Abstract
Background:
McKesson’s InterQual criteria are widely used in hospitals to determine if patients should be classified as observation or inpatient status, but the accuracy of criteria is unknown.
Objectives:
We sought to determine whether InterQual criteria accurately predicted length of stay in older patients with syncope.
Methods:
We conducted a secondary analysis of a cohort study of adults ≥60 years with syncope. We calculated InterQual criteria and classified the patient as observation or inpatient status. Outcomes were whether LOS were less than or greater than two midnights.
Results:
We analyzed 2361 patients and 1,227 (52.0%) patients were male and 1,945 (82.8%) were white, with a mean age of 73.2 +/− 9.0 years. The median LOS was 32.6 hours (IQR 24.2–71.8). The sensitivity of InterQual criteria for LOS was 60.8% (95% CI 57.9–63.6%); specificity 47.8% (95% CI 45.0–50.5%).
Conclusion:
In older adults with syncope, those who met InterQual criteria for inpatient status had longer LOS compared to those who did not; however, the accuracy of the criteria to predict length of stay over 2 days is poor, with sensitivity of 60% and sensitivity of 48%. Future research should identify criteria to improve LOS prediction.
Keywords: syncope, geriatrics, interqual, case management
Introduction:
Observation care has grown as an alternative to “short-stay” inpatient admissions since the 1980s.1,2 Observation status is on the rise: between 2007 and 2012, observation stays for short-term acute care treatment and assessment grew by 57% among Medicare patients.3–6 This trend may have been influenced by multiple factors, including increasing hospital boarding and crowding,7,8 and faster diagnostic and treatment protocols. In 2006, the Centers for Medicare and Medicaid Services (CMS) initiated the Recovery Audit Contractor (RAC) program with the goal of identifying potential waste in the program.4 One targets of this program were “short stay” hospital admissions. RACs review claims for inpatient stays and determine if the admission to the hospital was medically reasonable and necessary. If a RAC determines that the inpatient admission was not necessary and the care should have been provided on an outpatient basis, then the inpatient claim would be denied. To provide clarity, in 2014 CMS specifically identified a stay that spans two midnights or longer (“two midnight rule”) as inpatient stays.4,9 RACs would not review inpatient claims that crossed two midnights and would be presumed to be medically necessary. For fiscal year 2013 CMS estimated that the improper payment rate was 10.1 percent, which represented $36 billion.10) To assist in appropriately classifying patients, hospitals have employed case managers to differentiate between observation or acute inpatient status. McKesson’s InterQual criteria are one of the tools used by case management to determine if a patient qualifies for inpatient versus observation status.11 Patients with higher severity of illness, increasing comorbidities and requiring more intensive treatment often meet InterQual criteria for inpatient status.12,13 Historically, RACs have used InterQual criteria during review and so hospitals have turned to InterQual to align hospitalization status with what could turn up in an audit. Given the widespread use, it is important to understand whether InterQual accurately predicts length of stay.
One of the leading diagnosis associated with payment denials by CMS is syncope.14 In a recent analysis of the California Statewide Database showed that the median length of stay for a syncope evaluation is 2 days without significant change over 6 years.15 Syncope is a chief common complaint for older adults in the ED, and often presents a diagnostic challenge.16,17 Approximately 1% of all ED visits are for syncope, and almost one third of these cases are admitted. Given the variation in the evaluation of syncope and potential costs to hospitals,it is imperative to appropriately classify patients in observation or inpatient status. We evaluated the accuracy of InterQual criteria to determine LOS of less than or greater than two midnights in older adults with syncope.
Materials and Methods:
This is a secondary analysis of a large, multicenter, prospective cohort study of older adults with unexplained syncope (ClinicalTrials.gov identifier NCT01802398)18 to determine whether InterQual criteria predicted the need for observation (less than two midnights) vs. acute hospitalization (more than 2 midnights). The study was approved by the institutional review boards at all sites and written, informed consent was obtained from all participating subjects.
Briefly, this study was conducted at 11 academic emergency departments across the United States from April 28, 2013 to September 21, 2016. ED annual volumes ranged from 47,000 to 120,000. Eligible patients were ≥60 years of age with a complaint of syncope or near-syncope at 11 academic United States EDs. Exclusion criteria were: intoxication, medical or electrical intervention to restore consciousness, and inability or unwillingness to provide informed consent or follow-up information. Patients with a presumptive cause of loss of consciousness due to seizure, stroke or transient ischemic attack, or hypoglycemia were also excluded.
All patients underwent standardized history, physical examination, laboratory testing, and 12-lead ECG testing. Additional testing and patient disposition were directed by the treating clinical providers. We conducted 30-day patient follow-up using previously described methods,19 including a review of the electronic medical records by local research personnel to evaluate for serious outcomes within 30 days from the index ED evaluation.
Patients were excluded if they were discharged, transferred, eloped or left against medical advice after initial evaluation in the ED or if they had any identified causes of syncope in the ED meeting objective immediate inpatient admission criteria, including cardiac arrhythmias, myocardial infarction, cardiac intervention, new diagnosis of structural heart disease, stroke, pulmonary embolism, aortic dissection, subarachnoid hemorrhage, cardiopulmonary resuscitation, or internal hemorrhage/anemia requiring transfusion. LOS was calculated by using patient arrival time in the ED and discharge time from the hospital per the local electronic health record, and how many midnights the stay was.
The primary outcome was LOS over two midnights. The predictor of interest was InterQual classification of observation versus inpatient status. InterQual criteria are based on the 2018 guidebook (https://www.changehealthcare.com/solutions/interqual). To explore whether InterQual criteria have improved over time, we conducted a secondary analyses assessing the 2009 InterQual criteria, which required only one of two criteria (known cardiac disease or drug induced cardiac disorder) to meet inpatient criteria of having history of cardiac disease. Interqual uses a branching logic, which consists of findings on echocardiography, electrocardiogram, and symptoms. In order to meet inpatient criteria, the patient needs to meet a criteria in each of the category within history, associated symptoms, ECG finding, or have aortic stenosis with valve area <1.0 cm2. Criteria used in our analysis are included in Table 1.
Table 1.
InterQual criteria used for observation versus inpatient status recommendation
| History of (one) |
| Ejection Fraction <40% |
| Premature sudden death in family |
| Associated symptoms (one) |
| Dyspnea |
| Palpitations |
| Syncope During Exertion |
| Syncope While Supine Hypotension |
| Heart Rate <60/min |
| ECG findings (one) |
| QRS duration ≥120 ms |
| Prolonged QTc (>440 ms in men, >460 ms in women) |
| Short QTc (<340 ms) |
| Abnormal ECG |
| Abnormal ECG - Short PR Interval (<10 ms) |
| Abnormal ECG - Brugada Pattern |
| Abnormal ECG - Wolff-Parkinson White |
| Aortic Stenosis ≤1.0 cm2 |
ECG: electrocardiogram, ms: millisecond
Patient characteristics were described as number and percentage or mean and SD. Differences between categorical variables are analyzed with a chi-square test or Fisher’s exact test and differences between continuous variables with two sample t-tests. Significance was defined as p<0.05. We calculated the sensitivity, specificity, negative and positive predictive values of the InterQual criteria. Data analyses were performed using the R package (R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/).
Results:
Overall, 3,686 patients were enrolled in the study, 674 patients were discharged after initial evaluation in the ED and 62 patients had other dispositions, 376 patients had a serious diagnosis found during the ED encounter, and 108 patients had missing LOS information (Figure 1). After exclusions, there were 2361 patients available for analysis. Overall, 1,227 (52.0%) patients were male, 1,945 (82.8%) were white, with a mean age of 73.2 +/− 9.0. The median LOS was 32.6 (IQR 24.2–71.8) hours and mean LOS 61.3+/− 82h. Table 2 describes the individual characteristics of the cohort. Over half (54.0%) of patients were initially categorized as observation status.
Figure 1.

Patients screened and enrolled for analysis
Table 2.
Patient demographics
| Variable | Overall Cohort (n=2361) | InterQual not met (n=1033) | InterQual met (n=1328) | p-value |
|---|---|---|---|---|
| Age | 0.037 | |||
| 60 to <70 | 975 (41.3) | 461 (44.7) | 514 (38.8) | |
| 70 to <80 | 764 (32.4) | 313 (30.3) | 451 (34.0) | |
| 80 to <90 | 514 (21.8) | 213 (20.6) | 301 (22.7) | |
| 90+ | 105 (4.5) | 45 (4.4) | 60 (4.5) | |
| Male Gender | 1227 (52.0) | 414 (40.1) | 813 (61.2) | <0.001 |
| Race | 0.199 | |||
| White or Caucasian | 1945 (82.8) | 854 (82.8) | 1091 (82.8) | |
| Black or African American | 331 (14.1) | 137 (13.3) | 194 (14.7) | |
| Asian | 29 (1.2) | 17 (1.7) | 12 (0.9) | |
| Other | 44 (1.9) | 23 (2.2) | 21 (1.6) | |
| Length of Stay (hours), median [IQR] | 32.6 [24.2, 71.8] | 30.1 [23.6, 66.6] | 41.6 [24.8, 74.0] | <0.001 |
| Length of Stay Crosses 2 Midnights | 1109 (47.0) | 435 (42.1) | 674 (50.8) | <0.001 |
| Initial Disposition | 0.033 | |||
| Inpatient | 1087 (46.0) | 450 (43.6) | 637 (48.0) | |
| Observation | 1274 (54.0) | 583 (56.4) | 691 (52.0) | |
| History of | ||||
| Congestive Heart Failure | 318 (13.5) | 66 (6.4) | 252 (19.0) | <0.001 |
| Coronary Artery Disease | 673 (28.5) | 204 (19.8) | 469 (35.4) | <0.001 |
| Arrhythmia | 493 (20.9) | 156 (15.1) | 337 (25.5) | <0.001 |
| Ejection Fraction < 40% | 78 (3.3) | 0 (0.0) | 78 (5.9) | <0.001 |
| Premature sudden death in family | 23 (1.0) | 0 (0.0) | 23 (1.7) | <0.001 |
| Prescribed Medication | ||||
| Beta Blockers | 964 (40.9) | 348 (33.7) | 616 (46.5) | <0.001 |
| Calcium Channel Blockers | 449 (19.0) | 196 (19.0) | 253 (19.1) | 0.957 |
| Diuretics | 732 (31.0) | 270 (26.2) | 462 (34.8) | <0.001 |
| Dyspnea | 477 (20.2) | 198 (19.2) | 279 (21.0) | 0.269 |
| Palpitations | 298 (12.6) | 133 (12.9) | 165 (12.4) | 0.744 |
| Syncope During Exertion | 424 (18.0) | 179 (17.3) | 245 (18.4) | 0.482 |
| Syncope While Supine | 87 (3.7) | 37 (3.6) | 50 (3.8) | 0.815 |
| Hypotension | 269 (11.4) | 106 (10.3) | 163 (12.3) | 0.127 |
| Heart Rate <60/min | 298 (12.7) | 0 (0.0) | 298 (22.6) | <0.001 |
| QRS duration ≥ 120 ms | 435 (18.7) | 0 (0.0) | 435 (32.8) | <0.001 |
| Prolonged QTc (>440 ms in men, >460 ms in women) | 1040 (44.6) | 0 (0.0) | 1040 (78.5) | <0.001 |
| Short QTc (<340 ms) | 6 (0.3) | 0 (0.0) | 6 (0.5) | 0.040 |
| Abnormal ECG | 1282 (54.9) | 386 (38.3) | 896 (67.6) | <0.001 |
| Abnormal ECG - Short PR Interval (<10 ms) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1.000 |
| Abnormal ECG - Brugada Pattern | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1.000 |
| Abnormal ECG - Wolff-Parkinson White | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1.000 |
| Aortic Stenosis ≤ 1.0 cm2 | 9 (0.4) | 0 (0.0) | 9 (0.7) | 0.006 |
| Physician Risk Assessment, mean (SD) | 9.2 (11.8) | 8.0 (10.7) | 10.1 (12.6) | <0.001 |
Primary Results:
Table 2 describes the individual characteristics of the cohort: 1252 (53.0%) of patients had LOS more than 2 midnights and Figure 2 shows the LOS for study patients. Using InterQual criteria, 1,328 (56.2%) of patients would meet criteria for inpatient hospitalization. These patients tended to be older, more likely to be male and had higher history of cardiovascular disease, including heart failure, coronary artery disease, and arrhythmias (all p<0.05). However, patients had similar symptoms, including dyspnea, palpitations, syncope during exertion or supine, and hypotension.
Figure 2.
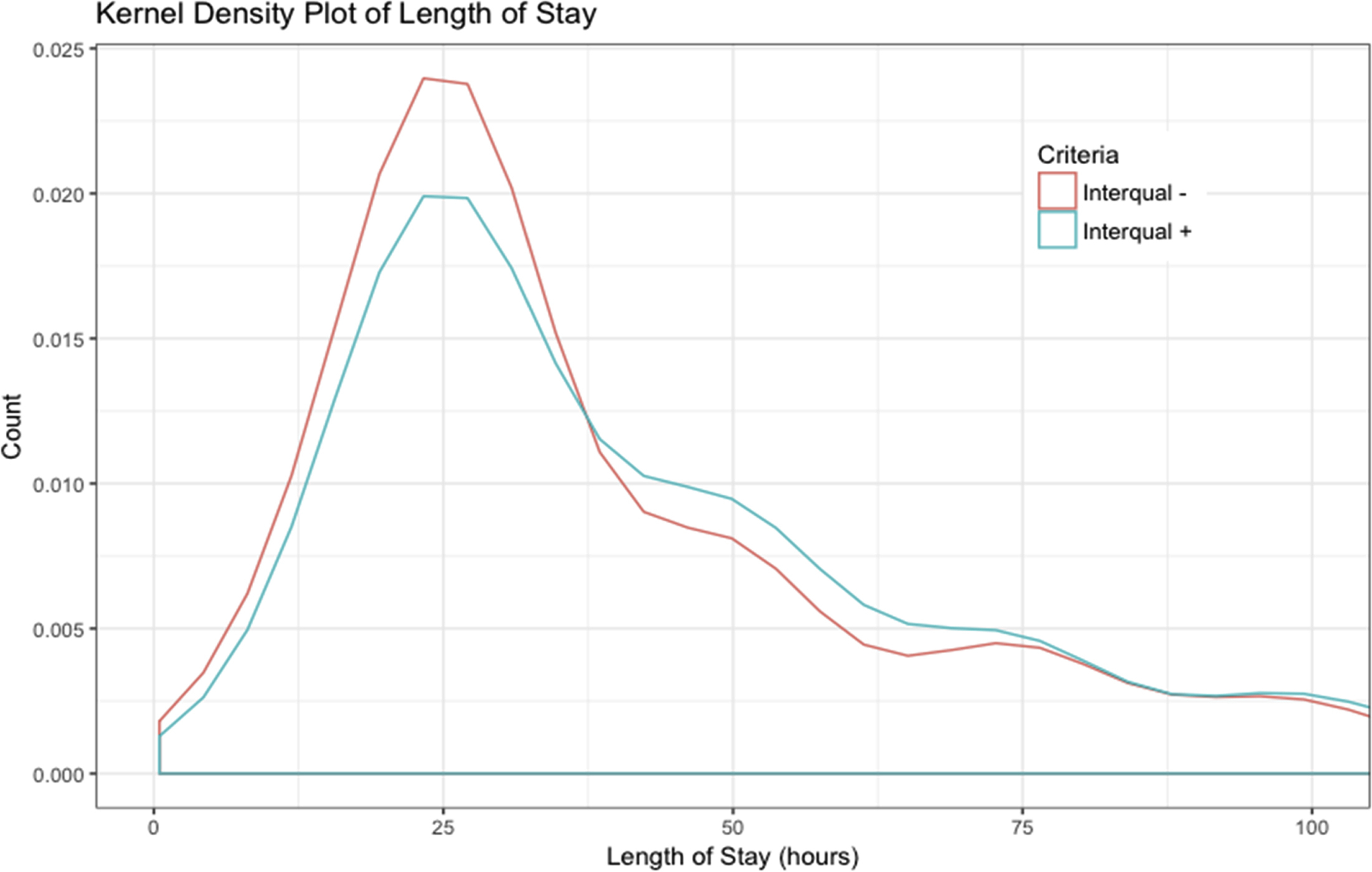
Length of stay of those who met and did not meet InterQual acute stay for syncope.
Meeting InterQual criteria did predict LOS over 2 midnights (odds ratio 1.42; 95% CI 1.20–1.67). However, the accuracy of InterQual criteria to predict LOS was modest (Table 3). The sensitivity of InterQual criteria for LOS over two midnights was 60.8% (95% CI 57.9–63.6%); specificity 47.8% (95% CI 45.0–50.5%); PPV 50.8% (48.1–53.4%); NPV 57.9% (54.9–60.9%).
Table 3.
InterQual sensitivity, specificity, PPV and NPV
| Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | PLR (95% CI) | NLR (95% CI) | |
|---|---|---|---|---|---|---|
| LOS crossing two midnights | 60.8% (57.9%, 63.6%) | 47.8% (45.0%, 50.5%) | 50.8% (48.1%, 53.4%) | 57.9% (54.9%, 60.9%) | 1.16 (1.08, 1.25) | 0.82 (0.75, 0.9) |
| LOS ≥ 48 hours | 60.7% (57.6%, 63.8%) | 46.8% (44.2%, 49.4%) | 43.6% (40.9%, 46.3%) | 63.7% (60.8%, 66.6%) | 1.14 (1.06, 1.22) | 0.84 (0.76, 0.93) |
CI: confidence interval
PPV: positive predictive value
NPV: negative predictive value
PLR: positive likelihood ratio
NLR: negative likelihood ratio
Additional analysis assessed the 2009 InterQual criteria to meet inpatient criteria of any cardiac disease. Similar to current criteria, InterQual criteria did predict increased LOS (odds ratio 1.66; 95% CI 1.41–1.96). The sensitivity of InterQual criteria was 57.5% (95% CI 54.3–60.6%); specificity was higher at 55.2% (95% CI 52.6–57.8%); PPV46.5% (43.6–49.3%); NPV 65.7% (63.0–68.4%).
Discussion:
InterQual criteria are used by case management and utilization staff as a screening tool to assist physicians in determining the appropriate level of care when patients require hospitalization. In our study, we found that InterQual criteria have only modest sensitivity and specificity for assigning older syncope patients to the appropriate disposition status. In addition, our analyses showed that there is no evidence that InterQual criteria have improved performance over time.
Previous studies that focused on the accuracy of InterQual criteria for other patients requiring acute care had similar results: a small study of patients with gastrointestinal bleeding showed poor prediction of need for admission, and over 50% of those recommended for discharge would have needed further care including blood transfusion, need for over 500 mL fluid bolus, >2 gm drop in hemoglobin, new congestive heart failure or chest pain, intensive care unit transfer, new need for telemetry, new ECG ischemia, need for surgery, intravenous vasopressors, endoscopic intervention, variceal bleeding, or death.20 In another study, InterQual criteria differed significantly from a panel of psychiatrists reviewing charts for the appropriateness for psychiatric admissions and continued stays.21 More recently, Wang et al. evaluated the accuracy of 2012 InterQual criteria for predicting LOS in patients with congestive heart failure. Overall, InterQual criteria was a poor predictor of LOS.12 In a large study of over 40,000 hospitalizations, the authors found that observation stays “did not meet the CMS definition of observation” Over 16.5% of observation patients stayed more than 48 hours. The authors also found that there were 1,141 distinctly billed observation codes. This wide variety of diagnoses, combined with complicated InterQual criteria, suggest that observation status is not well defined.5
The differentiation between observation and inpatient is important for several reasons. Time in the hospital in observation status is considered outpatient rather than inpatient, it is not counted toward the three-day inpatient stay requirement that, among other requirements, qualifies a Medicare beneficiary for subsequent skilled nursing facility care. While observation services are often appropriate, the extended use of such services could have unintended consequences for some Medicare beneficiaries. There is concern that Medicare beneficiaries have increased out-of-pocket expenses for observation admissions.22 However, a report in 2013 from the Office of the Inspector General, which shows that the patient expense for an observation stay was less than the expense for a short inpatient stay 94% of the time. For hospitals, inpatient and observation status also differ in payment: a recent analysis of a hypothetical 3-day hospitalization for syncope showed that the total hospital revenue would be almost $4,000 if billed as an inpatient hospitalization versus only $1,500 for an observation stay.22 Given almost 460,000 hospitalizations for syncope annually, this represents millions in potential difference in payments. This is balanced by RAC audits and denials of payment.23
Limitations
There are several limitations to our analysis. We had data on patients with ejection fractions <40%, while InterQual categorizes those with ejection fraction <35% as the cut point. This may cause us to categorize more patients as acute vs observation. However, there were only 78 patients in this category and would not have significantly changed the test characteristics and diagnostic accuracy of the InterQual criteria. In addition, we did not have any patients who had significant findings such as short PR interval, Brugada or Wolf-Parkinson-White syndrome. This is most likely due to our cohort of older adults, as these conditions are usually diagnosed at a younger age. We also recognize there may be bias in LOS as patients who are designated as observation status tend to have shorter LOS. However, we found that in both the observation and inpatient assigned groups, LOS were similar. Overall, we were only missing LOS data on less than 5% of our cohort. We did not collect information on individual site policies and practices for classification of observation versus admission, but by including 11 hospitals, we hope to have captured variation within the data. Lastly, while this was a multicenter study, all centers were academic medical centers and practices may not be generalizable to community hospitals.
Conclusion
In older adults with syncope, those who met InterQual criteria for inpatient status had longer LOS compared to those who did not; however, the accuracy of the criteria is poor, with sensitivity of 60% and sensitivity of 48%. Future research should identify criteria to improve LOS prediction.
Article summary:
1. Why is this topic important?
Syncope is a common chief complaint in older adults in the emergency department, and frequently placed in observation status. To assist in appropriately classifying patients, hospitals have employed case managers often using InterQual criteria to differentiate between observation or acute inpatient status, which may be different than physician judgment.
2. What does this study attempt to show?
This study show that InterQual criteria have only modest sensitivity and specificity for assigning older syncope patients to the appropriate disposition status.
3. What are the key findings?
This study show that InterQual criteria have only modest sensitivity and specificity for assigning older syncope patients to the appropriate disposition status. While those with inpatient status have longer lengths of stay, the difference is only modest.
4. How is patient care impacted?
Using InterQual criteria to assign disposition status may not be beneficial for patients.
Acknowledgments
Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award R01HL111033.
Funding Sources and Support:
This work was supported by a grant from the National Heart Lung and Blood Institute (Grant Number NIH R01 HL 111033). The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. The contents do not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Trial registration number: NCT01802398
Conflicts of interest:
AMC has received funding from Ortho Diagnostics, Bristol Meyers Squibb, Abbott, Roche, Entegrion, Nanomix, Alere, the National Institutes of Health and PCORI. JEH’s institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health and JEH’s institution has received contract funding from Alere, Siemens, Roche and Trinity for industry-initiated research institutional research. CLC’s institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health. CLC’s institution has received contract funding from Radiometer and Ortho Scientific for industry-initiated research. TAG’s institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health. REW’s institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health. ANY’s institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health. SEM’s institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health. DHA’s institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health institution and has received contract funding for industry-initiated research from Roche. AB’s institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health. AB’s institution has received contract funding f from Radiometer and Ortho Scientific for industry-initiated research. CWB’s institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health. CWB has received funding personally from Roche for speaking and Janssen Pharmaceuticals for advisory board participation. JMC institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health. JMC’s institution has received funding for industry initiated research from Entegrion and Astra Zeneca. JMC has received funding from Wellstat Therapeutics. DBD institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health. DBD has received funding personally from Roche for consulting and DBD’s institution has received contract funding from Novartis, Ortho Scientific, and Roche for industry-initiated research institutional research. DKN’s institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health. DKN has received funding personally from Pfizer for consulting. MNS institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health. MNS’ institution has received contract funding from Roche and Omron for industry-initiated research. KAS’s institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health. ABS’s institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health. ABS has received funding personally from Siemens and Quidel for consulting. STW’s institution has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health. BCS has received grant funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health. BCS has received funding personally from Medtronic and received diagnostic testing platforms for this study from Roche.
References
- 1.Yealy DM, De Hart DA, Ellis G, Wolfson AB. A survey of observation units in the United States. The American Journal of Emergency Medicine 1989;7(6):576–580. doi: 10.1016/0735-6757(89)90277-5. [DOI] [PubMed] [Google Scholar]
- 2.Mace SE, Graff L, Mikhail M, Ross M. A national survey of observation units in the United States. The American Journal of Emergency Medicine 2003;21(7):529–533. doi: 10.1016/j.ajem.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 3.Venkatesh AK, Wang C, Ross JS, Altaf FK, Suter LG, Vellanky S, Grady J, Bernheim SM. Hospital Use of Observation Stays: Cross-Sectional Study of the Impact on Readmission Rates. Med Care 2016;54(12):1070–1077. doi: 10.1097/MLR.0000000000000601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Two-Midnight Rule. 10.1377/hpb20150122.963736/full/. Accessed December 27, 2018. [DOI]
- 5.Sheehy AM, Graf B, Gangireddy S, Hoffman R, Ehlenbach M, Heidke C, Fields S, Liegel B, Jacobs EA. Hospitalized but Not Admitted: Characteristics of Patients With “Observation Status” at an Academic Medical Center. JAMA Intern Med 2013;173(21):1991–1998. doi: 10.1001/jamainternmed.2013.8185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sheehy AM, Caponi B, Gangireddy S, Hamedani AG, Pothof JJ, Siegal E, Graf BK. Observation and inpatient status: Clinical impact of the 2-midnight rule. Journal of Hospital Medicine 9(4):203–209. doi: 10.1002/jhm.2163. [DOI] [PubMed] [Google Scholar]
- 7.Hoot NR, Aronsky D. Systematic Review of Emergency Department Crowding: Causes, Effects, and Solutions. Annals of Emergency Medicine 2008;52(2):126–136.e1. doi: 10.1016/j.annemergmed.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pines JM, Griffey RT. What We Have Learned From a Decade of ED Crowding Research. Acad Emerg Med 2015;22(8):985–987. doi: 10.1111/acem.12716. [DOI] [PubMed] [Google Scholar]
- 9.Fact Sheet: Two-Midnight Rule | CMS. https://www.cms.gov/newsroom/fact-sheets/fact-sheet-two-midnight-rule-0. Accessed December 7, 2018.
- 10.MedicareFee-for-Service2013ImproperPaymentsReport.pdf. https://www.cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/Medicare-FFS-Compliance-Programs/CERT/CERT-Reports-Items/Downloads/MedicareFee-for-Service2013ImproperPaymentsReport.pdf. Accessed December 27, 2018.
- 11.Mitus AJ. The Birth of InterQual: Evidence-Based Decision Support Criteria That Helped Change Healthcare. Professional Case Management 2008;13(4):228. doi: 10.1097/01.PCAMA.0000327413.01849.04. [DOI] [PubMed] [Google Scholar]
- 12.Wang H, Robinson RD, Coppola M, Fernandez D, Ros F, Zenarosa NR, Burton MJ, Delaney KA. The Accuracy of Interqual Criteria in Determining the Need for Observation Versus Hospitalization in Emergency Department Patients With Chronic Heart Failure. Critical Pathways in Cardiology 2013;12(4):192. doi: 10.1097/HPC.0b013e3182a313e1. [DOI] [PubMed] [Google Scholar]
- 13.InterQual® | Change Healthcare. https://www.changehealthcare.com/solutions/interqual. Accessed December 7, 2018.
- 14.Exploring the Impact of the RAC Program on Hospitals Nationwide May 2014. https://www.aha.org/system/files/2018-03/14q1ractracresults.pdf. Accessed December 20, 2018.
- 15.Joy PS, Kumar G, Olshansky B. Syncope: Outcomes and Conditions Associated with Hospitalization. Am J Med January 2017. doi: 10.1016/j.amjmed.2016.12.030. [DOI] [PubMed] [Google Scholar]
- 16.Walsh K, Hoffmayer K, Hamdan MH. Syncope: diagnosis and management. Curr Probl Cardiol 2015;40(2):51–86. doi: 10.1016/j.cpcardiol.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 17.Task Force for the D, Management of S, European Society of C, European Heart Rhythm A, Heart Failure A, Heart Rhythm S, Moya A, Sutton R, Ammirati F, Blanc JJ, Brignole M, Dahm JB, Deharo JC, Gajek J, Gjesdal K, Krahn A, Massin M, Pepi M, Pezawas T, Ruiz Granell R, Sarasin F, Ungar A, van Dijk JG, Walma EP, Wieling W. Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J 2009;30(21):2631–2671. doi: 10.1093/eurheartj/ehp298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Probst M, Gibson T, Weiss RE, Yagapen AN, Malveau SE, Adler DH, Bastani A, Baugh C, Caterino JM, Clark CL, Diercks DB, Hollander JE, Nicks BA, Nishijima DK, Shah MN, Stiffler KA, Storrow AB, Wilber ST, Sun BC. Risk Stratification of Older Adults Who Present to the Emergency Department With Syncope: The FAINT Score. Annals of Emergency Medicine 2020;75(2):147–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nicks BA, Shah MN, Adler DH, Bastani A, Baugh CW, Caterino JM, Clark CL, Diercks DB, Hollander JE, Malveau SE, Nishijima DK, Stiffler KA, Storrow AB, Wilber ST, Yagapen AN, Sun BC. Minimizing Attrition for Multisite Emergency Care Research. Acad Emerg Med 2017;24(4):458–466. doi: 10.1111/acem.13135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.null Irvin, null Nigl, null Lowe. Accuracy of interqual criteria in determining the hospitalization need in medicare patients with gastrointestinal bleeding. Acad Emerg Med 2000;7(10):1166. [PubMed] [Google Scholar]
- 21.Goldman RL, Weir CR, Turner CW, Smith CB. Validity of utilization management criteria for psychiatry. Am J Psychiatry 1997;154(3):349–354. doi: 10.1176/ajp.154.3.349. [DOI] [PubMed] [Google Scholar]
- 22.Baugh CW, Schuur JD. Observation Care — High-Value Care or a Cost-Shifting Loophole? New England Journal of Medicine 2013;369(4):302–305. doi: 10.1056/NEJMp1304493. [DOI] [PubMed] [Google Scholar]
- 23.25 Statistics on Hospitals and RAC Audits https://www.beckershospitalreview.com/finance/25-statistics-on-hospitals-and-racaudits.html. Accessed December 27, 2018.


