Abstract
Pseudoexfoliation syndrome (PEXS) is a systemic disease caused by defects in the extracellular matrix (ECM) remodelling process leading to the chronic deposition of extracellular, fibrillary, white flaky pseudoexfoliation material (PEXM) throughout the body. Specifically, PEXM deposits on the lens capsule cause open-angle glaucoma, cataracts and blindness in patients with PEXS. Several gene single nucleotide polymorphisms are linked to the development of PEXS in humans, including lysyl oxidase-like 1 gene, clusterin and fibulin-5. The exact reason for the PEXM generation and its resulting pathogenesis is not well understood. However, defective ECM remodelling and oxidative stress (OS) have been hypothesized as significant events leading to the PEXM. Specifically, the link between OS and PEXS has been well studied, although the investigation is still ongoing. The present review explored recent advances in various aspects of PEXS and the involvement of OS in the eye for PEXS development.
Keywords: pseudoexfoliation syndrome, oxidative stress, extracellular matrix remodelling, eye diseases, antioxidants
1. Introduction
Pseudoexfoliation syndrome (PEXS) is an age-associated systemic disorder characterised by abnormal production and turnover of extracellular matrix (ECM), leading to the progressive deposition of extracellular, fibrillary, white flaky deposits in different tissues and organs of the body. ECM is a 3-dimensional network of interacting macromolecular effectors that apart from tissue support and integrity affects growth factors availability, cell signaling and functional properties such as oxidative stress (OS) pathways (1,2). The most commonly affected ocular tissues reveal deposition of pseudoexfoliation material (PEXM) in the pupillary margin of the iris (3-5). These alterations are responsible for pathological changes and sequelae in the anterior part of the eye, such as cataracts, zonular weakness, phacodonesis, lens subluxation/dislocation, iris rigidity and synechiae, blood-aqueous barrier dysfunction, melanin dispersion, capillary haemorrhage, poor mydriasis, radial body complication, trabecula impairment, keratopathy, and even retinal vein occlusion in the posterior eye segment (6,7). As a result of the PEXM deposit on the lens capsule, a higher rate of open-angle glaucoma cataracts and resulting blindness was observed in most PEXS patients. In addition to the eye, deposits are also found around the blood vessels of the connective tissue and organs such as the lungs, heart, liver, kidneys, gallbladder, and meninges (8-10). Studies suggest that PEXM is associated with the development of systemic hypertension, myocardial infarction and cerebrovascular events.
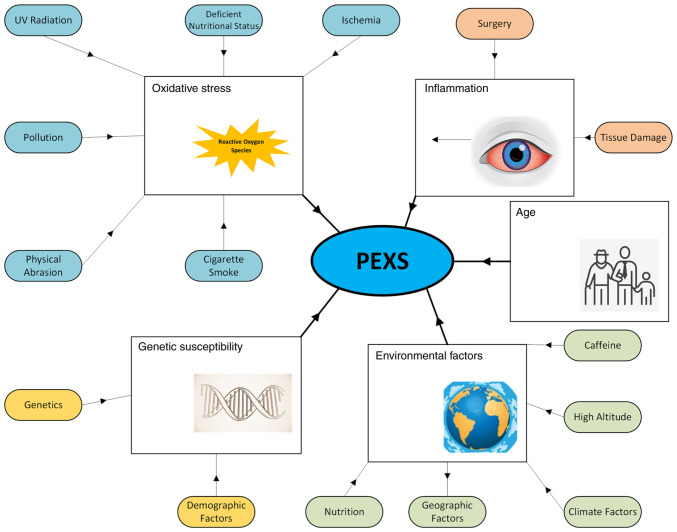
Lindberg firstly described PEXS in 1917, when observed the whitish-grey material deposit on the pupillary border in glaucoma patients. However, the term PEXS was coined later in 1954 by Dvorak-Theobald, who noticed the aggregation of PEXM on the lens capsule, ciliary body, and zonules (3-5). Ocular deposition of PEXM can be found in all structures of the anterior part of the eye (11,12). PEXM deposits can be macroscopically observed during the dilated slit-lamp examination and anterior segment optical coherence tomography. Although the production site of PEXM has not yet been identified, it is hypothesized to be synthesised either from the iris, lens epithelium, ciliary body or trabecula (11,13). Studies identified the chemical nature of the PEXM deposits, and it is made up of a complex glycoprotein/proteoglycan matrix comprising glycosaminoglycan, chondroitin and heparin sulfate, and tropoelastin. Further, it also consists of fibrillin-1, fibronectin, vitronectin, laminin, collagen, amyloid, nidogen/entactin, microfibril-associated glycoprotein, latent TGF-b binding proteins, residues of galactose, a-mannose, N-acetyl-D-glucosamine, lysyl oxidase-like 1 (LOXL1), and apolipoprotein E (14-16). The particles of this abnormal material are insoluble, follow the aqueous humor's (AH) natural flow, and are finally deposited in the trabecula. Gradually, they inhibit the normal outflow of AH, leading to an increase in the intraocular pressure (17) and the development of a severe type of open-angle glaucoma, identified as PEXG (pseudoexfoliation glaucoma). PEXG is the most commonly recognised cause of open-angle glaucoma worldwide, accounting for 25% of this type of glaucoma. The 10-year cumulative probability of PEXS patients developing PEXG is ~15% (18). PEXG is characterised by progressive degeneration of retinal ganglion cells, and their axons affect peripheral vision and result in a severe and irreversible visual loss (12,19). Therefore, prompt diagnosis of PEXS/PEXG is crucial because the affected patients have rapid and severe clinical course, poorer response to medications, higher rates of surgical complications, and worse prognosis than other forms of open-angle glaucoma (12). Considering this and the significant impact of PEXS and PEXG in terms of patient health and socio-economic costs, there is a necessity for innovative preventive and therapeutic policies. However, advances in treatment are mainly based upon an in-depth comprehension of the underlying molecular mechanisms, especially in the early stages of the disease (20). Although the specific pathogenesis of this condition remains unknown, various studies have suggested OS, diminished cellular defence status, and ischemia being the most frequently reported factors (Fig. 1) (21).
Figure 1.
Factors associated with the onset and progression of PEXS. PEXS, pseudoexfoliation syndrome.
Although the cause of the deposition and its resulting pathogenesis is not well understood, the role of ECM remodelling and OS has been studied in detail. Specifically, the link between OS and PEXS has been well established in recent years. In this review, we discuss advances in the pathogenesis of PEXS, especially the involvement of OS.
2. Methods
A systematic review of the literature published in English was performed from November 2021 to March 2022 in order to identify all published reports pertaining OS in PEXS in the eye. Studies were identified through a search consisting of: (1) a computerized search of Cochrane, Scopus and PubMed (National Library of Medicine) databases from January 1952 through January 2022, (2) review of major ophthalmic textbooks and (3) the database ClinicalTrials.gov (www.clinicaltrials.gov) was also searched for information about clinical trials. The following keywords and MeSH terms were used ‘pseudoexfoliation’, ‘pseudoexfoliation syndrome’, ‘pseudoexfoliation material’, ‘oxidative stress’, ‘reactive oxygen species’, ‘eye’, ‘pathogenesis’. The searches were performed by three independent investigators (MP, PP and KK had equal contribution and performed the literature review and analysed the data). We only included articles with full text available in English. All pertinent articles were thoroughly assessed, and their reference lists were searched to identify other potentially relevant studies. The reviewers came to consensus on the selection of full texts through discussion. CDG approved the final list of included studies, finalized the work and is the academic supervisor.
3. Incidence of PEXS
PEXS is a multifactorial disease which is widespread worldwide. Although PEXS occurrence is negligible in the middle-aged population, its global incidence varies considerably across populations and countries, with the reported prevalence of PEXS ranging from 1.5 to 40.9% worldwide (22,23). The prevalence of PEXS varies from 3.6 to 34.2% in European countries, from 1.5 to 22.1% in Asian countries, and from 1.5 to 40% in African countries, suggesting a general lack of consensus on these epidemiologic studies (22,23). As of yet, it is unclear whether incidence of PEXS varies across populations or whether the reported variation could be because of study parameters such as study design, location, age of the population and target sample size. Nevertheless, older age, Scandinavian and Mediterranean race, genetic mutations, and solar/cosmic radiation are considered major risk factors for PEXS (24,25). Especially, PEXS have a high incidence among Scandinavians, and half of open-angle glaucoma cases are caused by pseudoexfoliation in this population (7). Population studies have shown that PEXS is rarely observed before the age of 40, and its incidence increases with age (Fig. 1). Several studies on the PEXS estimated a 5 to 20% prevalence in an aged population regardless of geographical features (26). Specifically, PEXS is common in individuals >50 years, with its incidence increasing with age. Notably, the prevalence rates of PEXS are 25% in Icelanders over the age of 60, 20% in Finlanders, 0 in the Inuit population, 4.7% in Germans, and 4% in English individuals (27-29). Notably, the prevalence of PEXS was 5.0% over the age of 40 in Turkey. Further the population-based studies suggest the prevalence of PEXS in India (1.5%), Pakistan (6.4%), England (4.0%), Saudi Arabia (9.3%), China (0.4%), Germany (4.7%), Saudi Arabia (9.3%), Greece (11.5-17%) and Norway (6.3%). In general, there was no gender preference in PEXS occurrence (22,27-30). Besides, although PEXS is an age-related disorder and most affected individuals are over 50 years old, there are also reported cases at younger ages (31). In these cases, it was remarkable that all patients had previously undergone one or more intraocular procedures, and so it was suggested that might be a causative association (31).
4. Genetic susceptibility of PEXS
Genetic studies conducted in populations worldwide clearly suggest a significant role of genetics in the pathogenesis of PEXS (Fig. 1). Initially, the genetic basis of PEXS was uncovered through a genome-wide association study (GWAS) conducted on northern Europeans. Two single nucleotide polymorphisms (SNPs), rs1048661, and rs3825942, located in the coding region of the lysyl oxidase-like one gene (LOXL1), were linked to the development of PEXS in Scandinavians (32). LOXL1, a gene that encodes a lysyl oxidase, catalyses elastin and collagen crosslinking, located on chromosome region 15q24.1, is essential for elastin fibre formation and homeostasis. After this initial observation, the association between these LOXL1 variants and PEXS has been extensively studied worldwide. Subsequent genetic studies have demonstrated that SNPs in exon 1 of the LOXL1 gene indicate the critical genetic risk factor for PEXS and PEXG in different individuals (9,33). These two SNPs of the LOXL1 gene have been identified across the globe (80-100%) in PEXS/PEXG patients. Especially the association of LOXL1 SNPs with PEXS have been found in several human populations, including Europe, North America, Asia, Africa, and Australia.
In addition to LOXL1 polymorphisms, loss of heterozygosity (LOH) was observed in 94.11% of PEXS patients, with the highest incidence being observed in the markers D13S175, D7S478 and D7S479. The authors concluded that LOH possibly suggests a genetic role in PEXS pathogenesis (34,35). Its correlation with the altitude at which these patients lived could indicate an increased vulnerability to ultraviolet radiation (UVR) in the examined chromosomal regions (34,35). Similarly, genetic variants in Calcium Voltage-Gated Channel Subunit Alpha1 A (CACNA1A) are linked with susceptibility to PEXS. Studies indicate that CACNA1A could change calcium levels at the cell surface leading to PEXM deposition (9,33,36). Besides, PEXS pathogenesis has been linked to fibulin-5 (FBLN5), an extracellular framework protein that activates LOXL1, in PEXS progression. The authors reported that two novel noncoding polymorphisms within the FBLN5 gene were significantly associated with PEXS as risk factors (37). Interestingly, the mRNA and protein expression levels of FBLN5 are reduced in PEXS affected lens capsules, and this downregulation is associated with ECM remodelling (37).
5. Environmental factors affecting PEXS onset and progression
Nutrition plays an essential role in the progression and pathogenesis of PEXS (Fig. 1). A diet containing nutrients such as selenium can regulate the PEXS onset and progression. OS has also been linked to PEXS pathogenesis in the presence of nutrient deficiences (38). Specifically, regular consumption of dietary fibre-rich vegetables and fruits, particularly when started from a young age, has been related to a lower risk of PEXS occurrence, signifying an antioxidative and protective role against this condition. Similarly, mild to moderate caffeine consumers were less likely to present PEXS than those who consume a lot of coffee (39,40). It has been proposed that caffeine consumption on a long-term basis may contribute to a continuous PEXM accumulation in the eye.
Moreover, caffeine consumption has been shown to increase plasma homocysteine (Hcy) concentrations (41,42). Since Hcy has also been found elevated in AH, tear fluid and serum of PEXS patients (43), it could be suggested that the Hcy-increasing effect of caffeine may signify a good association between coffee consumption and PEXS (20). It is also known that Hcy has pro-oxidant action. Its high concentrations may participate in the abnormal ECM repair detected in PEXS and other tissues, thus explaining the high vascular risk observed in PEXS patients (11,12). Therefore, it would be rational for such patients, especially those with bilateral eye involvement, to have total serum Hcy levels screened.
In a study by Kozobolis et al (44) about the epidemiology of pseudoexfoliation on the island of Crete, Greece, the authors reported that the prevalence of PEXS was higher in men and increased with age. They also found a possible correlation with high altitude and that PEXS was a risk factor for early intraocular presure (IOP) disturbances, especially in women. In two large studies from the USA, demographic, geographic and climatic factors were associated with PEXS occurrence (45,46). The authors examined mainly Caucasian individuals of different European ancestry and could not identify differences in PEXS incidence among the various descents. They found that participants who lived in the middle and southern regions of the country exhibited a reduced risk of PEXS, and they concluded that ambient temperature and sun exposure might be significant environmental factors involved in PEXS pathogenesis, as recent studies also confirmed (47,48).
6. Pathogenesis of PEXS
The pathogenesis of PEXS manifested mainly through the generation and deposition of insoluble fibrillary extracellular material on connective tissues and tissues close to the bloodstream. Other pathological changes that contribute to the PEXS include dysregulated degradation and ECM production, increased inflammation, and enhanced OS. Since PEXM is insoluble, it aggregates at the trabecular meshwork and blocks the normal flow of AH and thus, increasing the intraocular pressure in the eye. Although the primary cause is not yet understood, it is hypothesized that the PEXM deposition is one of the reasons for complications, including cataracts, zonular weakness, and lens dislocation.
LOXL1
Defects in the functions of LOXL1 are one of the major contributors to abnormal deposits of PXEM in ocular tissues. LOXL1 essentially maintains the homeostasis of fibrillar ECM via regulating the generation, maintenance and repair of the elastic connective tissue (49). LOXL1 essentially acts as a framework element ensuring spatially defined elastin deposition. Particularly, LOXL1 is involved in the crosslinking of elastin and collagen through its pro-peptide, which binds to both fibulin-5 and tropoelastin to target elastic microfibrils at elastogenesis sites (49). It has been demonstrated that LOXL1 is a vital factor in preventing age-related elastic fibre damage and loss of elasticity (50). Furthermore, LOXL1 expression is essential for standard IOP control, while deficiency causes modified conventional outflow physiology and ECM repair and homeostasis (51). Specifically, the fibrillar material deposits found in PEXS patients contain elastin and tropoelastin, suggesting the link between defects of LOXL1 and the pathogenesis of PEXS. Changes in LOXL1 activation can result in an excessive aggregation of elastic fibre fragments into PEXS eyes.
Further, LOXL1 deficiency was found in the eye, and its deficiency increases susceptibility to optic nerve damage (52). Since the dysregulation in elastic fibre production and crosslinking is hypothesized to be the major contributor to the pathogenesis of PEXS, LOXL1 expression and polymorphisms have also been linked to the pathogenesis of this syndrome. Besides this, OXL1-AS1, a long non-coding RNA (lncRNA) synthesised from the LOXL1 gene, also has been linked to the PEXS. The nuclear LOXL1-AS1 selectively bind to the mRNA processing protein, the heterogeneous nuclear ribonucleoprotein-L (hnRNPL). Both have a vital role in regulating total gene expression in eye cells. Interestingly, SNPs regulating the expression of LOXL1-AS1 have been found in the patients of PEXS, suggesting the vital role of the LOXL1 gene in the pathogenesis of PEXS (53).
TGF-β1
Another critical protein involved in the ECM remodelling and the pathogenesis of PEXS is tumor growth factor-β1 (TGF-β1), a fibrosis-associated growth factor found in high levels, specifically in fibrotic diseases and experimental fibrosis models (54). Increased TGF-β1 levels were noted in the AH of PEXS patients, and it has been associated with the production of several elastic fibrillary elements, like fibrillin-1, that comprise the PEXM (55). Notably, TGF-b1 is one of the most vital factors that triggers the expression of both LOXL1 and fibrillin-1, which is the critical element of PEXS fibrils. Additionally, these factors also seemed to activate the construction of a specific elastic microfibrillar network into PEXS-like fibrils, suggesting the contribution of TGF-β1 in the PEXM deposition (56). Further, TGF-β1 expression is correlated with decreased degradation of ECM via regulation of the activities of matrix metalloproteases (MMPs) and their tissue inhibitors (TIMPs). Of note, TGF-β1 reduces the expression of MMP1 and MMP3 while increasing the expression of MMP2, TIMP1, and TIMP3, leading to reduced degradation of the newly synthesised matrix material. In patients with PEXS, inactive forms of MMP-2, MMP-3, and the active forms of TIMP1 and TIMP2 are higher than other MMPs. The aberrant expression of these tissue remodelling enzymes leads to insufficient degradation of excess matrix material leading to the accumulation of PEXM (57).
Clusterin
Studies suggest that TGF-β1 activation causes downregulation of clusterin (CLU), a molecular chaperone essential for folding denatured and misfolded proteins in the AH during the PEXM generation (58,59). CLU is a glycoprotein component of biological fluids and is found at higher levels in ocular cells. CLU isoforms act as an extracellular chaperone that reduces abnormal aggregation of proteins by favouring their unfolded state for proper refolding. Notably, the expression levels of CLU have been correlated with both physiological and pathological processes, including regulation of lipid transport, apoptosis, cell-cell and cell-matrix interactions, and OS. Interestingly, elevated levels of CLU are found in PEXM deposits, which are colocalised with exfoliation fibrils and LOXL1 (59,60). Furthermore, the expression of CLU decreases in PEX individuals, which could be responsible for reduced chaperone function and deposition of PEXM in the anterior segment of the eye (61).
Fibulin-5
Studies have suggested that LOXL1 activity is tightly regulated by fibulin-5 (FBLN5), an extracellular scaffold protein. FBLN5 plays a crucial role in the activation of LOXL1, thereby controlling the deposition of elastin in the ECM. Notably, FBLN5 activates LOXL1 via binding to the N-terminus of LOXL1. Studies have suggested that two polymorphisms that have been found in the noncoding part of the FBLN5 gene could be a risk factor for PEXS (37). Further, studies have shown that low mRNA and protein levels of FBLN5 in the lens of PEXS patients promote deposition of PEXM by affecting ECM dynamics. Remarkably, FBLN5 deficiency and the loss of interaction between FBLN5 and LOXL1 could cause accumulation of the inactive form of LOXL1, leading to the pathogenesis of PEXS.
7. Involvement of OS in PEXS
OS
OS is defined as excess reactive oxygen species (ROS) production in cells, mainly due to the imbalance in the generation and clearance of free radicals and reactive metabolites. The presence of active oxygen radicals in biological materials was first established in 1954 by Gerschman et al (62). Specifically, the toxic nature of oxygen was related to its partially reduced forms (63). Two years later, a hypothesis that oxygen radicals are produced as by-products of biological reactions were responsible for mutations, cellular damage, cancer, and ageing (64). The discovery of the enzyme peroxidase dismutase was the beginning of a new era for exploring the effects of ROS on living organisations (65). In the subsequent decade, extensive investigations revealed that ROS is capable of causing oxidative damage in DNA, lipids, proteins, and other cellular targets (66). Nowadays, it has become clear that living organisms have adapted to moderately increased levels of ROS and have also developed mechanisms for using them in numerous physiological functions. Free radicals are now products of normal cellular metabolism and play a dual role: either beneficial to cells and organisms or harmful, depending on the amount generated at a particular time (67).
In biological systems, OS typically occurs when ROS are overproduced or the antioxidant defense mechanisms are insufficient. The delicate balance between ROS's beneficial and harmful effects is critical to living organisms and is maintained by ‘redox regulation’. The redox regulation maintains homeostasis and protects living organisms from OS (68). Importantly, OS is essentially a disorder in the redox regulation (69), OS plays a significant role in biology and has been implicated in numerous pathophysiological processes (70). Depending on OS, a wide range of disorders may occur involving cellular dysregulation or altered processes such as inflammatory responses dysfunction, accelerated ageing, abnormal proliferation, carcinogenesis and even cell death (71).
OS in the eye
Recently we have reviewed the critical role of ECM in pathogenesis and treatment and particularly the roles of ECM effectors and biochemical pathways involved in the development and the progression of the PEXS (Fig. 1) (8). Here we further focused on the emerging roles of OS in PEXS. The eye is a highly metabolic organ devouring large amounts of energy. OS can affect the eye due to its anatomical and functional features. Specifically, the structural characteristics of the anterior eye segment tissues render them susceptible to a number of risk factors that can lead to an oxidative status (20). Notably, the eye is one of the organs constantly exposed to environmental factors that induce ROS production. Its anterior part and mainly the cornea is directly exposed to harmful atmospheric oxygen, toxins, radiation, physical abrasion, air pollution, artificial light, cigarette smoke, fumes and gases from household cleaning products, toxic chemicals and some drugs (72,73). Further, the solar UVR consists of UVA (315-400 nm), UVB (280-315 nm) and UVC (100-280 nm) is the primary source of ROS in the eye. The cornea is exposed directly to UVR and absorbs all UVC, 80% UVB and 34% UVA. Besides this, AH absorbs some of the UVB, the lens absorbs 66% of UVA and 20% of UVB, and the retina absorbs only a minimal percentage of UVA (<1%), but no UVB or UVC (72). Absorption of UVR by ocular tissues, especially UVC and UVB, eventually leads to photochemical production of ROS [e.g. singlet oxygen (1O2), superoxide (O2•-), hydroxyl radical (OH•), peroxyl radical (ROO•)] (73,74) causing UVR-induced molecular modifications (e.g. chain breaking, pyrimidine and thymine dimers and protein crosslinks) associated with pathological ophthalmic conditions such as cataract, glaucoma and age-related macular degeneration (AMD) (75,76).
In addition to UVR, some chemotherapeutic, phototoxic or even herbal origin drugs and diagnostic dyes can induce the generation of ROS in the eye and thus cause early cataracts or transient vision loss (77). For example, a drug widely used in photodynamic tumour therapy, such as γ-cyclodextrin bicapped C60 [(γCyD)2/C60, CDF0], can effectively produce 1O2 (78). Apart from its anatomical characteristics, the eye can also be affected by OS by virtue of its physical and metabolic characteristics. Notably, the mitochondria are a significant endogenous source of ROS in the eye, as it is a metabolically active organ that consumes large amounts of O2. Additionally, the eye's transparent structures, such as the cornea, AH, lens, vitreous and retina, allow continuous photochemical production of ROS (79). The biomolecular effectors of OS are summarised in Table I.
Table I.
Biomolecular effectors of OS in PEXS/PEXG.
| Author | Biomarkers | Sample source | Expression levels increase/decrease | (Refs.) |
|---|---|---|---|---|
| Koliakos et al | 8-Iso-PGF2a | ΑH | ↑ | (127) |
| Saxena et al | AGEs | ΑH, serum | ↑ | (92,110,111,112) |
| Aydın Yaz et al | ||||
| Schlötzer-Schrehardt U, Shirakami et al | ||||
| Botling Taube et al | Antothrombin III | ΑH | ↑ | (128) |
| Strzalka- Mrozik et al | ALDH1A1 (expression) | Anterior lens capsule | ↑ | (114) |
| Dursun et al | ARE | ΑH, serum | ↓ | (129) |
| Dmuchowska et al | Arginine and homo-arginine | AH | ↓ | (130) |
| Koliakos et al | Ascorbic acid | ΑH | ↑ | (130-132) |
| Ferreira et al | ||||
| Dmuchowska et al | ||||
| Yimaz et al | Ascorbic acid | Serum | ↓ | (108) |
| Botling Taube et al | C3 | ΑH | ↑ | (128) |
| Dmuchowska et al | Carnitine (Hydroxybutyryl- and decatrienoyl- ) | AH | ↓ | (130) |
| Dairou et al | CAT | serum | ↓ | (97,99,110) |
| Hosler et al | ||||
| Aydın Yaz et al | ||||
| Botling Taube et al | CLSTN1 | ΑH | ↑ | (128) |
| Doudevski et al | Clusterin | ΑH | ↑ | (59) |
| Zenkel et al | Clusterin | Lens epithelial cells | ↓ | (61) |
| Botling Taube et al | CPE | ΑH | ↓ | (128) |
| Sorkhabi et al | CRP | Serum | ↑ | (133) |
| Browne et al | CTGF | ΑH | ↑ | (117) |
| Botling Taube et al | DBP | ΑH | ↑ | (128) |
| Tetikoğlu et al | Disulphide | Serum | ↑ | (134) |
| Koliakos et al | ET-1 | ΑH | ↑ | (135,136) |
| Koukoula et al | ||||
| Park et al | Flt3 ligand | AH | ↑ | (137) |
| Park et al | Fractalkine | AH | ↓ | (137) |
| Botling Taube et al | GPX3 | ΑH | ↓ | (128) |
| Gartaganis et al | GSH | Lens epithelial cells | ↓ | (115) |
| Aydın Yaz et al | GSH | Serum | ↑ | (110) |
| Gartaganis et al | GSSG | ΑH | ↓ | (116) |
| Gartaganis et al | GSH/GSSG | ΑH | ↓ | (116) |
| Reddan et al | H2O2 | ΑH, serum | ↑ | (98,105) |
| Megaw Puustjärvi et al | Hcy | ΑH, serum | ↑ | (43) |
| Dmuchowska et al | Hydroxyanthranilic acid | AH | ↓ | (130) |
| Zenkel et al | IL-6 | ΑH | ↑ | (138) |
| Park et al | IL-8 | ΑH | ↑ | (137,138) |
| Zenkel et al | ||||
| Dmuchowska et al | Indoleacetaldehyde | AH | ↑ | (130) |
| Botling Taube et al | KNG-1 | ΑH | ↑ | (128) |
| Gartaganis et al | MDA | Lens epithelial cells | ↑ | (115) |
| Yağci et al | MDA | Serum | ↑ | (107,108,110) |
| Yimaz et al | ||||
| Aydın Yaz et al | ||||
| Strzalka-Mrozik et al | MGST1 (expression) | Anterior lens capsule | ↑ | (114) |
| Stafiej et al | MGST1 (expression) | Lens epithelial cells | ↓ | (139) |
| Park et al | MIP-1α | AH | ↑ | (137) |
| Schlötzer-Schrehardt et al | MMP-2 | ΑH | ↑ | (120) |
| Strzalka-Mrozik et al | mRNA of SOD2, ALDH1A1, MGST1 | Lens tissues | ↑ | (114) |
| Vulovic et al | NO• | ΑH | ↑ | (140) |
| Yağci et al | NO2- (levels) | Serum | ↑ | (107) |
| Turan G and Turan M | PCNA | Lens epithelial cells | ↓ | (141) |
| Dursun et al | PON (activity levels) | ΑH | ↓ | (129) |
| Yağci et al | PON (activity levels) | Serum | ↓ | (107) |
| Dursun et al | ↓ | (129) | ||
| Yağci et al | Protein carbonyls | ΑH | ↑ | (107,142) |
| Papadopoulou et al | ||||
| Papadopoulou et al | Protein carbonyls | Lens epithelial cells and Anterior lens capsule | ↑ | (142) |
| Yağci et al | Protein carbonyls | Serum | ↑ | (107) |
| Botling Taube et al | RBP3 | ΑH | ↓ | (128) |
| Dmuchowska et al | S-adenosylmethionine | AH | ↓ | (130) |
| Yimaz et al | Selenium | ΑH, serum | ↓ | (38) |
| Ferreira et al | SOD (activity levels) | ΑH | ↑ | (132) |
| Uçakhan et al | SOD (activity levels) | Lens capsule | ↑ | (143) |
| Yağci et al | SOD (activity levels) | Serum | ↑ | (107,110) |
| Aydın Yaz et al | ||||
| Strzalka-Mrozik et al | SOD2 (MnSOD) (expression) | Anterior lens capsule | ↑ | (114) |
| Tetikoğlu et al | SPA | Serum | ↓ | (144) |
| Dursun et al | TAC | ΑH | ↓ | (129) |
| Dursun et al | TAC | Serum | ↓ | (129) |
| Faschinger et al | TBARS | ΑH | ↑ | (109,116) |
| Gartaganis et al | ||||
| Schlötzer-Schrehardt et al | TGF-b1 | ΑH | ↑ | (56,137) |
| Park et al | ||||
| Schlötzer-Schrehardt et al | TIMP-2 | ΑH | ↑ | (120) |
| Fountoulakis et al | TIMP-4 | AH | ↑ | (145) |
| Vulovic et al | TNF-α | ΑH | ↑ | (140) |
| Sorkhabi et al | TNF-α | serum | ↑ | (133) |
| Dursun et al | TOS | ΑH | ↑ | (129) |
| Dursun et al | TOS | Serum | ↑ | (129) |
| Tetikoğlu et al | Total thiol and native thiol | Serum | ↓ | (134) |
| Tetikoğlu et al | Thiol/disulfide | Serum | ↓ | (134) |
| Turan G and Turan M | TUNEL | Lens epithelial cells | ↑ | (141) |
| Simavli et al | XO (activity levels) | ΑH | ↑ | (146) |
| Yağci et al | XO (activity levels) | Serum | ↑ | (107) |
| Yildirim et al | Zinc | Lens | ↓ | (22) |
8-iso-PGF2α, 8-iso-prostaglandin F2α; AGEs, advanced glycation end products; AH, aqueous humor; ALDH1A1, aldehyde dehydrogenase 1; ARE, arylesterase; C3, complement factor 3; CAT, catalase; CLSTN1, calsyntenin-1; CPE, carboxypeptidase E; CRP, C-reactive protein; CTGF, connective tissue growth factor; DBP, vitamin D-binding protein; ET-1, endothelin 1; GPX3, glutathione peroxidase 3; GSH, glutathione; GSSG, glutathione disulfide; H2O2, hydrogen peroxide; Hcy, homocycteine; IL-6, interleukin-6; IL-8, interleukin-8; KNG-1, kininogen-1; MDA, malondialdehyde, malonic aldehyde; MGST1, microsomal glutathione S transferase; MMPs, metalloproteinases; mRNA, messenger ribonucleic acid; NO•, Nitric oxide; NO2-, Nitrite (nitrogen oxoanion); PCNA, proliferating cell nuclear antigen; PON, paraoxonase; SOD, superoxide dismutase; SPA, serum prolidase activity; TAC, total antioxidant capacity; TBARS, thiobarbituric acid reactive substances; TIMPs, tissue inhibitors of metalloproteinases; TGF-b1, transforming growth factor beta 1; TNF-α, tumor necrosis factor; TOS, total oxidant status, total oxidative stress; TUNEL, terminal deoxynucleotidyl transferase-mediated dUTP-biotin nick end labeling; XO, xanthine oxidase.
OS in the crystalline lens
The lens is particularly vulnerable to OS due to its continuous exposure to solar UVR and oxidants throughout its life. Since the lens has mostly fibrous cells, it does not regenerate after damage. Moreover, the reduced levels of antioxidant molecules in the lens nucleus and the absence of protein turnover lead to an impaired ability to repair. Thus, damages accumulate over time (80). Except for solar UVR, other sources of OS in the lens include smoke and oxidants from AH or those produced by the lens cells themselves. The lens acts as a filter and absorbs over 60% of UVA and 20% of UVB, thus preventing much of the radiation to reach the retina (73). As a result, the photooxidation of the thiol groups of the lens's crystallins forms disulfide bridges between the molecules, leading to protein aggregation and cataract formation (81) ROS in the lens [e.g., O2•-, hydrogen peroxide (H2O2), OH•] can also be created endogenously through cellular metabolism in different cell compartments, such as mitochondria, peroxisomes and cytoplasm.
For example, O2•-can be produced by the typical electron transport system and the activity of cytochrome P450. The nicotinamide adenine dinucleotide phosphate (NADPH) oxidase complex with Rac GTPases, associated with activating plasma membrane receptors by external signals like growth factors, can also produce O2•-. In addition, growth factor receptors can be activated by the UVR and produce ROS. Intracellular H2O2 can be derived from superoxide dismutase (SOD) activity or created from ascorbate and O2 in the presence of Fe+3 or even generated from the AH. Finally, the reaction of H2O2 with metal ions (M+) can lead to OH• H O2•- via the Fenton reaction (82). However, the endogenous production of ROS in the lens does not necessarily lead to OS since low concentrations of H2O2 could play a role as a signal transduction factor in the differentiation of lens epithelial cells and also be a significant regulatory molecule of numerous vital enzymes, such as phosphatases and kinases (83). Under OS conditions, the selective oxidation of specific amino acids in the lens results in aggregation and degradation of proteins, reduction of water solubility, crosslinking, charge changes, etc. (84,85) can significantly contribute to cataract development (86).
Additionally, ROS causes increased oxidation of amino acid residues of methionine, cysteine, tryptophan and phenylalanine in the lens, as evidenced by the formation of protein disulfides kynurenine, o-Tyr and Met-SO (87,88). Specifically, the associated ageing increase in Met-SO formation is related to the loss of a number of protein activities that affect various functions of the lens (89,90). To protect against oxidation, the lens has evolved as an anaerobic system containing high concentrations of ascorbic acid and glutathione (GSH), an endogenous antioxidant molecule part of the antioxidant defence system (91). However, these defensive antioxidant molecules decrease with age, with GSH declining significantly in the lens nucleus. Subsequently, ascorbic acid is increasingly oxidised, leading to the accumulation of crystalline-bound advanced glycation end products (AGEs) that contribute to the cataractogenesis (92).
OS in the epithelium of the crystalline lens
The metabolically active lens epithelial cells are primarily responsible for their defence against OS (93). UVA is the main responsible for ROS production in the lens epithelial cells. About 70% of UVA passes through the cornea towards lens epithelial cells reacting with NADPH and nicotinamide adenine dinucleotide (NADH), which are present in high concentrations in these cells producing ROS (e.g., 1O2, O2•-, H2O2) (94). Exposure of lens epithelial cells to UVA results in increased lipid peroxidation, decreased antioxidant enzymes e.g. catalase (CAT), reduced viability and cell death (95). UVB is estimated to be only 3% of the total UVR reaching the lens and can trigger apoptotic mechanisms in the lens epithelial cells and inactivate enzymes (96,97).
In addition to UV-induced photooxidation, oxidative damage to the macromolecules of lens epithelial cells is also caused by elevated levels of cellular oxidants produced by exposure to toxic chemicals and failure of antioxidant defences (97). Moreover, lens epithelial cells can be affected by the high levels of H2O2 in the AH (98). H2O2 and peroxynitrite (ONOO-) are thought to be the essential oxidants of acute or chronic exposure of lens epithelial cells (97) and their elevated levels can cause oxidation-dependent inactivation of crucial enzymes such as CAT, proteasome, and arylamine N-acetyltransferases (NATs) (97,99). Oxidative damage to lens epithelial cells can also cause osmotic swelling of the lens and loss of its transparency (100).
OS in the AH
ROS production in AH is mainly due to UVR and inflammatory processes in adjacent structures, e.g., surgery (101,102). The AH contains ascorbic acid, proteins, certain amino acids (e.g. tyrosine, phenylalanine, cysteine, tryptophan) and uric acid, which act as filters absorbing the majority of UVR, leaving only a tiny part of it reaching the structures of the eye (103). Despite the critical role of endogenous UV filters like ascorbic acid, their photooxidation can produce potent oxidising molecules, such as 1O2 and H2O2 (104). The increased concentration of H2O2 in the AH has been found to reduce GSH metabolism (105). It may cause damage to the corneal endothelium, the lens and the radial body, particularly the trabecular meshwork. In vitro studies have associated increased H2O2 levels with reduced AH drainage, resulting in glaucoma (79).
In contrast to the findings mentioned earlier, there is a view that OS does not cause permanent damage to the AH. Any alterations of vital components are considered to be part of its antioxidant defence and are relatively reversible after restoring optimal conditions. However, long-term exposure to OS results in loss of antioxidants and tissue damage (89).
OS in the pathogenesis of PEXS
OS plays a crucial role in the pathogenesis of several eye diseases, including PEXS. Disturbances in the delicate balance between ROS and antioxidant defense mechanisms of the eye may contribute to the development of PEXS. Evidence suggests that high malondialdehyde (MDA) levels, which are the end-product of polyunsaturated fatty acid peroxidation reaction and a marker of free radical-mediated lipid peroxidation, are found in the patients of PEXS (106-108). Similarly, high levels of thiobarbituric acid reactive substances (TBARS), the major breakdown products of lipid peroxides, were significantly higher in the AH samples collected from primary open-angle glaucoma patients (109). Besides, increased levels of AGEs are also observed in the AH and serum of PEXS patients (110,111).
Additionally, these specific oxidation and glycation products could trigger the glaucoma formation associated with PEXS (112). Specifically, these end products can induce ROS generation, thus resulting in the deterioration of trabecular meshwork cells. Therefore, correcting the OS-induced damage using antioxidants could be considered a therapeutic strategy to prevent glaucoma in PEXS patients (113). According to these findings, OS and its end products might be a vital factor in PEXS pathogenesis. Further, the levels of superoxide dismutase 2 (SOD2), aldehyde dehydrogenase 1a1 (ALDH1A1), and microsomal glutathione transferase 1 (MGST1) which are part of the essential antioxidant defense system, are high in the anterior lens capsule of PEXS patients (114). However, antioxidant enzymes, SOD and CAT were significantly lower in PEXS patients (110). Similarly, the levels of GSH decrease in the lens epithelial cells of PXES patients (115,116). The antioxidant system defence failure could result in inadequate OS response and pseudoexfoliation development.
OS elevates the levels of free radicals, TGF-b1 and other growth factors in the eye. It is a critical factor in developing fibrosis in the PEXS-affected eyes (117). Also, OS disrupts the balance between MMPs and TIMPs, leading to dysregulated ECM in the eye of PEXS patients (118). TIMPs imbalance has been implicated in various abnormal fibroblastic disorders (119), including the development of PEXM and PEXG (120). Studies have found that TGF-b1 may up-regulate OS and have a synergic external role in the PEXS development (121,122). Especially, TGF-b1-mediated upregulation of LOXL1 could promote fibrosis in the eye of PEXS patients. Further, studies have indicated the synergy between TGF-β1 and OS in the activation of the LOXL1 (20,122). Therefore it could be suggested that the abnormal ECM deposition can be triggered by OS, and TGF-b1 under the high-risk LOXL1 haplotype may contribute to the PEXS aggregates in the ocular tissues (20).
OS is also known to modify glutamine synthase and thus influence glutamate/glutamine metabolism, leading to increased neurotoxic concentrations of glutamate (123). Further, OS can also damage the mitochondria present in the cells of optic nerves resulting in a reduced energy supply. Considering the critical role of mitochondrial disfunction in glaucoma evolution, therapies targeting mitochondria with specific antioxidants may improve the survival of retina ganglion cells to protect them from glaucomatous degeneration (124). Indirectly, OS can also cause vascular changes resulting in impaired blood flow to the optic nerve, injury to trabecular meshwork that decreases AH outflow and elevated IOP and glial cell dysfunction (110,125,126). Overall these studies point to the regulation of OS to regulate the pathogenesis of PEXS.
8. Conclusions and future directions
Numerous studies have shown that OS plays a crucial role in pseudoexfoliation and is critical for determining the onset and evolution of either the PEXS or PEXG. With human longevity increasing, PEXS and PEXG will become severe clinical problems as they cause several severe complications, including vision loss. Hence, a prompt diagnosis is essential to avoid a challenging clinical course with poor response to treatment, timely surgery and an overall good prognosis. Diagnostics have greatly improved, and standardised treatment protocols are currently available. Current disease management focuses primarily on increasing antioxidants concentrations to compensate for OS. Specifically, the diet modifications and various antioxidant supplements have been used in patients with PEXS, however, with limited success. Therefore, we need to develop novel tools to reduce OS in the eye of the patient with PEXS.
Over the past decade, several studies have been undertaken to elucidate the molecular basis of this disease. Still, the exact mechanism of triggering the PEXM and its deposition and associated pathologies remain unclear. Efforts to unearth the causes for this devastating disease should be a priority. At present, we better comprehend the genetic and environmental factors involved in the PEXS. However, the involvement of genetic and environmental factors in making one population susceptible has to be elucidated. Recent studies have uncovered several genes involved in the pathogenesis of PEXS/PEXG. Still, we do not have clear reasons for all the pathological processes. Thus, we may need to expand the studies on both population and molecular levels to get insights into the pathogenesis of PEXS. Also, future studies are required to uncover the reasons for varying degrees of susceptibility between human populations.
Acknowledgements
Not applicable.
Funding Statement
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
SM conceived, designed and wrote the review and is the corresponding author. MP, PP and KK had equal contribution, performed the literature review and analyzed the data. CDG reviewed and edited the manuscript, and supervised and administered the project. All authors read and approved the final manuscript. Data authentication is not applicable.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Karamanos NK, Theocharis AD, Piperigkou Z, Manou D, Passi A, Skandalis SS, Vynios DH, Orian-Rousseau V, Ricard-Blum S, Schmelzer CEH, et al. A guide to the composition and functions of the extracellular matrix. FEBS J. 2021;288:6850–6912. doi: 10.1111/febs.15776. [DOI] [PubMed] [Google Scholar]
- 2.Iozzo RV, Theocharis AD, Neill T, Karamanos NK. Complexity of matrix phenotypes. Matrix Biol Plus. 2020;6-7(100038) doi: 10.1016/j.mbplus.2020.100038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dvorak-Theobald G. Pseudo-exfoliation of the lens capsule: Relation to true exfoliation of the lens capsule as reported in the literature and role in the production of glaucoma capsulocuticulare. Am J Ophthalmol. 1954;37:1–12. [PubMed] [Google Scholar]
- 4.Roche J. Pseudo-exfoliation of the lens capsule. Br J Ophthalmol. 1968;52:265–269. doi: 10.1136/bjo.52.3.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shakib M, Ashton N, Blach R. Electron microscopic study of pseudo-exfoliation of the lens capsule. Ii. Iris and ciliary body. Invest Ophthalmol. 1965;4:154–161. [PubMed] [Google Scholar]
- 6.Conway RM, Schlötzer-Schrehardt U, Küchle M, Naumann GO. Pseudoexfoliation syndrome: Pathological manifestations of relevance to intraocular surgery. Clin Exp Ophthalmol. 2004;32:199–210. doi: 10.1111/j.1442-9071.2004.00806.x. [DOI] [PubMed] [Google Scholar]
- 7.Tekin K, Inanc M, Elgin U. Monitoring and management of the patient with pseudoexfoliation syndrome: Current perspectives. Clin Ophthalmol. 2019;13:453–464. doi: 10.2147/OPTH.S181444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mastronikolis S, Pagkalou M, Baroutas G, Kyriakopoulou K, Makri OE, Georgakopoulos CD. doi: 10.1002/iub.2606. Pseudoexfoliation syndrome: The critical role of the extracellular matrix in pathogenesis and treatment. IUBMB Life: Feb 24, 2022 (Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 9.Challa P. Genetics of pseudoexfoliation syndrome. Curr Opin Ophthalmol. 2009;20:88–91. doi: 10.1097/ICU.0b013e328320d86a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ariga M, Nivean M, Utkarsha P. Pseudoexfoliation syndrome. J Curr Glaucoma Pract. 2013;7:118–120. doi: 10.5005/jp-journals-10008-1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elhawy E, Kamthan G, Dong CQ, Danias J. Pseudoexfoliation syndrome, a systemic disorder with ocular manifestations. Hum Genomics. 2012;6(22) doi: 10.1186/1479-7364-6-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schlötzer-Schrehardt U, Naumann GO. Ocular and systemic pseudoexfoliation syndrome. Am J Ophthalmol. 2006;141:921–937. doi: 10.1016/j.ajo.2006.01.047. [DOI] [PubMed] [Google Scholar]
- 13.Ritch R. Ocular and systemic manifestations of exfoliation syndrome. J Glaucoma. 2014;23 (8 Suppl 1):S1–S8. doi: 10.1097/IJG.0000000000000119. [DOI] [PubMed] [Google Scholar]
- 14.Ovodenko B, Rostagno A, Neubert TA, Shetty V, Thomas S, Yang A, Liebmann J, Ghiso J, Ritch R. Proteomic analysis of exfoliation deposits. Invest Ophthalmol Vis Sci. 2007;48:1447–1457. doi: 10.1167/iovs.06-0411. [DOI] [PubMed] [Google Scholar]
- 15.Gartaganis SP, Georgakopoulos CD, Assouti M, Mela EK, Exarchou A, Giannelou I, Gotsis SS, Ziouti N, Vynios DH, Tripathi BJ, Tripathi RC. Changes in HNK-1 epitope and collagen type IX in the aqueous humour of patients with pseudoexfoliation syndrome. Curr Eye Res. 2004;28:5–10. doi: 10.1076/ceyr.28.1.5.23490. [DOI] [PubMed] [Google Scholar]
- 16.Sharma S, Chataway T, Burdon KP, Jonavicius L, Klebe S, Hewitt AW, Mills RA, Craig JE. Identification of LOXL1 protein and apolipoprotein E as components of surgically isolated pseudoexfoliation material by direct mass spectrometry. Exp Eye Res. 2009;89:479–485. doi: 10.1016/j.exer.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Tran VT. Washout of pseudoexfoliation material combined with cataract surgery: A new surgical approach to lower intraocular pressure in pseudoexfoliation syndrome. Int Ophthalmol. 2015;35:209–214. doi: 10.1007/s10792-014-9934-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ritch R, Schlötzer-Schrehardt U. Exfoliation syndrome. Surv Ophthalmol. 2001;45:265–315. doi: 10.1097/00055735-200104000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Schlötzer-Schrehardt UM, Koca MR, Naumann GO, Volkholz H. Pseudoexfoliation syndrome. Ocular manifestation of a systemic disorder? Arch Ophthalmol. 1992;110:1752–1756. doi: 10.1001/archopht.1992.01080240092038. [DOI] [PubMed] [Google Scholar]
- 20.Chiras D, Kitsos G, Petersen MB, Skalidakis I, Kroupis C. Oxidative stress in dry age-related macular degeneration and exfoliation syndrome. Crit Rev Clin Lab Sci. 2015;52:12–27. doi: 10.3109/10408363.2014.968703. [DOI] [PubMed] [Google Scholar]
- 21.Yüksel N, Karabaş VL, Arslan A, Demirci A, Cağlar Y. Ocular hemodynamics in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Ophthalmology. 2001;108:1043–1049. doi: 10.1016/s0161-6420(01)00572-3. [DOI] [PubMed] [Google Scholar]
- 22.Yildirim N, Yasar E, Gursoy H, Colak E. Prevalence of pseudoexfoliation syndrome and its association with ocular and systemic diseases in Eskisehir, Turkey. Int J Ophthalmol. 2017;10:128–134. doi: 10.18240/ijo.2017.01.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Topouzis F, Anastasopoulos E. Incidence of pseudoexfoliation syndrome. Am J Ophthalmol. 2009;148:181–182. doi: 10.1016/j.ajo.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 24.Chan TCW, Bala C, Siu A, Wan F, White A. Risk factors for rapid glaucoma disease progression. Am J Ophthalmol. 2017;180:151–157. doi: 10.1016/j.ajo.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 25.Aboobakar IF, Johnson WM, Stamer WD, Hauser MA, Allingham RR. Major review: Exfoliation syndrome; advances in disease genetics, molecular biology, and epidemiology. Exp Eye Res. 2017;154:88–103. doi: 10.1016/j.exer.2016.11.011. [DOI] [PubMed] [Google Scholar]
- 26.Mansour AM, Konstas AGP, Mansour HA, Charbaji AR, Jawhari KM. A case-cohort study of exfoliation risk factors and literature review. Middle East Afr J Ophthalmol. 2021;28:36–50. doi: 10.4103/meajo.MEAJO_358_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Whigham BT, Allingham RR. Review: The role of LOXL1 in exfoliation syndrome/glaucoma. Saudi J Ophthalmol. 2011;25:347–352. doi: 10.1016/j.sjopt.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Konstas AGP, Ringvold A. Epidemiology of exfoliation syndrome. J Glaucoma. 2018;27 (Suppl 1):S4–S11. doi: 10.1097/IJG.0000000000000908. [DOI] [PubMed] [Google Scholar]
- 29.Forsius H. Exfoliation syndrome in various ethnic populations. Acta Ophthalmol. 1988;Suppl (1985) 184:71–85. doi: 10.1111/j.1755-3768.1988.tb02633.x. [DOI] [PubMed] [Google Scholar]
- 30.Miglior S, Bertuzzi F. Exfoliative glaucoma: New evidence in the pathogenesis and treatment. Prog Brain Res. 2015;221:233–241. doi: 10.1016/bs.pbr.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 31.Amini H, Daneshvar R, Eslami Y, Moghimi S, Amini N. Early-onset pseudoexfoliation syndrome following multiple intraocular procedures. J Ophthalmic Vis Res. 2012;7:190–196. [PMC free article] [PubMed] [Google Scholar]
- 32.Thorleifsson G, Magnusson KP, Sulem P, Walters GB, Gudbjartsson DF, Stefansson H, Jonsson T, JonRasdottir A, Jonasdottir A, Stefansdottir G, et al. Common sequence variants in the LOXL1 gene confer susceptibility to exfoliation glaucoma. Science. 2007;317:1397–1400. doi: 10.1126/science.1146554. [DOI] [PubMed] [Google Scholar]
- 33.Schlötzer-Schrehardt U. Genetics and genomics of pseudoexfoliation syndrome/glaucoma. Middle East Afr J Ophthalmol. 2011;18:30–36. doi: 10.4103/0974-9233.75882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zalewska R, Pepinski W, Smolenska-Janica D, Mariak Z, Proniewska-Skretek E, Skawronska M, Janica J. Loss of heterozygosity in patients with pseudoexfoliation syndrome. Mol Vis. 2003;9:257–261. [PubMed] [Google Scholar]
- 35.Kozobolis VP, Detorakis ET, Sourvinos G, Pallikaris IG, Spandidos DA. Loss of heterozygosity in pseudoexfoliation syndrome. Invest Ophthalmol Vis Sci. 1999;40:1255–1260. [PubMed] [Google Scholar]
- 36.Aung T, Ozaki M, Mizoguchi T, Allingham RR, Li Z, Haripriya A, Nakano S, Uebe S, Harder JM, Chan AS, et al. A common variant mapping to CACNA1A is associated with susceptibility to exfoliation syndrome. Nat Genet. 2015;47:387–392. doi: 10.1038/ng.3226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Padhy B, Kapuganti RS, Hayat B, Pranjya Paramita Mohanty PP, Alone DP. De novo variants in an extracellular matrix protein coding gene, fibulin-5 (FBLN5) are associated with pseudoexfoliation. Eur J Hum Genet. 2019;27:1858–1866. doi: 10.1038/s41431-019-0482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yimaz A, Ayaz L, Tamer L. Selenium and pseudoexfoliation syndrome. Am J Ophthalmol. 2011;151:272–276.e1. doi: 10.1016/j.ajo.2010.08.032. [DOI] [PubMed] [Google Scholar]
- 39.Arnarsson A, Sasaki H, Jonasson F. Twelve-year incidence of exfoliation syndrome in the Reykjavik eye study. Acta Ophthalmol. 2013;91:157–162. doi: 10.1111/j.1755-3768.2011.02334.x. [DOI] [PubMed] [Google Scholar]
- 40.Arnarsson AM. Epidemiology of exfoliation syndrome in the Reykjavik eye study. Acta Ophthalmol 87 Thesis. 2009;3:1–17. doi: 10.1111/j.1755-3768.2009.01806.x. [DOI] [PubMed] [Google Scholar]
- 41.Pasquale LR, Wiggs JL, Willett WC, Kang JH. The relationship between caffeine and coffee consumption and exfoliation glaucoma or glaucoma suspect: A prospective study in two cohorts. Invest Ophthalmol Vis Sci. 2012;53:6427–6433. doi: 10.1167/iovs.12-10085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Christensen B, Mosdol A, Retterstol L, Landaas S, Thelle DS. Abstention from filtered coffee reduces the concentrations of plasma homocysteine and serum cholesterol-a randomized controlled trial. Am J Clin Nutr. 2001;74:302–307. doi: 10.1093/ajcn/74.3.302. [DOI] [PubMed] [Google Scholar]
- 43.Puustjärvi T, Blomster H, Kontkanen M, Punnonen K, Teräsvirta M. Plasma and aqueous humour levels of homocysteine in exfoliation syndrome. Graefes Arch Clin Exp Ophthalmol. 2004;242:749–754. doi: 10.1007/s00417-004-0918-7. [DOI] [PubMed] [Google Scholar]
- 44.Kozobolis VP, Papatzanaki M, Vlachonikolis IG, Pallikaris IG, Tsambarlakis IG. Epidemiology of pseudoexfoliation in the island of Crete (Greece) Acta Ophthalmol Scand. 1997;75:726–729. doi: 10.1111/j.1600-0420.1997.tb00640.x. [DOI] [PubMed] [Google Scholar]
- 45.Kang JH, Loomis S, Wiggs JL, Stein JD, Pasquale LR. Demographic and geographic features of exfoliation glaucoma in 2 United States-based prospective cohorts. Ophthalmology. 2012;119:27–35. doi: 10.1016/j.ophtha.2011.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stein JD, Pasquale LR, Talwar N, Kim DS, Reed DM, Nan B, Kang JH, Wiggs JL, Richards JE. Geographic and climatic factors associated with exfoliation syndrome. Arch Ophthalmol. 2011;129:1053–1060. doi: 10.1001/archophthalmol.2011.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pasquale LR, Jiwani AZ, Zehavi-Dorin T, Majd A, Rhee DJ, Chen T, Turalba A, Shen L, Brauner S, Grosskreutz C, et al. Solar exposure and residential geographic history in relation to exfoliation syndrome in the United States and Israel. Jama Ophthalmol. 2014;132:1439–1445. doi: 10.1001/jamaophthalmol.2014.3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pasquale LR, Kang JH, Fan B, Levkovitch-Verbin H, Wiggs JL. LOXL1 polymorphisms: Genetic biomarkers that presage environmental determinants of exfoliation syndrome. J Glaucoma. 2018;27 (Suppl 1):S20–S23. doi: 10.1097/IJG.0000000000000915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu X, Zhao Y, Gao J, Pawlyk B, Starcher B, Spencer JA, Yanagisawa H, Zuo J, Li T. Elastic fiber homeostasis requires lysyl oxidase-like 1 protein. Nat Genet. 2004;36:178–182. doi: 10.1038/ng1297. [DOI] [PubMed] [Google Scholar]
- 50.Oleggini R, Gastaldo N, Di Donato A. Regulation of elastin promoter by lysyl oxidase and growth factors: Cross control of lysyl oxidase on TGF-beta1 effects. Matrix Biol. 2007;26:494–505. doi: 10.1016/j.matbio.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 51.Li G, Schmitt H, Johnson WM, Lee C, Navarro I, Cui J, Fleming T, Gomez-Caraballo M, Elliott MH, Sherwood JM, et al. Integral role for lysyl oxidase-like-1 in conventional outflow tissue function and behavior. FASEB J. 2020;34:10762–10777. doi: 10.1096/fj.202000702RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schlötzer-Schrehardt U, Hammer CM, Krysta AW, Hofmann-Rummelt C, Pasutto F, Sasaki T, Kruse FE, Zenkel M. LOXL1 deficiency in the lamina cribrosa as candidate susceptibility factor for a pseudoexfoliation-specific risk of glaucoma. Ophthalmology. 2012;119:1832–1843. doi: 10.1016/j.ophtha.2012.03.015. [DOI] [PubMed] [Google Scholar]
- 53.Schmitt HM, Johnson WM, Aboobakar IF, Strickland S, Gomez-Caraballo M, Parker M, Finnegan L, Corcoran DL, Skiba NP, Allingham RR, et al. Identification and activity of the functional complex between hnRNPL and the pseudoexfoliation syndrome-associated lncRNA, LOXL1-AS1. Hum Mol Genet. 2020;29:1986–1995. doi: 10.1093/hmg/ddaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu RM, Gaston Pravia KA. Oxidative stress and glutathione in TGF-beta-mediated fibrogenesis. Free Radic Biol Med. 2010;48:1–15. doi: 10.1016/j.freeradbiomed.2009.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Takai Y, Tanito M, Ohira A. Multiplex cytokine analysis of aqueous humor in eyes with primary open-angle glaucoma, exfoliation glaucoma, and cataract. Invest Ophthalmol Vis Sci. 2012;53:241–247. doi: 10.1167/iovs.11-8434. [DOI] [PubMed] [Google Scholar]
- 56.Zenkel M, Krysta A, Pasutto F, Juenemann A, Kruse FE, Schlötzer-Schrehardt U. Regulation of lysyl oxidase-like 1 (LOXL1) and elastin-related genes by pathogenic factors associated with pseudoexfoliation syndrome. Invest Ophthalmol Vis Sci. 2011;52:8488–8495. doi: 10.1167/iovs.11-8361. [DOI] [PubMed] [Google Scholar]
- 57.Djordjević-Jocić J, Zlatanović G, Veselinović D, Jovanović P, Djordjević V, Zvezdanović L, Stanković-Babić G, Vujanović M, Cekić S, Zenkel M, Schlotzer-Schrehardt U. Transforming growth factor beta1, matrix-metalloproteinase-2 and its tissue inhibitor in patients with pseudoexfoliation glaucoma/syndrome. Vojnosanit Pregl. 2012;69:231–236. [PubMed] [Google Scholar]
- 58.Schlötzer-Schrehardt U, Zenkel M, Küchle M, Sakai LY, Naumann GO. Role of transforming growth factor-beta1 and its latent form binding protein in pseudoexfoliation syndrome. Exp Eye Res. 2001;73:765–780. doi: 10.1006/exer.2001.1084. [DOI] [PubMed] [Google Scholar]
- 59.Doudevski I, Rostagno A, Cowman M, Liebmann J, Ritch R, Ghiso J. Clusterin and complement activation in exfoliation glaucoma. Invest Ophthalmol Vis Sci. 2014;55:2491–2499. doi: 10.1167/iovs.13-12941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Morris J, Myer C, Cornet T, Junk AK, Lee RK, Bhattacharya SK. Proteomics of pseudoexfoliation materials in the anterior eye segment. Adv Protein Chem Struct Biol. 2021;127:271–290. doi: 10.1016/bs.apcsb.2021.03.004. [DOI] [PubMed] [Google Scholar]
- 61.Zenkel M, Kruse FE, Jünemann AG, Naumann GO, Schlötzer-Schrehardt U. Clusterin deficiency in eyes with pseudoexfoliation syndrome may be implicated in the aggregation and deposition of pseudoexfoliative material. Invest Ophthalmol Vis Sci. 2006;47:1982–1990. doi: 10.1167/iovs.05-1580. [DOI] [PubMed] [Google Scholar]
- 62.Gerschman R, Gilbert DL, Nye SW, Dwyer P, Fenn WO. Oxygen poisoning and x-irradiation: A mechanism in common. Science. 1954;119:623–626. doi: 10.1126/science.119.3097.623. [DOI] [PubMed] [Google Scholar]
- 63.Commoner B, Townsend J, Pake GE. Free radicals in biological materials. Nature. 1954;174:689–691. doi: 10.1038/174689a0. [DOI] [PubMed] [Google Scholar]
- 64.Harman D. Aging: A theory based on free radical and radiation chemistry. J Gerontol. 1956;11:298–300. doi: 10.1093/geronj/11.3.298. [DOI] [PubMed] [Google Scholar]
- 65.McCord JM, Fridovich I. Superoxide dismutase. An enzymic function for erythrocuprein (hemocuprein) J Biol Chem. 1969;244:6049–6055. [PubMed] [Google Scholar]
- 66.Beckman KB, Ames BN. The free radical theory of aging matures. Physiol Rev. 1998;78:547–581. doi: 10.1152/physrev.1998.78.2.547. [DOI] [PubMed] [Google Scholar]
- 67.Valko M, Rhodes CJ, Moncol J, Izakovic M, Mazur M. Free radicals, metals and antioxidants in oxidative stress-induced cancer. Chem Biol Interact. 2006;160:1–40. doi: 10.1016/j.cbi.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 68.Dröge W. Free radicals in the physiological control of cell function. Physiol Rev. 2002;82:47–95. doi: 10.1152/physrev.00018.2001. [DOI] [PubMed] [Google Scholar]
- 69.Jones DP. Redefining oxidative stress. Antioxid Redox Signal. 2006;8:1865–1879. doi: 10.1089/ars.2006.8.1865. [DOI] [PubMed] [Google Scholar]
- 70.Pizzino G, Irrera N, Cucinotta M, Pallio G, Mannino F, Arcoraci V, Squadrito F, Altavilla D, Bitto A. Oxidative stress: Harms and benefits for human health. Oxid Med Cell Longev. 2017;2017(8416763) doi: 10.1155/2017/8416763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Li R, Jia Z, Trush MA. Defining ROS in biology and medicine. React Oxyg Species (Apex) 2016;1:9–21. doi: 10.20455/ros.2016.803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Shoham A, Hadziahmetovic M, Dunaief JL, Mydlarski MB, Schipper HM. Oxidative stress in diseases of the human cornea. Free Radic Biol Med. 2008;45:1047–1055. doi: 10.1016/j.freeradbiomed.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 73.Cejka C, Cejkova J. Oxidative stress to the cornea, changes in corneal optical properties, and advances in treatment of corneal oxidative injuries. Oxid Med Cell Longev. 2015;2015(591530) doi: 10.1155/2015/591530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chen Y, Mehta G, Vasiliou V. Antioxidant defenses in the ocular surface. Ocul Surf. 2009;7:176–185. doi: 10.1016/s1542-0124(12)70185-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cai CX, Birk DE, Linsenmayer TF. Nuclear ferritin protects DNA from UV damage in corneal epithelial cells. Mol Biol Cell. 1998;9:1037–1051. doi: 10.1091/mbc.9.5.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sacca SC, Bolognesi C, Battistella A, Bagnis A, Izzotti A. Gene-environment interactions in ocular diseases. Mutat Res. 2009;667:98–117. doi: 10.1016/j.mrfmmm.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 77.Roberts JE. Screening for ocular phototoxicity. Int J Toxicol. 2002;21:491–500. doi: 10.1080/10915810290169918. [DOI] [PubMed] [Google Scholar]
- 78.Zhao B, He YY, Chignell CF, Yin JJ, Andley U, Roberts JE. Difference in phototoxicity of cyclodextrin complexed fullerene [(gamma-CyD)2/C60] and its aggregated derivatives toward human lens epithelial cells. Chem Res Toxicol. 2009;22:660–667. doi: 10.1021/tx800478u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cabrera MP, Chihuailaf RH. Antioxidants and the integrity of ocular tissues. Vet Med Int. 2011;2011(905153) doi: 10.4061/2011/905153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Beebe DC, Holekamp NM, Shui YB. Oxidative damage and the prevention of age-related cataracts. Ophthalmic Res. 2010;44:155–165. doi: 10.1159/000316481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ozaki Y, Mizuno A, Itoh K, Iriyama K. Inter- and intramolecular disulfide bond formation and related structural changes in the lens proteins. A Raman spectroscopic study in vivo of lens aging. J Biol Chem. 1987;262:15545–15551. [PubMed] [Google Scholar]
- 82.Berthoud VM, Beyer EC. Oxidative stress, lens gap junctions, and cataracts. Antioxid Redox Signal. 2009;11:339–353. doi: 10.1089/ars.2008.2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ohguro N, Fukuda M, Sasabe T, Tano Y. Concentration dependent effects of hydrogen peroxide on lens epithelial cells. Br J Ophthalmol. 1999;83:1064–1068. doi: 10.1136/bjo.83.9.1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bodaness RS, Leclair M, Zigler JS Jr. An analysis of the H2O2-mediated crosslinking of lens crystallins catalyzed by the heme-undecapeptide from cytochrome c. Arch Biochem Biophys. 1984;231:461–469. doi: 10.1016/0003-9861(84)90409-0. [DOI] [PubMed] [Google Scholar]
- 85.Zigler JS Jr, Huang QL, Du XY. Oxidative modification of lens crystallins by H2O2 and chelated iron. Free Radic Biol Med. 1989;7:499–505. doi: 10.1016/0891-5849(89)90025-7. [DOI] [PubMed] [Google Scholar]
- 86.McNamara M, Augusteyn RC. The effects of hydrogen peroxide on lens proteins: A possible model for nuclear cataract. Exp Eye Res. 1984;38:45–56. doi: 10.1016/0014-4835(84)90137-4. [DOI] [PubMed] [Google Scholar]
- 87.Garner MH, Spector A. Selective oxidation of cysteine and methionine in normal and senile cataractous lenses. Proc Natl Acad Sci USA. 1980;77:1274–1277. doi: 10.1073/pnas.77.3.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fu S, Dean R, Southan M, Truscott R. The hydroxyl radical in lens nuclear cataractogenesis. J Biol Chem. 1998;273:28603–28609. doi: 10.1074/jbc.273.44.28603. [DOI] [PubMed] [Google Scholar]
- 89.Vogt W. Oxidation of methionyl residues in proteins: Tools, targets, and reversal. Free Radic Biol Med. 1995;18:93–105. doi: 10.1016/0891-5849(94)00158-g. [DOI] [PubMed] [Google Scholar]
- 90.Truscott RJ, Augusteyn RC. Oxidative changes in human lens proteins during senile nuclear cataract formation. Biochim Biophys Acta. 1977;492:43–52. doi: 10.1016/0005-2795(77)90212-4. [DOI] [PubMed] [Google Scholar]
- 91.Rose RC, Richer SP, Bode AM. Ocular oxidants and antioxidant protection. Proc Soc Exp Biol Med. 1998;217:397–407. doi: 10.3181/00379727-217-44250. [DOI] [PubMed] [Google Scholar]
- 92.Saxena P, Saxena AK, Cui XL, Obrenovich M, Gudipaty K, Monnier VM. Transition metal-catalyzed oxidation of ascorbate in human cataract extracts: Possible role of advanced glycation end products. Invest Ophthalmol Vis Sci. 2000;41:1473–1481. [PubMed] [Google Scholar]
- 93.Spector A. Oxidative stress-induced cataract: Mechanism of action. FASEB J. 1995;9:1173–1182. [PubMed] [Google Scholar]
- 94.Dillon J, Zheng L, Merriam JC, Gaillard ER. The optical properties of the anterior segment of the eye: Implications for cortical cataract. Exp Eye Res. 1999;68:785–795. doi: 10.1006/exer.1999.0687. [DOI] [PubMed] [Google Scholar]
- 95.Rogers CS, Chan LM, Sims YS, Byrd KD, Hinton DL, Twining SS. The effects of sub-solar levels of UV-A and UV-B on rabbit corneal and lens epithelial cells. Exp Eye Res. 2004;78:1007–1014. doi: 10.1016/j.exer.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 96.Long AC, Colitz CM, Bomser JA. Apoptotic and necrotic mechanisms of stress-induced human lens epithelial cell death. Exp Biol Med (Maywood) 2004;229:1072–1080. doi: 10.1177/153537020422901012. [DOI] [PubMed] [Google Scholar]
- 97.Dairou J, Malecaze F, Dupret JM, Rodrigues-Lima F. The xenobiotic-metabolizing enzymes arylamine N-acetyltransferases in human lens epithelial cells: Inactivation by cellular oxidants and UVB-induced oxidative stress. Mol Pharmacol. 2005;67:1299–1306. doi: 10.1124/mol.104.009738. [DOI] [PubMed] [Google Scholar]
- 98.Reddan JR, Steiger CA, Dziedzic DC, Gordon SR. Regional differences in the distribution of catalase in the epithelium of the ocular lens. Cell Mol Biol (Noisy-le-grand) 1996;42:209–219. [PubMed] [Google Scholar]
- 99.Hosler MR, Wang-Su ST, Wagner BJ. Targeted disruption of specific steps of the ubiquitin-proteasome pathway by oxidation in lens epithelial cells. Int J Biochem Cell Biol. 2003;35:685–697. doi: 10.1016/s1357-2725(02)00397-7. [DOI] [PubMed] [Google Scholar]
- 100.Giblin FJ, McCready JP, Schrimscher L, Reddy VN. Peroxide-induced effects on lens cation transport following inhibition of glutathione reductase activity in vitro. Exp Eye Res. 1987;45:77–91. doi: 10.1016/s0014-4835(87)80080-5. [DOI] [PubMed] [Google Scholar]
- 101.Cejková J, Stípek S, Crkovská J, Ardan T, Pláteník J, Cejka C, Midelfart A. UV Rays, the prooxidant/antioxidant imbalance in the cornea and oxidative eye damage. Physiol Res. 2004;53:1–10. [PubMed] [Google Scholar]
- 102.Barros PS, Padovani CF, Silva VV, L Queiroz L, Barros SBM. Antioxidant status of dog aqueous humor after extracapsular lens extraction. Braz J Med Biol Res. 2003;36:1491–1494. doi: 10.1590/s0100-879x2003001100007. [DOI] [PubMed] [Google Scholar]
- 103.Ringvold A, Anderssen E, Jellum E, Bjerkås E, Sonerud GA, Haaland PJ, Devor TP, Kjønniksen I. UV-Absorbing compounds in the aqueous humor from aquatic mammals and various non-mammalian vertebrates. Ophthalmic Res. 2003;35:208–216. doi: 10.1159/000071172. [DOI] [PubMed] [Google Scholar]
- 104.Wielgus AR, Sarna T. Ascorbate enhances photogeneration of hydrogen peroxide mediated by the iris melanin. Photochem Photobiol. 2008;84:683–691. doi: 10.1111/j.1751-1097.2008.00341.x. [DOI] [PubMed] [Google Scholar]
- 105.Megaw JM. Glutathione and ocular photobiology. Curr Eye Res. 1984;3:83–87. doi: 10.3109/02713688408997189. [DOI] [PubMed] [Google Scholar]
- 106.Benoist d'Azy C, Pereira B, Chiambaretta F, Dutheil F. Oxidative and anti-oxidative stress markers in chronic glaucoma: A systematic review and meta-analysis. PLoS One. 2016;11(e0166915) doi: 10.1371/journal.pone.0166915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Yağci R, Gürel A, Ersöz I, Keskin UC, Hepşen IF, Duman S, Yiğitoğlu R. Oxidative stress and protein oxidation in pseudoexfoliation syndrome. Curr Eye Res. 2006;31:1029–1032. doi: 10.1080/02713680601001319. [DOI] [PubMed] [Google Scholar]
- 108.Yimaz A, Adigüzel U, Tamer L, Yildirim O, Oz O, Vatansever H, Ercan B, Değirmenci US, Atik U. Serum oxidant/antioxidant balance in exfoliation syndrome. Clin Exp Ophthalmol. 2005;33:63–66. doi: 10.1111/j.1442-9071.2005.00944.x. [DOI] [PubMed] [Google Scholar]
- 109.Faschinger C, Schmut O, Wachswender C, Mossböck G. Glaucoma and oxidative stress. Determination of malondialdehyde-a product of lipid peroxidation. Ophthalmologe. 2006;103:953–959. doi: 10.1007/s00347-006-1399-3. (In German) [DOI] [PubMed] [Google Scholar]
- 110.Aydın Yaz Y, Yildirim N, Yaz Y, Tekin N, İnal M, Şahin FM. Role of oxidative stress in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Turk J Ophthalmol. 2019;49:61–67. doi: 10.4274/tjo.galenos.2018.10734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Schlötzer-Schrehardt U. Oxidative stress and pseudoexfoliation glaucoma. Klin Monbl Augenheilkd. 2010;227:108–113. doi: 10.1055/s-0028-1109977. (In German) [DOI] [PubMed] [Google Scholar]
- 112.Shirakami T, Yamanaka M, Fujihara J, Matsuoka Y, Gohto Y, Obana A, Tanito M. Advanced glycation end product accumulation in subjects with open-angle glaucoma with and without exfoliation. Antioxidants (Basel) 2020;9(755) doi: 10.3390/antiox9080755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Park CH, Kim JW. Effect of advanced glycation end products on oxidative stress and senescence of trabecular meshwork cells. Korean J Ophthalmol. 2012;26:123–131. doi: 10.3341/kjo.2012.26.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Strzalka-Mrozik B, Prudlo L, Kimsa MW, Kimsa MC, Kapral M, Nita M, Mazurek U. Quantitative analysis of SOD2, ALDH1A1 and MGST1 messenger ribonucleic acid in anterior lens epithelium of patients with pseudoexfoliation syndrome. Mol Vis. 2013;19:1341–1349. [PMC free article] [PubMed] [Google Scholar]
- 115.Gartaganis SP, Patsoukis NE, Nikolopoulos DK, Georgiou CD. Evidence for oxidative stress in lens epithelial cells in pseudoexfoliation syndrome. Eye (Lond) 2007;21:1406–1411. doi: 10.1038/sj.eye.6702596. [DOI] [PubMed] [Google Scholar]
- 116.Gartaganis SP, Georgakopoulos CD, Patsoukis NE, Gotsis SS, Gartaganis VS, Georgiou CD. Glutathione and lipid peroxide changes in pseudoexfoliation syndrome. Curr Eye Res. 2005;30:647–651. doi: 10.1080/02713680590968367. [DOI] [PubMed] [Google Scholar]
- 117.Browne JG, Ho SL, Kane R, Oliver N, Clark AF, O'Brien CJ, Crean JK. Connective tissue growth factor is increased in pseudoexfoliation glaucoma. Invest Ophthalmol Vis Sci. 2011;52:3660–3666. doi: 10.1167/iovs.10-5209. [DOI] [PubMed] [Google Scholar]
- 118.Wang HJ, Kochevar IE. Involvement of UVB-induced reactive oxygen species in TGF-beta biosynthesis and activation in keratinocytes. Free Radical Bio Med. 2005;38:890–897. doi: 10.1016/j.freeradbiomed.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 119.Galli A, Svegliati-Baroni G, Ceni E, Milani S, Ridolfi F, Salzano R, Tarocchi M, Grappone C, Pellegrini G, Benedetti A, et al. Oxidative stress stimulates proliferation and invasiveness of hepatic stellate cells via a MMP2-mediated mechanism. Hepatology. 2005;41:1074–1084. doi: 10.1002/hep.20683. [DOI] [PubMed] [Google Scholar]
- 120.Schlötzer-Schrehardt U, Lommatzsch J, Küchle M, Konstas AG, Naumann GO. Matrix metalloproteinases and their inhibitors in aqueous humor of patients with pseudoexfoliation syndrome/glaucoma and primary open-angle glaucoma. Invest Ophthalmol Vis Sci. 2003;44:1117–1125. doi: 10.1167/iovs.02-0365. [DOI] [PubMed] [Google Scholar]
- 121.Majora M, Wittkampf T, Schuermann B, Schneider M, Franke S, Grether-Beck S, Wilichowski E, Bernerd F, Schroeder P, Krutmann J. Functional consequences of mitochondrial DNA deletions in human skin fibroblasts: Increased contractile strength in collagen lattices is due to oxidative stress-induced lysyl oxidase activity. Am J Pathol. 2009;175:1019–1029. doi: 10.2353/ajpath.2009.080832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Voloshenyuk TG, Hart AD, Khoutorova E, Gardner JD. TNF-α increases cardiac fibroblast lysyl oxidase expression through TGF-β and PI3Kinase signaling pathways. Biochem Biophys Res Commun. 2011;413:370–375. doi: 10.1016/j.bbrc.2011.08.109. [DOI] [PubMed] [Google Scholar]
- 123.Tezel G, Yang X, Cai J. Proteomic identification of oxidatively modified retinal proteins in a chronic pressure-induced rat model of glaucoma. Invest Ophthalmol Vis Sci. 2005;46:3177–3187. doi: 10.1167/iovs.05-0208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chrysostomou V, Rezania F, Trounce IA, Crowston JG. Oxidative stress and mitochondrial dysfunction in glaucoma. Curr Opin Pharmacol. 2013;13:12–15. doi: 10.1016/j.coph.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 125.Fan Gaskin JC, Shah MH, Chan EC. Oxidative stress and the role of NADPH oxidase in glaucoma. Antioxidants (Basel) 2021;10(238) doi: 10.3390/antiox10020238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Izzotti A, Bagnis A, Saccà SC. The role of oxidative stress in glaucoma. Mutat Res. 2006;612:105–114. doi: 10.1016/j.mrrev.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 127.Koliakos GG, Konstas AG, Schlötzer-Schrehardt U, Hollo G, Katsimbris IE, Georgiadis N, Ritch R. 8-Isoprostaglandin F2a and ascorbic acid concentration in the aqueous humour of patients with exfoliation syndrome. Br J Ophthalmol. 2003;87:353–356. doi: 10.1136/bjo.87.3.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Botling Taube A, Konzer A, Alm A, Bergquist J. Proteomic analysis of the aqueous humour in eyes with pseudoexfoliation syndrome. Br J Ophthalmol. 2019;103:1190–1194. doi: 10.1136/bjophthalmol-2017-310416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Dursun F, Vural Ozec A, Aydin H, Topalkara A, Dursun A, Toker MI, Erdogan H, Arici MK. Total oxidative stress, paraoxonase and arylesterase levels at patients with pseudoexfoliation syndrome and pseudoexfoliative glaucoma. Int J Ophthalmol. 2015;8:985–990. doi: 10.3980/j.issn.2222-3959.2015.05.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Dmuchowska DA, Pietrowska K, Krasnicki P, Kowalczyk T, Misiura M, Grochowski ET, Mariak Z, Kretowski A, Ciborowski M. Metabolomics reveals differences in aqueous humor composition in patients with and without pseudoexfoliation syndrome. Front Mol Biosci. 2021;8(682600) doi: 10.3389/fmolb.2021.682600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Koliakos GG, Konstas AG, Schlötzer-Schrehardt U, Bufidis T, Georgiadis N, Ringvold A. Ascorbic acid concentration is reduced in the aqueous humor of patients with exfoliation syndrome. Am J Ophthalmol. 2002;134:879–883. doi: 10.1016/s0002-9394(02)01797-x. [DOI] [PubMed] [Google Scholar]
- 132.Ferreira SM, Lerner SF, Brunzini R, Evelson PA, Llesuy SF. Antioxidant status in the aqueous humour of patients with glaucoma associated with exfoliation syndrome. Eye (Lond) 2009;23:1691–1697. doi: 10.1038/eye.2008.352. [DOI] [PubMed] [Google Scholar]
- 133.Sorkhabi R, Ghorbanihaghjo A, Ahoor M, Nahaei M, Rashtchizadeh N. High-sensitivity C-reactive protein and tumor necrosis factor alpha in pseudoexfoliation syndrome. Oman Med J. 2013;28:16–19. doi: 10.5001/omj.2013.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Tetikoğlu M, Aktas S, Sağdik HM, Özcura F, Uçar F, Koçak H, Neşelioğlu S, Erel Ö. Thiol disulfide homeostasis in pseudoexfoliation syndrome. Curr Eye Res. 2017;42:876–879. doi: 10.1080/02713683.2016.1256412. [DOI] [PubMed] [Google Scholar]
- 135.Koliakos GG, Konstas AG, Schlötzer-Schrehardt U, Hollo G, Mitova D, Kovatchev D, Maloutas S, Georgiadis N. Endothelin-1 concentration is increased in the aqueous humour of patients with exfoliation syndrome. Br J Ophthalmol. 2004;88:523–527. doi: 10.1136/bjo.2003.028290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Koukoula SC, Katsanos AK, Tentes IK, Labiris G, Kozobolis VP. Retrobulbar hemodynamics and aqueous humor levels of endothelin-1 in exfoliation syndrome and exfoliation glaucoma. Clin Ophthalmol. 2018;12:1199–1204. doi: 10.2147/OPTH.S155551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Park DY, Kim M, Cha SC. Cytokine and growth factor analysis in exfoliation syndrome and glaucoma. Invest Ophthalmol Vis Sci. 2021;62(6) doi: 10.1167/iovs.62.15.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Zenkel M, Lewczuk P, Jünemann A, Kruse FE, Naumann GO, Schlötzer-Schrehardt U. Proinflammatory cytokines are involved in the initiation of the abnormal matrix process in pseudoexfoliation syndrome/glaucoma. Am J Pathol. 2010;176:2868–2879. doi: 10.2353/ajpath.2010.090914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Stafiej J, Hałas-Wiśniewska M, Izdebska M, Gagat M, Grzanka D, Grzanka A, Malukiewicz G. Immunohistochemical analysis of microsomal glutathione S-transferase 1 and clusterin expression in lens epithelial cells of patients with pseudoexfoliation syndrome. Exp Ther Med. 2017;13:1057–1063. doi: 10.3892/etm.2017.4085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Sarenac Vulovic TS, Pavlovic SM, Jakovljevic VLj, Janicijevic KB, Zdravkovic NS. Nitric oxide and tumour necrosis factor alpha in the process of pseudoexfoliation glaucoma. Int J Ophthalmol. 2016;9:1138–1142. doi: 10.18240/ijo.2016.08.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Turan G, Turan M. The evaluation of TUNEL, PCNA and SOX2 expressions in lens epithelial cells of cataract patients with pseudoexfoliation syndrome. Curr Eye Res. 2020;45:12–16. doi: 10.1080/02713683.2019.1657463. [DOI] [PubMed] [Google Scholar]
- 142.Papadopoulou G, Zisimopoulos D, Kalaitzopoulou E, Makri OE, Tsapardoni FN, Georgakopoulos CD, Georgiou CD. Age-related aqueous humor (AH) and lens epithelial cell/capsule protein carbonylation and AH protein concentration in cataract patients who have pseudoexfoliative diseases. Mol Vis. 2018;24:890–901. [PMC free article] [PubMed] [Google Scholar]
- 143.Uçakhan OO, Karel F, Kanpolat A, Devrim E, Durak I. Superoxide dismutase activity in the lens capsule of patients with pseudoexfoliation syndrome and cataract. J Cataract Refract Surg. 2006;32:618–622. doi: 10.1016/j.jcrs.2006.01.018. [DOI] [PubMed] [Google Scholar]
- 144.Tetikoğlu M, Sağdik HM, Aktas S, Uçar F, Özcura F. Serum prolidase activity and oxidative stress in patients with pseudoexfoliation syndrome. Graefes Arch Clin Exp Ophthalmol. 2016;254:1339–1343. doi: 10.1007/s00417-016-3338-6. [DOI] [PubMed] [Google Scholar]
- 145.Fountoulakis N, Labiris G, Aristeidou A, Katsanos A, Tentes I, Kortsaris A, Kozobolis VP. Tissue inhibitor of metalloproteinase 4 in aqueous humor of patients with primary open angle glaucoma, pseudoexfoliation syndrome and pseudoexfoliative glaucoma and its role in proteolysis imbalance. BMC Ophthalmol. 2013;13(69) doi: 10.1186/1471-2415-13-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Simavli H, Tosun M, Bucak YY, Erdurmus M, Ocak Z, Onder HI, Acar M. Serum and aqueous xanthine oxidase levels, and mRNA expression in anterior lens epithelial cells in pseudoexfoliation. Graefes Arch Clin Exp Ophthalmol. 2015;253:1161–1167. doi: 10.1007/s00417-015-3043-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.