Abstract
As effector innate immune cells and as a host to the protozoan parasite Leishmania, macrophages play a dual role in antileishmanial immunoregulation. The 2 key players in this immunoregulation are the macrophage-expressed microRNAs (miRNAs) and the macrophage-secreted cytokines. miRNAs, as small noncoding RNAs, play vital roles in macrophage functions including cytokines and chemokines production. In the reverse direction, Leishmania-regulated cytokines alter miRNAs expression to regulate the antileishmanial functions of macrophages. The miRNA patterns vary with the time and stage of infection. The cytokine-regulated macrophage miRNAs not only help parasite elimination or persistence but also regulate cytokine production from macrophages. Based on these observations, we propose a novel immunoregulatory framework as a scientific rationale for antileishmanial therapy.
1. Introduction
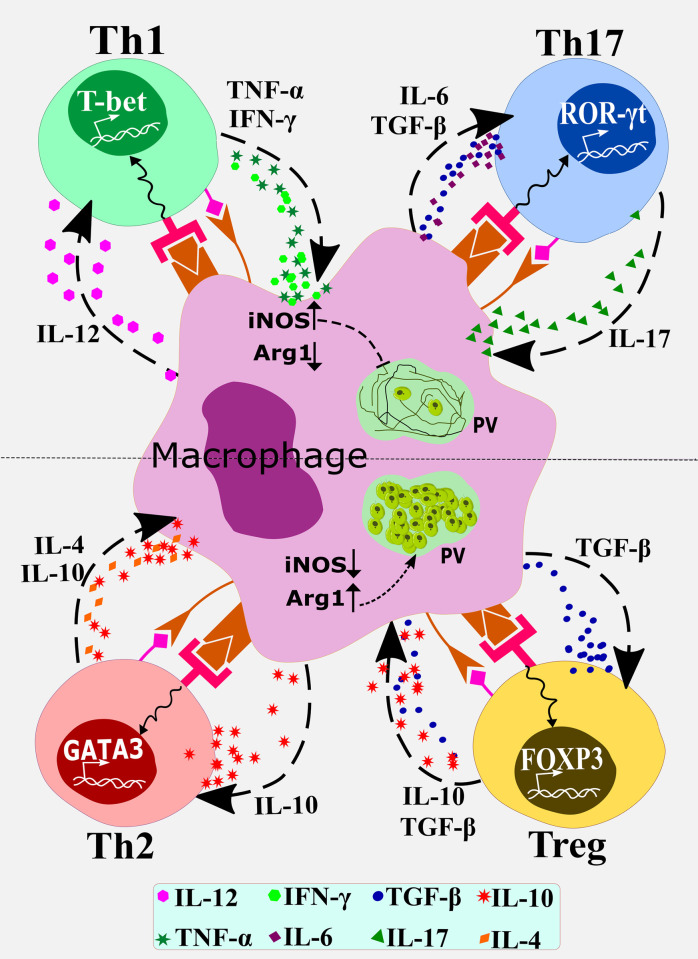
Tissue macrophages are differentiated from the bone marrow–derived monocytes that are recruited to the tissues [1]. During chronic infections, progenitor cells are mobilized from bone marrow, recruited at the site of infection, and the macrophages can be differentiated in situ. Macrophages play dual roles in many infectious diseases: playing host to an intracellular pathogen such as Leishmania or acting as an executioner eliminating the pathogen by eliciting antileishmanial immune effectors such as cytokines [1,2]. Thus, macrophages can be polarized to host-protective (M1 macrophages) or proparasitic phenotype (M2 macrophages) [3]. Macrophages are the major producers of IL-1β, IL-6, IL-12, IL-10, and IL-23 [4]. IL-12 contributes to Th1 cell polarization, while IL-1β, IL-6, and IL-23 trigger and maintain Th17 cell polarization [5]. Although Th1 and Th17 cell subsets play complementary roles in protecting against Leishmania donovani and Leishmania infantum infections, there are ambiguities regarding the role of Th17 cells in L. major infection [6,7]. IFN-γ and TNF-α from Th1 cells activate macrophages to induce NO and ROS eliminating Leishmania, while IL-4, IL-10, and TGF-β from Th2 and Treg cells inhibit the leishmanicidal functions of macrophages [6,7]. Macrophage-derived IL-10 and TGF-β exert preventive effects on the M1 macrophages and Th1 cells while promoting Th2/Treg cell differentiation [8,9]. A basic macrophage—T-cell network is shown in Fig 1.
Fig 1. A basic macrophage-T cell subset differentiation scheme that counteractively regulates the alternative outcomes of Leishmania infection.
Macrophages are the host cells for the protozoan parasite Leishmania (PV with amastigotes are shown in green). The top half (above the broken line) shows the condition when Th1 and Th17 cells are differentiated in presence of the respective signature transcription factors T-bet and ROR-γt. These cells activate macrophages to induce iNOS but to reduce arginase (Arg1). iNOS catalyzes the formation of nitric oxide that kills the amastigotes within macrophages. The bottom half shows the differentiation of Th2 ad Treg cells in presence of the respective signature transcription factors GATA-3 and FOXP3. IL-4 and IL-10 secreted by these cells deactivate macrophages to reduce iNOS, but increase Arg1, expression resulting in parasite growth in macrophages. miRs target these macrophage–T cell interactions to manipulate the outcomes of Leishmania infection. iNOS, inducible nitric oxide synthase; PV, parasitophorous vacuole.
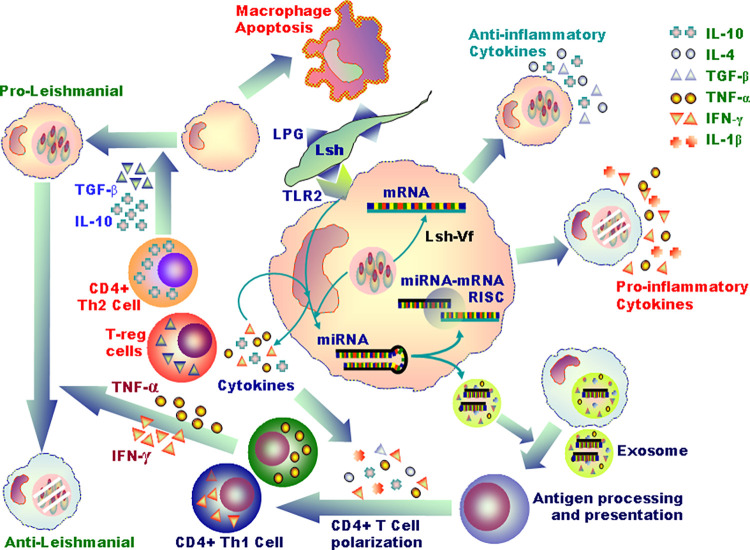
In this intriguing battle between the host and the parasite, Leishmania the parasite enters the host macrophages and subverts its defense mechanisms—phagosomal maturation, MHC class-I and -II-mediated antigen presentation, inflammatory cytokine productions, activation of leishmanicidal mechanisms such as generation of reactive oxygen species (ROS), and nitric oxide (NO)—and multiply within phagolysosomes [10–12]. On the other hand, macrophages marshal an intense but diverse immune attack on the parasite to eliminate it. As these 2 counter-forces face off, microRNAs (miRNAs) regulate the outcome of the duel (Fig 2).
Fig 2. Leishmania-expressed ligands such as LPG interact with corresponding receptors (e.g., TLR2 for LPG) on macrophages and signal altered miRNA expression (at the centre of the figure).
As shown clockwise surrounding the central macrophage, these miRNAs affect macrophage production of proinflammatory and anti-inflammatory cytokines, antigen processing and presentation of macrophages, CD4+ T cell polarization into opposing effector subsets, antileishmanial or proleishmanial effects, and macrophage apoptosis or survival. Proleishmanial to antileishmanial functions are induced by the Th1 cell secreted IFN-γ and TNF-α. A balance between these counteractive functions regulated by miRNAs, which can be altered by Leishmania, determines the outcome of the infection. The Leishmania-infected macrophages secrete exosomes filled with different antigens and miRs. The exosomes can be taken up by the neighboring uninfected macrophages, wherein these miRs can execute their functions. The key to the cytokines are shown on the upper right corner of the figure. LPG, lipophosphoglycan; miRNA, microRNA.
miRNAs are 20 to 22 nucleotides long noncoding RNAs regulating gene expression by target mRNA degradation or translational repression [13,14] and potentiate or inhibit macrophage activities against infectious agents [13]. We propose that Leishmania-regulated aberrant miRNA expression in macrophages affects the production of leishmanicidal cytokines, whereas macrophage-deactivating cytokines regulate miRNAs to support the parasite. Finally, we invoke an immunoregulatory framework as a scientific rationale for designing an antileishmanial therapy.
2. The biogenesis of microRNAs
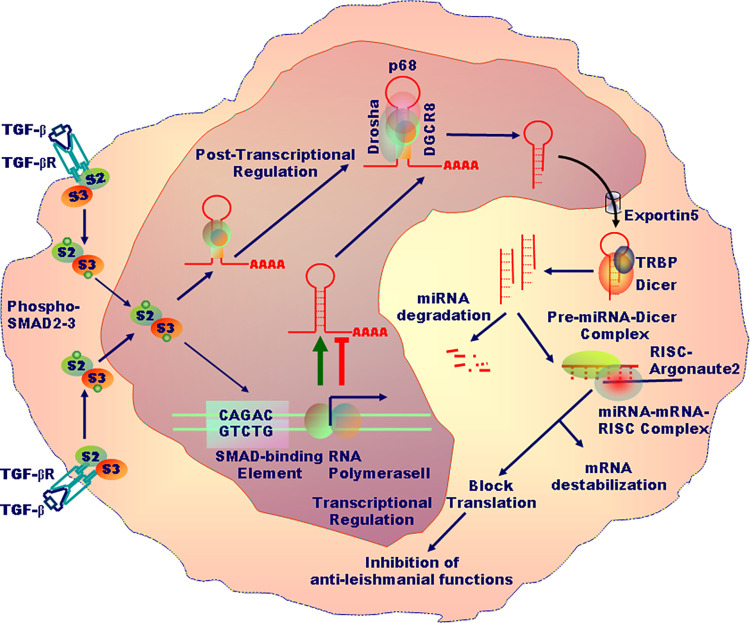
Within the nucleus, RNA polymerase II transcribes the DNA to primary miRNA (pri-miRNA; >1 kb) with a local stem-loop structure, wherein the mature miRNA is embedded [15,16]. The pri-miRNA is then cropped by the RNAse III Drosha and its key cofactor, DGCR8 (DiGeorge Syndrome Critical Region 8) to create a small hairpin-shaped miRNA precursor (pre-miRNA; approximately 65 nucleotides). Once exported to the cytoplasm, pre-miRNA is further pruned by an RNAse III Dicer to generate the miRNA duplex, which is next loaded onto Ago2, an Argonaut protein, to form the effector complex called RISC (RNA-induced silencing complex) [16]. Within the RISC, Ago2 guides the binding of the nucleotides 2 to 8 of the 5′ end of miRNAs to a complementary region of 6 to 7 nucleotides placed in the 3′-untranslated region (UTR) of target mRNAs [15,16] (Fig 3).
Fig 3. TGF-β induced by Leishmania infection binds to TGF-β receptor causing its phosphorylation and subsequent SMAD2/SMAD3-dependent transcriptional and posttranscriptional regulation of miRNA expression in macrophages.
These miRNAs make complexes with the target mRNAs—one miRNA binding to many mRNAs—to destabilize or suppress mRNAs translation. Depending on the miRNAs up-regulated or down-regulated, proleishmanial or antileishmanial effects are observed. miRNA, microRNA.
3. Leishmania regulates microRNAs expression in macrophages
L. major, L. donovani, L. amazonensis, or L. infantum infect macrophages—of both mice and humans—altering the expression of numerous miRNAs [17–21] that inhibit the leishmanicidal functions of macrophages [22]. These miRNAs target various biological processes such as macrophage polarization, NO production, apoptosis and autophagy, cytokine and chemokine production, phagosome maturation, drug response, and T-cell polarization [23,24] (Fig 1).
The L. major and L. donovani-infected human macrophages and dendritic cells (DCs) exhibit different patterns of miRNA expression [21]. Parasite strain, isolate, load, and virulence factors may affect the expression of macrophage miRNAs. For example, in the L. infantum-infected dogs PBMCs, miR-194 and miR-371 expression show a positive association, but miR-150 expression shows a negative relationship, with the parasite load [25]. Among the same species of Leishmania, different strains can exhibit differential effects on miRNA expression [21]. A more infective L. infantum strain causes higher miR-155 expression in macrophages than a less infective strain [20]. L. donovani isolates from visceral leishmaniasis (VL) and post-kala-azar dermal leishmaniasis (PKDL) patients differentially influenced the expression of miRNAs in the THP-1-derived macrophages. Differentially expressed miRNAs influence various biological processes such as PI3K signaling, cell cycle regulation, immunomodulation, apoptosis inhibition, and cytokine production [26].
In humans, most miRNAs were overexpressed in L. donovani-infected, but not as much in L. major-infected, macrophages and DCs [21]. Although up-regulation of many miRNAs in L. donovani-infected macrophages was reported, miRNA down-regulation was attributed to the enhanced stability of c-Myc, a transcription factor that binds to the miRNA-related promoters and influences deacetylation to repress miRNA biosynthesis but promote parasite survival; c-Myc blockade reduced amastigote survival [27,28]. Wild-type and arginase-deficient L. amazonensis differentially influence miRNA expression in mouse macrophages suggesting a role for Leishmania-expressed arginase in modulating the macrophage miRNA expression [19].
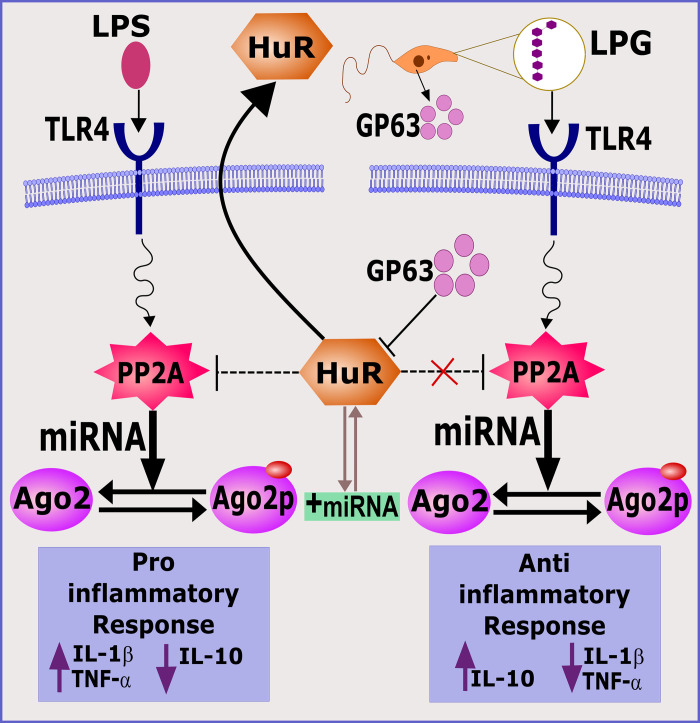
Antimony-resistant (R-LD) and antimony-sensitive L. donovani (S-LD) selectively influence miRNAs in macrophages leading to discernible cytokine responses. R-LD and S-LD up-regulate protein phosphatase 2A (PP2A) but down-regulate Hu-antigen R (HuR) at different magnitudes. PP2A increases miRNA activity while HuR antagonizes it, leading to anti-inflammatory or proinflammatory cytokine responses, respectively [17]. Ago2 phosphorylation impairs its ability to bind target mRNAs but Leishmania-induced PP2A-mediated dephosphorylation reactivates it [17]. The binding of dephosphorylated Ago2 with miRNAs suppresses the expression of miRNA-associated proinflammatory cytokines in infected macrophages [17,29]. As HuR inhibits PP2A expression, HuR overexpression induces a significant proinflammatory macrophage response reducing L. donovani infection [29] (Fig 4).
Fig 4. HuR and Phosphatases reciprocally regulate proinflammatory and anti-inflammatory cytokines.
While Protein Phosphatase 2A (PP2A) increases miRNA activity, HuR overexpression down-regulates PP2A activation, and thereby miRNA expression, leading to increased proinflammatory cytokines. Leishmania-derived protease Gp-63 degrades HuR making active PP2A available for enhancing anti-inflammatory cytokines. On the other hand, Leishmania-derived LPG may activate TLRs to regulate PP2A activation that through regulation of argonaute proteins modulates cytokine response. LPG, lipophosphoglycan; miRNA, microRNA.
Leishmania amazonensis-expressed phosphatidylserine (PS) on the outer side of the cytoplasmic membrane is recognized by macrophage-expressed molecules and may cause silent invasion of macrophages without activation and increase parasite proliferation by IL-10 and TGF-β induction [30,31]. In an L. donovani infection model, macrophages dynamically regulate more than 900 miRs, of which miR-6540 may target PS and influence the parasite’s fate within macrophages [22]. However, the exact mechanism of PS-miRNA-6540 interaction awaits elucidation. Once inside, the parasite proliferates causing a hypoxic condition that induces hypoxia-inducible factor-1α (HIF-1α) expression potentiating macrophage-mediated immunity against L. amazonensis and L. major while attenuating the responses against L. donovani [8,32]. miR-3620 and miR-6385 are highly elevated in L. donovani infected macrophages, which probably down-regulate hypoxia-induced genes [22]. miR-3620 up-regulation controls iron homeostasis-related genes to ensure maximum iron availability to the parasite [22]. In L. donovani-infected macrophages, miR-210 is up-regulated in a HIF-1α-dependent manner and targets NF-κB p50 and TNF-α receptor mRNAs, limiting the production of proinflammatory cytokines while enhancing IL-10, aiding parasite survival. HIF-1α and miR-210 silencing promotes TNF-α and IL-12, but reduces IL-10, expression in these macrophages [33].
4. Macrophage-related microRNAs influence the macrophages polarization
Proinflammatory macrophages or M1 cells express proinflammatory genes such as IL-1β, IL-12, IFN-γ, and TNF-α in NF-κB-, STAT1-, interferon regulatory factor 1 (IRF-1)-, activator protein 1 (AP-1)-dependent manner [34,35]. M1 macrophages up-regulate NOS2 but down-regulate Arginase 1 (ARG1), limiting the parasite infection [36] while the reverse is observed in M2 macrophages [18]. Th2 cytokines such as IL-4, IL-10, IL-13, TGF-β, and M-CSF promote M2 polarization with the transcription factors STAT6, CCAAT/enhancer-binding protein beta (c/EBPβ), and surface molecules chitinase 3 like-3 (YM-1) and resistin-like molecule alpha (FIZZ1) as markers [34,35].
While miR-26a, miR-26b, miR-125a, miR-125b, miR-155, miR-181, and miR-720 contribute to the induction of M1 macrophages but suppressing M2 phenotype [13,37], whereas miR-146a, miR-146b, miR-125a, let-7c, and miR-181a contribute to the induction of M2 macrophages but suppression of M1 phenotype [13,37]. The miR-125a and miR-125b can up-regulate the M1 macrophage markers, while repressing M2 macrophage polarization by targeting interferon regulatory factor 4 (IRF4) [38]. However, Banerjee and colleagues indicated that Kruppel-like factor 13 (KLF13), a transcriptional factor that play a key role in M1 macrophage activation, is targeted by miR-125a-5p, which suppresses M1 macrophage activity, while increasing M2 macrophage response [39]. It is thus possible that miR-125 may both suppress and activate macrophages depending on the existing state of cellular activation and availability of a co-factor. Such a duality has also been reported for miR155, as discussed elsewhere in this review. miR-720 inhibits M2 polarization by reducing GATA3 expression, an M2-related transcription factor [40]. The importance of these M1- and M2-inducing miRNAs in leishmaniasis remains less understood. In L. donovani-infected BALB/c monocyte-derived macrophages (MDMs) and in spleen/liver, up-regulation of M2 macrophage-related miRNAs (miR146a-5p, miR-181a-5p, and miR-125a-5p) and down-regulation of an M1 macrophage-related miRNA (miR26a-5p) were observed [36]. miR-146a-5p down-regulates iNOS, but promotes Arg1, expression during L. donovani infection. miR-146a-5p inhibition reduced the expression of M2 markers and parasite burden but enhanced the expression of M1 markers (iNOS and IL-12) in the spleen and liver of these L. donovani-infected mice. The silencing of the bromodomain-containing protein 4 (BRD4), an epigenetic and transcriptional regulator, abrogated miR-146a-induced M2 polarization suggesting that BRD4-dependent super-enhancer regulated miR-146a expression in L. donovani infection [36]. By contrast, miR-146a is up-regulated in L. major-infected human macrophages and aids in killing of the parasite by targeting the SMAD4 in the TGF-β signaling cascade [41]. Although these discrepancies remain unsolved till date, it is plausible that the L. donovani and L. major express different LPGs and thereby interacts with different heterodimers of TLR2 to trigger opposite outcomes of the infection. Similar paradox exists in miR-155 functions as well. On the one hand, miR-155 promotes M1 polarization while preventing M2 polarization and facilitates Leishmania elimination [3,37,42]; on the other hand, miR-155 promotes Leishmania persistence via inhibition of macrophage apoptosis [43]. Thus, a balanced miR-155 expression within macrophages needs to maintain M1 macrophage polarization without repressing apoptosis.
5. Macrophage-related microRNAs influence the NOS production
In macrophages, the up-regulation of NOS2 and NO production during the initial steps of infection exerts robust leishmanicidal activity [7,44]. Th1-related cytokines including IL-2, IFN-γ, and TNF-α induced NO production that reduced the infectivity, whereas Th2- and Treg-related cytokines such as IL-4, IL-10, and TGF-β suppress NOS2 expression promoting infectivity [7,44]. In L. amazonensis-infected macrophages, down-regulation of miR-30e-5p, miR-181c-5p, and miR-302d-3p leads to the up-regulation of NOS2 expression, which could reduce infectivity [18]. The expression of miR-294-3p and miR-721 is increased in L. amazonensis-infected macrophages up to 48 hours following infection, targeting NOS2 mRNA; reduced NOS2 expression and NO production support the L. amazonensis infectivity. miR-294 and miR-721 inhibition increased NOS2 expression and NO production, while reducing L. amazonensis infectivity. Thus, miR-294 and miR-721 can be considered a possible targets for development of drugs against L. amazonensis [19]. The expression of miR-294-3p and miR-721 are reduced in arginase-deficient L. amazonensis-infected macrophages compared with wild-type L. amazonensis-infected macrophages [19]. Thus, NOS2 was up-regulated in the arginase-deficient L. amazonensis-infected macrophages, promoting NO production while reducing infectivity in infected macrophages. let-7e overexpression reduces NOS2 expression, whereas let-7e inhibition enhances the NOS2 expression and NO generation in L. amazonensis-infected macrophages [45].
6. Macrophage-related microRNAs influence the cytokine and chemokine production
Infection with R-LD leads to aggressive infection accompanied by higher production of IL-10 and TGF-β compared with S-LD infection. R-LD infection results in the NF-κB activation via ligation with TLR2/TLR6, leading to up-regulation of miR-466i in the initial hours of infection, whereas inducing high amounts of IL-10 in late hours [17]. Indeed, miR-466i may competitively interact with the IL-10 3′ UTR AU-rich sequences, which act as a binding site for an RNA-binding protein, tristetraprolin, mediating quick IL-10 mRNA degradation. Thus, miR-446i may compete out tristetrapolin from IL-103′ AU-rich sequence and prevent IL-10 mRNA degradation resulting in increased IL-10 expression in macrophages [46]. IL-10 up-regulates multidrug-resistant protein-1 (MDR-1) transporter, which effluxes antimonials from R-LD-infected cells. R-LD induces IL-10/MDR1 to expel antimonial drugs and confer a survival benefit to R-LD parasites [17]. As TLRs perform a key role in the cytokine and chemokine production by Leishmania-infected macrophages [47], miRNAs can directly influence cytokine and chemokine generation by targeting their genes or indirectly via the TLR-mediated signaling pathways. As most TLRs recruit general adaptor protein MyD88 to activate NF-κB, infection of MyD88-deficient macrophages, as compared to wild-type macrophages, with R-LD leads to a remarkable greater amastigote numbers accompanied by elevated IL-10/IL-12 ratio.
Unlike S-LD, R-LD infection up-regulates miR-466i that targets MyD88 mRNA, leading to its down-regulation. In S-LD-infected macrophages, HuR overexpression suppresses the pathogen-induced anti-inflammatory immune response, thereby suppressing the infection process [17]. R-LD-induced PP2A triggers anti-inflammatory responses that help parasite persistence. Thus, S-LD infection heightens HuR/PP2A ratio, causing proinflammatory macrophage responses, limiting parasite expansion [17].
The expression of CCR2, CCL5, and CXCL10 mRNAs was remarkably inhibited upon L. major infection of human macrophages [48]. Expression of let-7a, miR-25, miR-26a, miR-140, miR-146a, and miR-155, miR-23b, and miR-132 is inversely related with the CCL2, CCL5, CXCL10, CXCL11, and CXCL12 expression during the first day of infection with L. major in human macrophages [49].
In L. amazonensis-infected BALB/c macrophages, suppression of miR-30e-5p, miR-181c-5p, miR-294-3p, and miR-302d-3p decreased the parasite load. Inhibition of miR-294-3p enhanced the expression of TNF-α and MCP-1/CCL2 mRNA; inhibition of miR-30e and miR-302d promoted the RANTES/CCL5 expression and reduced the parasite infectivity [18]. miR-181c-5p inhibition reduced MCP-1 expression. RANTES/CCL5 are associated with neutrophil, monocyte, and lymphocyte recruitment to the inflammatory sites. miR-294-3p and miR-302d-3p inhibition increased TNF-α and MCP-1 expression in L. amazonensis-infected macrophages [18].
SOCS4, a suppressor of JAK-STAT-related signaling, was predicted as a target of let7a, a miRNA that is overexpressed in L. donovani-infected DCs and macrophages but is suppressed in L. major-infected cells [21]. As let-7 family miRNAs target the proinflammatory genes, their reduced expression leads to greater expression of proinflammatory cytokines in the L. major-infected cells compared to L. donovani-infected cells [21,50]. let-7e expression requires TLR2, TLR4, and MyD88-mediated signaling in L. amazonensis-infected macrophages from C57BL/6 mice. Let-7e controls the expression of proinflammatory cytokines and chemokines—IL-1, IL-6, TNF-α and MCP-1- and NOS2 in Leishmania-infected macrophages by targeting TLR, adaptors, and transcription factors [45].
7. Macrophage-related microRNAs influence CD4+ T-cell polarization
IL-10-induced immunosuppression plays a prominent role in PKDL development [8]. The L. donovani isolates from VL patients induce more IL-10 in macrophages than the L. donovani isolates from PKDL patients perhaps due to differential expression of miRNAs [26]. The miR-93-5p inhibition in the L. donovani-infected human macrophages promotes IL-12 production while reducing IL-10 expression [26]. miR-146, miR-155, miR-221, and miR-324 overexpression down-regulates the IFN-γR signaling in PKDL patients [26]. Bioinformatics analyses predicted that miR-29a and miR-29b would target transcription factor T-bet suppressing protective Th1 response in VL. miR-135 and miR-126 can suppress Th2 response by targeting GATA3 [24]. miR-21 and miR-590-5b can target IL-12, while miR-98 and let-7a target IL-10 suppressing Th1 and Th2-related responses, respectively [24].
miR-340 expression was down-regulated, while IL-10 and TGF-β1 were up-regulated in L. major-infected macrophages. Accordingly, a miR-340 mimic down-regulated both TGF-β1 and IL-10 and the combination of miR-340 and miR-27a exerted more impacts on target genes [51]. Overexpression of miR-340 and miR-27a reduced macrophage infectivity suggesting their plausible therapeutic utility in cutaneous leishmaniasis [51]. Alteration of miR-3473f and miR-8113 in L. donovani-infected macrophages can affect Th1/Th2 cell polarization mainly via influencing IL-12 [22]. Up-regulation of miR-6973a prevents IL-12 production and shift protective Th1 type response to Th2 type, promoting parasite survival [22]. miR-155 performs a dual role in leishmaniasis by promoting parasite persistence through prevention of apoptosis of infected macrophages (37) and VL resolution by targeting SHIP-1 and SOCS1 to enhance IFN-γ secretion from CD4+ Th1 responses [52]. In L. donovani-infected miR155-deficient mice, SHIP-1 and SOCS1 expression in liver and spleen was increased but initially accompanied by IFN-γ production but reduced IL-4 and IL-10 production at a later time point [52].
8. Macrophage-related microRNAs influence the macrophages apoptosis
Apoptosis of the Leishmania-infected macrophage is delayed promoting survival and immune escape of the parasite [53–55]. Therefore, targeting the apoptosis-regulating miRNAs in Leishmania-infected macrophages may have potential to control the infection. Indeed, miR-15a expression decreases while miR-155 increases in mouse macrophages after L. major infection [43]. miR-155 prevents macrophage apoptosis by targeting caspase 3, caspase 10, and APAF1 [56–59]. miR-15a targets antiapoptotic genes such as Bcl2 [60]. miR-15a mimics and miR-155 inhibitor increased apoptosis of L. major-infected macrophages. In L. major-infected Balb/c mice, application of miR-155 inhibitor plus a miR-15a mimic reduced parasite load and decreased the lesion sizes within 6 weeks of infection. L. infantum infection in macrophages results in the miR-155 up-regulation—greater the infectivity, higher the expression of miR-155 [20]. In fact, the L. guyanensis-expressed Leishmania RNA virus 1 (LRV1) increases macrophage miR-155 expression in a TLR3-dependent manner to prolong the survival of macrophage and the parasite [61]. miR-155 inhibits apoptosis by targeting Fas-associated death domain-containing protein (FADD), caspase 3, and caspase 7 [59]. miR-24-3p expression was also up-regulated in L. major-infected macrophages quickly after the infection [62]. Bioinformatics analyses indicated that miR-24-3p exerts antiapoptotic impacts by repressing the apoptotic genes such as caspases 3 and 7. miR-24-3p inhibitors may thus have the therapeutic potential against L. major infection [62].
miR-3473f, miR-763, and miR-8113 were associated with negative regulation of apoptotic process in L. donovani-infected macrophages [22]. let-7a was up-regulated in the L. donovani-infected DCs and macrophages [21]. As let-7a inhibition in macrophages increased apoptosis and necrosis, let-7a inhibition may be a potential strategy to treat leishmaniasis [63]. In the L. donovani-infected macrophages, miR-155, miR-335, miR-143, miR-221, miR-93, and let7c were associated with negative regulation of apoptosis [26]. Inhibition of antiapoptosis miRNAs can be proposed as a new strategy for treating leishmaniasis [43].
9. Macrophage-related microRNAs influence the macrophages autophagy
Macrophage autophagy can eliminate intracellular microorganisms, which use strategies to prevent autophagy. While miR-3473f has been implicated in the prevention of autophagy [22,31], miR-30a-3p is up-regulated early after L. donovani infection preventing macrophage autophagy but promoting parasite survival [64]. miR-30a-3p targets BECN1—an essential autophagy-promoting protein—reducing the L. donovani survival within the macrophages [64]. Likewise, miR-101c, miR-129-5p, and miR-210-5p can influence autophagy via targeting the autophagy-related 4 (ATG4), specificity protein 1 (SP1) (a CTSE expression regulator), and BNIP3, respectively. Transfection of L. major-infected MDM with miR-101c and miR-129-5p mimics, or with a miR-210-5p inhibitor decreases infection load [65]. L. major-infected macrophages’ autophagy was correlated with miR-101c and miR-129-5p overexpression and the low miR-210 expression [65]. Autophagy targeting in Leishmania-infected macrophages can be considered as a plausible antileishmanial therapy.
10. Macrophage-related microRNAs influence the phagosome maturation and drug resistance
Following internalization, the pathogen-containing phagosome undergoes sequential maturation including the early-, intermediate-, and late phagosome formation. The late phagosome is fused with lysosomes to form phagolysosomes, resulting in degradation of phagosomal contents. The maturation processes are regulated by several factors, the incredibly sequential shift from the early endosomal Rab5 to the late endosomal Rab7 [66]. Following internalization, L. donovani secretes gp63 that inactivates c-Jun to down-regulate the miR-494 expression, thereby leads to the Rab5a overexpression in the infected cells [67]. Subsequently, L. donovani recruits and preserves Rab5a on its parasitophorous vacuoles to persist in the early endosomes and suppresses their merging with lysosomes. miR-494 negatively regulates Rab5a expression limiting parasite survival [67]. miRNAs play an important role in drug resistance in infectious and noninfectious diseases [68,69]. Leishmania can induce ABC transporters overexpression in macrophages by down-regulating miR-763, miR-1264, and miR-3473f that help the drug efflux from the Leishmania-infected cells [22].
11. Regulation of miRNA expression by inflammatory cytokines and mediators
There is a reciprocal regulatory relationship between miRNAs and inflammatory mediators/cytokines. For example, miR-187 has been identified as an IL-10-associated miRNA playing a role in IL-10-related suppression of TNF-α, IL-6, and the IL-12p40 by primary human monocytes following TLR4 stimulation [70]. IL-10 attenuates inflammatory responses by suppressing the expression of miR-155 in LPS-stimulated macrophages. miR-155 promotes the expression of proinflammatory cytokines such as TNF-α and inhibits the expression of anti-inflammatory elements as SOCS1. IL-10 had no effect on miR-155 gene transcription or nuclear export of pre-miR-155, but it destabilized both pri-miR-155 and pre-miR-155 transcripts, as well as interfered with miR-155 maturation [71]. The inhibitory impact of IL-10 on miR-155 expression was mediated via STAT3 and SHIP1, as IL-10-mediated inhibition of miR-155 expression was hampered in SHIP1-deficient macrophages but a SHIP1 activator restored this inhibition [71] and a STAT3 inhibitor reduced IL-10-mediated inhibition of miR-155. IL-10-induced SHIP1 prevents AKT-related signaling and lowers miR-155 expression [71]. IL-10-mediated miR-155 down-regulation led to the overexpression of the miR-155 target, SHIP1 [72]. IL-10 had no influence on miR-21 or miR-146a expression but it induced miR-146b in LPS-treated human and mouse macrophages, as IL-10-deficient macrophages had less miR-146b expression [73]. Once expressed, miR-146b targets TLR4 mRNA as well as critical adaptor/signaling factors such as MyD88, IRAK1, and TRAF6 leading to anti-inflammatory effects [73]. As an IL-10-dependent miRNA, miR-146b thus exerts anti-inflammatory activity by targeting of TLR4-related signaling components in macrophages [73]. In LPS-stimulated mouse macrophages, IL-10 suppresses the expression of miR-147, while increasing the expression of miR-455. The inhibition of miR-147 by IL-10 implies that miR-147 may have a proinflammatory role in TLR-activated macrophages [74].
IL-4 and IL-13, the cytokines secreted from Th2 cells, up-regulate miR-142-5p and down-regulate miR-130a-3p that play a key role in M2 polarization of macrophages [75]. The miR-142-5p overexpression by IL-4 suppresses SOCS1, a negative regulator of STAT-6, and thereby prolongs the life of phospho-STAT-6. STAT6-induced SOCS1 expression thus provides a negative feedback loop. A robust M2 polarization needs the involvement of PPAR, which is down-regulated in M1 macrophages but up-regulated in M2 macrophages [75]. IL-4 promotes histone deacetylation at the promoter of miR-130a-3p to reduce its expression and eliminate the suppressive effect of miR-130a-3p on the PPAR expression [76]. LPS represses PPAR expression by up-regulating miR-27b in M1 macrophages [76]. Differently expressed miRNAs in polarized macrophages may thus play a role in the maintenance of their activation [76].
The activation of classical M1 macrophages requires priming with IFN-γ followed by TLR stimulation. The IFN-γ priming causes macrophages to produce more proinflammatory, but less anti-inflammatory, cytokines and to boost their microbicidal and tumoricidal activities. IFN-γ reduces miR-3473b expression. miR-3473b promotes Akt/glycogen synthase kinase 3 signaling and IL-10 generation by directly targeting phosphatase and tensin homolog (PTEN) to decrease macrophage activation and inflammatory response [77]. The IFN-γ/miR-3473b/PTEN axis suggests a positive feedback loop whereby IFN-γ targets miR-3473b and allows de-repression of PTEN that inhibits Akt signaling and IL-10 production to eventuate in the activation of IFN-γ-primed macrophages [77].
TGF-β, a Leishmania-induced cytokine that is involved in Treg cells differentiation, regulates miRNA expression. TGF-β augments the expression of miR-29b that promotes the expression of Cyclooxygenase-2—catalyzing arachidonic acid conversion to prostaglandins (PG), reduces the bactericidal activity of macrophages [78]. Prostaglandin E2 (PGE2)-mediated macrophage polarization is regulated by miR-21 [79], as PGE2 down-regulates miR-21 that influences the M2 macrophage-associated genes expression [80]. Type-I IFNs down-regulates miR-145 expression. miR-145 targets the IL-10 gene silencer histone deacetylase 11 (HDAC11) leading to higher IL-10 expression in macrophages [81]. As Type-I IFNs suppress miR-145, the type I IFN/miR-145/HDAC11 axis thus suppresses IL-10 production by relieving HDAC11 from the miR-145 targeting [81].
12. Limitations in the studies on miR-regulation of Leishmania infection and antileishmanial immune response
Herein, we have extensively reviewed the available reports on the roles of miRs at the interface of Leishmania-macrophage interaction. Although efforts are made to align these reports to develop a generalized framework of Leishmania-modulating miRs expression and miRs-regulating antileishmanial immune response, it is limited by the lack of mechanistic details, incomparability between the model systems used, contradictions between the reported effects, Leishmania species-dependent variations in the miRs and their effects, heterogeneity of macrophages and dynamicity in the regulation of miRs expression, and effects on Leishmania infection. Understanding the evolution of the regulation of miRs expression and activities will require extensive coordinated interdisciplinary investigations using 1 system of host macrophage and 1 Leishmania species at a time.
13. Conclusions
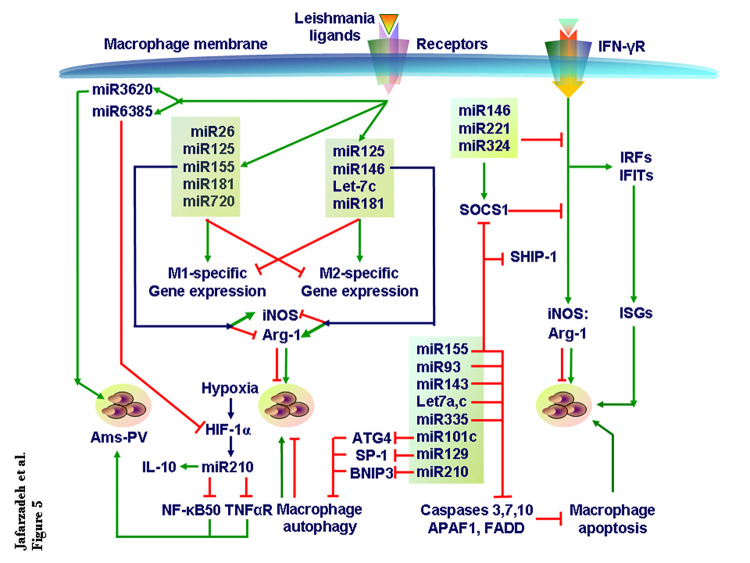
miRNAs play pivotal roles in the macrophage-mediated antileishmanial responses such as NOS2 and cytokine expression (Fig 5). In turn, the parasite and the cytokines regulate the expression of multiple miRNAs. Two different mechanisms operate simultaneously: An individual miRNA may target multiple genes and several miRNAs may target 1 particular gene. Following this bidirectional miRNA-based immunoregulatory framework may identify the cocktail of the miRNA mimics or miRNA inhibitors for an efficient antileishmanial therapy.
Fig 5. miRNA regulation of Leishmania infection.
TGF-β, and perhaps other cytokines too, regulate miRNA expression in macrophages. As Leishmania infection renders the intracellular environment hypoxic, the HIF-1α induces miR210 to enhance IL-10 production but reduce NF-κB activation and TNF-αR expression to enhance parasite load in the parasitophorous vacuoles in macrophages. Various miRNAs expressed during Leishmania infection modulate cellular processes including cytokine signaling that affects the outcome of Leishmania infection. Similarly, 2 counteractive sets of miRs reciprocally regulate M1 and M2 macrophage subsets differentiation that affects parasite growth. The other miRs regulate macrophage Autophagy and apoptosis and IFN-γR signaling to alter intracellular amastigote numbers. The available literature is too diverse in terms of Leishmania species, macrophage populations, experimental models, and assays to derive a coherent and integrative view of miRs role in Leishmania infection. Therefore, only a fraction of the literature is used to develop the current perspective. HIF-1α, hypoxia-inducible factor-1α; miRNA, microRNA.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Röszer T. Understanding the Biology of Self-Renewing Macrophages. Cells. 2018;7(8):103. doi: 10.3390/cells7080103 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jafarzadeh A, Chauhan P, Saha B, Jafarzadeh S, Nemati M. Contribution of monocytes and macrophages to the local tissue inflammation and cytokine storm in COVID-19: Lessons from SARS and MERS, and potential therapeutic interventions. Life Sci. 2020;257:118102. Epub 2020/07/21. doi: 10.1016/j.lfs.2020.118102 ; PubMed Central PMCID: PMC7367812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vellozo NS, Rigoni TS, Lopes MF. New Therapeutic Tools to Shape Monocyte Functional Phenotypes in Leishmaniasis. Front Immunol. 2021;12:704429. Epub 2021/07/13. doi: 10.3389/fimmu.2021.704429 ; PubMed Central PMCID: PMC8267810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roberts CA, Dickinson AK, Taams LS. The Interplay Between Monocytes/Macrophages and CD4(+) T Cell Subsets in Rheumatoid Arthritis. Front Immunol. 2015;6:571. Epub 2015/12/05. doi: 10.3389/fimmu.2015.00571 ; PubMed Central PMCID: PMC4652039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jafarzadeh A, Larussa T, Nemati M, Jalapour S. T cell subsets play an important role in the determination of the clinical outcome of Helicobacter pylori infection. Microb Pathog. 2018;116:227–36. Epub 2018/02/07. doi: 10.1016/j.micpath.2018.01.040 . [DOI] [PubMed] [Google Scholar]
- 6.Jafarzadeh A, Nemati M, Chauhan P, Patidar A, Sarkar A, Sharifi I, et al. Interleukin-27 Functional Duality Balances Leishmania Infectivity and Pathogenesis. Front Immunol. 2020;11:1573. Epub 2020/08/28. doi: 10.3389/fimmu.2020.01573 ; PubMed Central PMCID: PMC7427467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jafarzadeh A, Nemati M, Sharifi I, Nair A, Shukla D, Chauhan P, et al. Leishmania species-dependent functional duality of toll-like receptor 2. IUBMB Life. 2019;71(11):1685–700. Epub 2019/07/23. doi: 10.1002/iub.2129 . [DOI] [PubMed] [Google Scholar]
- 8.Jafarzadeh A, Nair A, Jafarzadeh S, Nemati M, Sharifi I, Saha B. Immunological role of keratinocytes in leishmaniasis. Parasite Immunol. 2021;43(9):e12870. Epub 2021/05/25. doi: 10.1111/pim.12870 . [DOI] [PubMed] [Google Scholar]
- 9.Yoshimura A, Wakabayashi Y, Mori T. Cellular and molecular basis for the regulation of inflammation by TGF-beta. J Biochem. 2010;147(6):781–92. Epub 04/20. doi: 10.1093/jb/mvq043 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arango Duque G, Descoteaux A. Leishmania survival in the macrophage: where the ends justify the means. Curr Opin Microbiol. 2015;26:32–40. Epub 2015/05/20. doi: 10.1016/j.mib.2015.04.007 . [DOI] [PubMed] [Google Scholar]
- 11.Podinovskaia M, Descoteaux A. Leishmania and the macrophage: a multifaceted interaction. Future Microbiol. 2015;10(1):111–29. Epub 2015/01/20. doi: 10.2217/fmb.14.103 . [DOI] [PubMed] [Google Scholar]
- 12.Matheoud D, Moradin N, Bellemare-Pelletier A, Shio MT, Hong WJ, Olivier M, et al. Leishmania evades host immunity by inhibiting antigen cross-presentation through direct cleavage of the SNARE VAMP8. Cell Host Microbe. 2013;14(1):15–25. Epub 2013/07/23. doi: 10.1016/j.chom.2013.06.003 . [DOI] [PubMed] [Google Scholar]
- 13.Curtale G, Rubino M, Locati M. MicroRNAs as Molecular Switches in Macrophage Activation. Front Immunol. 2019;10:799. Epub 2019/05/07. doi: 10.3389/fimmu.2019.00799 ; PubMed Central PMCID: PMC6478758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jafarzadeh A, Marzban H, Nemati M, Jafarzadeh S, Mahjoubin-Tehran M, Hamblin MR, et al. Dysregulated expression of miRNAs in immune thrombocytopenia. Epigenomics. 2021. Epub 2021/09/10. doi: 10.2217/epi-2021-0092 . [DOI] [PubMed] [Google Scholar]
- 15.Kundu M, Basu J. The Role of microRNAs and Long Non-Coding RNAs in the Regulation of the Immune Response to Mycobacterium tuberculosis Infection. Front Immunol. 2021;12:687962. doi: 10.3389/fimmu.2021.687962 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ha M, Kim VN. Regulation of microRNA biogenesis. Nat Rev Mol Cell Biol. 2014;15(8):509–24. Epub 2014/07/17. doi: 10.1038/nrm3838 . [DOI] [PubMed] [Google Scholar]
- 17.Mukherjee B, Mukherjee K, Nanda P, Mukhopadhayay R, Ravichandiran V, Bhattacharyya SN, et al. Probing the molecular mechanism of aggressive infection by antimony resistant Leishmania donovani. Cytokine. 2021;145:155245. Epub 2020/08/31. doi: 10.1016/j.cyto.2020.155245 . [DOI] [PubMed] [Google Scholar]
- 18.Fernandes JCR, Aoki JI, Maia Acuña S, Zampieri RA, Markus RP, Floeter-Winter LM, et al. Melatonin and Leishmania amazonensis Infection Altered miR-294, miR-30e, and miR-302d Impacting on Tnf, Mcp-1, and Nos2 Expression. Front Cell Infect Microbiol. 2019;9:60. Epub 2019/04/06. doi: 10.3389/fcimb.2019.00060 ; PubMed Central PMCID: PMC6435487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muxel SM, Laranjeira-Silva MF, Zampieri RA, Floeter-Winter LM. Leishmania (Leishmania) amazonensis induces macrophage miR-294 and miR-721 expression and modulates infection by targeting NOS2 and L-arginine metabolism. Sci Rep. 2017;7:44141. doi: 10.1038/srep44141 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Silva SC, Silva DF, Almeida TC, Perasoli FB, da Silva ATP, da Silva GN, et al. Behavior of two Leishmania infantum strains-evaluation of susceptibility to antimonials and expression of microRNAs in experimentally infected J774 macrophages and in BALB/c mice. Parasitol Res. 2018;117(9):2881–93. Epub 2018/06/27. doi: 10.1007/s00436-018-5979-3 . [DOI] [PubMed] [Google Scholar]
- 21.Geraci NS, Tan JC, McDowell MA. Characterization of microRNA expression profiles in Leishmania-infected human phagocytes. Parasite Immunol. 2015;37(1):43–51. Epub 2014/11/08. doi: 10.1111/pim.12156 ; PubMed Central PMCID: PMC4287219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tiwari N, Kumar V, Gedda MR, Singh AK, Singh VK, Singh SP, et al. Identification and Characterization of miRNAs in Response to Leishmania donovani Infection: Delineation of Their Roles in Macrophage Dysfunction. Front Microbiol. 2017;8(314). doi: 10.3389/fmicb.2017.00314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wei Y, Schober A. MicroRNA regulation of macrophages in human pathologies. Cell Mol Life Sci. 2016;73(18):3473–95. Epub 2016/05/04. doi: 10.1007/s00018-016-2254-6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pandey RK, Sundar S, Prajapati VK. Differential Expression of miRNA Regulates T Cell Differentiation and Plasticity During Visceral Leishmaniasis Infection. Front Microbiol. 2016;7:206. Epub 2016/03/05. doi: 10.3389/fmicb.2016.00206 ; PubMed Central PMCID: PMC4766295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bragato JP, Melo LM, Venturin GL, Rebech GT, Garcia LE, Lopes FL, et al. Relationship of peripheral blood mononuclear cells miRNA expression and parasitic load in canine visceral leishmaniasis. PLoS ONE. 2018;13(12):e0206876. Epub 2018/12/06. doi: 10.1371/journal.pone.0206876 ; PubMed Central PMCID: PMC6281177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kumar A, Vijaykumar S, Dikhit MR, Abhishek K, Mukherjee R, Sen A, et al. Differential Regulation of miRNA Profiles of Human Cells Experimentally Infected by Leishmania donovani Isolated From Indian Visceral Leishmaniasis and Post-Kala-Azar Dermal Leishmaniasis. Front Microbiol. 2020;11:1716. doi: 10.3389/fmicb.2020.01716 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nandan D, Rath CT, Reiner NE. Leishmania regulates host macrophage miRNAs expression by engaging transcription factor c-Myc. J Leukoc Biol. 2021;109(5):999–1007. Epub 2020/11/20. doi: 10.1002/JLB.4RU0920-614R . [DOI] [PubMed] [Google Scholar]
- 28.Colineau L, Lambertz U, Fornes O, Wasserman WW, Reiner NE. c-Myc is a novel Leishmania virulence factor by proxy that targets the host miRNA system and is essential for survival in human macrophages. J Biol Chem. 2018;293(33):12805–19. Epub 2018/06/24. doi: 10.1074/jbc.RA118.002462 ; PubMed Central PMCID: PMC6102154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goswami A, Mukherjee K, Mazumder A, Ganguly S, Mukherjee I, Chakrabarti S, et al. MicroRNA exporter HuR clears the internalized pathogens by promoting pro-inflammatory response in infected macrophages. EMBO Mol Med. 2020;12(3):e11011. Epub 2020/02/08. doi: 10.15252/emmm.201911011 ; PubMed Central PMCID: PMC7059013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Manzano JI, Perea A, León-Guerrero D, Campos-Salinas J, Piacenza L, Castanys S, et al. Leishmania LABCG1 and LABCG2 transporters are involved in virulence and oxidative stress: functional linkage with autophagy. Parasit Vectors. 2017;10(1):267. Epub 2017/06/01. doi: 10.1186/s13071-017-2198-1 ; PubMed Central PMCID: PMC5450059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wanderley JLM, Thorpe PE, Barcinski MA, Soong L. Phosphatidylserine exposure on the surface of Leishmania amazonensis amastigotes modulates in vivo infection and dendritic cell function. Parasite Immunol. 2013;35(3–4):109–19. Epub 2012/11/21. doi: 10.1111/pim.12019 ; PubMed Central PMCID: PMC3565004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schatz V, Neubert P, Rieger F, Jantsch J. Hypoxia, Hypoxia-Inducible Factor-1α, and Innate Antileishmanial Immune Responses. Front Immunol. 2018;9:216. doi: 10.3389/fimmu.2018.00216 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kumar V, Kumar A, Das S, Kumar A, Abhishek K, Verma S, et al. Leishmania donovani Activates Hypoxia Inducible Factor-1α and miR-210 for Survival in Macrophages by Downregulation of NF-κB Mediated Pro-inflammatory Immune Response. Front Microbiol. 2018;9:385. doi: 10.3389/fmicb.2018.00385 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Platanitis E, Decker T. Regulatory Networks Involving STATs, IRFs, and NFκB in Inflammation. Front Immunol. 2018;9:2542. doi: 10.3389/fimmu.2018.02542 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yao Y, Xu X-H, Jin L. Macrophage Polarization in Physiological and Pathological Pregnancy. Front Immunol. 2019;10:792. doi: 10.3389/fimmu.2019.00792 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Das S, Mukherjee S, Ali N. Super enhancer-mediated transcription of miR146a-5p drives M2 polarization during Leishmania donovani infection. PLoS Pathog. 2021;17(2):e1009343–e. doi: 10.1371/journal.ppat.1009343 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tomiotto-Pellissier F, Bortoleti BTdS, Assolini JP, Gonçalves MD, Carloto ACM, Miranda-Sapla MM, et al. Macrophage Polarization in Leishmaniasis: Broadening Horizons. Front Immunol. 2018;9:2529. doi: 10.3389/fimmu.2018.02529 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li H, Jiang T, Li M-Q, Zheng X-L, Zhao G-J. Transcriptional Regulation of Macrophages Polarization by MicroRNAs. Front Immunol. 2018;9:1175. doi: 10.3389/fimmu.2018.01175 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Banerjee S, Cui H, Xie N, Tan Z, Yang S, Icyuz M, et al. miR-125a-5p regulates differential activation of macrophages and inflammation. J Biol Chem. 2013;288(49):35428–36. Epub 10/22. doi: 10.1074/jbc.M112.426866 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhong Y, Yi C. MicroRNA-720 suppresses M2 macrophage polarization by targeting GATA3. Biosci Rep. 2016;36(4). Epub 2016/06/30. doi: 10.1042/BSR20160105 ; PubMed Central PMCID: PMC4974597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nimsarkar P, Ingale P, Singh S. Systems Studies Uncover miR-146a as a Target in Leishmania major Infection Model. ACS Omega. 2020;5(21):12516–26. doi: 10.1021/acsomega.0c01502 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pasca S, Jurj A, Petrushev B, Tomuleasa C, Matei D. MicroRNA-155 Implication in M1 Polarization and the Impact in Inflammatory Diseases. Front Immunol. 2020;11:625. Epub 2020/05/01. doi: 10.3389/fimmu.2020.00625 ; PubMed Central PMCID: PMC7174664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gholamrezaei M, Rouhani S, Mohebali M, Mohammadi-Yeganeh S, Haji Molla Hoseini M, Haghighi A, et al. MicroRNAs Expression Induces Apoptosis of Macrophages in Response to Leishmania major (MRHO/IR/75/ER): An In-Vitro and In-Vivo Study. Iran J Parasitol. 2020;15(4):475–87. doi: 10.18502/ijpa.v15i4.4851 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Muxel SM, Aoki JI, Fernandes JCR, Laranjeira-Silva MF, Zampieri RA, Acuña SM, et al. Arginine and Polyamines Fate in Leishmania Infection. Front Microbiol. 2017;8:2682. Epub 2018/01/31. doi: 10.3389/fmicb.2017.02682 ; PubMed Central PMCID: PMC5775291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Muxel SM, Acuña SM, Aoki JI, Zampieri RA, Floeter-Winter LM. Toll-Like Receptor and miRNA-let-7e Expression Alter the Inflammatory Response in Leishmania amazonensis-Infected Macrophages. Front Immunol. 2018;9:2792. Epub 2018/12/18. doi: 10.3389/fimmu.2018.02792 ; PubMed Central PMCID: PMC6283264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ma F, Liu X, Li D, Wang P, Li N, Lu L, et al. MicroRNA-466l upregulates IL-10 expression in TLR-triggered macrophages by antagonizing RNA-binding protein tristetraprolin-mediated IL-10 mRNA degradation. J Immunol (Baltimore, Md: 1950). 2010;184(11):6053–9. Epub 2010/04/23. doi: 10.4049/jimmunol.0902308 . [DOI] [PubMed] [Google Scholar]
- 47.Jafarzadeh A, Nemati M, Khorramdelazad H, Mirshafiey A. The Toll-like Receptor 2 (TLR2)-related Immunopathological Responses in the Multiple Sclerosis and Experimental Autoimmune Encephalomyelitis. Iran J Allergy Asthma Immunol. 2019;18(3):230–50. Epub 2019/09/16. doi: 10.18502/ijaai.v18i3.1117 . [DOI] [PubMed] [Google Scholar]
- 48.Guerfali FZ, Laouini D, Guizani-Tabbane L, Ottones F, Ben-Aissa K, Benkahla A, et al. Simultaneous gene expression profiling in human macrophages infected with Leishmania major parasites using SAGE. BMC Genomi. 2008;9:238. Epub 2008/05/23. doi: 10.1186/1471-2164-9-238 ; PubMed Central PMCID: PMC2430024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lemaire J, Mkannez G, Guerfali FZ, Gustin C, Attia H, Sghaier RM, et al. MicroRNA expression profile in human macrophages in response to Leishmania major infection. PLoS Negl Trop Dis. 2013;7(10):e2478. Epub 2013/10/08. doi: 10.1371/journal.pntd.0002478 ; PubMed Central PMCID: PMC3789763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Favila MA, Geraci NS, Zeng E, Harker B, Condon D, Cotton RN, et al. Human dendritic cells exhibit a pronounced type I IFN signature following Leishmania major infection that is required for IL-12 induction. J Immunol (Baltimore, Md: 1950). 2014;192(12):5863–72. Epub 2014/05/09. doi: 10.4049/jimmunol.1203230 ; PubMed Central PMCID: PMC4052223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hamidi F, Mohammadi-Yeganeh S, Haji Molla Hoseini M, Seyyed Tabaei SJ, Taghipour N, Lasjerdi Z, et al. Inhibition of anti-inflammatory cytokines, IL-10 and TGF-β, in Leishmania major infected macrophage by miRNAs: A new therapeutic modality against leishmaniasis. Microb Pathog. 2021;153:104777. Epub 2021/02/17. doi: 10.1016/j.micpath.2021.104777 . [DOI] [PubMed] [Google Scholar]
- 52.Varikuti S, Natarajan G, Volpedo G, Singh B, Hamza O, Messick GV, et al. MicroRNA 155 Contributes to Host Immunity against Leishmania donovani but Is Not Essential for Resolution of Infection. Infect Immun. 2019;87(8). Epub 2019/06/12. doi: 10.1128/iai.00307-19 ; PubMed Central PMCID: PMC6652779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moore KJ, Matlashewski G. Intracellular infection by Leishmania donovani inhibits macrophage apoptosis. J Immunol (Baltimore, Md: 1950). 1994;152(6):2930–7. Epub 1994/03/15. . [PubMed] [Google Scholar]
- 54.Cianciulli A, Porro C, Calvello R, Trotta T, Panaro MA. Resistance to apoptosis in Leishmania infantum-infected human macrophages: a critical role for anti-apoptotic Bcl-2 protein and cellular IAP1/2. Clin Exp Med. 2018;18(2):251–61. Epub 2017/12/09. doi: 10.1007/s10238-017-0482-1 . [DOI] [PubMed] [Google Scholar]
- 55.Aghaei M, KhanAhmad H, Aghaei S, Ali Nilforoushzadeh M, Mohaghegh MA, Hejazi SH. The role of Bax in the apoptosis of Leishmania-infected macrophages. Microb Pathog. 2020;139:103892. Epub 2019/11/30. doi: 10.1016/j.micpath.2019.103892 . [DOI] [PubMed] [Google Scholar]
- 56.Rajasekhar M, Olsson AM, Steel KJ, Georgouli M, Ranasinghe U, Brender Read C, et al. MicroRNA-155 contributes to enhanced resistance to apoptosis in monocytes from patients with rheumatoid arthritis. J Autoimmun. 2017;79:53–62. Epub 2017/01/26. doi: 10.1016/j.jaut.2017.01.002 ; PubMed Central PMCID: PMC5397583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Li GS, Cui L, Wang GD. miR-155-5p regulates macrophage M1 polarization and apoptosis in the synovial fluid of patients with knee osteoarthritis. Exp Ther Med. 2021;21(1):68. Epub 2020/12/29. doi: 10.3892/etm.2020.9500 ; PubMed Central PMCID: PMC7716652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Alizadeh S, Kaviani S, Soleimani M, Abroun S, Kashani-Khatib Z, Asgharzadeh A, et al. Mir-55 inhibition can reduce cell proliferation and induce apoptosis in Jurkat (Acute T cell Leukemia) cell line. Iran J Pediatr Hematol Oncol. 2014;4(4):141–50. Epub 2015/01/20. ; PubMed Central PMCID: PMC4293513. [PMC free article] [PubMed] [Google Scholar]
- 59.De Santis R, Liepelt A, Mossanen JC, Dueck A, Simons N, Mohs A, et al. miR-155 targets Caspase-3 mRNA in activated macrophages. RNA Biol. 2016;13(1):43–58. Epub 2015/11/18. doi: 10.1080/15476286.2015.1109768 ; PubMed Central PMCID: PMC4829287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Abdullah OA, El Gazzar WB, Salem TI, Elmohamady MN, Nasif SN, Eltaher SM. miR-15a: a potential diagnostic biomarker and a candidate for non-operative therapeutic modality for age-related cataract. Br J Biomed Sci. 2019;76(4):184–9. Epub 2019/07/03. doi: 10.1080/09674845.2019.1639337 . [DOI] [PubMed] [Google Scholar]
- 61.Eren RO, Reverte M, Rossi M, Hartley MA, Castiglioni P, Prevel F, et al. Mammalian Innate Immune Response to a Leishmania-Resident RNA Virus Increases Macrophage Survival to Promote Parasite Persistence. Cell Host Microbe. 2016;20(3):318–28. Epub 2016/09/07. doi: 10.1016/j.chom.2016.08.001 ; PubMed Central PMCID: PMC5493041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lasjerdi Z, Ghanbarian H, Mohammadi Yeganeh S, Seyyed Tabaei SJ, Mohebali M, Taghipour N, et al. Comparative Expression Profile Analysis of Apoptosis-Related miRNA and Its Target Gene in Leishmania major Infected Macrophages. Iran J Parasitol. 2020;15(3):332–40. Epub 2020/10/22. doi: 10.18502/ijpa.v15i3.4197 ; PubMed Central PMCID: PMC7548466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hashemi N, Sharifi M, Masjedi M, Tolouei S, Hashemi M, Mortazavidehkordi N, et al. Locked nucleic acid -anti- let-7a induces apoptosis and necrosis in macrophages infected with Leishmania major. Microb Pathog. 2018;119:193–9. Epub 2018/04/16. doi: 10.1016/j.micpath.2018.03.057 . [DOI] [PubMed] [Google Scholar]
- 64.Singh AK, Pandey RK, Shaha C, Madhubala R. MicroRNA expression profiling of Leishmania donovani-infected host cells uncovers the regulatory role of MIR30A-3p in host autophagy. Autophagy. 2016;12(10):1817–31. Epub 2016/07/28. doi: 10.1080/15548627.2016.1203500 ; PubMed Central PMCID: PMC5079678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Frank B, Marcu A, de Oliveira Almeida Petersen AL, Weber H, Stigloher C, Mottram JC, et al. Autophagic digestion of Leishmania major by host macrophages is associated with differential expression of BNIP3, CTSE, and the miRNAs miR-101c, miR-129, and miR-210. Parasit Vectors. 2015;8:404. doi: 10.1186/s13071-015-0974-3 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lee H-J, Woo Y, Hahn T-W, Jung YM, Jung Y-J. Formation and Maturation of the Phagosome: A Key Mechanism in Innate Immunity against Intracellular Bacterial Infection. Microorganisms. 2020;8(9):1298. doi: 10.3390/microorganisms8091298 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Verma JK, Rastogi R, Mukhopadhyay A. Leishmania donovani resides in modified early endosomes by upregulating Rab5a expression via the downregulation of miR-494. PLoS Pathog. 2017;13(6):e1006459–e. doi: 10.1371/journal.ppat.1006459 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ren N, Gao G, Sun Y, Zhang L, Wang H, Hua W, et al. MicroRNA signatures from multidrug-resistant Mycobacterium tuberculosis. Mol Med Rep. 2015;12(5):6561–7. Epub 2015/09/02. doi: 10.3892/mmr.2015.4262 ; PubMed Central PMCID: PMC4626138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lampis A, Hahne JC, Hedayat S, Valeri N. MicroRNAs as mediators of drug resistance mechanisms. Curr Opin Pharmacol. 2020;54:44–50. Epub 2020/09/09. doi: 10.1016/j.coph.2020.08.004 . [DOI] [PubMed] [Google Scholar]
- 70.Rossato M, Curtale G, Tamassia N, Castellucci M, Mori L, Gasperini S, et al. IL-10-induced microRNA-187 negatively regulates TNF-α, IL-6, and IL-12p40 production in TLR4-stimulated monocytes. Proc Natl Acad Sci U S A. 2012;109(45):E3101–10. Epub 2012/10/17. doi: 10.1073/pnas.1209100109 ; PubMed Central PMCID: PMC3494907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cheung ST, So EY, Chang D, Ming-Lum A, Mui AL. Interleukin-10 inhibits lipopolysaccharide induced miR-155 precursor stability and maturation. PLoS ONE. 2013;8(8):e71336. Epub 2013/08/21. doi: 10.1371/journal.pone.0071336 ; PubMed Central PMCID: PMC3741136 pharmaceuticals. She holds less than 5% of the company shares and does not receive any compensation nor involved in any company activity. This does not alter the authors’ adherence to all the PLOS ONE policies on sharing data and materials. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.McCoy CE, Sheedy FJ, Qualls JE, Doyle SL, Quinn SR, Murray PJ, et al. IL-10 inhibits miR-155 induction by toll-like receptors. J Biol Chem. 2010;285(27):20492–8. Epub 2010/05/04. doi: 10.1074/jbc.M110.102111 ; PubMed Central PMCID: PMC2898307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Curtale G, Mirolo M, Renzi TA, Rossato M, Bazzoni F, Locati M. Negative regulation of Toll-like receptor 4 signaling by IL-10-dependent microRNA-146b. Proc Natl Acad Sci U S A. 2013;110(28):11499–504. Epub 06/24. doi: 10.1073/pnas.1219852110 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cardwell L, Weaver B. IL-10 Inhibits LPS-Induced Expression of miR-147 in Murine Macrophages. Adv Biol Chem. 2014;4:261–73. doi: 10.4236/abc.2014.44032 [DOI] [Google Scholar]
- 75.Penas F, Mirkin GA, Vera M, Cevey Á, González CD, Gómez MI, et al. Treatment in vitro with PPARα and PPARγ ligands drives M1-to-M2 polarization of macrophages from T. cruzi-infected mice. Biochim Biophys Acta. 2015;1852(5):893–904. Epub 2015/01/06. doi: 10.1016/j.bbadis.2014.12.019 . [DOI] [PubMed] [Google Scholar]
- 76.Jennewein C, von Knethen A, Schmid T, Brüne B. MicroRNA-27b contributes to lipopolysaccharide-mediated peroxisome proliferator-activated receptor gamma (PPARgamma) mRNA destabilization. J Biol Chem. 2010;285(16):11846–53. Epub 2010/02/19. doi: 10.1074/jbc.M109.066399 ; PubMed Central PMCID: PMC2852921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wu C, Xue Y, Wang P, Lin L, Liu Q, Li N, et al. IFN-γ primes macrophage activation by increasing phosphatase and tensin homolog via downregulation of miR-3473b. J Immunol (Baltimore, Md: 1950). 2014;193(6):3036–44. Epub 2014/08/06. doi: 10.4049/jimmunol.1302379 . [DOI] [PubMed] [Google Scholar]
- 78.Domingo-Gonzalez R, Wilke CA, Huang SK, Laouar Y, Brown JP, Freeman CM, et al. Transforming growth factor-β induces microRNA-29b to promote murine alveolar macrophage dysfunction after bone marrow transplantation. Am J Physiol Lung Cell Mol Physiol. 2015;308(1):L86–95. Epub 2014/11/02. doi: 10.1152/ajplung.00283.2014 ; PubMed Central PMCID: PMC4281703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Self-Fordham JB, Naqvi AR, Uttamani JR, Kulkarni V, Nares S. MicroRNA: Dynamic Regulators of Macrophage Polarization and Plasticity. Front Immunol. 2017;8. doi: 10.3389/fimmu.2017.01062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wang Z, Brandt S, Medeiros A, Wang S, Wu H, Dent A, et al. MicroRNA 21 is a homeostatic regulator of macrophage polarization and prevents prostaglandin E2-mediated M2 generation. PloS ONE. 2015;10(2):e0115855. Epub 2015/02/24. doi: 10.1371/journal.pone.0115855 ; PubMed Central PMCID: PMC4338261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lin L, Hou J, Ma F, Wang P, Liu X, Li N, et al. Type I IFN inhibits innate IL-10 production in macrophages through histone deacetylase 11 by downregulating microRNA-145. J Immunol (Baltimore, Md: 1950). 2013;191(7):3896–904. Epub 2013/08/28. doi: 10.4049/jimmunol.1203450 . [DOI] [PubMed] [Google Scholar]