Abstract
Lateral meniscal posterior root tears are defined as tears of meniscus within 9 mm from the bony root attachment. Unrepaired root tears significantly compromise the biomechanical functions of the meniscus, resulting in early and accelerated osteoarthritis. Several authors have described various techniques to reattach the posterior root of the lateral meniscus, and decent short-term results have been observed. Although most previous techniques are capable of repairing radial root tears, difficulties are encountered when repairing oblique type IV tears. In this technique note, the author describes an efficient side-to-side repair technique using the FAST-FIX system, which is practical in repairing the type IV tears of the lateral meniscus. This technique includes certain sequence of the stitches and skills of controlling the root remnant, which makes it easy to penetrate the meniscus and to achieve anatomic repair.
Technique Video
An all-inside repair technique for a type IV lateral meniscal posterior root tear using the FAST-FIX device. The patient lies supine with the operative knee (left knee) in 90° flexion. Viewing from the anteromedial portal, a type-IV LMPRT is confirmed. The FAST-FIX meniscal repair device is introduced through the anterolateral portal. Two simple sutures are placed across the tear gap with a special sequence of the four stitches. Skills of using the thread end and the meniscal repair device as controllers of the root remnant are crucial for efficiently performing the third stitch.
Introduction
The lateral meniscus (LM) is a semicircular-shaped fibrocartilage anchored to the tibial plateau by the lateral meniscus roots. The essential biomechanical functions of the LM include shock absorption, load conversion, contact pressure distribution, and joint stabilization.1,2 The integrity of the posterior lateral meniscus root prevents meniscus extrusion, thereby enabling the LM to convert tibiofemoral pressure into hoop stress and, thus, protecting the knee joint cartilage.3,4
The lateral meniscal posterior root tear (LMPRT) is described as the disruption of the meniscus within 9 mm to the insertion point. In the setting of anterior cruciate ligament reconstruction (ACLR), LMPRT is identified in 7-12% of patients.5 LMPRT compromises the biomechanical functions of the LM, resulting in increased contact pressure, increased knee instability, and even accelerated osteoarthritis.6 Although conservative treatments delayed osteoarthritis progression in selected patients,7,8 repairing the meniscus root tears is the only possible way to restore the biomechanical properties of the LM. Recently, various techniques have been introduced to repair LMPRT and decent short-term results have been reported.9, 10, 11
While most techniques are suitably applied to type II tears, described as complete radial tears within 9 mm from the bony root attachment,2 we found some limitations of these previous techniques when facing type IV tears (complex oblique or longitudinal tears with complete root detachment) in clinical practice. This type of lesion created an acute-angled root remnant with the inner rim much longer than the outer rim, rather than the radial-directional tears in the type II tears, resulting in difficulty of penetrating the meniscal tissue, inadequacy of shortening the gap, and nonanatomic repair (Fig 1). Therefore, we introduced an all-inside side-to-side repair technique for the type IV LMPRT, using the FAST-FIX 360 all-inside meniscal repair device (Smith & Nephew, Andover, MA). This technique makes it easy to penetrate the meniscal tissue, shorten the gap, and achieve anatomic repair.
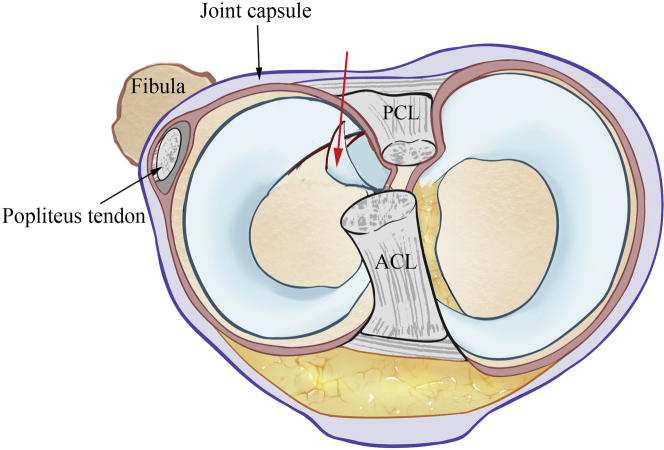
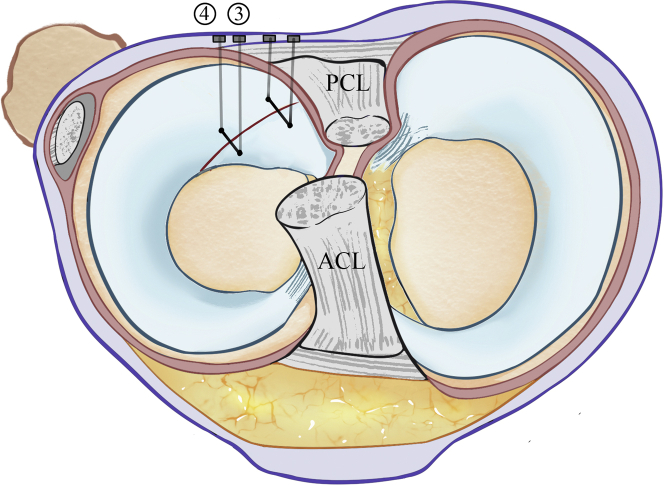
Fig 1.
The schematic diagram of an unstable type IV lateral meniscal posterior root tear. Different from the type II radial root tear, the type IV root tear has an acute-angled root remnant, which is frequently folded (red arrow). When repairing the type IV LMPRTs, difficulty in penetrating the root remnant could be encountered, resulting in inaccurate penetration location and nonanatomic repair. This diagram is the basic view of the latter explanation. ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
Surgical Technique
Patient Positioning and Anesthesia
The patient is positioned supine, and a tourniquet is placed on the operative thigh. After general anesthesia is induced, the foot of the operative table is removed. The knee is prepared and draped for routine knee arthroscopy after the examination of knee stability and range of motion.
Diagnostic Arthroscopy
Standard anteromedial and anterolateral portal are made. The anterior cruciate ligament (ACL) remnants are debrided first to provide a clearer view of the lateral compartment if concomitant ACL rupture is detected. The LM root is inspected and probed to classify the type of the tear. In most type IV tears of the LMPRT, the acute-angled root remnant folds back toward the bony root attachment, which should be unfolded carefully in order to examine the gap between the root remnant and the posterior horn. The length of the root remnant and the state of the damaged meniscus are also assessed to determine whether the tear is repairable. The surgical techniques are explained in Video 1.
All-Inside Repair Technique
The repair devices are introduced through the anterolateral portal, while visualization was conducted through the anteromedial portal. A shaver is used for the debridement of meniscus root lesion, then the FAST-FIX 360 all-inside meniscal repair device (Smith & Nephew, Andover, MA) is inserted.
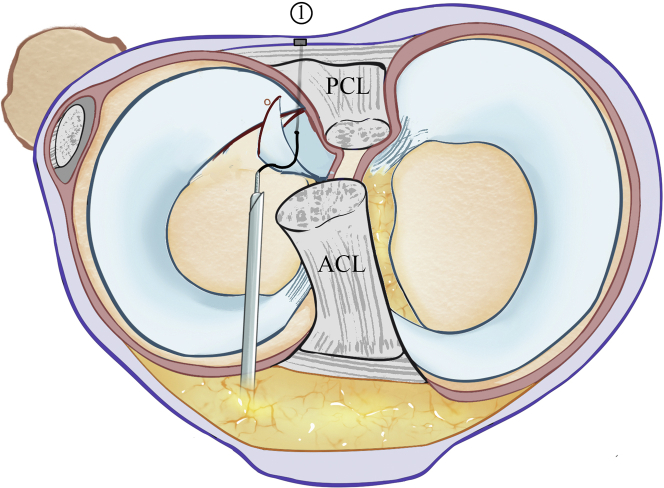
The first penetration spot is located at the outer rim of the root remnant (penetration depth 12-14 mm). The outer rim is shorter in length and secured by the joint capsule, which makes it easier to penetrate exactly at the spot anticipated (Fig 2). The second penetration spot is located at the outer rim of the end of the meniscus across the tear line. After these two suture bar anchors are inserted into the joint capsule, the pretied knot is slowly tightened to make sure the gap between the two ends of the meniscus is well eliminated. The thread end of the first suture is left without clipping and is pulled out through the anterolateral portal.
Fig 2.
First suture. The view is obtained from the anteromedial portal, and the meniscal repair device is introduced through the anterolateral portal. The first suture is placed on the outer rim of the lateral meniscus for the purpose of easy penetration since the joint capsule confines its mobility. The first penetration spot is located at the outer rim of the root remnant while the second penetration spot is located at the outer rim of the meniscus across the tear line (red circle). The thread end of the first suture will be unclipped and pulled out of the anterolateral portal. The number shows the sequence of the stitches. ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
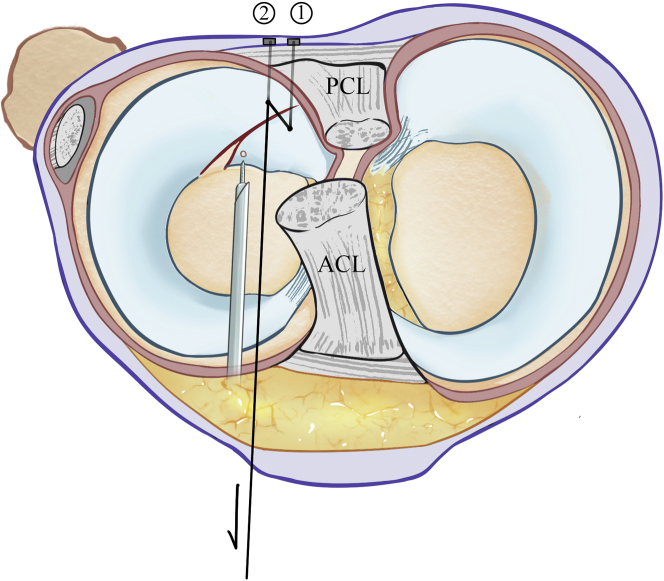
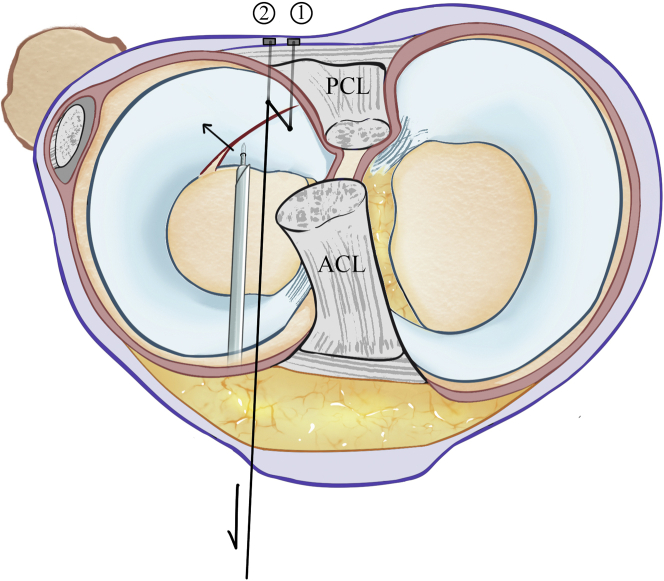
The second suture is placed parallel to the first one at the inner rim to form a two-single-suture configuration. The third penetration spot (the first stitch of the second suture) is placed at the inner rim of the root remnant, which is close to the tail-end (Fig 3). Unlike the outer rim which is limited by the meniscocapsular attachments, the inner rim is usually floating in the saline solution. The needle tip always pushes the root remnant forwards rather than penetrates the tissue, not to mention the precision of the penetration. Therefore, by pulling the thread end of the first suture, a tractive force is applied on the root remnant, which makes easy and precise penetration possible. The needle tip first penetrates the root remnant without the joint capsule; therefore, both the thread end and the FAST-FIX device are used as the controllers of the root remnant (Fig 4). After the tear gap is smoothly eliminated, the needle tip continues to penetrate the joint capsule, and the suture bar anchor is released afterward. The fourth and last penetration spot is located at the inner rim of the end of the meniscus across the tear line. Finally, the second suture is tightened to completely eliminate the gap and integrate the root remnant and the posterior horn of the LM. After the repair procedures, a probe is used to examine the tension of the LM, and then the thread ends are clipped (Fig 5).
Fig 3.
Second suture. The second suture is placed on the inner rim of the meniscus parallel to the first one. The acute-angled root remnant is difficult to penetrate due to its high mobility. When performing the third penetration (red circle indicates the penetration spot), the unclipped thread end of the first suture is pulled to stabilize the root remnant. The black arrow indicates the tractive force applied on the root remnant via the thread. ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
Fig 4.
Second suture. When performing the third penetration, the needle tip initially penetrates the root remnant without the joint capsule. Thus, both the thread end and the FAST-FIX device are used as the controllers of the root remnant. The black arrows indicate the two forces applied on the root remnant to control its movement. The tear gap is smoothly eliminated, and anatomic repair is exercisable. ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
Fig 5.
Final view. After examining the lateral meniscus, the thread ends are clipped. A two-simple-suture configuration is established. The type IV lateral meniscal posterior root tear is anatomically repaired, and the tear gap is completely eliminated. The numbers show the sequence of the stitches. ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
Postoperative Protocol
The patient is not allowed any weightbearing on the affected knee until 4 weeks, while range of motion is limited from 0 to 90°. Quadriceps sets, straight-leg raises, and prone hangs are initiated on day 1, and passive motion exercise starts from week 2. Full weight-bearing and full flexion of the knee are achieved around week 8. Full sports activities are allowed after 6 months.
Discussion
LMPRT is frequently concomitant with ACL rupture and disturbs the biomechanical function of the lateral meniscus, resulting in the deficiency of the hoop stress and increased tibiofemoral pressure. Though only mild joint-space narrowing was observed in the long term,7 more researchers have advocated repairing the LMPRT when possible, as it restores the biomechanical function of the LM. Conventional techniques of side-to-side repairs target the type II root tears, while limitations have been shown when repairing the type IV root tears. Therefore, we described a technique specialized for type IV root tears to achieve easy operation and anatomic repair.
Recently, various techniques, such as transtibial pull-out repair, all-inside repair have been introduced as treatments of the LMPRT, and favorable results have been shown in several studies. Zheng et al.11 performed a meta-analysis, including 215 cases of LMPRT and concluded that clinical, radiographic, and arthroscopic outcomes improved at short-term follow-ups. Although few studies have compared the long-term results of repairing LMPRT with conservative treatments, it is known that unrepaired root lesions will increase the tibiofemoral contact pressure and might cause accelerated osteoarthritis.12 Thus, it is more recognized by surgeons that the LMPRT should be repaired as much as possible whenever identified.
The type II root tear is characterized as a radial root tear while the type IV root tear is defined as an oblique tear. This morphological difference of the LMPRT emphasizes different technical key points during arthroscopic repairing. Unlike the broad square-shaped root remnant of the type II tear, the type IV root tear forms a narrow tail-shaped root remnant that is always floating and folded when inspected. This feature makes it difficult to 1) penetrate and precisely penetrate the meniscus tissue, especially for the stitch aiming at the tail end of the root remnant (the inner rim of the root remnant), and 2) smoothly and completely eliminate the tear gap when employing the conventional techniques to the type IV root tears.
We described an efficient side-to-side repair technique using the FAST-FIX system, which was practical in repairing the type IV tears of LMPRT. Our technique tackled the two difficulties mentioned above by 1) adjusting and determining a routine sequence of the four stitches, 2) leaving the thread end of the first suture unclipped, 3) initially penetrating the inner rim of the root remnant without the joint capsule, and 4) using them as controllers of the root remnant when performing the second suture. The first suture was placed on the outer rim as the meniscocapsular junction stabilized the meniscal tissue and made it easy to insert the needle tip. Then, by pulling the thread end of the first suture, the tail-shaped root remnant was adjusted to a proper position and relatively immobilized, which made easy and precise penetration on the inner rim possible. After initially penetrating the root remnant without the joint capsule, both the thread end and the meniscal repair device were used to move the root remnant to align the edges of the two sides and to smoothly eliminate the tear gap. Therefore, by applying this technique to the type IV LMPRTs, anatomic repair was feasible. Daney et al.3 reported a remarkable biomechanical function recovery of the anatomic repair, while nonanatomic repair resulted in significantly higher pressure and decreased tibiofemoral contact area.
This technique provides an easy and efficient way of repairing type IV root tears of the lateral meniscus. Surgeons experienced in knee arthroscopy and with the mastery of the meniscal repair device are competent to perform this technique. No arthroscopic suture-passing and knot-tying techniques are required. Other advantages include easy and precise penetration as well as anatomic repair. However, surgeons should also be alerted that popliteal vessels damages could happen in LMPRT repairs with all-inside repair techniques.13 The advantages, risks, and limitations are listed in Table 1.
Table 1.
Advantages, Risks, and Limitations
| Advantages |
| Only standard anterior portals are used |
| No need for arthroscopic suture-passing and knot-tying techniques |
| No bone tunnels are required |
| Easy and precise penetration for every stitch |
| Smooth and complete elimination of the tear gap |
| Allows for anatomic repair: restore the biomechanical functions |
| Risk and limitations |
| Potential risks of popliteal vessel damages |
| The threads may cut out the meniscus. |
| Meniscal repair devices are needed. |
Posterior root tear of the lateral meniscus should be identified and repaired to protect the knee joint. We developed an all-inside repair technique specialized for the type IV LMPRT, which allows easy and precise penetration and anatomic repair. This technique is an available option and could be a standard procedure for the repair of the type IV LMPRTs.
Footnotes
The authors report the following potential conflicts of interest or sources of funding. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
An all-inside repair technique for a type IV lateral meniscal posterior root tear using the FAST-FIX device. The patient lies supine with the operative knee (left knee) in 90° flexion. Viewing from the anteromedial portal, a type-IV LMPRT is confirmed. The FAST-FIX meniscal repair device is introduced through the anterolateral portal. Two simple sutures are placed across the tear gap with a special sequence of the four stitches. Skills of using the thread end and the meniscal repair device as controllers of the root remnant are crucial for efficiently performing the third stitch.
References
- 1.Frank J.M., Moatshe G., Brady A.W., et al. Lateral meniscus posterior root and meniscofemoral ligaments as stabilizing structures in the ACL-deficient knee: A biomechanical study. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117695756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krych A.J., Hevesi M., Leland D.P., Stuart M.J. Meniscal root injuries. J Am Acad Orthop Sur. 2020;28:491–499. doi: 10.5435/JAAOS-D-19-00102. [DOI] [PubMed] [Google Scholar]
- 3.Daney B.T., Aman Z.S., Krob J.J., et al. Utilization of transtibial centralization suture best minimizes extrusion and restores tibiofemoral contact mechanics for anatomic medial meniscal root repairs in a cadaveric model. Am J Sports Med. 2019;47:1591–1600. doi: 10.1177/0363546519844250. [DOI] [PubMed] [Google Scholar]
- 4.Zhuo H., Pan L., Xu Y., Li J. Functional, magnetic resonance imaging, and second-look arthroscopic outcomes after pullout repair for avulsion tears of the posterior lateral meniscus root. Am J Sports Med. 2021;49:450–458. doi: 10.1177/0363546520976635. [DOI] [PubMed] [Google Scholar]
- 5.Feucht M.J., Salzmann G.M., Bode G., et al. Posterior root tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2015;23:119–125. doi: 10.1007/s00167-014-2904-x. [DOI] [PubMed] [Google Scholar]
- 6.Pache S., Aman Z.S., Kennedy M., et al. Meniscal root tears: Current concepts review. Arch Bone Joint Surg. 2018;6:250–259. [PMC free article] [PubMed] [Google Scholar]
- 7.Shelbourne K.D., Roberson T.A., Gray T. Long-term evaluation of posterior lateral meniscus root tears left in situ at the time of anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:1439–1443. doi: 10.1177/0363546511398212. [DOI] [PubMed] [Google Scholar]
- 8.Shumborski S.J., Salmon L.J., Monk C.I., Pinczewski L.A. Stable lateral meniscal posterior root tears left in situ at time of anterior cruciate ligament reconstruction are of minimal long-term clinical detriment. Arthroscopy. 2021;37:3500–3506. doi: 10.1016/j.arthro.2021.04.075. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Z., Zhou Y., Luo H., et al. A novel surgical technique for arthroscopic repair of type II posterior lateral meniscal root tear. Knee. 2020;27:1560–1566. doi: 10.1016/j.knee.2020.07.100. [DOI] [PubMed] [Google Scholar]
- 10.Mao D.W., Lee Y.H.D. All-inside techniques for meniscal radial root tear repair. Arthrosc Tech. 2020;9:e1541–e1545. doi: 10.1016/j.eats.2020.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zheng T., Song G., Li Y., et al. Clinical, radiographic, and arthroscopic outcomes of surgical repair for radial and avulsed lesions on the lateral meniscus posterior root during ACL reconstruction: A systematic review. Orthop J Sports Med. 2021;9 doi: 10.1177/2325967121989678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang Z., Luo H., Zhang H., et al. H-Plasty repair technique improved tibiofemoral contact mechanics after repair for adjacent radial tears of posterior lateral meniscus root: A biomechanical study. Arthroscopy. 2021;37:2204–2216.e2. doi: 10.1016/j.arthro.2021.02.017. [DOI] [PubMed] [Google Scholar]
- 13.Oehler N., Foerg A., Haenle M., Blanke F., Vogt S. Assessment of popliteal neurovascular safety during all-inside suturing of the posterior horn of the lateral meniscus using Upright MRIs of the knee joint. Knee. 2021;33:234–242. doi: 10.1016/j.knee.2021.10.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
An all-inside repair technique for a type IV lateral meniscal posterior root tear using the FAST-FIX device. The patient lies supine with the operative knee (left knee) in 90° flexion. Viewing from the anteromedial portal, a type-IV LMPRT is confirmed. The FAST-FIX meniscal repair device is introduced through the anterolateral portal. Two simple sutures are placed across the tear gap with a special sequence of the four stitches. Skills of using the thread end and the meniscal repair device as controllers of the root remnant are crucial for efficiently performing the third stitch.
An all-inside repair technique for a type IV lateral meniscal posterior root tear using the FAST-FIX device. The patient lies supine with the operative knee (left knee) in 90° flexion. Viewing from the anteromedial portal, a type-IV LMPRT is confirmed. The FAST-FIX meniscal repair device is introduced through the anterolateral portal. Two simple sutures are placed across the tear gap with a special sequence of the four stitches. Skills of using the thread end and the meniscal repair device as controllers of the root remnant are crucial for efficiently performing the third stitch.