Abstract
The onset and progression of non-alcoholic fatty liver disease (NAFLD) remains unclear, but short-chain fatty acids (SCFAs) in circulation may participate in its pathogenesis by acting as inflammation inhibitors. The aim of this retrospective study was to investigate plasma concentrations of general SCFAs in healthy individuals and in patients with distinct stages of NAFLD. Three main SCFAs (including acetate, propionate and butyrate) were analyzed by gas chromatography. The plasma TNF-α concentration was measured by ELISA. One-way ANOVA, Spearman's correlation and Pearson's correlation analysis were performed to estimate the associations between SCFAs, TNF-α and disease progression. Multiple linear stepwise regression was computed to explore the predictor variables of TNF-α in circulation. A total of 71 patients with NAFLD [including 27 patients with NAFL, 20 patients with non-alcoholic steatohepatitis (NASH) and 24 patients with NAFLD-related cirrhosis (NAFLD-cirrhosis)] and 9 healthy control (HC) subjects were enrolled for analysis. Although not statistically significant, plasma SCFAs were elevated in patients with NAFL compared with HC subjects, whereas the vast majority of SCFAs were statistically reduced in patients with NASH or NAFLD-cirrhosis compared with patients with NAFL. Plasma SCFAs had no significant differences in NASH or NAFLD-cirrhosis patients compared with HC subjects. In addition, significant negative correlations were observed between TNF-α and SCFAs. The progression of NAFLD (β=0.849; P<0.001) and the decline of the total three SCFA concentrations (β=-0.189; P<0.001) were recognized as independent risk variables related to the elevated peripheral TNF-α in the multiple linear stepwise regression model. Plasma SCFA concentrations may alter with the development of NAFLD and may have a potential link to TNF-α and the progression of NAFLD, which may serve a protective role toward disease advancement. Further mechanistic studies, such as analysis of gastrointestinal microecology, signaling pathways and functions involved in TNF-α, need to be performed. Also, therapeutic supplementation of SCFAs for NASH and NAFLD-cirrhosis needs further research and verification.
Keywords: gastrointestinal microbiome, short-chain fatty acids, non-alcoholic fatty liver disease, liver cirrhosis, TNF-α
Introduction
Non-alcoholic fatty liver disease (NAFLD), pathogenically reflected more accurately as metabolic-associated fatty liver disease (1,2), has been recognized as the most common chronic liver disease, affecting one-quarter of the population worldwide. While the general incidence of liver-related outcomes in NAFLD is only 0.97/1,000 person-years, the health burden of NAFLD remains heavy in consideration of its huge patient population (3). The spectrum of NAFLD ranges from simple NAFL to non-alcoholic steatohepatitis (NASH) to NAFLD-related cirrhosis (NAFLD-cirrhosis). NASH is characterized by histological hepatic steatosis, lobular inflammation and cell injury; NAFLD-cirrhosis (characterized by increased liver hardness, formation of pseudolobules and even increased portal vein pressure) has a relatively poor prognosis with higher risk for cardiovascular disease and hepatic cell cancer (4-6). Despite the rising prevalence of NAFLD, its onset and progression remains unclear; it is most likely to have multiple etiologies, intimately linked to metabolic abnormalities such as obesity, hypertension, dyslipidemia and type 2 diabetes (T2DM) (7). The widely accepted mechanisms include inflammation, oxidative stress, insulin resistance, dyslipidemia and obesity (8,9). A number of studies suggest that intestinal microbiota serve an important role in the development of NAFLD (10,11), which works through the regulation of gut barrier and liver inflammation response via Toll-like receptor (TLR)4 signaling (12), which enables the release of TNF-α and the activation of hepatic stellate cells (13).
As the metabolites of gut bacteria, short-chain fatty acids (SCFAs) are small molecular compounds with fewer than six carbon atoms; they are mainly produced from fermentation of dietary fibers by gut bacteria (14). The most abundant SCFAs are acetate, propionate and butyrate, which account for >90% of those present in the intestines (15); most (90-95%) SCFAs are absorbed in the colon. SCFAs not only provide energy for intestinal epithelium, but they also perform a number of biological functions, such as the regulation of immunity, lipometabolism and glycometabolism (16). As the liver is linked to the intestines through the hepatic portal circulation, gut-derived SCFAs will arrive to the liver first, and could be recognized as a type of signal molecule connecting gut dysbiosis to the development of NAFLD. In vitro and animal studies have previously demonstrated that SCFAs participate in nutrient absorption and insulin sensitivity through activating G-protein coupled receptors (GPCRs) (17,18). Furthermore, SCFAs may serve roles in suppressing the immune response and reducing liver inflammation through histone deacetylases (HDACs), and then downgrade the number of regulatory T cells (19). SCFAs also modulate the production of several inflammatory cytokines such as TNF-α, which is one of the terminal products of the TLR4 signal pathway, as well as the key to liver inflammation and fibrosis (enhancing the mRNA expression of tissue inhibitor of metalloproteinase 1 in activated hepatic stellate cells and suppressing apoptosis of hepatic stellate cells) (20).
Previous studies have reported the content alterations of SCFAs in feces in patients of NAFLD (21,22). However, clinical evidence of SCFAs associated with the severity of NAFLD remains inadequately documented in humans. To the best of our knowledge, no previous study has explored the association between plasma SCFAs and TNF-α. In this retrospective cross-sectional study, plasma concentrations of general SCFAs were measured in healthy control (HC) individuals and patients with NAFLD of distinct stages for a better understanding of the progression of NALFD. In addition, correlation analysis between plasma SCFAs and TNF-α in circulation was conducted. Multiple linear stepwise regression analysis was used to look for variables that affected TNF-α in circulation. This study may provide insight into the potential interplay of cytokines and microbial metabolites in the development of NAFLD.
Materials and methods
Ethics approval and consent to participate
This study was approved by the Ethics Committee of The Sixth People's Hospital of Chengdu (Chengdu, China; reference no. 2020-L-004; December 2, 2020) and conformed to the ethical guidelines of The Declaration of Helsinki (2000) of the World Medical Association. Written informed consent was obtained from all participants.
Patients
Finally, 71 patients with NAFLD and 9 HC volunteers who came to the hospital for routine health assessment were consecutively included between May 2018 and March 2019 at The Sixth People's Hospital of Chengdu (Chengdu, China). Study participants of both sexes were all >18 years old. All HC volunteers were individuals without evidence or history of liver or metabolic diseases. Patients with NAFLD met the diagnostic criteria for the Prevention and Treatment for Non-Alcoholic Fatty Liver Disease of the Chinese Society of Hepatology, Chinese Medical Association, updated in 2018(5). Patients with NASH (n=20) were screened out from normal NAFL (n=27) based on elevated transaminases [alanine transaminase (ALT) or aspartate transaminase (AST) >45 U/l] and abnormal medical images (inflammation or swelling of the liver according to color doppler ultrasound, computed tomography or magnetic resonance imaging). If there was any doubt about the stage of disease, a liver biopsy was performed by the clinical team, comprising a clinical doctor, a radiology expert and a pathology doctor, all of whom had >10 years of work experience in their respective fields. NAFLD-cirrhosis (n=24) was defined as the appearance of features in radiology or endoscopy [hepatatrophia, widened portal vein, varicose esophageal vein or liver stiffness measurement ≥15.0 kPa from Fibroscan (FibroScan®502 CAP™; Shenzhen Echosens Medical Equipment Co., Ltd.)] on the basis of NAFLD. All subjects with the following conditions were excluded from the study: Significant alcohol consumption (males, >30 g/day; females, >20 g/day), chronic hepatitis B or hepatitis C infection, autoimmune liver diseases, drug-induced liver disease, cancer, diabetes mellitus or any other disease associated with the liver, or if they had been treated with antibiotics or probiotics within the 6 months before inclusion. Written informed consent was obtained from each participant.
Blood sample collection and assay
For each patient, blood samples of 5 ml were collected in EDTA tubes for blood routine test using a CAL8000 blood analysis pipeline (Shenzhen Mindray Bio-medical Electronics Co., Ltd) and 5 ml blood samples were collected by common yellow tubes for blood biochemical assay using the Roche Cobas c702 Automatic Biochemical Analyzer (Roche Diagnostics). Another 10 ml of blood sample was collected using a heparin-coated anticoagulation tube for the detection of SCFAs and TNF-α. All blood samples were collected from the elbow vein one day following inclusion with overnight fasting for 12 h. Blood routine test and blood biochemical test were performed immediately after receiving the samples by the Clinical Laboratory Center of The Sixth People's Hospital of Chengdu. The samples for the detection of SCFAs and TNF-α were ultracentrifuged at 1,500 x g for 5-10˚C for 10 min for separating plasma and immediately stored at -20˚C and detected within 7 days. The plasma concentrations of the three main SCFAs (acetate, propionate and butyrate) were measured using an Agilent 8890B-5977B gas chromatograph (Shanghai Majorbio Bio-Pharm Technology Co., Ltd.). The concentration of plasma TNF-α was measured by the Clinical Laboratory Center of The Sixth People's Hospital of Chengdu (Chengdu, China) using ELISA, with a testing kit (cat. no. M-KMLJ61715; Nanjing Camilo Biological Engineering Co., Ltd). The fibrosis-4 (FIB-4) index was the square root of [age (years) x AST (U/l)]/[platelet count (109/l) x ALT (U/l)].
Statistical analysis
All statistical analyses were performed using SPSS statistical software (version 22.0; IBM Corp). All data corresponded to a normal or approximate normal distribution, which was checked by the Kolmogorov-Smirnov test, and all data were expressed as the mean ± standard error of the mean. Qualitative variables were compared using χ2 test or Fisher's exact test. Comparisons between quantitative variables were made using one-way ANOVA; Bonferroni's post-hoc test was performed for multiple comparisons. Spearman's analysis and Pearson's correlation analysis were used to estimate the correlations between SCFAs and TNF-α. A multiple linear stepwise regression model was computed to investigate predictor variables that had a significant influence on TNF-α in the circulation. P<0.05 was considered to indicate a statistically significant difference.
Results
Recruitment of participants
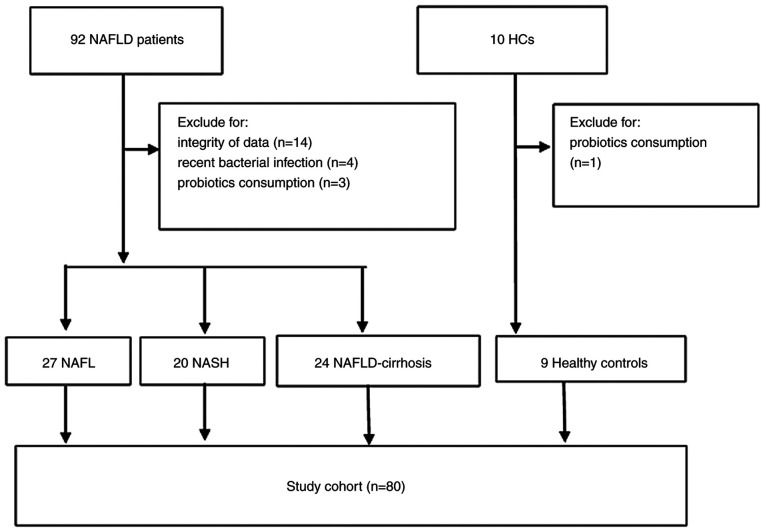
The medical records of 92 patients with NAFLD and 10 HC volunteers were reviewed. In total, 22 patients were excluded from the study due to lacking complete data (n=14 NAFLD), history of recent bacterial infection (n=4 NAFLD) or consumption of probiotics (n=3 NAFLD; n=1 HC). Finally, 71 patients with NAFLD (including 27 patients with NAFL, 20 patients with NASH and 24 patients with NAFLD-cirrhosis) and 9 HCs were included in this retrospective study for analysis. A total of 11 patients underwent liver biopsy for the diagnosis of NASH. An overview of the study participants is depicted in Fig. 1.
Figure 1.
Flow diagram of the study showing the inclusion and exclusion of participants with NAFLD and HCs. HCs, healthy controls; NAFLD, non-alcoholic fatty liver disease; NAFLD-cirrhosis, NAFLD-related cirrhosis; NASH, non-alcoholic steatohepatitis.
Baseline characteristics of the study cohort
The baseline characteristics of the 80 participants were summarized in Table I. The mean age of the whole study population was 49.98±9.46 years and 43.75% of the participants were males. The four groups were comparable in terms of age and sex. Patients with NAFL, NASH and NAFLD-cirrhosis were more likely to be obese compared with the HC group (P<0.001); they were also more likely to have T2DM, hypertension or dyslipidemia compared with the HC group, though not statistically significant. The concentrations of ALT, AST and alkaline phosphatase, FIB-4 index and TNF-α were significantly elevated in the NASH and NAFLD-cirrhosis groups compared with the HC and NAFL groups (P<0.05).
Table I.
Baseline characteristics of the patient cohort.
| Characteristic | HC (n=9) | NAFL (n=27) | NASH (n=20) | NAFLD-cirrhosis (n=24) |
|---|---|---|---|---|
| Age, years | 53.78±6.96 | 47.56±10.01 | 52.50±9.76 | 49.17±8.91 |
| Male sex | 4 (44.44) | 12 (44.44) | 11 (55.00) | 8 (33.33) |
| BMI, kg/m2 | 22.46±1.76 | 27.40±3.17a | 28.81±3.34a | 28.29±2.47a |
| T2DM | 0 (0.00) | 5 (18.52) | 4 (20.00) | 6 (25.00) |
| Hypertension | 0 (0.00) | 4 (14.81) | 3 (15.00) | 4 (16.67) |
| Dyslipidemia | 0 (0.00) | 9 (33.33) | 7 (35.00) | 8 (33.33) |
| ALT, U/l | 26.89±9.35 | 38.04±12.06 | 108.35±40.99a,b | 59.71±30.38c,d |
| AST, U/l | 24.22±7.41 | 30.00±7.71 | 67.70±29.85a,b | 58.63±23.26a,b |
| ALP, U/l | 55.00±17.08 | 61.11±17.81 | 118.50±65.09b,e | 135.79±55.87a,b |
| FIB-4 index | 1.11±0.43 | 1.57±0.69 | 2.63±0.72a,b | 3.36±0.59a,b |
| TNF-α, pg/ml | 0.050±0.011 | 0.062±0.035 | 0.158±0.032a,b | 0.251±0.022a,b |
aP<0.001 vs. HC;
bP<0.001 vs. NAFL;
cP<0.05 vs. HC;
dP<0.05 vs. NAFL; and
eP<0.01 vs. HC. Values are expressed as the mean ± standard error of the mean or n (%). ALP, alkaline phosphatase; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BMI, body mass index; FIB-4, fibrosis-4; HC, healthy control; NAFLD, non-alcoholic fatty liver disease; NASH, non-alcoholic steatohepatitis; NAFLD-cirrhosis, NAFLD-related cirrhosis; T2DM, type 2 diabetes mellitus.
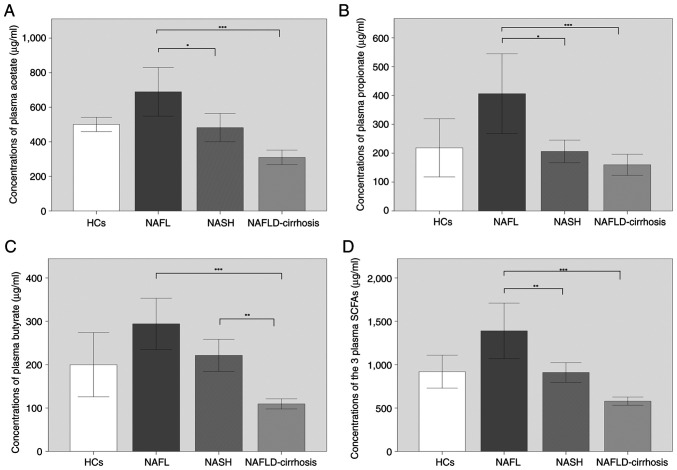
Plasma SCFA levels vary with the development of NAFLD
Comparisons of the plasma concentrations of acetate, propionate, butyrate and the sum of the three were displayed in Fig. 2. Although not statistically significant, acetate, propionate, butyrate and the combined SCFA levels were increased in patients with NAFL compared with those in the HCs. The concentrations of acetate, propionate, butyrate and the total three SCFAs were significantly decreased in NAFLD-cirrhosis compared with NAFL (P<0.001; Fig. 2A-D). The concentrations of acetate (P<0.05), propionate (P<0.05) and the total three SCFAs (P<0.01) in NASH were significantly decreased compared with those in NAFL (Fig. 2A, B and D). Although not statistically significant, the concentration of butyrate in the patients with NASH was lower compared with that of the patients with NAFL (Fig. 2C). In addition, the concentration of butyrate was significantly lower in patients with NAFLD-cirrhosis compared with that in patients with NASH (P<0.01; Fig. 2C); the concentrations of acetate, propionate and total SCFAs were also lower in patients with NAFLD-cirrhosis compared with those in patients with NASH, but no significant differences were identified (Fig. 2A, B and D).
Figure 2.
Comparison of the plasma concentrations of acetate, propionate, butyrate and the total of the three SCFAs in patients with NAFL, NASH and NALFD-cirrhosis and participants with HCs. (A) Concentrations of acetate in HCs (500.59±53.48 µg/ml), and in patients with NAFL (689.28±355.86 µg/ml), NASH (482.13±174.61 µg/ml) and NAFLD-cirrhosis (309.93±99.83 µg/ml). (B) Concentrations of propionate in HCs (218.76±131.06 µg/ml) and in patients with NAFL (406.24±349.64 µg/ml), NASH (206.16±83.86 µg/ml) and NAFLD-cirrhosis (159.99±86.42 µg/ml). (C) Concentrations of butyrate in HCs (199.91±96.30 µg/ml) and in patients with NAFL (294.13±149.36 µg/ml), NASH (221.39±79.06 µg/ml) and NAFLD-cirrhosis (109.52±124.65 µg/ml). (D) Concentrations of the total three SCFAs in HCs (919.27±247.06 µg/ml) and in patients with NAFL (1,389.64±809.15 µg/ml), NASH (909.68±243.02 µg/ml) and NAFLD-cirrhosis (579.44±112.09 µg/ml). *P<0.05, **P<0.01 and ***P<0.001. HCs, healthy controls; NAFLD, non-alcoholic fatty liver disease; NAFLD-cirrhosis, NAFLD-related cirrhosis; NASH, non-alcoholic steatohepatitis; SCFAs, short-chain fatty acids.
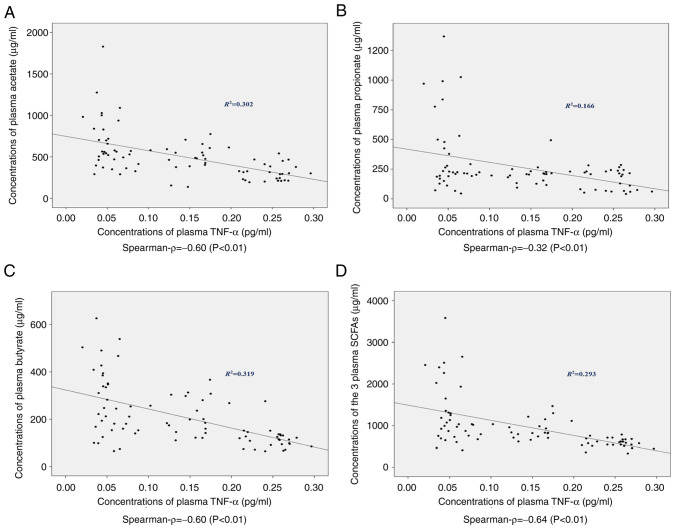
Concentrations of plasma SCFAs are negatively correlated with peripheral TNF-α plasma concentration
The concentrations of plasma TNF-α in the different groups are presented in Table I. The levels of TNF-α were comparable in HCs and patients with NAFL (P=0.268), whereas the levels were significantly increased in NASH and NAFLD-cirrhosis patients compared with the other two groups (P<0.001). The associations between plasma SCFAs and peripheral TNF-α were analyzed. Significant negative correlations were observed between the concentrations of TNF-α and acetate (R2=0.302; ρ=-0.60; P<0.01), propionate (R2=0.166; ρ=-0.32; P<0.01), butyrate (R2=0.319; ρ=-0.60; P<0.01) and the total three SCFAs (R2=0.293; ρ=-0.64; P<0.01) in this study (Fig. 3).
Figure 3.
Correlations between plasma SCFA and TNF-α concentrations. Negative correlations were identified between TNF-α levels and (A) acetate, (B) propionate, (C) butyrate and (D) the total three SCFAs. SCFAs, short-chain fatty acids.
NAFLD progression and the reduction in the total level of the three SCFAs are independent variables to predict elevated TNF-α in circulation
A multiple linear stepwise regression model was computed to investigate predictor variables that may have a significant influence on the level of plasma TNF-α concentration (Table II). Age, sex, NAFLD stage, BMI, T2DM, hypertension, dyslipidemia, elevated aminotransferases, FIB-4, acetate, propionate, butyrate and the total three SCFAs were entered into the regression model. The model was statistically significant, with adjusted R2=0.871, F (3,76)=178.998 and P<0.001. NAFLD stage, T2DM and the total three SCFAs fitted well. TNF-α was calculated as follows: TNF-α=-0.028 + (0.073 x NAFLD stage)-(0.017 x T2DM)-(0.0001 x the total three SCFAs). The NAFLD stage was observed to have a significantly positive impact on the concentration of plasma TNF-α (β=0.849; P<0.001), whereas the total three SCFAs had significantly negative influence (β=-0.189; P<0.001). Therefore, the development of NAFLD and the decline of the total SCFAs in plasma were recognized as independent risk factors associated with the elevated TNF-α level in circulation.
Table II.
Multiple linear stepwise regression analysis for prediction the independent risk variables of plasma TNF-α.
| TNF-α concentration | ||||||
|---|---|---|---|---|---|---|
| Variable | Unstandardized β | SE (β) | Standardized β | P-value | VIF | 95% CI |
| Constant | -0.028 | 0.015 | - | 0.06 | - | -0.057-0.001 |
| Age | 0.000 | 0.000 | 0.050 | 0.285 | 1.249 | -0.000-0.001 |
| Sex | 0.004 | 0.008 | 0.023 | 0.598 | 1.104 | -0.011-0.019 |
| BMI | -0.001 | 0.001 | 0.911 | 0.548 | 1.505 | -0.003-0.002 |
| NAFLD stage | 0.073 | 0.004 | 0.849 | <0.001 | 1.241 | 0.066-0.081 |
| T2DM | -0.017 | 0.009 | -0.076 | 0.068 | 1.026 | -0.035-0.001 |
| Hypertension | -0.001 | 0.011 | -0.004 | 0.933 | 1.100 | -0.022-0.021 |
| Dyslipidemia | -0.006 | 0.008 | -0.034 | 0.453 | 1.157 | -0.023-0.010 |
| Acetate | -0.000 | 0.000 | -0.108 | 0.156 | 3.328 | -0.000-0.000 |
| Propionate | -0.000 | 0.000 | -0.035 | 0.662 | 3.786 | -0.000-0.000 |
| Butyrate | -0.000 | 0.000 | -0.058 | 0.458 | 3.485 | -0.000-0.000 |
| Total main SCFAs | -0.0001 | 0.000 | -0.189 | <0.001 | 1.212 | -0.000-0.000 |
| Elevated aminotransferases | -0.013 | 0.010 | -0.072 | 0.214 | 1.931 | -0.032-0.007 |
| FIB-4 | -0.000 | 0.006 | -0.003 | 0.965 | 3.397 | -0.013-0.012 |
BMI, body mass index; NAFLD, non-alcoholic fatty liver disease; T2DM, type 2 diabetes mellitus; SCFA, short-chain fatty acid; FIB-4, fibrosis-4; β, regression coefficient; SE, standardized error; VIF, variance inflation factor; CI, confidence interval.
Discussion
In the present study, plasma concentrations of SCFAs and TNF-α, a key product of the TLR4 signaling pathway in liver inflammation, were analyzed in 71 patients with NAFLD and 9 HC patients. Although not statistically significant, plasma SCFA levels were elevated in patients with NAFL compared with those in HCs, and plasma SCFAs were reduced in NASH and NAFLD-cirrhosis patients compared with those in patients with NAFL. In addition, the decrease in SCFAs was negatively related to the elevated TNF-α in plasma, particularly acetate and butyrate. The progression of NAFLD and the decline in total SCFA levels were identified as independent risk variables associated with the elevation of TNF-α in circulation.
Currently, there is still no established and effective medical treatment for NAFLD. Recent evidence suggested that supplementation of dietary fibers was beneficial to the metabolism of patients with NAFLD (23). As the main products of dietary fibers in the bowel, SCFAs participate in the development of NAFLD through several ways. For example, in the intestinal cavity, SCFAs stimulate secretions of peptide YY and the gut-derived hormone glucagon-like peptide 1 (GLP-1) through GPCR41 and GPCR43(18). Peptide YY slows intestinal transport and increases satiety. GLP-1 promotes the development of NAFLD by regulating fatty acid oxidation and insulin sensitivity (24). In the circulation, SCFAs directly regulate liver metabolism. For example, they affect the expression of peroxisome proliferator-activated receptor α target genes through AMP-activated protein kinase (AMPK) phosphorylation, which reduces free fatty acid (FFA) from adipose tissue to the liver (25,26). Previous studies showed that a rectal infusion of acetate and propionate achieved 40% reduction in serum FFA levels (27). It was reported that serum FFA contributed 60% of fatty acids to the newly synthesized triglyceride in the liver (28). However, the role of SCFAs in the development of NAFLD remains controversial. One published study reported higher concentrations of fecal SCFAs in patients with NAFL compared with those in HCs owing to the predominance of SCFA-producing families and bacterium, such as Bifidobacterium bifidum, Butyrivibrio, Megasphaera and Prevotella (29); another study suggested that the reduction in plasma SCFAs was associated with more advanced liver fibrosis or cirrhosis (30). Therefore, it is necessary to investigate SCFA levels in blood and stool with regard to the changes along the NAFLD spectrum. The present study found that the plasma levels of acetate, propionate, butyrate and the total of the three SCFAs combined were increased in patients with NAFL compared with those in HCs, although this result was not statistically significant, whereas the levels were significantly decreased in patients with NAFLD-cirrhosis compared with NAFL. The levels were also significantly lower in patients with NASH compared with NAFL, except for butyrate; however, the concentration of butyrate in patients with NAFLD-cirrhosis was lower compared with that in patients with NASH. Taken together, these data suggest that the plasma levels of SCFAs may increase in early stage NAFLD (although this requires further verification), and the concentrations subsequently decrease in the advanced stages of NAFLD. One explanation hypothesized by us is that SCFAs may serve a protective role and a phenomenon like ‘decompensation’ happens when inflammation and fibrosis occur. Another explanation is that SCFAs vary with the change of SCFA-producing microbiota in the intestine. As aforementioned, patients with NAFL are characterized with a higher abundance of SCFA-producing bacterium. For example, Blautia obeum may be the most reliable biological marker for the differentiation between mild NASH and NAFLD (31). The populations of main SCFA-producing bacterial phyla, such as Firmicutes and Bacteroidetes, are significantly reduced in the advanced stages of cirrhosis (30). It may be cautiously hypothesized that the alteration of intestinal microflora with the development of NAFLD may be another manifestation of the ‘two hits’ or ‘multiple hits’ theory, according to which lipotoxicity of adipose tissue, gut microbiome, microbiota-related metabolites, dietary components and genetic pathways evolved as crucial factors in the pathogenesis of NAFLD (32). The present results obtained with the specimens of human subjects suggested that maintaining plasma SCFA levels may be beneficial for advanced NAFLD, such as NASH and NAFLD-cirrhosis, but not for NAFL.
It is well documented that macrophages serve a major role in inflammatory responses in the pathology of NASH and NAFLD-related cirrhosis (33,34). TNF-α is one of the most important pro-inflammatory cytokines secreted by macrophages. Pathogen- or damage-associated molecular substances, e.g., lipopolysaccharide (LPS), stimulate the canonical NF-κB signaling pathway by binding TLR4(35). NF-κB activation induces the transcription of a variety of inflammatory cytokines and chemokines, including TNF-α. TNF-α may then act as a mediator of hepatotoxicity, inflammation and NAFLD development. Once produced, TNF-α enhances the mRNA expression levels of tissue inhibitor of metalloproteinase 1 in activated hepatic stellate cells and suppresses the induction of apoptosis, and then promotes the process of hepatocyte injury (36). Increased TNF-α expression and that of its receptors have been reported in patients with NASH (37). Notably, high basal TNF-α levels could be a risk factor of developing NAFLD, even in healthy individuals (38). A number of previous studies have identified TNF-α as a predictor of NASH and liver cirrhosis (20,36,38). As SCFAs act as inflammation inhibitors in respiratory infections and in kidney injury (39,40), it may be assumed that SCFAs may induce a similar anti-inflammatory effect in NAFLD.
Results from the present study demonstrated that the level of TNF-α was increased with NAFLD progression, which was consistent with the aforementioned previous studies. In addition, significant negative correlations between SCFAs and TNF-α were identified and supported by multiple linear stepwise regression model calculations, with an adjusted R2=0.871, which means that an 87.1% change of TNF-α in circulation may be explained by variables in this model. Rather than age, sex, BMI, metabolic disorders, abnormal liver function, FIB-4 or any single SCFA alone, the progression of NAFLD and decreased total SCFA concentration in the blood were recognized as independent risk factors associated with the elevation of TNF-α in circulation. However, the correlation coefficients between TNF-α and acetate, propionate and butyrate were not the same, ρ was -0.60, -0.32 and -0.60, respectively. It may be hypothesized that this apparent discrepancy arises from that acetate and butyrate are incorporated in lipid metabolism, whereas propionate is mainly involved in gluconeogenesis (26). For instance, acetate increases the expression of genes for fatty acid oxidation by activating AMPK (26). Butyrate, on the one hand, suppresses the immune response and reduces liver inflammation through HDACs; on the other hand, it also ameliorates liver inflammation by promoting the expression of tight junction protein in the colon (41). The correlation results between SCFAs and TNF-α from the present study were also consistent with recent findings in studies using animals. For example, oral supplementation of acetate decreased macrophage aggregation and TNF-α level in methionine- and choline-deficient diet-induced NASH mice (42). Treatment with butyrate for 6 weeks reduced hepatic injury by downregulation of TNF-α in mice with NASH (41). In addition, the differences between the correlation coefficients in the present study may help us search for more representative biological markers of NAFLD. On the whole, the putative protective affection of SCFAs may be achieved through alleviating inflammation, in which TNF-α serves a role.
There are several limitations to the present study. First, the study was cross-sectional research and it was limited by sample size. Continuous investigations were lacking and baseline data of participants may have been confounded by the patients' condition at the time of enrollment. It might thus be difficult to distinguish cause from effect. However, considering the relatively large number of risk factors and the good stability of the regression model, the research results were still worthy of attention. Second, owing to the retrospective nature of the study, dietary composition and microbiome analysis were not performed, and additional samples (such as blood, stool, liver tissue and intestinal tissue) could not be obtained for further investigation. Therefore, further investigations are required, which may include a prospective exploration of the intestinal flora, tight junction proteins and their associations with SCFAs at different stages of NAFLD. In addition, the concentration of LPS in blood and the association between LPS and SCFAs can be investigated. As NAFLD progresses, downregulated SCFA levels may increase the concentration of LPS in the blood due to damage to the intestinal barrier and production of more gram-negative bacteria. The expression levels of TLR-4 and NK-κB in liver can also be examined, as LPS may activate hepatic stellate cells by TLR-4, and thus promote the release of inflammatory factors, such as TNF-α, through the NF-κB signaling pathway. Furthermore, hepatocyte apoptosis and production of reactive oxygen species can be investigated, which may be associated with the functions of TNF-α in NAFLD progression (35,36,43-45). Finally, in the present study, elevated serum transaminases and abnormal medical images were used for the diagnosis of NASH (details were provided in the methods section), but not all patients underwent liver biopsy to confirm the diagnosis of NASH due to invasive examination.
The present study revealed variations in plasma SCFA concentrations within the spectrum of NAFLD, as well as significant negative correlations between SCFAs and peripheral TNF-α, which may be beneficial for a better understanding of the pathogenesis of NAFLD. The results may provide a glimpse into the potential links between intestinal microecology, inflammatory response and the development of NAFLD. In addition, they may provide a new way to explore disease pathogenesis in terms of disease spectrum. Further research is needed, such as analysis of the intestinal microecology, signaling pathways and functions involved in TNF-α. Additional SCFA supplementation for NASH and NAFLD-cirrhosis may serve as a potential therapeutic strategy, which needs further research and verification.
Acknowledgements
Not applicable.
Funding Statement
Funding: This study was supported by The Chinese Foundation for Hepatitis Prevention and Control (grant no. TQGB20180125).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
QX and JX designed and performed the study together, and they are responsible for data analysis, writing and revising the paper. QX, JX, YL and TZ are responsible for data collection and detection of samples. XC and ZJZ were responsible for data analysis, interpretation of the data, obtaining ethics approval and confirming the authenticity of all the raw data. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of The Sixth People's Hospital of Chengdu (Chengdu, China; reference no. 2020-L-004; December 2, 2020). Written informed consent was obtained from all participants for the use of their samples for detection and publication of their relevant data.
Patient consent for publication
All participants in this study provided written informed consent for the use of their samples and publication of their data.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Eslam M, Sanyal AJ, George J. MAFLD: A consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology. 2020;158:1999–2014.e1. doi: 10.1053/j.gastro.2019.11.312. International Consensus Panel. [DOI] [PubMed] [Google Scholar]
- 2.Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, Zelber-Sagi S, Wai-Sun Wong V, Dufour JF, Schattenberg JM, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020;73:202–209. doi: 10.1016/j.jhep.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 3.Männistö VT, Salomaa V, Färkkilä M, Jula A, Männistö S, Erlund I, Sundvall J, Lundqvist A, Perola M, Åberg F. Incidence of liver-related morbidity and mortality in a population cohort of non-alcoholic fatty liver disease. Liver Int. 2021;41:2590–2600. doi: 10.1111/liv.15004. [DOI] [PubMed] [Google Scholar]
- 4.Calzadilla Bertot L, Adams LA. The natural course of non-alcoholic fatty liver disease. Int J Mol Sci. 2016;17(774) doi: 10.3390/ijms17050774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guidelines of prevention and treatment for nonalcoholic fatty liver disease: A 2018 update. Zhonghua Gan Zang Bing Za Zhi. 2018;26:195–203. doi: 10.3760/cma.j.issn.1007-3418.2018.03.008. National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association; Fatty Liver Expert Committee, Chinese Medical Doctor Association. (In Chinese) [DOI] [PubMed] [Google Scholar]
- 6.Li B, Zhang C, Zhan YT. Nonalcoholic fatty liver disease cirrhosis: A review of its epidemiology, risk factors, clinical presentation, diagnosis, management, and prognosis. Can J Gastroenterol Hepatol. 2018;2018(2784537) doi: 10.1155/2018/2784537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cobbina E, Akhlaghi F. Non-alcoholic fatty liver disease (NAFLD)-pathogenesis, classification, and effect on drug metabolizing enzymes and transporters. Drug Metab Rev. 2017;49:197–211. doi: 10.1080/03602532.2017.1293683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sangouni AA, Ghavamzadeh S. A review of synbiotic efficacy in non-alcoholic fatty liver disease as a therapeutic approach. Diabetes Metab Syndr. 2019;13:2917–2922. doi: 10.1016/j.dsx.2019.07.063. [DOI] [PubMed] [Google Scholar]
- 9.Tarantino G, Citro V, Capone D. Nonalcoholic fatty liver disease: A challenge from mechanisms to therapy. J Clin Med. 2019;9(15) doi: 10.3390/jcm9010015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Safari Z, Gérard P. The links between the gut microbiome and non-alcoholic fatty liver disease (NAFLD) Cell Mol Life Sci. 2019;76:1541–1558. doi: 10.1007/s00018-019-03011-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Astbury S, Atallah E, Vijay A, Aithal GP, Grove JI, Valdes AM. Lower gut microbiome diversity and higher abundance of proinflammatory genus Collinsella are associated with biopsy-proven nonalcoholic steatohepatitis. Gut Microbes. 2020;11:569–580. doi: 10.1080/19490976.2019.1681861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miura K, Ohnishi H. Role of gut microbiota and Toll-like receptors in nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20:7381–7391. doi: 10.3748/wjg.v20.i23.7381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Csak T, Ganz M, Pespisa J, Kodys K, Dolganiuc A, Szabo G. Fatty acid and endotoxin activate inflammasomes in mouse hepatocytes that release danger signals to stimulate immune cells. Hepatology. 2011;54:133–144. doi: 10.1002/hep.24341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Silva YP, Bernardi A, Frozza RL. The role of short-chain fatty acids from gut microbiota in gut-brain communication. Front Endocrinol (Lausanne) 2020;11(25) doi: 10.3389/fendo.2020.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan JC, Kioh DY, Yap GC, Lee BW, Chan EC. A novel LCMSMS method for quantitative measurement of short-chain fatty acids in human stool derivatized with 12C- and 13C-labelled aniline. J Pharm Biomed Anal. 2017;138:43–53. doi: 10.1016/j.jpba.2017.01.044. [DOI] [PubMed] [Google Scholar]
- 16.Canfora EE, Meex RCR, Venema K, Blaak EE. Gut microbial metabolites in obesity, NAFLD and T2DM. Nat Rev Endocrinol. 2019;15:261–273. doi: 10.1038/s41574-019-0156-z. [DOI] [PubMed] [Google Scholar]
- 17.Koh A, De Vadder F, Kovatcheva-Datchary P, Bäckhed F. From dietary fiber to host physiology: Short-chain fatty acids as key bacterial metabolites. Cell. 2016;165:1332–1345. doi: 10.1016/j.cell.2016.05.041. [DOI] [PubMed] [Google Scholar]
- 18.Aragonès G, González-García S, Aguilar C, Richart C, Auguet T. Gut microbiota-derived mediators as potential markers in nonalcoholic fatty liver disease. Biomed Res Int. 2019;2019(8507583) doi: 10.1155/2019/8507583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schilderink R, Verseijden C, de Jonge WJ. Dietary inhibitors of histone deacetylases in intestinal immunity and homeostasis. Front Immunol. 2013;4(226) doi: 10.3389/fimmu.2013.00226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stojsavljević S, Gomerčić Palčić M, Virović Jukić L, Smirčić Duvnjak L, Duvnjak M. Adipokines and proinflammatory cytokines, the key mediators in the pathogenesis of nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20:18070–18091. doi: 10.3748/wjg.v20.i48.18070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Michail S, Lin M, Frey MR, Fanter R, Paliy O, Hilbush B, Reo NV. Altered gut microbial energy and metabolism in children with non-alcoholic fatty liver disease. FEMS Microbiol Ecol. 2015;91:1–9. doi: 10.1093/femsec/fiu002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rau M, Rehman A, Dittrich M, Groen AK, Hermanns HM, Seyfried F, Beyersdorf N, Dandekar T, Rosenstiel P, Geier A. Fecal SCFAs and SCFA-producing bacteria in gut microbiome of human NAFLD as a putative link to systemic T-cell activation and advanced disease. United European Gastroenterol J. 2018;6:1496–1507. doi: 10.1177/2050640618804444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kundi ZM, Lee JC, Pihlajamäki J, Chan CB, Leung KS, So SSY, Nordlund E, Kolehmainen M, El-Nezami H. Dietary fiber from oat and rye brans ameliorate western diet-induced body weight gain and hepatic inflammation by the modulation of short-chain fatty acids, bile acids, and tryptophan metabolism. Mol Nutr Food Res. 2021;65(e1900580) doi: 10.1002/mnfr.201900580. [DOI] [PubMed] [Google Scholar]
- 24.Svegliati-Baroni G, Saccomanno S, Rychlicki C, Agostinelli L, De Minicis S, Candelaresi C, Faraci G, Pacetti D, Vivarelli M, Nicolini D, et al. Glucagon-like peptide-1 receptor activation stimulates hepatic lipid oxidation and restores hepatic signalling alteration induced by a high-fat diet in nonalcoholic steatohepatitis. Liver Int. 2011;31:1285–1297. doi: 10.1111/j.1478-3231.2011.02462.x. [DOI] [PubMed] [Google Scholar]
- 25.He J, Zhang P, Shen L, Niu L, Tan Y, Chen L, Zhao Y, Bai L, Hao X, Li X, et al. Short-Chain fatty acids and their association with signalling pathways in inflammation, glucose and lipid metabolism. Int J Mol Sci. 2020;21(6356) doi: 10.3390/ijms21176356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.den Besten G, Bleeker A, Gerding A, van Eunen K, Havinga R, van Dijk TH, Oosterveer MH, Jonker JW, Groen AK, Reijngoud DJ, Bakker BM. Short-Chain fatty acids protect against high-fat diet-induced obesity via a PPARγ-Dependent switch from lipogenesis to fat oxidation. Diabetes. 2015;64:2398–2408. doi: 10.2337/db14-1213. [DOI] [PubMed] [Google Scholar]
- 27.Donnelly KL, Smith CI, Schwarzenberg SJ, Jessurun J, Boldt MD, Parks EJ. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J Clin Invest. 2005;115:1343–1351. doi: 10.1172/JCI23621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolever TM, Brighenti F, Royall D, Jenkins AL, Jenkins DJ. Effect of rectal infusion of short chain fatty acids in human subjects. Am J Gastroenterol. 1989;84:1027–1033. [PubMed] [Google Scholar]
- 29.de la Cuesta-Zuluaga J, Mueller NT, Corrales-Agudelo V, Velásquez-Mejía EP, Carmona JA, Abad JM, Escobar JS. Metformin is associated with higher relative abundance of mucin-degrading akkermansia muciniphila and several short-chain fatty acid-producing microbiota in the gut. Diabetes Care. 2017;40:54–62. doi: 10.2337/dc16-1324. [DOI] [PubMed] [Google Scholar]
- 30.Juanola O, Ferrusquía-Acosta J, García-Villalba R, Zapater P, Magaz M, Marín A, Olivas P, Baiges A, Bellot P, Turon F, et al. Circulating levels of butyrate are inversely related to portal hypertension, endotoxemia, and systemic inflammation in patients with cirrhosis. FASEB J. 2019;33:11595–11605. doi: 10.1096/fj.201901327R. [DOI] [PubMed] [Google Scholar]
- 31.Aoki R, Onuki M, Hattori K, Ito M, Yamada T, Kamikado K, Kim YG, Nakamoto N, Kimura I, Clarke JM, et al. Commensal microbe-derived acetate suppresses NAFLD/NASH development via hepatic FFAR2 signalling in mice. Microbiome. 2021;9(188) doi: 10.1186/s40168-021-01125-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tilg H, Adolph TE, Moschen AR. Multiple parallel hits hypothesis in nonalcoholic fatty liver disease: Revisited after a decade. Hepatology. 2021;73:833–842. doi: 10.1002/hep.31518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mridha AR, Wree A, Robertson AAB, Yeh MM, Johnson CD, Van Rooyen DM, Haczeyni F, Teoh NC, Savard C, Ioannou GN, et al. NLRP3 inflammasome blockade reduces liver inflammation and fibrosis in experimental NASH in mice. J Hepatol. 2017;66:1037–1046. doi: 10.1016/j.jhep.2017.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alisi A, Carpino G, Oliveira FL, Panera N, Nobili V, Gaudio E. The role of tissue macrophage-mediated inflammation on NAFLD pathogenesis and its clinical implications. Mediators Inflamm. 2017;2017(8162421) doi: 10.1155/2017/8162421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Robinson SM, Mann DA. Role of nuclear factor kappa B in liver health and disease. Clin Sci (Lond) 2010;118:691–705. doi: 10.1042/CS20090549. [DOI] [PubMed] [Google Scholar]
- 36.Tomita K, Tamiya G, Ando S, Ohsumi K, Chiyo T, Mizutani A, Kitamura N, Toda K, Kaneko T, Horie Y, et al. Tumour necrosis factor alpha signalling through activation of Kupffer cells plays an essential role in liver fibrosis of non-alcoholic steatohepatitis in mice. Gut. 2006;55:415–424. doi: 10.1136/gut.2005.071118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alaaeddine N, Sidaoui J, Hilal G, Serhal R, Abedelrahman A, Khoury S. TNF-α messenger ribonucleic acid (mRNA) in patients with nonalcoholic steatohepatitis. Eur Cytokine Netw. 2012;23:107–111. doi: 10.1684/ecn.2012.0313. [DOI] [PubMed] [Google Scholar]
- 38.Seo YY, Cho YK, Bae JC, Seo MH, Park SE, Rhee EJ, Park CY, Oh KW, Park SW, Lee WY. Tumor necrosis factor-α as a predictor for the development of nonalcoholic fatty liver disease: A 4-year follow-up study. Endocrinol Metab (Seoul) 2013;28:41–45. doi: 10.3803/EnM.2013.28.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Machado MG, Sencio V, Trottein F. Short-chain fatty acids as a potential treatment for infections: A closer look at the lungs. Infect Immun. 2021;89(e0018821) doi: 10.1128/IAI.00188-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang S, Lv D, Jiang S, Jiang J, Liang M, Hou F, Chen Y. Quantitative reduction in short chain fatty acids, especially butyrate, contributes to the progression of chronic kidney disease. Clin Sci (Lond) 2019;133:1857–1870. doi: 10.1042/CS20190171. [DOI] [PubMed] [Google Scholar]
- 41.Yang T, Yang H, Heng C, Wang H, Chen S, Hu Y, Jiang Z, Yu Q, Wang Z, Qian S, et al. Amelioration of non-alcoholic fatty liver disease by sodium butyrate is linked to the modulation of intestinal tight junctions in db/db mice. Food Funct. 2020;11:10675–10689. doi: 10.1039/d0fo01954b. [DOI] [PubMed] [Google Scholar]
- 42.Deng M, Qu F, Chen L, Liu C, Zhang M, Ren F, Guo H, Zhang H, Ge S, Wu C, Zhao L. SCFAs alleviated steatosis and inflammation in mice with NASH induced by MCD. J Endocrinol. 2020;245:425–437. doi: 10.1530/JOE-20-0018. [DOI] [PubMed] [Google Scholar]
- 43.Liedtke C, Trautwein C. The role of TNF and Fas dependent signaling in animal models of inflammatory liver injury and liver cancer. Eur J Cell Biol. 2012;91:582–589. doi: 10.1016/j.ejcb.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 44.Li KZ, Liao ZY, Li YX, Ming ZY, Zhong JH, Wu GB, Huang S, Zhao YN. A20 rescues hepatocytes from apoptosis through the NF-κB signaling pathway in rats with acute liver failure. Biosci Rep. 2019;39(BSR20180316) doi: 10.1042/BSR20180316. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 45.García-Ruiz I, Rodríguez-Juan C, Díaz-Sanjuan T, del Hoyo P, Colina F, Muñoz-Yagüe T, Solís-Herruzo JA. Uric acid and anti-TNF antibody improve mitochondrial dysfunction in ob/ob mice. Hepatology. 2006;44:581–591. doi: 10.1002/hep.21313. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.