Abstract
Experiencing stressors related to the COVID-19 pandemic such as health-related concern, social isolation, occupational disruption, financial insecurity, and resource scarcity can adversely impact mental health; however, the extent of the impact varies greatly between individuals. In this study, we examined the role of neuroticism as an individual-level risk factor that exacerbates the association between pandemic stressors and depressive symptoms. With repeated assessments of pandemic stressors and depressive symptoms collected from 3181 participants over the course of the pandemic, we used multilevel modeling to test if neuroticism moderated the association between pandemic stressors and depressive symptoms at both between- and within-person levels. At the between-person level, we found that participants who reported more pandemic stressors on average had higher levels of depressive symptoms and that this association was stronger among those high in neuroticism. At the within-person level, reporting more pandemic stressors relative to one's average on any given occasion was also associated with heightened depressive symptoms and this effect was similarly exacerbated by neuroticism. The findings point to pandemic stressor exposure and neuroticism as risk factors for depressive symptoms and, in demonstrating their synergistic impact, may help identify individuals at greatest risk for adverse psychological responses to the COVID-19 pandemic.
Keywords: Neuroticism, Stressors, Depressive symptoms, COVID-19, Pandemic, Multilevel modeling
1. Introduction
The psychosocial ramifications of the COVID-19 pandemic have been profound on a societal level, yet there are large individual differences in the impact. As one of the most common clinical manifestations of psychological distress, depressive symptoms are a threat to individual and public health that need to be closely monitored both during, and in the aftermath of, the pandemic (McLaughlin, 2011; Santomauro et al., 2021). Although heightened depressive symptoms have been reported globally during the pandemic, the questions of for whom, and under what conditions these symptoms manifest, are less understood. Increased understanding of these issues will facilitate both prevention and early intervention (Santomauro et al., 2021). Taking a social-contextual approach involves examining the dynamic interplay of situational and dispositional factors contributing to mental and physical health outcomes (DeLongis & Holtzman, 2005). In the context of the pandemic, situational stressors such as health-related concerns, social isolation, occupational disruptions, financial insecurity, and resource scarcity have been associated with depressive symptoms (Ettman et al., 2020; Leach et al., 2021; Raina et al., 2021; Zheng et al., 2021). Neuroticism, the dispositional tendency to experience negative emotionality, is a key facet in most multidimensional models of personality, and a major risk factor for depression (Lahey, 2009). Those high in neuroticism tend to experience heightened negative affect, as well as greater negative affect reactivity in response to environmental stressors (Bolger et al., 1991; Gunthert et al., 1999; Suls & Martin, 2005). Although neuroticism has been associated with heightened depressive symptoms during the COVID-19 pandemic (Gallagher et al., 2021; Nudelman et al., 2021), its role in the association between pandemic stressors and depressive symptoms remains unclear.
Neuroticism has been consistently linked to stressor appraisal, with those high in neuroticism more likely to appraise stressors as threatening (Kilby et al., 2018). One cross-sectional study conducted during the COVID-19 pandemic found that neuroticism contributed to stress appraisals over and above the effects of stressor exposure (Bellingtier et al., 2021). This heightened threat perception can also translate to individuals high in neuroticism perceiving more stressors in the environment (Suls & Martin, 2005). This in turn is linked to greater distress (Gunthert et al., 1999), a relationship in part perpetuated by greater use of coping strategies that are ill-suited to deal with situational demands (DeLongis & Holtzman, 2005). Heightened negative affect and depressive symptoms among those high in neuroticism in the context of the COVID-19 pandemic may be a function of perceiving more stressors in the environment. However, negative affect reactivity in response to pandemic stressors may also contribute to the relationship. Evidence of this in the context of the COVID-19 pandemic is provided by one study that found negative affect reactivity in response to threats posed by COVID-19 to be greater among those high in neuroticism (Kroencke et al., 2020). The study also found that neuroticism moderated the within-person association between COVID-19-related worry and psychological distress, exacerbating the association among individuals who were higher in neuroticism (Kroencke et al., 2020). This work points to neuroticism as a factor that may increase risk of adverse psychological repercussions of the pandemic. Further, the study underscores the need to consider the role of neuroticism when examining the relationship between pandemic stressors and depressive symptoms.
In the present study, we built on work examining how sources of stress associated with the COVID-19 pandemic have adversely impacted mental health by examining neuroticism as a contributor to individual differences in strength of the association. With repeated assessments of pandemic stressors and depressive symptoms collected over nearly two years of the pandemic, we used multilevel modeling to uncover not only whether higher average levels of pandemic stressors were associated with heightened depressive symptoms, but also whether individuals experienced increases in depressive symptoms on occasions when they reported more pandemic stressors relative to their own average. We hypothesized that both of these associations would be exacerbated among individuals higher in neuroticism. Although we expected the same direction of effects at the within- and between-person levels, modeling these effects simultaneously is crucial given the results at each level provide differing insight into how pandemic stressors and neuroticism function as risk factors for depressive symptoms. Specifically, a within-person association provides insight into depressive symptom trajectories of individuals, whereas an association at the between-person level helps identify population-level risk factors for heightened depressive symptoms (Luo et al., 2022). Both of these associations are critical to consider.
2. Methods
2.1. Data collection and participants
Data for the present analyses come from a longitudinal study that began in March 2020 to assess the psychosocial impacts of the COVID-19 pandemic. Publications off prior waves of study data have been reported elsewhere (Morstead et al., 2022; Zheng et al., 2021). The baseline survey included questions on demographics, trait neuroticism, pandemic stressors and depressive symptoms. Follow-up surveys contained assessments of pandemic stressors and depressive symptoms. Recruitment for the study was done through English-language, primarily North American, news and social media outlets. Participants accessed the baseline survey via a link on the study webpage. Follow-up surveys were sent to participants who provided their email address in the baseline survey. The follow-up surveys were distributed weekly from March through May 2020, and monthly from June 2020 onwards. This reduction in frequency was to limit participant burden and reduce attrition as the pandemic wore on, resulting in a shift in time intervals between surveys part way through the study. Included in the present sample are data from North American participants who completed the baseline survey and at least two follow-up assessments between March 18, 2020 (the start of the study) and November 5, 2021 (when data analysis began).
Of 4708 North American participants who completed a baseline survey, 3316 completed at least two follow-up assessments at the time of data analysis. After listwise deletion on all study variables, the analytic sample consisted of 3181 participants and 40,729 measurement occasions. The number of measurement occasions per participant ranged from three to 27 (M = 13.19 SD = 7.76). The mean age of the sample was 45.81 (SD = 15.42), and the sample was predominantly made up of women (84 %), with 14 % and 2 % identifying as men and other genders, respectively. The majority of participants were also college educated (71 % had at least a four-year bachelor's degree). Most participants were living in Canada (73 %), with the remaining 27 % in the United States. Participation in the study was voluntary and no compensation was offered. Informed consent was obtained from all participants and the study protocol was approved by the UBC Behavioural Research Ethics Board.
2.2. Measures
2.2.1. Depressive symptoms
Depressive symptoms were assessed at each timepoint using the Center for Epidemiologic Studies Short Depression Scale (CESD-10; Andresen et al., 1994). This scale has been widely used to assess depressive symptoms in community samples (Irwin et al., 1999), including in the context of the COVID-19 pandemic (Raina et al., 2021). The 10-item scale includes items such as “I felt depressed,” and “I felt that everything I did was an effort.” Items were rated on a 5-point scale ranging from 0 (rarely or none of the time) to 5 (all of the time). Item responses were added together at each assessment to create a composite score for each timepoint. At the first timepoint, scores ranged from 0 to 30 (M = 13.41, SD = 7.12), and reliability (total omega, ωt) was 0.91.
2.2.2. Neuroticism
Neuroticism was assessed at baseline using the two-item neuroticism subscale from the 10-item version of the Big Five Inventory (Rammstedt & John, 2007). The scale has demonstrated good internal consistency and scores correlate highly with those obtained using the longer version (Thalmayer et al., 2011). Participants rated the extent to which they agreed they are someone who “gets nervous easily” and “is relaxed, handles stress well.” The items were rated on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The latter item was reverse scored before computing the scale mean. Responses ranged from 1 to 5 (M = 3.10, SD = 0.95) and reliability (Spearman-Brown coefficient, ρ) was 0.67.
2.2.3. Pandemic stressors
Pandemic stressors were assessed at each timepoint by tallying six stressors that participants could indicate they had experienced since their prior assessment. Stressors were chosen based on those identified as prevalent during the COVID-19 pandemic, and associated with depressive symptoms (Ettman et al., 2020; Leach et al., 2021), including in research conducted with an earlier wave of data from the present study (Zheng et al., 2021). Similar checklist measures have been used in prior work to quantify stressor exposure across an array of domains during the pandemic (Park et al., 2021). Items pertained to concern about one's own health (“I was concerned about my own health and well-being”), concern about the health of family and friends (“I was concerned about close family and friends' health and well-being”), social isolation (“I felt socially isolated”), occupational difficulty (“I found work/school more difficult”), resource scarcity (“I was concerned about getting basic necessities such as food and supplies”), and financial insecurity (extent to which “a strain on your financial resources” had been of concern). All stressors had a dichotomous response option aside from the financial insecurity which was assessed on a 4-point Likert scale and dichotomized for the purpose of creating a tallied score (responses indicating a moderate amount or a great deal were categorized as indicative of financial insecurity). At the first timepoint, the number of stressors endorsed ranged from 0 to 6 (M = 3.83, SD = 1.55) and reliability (total omega, ωt) was 0.69.
2.2.4. Covariates
Age, gender, education, and country of residence were provided by participants in the baseline survey. These variables were included in the analyses given their previously documented association with pandemic stressor exposure and depressive symptoms (Ettman et al., 2020; Leach et al., 2021; Raina et al., 2021; Zheng et al., 2021). To account for the rapidly changing pandemic landscape, we included a variable capturing the number of days since COVID-19 was declared a pandemic by the WHO (March 11, 2020) at each timepoint. This variable ranged from 8.02 to 506.85 (M = 39.35, SD = 64.03) at baseline assessment, and from 8.02 to 598.28 (M = 221.12, SD = 173.62) across all timepoints.
2.3. Analytic strategy
We first examined univariate and bivariate statistics. Then, given the hierarchically structured nature of the data (timepoints nested within individuals), we used multilevel modeling to test our hypotheses (Raudenbush & Bryk, 2002). We used centering to partition the within- and between-person associations between stressors and depressive symptoms into two components (West et al., 2011). We person-mean centered pandemic stressors creating a level-1 variable, referred to as “person-centered (PC) pandemic stressors.” This variable removed between-person variation and allowed us to examine whether increases in stressor reporting relative to one's average was associated with heightened depressive symptoms (within-person effect). We created a level-2 variable to examine whether reporting more stressors on average was associated with heightened depressive symptoms (between-person effect). We computed this variable, referred to as “person-mean (PM) pandemic stressors,” by taking each participant's mean across timepoints and grand-mean centering. We grand-mean centered the hypothesized moderator, neuroticism. Gender, education, and country were dummy-coded. For gender, we included those identifying as men or other genders as dummy codes, with women as the reference category. We coded education such that 1 indicated the participant had at least a four-year bachelor's degree in college and 0 indicated that the participant has less than a four-year bachelor's degree. We coded country as 1 if the participant resided in Canada, and 0 if they resided in the United States. To aid in model convergence, we rescaled the time variable to reflect months since the pandemic was declared and age to correspond to decades.
We estimated an unconditional model to compute the intraclass correlation coefficient (ICC) reflecting the degree of similarity between measurements of depressive symptoms within individuals across timepoints. We then estimated a main effects model with PC pandemic stressors, PM pandemic stressors, neuroticism, time, and demographic covariates (age, gender, education, and country) as predictors, including both PC pandemic stressors and time as random slopes. We next estimated an interaction model, adding an interaction between neuroticism and PC pandemic stressors (cross level interaction) and an interaction between neuroticism and PM pandemic stressors (a level-2 interaction). The equation for this model was:
- Level 1 (within-person):
- Level 2 (between-person):
The between-person effect of pandemic stressors (conditional on neuroticism) is represented by γ06 + γ08 neuroticism j, and γ08 reflects the expected change in the between-person effect per unit increase in neuroticism. The within-person effect of pandemic stressors is represented by γ10 + γ11 neuroticism j, and γ11reflects the expected change in the within-person effect per unit increase in neuroticism. To account for serial dependence of residuals, we included a first-order autoregressive error structure, which accommodates the unequal time intervals between measurement occasions. We used restricted maximum likelihood (REML) to estimate all models. To compare the main effect and interaction models using a likelihood ratio test, we re-fit the models using maximum likelihood (ML) estimation. We conducted all analyses in R version 4.1.0 (R Core Team, 2021) and RStudio version 1.4.1106 (RStudio Team, 2021), using the nlme (Pinheiro et al., 2021) R package for multilevel modeling and the r2mlm (Shaw et al., 2022) R package for computing R2 values.
3. Results
Univariate and bivariate statistics are outlined in Table 1 . Depressive symptoms, neuroticism, and pandemic stressors assessed at baseline were all moderately to highly inter-correlated. We also found that 59 % of the variance in stressor reporting was attributable to between-person differences. In Table 2 , the ICC obtained from the unconditional model indicated that 73 % of the variance in depressive symptoms was attributable to between-person differences. In the main effects model, we found that neuroticism, PM pandemic stressors, and PC pandemic stressors, were all associated with heightened depressive symptoms. A four-year college degree and residing in Canada were associated with lower depressive symptoms. Participants reported lower depressive symptoms at later timepoints. Reporting one's gender as “other” was associated with higher depressive symptoms (compared to identifying as a woman).
Table 1.
Descriptive statistics of study variables at baseline assessment.
| Variable | M(SD) or n(%) | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|
| 1 | Depressive Symptoms | 13.41 (7.12) | ||||||
| 2 | Pandemic Stressors | 3.83 (1.55) | 0.55⁎⁎⁎ | |||||
| 3 | Neuroticism | 3.10 (0.95) | 0.47⁎⁎⁎ | 0.28⁎⁎⁎ | ||||
| 4 | Age | 45.81 (15.42) | −0.28⁎⁎⁎ | −0.31⁎⁎⁎ | −0.25⁎⁎⁎ | |||
| 5 | College Degreea | 2253 (71 %) | −0.01 | 0.05⁎⁎ | −0.03 | −0.04⁎ | ||
| 6 | Country (Canada)b | 2328 (73 %) | −0.15⁎⁎⁎ | −0.11⁎⁎⁎ | −0.02 | 0.04⁎ | −0.19⁎⁎⁎ | |
| 7 | Timec | 39.35 (64.03) | 0.04⁎ | −0.16⁎⁎⁎ | 0.03 | −0.02 | −0.04⁎ | −0.08⁎⁎⁎ |
Coded 1 = bachelor's degree (4-year) or higher, 0 = less than bachelor's degree.
Coded 1 = Canada, 0 = United States.
Date of assessment expressed as days since COVID-19 was declared a pandemic (March 11, 2020).
p < .05.
p < .01.
p < .001.
Table 2.
Results from multilevel models predicting depressive symptoms.
| Effect | Depressive Symptoms |
|||
|---|---|---|---|---|
| Unconditional Model | Main Effects Model | Interaction Model | ||
| Fixed effects | ||||
| Intercept | 12.23⁎⁎⁎ (0.11) | 13.10⁎⁎⁎ (0.21) | 13.02⁎⁎⁎ (0.21) | |
| Gender (Men) | −0.11 (0.22) | −0.14 (0.22) | ||
| Gender (Other) | 1.06⁎ (0.53) | 1.04 (0.53) | ||
| Age | 0.05 (0.05) | 0.04 (0.05) | ||
| College Degree | −0.62⁎⁎⁎ (0.17) | −0.62⁎⁎⁎ (0.17) | ||
| Country (Canada) | −0.99⁎⁎⁎ (0.17) | −0.98⁎⁎⁎ (0.17) | ||
| PM Pandemic Stressors | 2.76⁎⁎⁎ (0.06) | 2.77⁎⁎⁎ (0.06) | ||
| Neuroticism | 1.77⁎⁎⁎ (0.08) | 1.76⁎⁎⁎ (0.08) | ||
| PM Pandemic Stressors × Neuroticism | 0.16⁎⁎ (0.06) | |||
| PC Pandemic Stressors | 0.93⁎⁎⁎ (0.02) | 0.93⁎⁎⁎ (0.02) | ||
| PC Pandemic Stressors × Neuroticism | 0.08⁎⁎⁎ (0.02) | |||
| Time | −0.04⁎⁎⁎ (0.01) | −0.04⁎⁎⁎ (0.01) | ||
| Random effects | ||||
| Variance | ||||
| Level 1 | 36.32 | 11.50 | 11.50 | |
| Level 2 | 13.65 | 14.81 | 14.78 | |
| 0.48 | 0.48 | |||
| 0.04 | 0.04 | |||
| Goodness of Fit | ||||
| AIC | 232,690.9 | 222,353.9 | 222,348.4 | |
| BIC | 232,716.8 | 222,508.9 | 222,520.7 | |
Note. Standard errors are in parentheses. All models fit using restricted maximum likelihood (REML) estimation. In the main effects and interaction models, slopes of time and PC pandemic stressors were free to vary. PM = person-mean, PC = person-centered.
p < .05.
p < .01.
p < .001.
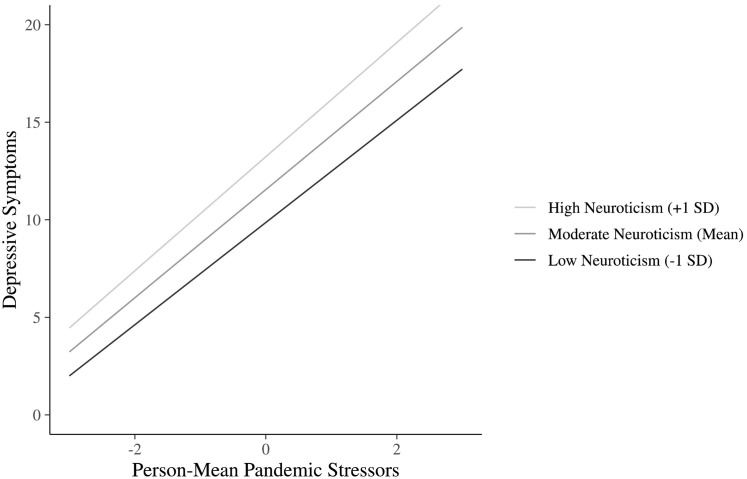
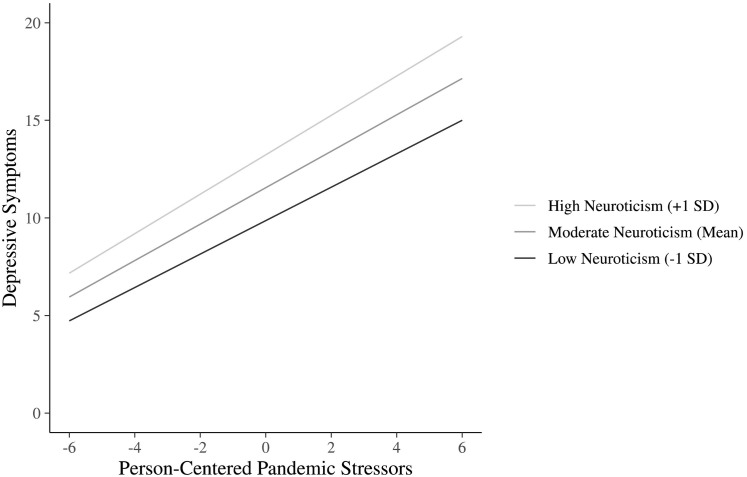
In the interactions model, both the level-2 interaction (reflecting differences in the between-person effect of stressors across levels of neuroticism) and the cross-level interaction (reflecting differences in the within-person effect of stressors across levels of neuroticism) were significant. Fig. 1, Fig. 2 depict the between- and within-person effects respectively. At the between-person level, the positive association between PM pandemic stressors and depressive symptoms was stronger among those high in neuroticism. At the within-person level, increases in pandemic stressors on any given timepoint (PC pandemic stressors) were associated with heightened depressive symptoms. This effect was similarly stronger among those high in neuroticism. However, as Fig. 1, Fig. 2 indicate, even among those low in neuroticism, there was still a strong positive association between depressive symptoms and both PM pandemic stressors, and PC pandemic stressors. Simple slopes analysis revealed that the association between pandemic stressors and depressive symptoms remained significant (p < .001) one standard deviation above and below the mean on neuroticism at both the within- and between-person level. In both the main effects and interaction models 47 % of variance in depressive symptoms was accounted for by fixed and random slopes (the predictors; Rights & Sterba, 2019). To compare the main effects and interaction models, we re-fit the models using ML estimation and conducted a likelihood ratio test which indicated that the inclusion of the interaction terms resulted in significant improvement in model fit compared to the model including only main effects, χ2(2) = 19.07, p < .001.
Fig. 1.
Between-person association between pandemic stressors and depressive symptoms moderated by neuroticism.
Note. Values on the x-axis reflect participants’ mean level of pandemic stressors across all timepoints, relative to the grand mean for the sample.
Fig. 2.
Within-person association between pandemic stressors and depressive symptoms moderated by neuroticism.
Note. Values on the x-axis reflect participants’ deviation from their mean level of reported pandemic stressors on a given timepoint.
4. Discussion
Results from the present study align with prior work documenting an association between pandemic stressors and depressive symptoms (Ettman et al., 2020; Leach et al., 2021; Raina et al., 2021; Zheng et al., 2021). The findings expand on this demonstrating that not only does the association exist at the between-person level of analysis, but also at the within-person level. Such knowledge is crucial given that effects at each level of analysis can offer insights into the functioning of individual-level risk factors (Luo et al., 2022). Participants reporting a higher average number of pandemic stressors across time had higher levels of depressive symptoms, and this association was stronger among those high in neuroticism. Increases in pandemic stressors on any given timepoint were similarly associated with heightened depressive symptoms, and the effect was again exacerbated among those high in neuroticism. These findings are in line with theory and research suggesting that both increased stressor perception (Kilby et al., 2018) and heightened emotional reactivity to stressors (Bolger et al., 1991; Gunthert et al., 1999; Suls & Martin, 2005) contribute to greater psychological distress among those high in neuroticism. Further, our findings indicate that pandemic stressors and neuroticism contribute to depressive symptoms independently of each other. This is notable given that the effect of stressors on mental health outcomes has occasionally been suggested to be attributable to individual differences in neuroticism (Espejo et al., 2011; McCrae, 1990).
There are limitations of our work that should be noted. Our results held controlling for education, providing preliminary evidence that the effects exist independent of socioeconomic status (SES). However, future work will need to explicate these effects further given the inherent limitation of using a single indicator to examine a variable as complex as SES (Braveman et al., 2005). It is possible that the magnitude of the observed effects are underestimated due to the relatively high SES of many participants in the present sample. The small magnitude of the interaction effects observed indicates that even among those low in neuroticism, pandemic stressors remained significantly associated with depressive symptoms. Although this could be a function of the pandemic context and the uniquely pervasive impact of pandemic stressors on mental health, it could also be due to a lack of sensitivity with our two-item measure of neuroticism. Inclusion of a more comprehensive assessment of neuroticism in future studies could provide greater confidence in the observed effects. Furthermore, the mechanisms through which the observed associations manifest should be examined (e.g., coping responses; DeLongis & Holtzman, 2005), perhaps by collecting assessments more closely spaced in time through the use of daily diary or experience-sampling methodologies (Bolger et al., 1991). Such work would advance understanding of the temporal ordering of events.
By examining data collected over the course of 19 months during the COVID-19 pandemic, this study provides unique insight into the role of neuroticism in the association between stressors and depressive symptoms in the pandemic context. The time range of data examined also provides support for the stability of this relationship across a range of key events during the pandemic. For example, data collection took place during a time when new insights about the virus were rapidly emerging and mechanisms of transmission were largely unclear (Carvalho et al., 2021). Additionally, the data acquired encompasses a period during which behavioural measures were the sole means of controlling disease spread, and extends into a time when vaccination programs were underway (Webster, 2021). That said, the pervasive impact of pandemic stressors and high levels of depression observed also limit the generalizability of the findings beyond the time period examined. It will be crucial to examine the role of neuroticism in the association between pandemic stressors and depressive symptoms as the pandemic progresses, restrictions ease, and individuals adapt. For most, depressive symptoms will likely be transient. This is supported by evidence of a downward trend in average levels of depressive symptoms over the course of the pandemic (Bendau et al., 2021; Fancourt et al., 2021). However, there are key individual differences. Among some individuals with heightened exposure to pandemic stressors, increases in depressive symptoms have been observed (Ettman et al., 2020). As such, examining individual differences, including neuroticism, will remain crucial to ascertain for whom, and under what conditions, adverse psychological symptoms persist and necessitate intervention.
Funding
This work was supported by the Social Sciences and Humanities Research Council of Canada by grants 435-2016-1350 to AD and 435-2019-0608 to NLS, and by a graduate fellowship to TM.
CRediT authorship contribution statement
Talia Morstead: Conceptualization, Methodology, Formal analysis, Writing – original draft, Writing – review & editing. Jason Zheng: Conceptualization, Methodology, Formal analysis, Writing – review & editing. Nancy L. Sin: Conceptualization, Writing – review & editing, Funding acquisition. Jason D. Rights: Conceptualization, Methodology, Formal analysis, Writing – review & editing. Anita DeLongis: Conceptualization, Writing – review & editing, Supervision, Funding acquisition.
Declaration of competing interest
None.
Data availability
Data will be made available on request.
References
- Andresen E.M., Malmgren J.A., Carter W.B., Patrick D.L. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) American Journal of Preventive Medicine. 1994;10(2):77–84. doi: 10.1016/s0749-3797(18)30622-6. [DOI] [PubMed] [Google Scholar]
- Bellingtier J.A., Mund M., Wrzus C. The role of extraversion and neuroticism for experiencing stress during the third wave of the COVID-19 pandemic. Current Psychology. 2021 doi: 10.1007/S12144-021-02600-Y/FIGURES/2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendau A., Kunas S.L., Wyka S., Petzold M.B., Plag J., Asselmann E., Ströhle A. Longitudinal changes of anxiety and depressive symptoms during the COVID-19 pandemic in Germany: The role of pre-existing anxiety, depressive, and other mental disorders. Journal of Anxiety Disorders. 2021;79 doi: 10.1016/J.JANXDIS.2021.102377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolger N., Schilling E.A., Bem D., Coyne J.C., Cor-Nelius S., Downey G., Gouob H., Henderson C., Kessler R., Olson J. Personality and the problems of everyday life: The role of neuroticism in exposure and reactivity to daily stressors. Journal of Personality. 1991;59(3):355–386. doi: 10.1111/J.1467-6494.1991.TB00253.X. [DOI] [PubMed] [Google Scholar]
- Braveman P.A., Cubbin C., Egerter S., Chideya S., Marchi K.S., Metzler M., Posner S. Socioeconomic status in Health Research: One size does not fit all. JAMA. 2005;294(22):2879–2888. doi: 10.1001/JAMA.294.22.2879. [DOI] [PubMed] [Google Scholar]
- Carvalho T., Krammer F., Iwasaki A. The first 12 months of COVID-19: A timeline of immunological insights. Nature Reviews Immunology. 2021;21(4):245–256. doi: 10.1038/s41577-021-00522-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLongis A., Holtzman S. Coping in context: The role of stress, social support, and personality in coping. Journal of Personality. 2005;73(6):1633–1656. doi: 10.1111/j.1467-6494.2005.00361.x. [DOI] [PubMed] [Google Scholar]
- Espejo E.P., Ferriter C.T., Hazel N.A., Keenan-Miller D., Hoffman L.R., Hammen C. Predictors of subjective ratings of stressor severity: The effects of current mood and neuroticism. Stress & Health. 2011;27(1):23–33. doi: 10.1002/SMI.1315. [DOI] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open. 2020;3(9) doi: 10.1001/JAMANETWORKOPEN.2020.19686. e2019686-e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. The Lancet Psychiatry. 2021;8(2):141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher S., Sumner R., Creaven A.-M., O’Súilleabháin P.S., Howard S. Allostatic load and mental health during COVID-19: The moderating role of neuroticism. Brain, Behavior, & Immunity – Health. 2021;16 doi: 10.1016/J.BBIH.2021.100311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunthert K.C., Cohen L.H., Armeli S. The role of neuroticism in daily stress and coping. Journal of Personality and Social Psychology. 1999;77(5):1087–1100. doi: 10.1037/0022-3514.77.5.1087. [DOI] [PubMed] [Google Scholar]
- Irwin M., Artin K.H., Oxman M.N. Screening for depression in the older adult: Criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D) Archives of Internal Medicine. 1999;159(15):1701–1704. doi: 10.1001/ARCHINTE.159.15.1701. [DOI] [PubMed] [Google Scholar]
- Kilby C.J., Sherman K.A., Wuthrich V. Towards understanding interindividual differences in stressor appraisals: A systematic review. Personality and Individual Differences. 2018;135:92–100. doi: 10.1016/J.PAID.2018.07.001. [DOI] [Google Scholar]
- Kroencke L., Geukes K., Utesch T., Kuper N., Back M.D. Neuroticism and emotional risk during the COVID-19 pandemic. Journal of Research in Personality. 2020;89 doi: 10.1016/j.jrp.2020.104038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey B.B. Public health significance of neuroticism. American Psychologist. 2009;64(4):241–256. doi: 10.1037/A0015309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leach C.R., Rees-Punia E., Newton C.C., Chantaprasopsuk S., Patel A.V., Westmaas J.L. Stressors and other pandemic-related predictors of prospective changes in psychological distress. The Lancet Regional Health - Americas. 2021;4 doi: 10.1016/J.LANA.2021.100069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo J., Zhang B., Estabrook R., Graham E.K., Driver C.C., Schalet B.D., Turiano N.A., Spiro A., Mroczek D.K. Personality and health: Disentangling their between-person and within-person relationship in three longitudinal studies. Journal of Personality and Social Psychology. 2022;122(3):493–522. doi: 10.1037/pspp0000399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrae R.R. Controlling neuroticism in the measurement of stress. Stress Medicine. 1990;6(3):237–241. doi: 10.1002/SMI.2460060309. [DOI] [Google Scholar]
- McLaughlin K.A. The public health impact of major depression: A call for interdisciplinary prevention efforts. Prevention Science. 2011;12(4):361–371. doi: 10.1007/s11121-011-0231-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morstead T., Zheng J., Sin N.L., King D.B., DeLongis A. Adherence to recommended preventive behaviors during the COVID-19 pandemic: The role of empathy and perceived health threat. Annals of Behavioral Medicine. 2022;56(4):381–392. doi: 10.1093/abm/kaab107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nudelman G., Kamble S.V., Otto K. Can personality traits predict depression during the COVID-19 pandemic? Social Justice Research. 2021;34(2):218–234. doi: 10.1007/s11211-021-00369-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park C.L., Finkelstein-Fox L., Russell B.S., Fendrich M., Hutchison M., Becker J. Americans’ distress early in the COVID-19 pandemic: Protective resources and coping strategies. Psychological Trauma: Theory, Research, Practice, and Policy. 2021;13(4):422–431. doi: 10.1037/tra0000931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinheiro J., Bates D., R Core Team . 2021. nlme: Linear and nonlinear mixed effects models.https://CRAN.R-project.org/package=nlme [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; 2021. R: A language and environment for statistical computing.https://www.r-project.org/ [Google Scholar]
- Raina P., Wolfson C., Griffith L., Kirkland S., McMillan J., Basta N., Joshi D., Oz U.E., Sohel N., Maimon G., Thompson M., Costa A., Anderson L., Balion C., Yukiko A., Cossette B., Levasseur M., Hofer S., Paterson T., Cosco T.… A longitudinal analysis of the impact of the COVID-19 pandemic on the mental health of middle-aged and older adults from the Canadian Longitudinal Study on Aging. Nature Aging. 2021;1(12):1137–1147. doi: 10.1038/s43587-021-00128-1. [DOI] [PubMed] [Google Scholar]
- Rammstedt B., John O.P. Measuring personality in one minute or less: A 10-item short version of the Big Five Inventory in English and German. Journal of Research in Personality. 2007;41(1):203–212. doi: 10.1016/J.JRP.2006.02.001. [DOI] [Google Scholar]
- Raudenbush S.W., Bryk A.S. 2nd ed. Sage; 2002. Hierarchical linear models: Applications and data analysis methods. [Google Scholar]
- Rights J.D., Sterba S.K. Quantifying explained variance in multilevel models: An integrative framework for defining R-squared measures. Psychological Methods. 2019;24(3):309–338. doi: 10.1037/MET0000184. [DOI] [PubMed] [Google Scholar]
- RStudio Team . RStudio, PBC; 2021. RStudio: Integrated development for R.http://www.rstudio.com/ [Google Scholar]
- Santomauro D.F., Herrera A.M.M., Shadid J., Zheng P., Ashbaugh C., Pigott D.M., Ferrari A.J.… Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet. 2021;398(10312):1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw M., Rights J.D., Sterba S.S., Flake J.K. r2mlm: An R package calculating R-squared measures for multilevel models. Behavior Research Methods. 2022 doi: 10.3758/s13428-022-01841-4. [DOI] [PubMed] [Google Scholar]
- Suls J., Martin R. The daily life of the garden-variety neurotic: Reactivity, stressor exposure, mood spillover, and maladaptive coping. Journal of Personality. 2005;73(6):1485–1510. doi: 10.1111/J.1467-6494.2005.00356.X. [DOI] [PubMed] [Google Scholar]
- Thalmayer A.G., Saucier G., Eigenhuis A. Comparative validity of brief to medium-length Big Five and Big Six personality questionnaires. Psychological Assessment. 2011;23(4):995–1009. doi: 10.1037/A0024165. [DOI] [PubMed] [Google Scholar]
- Webster P. COVID-19 timeline of events. Nature Medicine. 2021;27(12):2054–2055. doi: 10.1038/s41591-021-01618-w. [DOI] [PubMed] [Google Scholar]
- West S.G., Ryu E., Kwok O.M., Cham H. Multilevel modeling: Current and future applications in personality research. Journal of Personality. 2011;79(1):2–50. doi: 10.1111/j.1467-6494.2010.00681.x. [DOI] [PubMed] [Google Scholar]
- Zheng J., Morstead T., Sin N., Klaiber P., Umberson D., Kamble S., DeLongis A. Psychological distress in North America during COVID-19: The role of pandemic-related stressors. Social Science & Medicine. 2021;270 doi: 10.1016/j.socscimed.2021.113687. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.