African relevance
-
•
There is an urgent need to scale up training of the emergency care workforce.
-
•
Virtual education platforms provide the opportunity to extend emergency medicine education, especially in light of disruptions caused by COVID-19.
-
•
Project ECHO telementoring is a robust model that is amenable to emergency medical education.
-
•
This paper describes the use of Project ECHO telementoring for PoCUS training in Kenya.
-
•
We describe the challenges of implementation and potential ways to overcome them.
Keywords: Project ECHO, Telementoring, Emergency care
Abstract
The COVID-19 pandemic has led to global disruptions in emergency medicine (EM) teaching and training and highlighted the need to strengthen virtual learning platforms. This disruption coincides with essential efforts to scale up training of the emergency healthcare workforce, particularly in low-resource settings where the specialty is not well developed. Thus, there is growing interest in strengthening virtual platforms that can be used to support emergency medicine educational initiatives globally. These platforms must be robust, context specific and sustainable in low-resource environments. This report describes the implementation of Project ECHO (Extension for Community Healthcare Outcomes), a telementoring platform originally designed to extend specialist support to health care workers in rural and underserved areas in New Mexico. This platform has now been implemented successfully across the globe. We describe the challenges and benefits of the Project ECHO model to support a Point-of-Care Ultrasound (POCUS) training program for health care providers in Kenya who do not have specialty training in emergency medicine. Our experience using this platform suggests it is amenable to capacity building for non-specialist emergency care providers in low-resource settings, but key challenges to implementation exist. These include unreliable and costly internet access and lack of institutional buy-in.
Background
The COVID-19 pandemic has placed significant strain on healthcare systems and disrupted medical education. Simultaneously, there is growing attention to the looming crisis of health care workforce limitations in low-resource settings. The WHO predicts that the world will be short of 12.9 million healthcare workers by 2035, and these shortages will be felt more acutely in Sub-Saharan Africa [1]. In this environment, virtual education has gained increased prominence and proved essential to supporting medical education, building the healthcare workforce and supporting equitable health systems [2].
The global flow of ideas and knowledge is crucial to the development of a skilled healthcare workforce [3]. Even prior to the COVID-19 pandemic, virtual training programs created opportunities to democratize knowledge, particularly in low-resource settings. Within emergency medicine, virtual education and training has become more prevalent in recent years [4,5]. Evidence from the African region shows that emergency healthcare professionals are increasingly looking online for free and open access medical education (FOAM) resources to augment their training and support patient care [6]. Internationally, the growing demand for online, structured emergency medicine content to support remote learning has become even more pressing in the setting of significant travel restrictions during the pandemic [7].
In this push for virtual learning, telementoring stands out as a modality for structured, equitable and collaborative learning within institutions, regions and across borders. It is also an effective tool for healthcare worker capacity building. Telementoring seeks to build a community in which specialists can successfully guide and support primary healthcare workers in remote and underserved areas [8]. This remote training and support leads to improvements in quality of patient care, accuracy of patient diagnosis, and reduction in medical costs [9], [10], [11], [12].
Project ECHO: A telementoring platform for multidirectional education and remote collaboration
Project ECHO was developed at the University of New Mexico Health Sciences Center with the goal of expanding specialist Hepatitis C management into underserved regions within the state [13]. This model was invented to address the needs of primary health care providers with limited specialist training who were working in rural clinics treating patients with Hepatitis C.
The Project ECHO model is distinct from telemedicine, which is described as “the use of medical information from one site to another via electronic communications to improve a patient's clinical health status” [14]. Telemedicine allows a healthcare provider to connect directly to a patient through different modalities such as video calls, video conferencing, secure telephone calls, emails, web portals and mobile health applications (m-health) [15]. Telemedicine can further be divided into synchronous interactions which occur in real time, versus asynchronous interaction where data is obtained, transmitted and stored for later review. Telementoring on the other hand involves the use of telecommunication technology to enable a mentor/expert to provide remote guidance to a trainee. Telementoring has been used successfully in different settings, including on-time specialist guidance to a trainee performing a surgical procedure [16]. Teleultrasound is an example of a synchronous telementoring interaction where an expert provides real time guidance to a trainee [17].
Project ECHO telementoring is distinct in that it brings together a group of experts to support teams of healthcare workers in underserved rural or isolated regions. The model works through regularly planned videoconferences known as Tele-ECHO clinics, where primary healthcare providers or trainees present patient cases using a standardized case format, and specialists at academic health centres provide feedback about best practices. This flipped classroom model allows the primary providers to discuss cases that are relevant to their daily work and receive guidance on best practices and evidence-based care. Thus, the providers from isolated and underserved healthcare facilities can care for patients at their medical clinics without the need for referrals that would previously take months to complete.
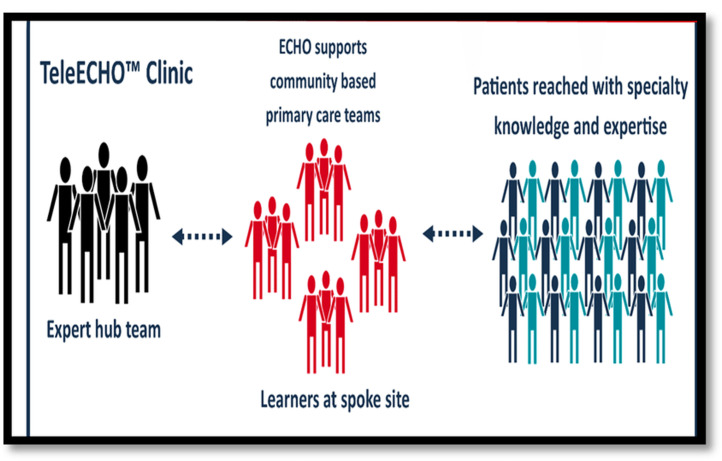
The Project ECHO platform uses a ‘Hub” and ‘Spoke’ model where experts/ trainers at a central Hub location connect with health care providers at multiple spoke sites through regular Tele-ECHO video conferencing sessions (Fig. 1). The platform also incorporates a management tool called iECHO that allows program managers to organize and collect data on trainee participation.
Fig. 1.
Project ECHO model of care. Source: ECHO Institute UNM.
Since its inception, Project ECHO has expanded to create hundreds of training programs in a variety of fields in the U.S. and around the world [18], [19], [20]. Recent applications include training teams of frontline healthcare workers from 55 countries on patient care principles e.g. infection prevention and control, patient screening and triage during the COVID-19 pandemic [21]. Other uses include overcoming barriers to geriatric post-acute and long term care due to COVID-19 [22]. Project ECHO stands out as a virtual training model since it makes use of structured, regularly scheduled sessions (Tele-ECHO clinics), and emphasizes the use of a set curriculum that is developed and updated based on trainee needs.
Rationale for the use of Project ECHO model for POCUS training in rural Kenya
There is a growing recognition for the value of POCUS use in acute and critical care practice in low-resource settings. Many aspects of POCUS such as portability and increasing affordability make it uniquely suited to low-resource settings. The WHO essential package of emergency care now includes availability of POCUS as an important tool to be made available in LMIC emergency centres [23]. Thus the demand for POCUS education has increased, both within emergency medicine training programs and for non-specialist health care workers providing emergency care.
In 2013, we developed a POCUS training program for healthcare workers in rural areas and small towns in Kenya [24]. The training was focused on the Extended Focused Assessment with Sonography in Trauma (E-FAST) and focused obstetrics. Trainees were medical officers (graduates from medical school who have completed 1-year internship), clinical officers (mid-level providers with a 3-year diploma in clinical practice), nurses and radiographers without specific training in emergency medicine. Trainees received a pre-course multimedia manual and pre-course testing prior to presenting for hands-on training. After the training, they received an ultrasound machine to continue POCUS practice at their facilities. Follow-up re-evaluation and re-training was scheduled 3-4 months afterwards, and the process was repeated until the trainee was deemed competent. There were 3 core POCUS trainers in this program who worked with a rotating group of visiting specialists during hands-on training sessions. Through this program, approximately 150 primary health care providers from 60 health facilities across the country were trained.
However, we found that trainees required closer supervision and ongoing guidance outside of the regularly scheduled facility visits 3-4 months post-training. These circumstances led us to consider a telementoring platform while working to increase our pool of trainers. Since our trainees were located in different facilities across the country, it was necessary to consider a platform that brought together multiple geographically isolated teams in a single learning environment. This led our team to trial project ECHO.
Development process
The first step involved selecting a local organization that was focused on the development of emergency medicine in Kenya and that had a national reach. We chose to work with Emergency Medicine Kenya Foundation (EMKF), a non-governmental organization that was formed in 2015 and that has been actively promoting emergency medicine through education, research, and advocacy. Second, the POCUS training group underwent Project ECHO training at the ECHO institute in New Mexico. This training consisted of 2 parts: A 90-minute introduction via videoconference and a 3-day on-site training. Upon successful completion of the training, EMKF was signed on as a project ECHO collaborating partner.
Implementation phase
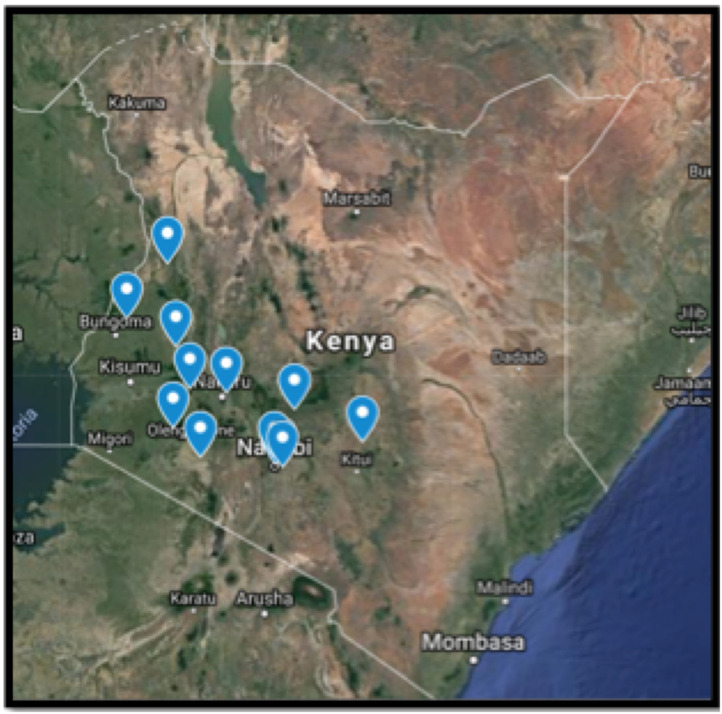
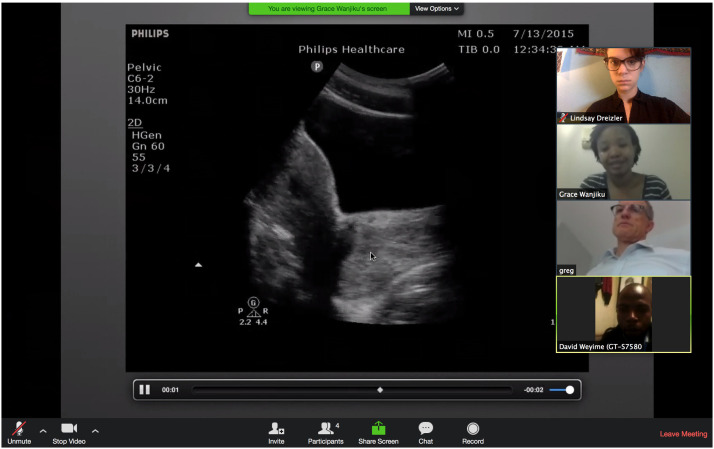
In 2018, we undertook a 16-week pilot study to investigate the feasibility of Project ECHO as a telementoring model. Fourteen trainees (3 doctors, 3 clinical officers, 4 nurses and 4 radiographers) from 11 healthcare facilities (Fig. 2) who had recently received hands-on training in E-FAST and focused obstetrics were chosen to participate. The study participants received funds to purchase 3G-network access from their mobile phone service provider, and to download zoom onto their smartphones. Every 2 weeks, study participants received a link via WhatsApp to log-on for a 2-hour Tele-ECHO session on Zoom (Fig. 3). The curriculum for the 16 weeks was based on topics covered during the POCUS training program, and is outlined on Table 1. The telementoring sessions were structured to primarily focus on discussing the cases submitted by the trainees, followed by a didactic on the topic outlined on the curriculum. The cases that trainees submitted for discussion are also outlined on Table 1. At the end of the pilot, a qualtrics survey was used to collect participant feedback. The link to the survey was sent to the participants via WhatsApp.
Fig. 2.
Tele-ECHO clinic participant locations.
Fig. 3.
Kenya rural POCUS Tele-ECHO clinic on zoom.
Table 1.
Tele-ECHO curriculum
| Date | Topic | Cases |
|---|---|---|
| Week 1 | Introduction to point-of-care ultrasound | None |
| Week 3 | E-FAST / Trauma ultrasound | -Motor vehicle accident victim with splenic rupture -Blunt trauma following assault |
| Week 5 | First trimester ultrasound: Establishing an Intra-Uterine Pregnancy (IUP) | -Normal early pregnancy -Ectopic pregnancy |
| Week 7 | First trimester dating | -Use of crown-lump length for dating |
| Week 9 | First trimester pain and bleeding | -Spontaenous abortion -Heterotropic pregnancy |
| Week 11 | Second trimester dating | -Multiple pregnancy |
| Week 13 | Establishing Fetal Heart Rate (FHR) | -Placental abruption and low FHR after motor vehicle accident |
| Week 15 | Establishing fetal presentation and placental location. | -Placenta Previa |
| Week 17 | Review, Q &A |
Outcomes
The RE-AIM framework (Reach, Effectiveness, Adoption Implementation and Maintenance) was used to evaluate the feasibility of Project ECHO telementoring in this pilot study [25]. These outcomes are based on the qualtrics survey that was sent to the trainees, and also based on observations and adaptations made during the implementation of the study.
Reach
When approached, all 14 POCUS trainees were willing to participate in the telementoring study. In addition, all the trainees had smartphones which are the primary mode of Internet access in Kenya. Smartphone penetration continues to accelerate in Sub-Saharan Africa, and with it, access to 3G and 4G broadband networks through mobile phone operators [26]. Thus, all the trainees, including those in the very remote clinics, had the ability to connect to zoom on their phone. However, the strength of the internet connection varied, and up to 50% of the trainees reported that at times their connection was poor and would drop off during telementoring sessions. Additional challenges included the phone powering off due to lack of electricity.
Effectiveness
The majority of the trainees (83%) felt that the material presented to them was relevant for their practice, and 100% felt that the cases were clear and well presented. When asked if the sessions increased their confidence in ultrasound scanning, 40% replied Strongly agree, and 40 % replied Agree.
Adoption
In assessing adoption, we considered the setting in which the trainees work, the nature of their work environment and how that impacted the ability to participate in POCUS telementoring. The significant challenging factor here was competing clinical obligations. Up to 67% of the trainees reported that work obligations kept them from participating in the sessions. It was difficult to find a day and time when all the trainees were available, and they settled on Fridays from 5pm to 7pm. This time slot proved difficult since trainees had to rush to complete clinic activities, commute to their homes and care for their families.
Implementation
When the pilot study started, trainees attempted to use their hospital or personal computers to log onto zoom. In addition, weekly notifications were initially sent to their emails. This approach did not work and the option preferred by the trainees was to use their smartphones for internet access and the WhatsApp messaging application for weekly notifications. However, internet access through the smartphone is expensive and financially prohibitive. Therefore, we had to provide financial support to offset this cost (10 USD per trainee per month to enable participation in 2-hour video conferences twice a month).
Maintenance
Maintenance was not evaluated on this pilot study. However, the outcomes so far indicate that telementoring through Project ECHO provided desired ongoing education and would be feasible if key infrastructural and institutional barriers are addressed ahead of implementation.
Discussion
Our experiences using Project ECHO telementoring to support POCUS training in rural Kenya is an instructive case study on the opportunities and challenges in the use of virtual platforms to support collaborative emergency medical education in low-resource settings. The goal of Project ECHO is to create learning networks and foster a community of learners who share evidence and best practices to improve patient care. This platform is amenable to emergency medicine training due to its structured nature, the ability to utilize a case-based curriculum during regularly scheduled sessions, and built-in tools to evaluate trainee outcomes concurrent with implementation.
However, significant challenges still exist in the effort to create sustainable virtual emergency medicine training platforms in rural Kenya and other similar low-resource environments. A 2018 review of the barriers to virtual medical education cited poor infrastructure and lack of institutional plans for implementation [27]. Our experiences highlight that while internet quality and access is improving, many places still face significant issues with bandwidth and reliability. Most people in Kenya access the Internet through their phones, which can be expensive and create barriers to widespread integration.
Institutional buy-in is important when it comes to investing in Internet connectivity and releasing health-care workers at scheduled times to participate in online instruction. To support trainee buy-in, telementoring modules can be packaged to provide Continuing Medical Education (CME) points in order to stimulate and reward participation [28]. Importantly there needs to be a thorough evaluation of institutional and individual readiness to participate in such a program. This would ensure that the institution is prepared to make the investments to support telementoring infrastructure and that trainees are willing to participate and engage in the program.
Telementoring via project ECHO is well suited for emergency medicine training programs that already have dedicated time for medical education. This is different from our pilot, where trainees from rural facilities did not have scheduled educational sessions. POCUS training is a key milestone in post-graduate emergency medicine training. Many POCUS training models involve a “boot camp” style introduction with hands-on supervised scanning, followed by routine follow-up training, image review for quality assurance and feedback. The follow-up process can be challenging in low-resource settings with few POCUS educators. Under these circumstances, virtual ultrasound instruction has shown promising potential to improve provider knowledge and patient outcomes [29], [30], [31]. Since EM trainees have protected time for education, it is feasible to hold regular image review and case discussions via videoconference. POCUS trainers from large academic centres can create a “Hub” that allows them to hold virtual image review and teach learners in multiple “spoke sites” locally or internationally. They can also evaluate trainee outcomes by performing remote image review and providing online pre and post tests. However, this still requires stable internet and the ability to de-identify, store and forward ultrasound images and clips for review during the telementoring session.
This study is limited in that it is a very small pilot study carried out in rural areas in a low-resource country. Thus, our results may not be generalizable across different low-resource settings due to variations in telecommunications infrastructure. However, since our trainees were located in different facilities across the country, our outcomes are a better indicator of the challenges involved in creating a telementoring network as opposed to studies involving one or two facilities. Telecommunications continue to improve and ultrasound technology is simultaneously evolving to include smart-phone connected devices that simplify the process of image transmission for remote review. Some of the newer ultrasound devices also have in-built teleultrasound capability. This will facilitate future implementation of larger scale POCUS telementoring programs that include robust image review and feedback mechanisms.
Conclusion
Structured virtual education has significant potential to boost emergency care education, especially during the disruptions imposed by the COVID-19 pandemic. The Project ECHO platform is well suited to extend specialist knowledge into underserved areas, and to build a community of practice among specialist and non-specialist emergency care providers. Our experiences using the Project ECHO telementoring platform for POCUS education in rural Kenya demonstrated its potential, but significant challenges still exist. There is a need for investment into internet access, and the provision of protected time for healthcare providers to participate in scheduled tele-ECHO clinics. There is also a need for further research into telementoring platforms in low-resource settings to find out which ones work best and why, and what the cost implications are. This will continue to further the goal of sustainably engaging emergency care learners in a structured, context specific virtual training environment.
Dissemination of results
This commentary aims to present our experiences with the Project ECHO telementoring platform within the context of emergency medicine education in the African region. We present the opportunities and challenges of its use, and tools to guide educators in the region who may wish to implement it.
Authors contribution
Authors contributed as follows to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: GW contributed 50%, LD contributed 25%, GB and BW contributed 12.5% each. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of Competing Interest
The authors declared no conflicts of interest.
Acknowledgment
We thank the ECHO Institute at the University of New Mexico for in-kind support of our work through the following: Providing free introductory and immersion ECHO training, free access to Zoom, iECHO and technical support. We would like to thank Sonja Kapadia BA for editing the manuscript.
References
- 1.WHO . WHO. World Health Organization; 2022. A Universal Truth: No Health Without a Workforce [Internet]https://www.who.int/workforcealliance/knowledge/resources/hrhreport2013/en/ [cited 2022 Mar 18]. Available from. [Google Scholar]
- 2.TABATABAI S. COVID-19 impact and virtual medical education. J Adv Med Educ Prof. 2020;8(3):140–143. doi: 10.30476/jamp.2020.86070.1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376(9756):1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 4.Leszczyński P, Gotlib J, Kopański Z, Wejnarski A, Świeżewski S, Gałązkowski R. Analysis of Web-based learning methods in emergency medicine: randomized controlled trial. Arch Med Sci AMS. 2018;14(3):687–694. doi: 10.5114/aoms.2015.56422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Windish R, Stuart P, de la Cruz R, Murray A. Enhancing intern emergency medicine education using a combined didactic and web-based learning curriculum: The EDGE programme. Emerg Med Australas EMA. 2019;31(5):837–842. doi: 10.1111/1742-6723.13352. [DOI] [PubMed] [Google Scholar]
- 6.Palliam S, Mahomed Z, Hoffman D, Laher AE. Learning in the digital era – awareness and usage of free open access meducation among emergency department doctors. Cureus. 2022;11(11):e6223. doi: 10.7759/cureus.6223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cevik AA, Cakal ED, Kwan J. From the pandemic's front lines: a social responsibility initiative to develop an international free online emergency medicine course for medical students. Afr J Emerg Med Rev Afr Med Urgence. 2021;11(1):1–2. doi: 10.1016/j.afjem.2020.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McConnell KA, Krisher LK, Lenssen M, Bunik M, Bunge Montes S, Domek GJ. Telehealth to expand community health nurse education in Rural Guatemala: a pilot feasibility and acceptability evaluation. Front Public Health. 2017;5:60. doi: 10.3389/fpubh.2017.00060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lopez-Bushnell FK. Increasing communication with healthcare providers for patients with limited english proficiency through interpreter language services education. MEDSURG Nurs. 2020;29(2):89–95. [Google Scholar]
- 10.Matimba A, Woodward R, Tambo E, Ramsay M, Gwanzura L, Guramatunhu S. Tele-ophthalmology: opportunities for improving diabetes eye care in resource- and specialist-limited Sub-Saharan African countries. J Telemed Telecare. 2016;22(5):311–316. doi: 10.1177/1357633X15604083. Jul. [DOI] [PubMed] [Google Scholar]
- 11.Qaddoumi I, Mansour A, Musharbash A, Drake J, Swaidan M, Tihan T, et al. Impact of telemedicine on pediatric neuro-oncology in a developing country: the Jordanian-Canadian experience. Pediatr Blood Cancer. 2007;48(1):39–43. doi: 10.1002/pbc.21085. [DOI] [PubMed] [Google Scholar]
- 12.Bagayoko CO, Traoré D, Thevoz L, Diabaté S, Pecoul D, Niang M, et al. Medical and economic benefits of telehealth in low- and middle-income countries: results of a study in four district hospitals in Mali. BMC Health Serv Res. 2014;14(1):S9. doi: 10.1186/1472-6963-14-S1-S9. Suppl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arora S, Thornton K, Jenkusky SM, Parish B, Scaletti JV. Project ECHO: linking university specialists with rural and prison-based clinicians to improve care for people with chronic hepatitis C in New Mexico. Public Health Rep Wash DC 1974. 2007;122(2):74–77. doi: 10.1177/00333549071220S214. Suppl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schlachta CM, Nguyen NT, Ponsky T, Dunkin B. Project 6 Summit: SAGES telementoring initiative. Surg Endosc. 2016;30(9):3665–3672. doi: 10.1007/s00464-016-4988-5. [DOI] [PubMed] [Google Scholar]
- 15.Shanbehzadeh M, Kazemi-Arpanahi H, Kalkhajeh SG, Basati G. Systematic review on telemedicine platforms in lockdown periods: lessons learned from the COVID-19 pandemic. J Educ Health Promot. 2021;10:211. doi: 10.4103/jehp.jehp_1419_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Erridge S, Yeung DKT, Patel HRH, Purkayastha S. Telementoring of Surgeons: A Systematic Review. Surg Innov. 2019;26(1):95–111. doi: 10.1177/1553350618813250. [DOI] [PubMed] [Google Scholar]
- 17.Recker F, Höhne E, Damjanovic D, Schäfer VS. Ultrasound in Telemedicine. A Brief Overview. Appl Sci. 2022;12(3):958. [Google Scholar]
- 18.Mazurek MO, Parker RA, Chan J, Kuhlthau K, Sohl K, for the ECHO Autism Collaborative Effectiveness of the extension for community health outcomes model as applied to primary care for autism: a partial stepped-wedge randomized clinical trial. JAMA Pediatr. 2020;174(5) doi: 10.1001/jamapediatrics.2019.6306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Babu R, Dhanasekaran K, Mehrotra R, Hariprasad R. Leveraging technology for nation-wide training of healthcare professionals in cancer screening in india: a methods article. J Cancer Educ Off J Am Assoc Cancer Educ. 2021;36(5):950–956. doi: 10.1007/s13187-020-01720-6. [DOI] [PubMed] [Google Scholar]
- 20.Arora S, Mate KS, Jones JL, Sevin CB, Clewett E, Langley G, et al. Enhancing collaborative learning for quality improvement: evidence from the improving clinical flow project, a breakthrough series collaborative with project ECHO. Jt Comm J Qual Patient Saf. 2020;46(8):448–456. doi: 10.1016/j.jcjq.2020.04.013. [DOI] [PubMed] [Google Scholar]
- 21.Kharel R, Baird J, Vaishnav H, Chillara N, Lee JA, Genisca A, et al. Development and assessment of novel virtual COVID-19 trainer-of trainers course implemented by an academic-humanitarian partnership. Glob Health Action. 2022;15(1) doi: 10.1080/16549716.2021.2010391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Archbald-Pannone LR, Harris DA, Albero K, Steele RL, Pannone AF, Mutter JB. COVID-19 collaborative model for an academic hospital and long-term care facilities. J Am Med Dir Assoc. 2020;21(7):939–942. doi: 10.1016/j.jamda.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reynolds TA, Sawe H, Rubiano AM, Shin SD, Wallis L, Mock CN. Disease Control Priorities: Improving Health and Reducing Poverty [Internet] 3rd ed. The International Bank for Reconstruction and Development /The World Bank; Washington (DC): 2017. Strengthening health systems to provide emergency care.http://www.ncbi.nlm.nih.gov/books/NBK525279/ In: Jamison DT, Gelband H, Horton S, Jha P, Laxminarayan R, Mock CN, et al., editors. [cited 2022 Jan 31]. Available from. [PubMed] [Google Scholar]
- 24.Wanjiku GW, Bell G, Wachira B. Assessing a novel point-of-care ultrasound training program for rural healthcare providers in Kenya. BMC Health Serv Res. 2018;18(1):607. doi: 10.1186/s12913-018-3196-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Glasgow RE, Harden SM, Gaglio B, Rabin B, Smith ML, Porter GC, et al. RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Front Public Health. 2019;7:64. doi: 10.3389/fpubh.2019.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The State of Mobile Internet Connectivity Report 2019 [Internet]. Mobile for Development. [cited 2022 Mar 18]. Available from: https://www.gsma.com/mobilefordevelopment/resources/the-state-of-mobile-internet-connectivity-report-2019/
- 27.Dreizler L, Wanjiku GW. Tele-ECHO for point-of-care ultrasound in rural kenya: a feasibility study. R I Med J. 2013;102(7):28–31. 2019 Sep 3. [PubMed] [Google Scholar]
- 28.Smith A, Addison R, Rogers P, Stone-McLean J, Boyd S, Hoover K, et al. Remote mentoring of point-of-care ultrasound skills to inexperienced operators using multiple telemedicine platforms: is a cell phone good enough? J Ultrasound Med Off J Am Inst Ultrasound Med. 2018;37(11):2517–2525. doi: 10.1002/jum.14609. [DOI] [PubMed] [Google Scholar]
- 29.Poland S, Frey JA, Khobrani A, Ondrejka JE, Ruhlin MU, George RL, et al. Telepresent focused assessment with sonography for trauma examination training versus traditional training for medical students: a simulation-based pilot study. J Ultrasound Med Off J Am Inst Ultrasound Med. 2018;37(8):1985–1992. doi: 10.1002/jum.14551. [DOI] [PubMed] [Google Scholar]
- 30.Winn S, McKeown P, Lotfipour S, Maguire GA, Youm JH, Wiechmann W, et al. Remote, synchronous, hands-on ultrasound education. Telemed J E-Health Off J Am Telemed Assoc. 2015;21(7):593–597. doi: 10.1089/tmj.2014.0050. [DOI] [PubMed] [Google Scholar]
- 31.O'Doherty D, Dromey M, Lougheed J, Hannigan A, Last J, McGrath D. Barriers and solutions to online learning in medical education – an integrative review. BMC Med Educ. 2018;18(1):130. doi: 10.1186/s12909-018-1240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]