Abstract
Background
There has been growing evidence of comorbidity between internet addiction and depression in youth during the COVID-19 period. According to the network theory, this may arise from the interplay of symptoms shared by these two mental disorders. Therefore, we examined this underlying process by measuring the changes in the central and bridge symptoms of the co-occurrence networks across time.
Methods
A total of 852 Chinese college students were recruited during two waves (T1: August 2020; T2: November 2020), and reported their internet addiction symptoms and depressive symptoms. Network analysis was utilized for the statistical analysis.
Results
The internet addiction symptoms “escape” and “irritable,” and depression symptoms “energy” and “guilty” were the central symptoms for both waves. At the same time, “guilty” and “escape” were identified as bridge symptoms. Notably, the correlation between “anhedonia” and “withdrawal” significantly increased, and that between “guilty” and “escape” significantly decreased over time.
Conclusions
This study provides novel insights into the central features of internet addiction and depression during the two stages. Interestingly, “guilty” and “escape,” two functions of the defense mechanism, are identified as bridge symptoms. These two symptoms are suggested to activate the negative feedback loop and further contribute to the comorbidity between internet addiction and depression. Thus, targeting interventions on these internalized symptoms may contribute to alleviating the level of comorbidity among college students.
Keywords: Internet addiction, Depression, Network analysis, Central symptoms, Bridge symptoms, Longitudinal data
The COVID-19 pandemic has ravaged countries worldwide (Belkin et al., 2021; Hau et al., 2020), and has long and far-reaching effects on individuals' physical and mental health (Holman et al., 2020; Tateno et al., 2019), especially on students (Hwang et al., 2020). Due to preventative measures—e.g., quarantine, isolation, lockdown, and social distancing—students have to stay at home and study online (Unger & Meiran, 2020), which may result in a significant increase of internet overuse (Fung et al., 2021), or even internet addiction (IA; Ustun, 2021; Masaeli and Farhadi, 2021; Yu et al., 2021). For instance, several studies have confirmed that students’ internet use problems increased significantly and were exacerbated during the COVID-19 pandemic (Dong et al., 2020).
Internet addiction (IA) refers to excessive internet use that may lead to significant impairment or distress (Laconi et al., 2014; Young, 2004). To date, IA has not been identified as an official mental disorder in the Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (DSM-5), but determined to be a condition warranting more clinical research and studies (Andreassen et al., 2017; Young, 2017). Given the strong correlation between IA and other mental health disorders (e.g., depression; Carli et al., 2013; Ha et al., 2007; Orsal et al., 2013), the dangerous consequences of the comorbidity of IA and other mental health disorders—e.g., depression—for students’ health outcomes have been highlighted. For example, a previous study found that suffering from comorbidity results in a poorer prognosis, greater interference in daily life, and more severe impairment in social function (Albert et al., 2008; Cramer et al., 2010).
In addition, this situation may worsen during pandemic times. For example, the increase of IA may exacerbate pre-existing depression (Steffen et al., 2020). Previous studies found that the prevalence of depression among students increased dramatically during this period (Brailovskaia et al., 2021; Yang et al., 2021). Yang et al. (2021) also reported a high rate of co-occurrence between IA and depression. Considering the ever-increasing number of these problems and their elevated relapse risk (Penner & Paul, 2017), the present study thus aims to investigate the comorbid relationship between IA and depression in Chinese college students during the COVID-19 pandemic.
Network theory is used to explain the co-occurring disorders. According to network theory, a mental disorder is the presentation of interactions between symptoms (Borsboom, 2008; Borsboom & Cramer, 2013). Within a disorder, the onset of some symptoms that have a strong influence in the network will lead to the onset of other symptoms (e.g., symptoms exhibiting the strongest association with other symptoms are known as central symptoms; Borsboom, 2017; Cramer et al., 2016; McNally et al., 2015). Moreover, a symptom in one disorder could also activate symptoms in another one, creating a negative loop between the two disorders and thereby resulting in the onset and maintenance of comorbidity (Cramer et al., 2010). Symptoms linking different disorders are considered bridge symptoms (Kaiser et al., 2021). Thus, identifying the central and bridge symptoms within the symptom network may contribute to understanding the mechanism of comorbidity and to a more cost-effective intervention (Fried & Cramer, 2017; Meuret et al., 2020).
Specifically, the compensatory internet-use theory posits that individuals may use the internet as a maladaptive strategy to cope with real-life problems (Gao et al., 2018). Students may consider the internet as a way to either escape from their negative feelings (e.g., depressive mood; Li, G et al., 2019; Lovibond & Lovibond, 1995) or satisfy a need that is unmet in their offline lives (Caplan, 2002). The continuous positive experience students found in internet applications can lead to addiction-like symptoms (Davis, 2001). Thus, they become reliant on the internet and engage with it more frequently, which may lead to more other IA symptoms and finally form IA. Meanwhile, IA symptoms may activate other affective disorders' symptoms (Seki et al., 2019). According to the social displacement hypothesis, indulgence in social interactions through the internet reduces an individual's time spent on offline communication, which might lead to social withdrawal and an inability to solve problems in real life (Bessiere et al., 2008). These influences increase adolescents' risk of depressive symptoms (Cheng et al., 2015). Along this argument, some symptoms—e.g., “escape” and “withdrawal”—may play important roles in the onset and maintenance of the co-occurrence between depression and IA. However, the underlying mechanisms—e.g., the central and bridge symptoms—behind this co-existence still need further exploration through network analysis.
Furthermore, the development of a symptom network is not static but instead a dynamic process (Forbes et al., 2017; Robinaugh et al., 2020). Measuring the changes between symptoms within two disorders may provide a more in-depth understanding of the mechanisms behind the persistence or resistance of comorbidity (Bringmann et al., 2015). For example, Wang et al. (2020) reported, by using network analysis, the increase of connection between insomnia as a depression symptom and nervousness as a symptom of anxiety, as well as the decrease of connection between “inability to relax” as an anxiety symptom and “guilty” as a depressive symptom throughout the COVID-19 outbreak and the after peak. However, to our knowledge, only one study utilized network analysis to investigate the cross-sectional relationship between depression and IA symptoms among Chinese adolescents in Macau (Cai et al., 2022). The longitudinal feature of symptom networks in depression and IA among college students is still unknown.
Taken together, the co-occurrence of depression and IA has been well documented in previous studies, but few have provided insight into the underlying mechanisms of symptomology or the changes in the network structures between two mental disorders over time. The neglect of symptom changes across time may result in a limited effect of prevention or treatments (Nickerson et al., 2017). Inspired by the network approach, this exploratory study conceptualizes longitudinal comorbidity networks and aims to (a) identify the central symptoms, (b) identify the bridge symptoms, and (c) assess the dynamic changes in interactions between depression and IA symptoms among Chinese college students throughout the COVID-19 pandemic. With this research, we hope to provide useable suggestions for relevant interventions and policies.
1. Methods
1.1. Participants and procedure
From August to November 2020, using a cluster sampling method, 1,162 college students completed a survey via a Chinese online questionnaire at T1 (August 2020). The second wave (T2: November 2020) of data collection included 1,082 participants. Missing complete at random (MCAR) proposed by Little (1988) was utilized to assess whether the missing data were random. It is worth noting that during T1, college students were preparing to return to school, and T2 took place three months later to allow students to settle in.
A total of 852 students who completed the questionnaire during both waves—through the matching of their phone numbers—were included in the final analysis. No missing data needed rejection because all items were required to be answered before submission. The research collected information including demographics, age, gender, family structure, current location, whether the participants had siblings or not, depression, and IA. The sample consisted of 300 (35.21%) males (Mean age = 20.22, SD = 2.07) and 552 (64.79%) females (Mean age = 20.79, SD = 2.15), with ages ranging from 17 to 28.
Participants were recruited from social platforms—e.g., WeChat and Tencent QQ—and received RMB 10 (USD 1.58) as a reward via online payment if they completed all questionnaires. Students who agreed to take part signed an electronic informed consent form before filling out the questionnaires. The research ethics board at Shenzhen University approved the data collection (grant number: 2020005).
1.2. Measures
The Patient Health Questionnaire-9 (PHQ-9). Depression symptoms were assessed using the Patient Health Questionnaire-9 items (PHQ-9; Diez-Quevedo et al., 2001). Responses were made on a four-point Likert-type scale with each item scored from 0 (not at all) to 3 (nearly every day). Participants were required to report their feelings over the past two weeks (e.g., “Little interest or pleasure in doing things,” “Feeling down, depressed, or hopeless”). The sum total score ranged from 0 to 27, and higher scores denoted a more severe level of depression. A total score of >10 indicated the risk of depression. The Chinese version of the PHQ-9 has been proven to have good validity and reliability (Sun et al., 2020). The Cronbach's alpha value was 0.89 at T1 and 0.88 at T2.
The Internet Addiction Test-10 (IA-10). IA symptoms were assessed using the 10-item Internet Addiction Test, which was translated into Chinese by Shek (Shek et al., 2008). This scale was created using a two-point Likert-type format (0 = no, 1 = yes). Participants needed to report whether they mentioned symptoms over one year (e.g., “Do you find there is a diminished effect with continued use of the same time spent on the internet?“). Total scores ranged from 0 to 10, and a total score above 4 was considered indicative of IA. The Chinese version of the IA-10 has been proven to have good psychometric properties among Chinese college students. In this study, Cronbach's alpha was .82 at T1 and 0.82 at T2.
1.3. Statistical analysis
The mean scores and standard deviation (SD) of depression symptoms and IA symptoms in the two waves were calculated using IBM SPSS Statistics (Version 25). The chi-squared test was then utilized to examine the significance of the difference in the prevalence of depression, IA, and comorbidity between T1 and T2, with the significance level set at 0.05. The RStudio program (Version 4.1.2) was used to conduct network analysis. Four domains were included: network estimation, centrality estimation, network accuracy and stability estimation, and network comparison.
Network estimation. The mixed graphical model (MGM), proposed by van Borkulo et al. (2015), was utilized to estimate the network structure. This estimation approach was appropriated for both non-binary (depression symptoms) and binary (IA symptoms) data. The R package “mgm” was applied to complete this estimating procedure (Haslbeck & Waldorp, 2015; McNally et al., 2015). In the network, symptoms were visualized as nodes, and interconnections between symptoms were denoted as edges between nodes. The strength of the association between each two symptoms was computed using the generalized linear regression model (Isvoranu & Epskamp, 2021). According to recommendations made by Burger et al. (2022), raw data were used for analysis, and we set “lambdaSel = EBIC” for model selection. The regularization method estimated edge weights through penalizing maximum likelihood estimation (Lin et al., 2020). The penalty parameter γ was set to 0.25 in the MGM, which was beneficial for obtaining a sparse model. The algorithm of the Least Absolute Shrinkage and Selection Operate (LASSO) contributed to confirming the best connection between individual symptoms (Friedman et al., 2008). Small correlations were put to zero, thus leading to a sparse network. In addition, the Extend Bayesian Information Criterion (EBIC) was applied for model optimization (Chen & Chen, 2008). The hypertuning-parameter λ of EBIC was set to 0.5 in MGM, as recommended. The layout of the network structure uses the Fruchterman-Reingold algorithm (Fruchterman & Reingold, 1991). The stronger the symptoms connected, the closer their positions were in the network. Of note, the different networks were visualized in the same layout with the function “AverageLayout” in the R package “qgraph” (Epskamp et al., 2012).
Centrality estimation. To quantify how central a node was in the network, we computed centrality indices to measure connectivity of nodes with the function “centralityPlot” in the R package “qgraph”. Four centrality metrics were commonly used: strength, expected influence, betweenness, and closeness. Of note, strength and expected influence described directed connectivity, and betweenness and closeness indicated indirect connectivity (Opsahl et al., 2010). Strength was suggested as a more reliable metric to measure the central role if there was no negative correlation in the network. It is the sum of the absolute edge weights connected to a node (Richetin et al., 2017). In addition, considering that our network consisted of two symptom communities—depression and IA—bridge strength was also computed to quantify how well symptoms in one disorder connected to those in other disorders (Jones et al., 2021). The activation of symptoms with higher bridge strength resulted in comorbidity.
Accuracy and stability estimation. Considering that the estimated network model was subject to sampling variation, checks for the accuracy and stability of edge weights and centrality indices were necessary (Borsboom et al., 2018). The R package “bootnet” was utilized to perform this analysis using the bootstrapping method (Borsboom et al., 2018; Epskamp et al., 2018). By re-sampling the data with replacement, the parameter estimates obtained from these re-sampled samples were used to construct 95% CIs (Hastie et al., 2015). The non-parametric bootstrap was applied to evaluate the accuracy of edges. Narrower constructed CIs indicated a trustworthy network (Marchetti, 2019). However, considering that centrality indices were mostly computed with absolute edge weights, we cannot rely on the CIs to assess the stability of centrality (Epskamp et al., 2018). Epskamp et al. (2018) introduced the case-drop bootstrap to inspect how accurately centrality indices were estimated. This procedure examined stability by checking the correlations of estimated centrality in the original and subset samples. If centrality indices—e.g., strength—did not change significantly in the minimum sub-sample (excluding 70% of data in the original dataset randomly), they were considered to be stable. The correlation stability (CS) coefficients were computed to quantify stability. Epskamp et al. (2018) recommended that CS coefficients should exceed 0.5 but be no less than 0.25. Finally, the bootstrapped differences test could also be assessed in the non-parametric bootstrap. The CI, which included the difference between two edges (e.g., the EW of A - B minus the EW of B - C; or two centrality metrics, and the value of strength of node A minus node B), were checked—whether zero was included—to determine if one EW or centrality was different from another. All bootstrapping processes were conducted 2,000 times.
Network comparison. The network comparison test in the R package “NetworkComparisonTest” (NCT) was used to examine the network structure difference between the two estimated models, using a permutation test (van Borkulo et al., 2022). The invariance of the global strength and edge weight was computed to describe differences in global and local characteristics. Global strength was the sum of all edges (Opsahl et al., 2010). In the symptom network, global strength could reveal the vulnerability of the disorder. The higher value of global strength indicated stronger connectivity among symptoms (van de Geer et al., 2014). Local variance referred to differences between individual edge weights or centrality indices. Of note, the current study also compared the network structure between male and female groups at the same time.
2. Results
2.1. Descriptive analysis of depression and IA symptoms
The chi-squared test and the independent t-test were applied to examine the differences between participants who finished both questionnaires and those who only completed one. The results showed no differences with respect to sex χ2(1)¼ = 1.94, p = 0.08; age t (848)¼ = 0.92, p = 0.12, depression status t (848)¼ = 0.89, p = 0.10, or IA status χ2 (1)¼ = 0.93, p = 0.13, indicating that there were no significant differences between the missing and complete data. Based on the chi-squared test results, the prevalence of depression symptoms was not found to have a significant difference between T1 and T2 (T1: 22.8%, T2: 22.0%, χ2 = 2.22, p = 0.10). IA symptoms showed a significant change from T1 to T2 (T1: 54.1%, T2: 44.5%, χ2 = 2.22, p < 0.001), and participants at T2 were less likely to be addicted to the internet than at T1. The co-occurrence between depression and IA did not change significantly (T1: 18.7%, T2: 14.9%, χ2 = 1.71, p = 0.19). The mean scores and standard deviations of depression and IA symptoms are shown in Table 1 . The content, abbreviations, mean scores, and standard deviations of each symptom are also shown in Table A1.
Table 1.
Descriptive statistics of depression and internet addiction.
| T1 | T2 | |||
|---|---|---|---|---|
| M | SD | M | SD | |
| Depression | 7.11 | 4.89 | 6.35 | 4.48 |
| Internet Addiction | 4.11 | 2.77 | 3.43 | 2.81 |
Note: M = Mean score, SD = Standard Deviation, T1 = 2020.8, T2 = 2020.11, Total sample = 852.
Table A1.
Symptoms' content, abbreviation, and M±SD of PHQ-9 and IA-10.
| Symptoms' content | Abbreviation | T1 | T2 | ||
|---|---|---|---|---|---|
| Depression symptoms (PHQ-9) | M | SD | M | SD | |
| PHQ1: Little interest or pleasure in doing things. | Anhedonia | 2.06 | 0.93 | 0.75 | 0.66 |
| PHQ2: Feeling down, depressed, or hopeless. | Sad Mood | 1.96 | 0.96 | 0.87 | 0.68 |
| PHQ3: Trouble falling or staying asleep, or sleeping too much | Sleep | 2.08 | 0.75 | 0.78 | 0.80 |
| PHQ4: Feeling tired or having little energy. | Energy | 1.77 | 0.81 | 0.79 | 0.77 |
| PHQ5: Poor appetite or overeating. | Appetite | 1.92 | 0.20 | 0.86 | 0.50 |
| PHQ6: Feeling bad about yourself, or that you are a failure or have let yourself or your family down. | Guilty | 1.76 | 0.66 | 0.83 | 0.75 |
| PHQ7: Trouble concentrating on things, such as reading the newspaper or watching television. | Concentration | 1.47 | 0.83 | 0.72 | 0.80 |
| PHQ8: Moving or speaking so slowly that other people can notice. Or the opposite: being so fidgety or restless that you have been moving around a lot more than usual. | Motor | 1.80 | 0.79 | 0.72 | 0.64 |
| PHQ9: Thoughts that you would be better off dead, or of hurting yourself in some way. | Suicide | 1.24 | 0.46 | 0.58 | 0.68 |
| Internet Addiction symptoms (IA-10) | |||||
| IA1: Do you feel preoccupied with the internet (thinking about previous online activity or anticipating the next online session)? | Salience | 0.47 | 0.37 | 0.52 | 0.48 |
| IA2: Do you feel the need to use the internet with increasing amounts of time in order to achieve satisfaction? | Satisfaction | 0.71 | 0.47 | 0.48 | 0.50 |
| IA3: Have you repeatedly made unsuccessful efforts to control, cut back, or stop internet use? | Relapse | 0.36 | 0.47 | 0.50 | 0.50 |
| IA4: Do you feel restless, moody, depressed, or irritable when attempting to cut down or stop internet use? | Irritable | 0.30 | 0.23 | 0.48 | 0.42 |
| IA5: Do you stay online longer than originally intended? | Overuse | 0.27 | 0.64 | 0.47 | 0.48 |
| IA6: Have you jeopardized or risked the loss of a significant relationship, job, or educational or career opportunity because of the internet? | Conflict | 0.42 | 0.27 | 0.52 | 0.45 |
| IA7: Have you lied to family members, therapists, or others to conceal the extent of your involvement with the internet? | Lie | 0.29 | 0.26 | 0.48 | 0.44 |
| IA8: Do you use the internet as a way of escaping from problems or of relieving a dysphoric mood (e.g., feelings of helplessness, guilt, anxiety, or depression)? | Escape | 0.15 | 0.40 | 0.38 | 0.49 |
| IA9: Do you feel unsettled or irritable when you cannot be on the internet? | Withdrawal | 0.54 | 0.24 | 0.52 | 0.43 |
| IA10: Do you still use the internet even if it costs a lot of money? | Money Problem | 0.51 | 0.15 | 0.52 | 0.36 |
Note: M = Mean, SD = Standard Deviation, T1 = 2020.8, T2 = 2020.11, Total sample = 852.
2.2. Comorbidity network of depression and IA
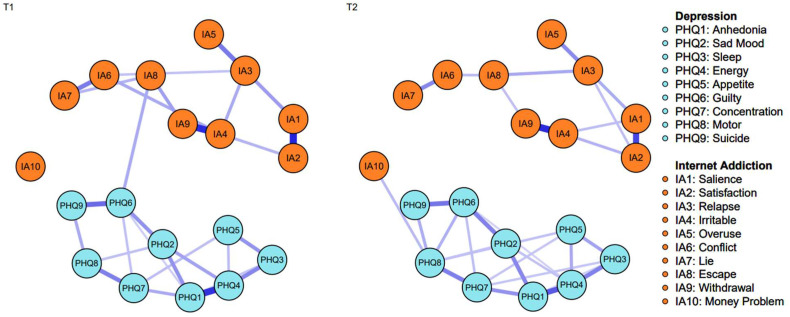
Network estimation. The symptom networks are presented in Fig. 1 . Among the 171 edges, 141 were removed in the T1 network, and 138 edges were shrunk to zero in the T2 network. The sparsity of the network was 0.16 and 0.19 at T1 and T2, respectively. The edge weights between “anhedonia” and “energy,” and “salience” and “satisfaction” were the highest in both networks. Moreover, the edge weight between depression symptom “guilty” and IA symptom “escape” decreased significantly from T1 to T2. The specific values of the edge weights are shown in Table A2.
Fig. 1.
The comorbidity network structure of internet addiction and depression (N = 852). Blue nodes indicate depression symptoms, and orange nodes indicate IA symptoms. Thicker edges between symptoms denote stronger associations. All edges denote positive interconnections; T1 = 2020.8, T2 = 2020.11.
Table A2.
Values of edge weights between each of the two symptoms of depression and IA.
| T1 | |||||||||||||||||||
| PHQ1 | PHQ2 | PHQ3 | PHQ4 | PHQ5 | PHQ6 | PHQ7 | PHQ8 | PHQ9 | IA1 | IA2 | IA3 | IA4 | IA5 | IA6 | IA7 | IA8 | IA9 | IA10 | |
| PHQ1 | 1 | ||||||||||||||||||
| PHQ2 | 0.19 | 1 | |||||||||||||||||
| PHQ3 | 0.10 | 0.00 | 1 | ||||||||||||||||
| PHQ4 | 0.36 | 0.16 | 0.22 | 1 | |||||||||||||||
| PHQ5 | 0.00 | 0.00 | 0.17 | 0.11 | 1 | ||||||||||||||
| PHQ6 | 0.08 | 0.20 | 0.00 | 0.06 | 0.09 | 1 | |||||||||||||
| PHQ7 | 0.16 | 0.05 | 0.00 | 0.05 | 0.10 | 0.11 | 1 | ||||||||||||
| PHQ8 | 0.00 | 0.10 | 0.00 | 0.00 | 0.08 | 0.08 | 0.21 | 1 | |||||||||||
| PHQ9 | 0.00 | 0.04 | 0.00 | 0.00 | 0.00 | 0.25 | 0.00 | 0.13 | 1 | ||||||||||
| IA1 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 1 | |||||||||
| IA2 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.35 | 1 | ||||||||
| IA3 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.15 | 0.06 | 1 | |||||||
| IA4 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.12 | 0.14 | 1 | ||||||
| IA5 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.05 | 0.00 | 0.00 | 0.00 | 0.00 | 0.23 | 0.00 | 1 | |||||
| IA6 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.04 | 0.00 | 0.00 | 0.00 | 0.00 | 0.11 | 0.15 | 0.07 | 1 | ||||
| IA7 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.07 | 0.00 | 0.00 | 0.22 | 1 | |||
| IA8 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.14 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.02 | 0.06 | 0.05 | 0.06 | 0.12 | 1 | ||
| IA9 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.38 | 0.00 | 0.00 | 0.00 | 0.15 | 1 | |
| IA10 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.03 | 0.08 | 0.00 | 1 |
| T2 | |||||||||||||||||||
| PHQ1 | PHQ2 | PHQ3 | PHQ4 | PHQ5 | PHQ6 | PHQ7 | PHQ8 | PHQ9 | IA1 | IA2 | IA3 | IA4 | IA5 | IA6 | IA7 | IA8 | IA9 | IA10 | |
| PHQ1 | 1 | ||||||||||||||||||
| PHQ2 | 0.21 | 1 | |||||||||||||||||
| PHQ3 | 0.08 | 0.07 | 1 | ||||||||||||||||
| PHQ4 | 0.35 | 0.10 | 0.21 | 1 | |||||||||||||||
| PHQ5 | 0.00 | 0.00 | 0.16 | 0.14 | 1 | ||||||||||||||
| PHQ6 | 0.06 | 0.22 | 0.00 | 0.06 | 0.00 | 1 | |||||||||||||
| PHQ7 | 0.21 | 0.04 | 0.08 | 0.04 | 0.09 | 0.12 | 1 | ||||||||||||
| PHQ8 | 0.00 | 0.09 | 0.00 | 0.00 | 0.11 | 0.14 | 0.23 | 1 | |||||||||||
| PHQ9 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.22 | 0.00 | 0.14 | 1 | ||||||||||
| IA1 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 1 | |||||||||
| IA2 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.31 | 1 | ||||||||
| IA3 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.03 | 0.00 | 0.00 | 0.14 | 0.10 | 1 | |||||||
| IA4 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.04 | 0.00 | 0.00 | 0.10 | 0.11 | 0.08 | 1 | ||||||
| IA5 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.05 | 0.00 | 0.00 | 0.00 | 0.06 | 0.21 | 0.00 | 1 | |||||
| IA6 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.05 | 0.00 | 0.08 | 0.00 | 0.00 | 1 | ||||
| IA7 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.05 | 0.00 | 0.00 | 0.09 | 0.00 | 0.09 | 0.00 | 1 | |||
| IA8 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.14 | 0.00 | 0.04 | 0.21 | 0.05 | 1 | ||
| IA9 | 0.06 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.06 | 0.00 | 0.04 | 0.00 | 0.06 | 0.31 | 0.10 | 0.11 | 0.08 | 0.11 | 1 | |
| IA10 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.10 | 0.00 | 0.04 | 0.00 | 0.00 | 0.00 | 0.00 | 0.04 | 0.06 | 0.10 | 0.09 | 1 |
Note: T1 = 2020.8, T2 = 2020.11, Total sample = 852. PHQ1: Anhedonia; PHQ2: Sad Mood; PHQ3: Sleep; PHQ4: Energy; PHQ5: Appetite; PHQ6: Guilty; PHQ7: Concentration; PHQ8: Motor; PHQ9: Suicide; IA1: Salience; IA2: Satisfaction; IA3: Relapse; IA4: Irritable; IA5: Overuse; IA6: Conflict; IA7: Lie; IA8: Escape; IA9: Withdrawal; IA10: Money Problem.
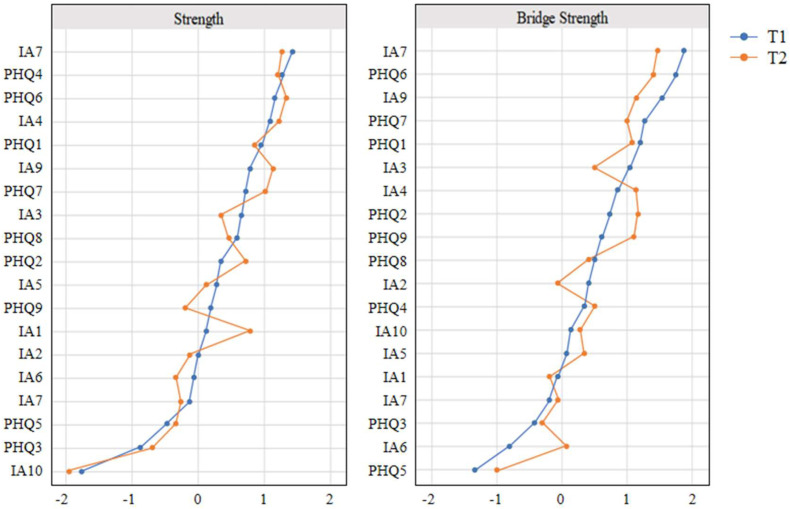
Centrality estimations. The plot of the strength and bridge strength of depression and IA symptoms is shown in Fig. 2 . In order to compare centrality more intuitively, we ranked symptoms in order of value in the plot. Within all symptoms, depression symptoms “energy” (strengthT1/T2 = 1.19/1.23), “guilty” (strengthT1/T2 = 1.10/1.26), and IA symptoms “escape” (T1 strengthT1/T2 = 1.22/1.16) and “irritable” (T1 strengthT1/T2 = 1.02/1.08) had the highest strength at T1. According to the centrality difference test results, the strengths of these four symptoms were significantly higher than other symptoms. At T2, the strengths of “energy,” “guilty,” “escape,” and “irritable” were still highest ones, indicating that their influential roles were stable across time. Of note, “money problems,” “sleep,” and “appetite” had the lowest strengths. The results of the strength difference test are shown in Fig. A1.
Fig. 2.
Strength and bridge strength of individual symptoms of IA and depression (N = 852). Blue value-nodes denote strength and bridge strength at T1 (2020.8), and orange value-nodes denote strength and bridge strength at T2 (2020.11). PHQ1: Anhedonia; PHQ2: Sad Mood; PHQ3: Sleep; PHQ4: Energy; PHQ5: Appetite; PHQ6: Guilty; PHQ7: Concentration; PHQ8: Motor; PHQ9: Suicide; IA1: Salience; IA2: Satisfaction; IA3: Relapse; IA4: Irritable; IA5: Overuse; IA6: Conflict; IA7: Lie; IA8: Escape; IA9: Withdrawal; IA10: Money Problem.
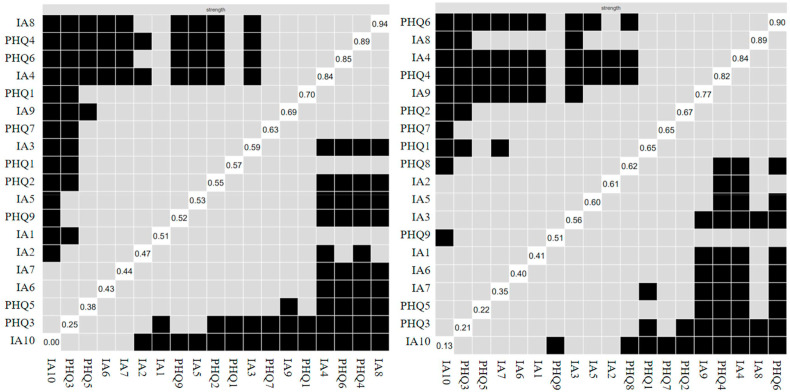
Fig. A1.
The difference test results of strength using the non-parametric bootstrapping method (N = 852). The black grid indicates a significant difference between the two corresponding edge weights, and the gray grid indicates no significant difference. The left two are the results of the strength and bridge strength difference test at T1, and the right ones are at T2. PHQ1: Anhedonia; PHQ2: Sad Mood; PHQ3: Sleep; PHQ4: Energy; PHQ5: Appetite; PHQ6: Guilty; PHQ7: Concentration; PHQ8: Motor; PHQ9: Suicide; IA1: Salience; IA2: Satisfaction; IA3: Relapse; IA4: Irritable; IA5: Overuse; IA6: Conflict; IA7: Lie; IA8: Escape; IA9: Withdrawal; IA10: Money Problem.
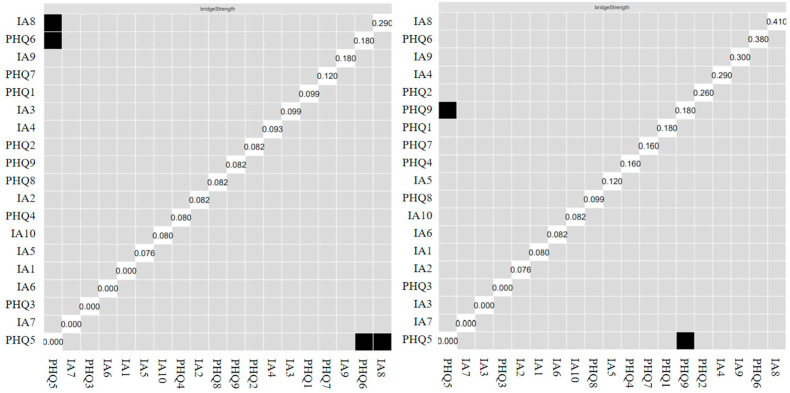
Centrality strength emphasizes the central effects of nodes in the entire comorbidity network, and interventions targeting such central symptoms contribute to reducing the overall severity of comorbidity. Bridge centrality is concerned with symptoms that link different disorders, and measures of bridge symptoms are beneficial for measuring the bridge effect. In this study, depression symptom “guilty” (bridge strengthT1/T2 = 1.87/1.24) and IA symptom “escape” (bridge strengthT1/T2 = 1.97/1.26) had the highest bridge strength at both T1 and T2. According to the results of the difference test shown in Fig. A2, most symptoms had no differences in bridge strength. Therefore, “guilty” and “escape,” with the strongest centrality of bridge strength, were identified as bridge symptoms, and were the only associated symptoms between depression and IA. The raw values of the centrality and bridge centrality indices are shown in Table A3 and Table A4.
Fig. A2.
The difference test results of bridge strength using the non-parametric bootstrapping method (N = 852). The black grid indicates a significant difference between the two corresponding edge weights, and the gray grid indicates no significant difference. The left two are the results of the strength and bridge strength difference test at T1, and the right ones are at T2. PHQ1: Anhedonia; PHQ2: Sad Mood; PHQ3: Sleep; PHQ4: Energy; PHQ5: Appetite; PHQ6: Guilty; PHQ7: Concentration; PHQ8: Motor; PHQ9: Suicide; IA1: Salience; IA2: Satisfaction; IA3: Relapse; IA4: Irritable; IA5: Overuse; IA6: Conflict; IA7: Lie; IA8: Escape; IA9: Withdrawal; IA10: Money Problem.
Table A3.
The raw values of strength, closeness, and betweenness.
| T1 | T2 | |||||
|---|---|---|---|---|---|---|
| strength | closeness | betweenness | strength | closeness | betweenness | |
| PHQ1 | 0.8924 | 0.0029 | 9 | 0.9157 | 0.0031 | 32 |
| PHQ2 | 0.6452 | 0.0031 | 28 | 0.7251 | 0.0027 | 6 |
| PHQ3 | 0.2847 | 0.0023 | 0 | 0.2963 | 0.0024 | 0 |
| PHQ4 | 0.9850 | 0.0027 | 17 | 0.8168 | 0.0028 | 11 |
| PHQ5 | 0.3586 | 0.0026 | 1 | 0.2895 | 0.0024 | 4 |
| PHQ6 | 0.9638 | 0.0037 | 65 | 0.8875 | 0.0027 | 6 |
| PHQ7 | 0.7614 | 0.0031 | 17 | 0.9310 | 0.0031 | 23 |
| PHQ8 | 0.7048 | 0.0026 | 1 | 0.7064 | 0.0033 | 39 |
| PHQ9 | 0.5261 | 0.0030 | 7 | 0.4513 | 0.0026 | 4 |
| IA1 | 0.5121 | 0.0022 | 3 | 0.6713 | 0.0023 | 0 |
| IA2 | 0.5022 | 0.0023 | 10 | 0.6499 | 0.0023 | 0 |
| IA3 | 0.7677 | 0.0027 | 15 | 0.4223 | 0.0026 | 11 |
| IA4 | 0.8992 | 0.0032 | 35 | 0.7772 | 0.0030 | 23 |
| IA5 | 0.4058 | 0.0025 | 10 | 0.3401 | 0.0026 | 10 |
| IA6 | 0.4495 | 0.0028 | 3 | 0.3627 | 0.0024 | 2 |
| IA7 | 0.4455 | 0.0029 | 8 | 0.3362 | 0.0027 | 14 |
| IA8 | 1.0034 | 0.0038 | 69 | 0.8336 | 0.0025 | 2 |
| IA9 | 0.8338 | 0.0033 | 38 | 0.7550 | 0.0032 | 40 |
| IA10 | 0.1107 | 0.0021 | 0 | 0.1908 | 0.0031 | 12 |
Note: Total sample = 852. PHQ1: Anhedonia; PHQ2: Sad Mood; PHQ3: Sleep; PHQ4: Energy; PHQ5: Appetite; PHQ6: Guilty; PHQ7: Concentration; PHQ8: Motor; PHQ9: Suicide; IA1: Salience; IA2: Satisfaction; IA3: Relapse; IA4: Irritable; IA5: Overuse; IA6: Conflict; IA7: Lie; IA8: Escape; IA9: Withdrawal; IA10: Money Problem.
Table A4.
The raw values of bridge strength, bridge betweenness, and bridge closeness.
| T1 | T2 | |||||
|---|---|---|---|---|---|---|
| bridge strength | bridge closeness | bridge betweenness | bridge strength | bridge closeness | bridge betweenness | |
| PHQ1 | 0.3629 | 0.0561 | 15 | 0.2884 | 0.0639 | 25 |
| PHQ2 | 0.3158 | 0.0577 | 12 | 0.3417 | 0.0587 | 11 |
| PHQ3 | 0.0593 | 0.0420 | 0 | 0.0890 | 0.0660 | 0 |
| PHQ4 | 0.2607 | 0.0508 | 10 | 0.2754 | 0.0563 | 13 |
| PHQ5 | 0.0408 | 0.0460 | 0 | 0.0629 | 0.0467 | 1 |
| PHQ6 | 0.4069 | 0.0785 | 28 | 0.3457 | 0.0568 | 5 |
| PHQ7 | 0.3803 | 0.0735 | 35 | 0.2701 | 0.0733 | 10 |
| PHQ8 | 0.2818 | 0.0642 | 3 | 0.2245 | 0.0720 | 10 |
| PHQ9 | 0.3099 | 0.0684 | 8 | 0.3264 | 0.0651 | 11 |
| IA1 | 0.1371 | 0.0489 | 6 | 0.1250 | 0.0463 | 2 |
| IA2 | 0.2577 | 0.0475 | 2 | 0.2699 | 0.0469 | 4 |
| IA3 | 0.3494 | 0.0599 | 20 | 0.3296 | 0.0572 | 4 |
| IA4 | 0.3232 | 0.0549 | 8 | 0.3430 | 0.0586 | 12 |
| IA5 | 0.2343 | 0.0693 | 35 | 0.1911 | 0.0668 | 12 |
| IA6 | 0.1590 | 0.0550 | 2 | 0.2667 | 0.0599 | 2 |
| IA7 | 0.0916 | 0.0539 | 3 | 0.0888 | 0.0677 | 17 |
| IA8 | 0.4331 | 0.0704 | 29 | 0.3871 | 0.0547 | 1 |
| IA9 | 0.3855 | 0.0565 | 10 | 0.2973 | 0.0641 | 18 |
| IA10 | 0.2574 | 0.0670 | 1 | 0.1557 | 0.0751 | 13 |
Note: Total sample = 852. PHQ1: Anhedonia; PHQ2: Sad Mood; PHQ3: Sleep; PHQ4: Energy; PHQ5: Appetite; PHQ6: Guilty; PHQ7: Concentration; PHQ8: Motor; PHQ9: Suicide; IA1: Salience; IA2: Satisfaction; IA3: Relapse; IA4: Irritable; IA5: Overuse; IA6: Conflict; IA7: Lie; IA8: Escape; IA9: Withdrawal; IA10: Money Problem.
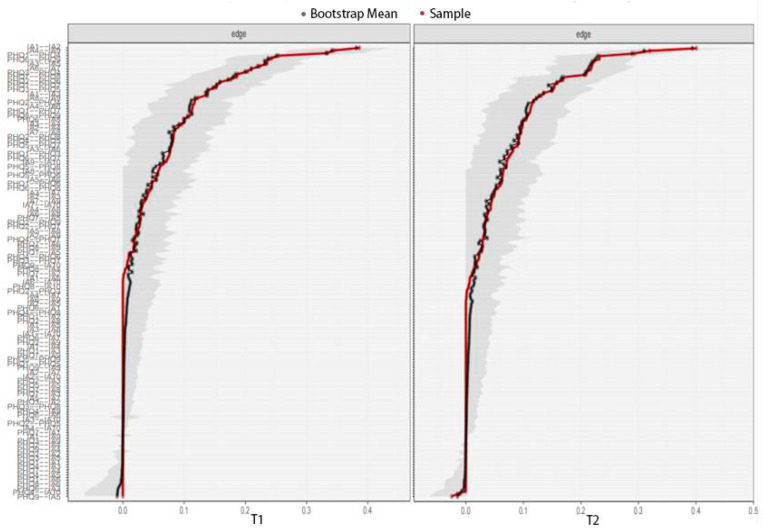
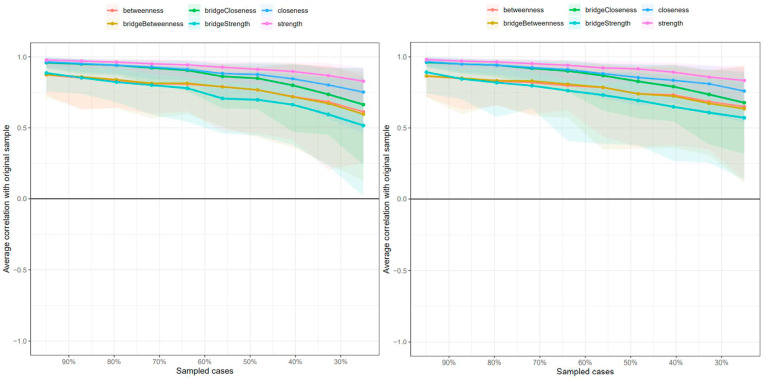
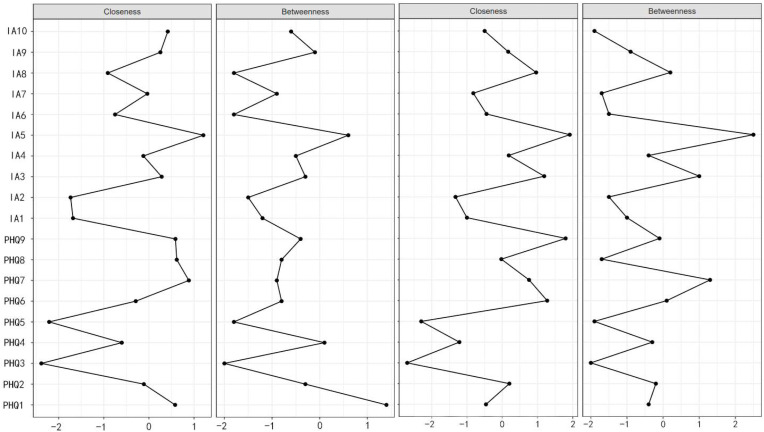
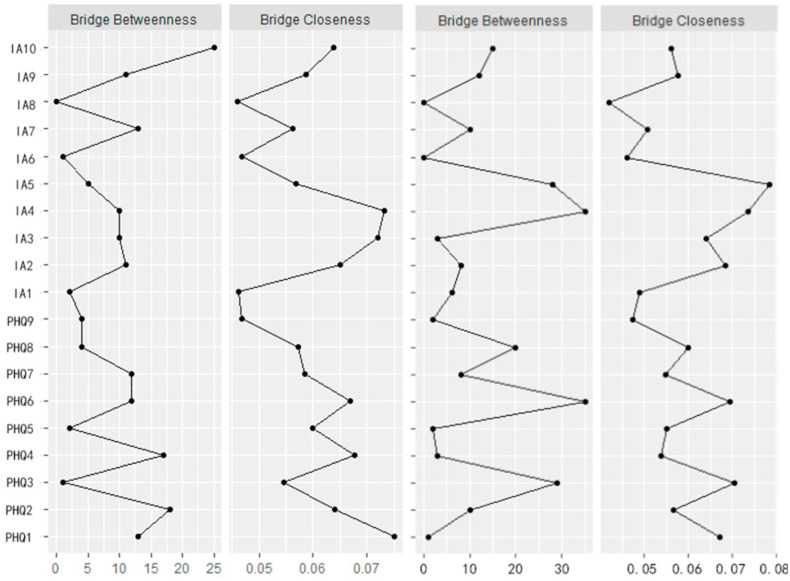
Accuracy and stability estimation. The stability and accuracy of the network structure are preferable in this study. Fig. A3 shows the estimated CIs of edge weights by bootstrapping. The relatively narrow CIs indicate acceptable accuracy. Fig. A4 shows the results of the centrality stability estimating procedure. The CS coefficients of strength and bridge strength are 0.75 and 0.68 at T1, and 0.75 and 0.72 at T2, respectively, indicating that they are reliable for measuring the characteristics of network nodes. In addition, the CS coefficients of closeness, betweenness, bridge closeness, and bridge betweenness are 0.47, 0.28, 0.26, and 0.28, respectively, and are plotted in Fig. A5 and Fig. A6.
Fig. A3.
Accuracy estimations of all edge weights using the non-parametric bootstrapping method (N = 852). Narrower CIs indicate reliable accuracy. The left one is the result of the accuracy test at T1, and the right one is at T2. PHQ1: Anhedonia; PHQ2: Sad Mood; PHQ3: Sleep; PHQ4: Energy; PHQ5: Appetite; PHQ6: Guilty; PHQ7: Concentration; PHQ8: Motor; PHQ9: Suicide; IA1: Salience; IA2: Satisfaction; IA3: Relapse; IA4: Irritable; IA5: Overuse; IA6: Conflict; IA7: Lie; IA8: Escape; IA9: Withdrawal; IA10: Money Problem.
Fig. A4.
Stability estimations of centrality indices using the case-drop bootstrapping method (N = 852). The left one is the result of the stability test at T1, and the right one is at T2.
Fig. A5.
The plot of centrality indices betweenness and closeness of every symptom (N = 852). The left two are betweenness and closeness at T1, and the right two are at T2.
Fig. A6.
The plot of bridge betweenness and bridge closeness of every symptom (N = 852). The left two are betweenness and closeness at T1, and the right two are at T2.
Network Comparison. We compared the global and local structures between networks at T1 and T2. The results showed no global difference (global strengthT1/T2 = 6.87/6.45, p = 0.42). However, there were significant differences between the edges. For example, the edge weight of “guilty” and “escape” decreased (edge weight difference = −0.12, p < 0.05), which could be concluded intuitively from cross-section networks. Moreover, the correlations of “escape” and “irritable,” “energy” and “anhedonia,” and “energy” and “sad mood” also decreased. Of note, the interconnection between “withdrawal” and “guilty” increased significantly (edge weight difference = 0.14, p < 0.01). Also, no significant differences were found in the network models between male and female groups at both T1 (global strengthmale/female = 6.90/6.88, p = 0.72) and T2 (global strengthmale/female = 6.56/6.51, p = 0.66).
3. Discussion
The novelty of the current study was the investigation of the comorbid relationship between IA and depression over time among Chinese college students during the COVID-19 pandemic, applying network analysis. Using longitudinal data, we identified central symptoms (e.g., depressive symptoms “energy” and “guilty”; IA symptoms “irritable” and “escape”) and bridge symptoms (e.g., “guilty” and “escape”) in the comorbidity network over time. We also found that the correlation between “guilty” and “escape” decreased, while the connection between “motor” and “withdrawal” increased from T1 to T2 within the network.
“Energy” and “guilty” were identified as central among the depression symptoms in the co-occurrence network. Similarly, a systematic review found that “energy” had the highest strength in most networks, and “guilty” was frequently considered a top-three central symptom (Malgaroli et al., 2021; Wasil et al., 2021). However, these two symptoms were not the core depressive symptoms; rather, “anhedonia” and “sad mood” were, as identified in the DSM-5 (APA, 2013; Billones et al., 2020). Given the lack of exercise and face-to-face social activities, “energy” as a central symptom for depression during the pandemic seems reasonable. Ye et al. (2020) also confirmed our findings by showing that loss of energy, or fatigue, is common in stressful situations like the COVID-19 period. In addition to causing impairment in physical functioning, the presence of low energy can also worsen an individual's moods (Brown & Schutte, 2006). For example, prior studies reported that “feeling tired or having little energy” could worsen depression by causing more negative emotions (Konstantopoulou & Raikou, 2020; Li, G et al., 2019). Meanwhile, the central role of “guilty” as a depressive symptom within the network might be explained by the fact that Chinese students are typically prone to internalizing the high expectations that parents and teachers have of them (Leung et al., 2011). Failing to achieve expected goals can easily bring about feelings of guilt or worthlessness (Wasil et al., 2021). Long-term or severe guilt can lead to self-blame or criticism, and further influence how they feel, think, and act, which consequently activates other depression symptoms (Wakefield & Schmitz, 2016).
Regarding IA, “escape” and “irritable” were the central symptoms within the co-occurrence network. This contributes to the understanding of this disease, especially given the controversial diagnosis of IA to date. A possible explanation for the core role of “escape” might be that internet addiction is a convenient way for students to escape from problems or to relieve a dysphoric mood—e.g., irritable feelings—during stressful times like the COVID-19 period (Berezovskaya et al., 2019). However, excessive internet use could deteriorate their normal social function and ability to focus on the present (De Leo & Wulfert, 2013). This might reinforce avoidance behaviors like hiding behind the internet (Turan et al., 2020). Meanwhile, students’ online internet use reduced significantly when they returned to school, and the absence of the previous delight offered by the internet made them feel irritable (Li, Q et al., 2019). These negative feelings may compel them to return to the internet until enough satisfaction is obtained (Longstreet et al., 2019). This could also explain why the edge weights between “irritable” and “satisfaction” are relatively strong.
More importantly, we found that the bridge symptoms were “escape” and “guilty” in the comorbidity network. Escapism or avoidance were two of the most common defense systems among individuals with depression (Chou & Hsiao, 2000; Kroska et al., 2017). In line with the compensatory internet-use theory, when suffering from negative feelings, individuals may be familiar with using avoidance strategies instead of seeking help from others or solving the problem (Quigley et al., 2017). For students, avoidance of real life may lead to harsh self-criticism, which aggravates their negative feelings (e.g., guilt; Guo et al., 2020). These overwhelming negative emotions may compel them to use the internet more frequently (Brailovskaia et al., 2020; Feng et al., 2019). In turn, the internet may provide a cover of anonymity to express emotions safely and help alleviate depression-related moods temporarily (Tichon & Shapiro, 2003). Therefore, a vicious circle of “negative moods experience - escape - re-experience - re-escape” forms, which reveals how depression and IA interact and finally develop into comorbidity.
As for the changes in the co-occurring networks, we found that the correlation between bridge symptoms—e.g., “escape” and “guilty”—decreased significantly over time. This may be due to the fact that students had already come back to school for a few months. The face-to-face teaching approach limited their internet use time and thereby alleviated the connection between “escape” and “guilty” (Daumiller et al., 2021). It is worth noting that the prevalence of co-occurrence between IA and depression decreased over time. These findings indicated that targeting “escape” and “guilty” as a priority in interventions may effectively remit the comorbidity between IA and depression, but this still needs further exploration. Interestingly, we also found an increased correlation between “withdrawal” as an IA symptom and “anhedonia” as a depression symptom within the co-occurring network. This may be due to the fact that, being separated from the internet, students may have lost the source of pleasure and had withdrawal reactions (Kato et al., 2020). Such withdrawal symptoms further forced students to spend their energy and attention on the internet (Chun et al., 2018), depriving them of interest in participating in other activities.
Taken together, the present study underscores the core role of escape behavior and feelings of guilt within the co-occurrence between IA and depression. Designing interventions that target college students' escape-style-coping behaviors by using the internet together with their feelings of guilt may help attenuate the maintenance of two mental disorders. For example, self-compassion strategies could be applied to treat feelings of guilt (Neff, 2011). Meanwhile, previous studies found that poor emotional regulation is a main cause for an individual's escaping behaviors (Tsai et al., 2020). Thus, future intervention programs may also consider improving emotion regulation strategies among students in addition to focusing on alleviating their guilty feelings.
3.1. Limitations
There are several limitations to this study that should be noted. First, although we used longitudinal data to complete the network analysis, directional analysis was not applied to investigate which symptoms influenced others. This approach needs to be utilized to explore dynamic changes in the future. Second, the surveys were conducted online, and self-reporting was adopted. Therefore, self-bias may have an influence on the accuracy of the results. Measurement methods that look at different aspects, such as scales evaluated by others or interviews, should be considered for referencing in future research. Third, for some Chinese youth, depression can have some externalized manifestations, such as aggression and bad socialization (Zhang et al., 2020), rather than just a sad mood or feelings of worthlessness. Thus, in future research, these areas could be considered for expansion. Finally, network analysis is still a new approach for revealing connections between different disorders or symptoms. There are many arguments and challenges among academic circles (Forbes et al., 2017; Fried & Cramer, 2017), and we therefore need to be cautious when generalizing results.
4. Conclusion
To our knowledge, this study is the first to investigate network structure and its dynamic changes between IA and depression in Chinese college students. The results revealed that the IA symptom “escape” and depression symptom “guilty,” two functions of the defense mechanism, showed both central and bridge characteristics. These two symptoms were suggested to activate the negative feedback loop and to further contribute to the comorbidity between IA and depression. These bridge symptoms have an enlightening effect on interventions and treatments of comorbidity of IA and depression.
CRediT authorship contribution statement
Yue Zhao: Methodology, Data curation, Formal analysis, Writing – original draft. Diyang Qu: Visualization, Writing – original draft. Shiyun Chen: Writing – review & editing. Xinli Chi: Conceptualization, Writing – review & editing, Supervision.
Data availability
The data that has been used is confidential.
References
- Albert U., Rosso G., Maina G., Bogetto F. Impact of anxiety disorder comorbidity on quality of life in euthymic bipolar disorder patients: Differences between bipolar I and II subtypes. Journal of Affective Disorders. 2008;105(1–3):297–303. doi: 10.1016/j.jad.2007.05.020. [DOI] [PubMed] [Google Scholar]
- Andreassen C.S., Pallesen S., Griffiths M.D. The relationship between addictive use of social media, narcissism, and self-esteem: Findings from a large national survey. Addictive Behaviors. 2017;64:287–293. doi: 10.1016/j.addbeh.2016.03.006. [DOI] [PubMed] [Google Scholar]
- APA . 5th ed. American Psychiatric Association; Washington, DC: 2013. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- Belkin G., Appleton S., Langlois K. Reimagining mental health systems post COVID-19. The Lancet Planetary Health. 2021;5(4):e181–e182. doi: 10.1016/s2542-5196(21)00037-1. [DOI] [PubMed] [Google Scholar]
- Berezovskaya I.P., Shipunova O.D., Kedich S.I. Proceedings of the XI international scientific conference communicative strategies of the information society. 2019. Internet addiction and youth coping strategies; pp. 1–6. [DOI] [Google Scholar]
- Bessiere K., Kiesler S., Kraut R., Boneva B.S. Effects of Internet use and social resources on changes in depression. Information, Community & Society. 2008;11(1):47–70. doi: 10.1080/13691180701858851. [DOI] [Google Scholar]
- Billones R.R., Kumar S., Saligan L.N. Disentangling fatigue from anhedonia: A scoping review. Translational Psychiatry. 2020;10(1):273. doi: 10.1038/s41398-020-00960-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Borkulo C.D., Boschloo L., Borsboom D., Penninx B.W., Waldorp L.J., Schoevers R. Association of symptom network structure with the course of depression. JAMA Psychiatry. 2015;72(12):1219–1226. doi: 10.1001/jamapsychiatry.2015.2079. [DOI] [PubMed] [Google Scholar]
- van Borkulo C.D., van Bork R., Boschloo L., Kossakowski J.J., Tio P., Schoevers R.A.…Waldorp L.J. Comparing network structures on three aspects: A permutation test. Psychological Methods. 2022 doi: 10.1037/met0000476. [DOI] [PubMed] [Google Scholar]
- Borsboom D. Psychometric perspectives on diagnostic systems. Journal of Clinical Psychology. 2008;64(9):1089–1108. doi: 10.1002/jclp.20503. [DOI] [PubMed] [Google Scholar]
- Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16(1):5–13. doi: 10.1002/wps.20375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D., Cramer A.O.J. Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Borsboom D., Robinaugh D.J., Rhemtulla M., Cramer A.O.J., Psychosyst G. Robustness and replicability of psychopathology networks. World Psychiatry. 2018;17(2):143–144. doi: 10.1002/wps.20515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brailovskaia J., Schillack H., Margraf J. Tell me why are you using social media (SM)! Relationship between reasons for use of SM, SM flow, daily stress, depression, anxiety, and addictive SM use-An exploratory investigation of young adults in Germany. Computers in Human Behavior. 2020;113 doi: 10.1016/j.chb.2020.106511. [DOI] [Google Scholar]
- Brailovskaia J., Teismann T., Friedrich S., Schneider S., Margraf J. Suicide ideation during the COVID-19 outbreak in German university students:Comparison with pre-COVID-19 rates. Journal of Affective Disorders Reports. 2021;6 doi: 10.1016/j.jadr.2021.100228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bringmann L.F., Lemmens L.H.J.M., Huibers M.J.H., Borsboom D., Tuerlinckx F. Revealing the dynamic network structure of the beck depression inventory-II. Psychological Medicine. 2015;45(4):747–757. doi: 10.1017/s0033291714001809. [DOI] [PubMed] [Google Scholar]
- Brown R. F, Schutte, N.S Direct and indirect relationships between emotional intelligence and subjective fatigue in university students. Journal of Psychosomatic Research. 2006;60(6):585–593. doi: 10.1016/j.jpsychores.2006.05.001. [DOI] [PubMed] [Google Scholar]
- Burger J., Isvoranu A.M., Lunansky G., Haslbeck J.M.B., Epskamp S., Hoekstra R.H.A., Fried E.I., Borsboom D., Blanken T.F. Reporting standards for psychological network analyses in cross-sectional data. Psychological Methods. 2022 Apr 11 doi: 10.1037/met0000471. Epub ahead of print. PMID: 35404629. [DOI] [PubMed] [Google Scholar]
- Cai H., Bai W., Sha S., Zhang L., Chow I.H., Lei S.-M., Grace K.I.…Xiang Y.T. Identification of central symptoms in internet addictions and depression among adolescents in Macau: A network analysis. Journal of Affective Disorders. 2022;302:415–423. doi: 10.7717/peerj.12907/table-1. [DOI] [PubMed] [Google Scholar]
- Caplan S.E.J. Problematic internet use and psychosocial well-being: Development of a theory-based cognitive–behavioral measurement instrument. Computers in Human Behavior. 2002;18(5):553–575. doi: 10.1016/s0747-5632(02)00004-3. [DOI] [Google Scholar]
- Carli V., Durkee T., Wasserman D., Hadlaczky G., Despalins R., Kramarz E., Kaess M. The association between pathological internet use and comorbid psychopathology: A systematic review. Psychopathology. 2013;46(1):1–13. doi: 10.1159/000337971. [DOI] [PubMed] [Google Scholar]
- Chen J., Chen Z. Extended Bayesian information criteria for model selection with large model spaces. Biometrika. 2008;95(3):759–771. doi: 10.1093/biomet/asn034. [DOI] [Google Scholar]
- Cheng C., Sun P., Mak K.-K. Internet addiction and psychosocial maladjustment: Avoidant coping and coping inflexibility as psychological mechanisms. Cyberpsychology, Behavior, and Social Networking. 2015;18(9):539–546. doi: 10.1089/cyber.2015.0121. [DOI] [PubMed] [Google Scholar]
- Chou C., Hsiao M.C. Internet addiction, usage, gratification, and pleasure experience: The taiwan college students' case. Computers & Education. 2000;35(1):65–80. doi: 10.1016/s0360-1315(00)00019-1. [DOI] [Google Scholar]
- Chun J.W., Choi J., Cho H., Choi M.R., Ahn K.J., Choi J.S., Kim D.J. Role of frontostriatal connectivity in adolescents with excessive smartphone use. Frontiers in Psychiatry. 2018;9:437. doi: 10.3389/fpsyt.2018.00437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer A. O. J, van Borkulo C. D, Giltay E. J, van Der Mass H. L, Kendler K. S, Scheffer M, Borsboom D, et al. Major depression as a complex dynamic system. PloS One. 2016;11(12) doi: 10.1371/journal.pone.0167490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer A.O.J., Waldorp L.J., van der Maas H.L., Borsboom D. Comorbidity: A network perspective. Behavioral and Brain Sciences. 2010;33(2–3):137. doi: 10.1017/s0140525x09991567. [DOI] [PubMed] [Google Scholar]
- Daumiller M., Rinas R., Hein J., Janke S., Dickhaeuser O., Dresel M. Shifting from face-to-face to online teaching during COVID-19: The role of university faculty achievement goals for attitudes towards this sudden change, and their relevance for burnout/engagement and student evaluations of teaching quality. Computers in Human Behavior. 2021;118 doi: 10.1016/j.chb.2020.106677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis R.A. A cognitive-behavioral model of pathological Internet use. Computers in Human Behavior. 2001;17(2):187–195. doi: 10.1016/s0747-5632(00)00041-8. [DOI] [Google Scholar]
- De Leo J.A., Wulfert E. Problematic internet use and other risky behaviors in college students: An application of problem-behavior theory. Psychology of Addictive Behaviors. 2013;27(1):133. doi: 10.1037/a0030823. [DOI] [PubMed] [Google Scholar]
- Diez-Quevedo C., Rangil T., Sanchez-Planell L., Kroenke K., Spitzer R.L. Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosomatic Medicine. 2001;63(4):679–686. doi: 10.1097/00006842-200107000-00021. [DOI] [PubMed] [Google Scholar]
- Dong H., Yang F., Lu X., Hao W. Internet addiction and related psychological factors among children and adolescents in China during the coronavirus disease 2019 (COVID-19) epidemic. Frontiers in Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.00751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Borsboom D., Fried E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods. 2018;50(1):195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Cramer A.O.J., Waldorp L.J., Schmittmann V.D., Borsboom D., Waldrop L.J., Schmittmann V.D., Borsboom D. qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software. 2012;48(4):1–18. doi: 10.18637/jss.v048.i04. [DOI] [Google Scholar]
- Feng Y., Ma Y., Zhong Q. The relationship between adolescents' stress and internet addiction: A mediated-moderation model. Frontiers in Psychology. 2019;10:2248. doi: 10.3389/fpsyg.2019.02248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes M.K., Wright A.G.C., Markon K.E., Krueger R.F. Evidence that psychopathology symptom networks have limited replicability. Journal of Abnormal Psychology. 2017;126(7):969–988. doi: 10.1037/abn0000276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried E.I., Cramer A.O.J. Moving forward: Challenges and directions for psychopathological network theory and methodology. Perspectives on Psychological Science. 2017;12(6):999–1020. doi: 10.1177/1745691617705892. [DOI] [PubMed] [Google Scholar]
- Friedman J.H., Hastie T., Tibshirani R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics. 2008;9(3):432–441. doi: 10.1093/biostatistics/kxm045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fruchterman T., Reingold E. Graph drawing by force-directed placement. Software: Practice and Experience. 1991;21(11):1129–1164. doi: 10.1007/978-3-658-21742-6_49. [DOI] [Google Scholar]
- Fung X.C., Siu A.M., Potenza M.N., O'brien K.S., Latner J.D., Chen C.Y.…Chen Y.L. Problematic use of internet-related activities and perceived weight stigma in schoolchildren: A longitudinal study across different epidemic periods of COVID-19 in China. Frontiers in Psychiatry. 2021;700 doi: 10.3389/fpsyt.2021.67583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao T., Li J., Zhang H., Gao J., Kong Y., Hu Y., Mei S. The influence of alexithymia on mobile phone addiction: The role of depression, anxiety and stress. Journal of Affective Disorders. 2018;225:761–766. doi: 10.1016/j.jad.2017.08.020. [DOI] [PubMed] [Google Scholar]
- van de Geer S., Bühlmann P., Ritov Y., Dezeure R. On asymptotically optimal confdence regions and tests for high-dimensional models. Annals of Statistics. 2014;42(3):1166–1202. doi: 10.1214/14-aos1221. [DOI] [Google Scholar]
- Guo Q., Zheng Y., Shi J., Wang J., Li G., Li C., Yang Z. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: A mixed-method study. Brain, Behavior, and Immunity. 2020;88:17–27. doi: 10.1016/j.bbi.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ha J.H., Kim S.Y., Bae S.C., Bae S., Kim H., Sim M., Cho S.C. Depression and Internet addiction in adolescents. Psychopathology. 2007;40(6):424–430. doi: 10.1111/j.1365-2869.2010.00883.x. [DOI] [PubMed] [Google Scholar]
- Haslbeck J., Waldorp L. 2015. mgm: Estimating time-varying mixed graphical models in high-dimensional data. arXiv preprint arXiv:1510.06871. [DOI] [Google Scholar]
- Hastie T., Tibshirani R., Wainwright M.J. CRC Press; Boca Raton, FL: 2015. Statistical learning with sparsity: The lasso and generalizations. [DOI] [Google Scholar]
- Hau H.-M., Weitz J., Bork U.J. Impact of the COVID-19 pandemic on student and resident teaching and training in surgical oncology. Journal of Clinical Medicine. 2020;9(11):3431. doi: 10.3390/jcm9113431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman E.A., Thompson R.R., Garfin D.R., Silver R.C. The unfolding COVID-19 pandemic: A probability-based, nationally representative study of mental health in the United States. Science Advances. 2020;6(42) doi: 10.1126/sciadv.abd5390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang T.J., Rabheru K., Peisah C., Reichman W., Ikeda M.J. Loneliness and social isolation during the COVID-19 pandemic. International Psychogeriatrics. 2020;32(10):1217–1220. doi: 10.31234/osf.io/3dwxq. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isvoranu A.M., Epskamp S. Which estimation method to choose in network psychometrics? Deriving guidelines for applied researches. Psychological Methods. 2021 doi: 10.1037/met0000439. [DOI] [PubMed] [Google Scholar]
- Jones P.J., Ma R., McNally R.J. Bridge centrality: A network approach to understanding comorbidity. Multivariate Behavioral Research. 2021;56(2):353–367. doi: 10.1080/00273171.2019.1614898. [DOI] [PubMed] [Google Scholar]
- Kaiser T., Herzog P., Voderholzer U., Brakemeier E.L. Unraveling the comorbidity of depression and anxiety in a large inpatient sample: Network analysis to examine bridge symptoms. Depression and Anxiety. 2021;38(3):307–317. doi: 10.1002/da.23136. [DOI] [PubMed] [Google Scholar]
- Kato T.A., Shinfuku N., Tateno M. Internet society, internet addiction, and pathological social withdrawal: The chicken and egg dilemma for internet addiction and hikikomori. Current Opinion in Psychiatry. 2020;33(3):264–270. doi: 10.1097/yco.0000000000000601. [DOI] [PubMed] [Google Scholar]
- Konstantopoulou G., Raikou N. Clinical evaluation of depression in university students during quarantine due to covid-19 pandemic. European Journal of Public Health Studies. 2020;3(1) doi: 10.46827/ejphs.v3i1.65. [DOI] [Google Scholar]
- Kroska E.B., Calarge C., O'Hara M.W., Deumic E., Dindo L. Burnout and depression in medical students: Relations with avoidance and disengagement. Journal of Contextual Behavioral Science. 2017;6(4):404–408. doi: 10.1016/j.jcbs.2017.08.003. [DOI] [Google Scholar]
- Laconi S., Rodgers R.F., Chabrol H. The measurement of internet addiction: A critical review of existing scales and their psychometric properties. Computers in Human Behavior. 2014;41:190–202. doi: 10.1016/j.chb.2014.09.026. [DOI] [Google Scholar]
- Leung S.A., Hou Z.J., Gati I., Li X. Effects of parental expectations and cultural-values orientation on career decision-making difficulties of Chinese university students. Journal of Vocational Behavior. 2011;78(1):11–20. doi: 10.1016/j.jvb.2010.08.004. [DOI] [Google Scholar]
- Li Q., Dai W., Zhong Y., Wang L., Dai B., Liu X. The mediating role of coping styles on impulsivity, behavioral inhibition/approach system, and internet addiction in adolescents from a gender perspective. Frontiers in Psychology. 2019;10 doi: 10.3389/fpsyg.2019.02402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li G., Hou G., Yang D., Jian H., Wang W. Relationship between anxiety, depression, sex, obesity, and internet addiction in Chinese adolescents: A short-term longitudinal study. Addictive Behaviors. 2019;90:421–427. doi: 10.1016/j.addbeh.2018.12.009. [DOI] [PubMed] [Google Scholar]
- Lin T.Y., Goyal P., Girshick R., He K., Dollar P. Focal loss for dense object detection. IEEE Transactions on Pattern Analysis and Machine Intelligence. 2020;42(2):318–327. doi: 10.1109/tpami.2018.2858826. [DOI] [PubMed] [Google Scholar]
- Little R.J. A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association. 1988;83(404):1198–1202. [Google Scholar]
- Longstreet P., Brooks S., Gonzalez E. Internet addiction: When the positive emotions are not so positive. Technology in Society. 2019;57:76–85. doi: 10.1016/j.techsoc.2018.12.004. [DOI] [Google Scholar]
- Lovibond P.F., Lovibond S.H. The structure of negative emotional states: Comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behaviour Research and Therapy. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- Malgaroli M., Calderon A., Bonanno G.A. Networks of major depressive disorder: A systematic review. Clinical Psychology Review. 2021;85 doi: 10.1016/j.cpr.2021.102000. [DOI] [PubMed] [Google Scholar]
- Marchetti I. Hopelessness: A network analysis. Cognitive Therapy and Research. 2019;43(3):611–619. doi: 10.1007/s10608-018-9981-y. [DOI] [Google Scholar]
- Masaeli N., Farhadi H. Prevalence of internet-based addictive behaviors during COVID-19 pandemic: A systematic review. Journal of Addictive Diseases. 2021;39(4):468–488. doi: 10.1080/10550887.2021.1895962. [DOI] [PubMed] [Google Scholar]
- McNally R.J., Robinaugh D.J., Wu G.W.Y., Wang L., Deserno M.K., Borsboom D. Mental disorders as causal systems: A network approach to posttraumatic stress disorder. Clinical Psychological Science. 2015;3(6):836–849. doi: 10.1177/2167702614553230. [DOI] [Google Scholar]
- Meuret A.E., Tunnell N., Roque A. Anxiety disorders and medical comorbidity: Treatment implications. Anxiety Disorders. 2020;1191:237–261. doi: 10.1007/978-981-32-9705-0_15. [DOI] [PubMed] [Google Scholar]
- Neff K.D. Self-compassion, self-esteem, and well-being. Social and personality psychology compass. 2011;5(1):1–12. doi: 10.1111/j.1751-9004.2010.00330.x. [DOI] [Google Scholar]
- Nickerson A., Schick M., Schnyder U., Bryant R.A., Morina N. Comorbidity of posttraumatic stress disorder and depression in tortured, treatment-seeking refugees. Journal of Traumatic Stress. 2017;30(4):409–415. doi: 10.1002/jts.22205. [DOI] [PubMed] [Google Scholar]
- Opsahl T., Agneessens F., Skvoretz J. Node centrality in weighted networks: Generalizing degree and shortest paths. Social Networks. 2010;32(3):245–251. doi: 10.1016/j.socnet.2010.03.006. [DOI] [Google Scholar]
- Orsal O., Orsal O., Unsal A., Ozalp S.S. Evaluation of internet addiction and depression among university students. Procedia-Social and Behavioral Sciences. 2013;82:445–454. doi: 10.1016/j.sbspro.2013.06.291. [DOI] [Google Scholar]
- Penner I.K., Paul F. Fatigue as a symptoms or comorbidity of neurological diseases. Nature Reviews Neurology. 2017;13(11):662–675. doi: 10.1038/nmeurol.2017.117. [DOI] [PubMed] [Google Scholar]
- Quigley L., Wen A., Dobson K.S. Avoidance and depression vulnerability: An examination of avoidance in remitted and currently depressed individuals. Behaviour Research and Therapy. 2017;97:183–188. doi: 10.1016/j.brat.2017.07.015. [DOI] [PubMed] [Google Scholar]
- Richetin J., Preti E., Costantini G., De Panfilis C. The centrality of affective instability and identity in Borderline Personality Disorder: Evidence from network analysis. PLoS One. 2017;12(10) doi: 10.1371/journal.pone.0186695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinaugh D.J., Hoekstra R.H.A., Toner E.R., Bosrboom D. The network approach to psychopathology: A review of the literature 2008-2018 and an agenda for future research. Psychological Medicine. 2020;50(3):353–366. doi: 10.1017/S0033291719003404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seki T., Hamazaki K., Natori T., Inadera H. Relationship between internet addiction and depression among Japanese university students. Journal of Affective Disorders. 2019;256:668–672. doi: 10.1016/j.jad.2019.06.055. [DOI] [PubMed] [Google Scholar]
- Shek D.T., Tang V.M., Lo C.Y. Internet addiction in Chinese adolescents in Hong Kong: Assessment, profiles, and psychosocial correlates. The Scientific World Journal. 2008;8:776–787. doi: 10.1100/tsw.2008.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffen A., Nübel J., Jacobi F., Bätzing J., Holstiege J. Mental and somatic comorbidity of depression: A comprehensive cross-sectional analysis of 202 diagnosis groups using German nationwide ambulatory claims data. BMC Psychiatry. 2020;20(1):142. doi: 10.1186/s12888-020-02546-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y., Fu Z., Bo Q., Mao Z., Ma X., Wang C. The reliability and validity of PHQ-9 in patients with major depressive disorder in psychiatric hospital. BMC Psychiatry. 2020;20(1) doi: 10.1186/s12888-020-02885-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tateno M., Teo A.R., Ukai W., Kanazawa J., Katsuki R., Kubo H., Kato T.A. Internet addiction, smartphone addiction, and hikikomori trait in Japanese young adult: Social isolation and social network. Frontiers in Psychiatry. 2019;10:455. doi: 10.3389/fpsyt.2019.00455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tichon J.G., Shapiro M. The process of sharing social support in cyberspace. CyberPsychology and Behavior. 2003;6(2):161–170. doi: 10.1089/109493103321640356. [DOI] [PubMed] [Google Scholar]
- Tsai J.K., Lu W.H., Hsiao R.C., Hu H.F., Yen C.F. Relationship between difficulty in emotion regulation and internet addiction in college students: A one-year prospective study. International Journal of Environmental Research and Public Health. 2020;17(13):4766. doi: 10.3390/ijerph17134766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan N., Durgun H., Kaya H., Asti T., Yilmaz Y., Gunduz G., Ertas G. Relationship between nursing students' levels of internet addiction, loneliness, and life satisfaction. Perspectives in Psychiatric Care. 2020;56(3):598–604. doi: 10.1111/ppc.12474. [DOI] [PubMed] [Google Scholar]
- Unger S., Meiran W.R. Student attitudes towards online education during the COVID-19 viral outbreak of 2020: Distance learning in a time of social distance. International Journal of Technology in Education and Science. 2020;4(4):256–266. doi: 10.46328/ijtes.v4i4.107. [DOI] [Google Scholar]
- Ustun G. Determining depression and related factors in a society affected by COVID-19 pandemic. International Journal of Social Psychiatry. 2021;67(1):54–63. doi: 10.1177/0020764020938807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakefield J.C., Schmitz M.F. Feelings of worthlessness during a single complicated major depressive episode predict postremission suicide attempt. Acta Psychiatrica Scandinavica. 2016;133(4):257–265. doi: 10.1111/acps.12521. [DOI] [PubMed] [Google Scholar]
- Wang Y., Hu Z., Feng Y., Wilson A., Chen R. Changes in network centrality of psychopathology symptoms between the COVID-19 outbreak and after peak. Molecular Psychiatry. 2020;25(12):3140–3149. doi: 10.1038/s41380-020-00881-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasil A.R., Gillespie S., Park S.J., Venturo-Conerly K.E., Osborn T.L., DeRubeis R.J., Jones P. Which symptoms of depression and anxiety are most strongly associated with happiness? A network analysis of Indian and Kenyan adolescents. Journal of Affective Disorders. 2021;295:811–821. doi: 10.1016/j.jad.2021.08.087. [DOI] [PubMed] [Google Scholar]
- Yang X., Hu H., Zhao C., Xu H., Tu X., Zhang G. A longitudinal study of changes in smart phone addiction and depressive symptoms and potential risk factors among Chinese college students. BMC Psychiatry. 2021;21(1):1–9. doi: 10.1186/s12888-021-03265-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye B., Zhou X., Im H., Liu M., Wang X.Q., Yang Q. Epidemic rumination and resilience on college students' depressive symptoms during the COVID-19 pandemic: The mediating role of fatigue. Frontiers in Public Health. 2020;8 doi: 10.3389/fpubh.2020.560983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young K. Internet addiction: A new clinical phenomenon and its consequences. American Behavioral Scientist. 2004;48(4):402–415. doi: 10.1177/0002764204270278. [DOI] [Google Scholar]
- Young K. The evolution of internet addiction disorder. Internet addiction. 2017:3–18. doi: 10.1007/978-3-319-46276-9_1. [DOI] [Google Scholar]
- Yu Y., She R., Luo S., Xin M., Li L., Wang S., Lau J.T. Factors influencing depression and mental distress related to COVID-19 among university students in China: Online cross-sectional mediation study. JMIR Ment Health. 2021;8(2) doi: 10.2196/22705. https://preprints.jmir.org/preprint/22705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L., Fang J., Wan Y., Gong C., Su P., Tao F., Sun Y. The patterns of adverse childhood experiences among Chinese children: Four-year longitudinal associations with psychopathological symptoms. Journal of Psychiatric Research. 2020;122:1–8. doi: 10.1016/j.jpsychires.2019.12.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that has been used is confidential.