechanism of injury was blunt trauma (46%), while fractures caused by explosions were rare (<1%).
DISCUSSION
This large retrospective study of 2140 fractures provides a characterization of phalangeal fractures in an adult US population. The incidence of phalangeal fractures is not distributed equally across the hand: the small finger proximal phalanx is the most common fracture location, 56% of phalangeal fractures occur in the nondominant hand, and about one in five is work-related.
Also, our results demonstrate that men sustain phalangeal fractures at a higher frequency than women and that the peak incidence in men occurs at a younger age compared with women. Higher rates of osteoporosis in women at older ages and a reduction in risk-taking behavior in older men may explain these differences.14,15 While the presence of osteoporosis was not assessed for this study, studies have found fractures to be more common in older women and have identified osteoporosis as an independent risk factor.16,17 And although the mechanisms of injury were not classified beyond being work-related or not, we found that men did suffer sharp injuries more frequently than women (30.3% versus 4.72%, P < 0.001). Also, the proportion of open fractures (36.2% versus 9.55%, P < 0.001) and comminuted fractures (48.5% versus 28.9%, P < 0.001) differed between men and women, respectively. An improved understanding of sex-related differences in fracture characteristics may improve clinical outcomes and influence surgical management.
The small finger sustained the most phalangeal fractures, which may be explained by its fragility as the smallest digit and its vulnerability at the hand’s outer and most ulnar aspect. This is consistent with findings in a pediatric population and one prior publication in an adult population.7,18 However, a general consensus on the digit most susceptible to fracture is lacking in adult populations. Brown19 found the middle finger to be the most common and suggested that the frequency of fractures is proportional to the length of the digit. In contrast, Kremer et al8 and Van Oosterom et al9 found that the index and ring fingers had the highest fracture rates, respectively. The reasons for the discrepancies across literature on adult populations remain unclear, although they may be due to different sample sizes in other studies.
The proximal and distal phalanges had similar fracture rates at 39% of total fractures each. The literature fails to reach a consensus on which phalanx is most susceptible to fracture in adult populations, although our findings are most consistent with those of Weum et al.7–9 The high frequency of blunt trauma injuries in the current population may explain the high fracture rate in the proximal phalanx, considering that a relationship between blunt trauma injuries and proximal phalanx injuries has been established in pediatric literature.18,20,21 Thus, these findings highlight the need to carefully examine the proximal phalanx for fractures in the setting of blunt trauma injuries, and future efforts may be directed at designing safety equipment that more specifically protects the proximal phalanges from blunt trauma.
Shaft and tuft fractures were the most common locations in the proximal and distal phalanges, respectively. A trend that was reported before in a pediatric population may explain this pattern. Cebula et al18 noted that younger patients (0‐8 years old) often sustain distal phalangeal fractures due to crush mechanisms (eg, finger jammed in door), and older patients (9‐16 years of age) sustain proximal phalangeal fractures secondary to sports and fights, highlighting how the mechanism of injury can change the fracture profile. In this adult population, blunt trauma (eg, falls and sports) and crush are the most common mechanisms of injury. The high rate of blunt trauma and crush injuries likely explains the shaft and tuft fracture pattern.
Forty-three percent of phalangeal fractures occurred in the right hand, while 57% were in the left. This is consistent with the findings of Weum et al7 (46% right, 54% left) but inconsistent with Kremer et al8 (53% right and 47% left). There is a small body of literature that suggests left-handedness is a risk factor for upper extremity fractures.22–24 The higher incidence of fractures in the nondominant hand may be due to performing different tasks when compared with the dominant hand (eg, holding a nail instead of wielding a hammer and catching baseballs instead of throwing) that increase the exposure of the nondominant hand to various trauma mechanisms.
Open fractures occurred in 28% of fractures in this study population, which is higher than previously reported in the literature.7 This finding may have two explanations. First, this study population represents hand fractures presenting to two level I trauma centers. The severity of the hand fractures that present to these hospitals is likely greater than those presenting to a tertiary health care facility. Second, the rate of open fractures may be inflated secondary to the method of categorization used. When a single fracture out of multiple fractures in the same phalanx was an open fracture, each of these individual fractures was counted as open. Since the radiographs and clinical notes were limited in their identification of open fractures within a multifracture phalanx, we were obligated to count all fractures within a multifracture phalanx as open.
The results of this retrospective cohort analysis should be interpreted in light of its limitations. While this study assesses a large cohort of patients who were treated at two high-volume centers, these were both urban level I trauma centers; therefore, the results may not be generalizable to hospitals across the United States. A second limitation is that the fracture-type categorization is subjective. Not all studies that we referred to used the same classification system for fracture types, which may impact the capacity to compare findings across publications. A third limitation of this analysis is that the patient cohort studied herein is not representative of the local or national diversity of race we observe in the United States.
Supplementary Material
Footnotes
Published online 4 August 2022.
Disclosure: This study was supported in part by the Jesse B. Jupiter/Wyss Medical Foundation Endowment. Dr. Eberlin is a consultant for AxoGen, Integra, and Checkpoint. Dr. Chen is a consultant for Biedermann Motech. The other authors have no financial interest to declare.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
This study was approved by the Institutional Review Board under protocol number 2019P000635.
REFERENCES
- 1.de Putter CE, Selles RW, Polinder S, et al. Economic impact of hand and wrist injuries: health-care costs and productivity costs in a population-based study. J Bone Joint Surg Am. 2012;94:e56. [DOI] [PubMed] [Google Scholar]
- 2.Ootes D, Lambers KT, Ring DC. The epidemiology of upper extremity injuries presenting to the emergency department in the United States. Hand (N Y). 2012;7:18–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Jonge JJ, Kingma J, Van Der Lei B, et al. Phalangeal fractures of the hand. An analysis of gender and age-related incidence and aetiology. J Hand Surg Am. 1994;19:168–170.. [DOI] [PubMed] [Google Scholar]
- 4.Williams SA, Chastek B, Sundquist K, et al. Economic burden of osteoporotic fractures in US managed care enrollees. Am J Manag Care. 2020;26:e142–e149. [DOI] [PubMed] [Google Scholar]
- 5.Hove LM. Fractures of the hand. Distribution and relative incidence. Scand J Plast Reconstr Surg Hand Surg. 1993;27:317–319. [PubMed] [Google Scholar]
- 6.Ip WY, Ng KH, Chow SP. A prospective study of 924 digital fractures of the hand. Injury. 1996;27:279–285. [DOI] [PubMed] [Google Scholar]
- 7.Weum S, Millerjord S, de Weerd L. The distribution of hand fractures at the university hospital of North Norway. J Plast Surg Hand Surg. 2016;50:146–150. [DOI] [PubMed] [Google Scholar]
- 8.Kremer L, Frank J, Lustenberger T, et al. Epidemiology and treatment of phalangeal fractures: conservative treatment is the predominant therapeutic concept. Eur J Trauma Emerg Surg. 2022;48:567–571.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Oosterom FJT, Brete GJV, Ozdemir C, et al. Treatment of phalangeal fractures in severely injured hands. J Hand Surg Am. 2001;26 B:108–111.. [DOI] [PubMed] [Google Scholar]
- 10.Oflazoglu K, Wilkens SC, Rakhorst H, et al. Postoperative dorsal proximal interphalangeal joint subluxation in volar base middle phalanx fractures. J Hand Microsurg. 2020;12:32–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oflazoglu K, Moradi A, Braun Y, et al. Mallet fractures of the thumb compared with mallet fractures of the fingers. Hand (N Y). 2017;12:277–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oflazoglu K, Wilkens SC, Rakhorst H, et al. Reoperation after operative fixation of proximal interphalangeal joint fractures. Hand (N Y). 2021;16:338–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oflazoglu K, de Planque CA, Guitton TG, et al. Dorsal subluxation of the proximal interphalangeal joint after volar base fracture of the middle phalanx. Hand (N Y). 2022;17:60–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lane NE. Epidemiology, etiology, and diagnosis of osteoporosis. Am J Obstet Gynecol. 2006;194(2 suppl):S3–S11. [DOI] [PubMed] [Google Scholar]
- 15.Gardner M, Steinberg L. Peer influence on risk taking, risk preference, and risky decision making in adolescence and adulthood: an experimental study. Dev Psychol. 2005;41:625–635. [DOI] [PubMed] [Google Scholar]
- 16.Woolf AD, Akesson K. Preventing fractures in elderly people. BMJ. 2003;327:89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iskrant AP. The classic: the etiology of fractured hips in females. 1968. Clin Orthop Relat Res. 2010;468:1731–1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cebula M, Modlińska S, Machnikowska-Sokołowska M, et al. Hand injuries in the polish Silesian paediatric population—an exploratory cross-sectional study of post-traumatic x-rays. Medicina (Kaunas). 2020;56:1–11.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown PW. A review of digital injuries. Br J Plast Surg. 1967;20:387–391.. [DOI] [PubMed] [Google Scholar]
- 20.Liu EH, Alqahtani S, Alsaaran RN, et al. A prospective study of pediatric hand fractures and review of the literature. Pediatr Emerg Care. 2014;30:299–304. [DOI] [PubMed] [Google Scholar]
- 21.Chew EM, Chong AK. Hand fractures in children: epidemiology and misdiagnosis in a tertiary referral hospital. J Hand Surg Am. 2012;37:1684–1688. [DOI] [PubMed] [Google Scholar]
- 22.Luetters CM, Kelsey JL, Keegan TH, et al. Left-handedness as a risk factor for fractures. Osteoporos Int. 2003;14:918–922. [DOI] [PubMed] [Google Scholar]
- 23.Hemenway D, Azrael DR, Rimm EB, et al. Risk factors for wrist fracture: effect of age, cigarettes, alcohol, body height, relative weight, and handedness on the risk for distal forearm fractures in men. Am J Epidemiol. 1994;140:361–367. [DOI] [PubMed] [Google Scholar]
- 24.Stellman SD, Wynder EL, DeRose DJ, et al. The epidemiology of left-handedness in a hospital population. Ann Epidemiol. 1997;7:167–171. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.