Abstract
The discoid meniscus is a congenital abnormality, with the vast majority occurring in the lateral meniscus. More commonly seen in pediatric populations, patients present with acute or chronic knee symptoms such as joint line pain, audible or palpable mechanical symptoms, and the inability to achieve terminal extension. The classic discoid classification system by Watanabe excludes anterior and horizontal instability and tearing that commonly occur with this pathology. A comprehensive classification, the Pediatric Research in Sports Medicine (PRiSM) Discoid Meniscus Classification, was developed to include these characteristics. To complement this classification system, we describe a complete arthroscopic examination of the discoid meniscus, assessing meniscal width, height, instability, and tearing. For thorough anterior assessment, the importance of medial portal viewing with lateral portal probing is highlighted. Assessment of the meniscus for tearing and instability should be performed before and after saucerization. Consistent use of a comprehensive classification system and a diagnostic arthroscopic exam will improve the understanding, treatment, and quality of research in the discoid meniscus.
Technique Video
Arthroscopic technique for discoid meniscus evaluation.
The lateral discoid meniscus (LDM) is the most common congenital anomaly of the knee, present in an estimated 5% of the population.1 Presentation can vary from the asymptomatic LDM, with minimally increased width and height and stable peripheral capsular attachments, to markedly thickened, displaced, and unstable meniscal tissue with central and peripheral tearing. This heterogeneity makes diagnosis, classification, and treatment of LDM difficult.
The classically described Watanabe classification2 does not capture the full spectrum of discoid menisci pathomorphology, as it splits the discoid meniscus into 3 basic categories: complete (type I), incomplete (type II), and posterior peripheral instability (type III, Wrisberg variant). This classification includes only LDM characteristics of width and posterior peripheral stability; it excludes a description of height, anterior and body instability, and tears of the meniscal tissue. Given the rarity of type III discoid menisci, the majority of LDMs are classified as type I or II, distinguished solely on the basis of meniscal width. Though simple to use, this classification lacks critical detail and the complexity required to guide diagnosis and treatment or provide consistent language for description in a clinical or research setting.
The Pediatric Research in Sports Medicine (PRiSM) LDM classification system was developed through a comprehensive review of existing classification systems, followed by nominal group technique consensus method. Four main features were included: meniscal width, meniscal height, peripheral stability, and meniscus tear (Table 1). To evaluate this classification, a comprehensive arthroscopic meniscal evaluation protocol was developed.3 Technique pearls (Table 2) were shared between authors for standardization of pathology definition and accuracy of diagnosis. This technique describes a thorough LDM evaluation while highlighting key components of the PRiSM LDM classification.
Table 1.
Pediatric Research in Sports Medicine (PRiSM) Lateral Discoid Meniscus Classification System
| Classification Component |
|---|
| Meniscal width/surface area |
| Incomplete |
| Near complete/complete |
| Meniscal height |
| Normal |
| Abnormal |
| Instability |
| Normal stability |
| Abnormal stability |
| In anterior half of meniscus |
| In posterior half of meniscus |
| In anterior and posterior meniscus |
| Tear type |
| No tear or tear in central portion/saucerization zone |
| Horizontal |
| Degenerative/complex/radial |
| Tear location |
| No tear or tear in central portion/saucerization zone |
| Anterior half |
| Posterior half |
| Anterior and posterior halves |
Table 2.
Pearls and pitfalls
| Pearls | Pitfalls |
|---|---|
| Evaluate magnetic resonance imaging preoperatively based on classification | Defining tear vs instability |
| Medial portal location more proximal and medial than standard medial portal | Complex, multiplanar tear patterns are difficult to describe |
| Use medial portal for arthroscopic viewing and lateral portal for working portal | |
| Consider smaller arthroscope in smaller knees | |
| Probe meniscus pre- and post-saucerization | |
| Probe anterior, midbody, and peripheral meniscocapsular attachments | |
| Be cautious around popliteal hiatus as may be enlarged or involved in tear |
Technique
The technique is illustrated in the Video 1. Standard anteromedial and anterolateral knee portals are established. The anteromedial portal can be established with spinal needle localization while viewing the lateral compartment if extensive lateral compartment work is expected or a tight lateral compartment is encountered. The traditional anteromedial portal may be shifted more proximal and medial to ease equipment passage over the tibial spines, facilitating usage in the lateral compartment. Lateral gutter visualization should include peripheral meniscus body quality and quantity evaluation to assist with determining saucerization thickness and repair technique options. Both figure-4 positioning or varus stress in a leg holder can be used for lateral compartment access based on surgeon preference.
Before saucerization, inspection of the entire lateral compartment and reduction of LDM tears should be completed to ascertain tissue quality, quantity, and location. Displaced or torn discoid meniscus tissue may be located within the notch, popliteal hiatus, or posterior to the femoral condyle and may be amendable to repair if reduced. Preoperative magnetic resonance imaging (MRI) evaluation can be a critical component of anticipating the location of pathology, location of displaced tissues, and repair technique options.
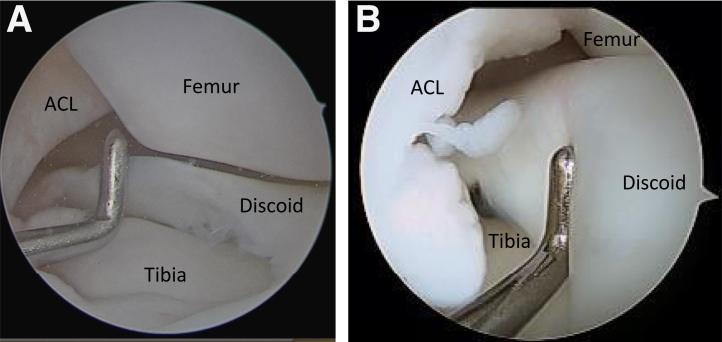
Starting with a standard 30° 4-mm arthroscope in the anterolateral portal and the probe in the medial portal, the width of the discoid meniscus is assessed relative to the tibial plateau (Fig. 1). Coverage of ≥90% of the tibial plateau indicates a near complete/complete discoid meniscus.
Figure 1.
Left knee arthroscopy with lateral viewing portal and medial probe. (A) Incomplete width. (B) Complete width,
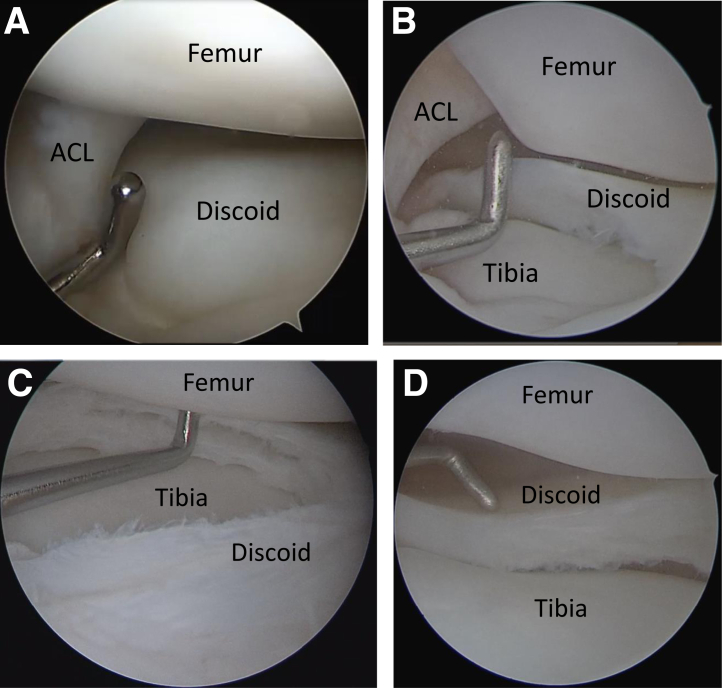
Next, the height of the discoid meniscus is assessed in comparison to the normal medial meniscus and relationship within the femoral tibial space. A meniscus of abnormal height shows excessive thickness for the femoral tibial joint space, increased thickness in comparison to the medial meniscus, or lacks gradual central tapering (Fig. 2).
Figure 2.
Left knee arthroscopy with lateral viewing portal and medial probe. (A and B) Abnormal height presaucerization. (C) Abnormal height post-saucerization. (D) Normal height post-saucerization.
Stability and tearing should be assessed via arthroscopic probing from both anteromedial and anterolateral portals. This improves diagnosis and accuracy of this patholog,y as normal arthroscopic meniscal evaluation with the camera in the lateral portal rarely involves a detailed anterior or body pathology evaluation.
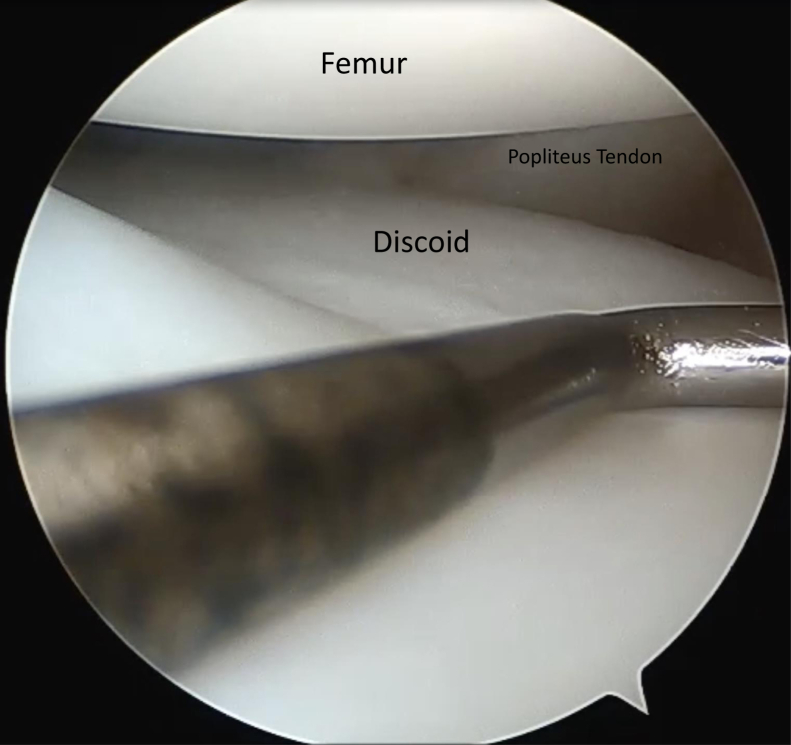
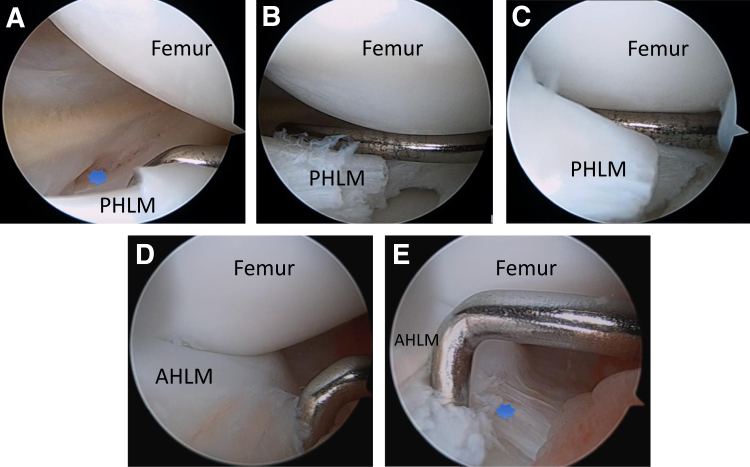
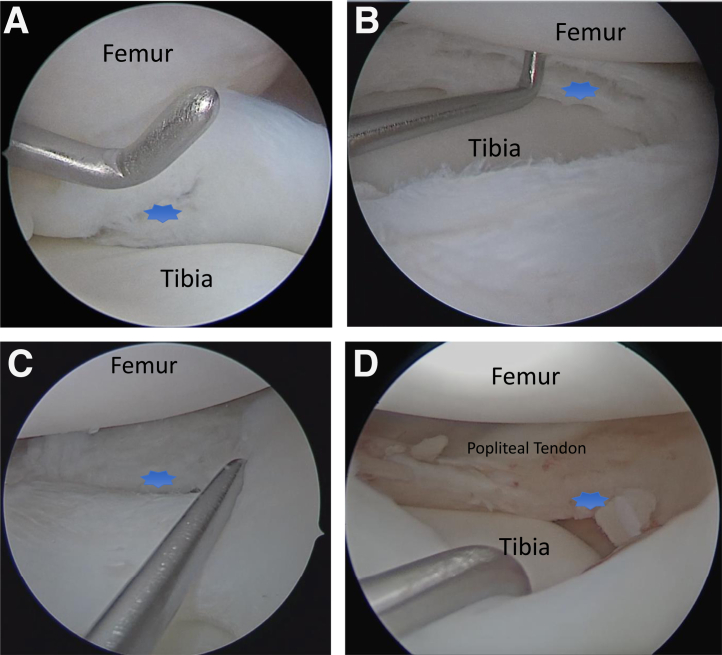
Stability is categorized as normal or abnormal. Abnormal stability is present if meniscal-capsular attachments are congenitally absent or deficient (the post-saucerization meniscus can translate past the midpoint/apex of the convexity of the lateral femoral condyle with probing) or in the presence of an unstable vertical tear in the postsaucerization peripheral meniscus or meniscal-capsular attachment. It is important to probe peripheral attachments posteriorly, at the midbody, and anteriorly, looking for translation of meniscus past the central weightbearing portion of the lateral femoral condyle. With the probe in the medial portal, posterior horn instability is assessed as the meniscus is pulled anteriorly from the posterior meniscocapsular junction and from the popliteal hiatus, and midbody instability is assessed by pulling the meniscus medially into the compartment. LDM can have an enlarged popliteal hiatus with abnormal capsular attachments increasing instability or tearing (Fig. 3). With the probe in the lateral portal and arthroscope in the medial portal, anterior instability is evaluated by pushing the anterior meniscus posteriorly under direct visualization into the lateral compartment (Fig. 4). Additionally, direct arthroscopic visualization of the lateral compartment during active range of motion from full flexion to full extension, looking for meniscal subluxation, can expose subtle instabilities.
Figure 3.
Left knee arthroscopy with lateral viewing portal and medial probe. Enlarged popliteal hiatus commonly seen in lateral discoid meniscus.
Figure 4.
Left knee arthroscopy with medial viewing portal and lateral probe. (A to C) Posterior meniscocapsular instability with anterior translation past the central weight bearing portion of the lateral femoral condyle. (D and E) Anterior meniscocapsular instability with posterior translation past the central weight bearing portion of the lateral femoral condyle. Abbreviations: AHLM, anterior horn lateral meniscus; PHLM, posterior horn lateral meniscus. ∗Meniscocapsular instability site.
Tears are determined to be present only if they are located within the post-saucerization, peripheral retained meniscus, making meniscal evaluation before and after saucerization important. Horizontal cleavage tears refer to those with >5 mm of horizontal width and a depth of >50% of the retained meniscus, or those extending into the vascular “red-red” zone, or peripheral third of the region of a normal meniscus. These horizontal tears are a finding unique to LDM and are caused by collagen disorganization within the central meniscal tissue. Other tear types can be present as well and are more familiar to experienced arthroscopists: radial, complex, or severely degenerative tears (Fig. 5).
Figure 5.
Left knee arthroscopy with lateral viewing portal and medial probe. (A) Central degeneration within the saucerization zone, not classified as a tear. (B) Horizontal tear. (C) Posterior horn “red-red” zone tear. (D) Posterior and midbody meniscocapsular tear.
Discussion
This arthroscopic technique enables arthroscopists to more thoroughly evaluate LDM (Table 3) and use the PRiSM Discoid Meniscus Classification,1 improving on Watanabe’s classification. Surgeons treating this pathology must understand the multiple subclassifications of LDM to best diagnose and treat their patients.
Table 3.
Advantages and disadvantages
| Advantages | Disadvantages |
|---|---|
| Improved visualization | Extra operating time |
| Improved ability to probe meniscus | |
| Improved discoid evaluation and diagnosis | |
| Improved ability to discuss discoid meniscus pathology with colleagues | |
| Improved ability to research discoid meniscus pathology, treatment, and outcomes |
Abnormal meniscal height and width are likely key factors in the development of LDM-associated pain, extension deficits, and eventually instability and tearing. Meniscal width is the first component assessed in the arthroscopic evaluation. Because of variation in knee size among pediatric patients and decreasing meniscal coverage of the tibial plateau with growth, a percentage of tibial plateau coverage is used for classification instead of a fixed-width measurement in millimeters. Surgeons should take note that meniscal position and plateau coverage vary depending on knee position during arthroscopy. Abnormal meniscus height likely interferes with normal femoral condyle and tibial plateau motion, particularly during deep squatting with rotation. This abnormal femoral roll back on the tibial plateau can lead to intrasubstance meniscal degeneration or peripheral tearing. Meniscal height is widely variable in normal meniscus, but experienced arthroscopists will find increased height in comparison to the medial meniscus, overfilling of the lateral femoral tibial space, and a lack of the expected central tapering of height.
After meniscal width and height, peripheral rim instability may be a key factor in the mechanical symptoms of a “snapping knee” presentation. There is a spectrum of instability from congenital absence of the meniscocapsular attachments to vertical tearing of the peripheral meniscus. Many LDMs may fall in the intermediate range of stability, wherein a thin rim of capsular attachments is difficult to distinguish as a congenital deficiency versus remodeled adhesions of a chronic tear. Regardless of cause, translation of the meniscus beyond the central condyle suggests poor meniscal function and risk for further degeneration from abnormal wear and mechanics. Because the anterior horn is incompletely visualized with anterolateral portal viewing, specifically viewing through the anteromedial portal and directly probing the anterior horn through the anterolateral portal is paramount to complex anterior horn stability assessment. Assessing both anterior and posterior peripheral stability intraoperatively should be a defining feature of diagnostic arthroscopy to determine the need for LDM stabilization.
Chronicity of symptoms likely determines the severity of tearing, whereas width, height, and congenital peripheral stability influence the tear type or pattern via the magnitude and vector of forces imposed on the discoid meniscus. Although the central meniscus is avascular and therefore susceptible to degenerative tears because of its collagen disorganization,4 this arthroscopic technique focuses on recognizing only the tearing that remains present after saucerization in the retained meniscal tissue. This exclusion is largely because saucerization is commonly performed to remove the central component, making tears involving the saucerized portion clinically unimportant because of a lack of influence on function or natural history of the retained meniscus. Conversely, for tears arising in or extending to the retained peripheral tissue, the tear type and tissue quality greatly influence the success of arthroscopic repair and may predict a patient’s long-term clinical outcome. Horizontal cleavage tears are frequently present in LDM and should be evaluated and defined separately from other tears.
This comprehensive arthroscopic evaluation is an easily adapted, stepwise approach to the discoid meniscus. We believe that standard inclusion of the anteromedial portal for viewing is superior to anterolateral-only evaluation of the meniscus. We believe that emphasis on assessing location and pattern of instability and tearing promotes a more systematic approach to LDM treatment.
Acknowledgments
This was a collaborative study of the PRiSM (Pediatric Research in Sports Medicine) Meniscus RIG (Research Interest Group). Other collaborators contributed significantly to this publication (in alphabetical order): Jay Albright, MD, Jennifer Brey, MD, Sasha Carsen, MD, Craig Finlayson, MD, Benjamin Heyworth, MD, Elaine Joughin, MD, Matthew Milewski, MD, Marie-Lyne Nault, MD, Jeffrey Nepple, MD, Emily Niu, MD, James L. Pace, MD, Tyler Stavinoha, MD, Zachary Stinson, MD, and Mark Tompkins, MD
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic technique for discoid meniscus evaluation.
References
- 1.Jordan M.R. Lateral meniscal variants: Evaluation and treatment. J Am Acad Orthop Surg. 1996;4:191–200. doi: 10.5435/00124635-199607000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Watanabe M., Takeda S., Ikeuchi H. Springer; 1969. Atlas of arthroscopy. [Google Scholar]
- 3.Lee R.J., Nepple J.J., Schmale G.A. PRISM Meniscus Research Interest Group, et al. Reliability of a new arthroscopic discoid lateral meniscus classification system: A multicenter video analysis. Am J Sports Med. 2022;50:1245–1253. doi: 10.1177/03635465221076857. [DOI] [PubMed] [Google Scholar]
- 4.Papadopoulos A., Kirkos J.M., Kapetanos G.A. Histomorphologic study of discoid meniscus. Arthroscopy. 2009;25:262–268. doi: 10.1016/j.arthro.2008.10.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic technique for discoid meniscus evaluation.
Arthroscopic technique for discoid meniscus evaluation.