Abstract
Objective
Many women experience traumatic events already prior to or during pregnancy, and delivery of a child may also be perceived as a traumatic event, especially in women with prior post-traumatic stress disorder (PTSD). Birth-related PTSD might be unique in several ways, and it seems important to distinguish between lifetime PTSD and birth-related traumatization in order to examine specific consequences for mother and child. This post-hoc analysis aims to prospectively examine the relation of both, lifetime PTSD (with/without interpersonal trauma) and birth-related traumatization (with/without postpartum depression) with specific maternal and infant outcomes.
Methods
In the prospective-longitudinal Maternal in Relation to Infants' Development (MARI) study, N = 306 women were repeatedly assessed across the peripartum period. Maternal lifetime PTSD and birth-related traumatization were assessed with the Composite International Diagnostic Interview for women. Maternal health during the peripartum period (incl. birth experience, breastfeeding, anxiety, and depression) and infant outcomes (e.g., gestational age, birth weight, neuropsychological development, and regulatory disorders) were assessed via standardized diagnostic interviews, questionnaires, medical records, and standardized observations.
Results
A history of lifetime PTSD prior to or during pregnancy was reported by 25 women who indicated a less favorable psycho-social situation (lower educational level, less social support, a higher rate of nicotine consumption during pregnancy). Lifetime PTSD was associated with pregnancy-related anxieties, traumatic birth experience, and anxiety and depressive disorders after delivery (and in case of interpersonal trauma additionally associated with infant feeding disorder). Compared to the reference group, women with birth-related traumatization (N = 35) indicated numerous adverse maternal and infant outcomes (e.g., child-related fears, sexual problems, impaired bonding). Birth-related traumatization and postpartum depression was additionally associated with infant feeding and sleeping problems.
Conclusion
Findings suggest that both lifetime PTSD and birth-related traumatization are important for maternal and infant health outcomes across the peripartum period. Larger prospective studies are warranted.
Implications
Women with lifetime PTSD and/or birth related traumatization should be closely monitored and supported. They may benefit from early targeted interventions to prevent traumatic birth experience, an escalation of psychopathology during the peripartum period, and adverse infant outcomes, which in turn may prevent transgenerational transmission of trauma in the long term.
Keywords: lifetime PTSD, birth-related traumatization, pregnancy, postpartum, infant outcomes
Introduction
Many women experience traumatic events already prior to or during pregnancy, and delivery of a child may also be perceived as a traumatic event, especially in women with prior post-traumatic stress disorder (PTSD). PTSD is one of the most debilitating mental disorders and the 12-month prevalence in the German general population is 2.3% (95%CI: 1.8–2.9) (1). Women are more often affected by PTSD than men (12 month-rate in women and men: 3.6%; 95%CI: 2.8–4.7; and 0.9%, 95%CI: 0.6–1.5) and most of them experience traumatic events already prior to pregnancy (1). Still, the peripartum period is considered to be a vulnerable time frame for the onset, recurrence, and exacerbation of PTSD symptoms and other mental disorders in women (e.g., peripartum anxiety and depressive disorders) (2). Due to traumatic experiences prior to or during pregnancy about 3.3% of pregnant women suffer from PTSD and prevalence rates in risk populations (e.g., history of intimate partner violence) are even higher (about 18%) (3). In addition, up to one-third of women who have recently given birth describe their birth experience as traumatic (4), up to 10% suffer from clinically relevant posttraumatic stress symptoms during the first weeks thereafter (5–8), and up to 4% develop the full clinical picture of PTSD (3, 7, 9, 10). The prevalence of postpartum PTSD is even higher in at-risk populations (e.g., up to 19% after preterm delivery, emergency cesarean section, or still birth) (3, 7, 9, 10).
Birth-related PTSD might be unique in several ways, and it seems important to distinguish between lifetime PTSD and birth-related traumatization. Birth experience may become traumatic if the birth involves actual or threatened death or an injury for a woman or for the infant (2, 11, 12). Birth-related traumatization affects the mother-child-dyad and childcare of the baby might trigger maternal traumatic memories of birth. Given that childcare is usually associated with an increased vigilance, the hyperarousal criteria should be considered with caution. Risk factors of birth-related traumatization are a history of sexual trauma and intimate partner violence, depression or anxiety in pregnancy, fear of childbirth, complications during pregnancy, obstetric interventions/ operative delivery, peripartum infant complications, a subjective negative birth experience, and perception of inadequate intrapartum care or lack of social support (5, 11–14).
Both, lifetime PTSD and birth-related traumatization may be associated with postpartum depressive and anxiety disorders, whereas the relation to pregnancy- and child-related fears is less studied (5, 15–17). Moreover, PTSD in the context of pregnancy and childbirth might affect the partnership (e.g., sexual problems) and the mother-child-dyad (e.g., bonding) (16, 18, 19). For instance, traumatic memories or re-experiencing of the childbirth might reduce emotional availability of the mother to the infant, especially if the infant serves as a trigger of the event. This, in turn, could be crucial for the type of attachment the infant develops to the mother. Mother-child dyads may be further fragiled by the numbness affected women are likely to perceive (20). Some studies showed that birth-related PTSD symptoms are associated with bonding and breastfeeding difficulties that may have long-term health implications for infants (21, 22). In addition, symptoms of hyperarousal and intrusion might lead to impaired childcare and interaction with the child (e.g., angry or intrusive interaction) (19, 23, 24) and comorbid maternal depression might contribute additionally to parenting impairment (25, 26). A review by Christie et al. (27) found that parental PTSD was associated with impaired functioning across various parenting domains and less optimal parent-child relationships (27). The Perinatal Interactional Model of Intergenerational transmission of traumatization proposes that maternal PTSD leads to suboptimal caregiving behavior and parent-child interactions, which undermine child regulatory capacity and increase distress leading to poorer social-emotional outcomes for offspring of parents with PTSD (28). Moreover, Pat-Horenczyk et al. (29) suggested the idea of relational emotional regulation in which difficulties with emotion regulation pass from mother faced with trauma to the child (29). In line with this, Davies and colleagues showed that women with postpartum PTSD symptoms following childbirth and postpartum depression perceive their attachment relationships to be less optimal and rated their infants as being temperamentally more difficult and less easy to soothe as compared to non-symptomatic women (9). Moreover, some prospective studies found maternal postpartum PTSD to be associated with difficult temperament and/ or poorer cognitive and social-emotional development in infants up to 2 years (19, 30). Especially interpersonal trauma might be crucial for the relation between mother and child and for early child development (e.g., neuropsychological development) (2, 31, 32).
Aims of the Study
In sum there is evidence that PTSD prior to and during pregnancy as well as birth-related traumatization are associated with adverse maternal and infant outcomes. As it has been argued that birth-related PTSD might be unique in several ways it seems important to distinguish between lifetime PTSD and birth-related traumatization in order to examine specific consequences for the mother and child (31, 33, 34). A post-hoc analysis of the data of the Maternal Anxiety in Relation to Infant Development (MARI) study was conducted to examine specific associations of lifetime PTSD and birth-related traumatization with the above mentioned outcomes. In the prospective-longitudinal MARI study (35, 36) women were recruited already during early pregnancy and reported their lifetime diagnostic status prior to pregnancy. Participants were followed up three times during pregnancy and three times after delivery within this multi-wave and multi-method study. Given that anxiety and depressive disorders occur frequently in expectant mothers and may be also relevant for the considered outcomes, we chose expectant mothers with no anxiety and/or depressive disorders prior to or during pregnancy as reference group. This allows the examination of specific associations of lifetime PTSD and birth-related traumatization with the specific outcomes.
Using the data of the MARI study we were able to examine (1) whether women with PTSD prior to or during pregnancy were at higher risk for poor maternal health during the peripartum period (e.g., pregnancy-related fears, maternal anxiety and depressive disorder, operative delivery), for a traumatic birth experience, and adverse gestational and infant outcomes (e.g., regulatory disorders, attachment, neuropsychological development) as compared to women with neither anxiety nor depressive disorder until third trimester of pregnancy. Further, we examined (2) whether women suffering from birth-related traumatization were at higher risk for adverse maternal and infant outcomes (e.g., child-related fears, maternal anxiety and depressive disorder, maternal sexual problems, infant regulatory disorders) as compared to women with no anxiety or depressive disorder prior to delivery and no birth-related traumatization. Here we additionally investigated the role of postpartum depression at 2, 4 or 16 month postpartum (25).
Methods
Procedure
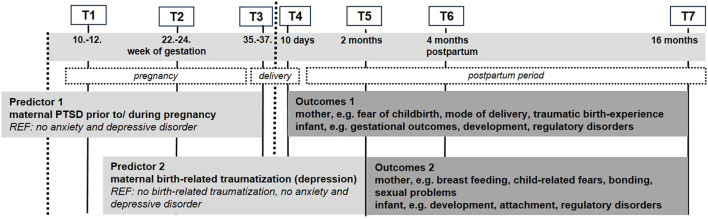
The prospective-longitudinal MARI Study was conducted among N = 306 expectant mothers, sampled from the community in gynecological outpatient settings in Dresden, Germany (study period: 01/2009 – 09/2012). Participating pregnant women (and their infants) completed up to seven assessments: T1 (baseline): week 10 to 12 of gestation; T2: week 22 to 24 of gestation; T3: week 35 to 37 of gestation; T4: 10 days postpartum; T5: 2 months postpartum; T6: 4 months postpartum; T7: 16 months postpartum (36).
Informed consent was obtained from all participants and all legal guardians of the infants. The MARI Study was carried out in accordance with the Helsinki Declaration (2013) and was reviewed by the Ethics Committee of the Technische Universität Dresden (No: EK 94042007). More detailed information including objectives, methods, design, and a detailed study flow chart has been published elsewhere (35, 36).
Participants
Overall, N = 533 pregnant women were approached by the study team in gynecological outpatient settings in Dresden (Germany) and screened for inclusion and exclusion criteria. Fifty women were excluded based on the exclusion criteria, which were as follows: gestational age >12 weeks (n = 8), younger than 18 or older than 40 years (n = 8), multiple pregnancy (n = 2), history of more than three spontaneous abortions/(induced) terminations of pregnancy/stillbirths or infant impairment (n = 2), invasive fertility treatment (n = 9), severe physical disease/microsomnia/skeletal malformation (n = 6), substance abuse or heroin substitution during the past 6 months (n = 0), severe psychiatric illness (n = 2), expectation to leave the area of Dresden (n = 6), and insufficient mastery of German language (n = 7). Additional 9 women did not participate due to spontaneous abortion before the baseline interview (T1), 10 due to lacking consent of the father of the infant, 154 due to lack of time, and 4 due to unknown reasons (36).
Overall, data of 306 women were eligible for the MARI study. Due to spontaneous abortion/induced termination of pregnancy, the participation of n = 8 women ended after T1. During the study, n = 3 women moved away, n = 5 women could not be reached any more by phone, postal, or personal contact, n = 9 women reported lack of time or interest for further participation, and n = 7 women refused contact for follow-up assessment. Overall, retention rate until 16 months after delivery (T7) was 89.5% (n = 274). Some women did not participate at single assessments, e.g. due to preterm delivery, own/infant sickness, or lack of time (T2: n = 0, T3: n = 10, T4: n = 2, T5: n = 5, T6: n = 1, T7: n = 7) (a detailed flow chart of the MARI study was presented by Martini et al. (36).
Measures and Procedures
Figure 1 presents the assessment points of the MARI study and predictors and outcomes of the present analyses. A Computer-Assisted Personal Interview (CAPI) version of the Composite International Diagnostic Interview for Women (CIDI-V) (37) was applied at each assessment wave except for T4 (10 days postpartum). Due to the special situation after delivery, questionnaires were used at T4 instead of the diagnostic interview to assess mode of delivery, birth experience, neonatal outcomes, and postpartum adjustment.
Figure 1.
Assessment waves, measures and outcomes for the post-hoc analyses of lifetime PTSD and birth-related traumatization with maternal and infant outcomes.
Predictors: PTSD Prior to or During Pregnancy and Birth-Related Traumatization
Maternal post-traumatic stress disorder as well as anxiety and depressive disorder were assessed using the CIDI lifetime version at baseline (T1) and the CIDI interval version at follow-up (T2, T3, T5, T6, T7). The CIDI-V is a modified version of the World Health Organization CIDI (WHO-CIDI) (38) that allows for a fully standardized assessment of DSM-IV-TR mental disorders in women (with specifying ICD-10 codes). Psychometric properties of the CIDI were modest to very good (39, 40). Diagnostic interviews were conducted by psychologists having received 1 week of intensive training and conducting a series of supervised interviews. Interviewers were closely monitored throughout the field period by experienced supervisors (clinical psychologists) (36).
Lifetime PTSD was assessed at Baseline (T1) and in Follow-up (T2, T3, T5, T6, and T7) interviews using the questions of the CIDI-V (Section N). Overall, n = 25 participants suffered from PTSD prior to or during pregnancy (35).
Birth-related traumatization was assessed at T5, T6, and T7 using adapted questions and lists of section N relating to the birth. It was defined as traumatic birth experience (A1: delivery as traumatic event or A2: intense fear, helplessness, or horror) AND hyperarousal or re-experiencing delivery or avoidance at T5, T6, or T7. Birth-related traumatization was indicated by N = 35 women. Of those women, N = 19 additionally indicated postpartum depression.
Since only N = 4 women indicated both PTSD prior to or during pregnancy and birth-related traumatization, this small group could not be analyzed in more detail.
Maternal and Infant Outcomes
Fear of childbirth during pregnancy and experience of childbirth was measured based on the German version of the Wijma Delivery Expectancy/ Experience Questionnaire (W-DEQ, Version A, Version B) (41–43). The W-DEQ is a reliable and valid 33-item questionnaire, with scores ranging from ‘not at all' (0) to ‘extremely' (5), yielding a minimum score of 0 and a maximum score of 165 (some items have to be reversed and a higher score indicates more intense fear of childbirth) (44, 45).
Maternal pregnancy- and child related fears were assessed at the end of the CIDI-V section on anxiety disorders with embedded questions and lists (37). During the assessments in pregnancy (T1–T3) the participants were instructed to read a list with pregnancy-related fears (e.g., rumination about current pregnancy, fear of labor pain, fear of vaginal delivery) and at T6 and T7 a list with child-related fears was provided (e.g., fear of mistakes concerning child care, fear of financial problems, fear of age-inappropriate development). The participants were asked “Have you ever (“Since the last interview, have you…”) had a strong fear or avoidance of any of the situations/things in the list?” If the participants indicated one or more of these fears, they were asked whether the fear was excessive or stronger compared to other women and to evaluate the burden of the reported fears. Further questions on the presentation of associated anxiety symptoms (e.g., racing heart, sweating, trembling/shaking, dry mouth, difficult breathing, sensation of choking), frequency (sometimes or most of the time vs. only once), and interference with daily live (not at all or somewhat vs. a lot or very much) were asked.
Information on gestational age, preterm delivery (<37 + 0 week of gestation), infant birth weight, and mode of delivery was collected via medical records (46).
Sexual problems were assessed at T7 using the German version of the Massachusetts General Hospital Sexual Function Questionnaire (MGH) (47, 48). The MGH is a five-item screening instrument that assesses sexual problems with respect to sexual interest, arousal, orgasm, lubrication, and overall sexual satisfaction: (i) “How has your interest in sex been over the past month?”; (ii) “How has your ability to become sexually aroused or excited been over the past month?”; (iii) “How has your ability to achieve orgasm been over the past month?”; (iv) “How has your ability to become or remain lubricated been over the past month?”; (v) “How would you rate your overall sexual satisfaction over the past month?”. Items are labeled: 1: greater than normal; 2: normal; 3: minimally diminished; 4: moderately diminished; 5: markedly diminished; and 6: totally absent. Based on previous studies (47), a cutoff score of three was used to differentiate normal sexual functioning (≤ 3) from putative sexual problems or dysfunctions (>3) on each item. Concurrent and predictive validity (with respect to sexual functioning and sexual dysfunctions assessed by other self-reports and diagnostic instruments) of the MGH have been shown to be high (47, 49).
Duration of breastfeeding and infant regulatory disorders were assessed with a structured diagnostic interview (Baby-DIPS) at T5, T6, and T7 (50). Excessive infant crying was defined according to the “rule of three” by Wessel et al. (51) as crying for ≥3 h per day on ≥3 days per week for ≥3 weeks (51). Feeding problems were defined as any feeding problem (from a list of 16 feeding problems), failure-to-thrive, or mothers worrying (a lot or very much) about infant growth over a period of at least 4 weeks. Sleeping problems were defined as difficulties in initiating or maintaining sleep for ≥3 nights per week for ≥3 months while the mother was somewhat, a lot, or very much impaired by her infant's sleeping difficulties between 6 and 16 months (52). Cases that were attributable to a concurrent medical condition were excluded. The Baby-DIPS comprises good to excellent inter-rater reliability as well as high acceptance rates for interviewers and participants (53). Rates and co-occurrence of regulatory problems in the MARI sample were comparable to rates reported by others (52, 54).
Maternal bonding was assessed with the German Version of the Postpartum Bonding Instrument (PBQ) at T5 (55). This self-report questionnaire consists of 25 items assessing impaired bonding, rejection and anger, anxiety about care, and risk of abuse (42, 56). The very good psychometric properties were confirmed for the German Version (55). For this analysis, the scales impaired bonding as well as rejection and anger were relevant.
Observations of the mothers and their infants were conducted using standardized observation paradigms to assess infants' temperament (57), neuropsychological development (58), and the quality of infant attachment (59). Standardized observations were conducted by two female psychologists who were blinded to the diagnosis of the mother and had received 2 weeks of training. All observations were recorded by three cameras and supervised to ensure a high assessment quality. Video coding was conducted with the software “Interact” (Mangold).
Neuropsychological development was assessed at T6 and T7 with the standardized procedure by Petermann and Renziehausen (58). The tasks allow for an assessment of developmental deficits in different areas (movement control, fine motor skills, visual perception, exploration behavior, receptive and expressive language, cognitive performance). Coding was conducted by graduate and postgraduate psychology students according to the manual guidelines (58).
Temperament was measured with the procedures developed by Kagan et al. (60). For the assessment of infant's reactivity at T6, the infants sat in a reclining cushioned seat and heard some taped sentences, saw three different colorful mobiles move back and forth, had a cotton swab dipped in dilute butyl alcohol placed under the nostrils, heard a female voice speaking different syllables, and saw a colored umbrella spread out. During these procedures the mother was out of view of the infant. Videotapes were coded for high motor activity (multiple arm, leg, and back movements) and crying (high percentage of time spent crying) in response to the stimuli. Infants were classified as “highly reactive” (high motor activity and crying), “low reactive” (low motor activity and crying), or neither (either high motor activity and low crying amount or the opposite). The assessment of behavioral inhibition at T7 involved the presentation of inanimate stimuli to the child (a spinning bingo wheel with noisy objects inside, rotating toys, a puppet show, and sweet and sour tastes). Moreover, strangers (a woman dressed in a white laboratory coat and surgical face mask and a woman with a black cloth over her head and shoulders) attempted to interact with the child. Video coding was conducted by graduate and postgraduate psychology students who were blinded and had received a training of 2 weeks for coding the infant's reactivity and behavioral inhibition (60). The average coding time was 45 min for reactivity and behavioral inhibition. At least 10 videos were coded during training sessions to yield an adequate observer agreement (kappa >0.8) and about 10% of all videos were randomly selected and re-analyzed for quality check to ensure observer agreement with satisfying results (61).
Attachment: At T7 mother-infant-dyads participated in the Strange Situation Procedure (59), which consisted of eight episodes, including two brief separations and reunions of the infant from/with the mother. Following the procedures described by Ainsworth et al. (59) and Main and Solomon (62), the attachment group classification was based primarily on the infant's reactions to the mother's return (59, 62). Infants who actively greeted and/or sought contact with the mother upon reunion and returned to exploration within 3 min were classified as secure (Typ B: secure). Infants who actively averted gaze or avoided or ignored the mother immediately upon reunion (Typ A: avoidant) and infants who sought to reunite with the mother but displayed ineffective proximity and contact-seeking behavior, showing anger and active resistance to contact or prolonged fussiness and persistent low-level distress (Typ C: ambivalent/resistant) were classified as insecure. Video coding was conducted by graduate and postgraduate psychology students who were blinded and had received the coding training. The average coding time for attachment videos was 60 min. Cohen's kappa coefficient for the secure and insecure (avoidant and resistant) attachment classifications was based on 20% of randomly selected and independently scored videotapes of the Strange Situation Test (63). Interrater reliability was conducted on 20% of the sample (κ = 1.00 for ABC classification). Final scores for difficult tapes and coder disagreements were based on consensus [for more information see (64)].
Statistical Analyses
All analyses were performed using STATA version 14 (65). For research question (1) linear and logistic regression analyses were conducted to examine concurrent and prospective associations (Beta, ß and odds ratios, OR) of maternal PTSD prior to or during pregnancy with and without interpersonal trauma with maternal and infant health outcomes (reference: women with neither anxiety nor depressive disorder until T3). For research question (2) linear and logistic regression analyses were conducted to examine betas/ORs including 95% confidence intervals (CI) of maternal birth-related traumatization (with and without depression) with maternal and infant health outcomes (reference: neither anxiety nor depressive disorder prior to or during pregnancy and no birth-related traumatization). Separate analyses were conducted for each outcome and no adjustment for multiple testing was applied, because the individual tests were related to individual hypotheses. Statistical significance was evaluated two-sided at the 5% level (p < 0.05).
Results
To investigate research question 1, analyses were based on the following three diagnostic groups:
Reference: neither anxiety nor depressive disorder prior to or during pregnancy (until T3) (N = 100)
PTSD prior to or during pregnancy (cumulative lifetime diagnosis until T3) (N = 25)
PTSD prior to or during pregnancy with interpersonal traumata (cumulative lifetime diagnosis until T3) (N = 17)
Women with PTSD prior to or during pregnancy were characterized by a lower educational level (education: ≤ 10 years: reference: 25.0%, PTSD prior to or during pregnancy: 52.0%; Chi2=6.891, p = 0.009) compared to women with neither anxiety nor depressive disorder until delivery (Table 1). Moreover, women with PTSD prior to or during pregnancy reported more often nicotine consumption during pregnancy (16.0% vs. 3.0%; Chi2=6.394, p = 0.001) and lower social support during pregnancy (F-Sozu: M=4.1, SD=0.7 vs. M=4.5, SD=0.4; t = 3.122, p > 0.001) as compared to the reference group. There were no significant differences between the groups with regard to age, marital status, and monthly household income (Table 1).
Table 1.
Sociodemographic and gynecological characteristics of women with any PTSD until T3 (with/without interpersonal trauma) (N = 25) as compared to women with neither anxiety nor depressive disorder until T3 (N = 100).
|
Women with neither anxiety nor depressive disorder until T3
(N = 100) |
PTSD prior to or during pregnancy with/without interpersonal trauma (N = 25) | Significant group differences | |
|---|---|---|---|
| N, % or M, SD | N, % or M, SD | ||
| Age (M, SD) | 27.9 (4.6) | 27.1 (3.7) | |
| Educational status (n, %) | |||
| Lower education (≤ 10 years) | 25 (25.0) | 13 (52.0) | Chi2=6.891, p = 0.009 |
| Higher education (>10 years) | 75 (75.0) | 12 (48.0) | |
| Marital status (n, %) | |||
| Not married | 64 (64.0) | 18 (72.0) | |
| Married | 36 (36.0) | 7 (28.0) | |
| Cohabitation (n, %) | |||
| Not living together | 6 (6.0) | 0 (0.0) | |
| Living together | 94 (94.0) | 25 (100.0) | |
| Working time at baseline (n, %) | |||
| Full-time job | 37 (37.0) | 8 (32.0) | |
| Part-time job | 26 (26.0) | 4 (16.0) | |
| Currently not working | 37 (37.0) | 13 (52.0) | |
| Monthly household income after taxes (n, %) | |||
| <500€ | 9 (9.0) | 1 (4.0) | |
| 500–1,500€ | 34 (34.0) | 11 (44.0) | |
| 1,500–2,500€ | 27 (27.0) | 9 (36.0) | |
| 2,500–3,500€ | 19 (19.0) | 2 (8.0) | |
| 3,500–4,500€ | 8 (8.0) | 2 (8.0) | |
| >4,500€ | 3 (3.0) | 0 (0.0) | |
| Parity (n, %) | |||
| Primipara | 60 (60.0) | 11 (44.0) | |
| Multipara | 40 (40.0) | 14 (56.0) | |
| Pregnancy planned/ desired: yes (n, %) | 86 (94.5) | 22 (95.7) | |
| Prior spontaneous abortions (n, %) | |||
| No | 79 (79.0) | 16 (64.0) | |
| Yes | 21 (21.0) | 9 (36.0) | |
| Any nicotine consumption during pregnancy (n, %) | 3 (3.0) | 4 (16.0) | Chi2=6.394, p = 0.011 |
| Any alcohol consumption during pregnancy (n, %) | 31 (31.0) | 7 (28.0) | |
| Social support during pregnancy (F-SozU, T2) (M, SD) | 4.5 (0.4) | 4.1 (0.7) | t = 3.122, p > 0.001 |
| Partnership quality during pregnancy (PFB, T2) (M, SD) | 72.8 (10.5) | 68.5 (18.1) |
T3, MARI assessment during third trimester of pregnancy; REF, reference; PTSD, post-traumatic stress disorder; n, number; %, percentage; M, mean; SD, standard deviation; Chi2, Chi-squared test; t, t-test; p, p-value. Bold: significant group differences.
Table 2 shows maternal and infant outcomes in women with PTSD prior to or during pregnancy compared with or without interpersonal trauma (N = 25) to women with neither anxiety nor depressive disorder until T3 (N = 100). Women with history of PTSD reported more fear of childbirth and fear of epidural anesthesia and perceived delivery more often as traumatic (including re-experiencing delivery later on). Moreover, infants of women with PTSD prior to delivery and interpersonal trauma (N = 17) were at higher risk for feeding problems.
Table 2.
Maternal and infant outcomes in women with PTSD prior to or during pregnancy (with interpersonal trauma) compared to women with neither anxiety nor depressive disorder until T3.
| Reference group: Neither anxiety nor depressive disorder prior to or during pregnancy (until T3) (N = 100) | PTSD prior to or during pregnancy (w/wo interpersonal trauma) (N = 25) | PTSD prior to or during pregnancy with interpersonal traumata (until T3) (N = 17) | |||
|---|---|---|---|---|---|
| N, % or M, SD | N, % or M, SD | OR (95%CI) or ß (95%CI) | N, % or M, SD | OR (95%CI) or ß (95%CI) | |
| Maternal health during pregnancy and birth experience | |||||
| Fear of childbirth (W-DEQ-A, T3) (M, SD) | 57.9 (21.5) | 69.3 (22.1) | ß = 11.40 (1.21–21.59) | 69.7 (19.0) | ß = 11.80 (0.08–23.51) |
| Birth experience (W-DEQ-B, T4) (M, SD) | 62.8 (21.8) | 67.3 (18.2) | 65.8 (18.8) | ||
| Pregnancy-related anxiety (n, %) | |||||
| Fear of labor pain | 19 (19.0) | 8 (32.0) | 5 (29.4) | ||
| Fear of vaginal delivery | 26 (26.0) | 10 (40.0) | 8 (47.1) | ||
| Fear of perineal rupture/episiotomy | 27 (27.0) | 6 (24.0) | 5 (29.4) | ||
| Fear of epidural anesthesia | 8 (8.0) | 10 (40.0) | OR = 7.67 (2.61–22.53) | 7 (41.2) | OR = 8.05 (2.41–26.89) |
| Excessive pregnancy-related fear | 7 (7.0) | 5 (20.0) | 3 (17.7) | ||
| Presentation of anxiety symptoms | 8 (8.0) | 4 (16.0) | 3 (17.7) | ||
| Interference with daily live | 3 (3.0) | 6 (24.0) | OR = 10.21 (2.35–44.43) | 3 (17.7) | OR = 6.93 (1.27–37.76) |
| Evaluation of fears as frequent | 9 (9.0) | 4 (16.0) | 3 (17.7) | ||
| Mode of delivery (n, %) | |||||
| Spontaneous delivery | 78 (85.7) | 20 (87.0) | 14 (87.5) | ||
| C-section/ Operative vaginal delivery | 13 (14.3) | 3 (13.4) | 2 (12.5) | ||
| Support and control during delivery (M, SD) | |||||
| Internal control (SCIB) | 32.2 (8.1) | 28.7 (9.2) | 27.9 (9.4) | ||
| External control (SCIB) | 38.1 (8.9) | 38.0 (8.2) | 38.4 (8.7) | ||
| Support (SCIB) | 46.9 (8.6) | 46.7 (11.3) | 44.6 (12.0) | ||
| DSM-VI criteria for traumatic birth experience (n, %) | |||||
| A1: delivery as traumatic event | 11 (12.1) | 9 (42.9) | OR = 5.45 (1.87–15.90) | 6 (42.9) | OR = 5.45 (1.59–18.70) |
| A2: intense fear, helplessness, or horror | 15 (16.5) | 8 (38.1) | OR = 3.12 (1.10–8.82) | 6 (42.9) | OR = 3.80 (1.15–12.55) |
| B: re–experiencing delivery | 1 (1.0) | 4 (16.0) | OR = 18.85 (2.00–177.37) | 2 (11.8) | OR = 13.20 (1.13–154.68) |
| C: avoidance of recollection due to delivery | 0 (0.0) | 0 (0.0) | omitted | 0 (0.0) | omitted |
| E: alterations in arousal following delivery | 6 (6.0) | 2 (8.0) | 0 (0.0) | omitted | |
| Any postpartum anxiety disorder (n, %) | 8 (8.8) | 11 (47.8) | OR = 9.51 (3.19–28.39) | 7 (43.8) | OR = 8.07 (2.37–27.49) |
| Postpartum depression (n, %) | 0 (0.0) | 7 (30.4) | omitted | 5 (31.3) | omitted |
| Infant health outcomes | |||||
| Gestational age (M, SD) | 39.5 (1.5) | 39.4 (1.2) | 39.4 (1.2) | ||
| Birth weight (M, SD) | 3,403.2 (58.1) | 3.510.7 (440.7) | 3,494.1 (440.6) | ||
| Excessive crying (n, %) | 6/91 (6.6) | 3/23 (13.0) | 2/16 (12.5) | ||
| Feeding problems (n, %) | 24/91 (26.4) | 10/23 (43.5) | 9/16 (56.3) | OR = 3.59 (1.20–10.70) | |
| Sleeping problems (n, %) | 9/91 (9.9) | 4/23 (17.4) | 4/16 (25.0) | ||
| Neuropsychological development (T6) (M, SD) | 11.6 (0.8) | 11.6 (0.6) | 11.6 (0.6) | ||
| Neuropsychological development (T7) (M, SD) | 13.3 (1.8) | 13.6 (1.6) | 13.1 (1.7) | ||
| Temperament: highly reactive (T6) (n, %) | 9/83 (10.8) | 5/22 (22.7) | 4/15 (26.7) | ||
| Temperament: Behavioral Inhibition (T7) (n, %) | 38/84 (45.2) | 5/20 (25.0) | 5/13 (38.5) | ||
| Insecure attachment (Strange Situation) (T7) (n, %) | 29/82 (35.4) | 7/20 (35.0) | 4/13 (30.8) | ||
T3, 3rd assessment during third trimester of pregnancy; T5, 5th assessment 2 months postpartum; T6, 6th assessment 4 months postpartum; T7, 7th assessment 16 months postpartum; REF, reference; Any PTSD until T3, women with any PTSD until T3, Any PTSD + man-made trauma until T3, women with any PTSD with manmade trauma until T3, W-DEQ, Wijma Delivery Expectancy/Experience Questionnaire; PBQ, Postpartum Bonding Questionnaire; N, number; %, percentage; M, mean; SD, standard deviation; OR, odds ratio; 95%CI, 95% confidence interval. Bold: significant group differences.
To investigate research question 2, analyses were based on the following three diagnostic groups:
Reference: neither anxiety nor depressive disorder prior to or during pregnancy (until T3) and no birth-related traumatization (traumatic birth experience (A1 or A2) AND no hyperarousal/ re-experiencing/ avoidance) (N = 70)
birth-related traumatization (traumatic birth experience (A1 or A2) AND hyperarousal or re-experiencing or avoidance) (N = 35)
birth-related traumatization (traumatic birth experience (A1 or A2) AND hyperarousal or re-experiencing or avoidance) AND depression (N = 19)
Table 3 shows maternal and infant outcomes in women with birth-related traumatization compared to women with neither anxiety nor depressive disorder until T3 and no birth-related traumatization. A higher risk for child-related fears, postpartum anxiety disorders, and sexual problems was reported by women with birth-related traumatization. Moreover, infants of mothers with birth-related traumatization and postpartum depression were at higher risk for feeding and sleeping problems.
Table 3.
Maternal and infant outcomes in women with birth-related traumatization (and depression) after delivery compared to women with neither anxiety nor depressive disorder until T3 and no birth-related traumatization.
| Reference group: Neither anxiety nor depressive disorder until T3 and no birth-related traumatization (N = 70) | Birth-related traumatization: Traumatic birth experience (A1/ A2) + (hyperarousal/ re-experiencing/ avoidance) (N = 35) | Birth-related traumatization: Traumatic birth experience (A1/ A2) + (hyperarousal/ re-experiencing/ avoidance) + depression (N = 19) | |||
|---|---|---|---|---|---|
| N, % or M, SD | N, % or M, SD | OR (95%CI) or ß (95%CI) | N, % or M, SD | OR (95%CI) or ß (95%CI) | |
| Maternal health during postpartum period | |||||
| Duration of breastfeeding (M, SD) | 9.4 (4.6) | 9.6 (4.5) | 8.8 (4.7) | ||
| Maternal impaired bonding (T5) (PBQ) (M,SD) | 4.3 (4.1) | 5.3 (4.3) | 5.5 (4.1) | ||
| Maternal rejection and anger (T5) (PBQ) (M,SD) | 1.5 (2.0) | 1.7 (2.2) | 1.8 (1.9) | ||
| Child-related fears/ anxiety (n, %) | |||||
| Fear of mistakes concerning child care | 9 (12.9) | 11 (31.4) | OR = 3.11 (1.14–8.44) | 6 (31.6) | |
| Fear of mistakes concerning child feeding | 12 (17.1) | 14 (40.0) | OR = 3.22 (1.29–8.07) | 7 (36.8) | |
| Fear of financial problems | 2 (2.9) | 2 (5.7) | 2 (10.5) | ||
| Fear of mistakes concerning child rearing | 3 (4.3) | 10 (28.6) | OR = 8.93 (2.27–35.14) | 6 (31.6) | OR = 10.31 (2.28–46.56) |
| Fear concerning quality of day care* | 7 (10.3) | 8 (23.5) | 3 (16.7) | ||
| Fear that child suffers from familial conflicts* | 0 (0.0) | 4 (11.8) | omitted | 1 (5.6) | omitted |
| Fear of separation from child | 3 (4.4) | 7 (20.6) | OR = 5.62 (1.35–23.36) | 3 (16.7) | |
| Fear of age-inappropriate infant development | 5 (7.1) | 5 (14.3) | 5 (26.3) | OR = 4.64 (1.18–18.23) | |
| Fear of viral or other infection/ disease | 8 (11.4) | 8 (22.9) | 4 (21.1) | ||
| Fear of infant injury | 11 (15.7) | 9 (25.7) | 3 (15.8) | ||
| Fear of infant death | 13 (18.6) | 16 (45.7) | OR = 3.69 (1.51–9.06) | 9 (47.4) | OR = 3.95 (1.34–11.66) |
| Evaluation of fear as excessive | 30 (42.9) | 23 (65.7) | OR = 2.56 (1.10–5.94) | 13 (68.4) | |
| Presentation of anxiety symptoms | 7 (10.0) | 10 (28.6) | OR = 3.60 (1.23–10.51) | 5 (26.3) | |
| Evaluation of fears as frequent | 6 (8.6) | 9 (25.7) | OR = 3.69 (1.19–11.42) | 4 (21.1) | |
| Interference with daily life | 2 (2.86) | 5 (14.3) | OR = 5.67 (1.04–30.87) | 4 (21.1) | OR = 9.07 (1.52–54.15) |
| Any anxiety disorder postpartum | 6 (8.6) | 14 (40.0) | OR = 7.11 (2.43–20.86) | 8 (42.1) | OR = 7.76 (2.25–26.72) |
| Postpartum depression | 0 (0.0) | 19 (54.3) | omitted | 19 (100.0) | group definition |
| Sexual problems (T7) (M, SD) | |||||
| Sexual interest | 3.2 (1.4) | 3.9 (1.3) | ß = 0.76 (0.18–1.33) | 4.2 (1.2) | ß = 1.02 (0.30–1.75) |
| Sexual arousal | 2.8 (1.4) | 3.4 (1.4) | ß = 0.60 (0.02–1.19) | 3.5 (1.4) | |
| Orgasm | 2.7 (1.4) | 3.6 (1.7) | ß = 0.90 (0.26–1.53) | 3.8 (1.8) | ß = 1.10 (0.29–1.91) |
| Lubrication | 2.3 (0.9) | 3.0 (1.4) | ß = 0.76 (0.28–1.24) | 2.9 (1.4) | ß = 0.67 (0.09–1.25) |
| Overall sexual satisfaction | 2.8 (1.3) | 3.9 (1.5) | ß = 1.1 (0.50–1.67) | 4.4 (1.5) | ß = 1.57 (0.84–2.29) |
| Infant Health and infant outcomes | |||||
| Excessive crying (n, %) | 5/70 (7.1) | 4/35 (11.4) | 3/19 (15.8) | ||
| Feeding problems (n, %) | 17/70 (24.3) | 15/35 (42.9) | 12/19 (63.2) | OR = 5.34 (1.81–15.74) | |
| Sleeping problems (n, %) | 8/70 (11.4) | 9/35 (25.7) | 8/19 (42.1) | OR = 5.64 (1.75–18.18) | |
| Neuropsychological development (T6) (M, SD) | 11.4 (0.9) | 11.6 (0.8) | 11.7 (0.8) | ||
| Neuropsychological development (T7) (M, SD) | 13.3 (1.9) | 13.1 (2.0) | 12.9 (2.3) | ||
| Temperament: highly reactive (T6) (n, %) |
7/63 (11.1) | 5/32 (15.6) | 2/17 (11.8) | ||
| Temperament: behavioral Inhibition (T7) (n, %) | 32/66 (48.5) | 14/31 (45.2) | 7/16 (43.8) | ||
| Insecure attachment (Strange Situation) (T7) (n, %) | 26/65 (40.0) | 15/31 (48.4) | 8/16 (50.0) | ||
T5, 5th assessment 2 months postpartum; T6, 6th assessment 4 months postpartum; T7, 7th assessment 16 months postpartum; REF, reference; A1, DSM–IV PTSD criteria A1; A2, DSM–IV PTSD criteria A2; PBQ, Postpartum Bonding Questionnaire; N, number; %, percentage; M, mean; SD, standard deviation; OR, odds ratio; ß, Beta-coefficient; 95%CI, 95% confidence interval; *Data of N = 267 participants available only. Bold: significant group differences.
Discussion
This prospective longitudinal study demonstrated that (1) women with PTSD prior to or during pregnancy presented with a disadvantageous psycho-social situation, reported more pronounced fear of childbirth, and indicated more often a traumatic birth experience compared to women without anxiety and depressive disorder prior to delivery. Moreover, infants of women with PTSD and interpersonal trauma, had a higher risk for feeding problems. (2) Women with birth-related traumatization indicated numerous adverse outcomes (e.g., postpartum anxiety and depression, child-related fears, sexual problems), and in case of additional postpartum depression, the infants were more often affected by feeding and sleeping problems.
The first research question examined the associations of PTSD prior to or during pregnancy with specific maternal and infant outcomes. As expected and in line with previous research, women with PTSD prior to or during pregnancy reported more often pregnancy- and child-related fears and they were further at higher risk for a traumatic birth experience compared to women without anxiety and depressive disorder prior to delivery (12). Moreover, those women presented with a disadvantageous psycho-social situation (lower educational level, less social support) and indicated more often nicotine consumption during pregnancy (66, 67). These factors can be associated with a cascade of behavioral health and neuroendocrine changes that may not only have negative consequences for the affected women, but also for the infants (68, 69). Regarding the current discussion on intergenerational transmission of trauma effects it is particularly interesting that women with lifetime PTSD reported more pronounced pregnancy-related fears (70). Yehuda and Lehrner recently highlighted that preconception trauma in parents might be associated with epigenetic changes and developmentally programmed effects that can result from offspring's early environmental in utero and postnatal exposures leading to an increased susceptibility of the infant to later environmental distress (70, 71). We found a higher risk for infant regulatory disorders (feeding problems) in mothers with PTSD prior to or during pregnancy and interpersonal traumata (2, 28, 29, 31, 32). However, no significant associations were seen for e.g., temperament, neuropsychological development, or bonding. One explanation could be that lifetime PTSD was not present anymore during the perinatal period in some of the women due to recovery or successful therapy. However, it still seems to be relevant for the development of infant feeding problems in case of interpersonal trauma. Another explanation might be the limited statistical power to detect differences between the respective groups (see limitations section).
The second research question pertains to birth-related traumatization. As expected, women with birth-related traumatization reported more often sexual problems as compared to the reference group (12). Given that sexual problems impede the partnership or interfere with further family planning, affected women might profit from targeted early interventions supporting them and their partners to successfully cope with sexual dysfunctions and associated problems (18, 72). In line with previous evidence, women with birth-related traumatization reported more often postpartum anxiety and depressive disorders as compared to the reference group (12). This is important to note, since traumatic birth experience might change the way affected mothers interact with their infants, especially if postpartum depression is also present (e.g., avoiding contact with or being emotionally unavailable for the infant) (73, 74). Moreover, we saw a higher risk for infant regulatory disorders (sleeping and feeding problems) in mothers with birth-related traumatization and postpartum depression. This was in line with the results by Garthus-Niegel and colleagues who reported an association of PTSD and impaired child sleep (75). However, no significant associations were seen for e.g., temperament, neuropsychological development, or bonding. This was surprising since other prospective studies found maternal postpartum PTSD to be associated with poorer cognitive and social-emotional development in infants up to 2 years (19, 30). However, Garthus-Niegel et al. (19) did not find significant associations with other domains of child development (fine/gross motor or communication development) which was also not seen in our sample (19).
Taken together, our findings highlight the importance of early targeted prevention and intervention for affected women (20) and the peripartum period represents an opportunity to interrupt the pattern of intergenerational transmission of trauma. Knowledge of PTSD prior to or during pregnancy that is also associated with a higher risk of traumatic birth experience (e.g., experience of fear, helplessness or horror, or re-experiencing delivery) is crucial for health-care providers to be alert of when they treat these high-risk women (20, 76). Moreover, trauma-informed interventions should be developed and tested especially for women with PTSD and a history of interpersonal trauma or comorbid depression (74, 77). Targets that should be addressed are prevention of re-traumatization during delivery, improvement of maternal partnership problems and social support, and sensitivity training to encourage mother-child-interaction and bonding/ attachment (78–80). First evidence shows that cognitive behavioral therapy (81) and Eye Movement Desensitization and Reprocessing approaches (82–84) may improve PTSD status but require investigation in randomized controlled trials (85). Debriefing may only be successful if women are requesting it themselves (86). Since PTSD can also affect the developing relationship with the child, mother-infant bonding problems should also be addressed (20, 23). For some mothers, their infants are a reminder of their traumatic birth and may therefore trigger avoidance behaviors (i.e., non-initiation of breastfeeding) (21). Here, Mother Baby Connections, a program involving interaction therapy, has brought first promising results (87).
Strengths and Limitations
A particular feature of this investigation was the recruitment already during early pregnancy and the consideration of lifetime diagnostic status. To our knowledge this is the first study investigating both, lifetime PTSD and birth-related traumatization, with associated maternal and infant outcomes. Strengths of this study include the prospective multi-wave design and the long follow-up period. Findings are limited by small cell sizes in some clinical groups. This limits power to detect differences between the respective groups. Thus, the absence of significant differences between infants of mothers with no anxiety and depressive disorder as compared to mothers with lifetime PTSD or birth-related traumatization regarding, e.g., temperament, neuropsychological development, or bonding, should not be interpreted as indicative of negative results. It was also not possible to explore the putative cumulative risk of lifetime PTSD and birth-related traumatization on maternal and infant outcomes. Moreover, sample size prohibited examination of third variables that might also be relevant (e.g., income, education, birth outcomes) (88).
Conclusion
The study shows that PTSD is a highly debilitating disorder and affected (expectant) mothers might profit from early interventions already during pregnancy and the initial postpartum period (89). Our results highlight the crucial role of early identification and treatment of affected women. Women's health care providers should screen for PTSD and subsyndromal posttraumatic stress symptoms in routine assessments during and after pregnancy, especially in women with a reported history of trauma. Such screening will allow women to receive needed treatment and referrals and mitigate the potentially negative sequelae of PTSD (14). However, screening without sufficient services is not helpful and could be triggering for both professionals and families. Thus, a fully trauma informed perinatal system and effective trauma specific interventions during pregnancy and immediately after traumatic births is warranted to ensure that the families receive help for parenting and early bonding (77).
Finally, this post-hoc analysis was conducted with the aim of generating hypotheses for future research. Larger prospective studies are warranted to examine why interpersonal trauma is especially harmful for perinatal outcomes, and to disentangle whether this is driven by the interpersonal trauma in general, or trauma related to mothers' own childhood attachment relationships. It will be important to examine the role of hormonal alterations and other biological or psychosocial factors in the context of perinatal PTSD and to include a comprehensive assessment on psychotherapeutic and pharmacological treatments. Finally, it is important to note, that paternal PTSD after childbirth is a highly understudied and unrecognized problem that should receive more attention.
Data Availability Statement
The datasets presented in this article are not readily available because after consulting the Ethics Committee and due to the sensitive nature of the questions asked in this study, participants were assured that all raw data would remain confidential and would not be shared. Therefore, no openly assessable data files are attached. Further information on the data can be obtained from the corresponding author (JM, email: julia.martini@tu-dresden.de), the Ethics Committee of the Medical Faculty of the Technische Universität Dresden (email: ethikkommission@mailbox.tu-dresden.de), and the Institute of Clinical Psychology and Psychotherapy of the Technische Universität Dresden.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of the Technische Universität Dresden (No: EK 94042007). Written informed consent to participate in this study was provided by the participants' legal guardian.
Author Contributions
JM conceptualized and designed the study, designed the data collection instruments, collected data for the study, carried out the statistical analyses and the interpretation of the data, drafted the initial manuscript, and approved the final manuscript as submitted. EA, SK, KW, JR, and SG-N critically reviewed the manuscript and approved the final manuscript as submitted. All authors contributed to the article and approved the submitted version.
Funding
The MARI study was funded by the Institute of Clinical Psychology and Psychotherapy, Technische Universität Dresden, Germany and supported in part by the Lundbeck Institute Skodsborg, Denmark. Parts of the field work were additionally supported by the Friends and Sponsors (Gesellschaft der Freunde und Förderer) of the Technische Universität Dresden, Germany.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
Principle investigators of the MARI study are JM and Prof. Dr. Hans-Ulrich Wittchen. Core staff members of the project are Dipl.-Psych. Yvonne Hansche, Dr. Michael Höfler, Dipl.-Psych. Julia Niehoff, Dr. Johanna Petzoldt, Dipl.-Math. Jens Strehle, Dr. Gesine Wieder, Dipl.-Psych. Susanne Müllender, and Dipl.- Psych. JuliaWittich. Advisors/consultants to the project are Prof. Dr. Katja Beesdo-Baum, Dr. Franziska Einsle, and SK. This paper contributes to the EU COST Action 18211 (DEVoTION - Perinatal Mental Health and Birth-Related Trauma: Maximizing best practice and optimal outcomes) supported by COST (European Cooperation in Science and Technology). SG-N is a management committee member of COST Action CA18211.
References
- 1.Jacobi F, Höfler M, Strehle J, Mack S, Gerschler A, Scholl L, et al. Twelve-months prevalence of mental disorders in the German Health Interview and Examination Survey for Adults–Mental Health Module (DEGS1-MH): a methodological addendum and correction. Int J Methods Psychiatr Res. (2015) 24:305–13. 10.1002/mpr.1479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Erickson N, Julian M. Perinatal depression, PTSD, and trauma: Impact on mother–infant attachment and interventions to mitigate the transmission of risk. Int Rev Psychiatry. (2019) 31:245–63. 10.1080/09540261.2018.1563529 [DOI] [PubMed] [Google Scholar]
- 3.Yildiz PD, Ayers S. The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. [[i]]J Affect Disord[[/i]]. (2017) 208:634–45. 10.1016/j.jad.2016.10.009 [DOI] [PubMed] [Google Scholar]
- 4.Slade P. Towards a conceptual framework for understanding post-traumatic stress symptoms following childbirth and implications for further research. J Psychosom Obstet Gynaecol. (2006) 27:99–105. 10.1080/01674820600714582 [DOI] [PubMed] [Google Scholar]
- 5.Creedy DK, Shochet IM. Childbirth and the development of acute trauma symptoms: Incidence and contributing factors. Birth. (2000) 27:104–11. 10.1046/j.1523-536x.2000.00104.x [DOI] [PubMed] [Google Scholar]
- 6.Olde E, van der Hart O, Kleber R, van Son M. Posttraumatic stress following childbirth: a review. [[i]]Clin Psychol Rev[[/i]]. (2006) 26:1-6Soet JE. 10.1016/j.cpr.2005.07.002 [DOI] [PubMed] [Google Scholar]
- 7.Soet JE, Brack GA, Dilorio C. Prevalence and predictors of women's experience of psychological trauma during childbirth. Birth. (2003) 30:36–46. 10.1046/j.1523-536X.2003.00215.x [DOI] [PubMed] [Google Scholar]
- 8.Ayers S. Delivery as a traumatic event: prevalence, risk factors, and treatment for postnatal posttraumatic stress disorder. Clin Obstet Gynecol. (2004) 47:552–67. 10.1097/01.grf.0000129919.00756.9c [DOI] [PubMed] [Google Scholar]
- 9.Davies J, Slade P, Wright I. Posttraumatic stress symptoms following childbirth and mothers' perceptions of their infants. Infant Ment Health Jl. (2008) 29:537–54. 10.1002/imhj.20197 [DOI] [PubMed] [Google Scholar]
- 10.Grekin R, O'Hara MW. Prevalence and risk factors of postpartum posttraumatic stress disorder: a meta-analysis. Clin Psychol Rev. (2014) 34:389–401. 10.1016/j.cpr.2014.05.003 [DOI] [PubMed] [Google Scholar]
- 11.Andersen LB. Melvaer LB, Videbech P, Lamont RF Risk factors for developing post-traumatic stress disorder following childbirth: a systematic review. Acta Obstet Gynecol Scand. (2012) 91:1261–72. 10.1111/j.1600-0412.2012.01476.x [DOI] [PubMed] [Google Scholar]
- 12.Ayers S, Bond R, Bertullies S. The aetiology of post-traumatic stress following childbirth: a meta-analysis and theoretical framework. Psychol Med. (2016) 46:1121–34. 10.1017/S0033291715002706 [DOI] [PubMed] [Google Scholar]
- 13.Garthus-Niegel S, von Soest T, Vollrath ME. The impact of subjective birth experiences on post-traumatic stress symptoms: a longitudinal study. Arch Womens Ment Health. (2013) 16:1–10. 10.1007/s00737-012-0301-3 [DOI] [PubMed] [Google Scholar]
- 14.Geller PA, Stasko EC. Effect of previous posttraumatic stress in the perinatal period. J Obstet Gynecol Neonatal Nurs. (2017) 46:912-22. 10.1016/j.jogn.2017.04.136 [DOI] [PubMed] [Google Scholar]
- 15.Cook CAL. Flick LH, Homan SM, Campbell C, McSweeney M Posttraumatic stress disorder in pregnancy: prevalence, risk factors, and treatment. Obstet Gynecol. (2004) 103:710–7. 10.1097/01.AOG.0000119222.40241.fb [DOI] [PubMed] [Google Scholar]
- 16.Parfitt YM. The effect of post-natal symptoms of post-traumatic stress and depression on the couple's relationship and parent–baby bond. J Reprod Infant Psychol. (2009) 27:127–42. 10.1080/02646830802350831 [DOI] [Google Scholar]
- 17.Skari H, Skreden M, Malt UF, Dalholt M, Ostensen AB, Egeland T, et al. Comparative levels of psychological distress, stress symptoms, depression and anxiety after childbirth: a prospective population-based study of mothers and fathers. BJOG Int J Obstet Gynaecol. (2002) 109:1154–63. 10.1111/j.1471-0528.2002.00468.x [DOI] [PubMed] [Google Scholar]
- 18.Asselmann E, Wittchen HU, Petzoldt J, Martini J. Peripartum changes in partnership quality among women with and without anxiety and depressive disorders prior to pregnancy: a prospective-longitudinal study. Arch Womens Ment Health. (2016) 19:281-90. 10.1007/s00737-015-0556-6 [DOI] [PubMed] [Google Scholar]
- 19.Garthus-Niegel S Ayers S Martini J von von Soest T The impact of postpartum post-traumatic stress disorder symptoms on child development: a population-based 2-year follow-up study . Psychol Med. (2017) 47:161–70. 10.1017/S003329171600235X [DOI] [PubMed] [Google Scholar]
- 20.Beck CT. Post-traumatic stress disorder due to childbirth: The aftermath. Nurs Res. (2004) 53:216–24. 10.1097/00006199-200407000-00004 [DOI] [PubMed] [Google Scholar]
- 21.Garthus-Niegel S, Horsch A, Ayers S, Junge-Hoffmeister J, Weidner K, Eberhard-Gran M. The influence of postpartum PTSD on breastfeeding: a longitudinal population-based study. Birth. (2018) 45:193–201. 10.1111/birt.12328 [DOI] [PubMed] [Google Scholar]
- 22.Horta BL Bahl R Martinés JC Victora CG World Health Organization . Evidence on the long-term effects of breastfeeding: systematic review and meta-analyses. [Google Scholar]
- 23.Ballard C, Stanley A. Post-traumatic stress disorder (PTSD) after childbirth. Br J Psychiatry. (1995) 166:525–8. 10.1192/bjp.166.4.525 [DOI] [PubMed] [Google Scholar]
- 24.Moleman N, Van der Hart O, Van der Kolk BA. The partus stress reaction: a neglected etiological factor in postpartum psychiatric disorders. J Nerv Ment Dis. (1992) 180:271–2. 10.1097/00005053-199204000-00010 [DOI] [PubMed] [Google Scholar]
- 25.Ammerman RT, Putnam FW, Chard KM, Stevens J. PTSD in depressed mothers in home visitation. Psychol Trauma. (2012) 4:186. 10.1037/a0023062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Muzik M, Morelen D, Hruschak J, Rosenblum KL, Bocknek E. Psychopathology and parenting: an examination of perceived and observed parenting in mothers with depression and PTSD. J Affect Disord. (2017) 207:242–50. 10.1016/j.jad.2016.08.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Christie H, Hamilton-Giachritsis C, Alves-Costa F, Tomlinson M, Halligan SL. The impact of parental posttraumatic stress disorder on parenting: a systematic review. Eur. J. Psychotraumatol. (2019) 10:1550345. 10.1080/20008198.2018.1550345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lang AJ, Gartstein MA. Intergenerational transmission of traumatization: Theoretical framework and implications for prevention. J Trauma Dissoc. (2018) 19:162–75. 10.1080/15299732.2017.1329773 [DOI] [PubMed] [Google Scholar]
- 29.Pat-Horenczyk R, Cohen S, Ziv Y, Achituv M, Asulin-Peretz L, Blanchard TR, et al. Emotion regulation in mothers and young children faced with trauma. Infant Ment Health J. 2015 36:337-48Parfitt Y. Pike A Infant developmental outcomes: a family systems perspective Infant Child Dev. (2014) 23:353–73. 10.1002/imhj.21515 [DOI] [PubMed] [Google Scholar]
- 30.Parfitt Y, Pike A. Infant developmental outcomes: a family systems perspective. Infant Child Dev. (2014) 23:353–73. 10.1002/icd.1830 [DOI] [Google Scholar]
- 31.Seng JS, D'Andrea W. Complex mental health sequelae of psychological trauma among women in prenatal care. Psychol Trauma Theory Res Pract Policy. (2014) 6:41. 10.1037/a0031467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wosu AC, Gelaye B. Childhood sexual abuse and posttraumatic stress disorder among pregnant and postpartum women: Review of the literature. Arch Womens Ment Health. (2015) 18:61–72. 10.1007/s00737-014-0482-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Horesh D, Garthus-Niegel S, Horsch A. Childbirth-related PTSD: is it a unique post-traumatic disorder. J Reprod Infant Psychol. (2021) 39:221–4. 10.1080/02646838.2021.1930739 [DOI] [PubMed] [Google Scholar]
- 34.McKenzie-McHarg K, Ayers S, Ford E, Horsch A, Jomeen J, Sawyer A, et al. Post-traumatic stress disorder following childbirth: An update of current issues and recommendations for future research. J Reprod Infant Psychol. (2015) 33:219–37. 10.1080/02646838.2015.1031646 [DOI] [Google Scholar]
- 35.Martini J, Petzoldt J, Einsle F, Beesdo-Baum K, Höfler M, Wittchen HU. Risk factors and course patterns of anxiety and depressive disorders during pregnancy and after delivery: a prospective-longitudinal study. J Affect Disord. (2015) 175:385–95. 10.1016/j.jad.2015.01.012 [DOI] [PubMed] [Google Scholar]
- 36.Martini J, Wittich J, Petzoldt J, Winkel S, Einsle F, Siegert J, et al. Maternal anxiety disorders prior to conception, psychopathology during pregnancy and early infants' development: A prospective-longitudinal study. Arch Womens Ment Health. (2013) 16:549–60. 10.1007/s00737-013-0376-5 [DOI] [PubMed] [Google Scholar]
- 37.Martini J, Wittchen HU, Soares CN, Rieder A, Steiner M. New women-specific diagnostic modules: the Composite International Diagnostic Interview for Women (CIDI-VENUS). Arch Womens Ment Health. (2009) 12:281–9. 10.1007/s00737-009-0077-2 [DOI] [PubMed] [Google Scholar]
- 38.Kessler RC, Ustun TB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res. (2004) 13:93–121. 10.1002/mpr.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reed V, Gander F, Pfister H, Steiger A, Sonntag H, Trenkwalder C, et al. To what degree does the Composite International Diagnostic Interview (CIDI) correctly identify DSM-IV disorders? Testing validity issues in a clinical sample. Int J Methods Psychiatr Res. (1998) 7:142–55. 10.1002/mpr.44 [DOI] [Google Scholar]
- 40.Wittchen HU, Lachner G, Wunderlich U, Pfister H. Test-retest reliability of the computerized DSM-IV version of the Munich-Composite International Diagnostic Interview (M-CIDI). Soc Psychiatry Psychiatr Epidemiol. (1998) 33:568–78. 10.1007/s001270050095 [DOI] [PubMed] [Google Scholar]
- 41.Hansche Y, Fischer J, Gloster A, Martini J. Wijma Fragebogen zum Geburtserleben, Version A und B. Dresden: TU Dresden. (2009). [Google Scholar]
- 42.Weigl T. Questionnaires for the assessment of birth expectancy and birth experience (Part 2 of a series on psychological assessment during the peripartum period). Z Geburtshilfe Neonatol. (2021). 225:392–6. 10.1055/a-1471-7714 [DOI] [PubMed] [Google Scholar]
- 43.Wijma K, Wijma B, Zar M. Psychometric aspects of the W-DEQ; a new questionnaire for the measurement of fear of childbirth. J Psychosom Obstet Gynaecol. (1998) 19:84–97. 10.3109/01674829809048501 [DOI] [PubMed] [Google Scholar]
- 44.Ryding EL, Persson A, Onell C. An evaluation of midwives' counseling of pregnant women in fear of childbirth. Acta Obstet Gynecol Scand. (2003) 82:10–7. 10.1034/j.1600-0412.2003.820102.x [DOI] [PubMed] [Google Scholar]
- 45.Wijma K, Wijma B, Zar M. Psychometric aspects of the W-DEQ: a new questionnaire for the measurement of fear of childbirth. J Psychosom Obstet Gynaecol. (1998) 19:84–97. 10.3109/01674829809048501 [DOI] [PubMed] [Google Scholar]
- 46.Gemeinsamer Bundesausschuss der Ärzte und Krankenkassen. German Mutterpass (2013). Available online at: https://www.g-ba.de/downloads/83-691-325/2013-07-01Mutterpass.pdf
- 47.Hoyer J . KfS: Kurzfragebogen zu sexuellen Funktionsstörungen. In: Strauß B, E. Brähler, editors. Deutschsprachige Verfahren in der Sexualwissenschaft. Göttingen: Hogrefe. (2015). pp. 113 [Google Scholar]
- 48.Hoyer J, Uhmann S, Rambow J. Reduction of sexual dysfunction: By-product of cognitive-behavioural therapy for psychological disorders? J Sex Marital Ther. (2009) 24:64–73. 10.1080/14681990802649938 [DOI] [Google Scholar]
- 49.Labbate LA, Lare SB. Sexual dysfunction in male psychiatric outpatients: Validity of the Massachusetts General Hospital Sexual Functioning Questionnaire. Psychother Psychosom. (2001) 70:221–5. 10.1159/000056257 [DOI] [PubMed] [Google Scholar]
- 50.Schneider S. [[i]]Diagnostisches Interview zur Erfassung von Regulationsstörungen im Säuglings-und Kleinkindalter (Baby-DIPS)[[/i]]. Basel: Universität Basel. (2007). [Google Scholar]
- 51.Wessel MA, Cobb JC, Jackson EB, Harris GS. Paroxysmal fussing in infancy, sometimes called “colic”. Pediatrics. (1954) 14:421–35. 10.1542/peds.14.5.421 [DOI] [PubMed] [Google Scholar]
- 52.Petzoldt J, Wittchen HU, Einsle F. Maternal anxiety versus depressive disorders: Specific relations to infants' crying, feeding and sleeping problems. Child Care Health Dev. (2016) 42:231–45. 10.1111/cch.12292 [DOI] [PubMed] [Google Scholar]
- 53.Popp L, Fuths S, Seehagen S, Bolten M, Gross-Hemmi M, Wolke D, et al. Inter-rater reliability and acceptance of the structured diagnostic interview for regulatory problems in infancy. Child Adolesc Psychiatry Ment Health. (2016) 10:1–10. 10.1186/s13034-016-0107-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Martini J, Petzoldt J, Knappe S, Garthus-Niegel S, Asselmann E, Wittchen HU. Infant, maternal, and familial predictors and correlates of regulatory problems in early infancy: The differential role of infant temperament and maternal anxiety and depression. Early Hum Dev. (2017) 115:23–31. 10.1016/j.earlhumdev.2017.08.005 [DOI] [PubMed] [Google Scholar]
- 55.Reck C, Klier CM, Pabst K, Stehle E, Steffenelli U, Struben K, et al. The German version of the postpartum bonding instrument: psychometric properties and association with postpartum depression. Arch Womens Ment Health. (2006) 9:265–71. 10.1007/s00737-006-0144-x [DOI] [PubMed] [Google Scholar]
- 56.Brockington IF. Fraser C. The Postpartum Bonding Questionnaire: a validation. Arch Womens Ment Health. (2006) 9:233–42. 10.1007/s00737-006-0132-1 [DOI] [PubMed] [Google Scholar]
- 57.Kagan J. Infant predictors of inhibited and uninhibited profiles. Psychol Sci. (1991) 2:40–4. 10.1111/j.1467-9280.1991.tb00094.x [DOI] [Google Scholar]
- 58.Petermann F, Renziehausen A. Neuropsychologisches Entwicklungs-Screening (NES). Bern: Huber. (2005). [Google Scholar]
- 59.Ainsworth M, Blehar M, Waters E. Patterns of attachments: a psychological study of the Strange Situation. Hillsdale: Earlbaum. (1978). [Google Scholar]
- 60.Kagan J. Galen's prophecy: temperament in human nature. New York, NY: Basic Books. (1994). [Google Scholar]
- 61.Bakeman R, McArthur D, Quera V. Detecting sequential patterns and determining their reliability with fallible observers. Psychol Methods. (1997) 2:357. 10.1037/1082-989X.2.4.357 [DOI] [Google Scholar]
- 62.Main M, Solomon J. Procedures for identifying infants as disorganized/disoriented during the Ainsworth Strange Situation. In: Greenberg M, Cicchetti D, Cummings E, editors. [[i]]Attachment in the preschool years: Theory, research, and intervention[[/i]]. (1990). p. 121–60. [Google Scholar]
- 63.Murray L, Fiori-Cowley A, Hooper R, Cooper P. The impact of postnatal depression and associated adversity on early mother-infant interactions and later infant outcome. Child Dev. (1996) 67:2512–26. 10.2307/1131637 [DOI] [PubMed] [Google Scholar]
- 64.Kraft A, Knappe S, Petrowski K, Petzoldt J. Maternal bonding and infant attachment in women with and without social phobia. Zeitschrift fur Kinder-und Jugendpsychiatrie und Psychotherapie. (2016) 45:49–57. 10.1024/1422-4917/a000454 [DOI] [PubMed] [Google Scholar]
- 65.StataCorp . Stata Statistical Software. Release. (2012) 12:1. [Google Scholar]
- 66.Blalock JA, Nayak N, Wetter DW, Schreindorfer L, Minnix JA, Canul J, et al. The relationship of childhood trauma to nicotine dependence in pregnant smokers. Psychol Addict Behav. (2011) 25:652. 10.1037/a0025529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gisladottir A, Harlow BL, Gudmundsdottir B, Bjarnadottir RI, Jonsdottir E, Aspelund T, et al. Risk factors and health during pregnancy among women previously exposed to sexual violence. Acta Obstet Gynecol Scand. (2014) 93:351–8. 10.1111/aogs.12331 [DOI] [PubMed] [Google Scholar]
- 68.Leeners B, Rath W, Block E, Görres G. Risk factors for unfavorable pregnancy outcome in women with adverse childhood experiences. J Perinat Med. (2014) 42:171–8. 10.1515/jpm-2013-0003 [DOI] [PubMed] [Google Scholar]
- 69.Morland L, Goebert D, Onoye J, Frattarelli L, Derauf C, Herbst M, et al. Posttraumatic stress disorder and pregnancy health: preliminary update and implications. Psychosomatics. (2007) 48:304–8. 10.1176/appi.psy.48.4.304 [DOI] [PubMed] [Google Scholar]
- 70.Yehuda R, Lehrner A. Intergenerational transmission of trauma effects: Putative role of epigenetic mechanisms. World Psychiatry. (2018) 17:243–57. 10.1002/wps.20568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Moisiadis VG, Matthews SG. Glucocorticoids and fetal programming part 2: Mechanisms. Nat Rev Endocrinol. (2014) 10:403–11. 10.1038/nrendo.2014.74 [DOI] [PubMed] [Google Scholar]
- 72.Asselmann E, Hoyer J, Wittchen HU, Martini J. Sexual problems during pregnancy and after delivery among women with and without anxiety and depressive disorders prior to pregnancy: a prospective-longitudinal study. J Sex Med. (2016) 13:95-104. 10.1016/j.jsxm.2015.12.005 [DOI] [PubMed] [Google Scholar]
- 73.Muzik M, Bocknek EL, Broderick A, Richardson P, Rosenblum KL, Thelen K, et al. Mother-infant bonding impairment across the first 6 months postpartum: the primacy of psychopathology in women with childhood abuse and neglect histories. Arch Womens Ment Health. (2013) 16:29–38. 10.1007/s00737-012-0312-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Seng JS, Sperlich M, Low LK, Ronis DL, Muzik M. Childhood abuse history, posttraumatic stress disorder, postpartum mental health, and bonding: prospective cohort study. J Midwifery Womens Health. (2013) 58:57–68. 10.1111/j.1542-2011.2012.00237.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Garthus-Niegel S, Horsch A, Graz MB, Martini J, von Soest T, Weidner K, et al. The prospective relationship between postpartum PTSD and child sleep: a 2-year follow-up study. J Affect Disord. (2018) 241:71–9. 10.1016/j.jad.2018.07.067 [DOI] [PubMed] [Google Scholar]
- 76.Choi KR., Seng JS. Predisposing and precipitating factors for dissociation during labor in a cohort study of posttraumatic stress disorder and childbearing outcomes. J Midwifery Womens Health. (2016) 61:68–76. 10.1111/jmwh.12364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Stevens NR Miller ML Puetz A-K Padin AC Adams N Psychological intervention and treatment for posttraumatic stress disorder during pregnancy: a systematic review and call to action . J Trauma Stress. (2021) 34:575–85. 10.1002/jts.22641 [DOI] [PubMed] [Google Scholar]
- 78.Asselmann E, Venz J, Wittchen HU, Martini J. Maternal anxiety and depressive disorders prior to, during and after pregnancy and infant interaction behaviors during the Face-to-Face Still Face Paradigm at 4 months postpartum: a prospective-longitudinal study. Early Hum Dev. (2018) 122:45–53. 10.1016/j.earlhumdev.2018.05.007 [DOI] [PubMed] [Google Scholar]
- 79.Furuta M, Horsch A, Ng ES, Bick D, Spain D. Effectiveness of trauma-focused psychological therapies for treating post-traumatic stress disorder symptoms in women following childbirth: a systematic review and meta-analysis. Front Psychiatry. (2018) 9:591. 10.3389/fpsyt.2018.00591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mantler T, Jackson KT, Walsh EJ, Jackson B, Baer JR, Davidson CA, et al. Promoting Attachment Through Healing (PATH): results of a retrospective feasibility study providing trauma-and-violence-informed care to pregnant women. J Adv Nurs. (2021). 10.1111/JAN.15117/v2/decision1 [DOI] [PubMed] [Google Scholar]
- 81.Nieminen K, Berg I, Frankenstein K, Viita L, Larsson K, Persson U, et al. Internet-provided cognitive behaviour therapy of posttraumatic stress symptoms following childbirth: a randomized controlled trial. Cogn Behav Ther. (2016) 45:287–306. 10.1080/16506073.2016.1169626 [DOI] [PubMed] [Google Scholar]
- 82.Chiorino V, Cattaneo MC, Macchi EA, Salerno R, Roveraro S, Bertolucci GG, et al. The EMDR Recent Birth Trauma Protocol: A pilot randomised clinical trial after traumatic childbirth. Psychol Health. (2020) 35:795–810. 10.1080/08870446.2019.1699088 [DOI] [PubMed] [Google Scholar]
- 83.Sandström M, Wiberg B, Wikman M, Willman AK, Högberg U. A pilot study of eye movement desensitisation and reprocessing treatment (EMDR) for post-traumatic stress after childbirth. Midwifery. (2008) 24:62-73. 10.1016/j.midw.2006.07.008 [DOI] [PubMed] [Google Scholar]
- 84.Stramrood CA van der Velde J Doornbos B Marieke Paarlberg K Weijmar Weijmar Schultz WC The patient observer: eye-movement desensitization and reprocessing for the treatment of posttraumatic stress following childbirth . Birth. (2012) 39:70–6. 10.1111/j.1523-536X.2011.00517.x [DOI] [PubMed] [Google Scholar]
- 85.Lapp K, Agbokou C, Peretti C-S. Management of post traumatic stress disorder after childbirth: a review. J Psychosom Obstet Gynaecol. (2010) 31:113–22. 10.3109/0167482X.2010.503330 [DOI] [PubMed] [Google Scholar]
- 86.Bruijn de, Stramrood LCA. Lambregtse-van den Berg MP, Rius Ottenheim N. Treatment of posttraumatic stress disorder following childbirth J Psychosom Obstet Gynaecol. (2020) 41:5–14. 10.1080/0167482X.2019.1593961 [DOI] [PubMed] [Google Scholar]
- 87.Geller PA, Posmontier B, Horowitz JA, Bonacquisti A. Introducing mother baby connections: a model of intensive perinatal mental health outpatient programming. J Behav Med. (2018) 41:600–13. 10.1007/s10865-018-9974-z [DOI] [PubMed] [Google Scholar]
- 88.Yonkers KA, Smith MV, Forray A, Epperson CN, Costello D, Lin H, et al. Pregnant women with posttraumatic stress disorder and risk of preterm birth. JAMA psychiatry. (2014) 71:897–904. 10.1001/jamapsychiatry.2014.558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Marchand A, Todorov C, Borgeat F. Effectiveness of a brief cognitive behavioural therapy for panic disorder with agoraphobia and the impact of partner involvement. Behav Cogn Psychother. (2007) 35:613–29. 10.1017/S1352465807003888 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets presented in this article are not readily available because after consulting the Ethics Committee and due to the sensitive nature of the questions asked in this study, participants were assured that all raw data would remain confidential and would not be shared. Therefore, no openly assessable data files are attached. Further information on the data can be obtained from the corresponding author (JM, email: julia.martini@tu-dresden.de), the Ethics Committee of the Medical Faculty of the Technische Universität Dresden (email: ethikkommission@mailbox.tu-dresden.de), and the Institute of Clinical Psychology and Psychotherapy of the Technische Universität Dresden.