Abstract
The emergence of the monkeypox outbreak in early 2022 has posed a new global health threat. As of July 8, 2022, 9069 laboratory-confirmed cases have been reported, and most of them are from non-endemic countries. The monkeypox virus is an enveloped double-stranded DNA virus, and preliminary genetic data suggest that the 2022 monkeypox virus belongs to the West African clade. In the current outbreak, human-to-human transmission has been the primary transmission mode. Although direct skin-to-skin contact with lesions during sexual activities can spread the virus, it remains unclear whether monkeypox can spread through sexual contact, specifically through contaminated body fluids. The typical presentation of monkeypox includes prodromal symptoms, followed by a rash that usually begins within 1–3 days of symptom onset, and the skin lesions can last for 2–4 weeks and then gradually resolve. However, the monkeypox outbreak in 2022 may exhibit atypical features. A definite diagnosis of monkeypox virus infection requires nucleic acid amplification testing via the polymerase chain reaction method. Supportive care is essential, and antiviral therapy is not considered for all affected patients, but recommended for those at highrisk for severe diseases. The mitigation of monkeypox outbreaks include enhanced case detection, case isolation, contact tracing, and post-exposure vaccination. In conclusion, the current monkeypox outbreak is a new threat during the COVID-19 pandemic. Clinicians should be aware of this new situation, which presents a different scenario from those of prior outbreaks. Global health systems should develop effective strategies to mitigate the spread of monkeypox.
Keywords: Monkeypox, COVID-19, Outbreak, Public health
Introduction
As of 18 July, 2022, more than 559 million cases of coronavirus disease (COVID-19) have been reported since the first outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in China. This outbreak has caused more than 6 million deaths globally.1 , 2 However, the impact of COVID-19 has been mitigated via the development of effective vaccines, antiviral agents, and other treatments.3, 4, 5, 6, 7, 8, 9 The emergence of the monkeypox outbreak in 2022 has posed another global health threat.10 Between January 1 and June 22, 2022, a total of 3413 laboratory-confirmed cases and 1 death have been reported to the World Health Organization (WHO) from 50 countries or territories in five WHO Regions.11 As of July 8, the cumulative confirmed case numbers increased to 9069.12 Because the rapid increase of monkeypox cases, WHO declared the escalating global monkeypox outbreak a Public Health Emergency of International Concern on Juy 23, 2022.
Monkeypox was first identified in colonies of monkeys in 1958. It was later detected in a 9-month child in a remote village in the Democratic Republic of Congo in 1970.13 Before the current outbreak, monkeypox was typically found in central and west Africa, where rodents live in tropical rainforests and may carry the virus. Occasionally, monkeypox was found in countries outside central and west Africa, owing to travel from regions where monkeypox is endemic. Notably, monkeypox in non-endemic areas not linked to travel from endemic countries is atypical, and these atypical cases have become increasingly prevalent.
Monkeypox is not typically highly contagious because it requires close physical contact with someone carrying the virus. Although the risk to the general public was considered low previously, the WHO is responding to this outbreak as a high priority to avoid further spread.11 In the 2022 outbreak, the reported cases did not have apparent links to travel history from endemic countries, or contact history with infected animals. Therefore, as the current outbreak is atypical and different from previous cases, a comprehensive understanding of monkeypox, including causative pathogen, possible transmission modalities, current epidemiology, risk factors, clinical manifestations, treatment, and prevention, is urgently needed. Hence, this review aims to provide updated information.
The virus
The monkeypox virus is a member of the Orthopoxvirus genus of the Poxviridae family. In the Orthopoxvirus genus, only four pathogens, including monkeypox virus, cowpox virus, vaccinia virus, and the eradicated variola virus—the causative agent of smallpox—have reportedly caused human infection.14
The monkeypox virus is an enveloped double-stranded DNA virus that comprises two genetic clades: Central African (Congo Basin) clade and West African clade. These two clades are divided geographically by Cameroon, the only country with both virus clades. The West African clade has been found in outbreaks in Nigeria, Liberia, Ivory Coast, Sierra Leone, and the USA (imported from Ghana). The Central African clade has been found in Gabon, Cameroon, the Republic of Congo, Central African Republic, Sudan, and the Democratic Republic of Congo.15, 16, 17, 18 In addition to geographical differences, these two clades significantly differ in epidemiologic and clinical characteristics. The Central African clade, endemic in the Democratic Republic of Congo, where more than 2000 suspected cases are reported yearly, is more prevalent than the West African clade.19 Compared with the West African clade, the Central African strain could be associated with more severe disease and higher transmissibility. The West African clade is associated with a low case fatality rate (CFR) of <1%, and no human-to-human transmission has ever been documented. In contrast, the CFR of the Congo Basin clade could be up to 11%, and documented human-to-human transmissions up to six sequential events have been reported.15 Similarly, a systematic review found a significant difference in CFR between the Central African clade (10.6%; 95% confidence interval [CI]: 8.4%–13.3%) and West African clade (3.6%; 95% CI: 1.7%–6.8%).20
Isidro et al. showed the first genome sequence of a case recently detected in Portugal. The authors used shotgun metagenomics for rapid reconstruction and phylogenomic characterization.21 Preliminary genomic data suggest that the 2022 monkeypox virus belongs to the West African clade21, 22, 23 and is most closely related to monkeypox viruses that spread from Nigeria to the UK, Israel, and Singapore in 2018 and 2019.21 , 24 , 25
Definition of the reported monkeypox
According to the WHO case definition, the criteria for a suspected case of monkeypox include (1) A person of any age presenting since 01 January 2022 with an unexplained acute rash or one or more acute skin lesions; (2) one of the prodromal symptom or symptoms of monkeypox infection—headache, acute onset of fever, lymphadenopathy, myalgia, back pain, and asthenia; and (3) the clinical picture cannot be fully explained by the common causes of an acute rash or skin lesions.26 A probable case is defined as a person meeting the case definition for a suspected case and one of the following criteria: (1) has an epidemiological link to a probable or confirmed case of monkeypox in the 21 days before symptom onset; (2) has had multiple or anonymous sexual partners in the 21 days before symptom onset; (3) has detectable levels of anti-orthopoxvirus IgM antibody or a four-fold rise in IgG antibody titer based on acute (up to days 5–7) and convalescent (day 21 onwards) samples but without recent smallpox or monkeypox vaccination or other known exposure; or (4) has a positive test result for orthopoxviral infection.26 A confirmed case was defined as a patient with a laboratory-confirmed monkeypox infection on polymerase chain reaction (PCR) testing or sequencing.26 , 27
Transmission
Many animal species are susceptible to the monkeypox virus, including rope squirrels, tree squirrels, Gambian pouched rats, dormice, and non-human primates. Although rodents are considered a potential natural reservoir of the monkeypox virus, the most important natural reservoir remains to be identified. The animal-to-human transmission of the monkeypox virus can occur through direct contact with an infected animal's blood, body fluid, skin, or mucosal lesions. In addition, consuming inappropriately cooked meat or products of infected animals could be another possible transmission route. Close physical contact is the main route of human-to-human transmission, which may require prolonged close contact. Transmission may occur through contact with skin lesions of infected patients, contaminated objects, and respiratory droplets. Rarely, congenital monkeypox results from viral transmission through the placenta. Because there are strict protocols for screening blood donations, there have been no reports of monkeypox spreading through blood transfusions. In the current outbreak, monkeypox rashes are commonly found in the genital area and likely contribute to transmission during sexual contact. In addition, monkeypox rashes can resemble those of sexually transmitted diseases, including herpes and syphilis. This may explain why several cases in the current outbreak have been identified among men seeking care in sexual health clinics.22 , 28, 29, 30 Although direct skin-to-skin contact during sexual activities can spread the virus, it remains unclear whether the monkeypox virus can spread through sexual contact, specifically through semen or vaginal fluids.
Epidemiology
Before the current monkeypox outbreak
Since the first report of human monkeypox in 1970,13 the number of human monkeypox cases has been on the rise, with the most dramatic increase occurring in the Democratic Republic of Congo. Before 2020, the incidence of monkeypox reportedly ranged from 0.64 per 100,000 in 2001 to as high as 50 per 10,000 in 2016.20 A systemic review involving 66 articles before September 2020 found that human monkeypox has been reported in 10 African countries, including the Democratic Republic of Congo, Nigeria, Côte d'Ivoire, Liberia, Cameroon, Sierra Leone, Gabon, Central African, Congo, and South Sudan and four non-African countries including Singapore, Israel, the UK, and the USA.20 Among these countries, the Democratic Republic of Congo is the most affected country.20
Index case of the current monkeypox outbreak
The current outbreak initiated from the first reported case in May 2022.31 The patient developed a rash on April 29, 2022, in Nigeria; departed Nigeria on May 3; and arrived in the UK on May 4. Monkeypox (West African clade) was confirmed on reverse transcriptase (RT)-PCR testing of a vesicular swab on May 6. Although extensive contact tracing has been undertaken to identify exposed contacts in healthcare settings, the community, and on international flights, no compatible symptoms have been reported as of May 11. Meanwhile, the patient did not report contact with anyone with a rash illness or known monkeypox in Nigeria; thus, the source of infection remains unknown.31
Current monkeypox outbreak
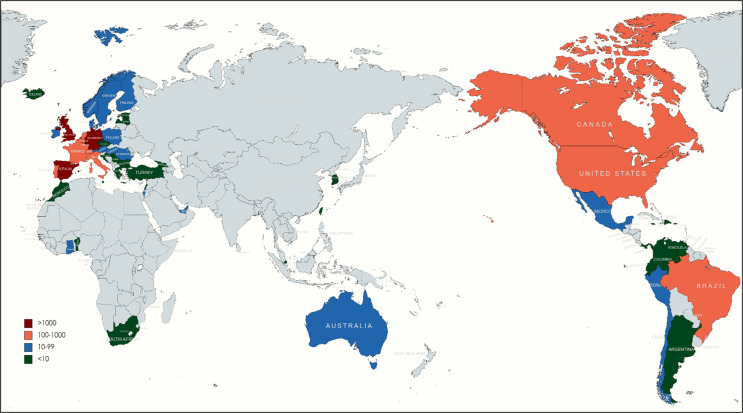
Several days after the index case was reported, two laboratory-confirmed and one probable case were identified within the same household on May 13. Four additional confirmed cases were reported among Sexual Health Service attendees (men who have sex with men) presenting with a vesicular rash illness on May 15 in the UK.32 As in the first case, the source of infection could not be identified, and local transmission in the UK was suspected.32 As of May 21, 92 laboratory-confirmed cases and 28 suspected cases of monkeypox were reported in 12 non-endemic countries, including Australia, Belgium, Canada, France, Germany, Italy, the Netherlands, Portugal, Spain, Sweden, the UK, and the USA.28 Although these cases had no direct travel links to an endemic area, many of them were identified among men who have sex with men seeking care in primary care and sexual health clinics.28 A similar finding was reported by other studies.21 , 23 , 29 , 30 , 33, 34, 35 Among 86 monkeypox cases reported during May 7–25 in the UK, only 1 case is known to have a travel history to a monkeypox endemic country; 79 patients were men and 66 of them reported being gay, bisexual, or other men who have sex with men.30 In Italy, four young adult men were reported to have a condomless sexual intercourse, and seminal fluid samples were positive for monkeypox viral DNA.29 In the USA, one investigation identified 17 cases, and most cases (n = 16) were gay, bisexual, or men who have sex with men.23 Although most current outbreaks occurred in European regions, more and more cases have been reported in the American, African, Eastern Mediterranean, and Western Pacific regions (Fig. 1 ).12
Figure 1.
Global distribution of confirmed monkeypox cases (as of July 8, 2022).
First case of monkeypox in Taiwan
In addition to Western countries, Africa, and the Eastern Mediterranean region, monkeypox cases have been reported in several Asian countries, including South Korea, Singapore, and Taiwan.12 In Taiwan, the first case was a young man who was studying in Germany and developed symptoms on June 20, 4 days after he arrived in Taiwan.36 His symptoms included fever, sore throat, muscle pain, swollen lymph nodes in the groin, and rash. On June 24, 2022, he tested positive for monkeypox, which was reported as a confirmed case. Thus, he was admitted to a negative pressure room and isolated until symptom resolution. Meanwhile, 19 people were listed as close contacts, including 10 medical workers and 2 relatives. Although none developed any symptoms, close observation was required to monitor their health for 21 days following exposure.36
Estimated burden
Bisanzioa et al. established a projected model based on a simulated population of 50 million people with socioeconomic and demographic characteristics typical of a high-income European country. They estimated that the introduction of 300 cases could result in 402 secondary cases without interventions. The median duration of these outbreaks for this scenario would be 37 (95% CI: 19–121) weeks following the introduction of 300 cases.37 Contact tracing with isolation of symptomatic cases would reduce the number of secondary cases by 68.9%. Moreover, adding ring vaccination to contact tracing would further reduce the number of secondary cases by 86.1%.37 This projection of monkeypox burden was compatible with the WHO's risk assessment of overall public health risk at a global level as currently moderate.38
Association between COVID-19 and monkeypox outbreaks
The rise in the number of monkeypox cases during the COVID-19 pandemic makes the situation more complicated. The clinical manifestations of SARS-CoV-2 infections are protean, including respiratory and extra-respiratory symptoms.39 COVID-19 may occasionally present with skin manifestations, such as an erythematous maculopapular rash, erythema multiforme, vesicular rash, vascular livedo reticularis, figurate erythema, or a flexural rash.40 Because COVID-19 and atypical monkeypox in the current outbreak may share a similar clinical picture, clinicians should remain alert to these two diseases during this period. In addition, co-infection with SARS-CoV-2 and other viruses is not uncommon.41 Therefore, the potential for co-infection of SARS-CoV-2 and the monkeypox virus cannot be neglected. However, the changes related to infectivity patterns, severity, management, or response to vaccination in one or both diseases are unknown. Therefore, further investigation is warranted to determine the association between COVID-19 and monkeypox outbreaks.
Risk factors
In addition to those who have close contact with patients with monkeypox or contact with an infected animal, immunocompromised patients may also be at risk of acquiring monkeypox.15 , 42, 43, 44 In the current outbreak, a small series of 27 confirmed cases in Portugal found more than half (n = 14) had human immunodeficiency virus (HIV) infection.22 Several studies also reported the development of monkeypox in patients with HIV during this outbreak.45 The main reason could be those HIV cases carry the same risk as men who have sex with men. Moreover, a recent analysis of 124 cases identified several preliminary risk factors, including being a young man, having sex with other men, engaging in risky behaviors and activities such as condomless sex, and HIV positivity.46 Finally, healthcare workers could have a higher risk owing to a longer duration of virus exposure.47
Clinical manifestations
The mean incubation period of monkeypox was 8.5 (95% CI: 4.2–17.3) days.48 Prodromal symptoms of monkeypox include fever, chills, sore throat, cough, headache, myalgia, blepharoconjunctivitis, lethargy, and adenopathy, followed by rashes that usually begin within 1–3 days of symptom onset. The rash typically appears on the face and then becomes generalized with the involvement of the palms and soles. Rashes can also be found in the mouth, genitals, and eyes. These lesions can be flat or slightly raised; filled with clear or yellowish fluid; and then crust, dry, and fall off. The number of skin lesions can range from a few to several thousands. The evolution of rashes is similar to that of smallpox, from macules, to papules, vesicles, pustules and scabs evolving over 2–4 weeks. Skin lesions typically last 2–4 weeks and gradually resolve without treatment. These dermatological characteristics of monkeypox with lymphadenopathy are different from those of chickenpox and smallpox and help clinicians make a differential diagnosis (Table 1 ). However, the current monkeypox outbreak in 2022 can have atypical features, including (a) only a few or even single lesions or the absence of skin lesions in some cases; (b) lesions mostly located in genital and perianal sites and presenting with anal pain and bleeding; (C) skin lesions restricted to genital, perineal or perianal areas; (D) asynchronous lesions, ranging from single or clustered spots to umbilicated papules with progressive central ulceration, and, finally, to scabs; (E) absence of prodromal symptoms, such as fever, malaise, and headache before the development of a rash; (F) presence of herald skin lesions at the point of sexual contact in some patients (Table 2 ).11 , 22 , 29 , 46 , 49
Table 1.
Clinical manifestations of typical monkeypox, chickenpox, and smallpox.
| Characteristic | Monkeypox | Chickenpox | Smallpox |
|---|---|---|---|
| Causative virus | Monkeypox virus | Varicella-zoster virus | Variola virus |
| Fever before rashes | 1–3 days | 1–2 days | 2–4 days |
| Dermatologic presentation | One stage in slow development | Multiple stages in rapid development | Multiple stages in rapid development |
| Initial site(s) | Face | Chest, back, and face | Tongue and moth |
| Involvement of palms and soles | Yes | No | Yes |
| Lymphadenopathy | Yes | No | No |
| Appearance of symptoms post-exposure | 5–21 days | 10–21 days | 7–19 days |
| Duration of illness | 2–4 weeks | 4–7 days | Up to 5 weeks |
| Vaccination | Smallpox vaccine | Chickenpox vaccine | Smallpox vaccine |
Table 2.
Atypical pictures of the current monkeypox outbreak, 2022.
| Epidemiology |
|---|
| ●Absence of epidemiological links to traveling to endemic countries |
| ●Outbreak in non-endemic countries |
| ●Sexual transmission via semen/vaginal fluids (uncertain) |
| Prodromal symptom |
| ●Appearance of rashes before the onset of fever, malaise, and other constitutional symptoms or even absence of a prodromal period |
| Skin lesions |
| ●Limited skin lesions or the absence of skin lesions |
| ●Mostly located in genital and perianal sites |
| ●No further spread from genital or perineal/perianal lesions |
| ●Asynchronous lesions, ranging from single or clustered spot to umbilicated papule with progressive central ulceration, and, finally, to scabs |
| ●Appearance of herald skin lesions at sexual contact points |
Laboratory diagnosis
Nucleic acid amplification testing can be generic to orthopoxvirus or specific to monkeypoxvirus. Definite diagnosis of monkeypox virus infection requires nucleic acid amplification testing using real-time or conventional PCR for the detection of viral DNA. Skin lesions, including swabs of the lesion surface or exudate, roofs from more than one lesion, or lesion crusts, are recommended clinical specimens for laboratory test. Serological testing for IgG, which may become detectable 8 days after symptom onset, requires paired acute and convalescent sera. Anti-monkeypox virus IgM may be positive within 5 days of presentation. However, antibody detection in plasma or serum should not be used alone to diagnose monkeypox.50 , 51
Treatment and outcomes
Currently, there is no standard-of-care treatment for monkeypox except supportive care.52 , 53 Although smallpox antivirals with poxvirus activity, such as cidofovir, brincidofovir, and tecovirimat, are active against the monkeypox virus, these antivirals would most likely be reserved for the treatment of severe cases or immunocompromised persons.53 Additionally, vaccinia immune globulin, a hyperimmune globulin licensed by the Food and Drug Administration of the United States (US FDA) for the treatment of certain complications of vaccinia vaccination, may be recommended for severe cases.53
Monkeypox is usually a self-limiting disease; however, newborns, children, and people with underlying immune deficiencies may be at risk of more serious illness and death.20 , 46 , 54 , 55 Complications from severe cases of monkeypox include skin, pneumonia, altered sensorium, and eye infections that can lead to loss of vision. A systematic review conducted before the current outbreak reported that the overall CFR was approximately 8.7% but CFR was different in different areas, ranging from 0 to 11%. However, this may be overestimated because surveillance in endemic countries is limited.20 In the current outbreak, only one death was reported in Nigeria in the second quarter of 2022, and the estimated CFR was only 0.03% (1/3413).11
Prevention and vaccination
Monkeypox can spread to people when they come into physical contact with infected animals. The animal hosts include rodents and primates. The risk of zoonotic transmission can be reduced by avoiding unprotected contact with wild animals, especially those sick or dead (including their meat and blood). In endemic countries, where animals may carry monkeypox, food containing animal meat or parts should be cooked thoroughly before eating.
Individuals with monkeypox are infectious and have symptoms. Rashes, bodily fluids (such as fluid, pus, or blood from skin lesions), and scabs are particularly infectious. Clothing, bedding, towels, or objects such as eating utensils/dishes that have been contaminated with the virus from an infected person can also infect others. Ulcers, lesions, and sores in the mouth can also be infectious, meaning that the virus can spread through saliva and respiratory droplets. Because close physical contact is the primary route for human-to-human transmission, limiting contact with people who have suspected or confirmed monkeypox is the key to prevention. People with multiple sexual partners, including those living with HIV-infected patients, are encouraged to reduce their risk of exposure to monkeypox by avoiding close contact with anyone with symptoms. Reducing the number of sexual partners also reduces the risk of infection.
Healthcare workers who take care of patients with monkeypox should encourage them to self-isolate and cover any skin lesions. A medical mask is essential when physically close to the patient, especially if the patient is coughing or has lesions in the mouth. Avoid skin-to-skin contact whenever possible, and use disposable gloves while directly contacting skin lesions. Hand hygiene with soap and water or an alcohol-based hand rub is needed, especially after contact with infected people and their clothes, bed sheets, towels, and other items or surfaces they have touched or that might have come into contact with their rash or respiratory secretions. Nörz et al. examined surfaces in rooms occupied by two monkeypox patients on their fourth hospitalization day. Contamination with up to 105 viral copies/cm2 on inanimate surfaces was detected.56 Regarding the concern of possible fomite transmission, thoroughly cleaning and disinfecting any potentially contaminated surfaces and disposing contaminated waste are essential.
People vaccinated against smallpox in the past may have some protection against monkeypox and its associated manifestations.57 , 58 However, original smallpox vaccines are no longer available, and people aged <40–50 years are unlikely to have been vaccinated. The US FDA approved JYNNEOSTM (also known as IMVAMUNE, IMVANEX, MVA-BN) in 2019 to prevent monkeypox in adults aged ≥18 years at high risk for smallpox or monkeypox.59 In addition, this vaccine has been approved in Europe for smallpox, although the UK has used it off-label in response to monkeypox cases. ACAM2000®, another smallpox vaccine, was licensed by the FDA in August 2007 and has been indicated for active immunization against smallpox disease for persons determined to be at high risk for smallpox infection. Because the Centers for Disease Control and Prevention has the emergency access to investigational new drugs, it allows the use of ACAM2000® for non-variola Orthopoxvirus infections, such as monkeypox, during an outbreak.60
Given the experience of combating COVID-19, all healthcare authorities are well versed in effectively mitigating an infectious disease.5 , 61, 62, 63, 64 Many infection control and prevention measures have been adopted to contain the current monkeypox outbreak. These policies include early identification of cases, contact tracing, travel and gathering restrictions according to the risk of infection, establishment of an adequate quarantine window, appropriate personal protective equipment provision for healthcare workers, avoidance of stigmatizing messaging circulating online related to monkeypox, and development of effective vaccines and postexposure prophylaxis.65 , 66
Unknowns
As of July 8, 2022, 9069 laboratory-confirmed cases have been reported, and most of them are from non-endemic countries (Supplemental Table). This indicates that person-to-person transmission occurred, with most cases seemingly unlinked to travel from an endemic country and the appearance of multiple unlinked clusters. This suggests that undetected chains of transmission occurred. Another unusual characteristic is that many cases of monkeypox are recognized among men who have sex with men. Many of these cases were diagnosed at sexually transmitted infection clinics. The virus may or may not spread sexually in this group and may be transmitted through skin-to-skin contact or respiratory droplets. Another unresolved issue is the cause of this outbreak, which is much larger and more widespread than previous monkeypox outbreaks outside Africa. Studies are underway in affected countries to determine the source of infection for each identified case. Actions were taken to provide medical care and limit the further spread of the disease.
Conclusion
The current monkeypox outbreak has become a new threat during the COVID-19 pandemic. Clinicians should be aware of this new situation, which has clinical features different from dermatological diseases with pustular or “pox” lesions (Table 1). Primary care physicians, urgent care physicians, emergency medicine physicians, dermatologists, and those working in sexually transmitted infection clinics may be most likely to encounter new patients with monkeypox should they continue to appear. Global health systems should develop effective strategies to mitigate the spread of monkeypox. However, precedence should be given to containment efforts that should rely on enhanced case finding, case isolation, contact tracing, and vaccination.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jmii.2022.07.004.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.World Health Organization https://covid19.who.int/ Accessed on July 19, 2022.
- 2.Lai C.C., Liu Y.H., Wang C.Y., Wang Y.H., Hsueh S.C., Yen M.Y., et al. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): facts and myths. J Microbiol Immunol Infect. 2020;53:404–412. doi: 10.1016/j.jmii.2020.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shao W., Zhang W., Fang X., Yu D., Wang X. Challenges of SARS-CoV-2 omicron variant and appropriate countermeasures. J Microbiol Immunol Infect. 2022;55:387–394. doi: 10.1016/j.jmii.2022.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai C.C., Chen I.T., Chao C.M., Lee P.I., Ko W.C., Hsueh P.R. COVID-19 vaccines: concerns beyond protective efficacy and safety. Expert Rev Vaccines. 2021;20:1013–1025. doi: 10.1080/14760584.2021.1949293. [DOI] [PubMed] [Google Scholar]
- 5.Lin K.Y., Wu P.Y., Liu W.D., Sun H.Y., Hsieh S.M., Sheng W.H., et al. Effectiveness of COVID-19 vaccination among people living with HIV during a COVID-19 outbreak. J Microbiol Immunol Infect. 2022;55:535–539. doi: 10.1016/j.jmii.2022.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lai C.C., Chao C.M., Hsueh P.R. Clinical efficacy of anti-viral agents against coronavirus disease 2019: a systematic review of randomized controlled trials. J Microbiol Immunol Infect. 2021;54:767–775. doi: 10.1016/j.jmii.2021.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang C.J., Wei Y.J., Chang H.L., Chang P.Y., Tsai C.C., Chen Y.H., et al. Remdesivir use in the coronavirus disease 2019 pandemic: a mini-review. J Microbiol Immunol Infect. 2021;54:27–36. doi: 10.1016/j.jmii.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shankar-Hari M., Vale C.L., Godolphin P.J., Fisher D., Higgins J.P.T., Spiga F., et al. Association between administration of IL-6 antagonists and mortality among patients hospitalized for COVID-19: a meta-analysis. JAMA. 2021;326:499–518. doi: 10.1001/jama.2021.11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lai C.C., Chen C.H., Wang C.Y., Chen K.H., Wang Y.H., Hsueh P.R. Clinical efficacy and safety of remdesivir in patients with COVID-19: a systematic review and network meta-analysis of randomized controlled trials. J Antimicrob Chemother. 2021;76:1962–1968. doi: 10.1093/jac/dkab093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahase E. Seven monkeypox cases are confirmed in England. BMJ. 2022;377:o1239. doi: 10.1136/bmj.o1239. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON396 Accessed on July 2, 2022.
- 12.https://ourworldindata.org/monkeypox Accessed on July 10, 2022.
- 13.Ladnyj I.D., Ziegler P., Kima E. A human infection caused by monkeypox virus in Basankusu Territory, Democratic Republic of the Congo. Bull World Health Organ. 1972;46:593–597. [PMC free article] [PubMed] [Google Scholar]
- 14.Sklenovská N., Van Ranst M. Emergence of monkeypox as the most important orthopoxvirus infection in humans. Front Public Health. 2018;6:241. doi: 10.3389/fpubh.2018.00241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jezek Z., Szczeniowski M., Paluku K.M., Mutombo M. Human monkeypox: clinical features of 282 patients. J Infect Dis. 1987;156:293–298. doi: 10.1093/infdis/156.2.293. [DOI] [PubMed] [Google Scholar]
- 16.Likos A.M., Sammons S.A., Olson V.A., Frace A.M., Li Y., Olsen-Rasmussen M., et al. A tale of two clades: monkeypox viruses. J Gen Virol. 2005;86:2661–2672. doi: 10.1099/vir.0.81215-0. [DOI] [PubMed] [Google Scholar]
- 17.Chen N., Li G., Liszewski M.K., Atkinson J.P., Jahrling P.B., Feng Z., et al. Virulence differences between monkeypox virus isolates from West Africa and the Congo basin. Virology. 2005;340:46–63. doi: 10.1016/j.virol.2005.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sbrana E., Xiao S.Y., Newman P.C., Tesh R.B. Comparative pathology of North American and central African strains of monkeypox virus in a ground squirrel model of the disease. Am J Trop Med Hyg. 2007;76:155–164. [PubMed] [Google Scholar]
- 19.Mwamba D., Kebela B., Shongo R., Pukuta E., Kayembe N. Profil épidemiologique du monkeypox en RDC, 2010–2014. Ann Afr Med. 2014;8:1855–1860. [Google Scholar]
- 20.Bunge E.M., Hoet B., Chen L., Lienert F., Weidenthaler H., Baer L.R., et al. The changing epidemiology of human monkeypox-A potential threat? A systematic review. PLoS Neglected Trop Dis. 2022;16 doi: 10.1371/journal.pntd.0010141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Isidro J., Borges V., Pinto M., Sobral D., Santos J.D., Nunes A., et al. Phylogenomic characterization and signs of microevolution in the 2022 multi-country outbreak of monkeypox virus. Nat Med. 2022 Jun 24 doi: 10.1038/s41591-022-01907-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perez Duque M., Ribeiro S., Martins J.V., Casaca P., Leite P.P., Tavares M., et al. Ongoing monkeypox virus outbreak, Portugal, 29 April to 23 May 2022. Euro Surveill. 2022;27:2200424. doi: 10.2807/1560-7917.ES.2022.27.22.2200424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Minhaj F.S., Ogale Y.P., Whitehill F., Schultz J., Foote M., Davidson W., et al. Monkeypox outbreak - nine States, may 2022. MMWR Morb Mortal Wkly Rep. 2022;71:764–769. doi: 10.15585/mmwr.mm7123e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Simpson K., Heymann D., Brown C.S., Edmunds W.J., Elsgaard J., Fine P., et al. Human monkeypox - after 40 years, an unintended consequence of smallpox eradication. Vaccine. 2020;38:5077–5081. doi: 10.1016/j.vaccine.2020.04.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mauldin M.R., McCollum A.M., Nakazawa Y.J., Mandra A., Whitehouse E.R., Davidson W., et al. Exportation of monkeypox virus from the african continent. J Infect Dis. 2022;225:1367–1376. doi: 10.1093/infdis/jiaa559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization https://www.who.int/emergencies/outbreak-toolkit/disease-outbreak-toolboxes/monkeypox-outbreak-toolbox Accessed on July 6, 2022.
- 27.https://www.gov.uk/guidance/monkeypox-case-definitions Accessed on July 6, 2022.
- 28.World Health Organization https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON385 Accessed on July 4, 2022.
- 29.Antinori A., Mazzotta V., Vita S., Carletti F., Tacconi D., Lapini L.E., et al. Epidemiological, clinical and virological characteristics of four cases of monkeypox support transmission through sexual contact, Italy, May 2022. Euro Surveill. 2022;27:2200421. doi: 10.2807/1560-7917.ES.2022.27.22.2200421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vivancos R., Anderson C., Blomquist P., Balasegaram S., Bell A., Bishop L., et al. Community transmission of monkeypox in the United Kingdom, April to may 2022. Euro Surveill. 2022;27:2200422. doi: 10.2807/1560-7917.ES.2022.27.22.2200422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON381 Accessed on July 4, 2022.
- 32.World Health Organization https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON383 Accessed on July 4, 2022.
- 33.Ferraro F., Caraglia A., Rapiti A., Cereda D., Vairo F., Mattei G., et al. Letter to the editor: multiple introductions of MPX in Italy from different geographic areas. Euro Surveill. 2022;27 doi: 10.2807/1560-7917.ES.2022.27.23.2200456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vallée A., Farfour E., Zucman D. Monkeypox virus: a novel sexually transmitted disease? A case report from France. Trav Med Infect Dis. 2022;49 doi: 10.1016/j.tmaid.2022.102394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mileto D., Riva A., Cutrera M., Moschese D., Mancon A., Meroni L., et al. New challenges in human monkeypox outside Africa: a review and case report from Italy. Trav Med Infect Dis. 2022;49 doi: 10.1016/j.tmaid.2022.102386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.https://focustaiwan.tw/society/202206240015 Accessed on July 6, 2022.
- 37.Bisanzio D., Reithinger R. Projected burden and duration of the 2022 Monkeypox outbreaks in non-endemic countries. Lancet Microbe. 2022;S2666S5247(22):183–185. doi: 10.1016/S2666-5247(22)00183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.World Health Organization https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON393 Accessed on July 4, 2022.
- 39.Lai CC, Ko WC, Lee PI, Jean SS, Hsueh PR. Extra-respiratory manifestations of COVID-19. Int J Antimicrob Agents;56:106024. [DOI] [PMC free article] [PubMed]
- 40.Mohammed G.F., Al-Dhubaibi M.S., Atef L. Cutaneous manifestations of coronavirus disease 2019: skin narratives and dialogues. J Clin Aesthet Dermatol. 2022;15:E77–E81. [PMC free article] [PubMed] [Google Scholar]
- 41.Lai C.C., Wang C.Y., Hsueh P.R. Co-infections among patients with COVID-19: the need for combination therapy with non-anti-SARS-CoV-2 agents? J Microbiol Immunol Infect. 2020;53:505–512. doi: 10.1016/j.jmii.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Parker S., Nuara A., Buller R.M., Schultz D.A. Human monkeypox: an emerging zoonotic disease. Future Microbiol. 2007;2:17–34. doi: 10.2217/17460913.2.1.17. [DOI] [PubMed] [Google Scholar]
- 43.Eltvedt A.K., Christiansen M., Poulsen A. A case report of monkeypox in a 4-year-old boy from the DR Congo: challenges of diagnosis and management. Case Rep Pediatr. 2020;2020 doi: 10.1155/2020/8572596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ogoina D., Izibewule J.H., Ogunleye A., Ederiane E., Anebonam U., Neni A., et al. The 2017 human monkeypox outbreak in Nigeria-Report of outbreak experience and response in the Niger Delta University Teaching Hospital, Bayelsa State, Nigeria. PLoS One. 2019;14 doi: 10.1371/journal.pone.0214229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hammerschlag Y., MacLeod G., Papadakis G., Adan Sanchez A., Druce J., Taiaroa G., et al. Monkeypox infection presenting as genital rash, Australia, May 2022. Euro Surveill. 2022;27:2200411. doi: 10.2807/1560-7917.ES.2022.27.22.2200411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bragazzi N.L., Kong J.D., Mahroum N., Tsigalou C., Khamisy-Farah R., Converti M., et al. Epidemiological trends and clinical features of the ongoing monkeypox epidemic: a preliminary pooled data analysis and literature review. J Med Virol. 2022 Jun 12 doi: 10.1002/jmv.27931. [DOI] [PubMed] [Google Scholar]
- 47.Vaughan A., Aarons E., Astbury J., Brooks T., Chand M., Flegg P., et al. Human-to-human transmission of monkeypox virus, United Kingdom, October 2018. Emerg Infect Dis. 2020;26:782–785. doi: 10.3201/eid2604.191164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Miura F., van Ewijk C.E., Backer J.A., Xiridou M., Franz E., Op de Coul E., et al. Estimated incubation period for monkeypox cases confirmed in The Netherlands, May 2022. Euro Surveill. 2022;27:2200448. doi: 10.2807/1560-7917.ES.2022.27.24.2200448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Otu A., Ebenso B., Walley J., Barceló J.M., Ochu C.L. Global human monkeypox outbreak: atypical presentation demanding urgent public health action. Lancet Microbe. 2022;S2666S5247(22):153–157. doi: 10.1016/S2666-5247(22)00153-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.World Health Organization https://www.who.int/publications/i/item/WHO-MPX-laboratory-2022.1 Accessed on July 5, 2022.
- 51.Petersen E., Kantele A., Koopmans M., Asogun D., Yinka-Ogunleye A., Ihekweazu C., et al. Human monkeypox: epidemiologic and clinical characteristics, diagnosis, and prevention. Infect Dis Clin. 2019;33:1027–1043. doi: 10.1016/j.idc.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.US, Centers for Disease Control and Prevention https://www.cdc.gov/poxvirus/monkeypox/clinicians/treatment.html Accessed on July 5, 2022.
- 53.Rizk J.G., Lippi G., Henry B.M., Forthal D.N., Rizk Y. Prevention and treatment of monkeypox. Drugs. 2022 Jun 28:1–7. doi: 10.1007/s40265-022-01742-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jezek Z., Grab B., Szczeniowski M., Paluku K.M., Mutombo M. Clinico-epidemiological features of monkeypox patients with an animal or human source of infection. Bull World Health Organ. 1988;66:459–464. [PMC free article] [PubMed] [Google Scholar]
- 55.Mbala P.K., Huggins J.W., Riu-Rovira T., Ahuka S.M., Mulembakani P., Rimoin A.W., et al. Maternal and fetal outcomes among pregnant women with human monkeypox infection in the Democratic Republic of Congo. J Infect Dis. 2017;216:824–828. doi: 10.1093/infdis/jix260. [DOI] [PubMed] [Google Scholar]
- 56.Nörz D., Pfefferle S., Brehm T.T., Franke G., Grewe I., Knobling B., et al. Evidence of surface contamination in hospital rooms occupied by patients infected with monkeypox, Germany, June 2022. Euro Surveill. 2022 Jun;27(26) doi: 10.2807/1560-7917.ES.2022.27.26.2200477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Heymann D.L., Szczeniowski M., Esteves K. Re-emergence of monkeypox in Africa: a review of the past six years. Br Med Bull. 1998;54:693–702. doi: 10.1093/oxfordjournals.bmb.a011720. [DOI] [PubMed] [Google Scholar]
- 58.Hammarlund E., Lewis M.W., Carter S.V., Amanna I., Hansen S.G., Strelow L.I., et al. Multiple diagnostic techniques identify previously vaccinated individuals with protective immunity against monkeypox. Nat Med. 2005;11:1005–1011. doi: 10.1038/nm1273. [DOI] [PubMed] [Google Scholar]
- 59.US F.D.A. https://www.fda.gov/news-events/press-announcements/fda-approves-first-live-non-replicating-vaccine-prevent-smallpox-and-monkeypox Accessed on July 5, 2022.
- 60.ACAM2000 [package insert] Emergent Product Development Gaithersburg Inc; Gaithersburg, MD: 2007. Accessed on July 6, 2022. [Google Scholar]
- 61.Lai C.C., Yen M.Y., Lee P.I., Hsueh P.R. How to keep COVID-19 at bay: a Taiwanese perspective. J Epidemiol Glob Health. 2021;11:1–5. doi: 10.2991/jegh.k.201028.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Huang C.P., Tsai C.S., Su P.L., Huang T.H., Ko W.C., Lee N.Y. Respiratory etiological surveillance among quarantined patients with suspected lower respiratory tract infection at a medical center in southern Taiwan during COVID-19 pandemic. J Microbiol Immunol Infect. 2022;55:428–435. doi: 10.1016/j.jmii.2021.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Huang J.H., Chang H.T., Liao C.H., Chiu K.M. Rapid response of a medical center upon the surge of COVID-19 epidemic in Taiwan. J Microbiol Immunol Infect. 2022;55:1–5. doi: 10.1016/j.jmii.2021.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wong N.S., Chung S.L., Lee S.S. The challenges of enhancing global preparedness in response to the impending Omicron pandemic. J Microbiol Immunol Infect. 2022;55:549–551. doi: 10.1016/j.jmii.2022.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Taiwan C.D.C. https://www.cdc.gov.tw/Category/MPage/Qb-Lfz8PNcjdNvrAVNCVtQ Accessed on July 6, 2022.
- 66.World Health Organization https://www.who.int/publications/i/item/WHO-MPX-Surveillance-2022.2 Accessed on July 6, 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.