Abstract
Background:
Psilocybin-containing mushrooms are used for recreational, spiritual, self-development and therapeutic purposes. However, physiologically relatively nontoxic, adverse reactions are occasionally reported.
Aims:
This study investigated the 12-month prevalence and nature of magic mushroom-related adverse reactions resulting in emergency medical treatment seeking in a global sample of people reporting magic mushroom use.
Methods:
We use data from the 2017 Global Drug Survey – a large anonymous online survey on patterns of drug use conducted between November 2016 and January 2017.
Results:
Out of 9233 past year magic mushroom users, 19 (0.2%) reported having sought emergency medical treatment, with a per-event risk estimate of 0.06%. Young age was the only predictor associated with higher risk of emergency medical presentations. The most common symptoms were psychological, namely anxiety/panic and paranoia/suspiciousness. Poor ‘mindset’, poor ‘setting’ and mixing substances were most reported reasons for incidents. All but one respondent returned back to normality within 24 h.
Conclusions:
The results confirm psilocybin mushrooms are a relatively safe drug, with serious incidents rare and short lasting. Providing harm-reduction information likely plays a key role in preventing adverse effects. More research is needed to examine the detailed circumstances and predictors of adverse reactions including rarer physiological reactions.
Keywords: Adverse effects, magic mushrooms, psilocybin, psychedelics, safety
Introduction
Psilocybin-containing mushrooms (‘magic mushrooms’) have been used in some ancient cultures from prehistoric times (Carod-Artal, 2015), but more widespread use of the psychedelic did not start until the 1970s, following modern western research on psilocybin and increased knowledge about identification and cultivation of magic mushroom species (Andersson et al., 2009). The subjective effect of psilocybin is likely determined by partial agonism at the 5-HT2A receptor, which includes perceptual alterations (e.g. synaesthesia), increased emotional lability and changes in sense of self, time and space (Nichols, 2016; Vollenweider et al., 1998). Re-emerging experimental research on psilocybin in the past two decades has highlighted promise in the treatment of various mental health conditions and addictions (Rucker et al., 2018) as well as potential to increase well-being (Nicholas et al., 2018) and trait openness (MacLean et al., 2011) in healthy individuals.
Similar to other classical psychedelics – such as lysergic acid diethylamide( LSD; Holze et al., 2021; Kopra et al., 2022; Petranker et al., 2020) and ayahuasca (Lawn et al., 2017) – psilocybin is a physiologically safe substance relative to other psychoactive drugs with no evidence of neurophysiological deficits, organ damage or addiction potential (Johnson et al., 2018; Nichols, 2016). Acute physiological effects of psilocybin are mild. In normal doses, ranging from 3 to 30 mg of psilocybin corresponding to roughly 5–50 g of fresh mushrooms, it induces slight increases in breathing frequency, heart rate and blood pressure (Carbonaro et al., 2018; Gouzoulis-Mayfrank et al., 1999). Magic mushroom overdoses have additionally been associated with nausea, dizziness, shivering and abdominal pain (Van Amsterdam et al., 2011), though some of these symptoms are believed to be either psychosomatic or induced by phenylethylamine found in some species of mushrooms (Beck et al., 1998). Magic mushroom-related presentations to emergency departments do occur, but are usually rare and non-severe, dominated by mainly psychological symptoms with majority discharged after a short duration of stay (Leonard et al., 2018; Peden et al., 1981; Satora et al., 2005).
There are only three known deaths attributed to magic mushroom toxicity (Gerault and Picart, 1996; Lim et al., 2012). The estimated lethal dose of psilocybin is approximately 6 g of psilocybin drug substance, in essence 1000 times more than the threshold dose of 6 mg (Gable, 2004) and equivalent to about 10 kg of fresh mushrooms. Lethal overdose from eating mushrooms is, therefore, impractical as emesis would likely occur before absorption of toxic levels of the drug. However, variations in magic mushrooms’ potency between species, growing conditions and preservation can make estimating dosage difficult, hence increasing the risk of non-critical overdoses and challenging experiences.
The powerful psychological effects of psilocybin can, even in moderate doses, induce adverse reactions characterized by, for instance, anxiety, disorientation, fear, grief, paranoia and panic attacks (Barrett et al., 2016; Riley and Blackman, 2008; Van Amsterdam et al., 2011). Symptoms usually resolve within 6 h once the substance’s effects wear off, but a proportion report experiencing long-term detrimental effects on mental health (Carbonaro et al., 2016) and, in rarer cases, ‘flashbacks’, recurrences of perceptual alterations or other sensations experienced during the trip (Baggott et al., 2011; Carhart-Harris and Nutt, 2010). Furthermore, psilocybin-induced panic reactions and impairments in judgement and perception (Wittmann et al., 2007) can contribute to dangerous behaviour, accidents, self-harming and even suicidality (Carbonaro et al., 2016; Strassman, 1984). For instance, a small number of deaths from falls or jumps from tall buildings have been attributed to magic mushroom use (Van Amsterdam et al., 2011).
The promising research on psilocybin’s healing potential has given the substance positive visibility in the media in recent years. In experimental settings, with comprehensive participant screenings, carefully measured doses and supporting dosing environments, adverse reactions are indeed rare and outcomes generally positive (Rucker et al., 2018). Concerns have been raised that positive recovery stories might not only encourage psychedelic use but simultaneously overshadow information on safety precautions with potentially detrimental consequences (see the studies by Carhart-Harris et al., 2018; Yaden et al., 2021). An alarming example came from a recent report of a man with bipolar disorder who, inspired by reports of psychedelics’ therapeutic effects, injected homemade magic mushroom solution intravenously in an attempt to treat his depression, subsequently developing a multi-organ failure and spending 8 days in intensive care (Giancola et al., 2021).
To avoid human tragedies as well as their impact on psychedelics’ public image and progression of research, investigations on psychedelics’ risks are needed to guide public policy and harm-reduction initiatives. This study is an exploratory analysis of the occurrence, predictors and nature of adverse experiences resulting in emergency medical treatment (EMT) seeking following magic mushroom use, in a large international sample of Global Drug Survey (GDS) respondents. Specifically, we investigate the potential of demographic variables, mental health conditions, use patterns and previous magic mushroom experience as predictors of EMT incidents; and explore the symptom profile and recovery time from these experiences, concomitant use of other substances, perceived reasons for incidents and experiences’ impact on subsequent substance use.
Methods
Design
This investigation is one part of two articles looking at EMT seeking in response to psilocybin mushroom and LSD use in the same survey (Kopra et al., 2022). The reported methods are substantially similar within the two articles but are reproduced in each for the convenience of the reader.
The GDS is an annual, anonymous and encrypted online survey on substance use. It is advertised in social networking sites in collaboration with media partners and harm-reduction organizations. Using a self-nominating sampling method, the survey can effectively reach large amounts of respondents engaging in rarer practices and stigmatized behaviours, who would be difficult to access through representative sampling frames.
GDS 2017 was launched in November 2016 and was available until January 2017, in 10 languages. Participants were not remunerated. Full details about the survey design and recruitment, including related discussion on the survey’s utility can be found elsewhere (Barratt et al., 2017). Multi-institutional ethical approval was obtained from the King’s College London Research Ethics Committee (11671/001: GDS), University of Queensland (No. 2017001452) and The University of New South Wales (HREC HC17769) Research Ethics Committees. Access to the relevant sections of the GDS 2017 dataset (demographic data and sections on psychedelics) was obtained through a data sharing agreement with the GDS.
Measures
At the start of the survey a wide range of demographical information was collected. In subsequent sections, participants were asked to indicate when they last used specific drugs from an extensive list of substances including magic mushrooms (never, in the last 30 days, between 31 days and 12 months ago, more than 12 months ago). Those indicating history of use with a drug were then redirected to sections with in-depth questions about the use of these substances. Among other questions, people who reported past year magic mushroom use were inquired about the number of days they used the drug in the last 12 months; whether they used magic mushrooms for the first time in the last 12 months; the number of magic mushrooms they normally take on a day of use; and whether they had sought EMT following the use of magic mushrooms in the past year. The number of EMT incidents experienced was not recorded.
Those indicating having sought EMT were then redirected to a further set of questions about that incident. Respondents were asked to tick the psychological and physiological symptoms they presented with from a list of 21, extrapolated from the available literature. Respondents were also asked about the number of magic mushrooms they had consumed during that session, what (if any) other substances they had taken, the duration of symptoms and whether they had required hospitalization. Participants were then asked about their perceptions of the reasons for the incident, picking a maximum of three out of six options; and asked about the impact of their experience on their use of magic mushrooms and other substances.
Towards the end of the survey, all participants were asked about their overall well-being and mental health, including whether they have ever been diagnosed with a mental illness. Ethical review boards required that participants were allowed to skip questions and leave empty responses if they did not want to complete specific items.
Data analysis
Per-event risk of seeking EMT was calculated by dividing the number of participants indicating past year EMT seeking with the total number of times magic mushrooms was used among past year users, specifically
Only those participants responding to the EMT question were included when calculating the estimated total times used (the denominator), therefore, creating a representative sample of those proceeding and choosing to respond to the EMT question. While median and interquartile range (IQR) of past year magic mushroom uses were used for descriptive data, mean was used in the above calculation for the most accurate estimate of total times used in the sample.
Non-parametric statistics were utilized because dependent variables were found to be non-normally distributed. Mann–Whitney U tests were used to investigate whether there were differences in the age, past-year frequency of use or number of mushrooms commonly consumed on a day of use between EMT seekers and non-seekers. Pearson’s Chi-square (χ2) or Fisher’s exact tests were used to investigate associations between treatment-seeking status and gender (male/female), previous magic mushroom experience status (first time in the past year/experienced) and presence of mental health diagnosis (yes/no). Descriptive statistics and graphs were created to explore the experiences and symptom profiles of EMT seekers. In addition, two multiple correspondence analyses (MCA; see Supplementary Methods and Abdi and Valentin, 2007) were conducted to explore pattern of relationships between different self-reported symptoms and between different self-reported reasons for incidents.
For all statistical analyses, complete case analysis was used, that is, responses with missing data on the variables of interest were excluded from those analyses. Analyses were performed using SPSS IBM Statistics 26.
Results
Frequency and risk of EMT incidents
GDS 2017 received a total of 119,108 responses, of which 24.5% (n = 29,124) reported lifetime use of magic mushrooms; 43.0% (n = 12,534) of those who reported lifetime magic mushroom use reported having used magic mushrooms within the past year; demographic profile of these participants is presented in Table 1. Of the 9233 participants responding to the EMT question, 0.2% (n = 19) indicated they had sought EMT following magic mushroom use in the past year.
Table 1.
Demographic profile of past year magic mushrooms users.
| N | Valid percentage | |
|---|---|---|
| N (percentage of lifetime users) | 12,534 | 43.0 a |
| Age | ||
| < 25 | 7890 | 62.9 |
| 25–34 | 3576 | 28.5 |
| 35+ | 1068 | 8.5 |
| Gender | ||
| Male | 9866 | 78.7 |
| Female | 2668 | 21.3 |
| Country of residence | ||
| Germany | 2591 | 20.7 |
| United States | 2134 | 17.0 |
| Canada | 1534 | 12.2 |
| Denmark | 1290 | 10.3 |
| United Kingdom | 1026 | 8.2 |
| Other | 3959 | 31.6 |
| Ethnicity | ||
| White | 6729 | 88.6 |
| Mixed | 338 | 4.4 |
| Hispanic/Latino | 228 | 3.0 |
| Other | 303 | 4.0 |
| Mental health diagnosis | ||
| None | 5636 | 73.1 |
| Yes | 2070 | 26.9 |
| Depression b | 1517 | 19.7 |
| Anxiety b | 1090 | 14.1 |
| ADHD b | 492 | 6.4 |
| Bipolar b | 202 | 2.6 |
| Psychosis b | 107 | 1.4 |
| Other b | 403 | 5.2 |
| Use patterns | ||
| Past-month users | 2835 | 22.6 |
| Past-year novel users | 3543 | 38.9 |
| Median days past-year use | 2 | 1–3 |
ADHD: attention deficit hyperactivity disorder.
Proportion of lifetime users.
Those with a diagnosis were able to tick more than one diagnosis, hence the total number being larger than above row.
Among responders to the EMT question, mean number of times magic mushrooms were used in the past year was 3.72 (SD = 13.1), resulting in the estimated 34,347 number of total times used. With 19 EMT seekers, this gave the per-event risk estimate of 0.00055, indicating 0.06% or approximately 1 in 1800 of past-year magic mushroom intakes led to EMT seeking in this sample.
Due to the high number of past-year users who did not respond to the EMT question, the potential for attrition bias as well as the estimated prevalence of skipping the question was investigated by examining the subsample of past-year users who completed the whole survey. Among these 1895 past-year users, the response rate to the EMT question was 98% (n = 1857), demonstrating that a large majority of missing responses have likely occurred due to dropouts. Among these 1857 responders, 0.3% (n = 6) indicated having sought EMT, indicating a low chance of significant attrition bias when compared to the rate in the total sample (0.2%).
Predictors of EMT seeking
Comparing the characteristics of EMT-seeking groups, Mann–Whitney U test revealed a significantly lower median age among EMT seekers (Median = 19, IQR: 18–23) compared to non-seekers (Median = 23, IQR: 20–27); Mann–Whitney test z = 3.09, p = 0.002. A Fisher’s Exact test showed no difference in the prevalence of EMT seeking between those with lifetime diagnoses of mental health conditions (0.2%) and those without (0.2%), p = 0.546. There was also no difference in the prevalence of EMT seeking between men (0.2%) and women (0.2%), p = 1.00.
Regarding patterns and history of use, Chi-square analysis showed no difference in the prevalence of EMT seeking between those who had used magic mushrooms for the first time the past year (0.2%) compared to those with previous experience (0.2%) χ2 (1, N = 9068) = 0.43, p = 0.512. There was also no significant difference between the number of commonly consumed mushrooms between seekers (Median = 4.0, IQR: 3.0–16.0) and non-seekers (Median = 4.0, IQR: 2.0–6.0), Mann–Whitney test z = 1.768, p = 0.077. There was also no significant difference in the past-year frequency of use of magic mushroom between EMT seekers (Median = 2.0, IQR: 1.0–6.5) and non-seekers (Median = 2.0, IQR: 1.0–3.0), Mann–Whitney test z = 1.479, p = 0.139.
Symptom profile and nature of EMT incidents
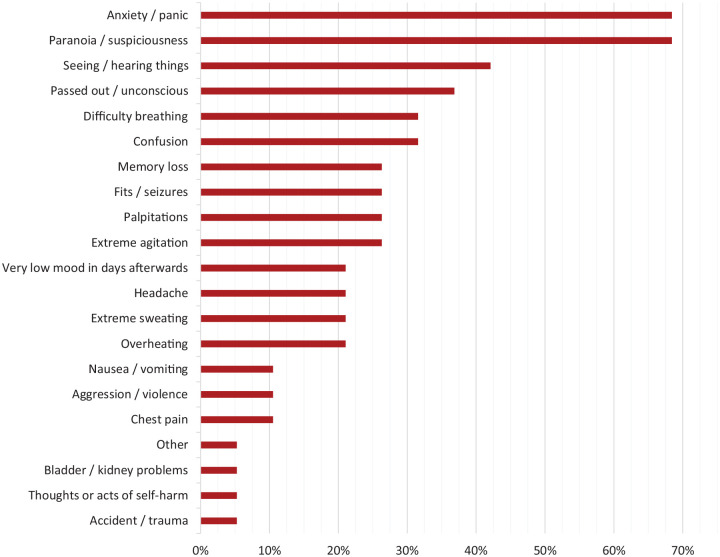
Frequency of different reported symptoms are shown in Figure 1. The median (IQR) number of reported symptoms was 5.0 (2.0–8.0). The most commonly occurring symptoms were anxiety/panic (68%), paranoia/suspiciousness (68%), seeing/hearing things (42%) and passing out/unconscious (37%). Observation of the MCA factor map (Supplementary Figure S1) showed that frequently reported anxiety/panic and paranoia/suspiciousness were very closely related, as were seeing/hearing things and extreme agitation. Furthermore, palpitations, overheating, self-harm and difficulty breathing tended to co-occur. A fourth cluster identified showed an association between symptoms such as passing out, seizures, sweating, confusion, memory loss and very low mood afterwards.
Figure 1.
Self-reported symptoms.
Eight EMT seekers (42%; 95% CI: 20–64%) were admitted to hospital. Table 2 shows the length of time it took for respondents to feel back to normal; all but one respondent reported returning to normality within 24 h, and all respondents recovered within 7 days.
Table 2.
Time to recovery.
| N | Valid percentage (95% CI) | Cu% | |
|---|---|---|---|
| 6 h | 12 | 67 (46–88) | 67 |
| 12 h | 3 | 17 (0–34) | 83 |
| 18 h | 1 | 6 (0–17) | 89 |
| 24 h | 1 | 6 (0–17) | 94 |
| 5–7 days | 1 | 6 (0–17) | 100 |
CI: confidence interval.
The median number of magic mushrooms consumed was 10.0 (IQR: 2.0–33.8). Table 3 shows other substances participants had used in the lead-up to the incident; 42% consumed no other substances, 37% of participants reported having used cannabis during the session while alcohol consumption was reported by 32%.
Table 3.
Other substances used preceding the incident.
| N | Percentage | |
|---|---|---|
| Cannabis | 7 | 37 |
| Alcohol | 6 | 32 |
| Cocaine | 1 | 5 |
| MDMA | 1 | 5 |
| Ketamine | 1 | 5 |
| Opioids | 1 | 5 |
| Nothing else | 8 | 42 |
MDMA: 3,4-methylenedioxymethamphetamine.
Reasons for why participants thought the incident had happened are presented in Table 4. The most common reason was wrong mind-set (47%), followed by wrong place (37%) and mixing with other substances (37%). Observation of the MCA factor map (Supplementary Figure S2) indicated wrong mind-set and mixing substances were commonly reported together.
Table 4.
Self-reported reasons for the incident.
| N | Percentage | |
|---|---|---|
| Mood/mind-set | 9 | 47 |
| Mixed substances | 7 | 37 |
| Place/setting | 7 | 37 |
| Took too much | 5 | 26 |
| Don’t know | 4 | 21 |
| Not magic mushrooms | 1 | 5 |
As a result of their experience, 58% of EMT seekers reported having cut down their magic mushroom use, while 37% reported no change in their magic mushroom use; 16% reduced and 0% increased their other illicit drug or alcohol use.
Discussion
This article examined the prevalence and nature of adverse experiences leading to EMT seeking following the use of magic mushrooms, in a large global sample. Consistent with expectations, EMT seeking was very rare, occurring in only 0.2% of people reporting past-year use, with an estimated 1 in 1800 of magic mushroom ingestions leading to these incidents. Adverse experiences were short term with only one respondent experiencing effects lasting over 24 h. These results largely replicate previous literature supporting magic mushrooms’ safety and are reassuring considering both the wider public health perspective and the potential future medicinal use of psilocybin.
The most prevalent symptoms were psychological in nature, namely anxiety/panic and paranoia/suspiciousness. These are consistent with previous reports of the nature of adverse reactions to psilocybin and other psychedelics and have been discussed in depth elsewhere (Barrett et al., 2016; Van Amsterdam et al., 2011). However, a number of concerning physiological symptoms also occurred; passing out or going unconscious, difficulty breathing and seizures were reported by 37%, 32% and 26%, respectively. While difficulty breathing is commonly related to panic and anxiety, aetiology behind the two others is less clear. Rapid changes in blood pressure induced either directly by the drug or by psychological reactions, as well as dehydration or undernutrition are plausible triggers for losing consciousness under psilocybin; however, it is also plausible that some participants have merely had a transient memory loss or had fallen asleep during the experience. Passing out could theoretically also result from cardiac arrhythmias associated with prolonged QT interval induced by psilocybin, although high doses would be needed for this to occur (Dahmane et al., 2021). A number of seizures following magic mushroom consumption have been reported, the exact causes being largely unascertained (De Sagun and Tabunar, 2012; Leonard et al., 2018; McCawley et al., 1962). It is possible that pre-existing conditions, interactions with other substances or medications as well as consumption of poisonous mushrooms may have played a role in a proportion of such reactions; specifically, lithium has consistently been linked to severe adverse reactions to psychedelics including seizures and fugue states (Nayak et al., 2021). Regardless, we cannot confirm whether all reported seizures in the survey have been true epileptic seizures in contrast to pseudoseizures triggered by psychological factors.
Contribution of polysubstance use to adverse psychedelic experiences have been reported previously (Bienemann et al., 2020; Van Amsterdam et al., 2011). In both this study as well as in our investigation on LSD-related EMT experiences (Kopra et al., 2022), majority of respondents consumed other substances prior to seeking EMT, most commonly cannabis and alcohol. Although we do not know the overall prevalence of concurrent use of these substances among the whole magic mushroom user sample, and therefore cannot infer based on these statistics alone to what extent their use is specifically linked to adverse experiences in contrast to magic mushroom use per se (previously both cannabis and alcohol has been found to be frequently co-administered with psilocybin; Barrett et al., 2006; Kuc et al., 2021; Licht et al., 2012); over one-third of our respondents reported mixing substances as a reason for their adverse experience. In a previous survey study on psilocybin-related challenging experiences, 53% reported having used cannabis and 19% alcohol during or immediately before their experience (Carbonaro et al., 2016). Of note, Carbonaro and colleagues also found 26% of respondents in the survey used cannabis to attempt calming down; however, only half of these reported their attempts to be successful, and in optional open-ended textual responses several participants spontaneously reported cannabis having significantly exacerbated their difficult experience (Carbonaro et al., 2016). Cannabis can cause acute psychotic-like symptoms, also prevalent in this survey (D’Souza et al., 2004), further supporting cannabis may be more likely to exacerbate than alleviate magic mushroom-related adverse reactions. A recent prospective survey study suggested the association with cannabis and challenging psychedelic experiences to be dose-dependent, with low and medium doses of cannabis linked to less challenging experiences, and high doses with more challenging experiences (Kuc et al., 2021).
Besides mixing substances, being in the wrong mood/mind-set and place/setting were among the most commonly reported reasons for incidents, consistent with extensive literature on the importance of these factors for preventing adverse reactions to psychedelics (Carhart-Harris et al., 2018). However, a significant proportion indicated uncertainty regarding the reason of the incident, two times higher than in our investigation on LSD (21% vs 10%; Kopra et al., 2022). Adverse reactions to psychedelics can occur even in optimized settings with adequate preparation (Carbonaro et al., 2016; Haijen et al., 2018). Anecdotal reports have described magic mushrooms’ effects as less predictable and less sensitive to ‘set and setting’ compared to LSD (Grey and Aremu, 2020; Third Wave, 2015). Therefore, despite being less likely to cause serious adverse experiences (Kopra et al., 2022; Leonard et al., 2018), higher proportion of these might be unexpected and triggered by unknown factors. More evidence is, however, needed to confirm the hypothesis. Results from the first experimental studies comparing the effects of LSD and psilocybin head-to-head are yet to be published (NCT03604744; NCT04227756).
The only predictor of EMT incidents in this study was younger age. Previous studies on psilocybin had similarly shown younger age to predict more challenging experiences (Carbonaro et al., 2016; Studerus et al., 2012). The association was also found in our investigation on LSD-related EMT incidents (Kopra et al., 2022), where we suggested potential explanations for the association including lower risk-averseness and higher impulsivity that could link to more risky drug use behaviours (Spear, 2000; Steinberg et al., 2008), as well as relative difficulty of emotional regulation in some younger people (Carstensen et al., 2011; Williams et al., 2006). Previous experience with psychedelics did not predict risk of incidents in either of our two investigations. Carbonaro et al. (2016) had previously found a negative correlation between past hallucinogen use and difficulty of psilocybin-induced challenging experiences; however, although significant, this association was small in magnitude. People with more experience with psychedelics do not, therefore, appear to be protected from adverse experiences but should remain mindful of the risks brought by experimenting with challenging environments, increasing dosages and mixing substances.
There was no indication for a higher risk of EMT seeking in people with lifetime mental health diagnoses. Previous research has suggested associations between serious adverse reactions to psychedelics and presence of mental health conditions; however, it is possible the risk is less pronounced in common mental health conditions compared to psychotic or bipolar disorders (Cohen, 1960; Strassman, 1984). Psychedelics, specifically psilocybin, show early promise in the treatment of depression, anxiety and addictions, highlighting the relationship between mental health and the nature and outcomes of psychedelic experiences is highly multifaceted, affected by various contextual factors and traits beyond the presence of psychopathology (Aday et al., 2021; Carhart-Harris et al., 2018). People who use psychedelics are a self-selective group and some individuals with certain predispositions may instinctively know not to take psychedelics or to use them with more care, therefore, making it more difficult to find predictors of effects from naturalistic use. It is also plausible that some of those with lifetime diagnoses in our survey were recovered or in remission during the reporting period. Regardless, the present findings conflict with our investigation on LSD-related EMT presentations, where mental health conditions did predict EMT incidents with a large effect size (Kopra et al., 2022). Given the low number of magic mushroom incidents, the present finding could have been a false negative; alternatively, it is not ruled out that differences between susceptibility to adverse LSD and psilocybin experiences exist, an area which would require further investigation.
The low rate of emergency presentations is in line with both expert analyses and assessments of people using substances, rating psilocybin as the drug of lowest harm among commonly used recreational substances (Carhart-Harris and Nutt, 2013; Nutt et al., 2010; Van Amsterdam et al., 2010). The prevalence of EMT seeking in this study was approximately five times lower when compared to LSD-related EMT incidents in the same survey (Kopra et al., 2022). Similarly, an analysis of LSD and magic mushroom exposures reported to United States poison centres observed lower occurrence of major incidents and hospital admissions associated with the latter (Leonard et al., 2018). Potential explanations for these differences include higher potency of LSD (Isbell, 1959) that likely increases the risk of accidental overdoses, whereas extreme overdoses from mushroom consumption is practically very difficult; ‘taking too much’ was, indeed, a less commonly reported reason of EMT incidents in this study compared to our report on LSD (26% vs 40%; Kopra et al., 2022). In addition, psilocybin’s duration of effects is two times shorter compared to LSD (Nichols, 2016), decreasing the risk of prolonged adverse experiences. Other differences in the substances’ pharmacology and subjective effects have been reported (Giacomelli et al., 1998; McCartney et al., 2021), but further, experimental research is needed to confirm these and how they may contribute to the substance’s differential safety profile.
While the low incidence of EMT incidents is a positive finding it can also be regarded as a limitation in the study, as predictors of incidents were difficult to establish and nature of experiences could only be analysed from 19 participants. Specifically, higher using frequency and higher dose showed a trend towards increasing the risk of incidents; however, very large samples would be needed for enough power to detect these and potential other predictors. Continued investigation on less severe (and more common) adverse experiences can contribute to our knowledge about serious reactions which, based on reported symptoms, are often similar in nature but only more intense. Investigation is, however, also required on the aetiology of some more rare emergencies including seizures; reaching people with such experiences for more thorough qualitative assessments could provide insights on their causes and impact, and supplement data from official records and large quantitative surveys.
It is, regardless, reassuring that despite varying symptomology, all but one respondent reported being back to normality within 24 h. However, we cannot confirm whether ‘back to normality’ has, for some, meant only the resolution of acute drug effects and complications, and not necessarily the absence of longer lasting psychological impact. Although most people reporting challenging psychedelic experiences also cite resulting therapeutic value and benefits to their well-being (Carbonaro et al., 2016), they can also be traumatizing and lead to psychological distress especially when negative aspects dominate the trip and where there is no adequate support during and after the experience (Carbonaro et al., 2016; Gashi et al., 2021; Gorman et al., 2021). Training mental health professionals in psychedelic integration and reducing stigma and criminalization associated with psychedelic drugs is important for encouraging people to come forward and seek and receive help when this is needed (Gorman et al., 2021).
Several other limitations need to be considered when appraising this study. Self-nominating, non-probability sampling is subject to sampling and volunteer biases that reduce sample representativeness. In essence, inherent differences may exist between people who are reached by the recruitment and choose to volunteer to participate compared to those who are not. Differences could also occur among those who drop out early or who choose not to respond to specific questions. Although our subanalysis among survey completers indicated a low chance of significant attrition bias, we cannot ascertain whether the rare case of skipping the EMT question may have been disproportionately more common among actual EMT seekers or non-seekers, therefore, biasing the rate of EMT seeking to either direction. Furthermore, retrospective self-reports are often affected by recall and response biases; answers might be influenced by, for instance, substances’ effects on cognition or by personal opinions about drugs. In addition, the options for perceived reasons for the incident did not include ‘Other’ nor a possibility for an open-ended text response; therefore, the question and the limited options may be leading the respondents’ answers. Limitations concerning sampling, participation bias and response bias are discussed in more depth in our twin articles (Kopra et al., 2022); see also study by Barratt et al. (2017).
Our survey cannot confirm the purity or potency of magic mushrooms and potential other substances used. Even if correct substances have been reported, contribution of each in inducing the symptoms cannot be ascertained; similarly, we cannot confirm the extent to which psilocybin versus other compounds in magic mushrooms, such as phenylethylamine, have contributed to the experience – although the purpose of the article is to investigate naturalistic magic mushroom use and not the effects of pure psilocybin. Furthermore, our variable ‘number of mushrooms’ is a vague indicator of quantity used; besides the high variation in sizes of mushrooms, many people who use mushrooms record their use in grams or consume readily grinded, dried mushrooms and are, therefore, not aware of the number of mushrooms they have used. Finally, our survey could not establish the exact circumstances surrounding the incidents or the determining factors leading to EMT seeking in each case.
Regardless of limitations, this investigation has provided valuable insights on the occurrence and nature of magic mushroom–related serious adverse experiences, from the world’s largest survey on drug use. Magic mushrooms are relatively innocuous substances and rarely cause harm to the individual consuming them nor to other people. Most adverse reactions are short-lived, and their risk can be minimized with certain safety precautions. The results are reassuring from the public health perspective, and support the reassessment of psilocybin’s legal status to aid the delivery of clinical research and effective harm-reduction services.
Supplemental Material
Supplemental material, sj-docx-1-jop-10.1177_02698811221084063 for Adverse experiences resulting in emergency medical treatment seeking following the use of magic mushrooms by Emma I Kopra, Jason A Ferris, Adam R Winstock, Allan H Young and James J Rucker in Journal of Psychopharmacology
Footnotes
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship and/or publication of this article: A.W. is the founder and owner of the Global Drug Survey. J.F. is part of the Global Drug Survey Core Research Team but has no conflict of interest. King’s College London receives grant funding for phase 1 and 2 trials of psilocybin-assisted psychotherapy for depression, led by J.R. and A.Y., from COMPASS Pathways Ltd. J.R. has attended trial-related meetings paid for by COMPASS Pathways Ltd and has received consulting fees from Clerkenwell Health and Beckley PsyTech. A.Y. has received honoraria for attending advisory boards and presenting lectures for Allergan, Astra Zeneca, Bionomics, COMPASS, Eli Lilly, Janssen, LivaNova, Lundbeck, Servier, Sumitomo Dainippon Pharma and Sunovion; and has received consulting fees from Johnson & Johnson and LivaNova. He is also a co-editor of the Journal of Psychopharmacology.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: Professor Young’s independent research is funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. James Rucker holds a Clinician Scientist Fellowship Award (CS-2017-17-007) provided by the National Institute for Health Research at the Institute of Psychiatry, Psychology and Neuroscience at King’s College London, UK, which is part-funded by the NIHR Biomedical Research Centre and South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
ORCID iDs: Emma I Kopra  https://orcid.org/0000-0003-4447-5393
https://orcid.org/0000-0003-4447-5393
Jason A Ferris  https://orcid.org/0000-0001-7474-0173
https://orcid.org/0000-0001-7474-0173
Adam R Winstock  https://orcid.org/0000-0001-7854-8015
https://orcid.org/0000-0001-7854-8015
James J Rucker  https://orcid.org/0000-0003-4647-8088
https://orcid.org/0000-0003-4647-8088
Supplemental material: Supplemental material for this article is available online.
References
- Abdi H, Valentin D. (2007) Multiple correspondence analysis. Encyclopedia of Measurement and Statistics 2(4): 651–657. [Google Scholar]
- Aday JS, Davis AK, Mitzkovitz CM, et al. (2021) Predicting reactions to psychedelic drugs: A systematic review of states and traits related to acute drug effects. ACS Pharmacology & Translational Science 4: 424–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson C, Kristinsson J, Gry J. (2009) Occurrence and Use of Hallucinogenic Mushrooms Containing Psilocybin Alkaloids. Copenhagen: Nordic Council of Ministers. [Google Scholar]
- Baggott MJ, Coyle JR, Erowid E, et al. (2011) Abnormal visual experiences in individuals with histories of hallucinogen use: A Web-based questionnaire. Drug and Alcohol Dependence 114(1): 61–67. [DOI] [PubMed] [Google Scholar]
- Barratt MJ, Ferris JA, Zahnow R, et al. (2017) Moving on from representativeness: Testing the utility of the Global Drug Survey. Substance Abuse: Research and Treatment 11: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett FS, Bradstreet MP, Leoutsakos JS, et al. (2016) The Challenging Experience Questionnaire: Characterization of challenging experiences with psilocybin mushrooms. Journal of Psychopharmacology 30(12): 1279–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett SP, Darredeau C, Pihl RO. (2006) Patterns of simultaneous polysubstance use in drug using university students. Human Psychopharmacology: Clinical and Experimental 21(4): 255–263. [DOI] [PubMed] [Google Scholar]
- Beck O, Helander A, Karlson-Stiber C, et al. (1998) Presence of phenylethylamine in hallucinogenic Psilocybe mushroom: Possible role in adverse reactions. Journal of Analytical Toxicology 22(1): 45–49. [DOI] [PubMed] [Google Scholar]
- Bienemann B, Ruschel NS, Campos ML, et al. (2020) Self-reported negative outcomes of psilocybin users: A quantitative textual analysis. PLoS ONE 15(2): e0229067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbonaro TM, Bradstreet MP, Barrett FS, et al. (2016) Survey study of challenging experiences after ingesting psilocybin mushrooms: Acute and enduring positive and negative consequences. Journal of Psychopharmacology 30(12): 1268–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbonaro TM, Johnson MW, Hurwitz E, et al. (2018) Double-blind comparison of the two hallucinogens psilocybin and dextromethorphan: Similarities and differences in subjective experiences. Psychopharmacology 235(2): 521–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carhart-Harris RL, Nutt DJ. (2010) User perceptions of the benefits and harms of hallucinogenic drug use: A web-based questionnaire study. Journal of Substance Use 15(4): 283–300. [Google Scholar]
- Carhart-Harris RL, Nutt DJ. (2013) Experienced drug users assess the relative harms and benefits of drugs: A Web-based survey. Journal of Psychoactive Drugs 45(4): 322–328. [DOI] [PubMed] [Google Scholar]
- Carhart-Harris RL, Roseman L, Haijen E, et al. (2018) Psychedelics and the essential importance of context. Journal of Psychopharmacology 32(7): 725–731. [DOI] [PubMed] [Google Scholar]
- Carod-Artal FJ. (2015) Hallucinogenic drugs in pre-Columbian Mesoamerican cultures. Neurología (English Edition) 30(1): 42–49. [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Turan B, Scheibe S, et al. (2011) Emotional experience improves with age: Evidence based on over 10 years of experience sampling. Psychology and Aging 26(1): 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S. (1960) Lysergic acid diethylamide: Side effects and complications. Journal of Nervous and Mental Disease 130: 30–40. [DOI] [PubMed] [Google Scholar]
- Dahmane E, Hutson PR, Gobburu JVS. (2021) Exposure-response analysis to assess the concentration-QTc relationship of psilocybin/psilocin. Clinical Pharmacology in Drug Development 10: 78–85. [DOI] [PubMed] [Google Scholar]
- De Sagun S, Tabunar SM. (2012) Seizure and transient expressive aphasia in hallucinogenic mushroom (psilocybe) poisoning: A case report. Journal of Emergency Medicine 43(5): 932. [Google Scholar]
- D’Souza DC, Perry E, MacDougall L, et al. (2004) The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: Implications for psychosis. Neuropsychopharmacology 29(8): 1558–1572. [DOI] [PubMed] [Google Scholar]
- Gable RS. (2004) Comparison of acute lethal toxicity of commonly abused psychoactive substances. Addiction 99(6): 686–696. [DOI] [PubMed] [Google Scholar]
- Gashi L, Sandberg S, Pedersen W. (2021) Making ‘bad trips’ good: How users of psychedelics narratively transform challenging trips into valuable experiences. International Journal of Drug Policy 87: 102997. [DOI] [PubMed] [Google Scholar]
- Gerault A, Picart D. (1996) Fatal poisoning after a group of people voluntarily consumed hallucinogenic mushrooms. Le Bulletin De La Societe Mycologique De France 112: 1–14. [Google Scholar]
- Giacomelli S, Palmery M, Romanelli L, et al. (1998) Lysergic acid diethylamide (LSD) is a partial agonist of D2 dopaminergic receptors and it potentiates dopamine-mediated prolactin secretion in lactotrophs in vitro. Life Sciences 63(3): 215–222. [DOI] [PubMed] [Google Scholar]
- Giancola NB, Korson CJ, Caplan JP, et al. (2021) A ‘trip’ to the ICU: Intravenous injection of psilocybin. Journal of the Academy of Consultation-Liaison Psychiatry 62: 370–371. [DOI] [PubMed] [Google Scholar]
- Gorman I, Nielson EM, Molinar A, et al. (2021) Psychedelic harm reduction and integration: A transtheoretical model for clinical practice. Frontiers in Psychology 12: 710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gouzoulis-Mayfrank E, Thelen B, Habermeyer E, et al. (1999) Psychopathological, neuroendocrine and autonomic effects of 3, 4-methylenedioxyethylamphetamine (MDE), psilocybin and d-methamphetamine in healthy volunteers Results of an experimental double-blind placebo-controlled study. Psychopharmacology 142(1): 41–50. [DOI] [PubMed] [Google Scholar]
- Grey KL, Aremu F. (2020) LSD vs. mushrooms: Same but different. Available at: https://www.healthline.com/health/substance-use/lsd-vs-shrooms
- Haijen EC, Kaelen M, Roseman L, et al. (2018) Predicting responses to psychedelics: A prospective study. Frontiers in Pharmacology 9: 897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holze F, Caluori TV, Vizeli P, et al. (2021) Safety pharmacology of acute LSD administration in healthy subjects. Psychopharmacology (Berlin). Epub ahead of print 13 September. DOI: 10.1007/s00213-021-05978-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isbell H. (1959) Comparison of the reactions induced by psilocybin and LSD-25 in man. Psychopharmacologia 1(1): 29–38. [DOI] [PubMed] [Google Scholar]
- Johnson MW, Griffiths RR, Hendricks PS, et al. (2018) The abuse potential of medical psilocybin according to the 8 factors of the Controlled Substances Act. Neuropharmacology 142: 143–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopra EI, Ferris JA, Rucker JJ, et al. (2022, forthcoming) Adverse experiences resulting in emergency medical treatment seeking following the use of lysergic acid diethylamide (LSD). Journal of Psychopharmacology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuc J, Kettner H, Rosas F, et al. (2021) Psychedelic experience dose-dependently modulated by cannabis: Results of a prospective online survey. Psychopharmacology. Epub ahead of print 4 November. DOI: 10.1007/s00213-021-05999-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawn W, Hallak JE, Crippa JA, et al. (2017) Well-being, problematic alcohol consumption and acute subjective drug effects in past-year ayahuasca users: A large, international, self-selecting online survey. Scientific Reports 7(1): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard JB, Anderson B, Klein-Schwartz W. (2018) Does getting high hurt? Characterization of cases of LSD and psilocybin-containing mushroom exposures to national poison centers between 2000 and 2016. Journal of Psychopharmacology 32(12): 1286–1294. [DOI] [PubMed] [Google Scholar]
- Licht CL, Christoffersen M, Okholm M, et al. (2012) Simultaneous polysubstance use among Danish 3, 4-methylenedioxymethamphetamine and hallucinogen users: Combination patterns and proposed biological bases. Human Psychopharmacology: Clinical and Experimental 27(4): 352–363. [DOI] [PubMed] [Google Scholar]
- Lim TH, Wasywich CA, Ruygrok PN. (2012) A fatal case of ‘magic mushroom’ ingestion in a heart transplant recipient. Internal Medicine Journal 42(11): 1268–1269. [DOI] [PubMed] [Google Scholar]
- McCartney A, McGovern HT, De Foe A. (2021) Predictors of psychedelic experience: A thematic analysis. Available at: https://psyarxiv.com/5d7fc/ [DOI] [PubMed]
- McCawley EL, Brummett RE, Dana GW. (1962) Convulsions from psilocybe mushroom poisoning. Proceedings of the Western Pharmacology Society 5: 27–33. [PubMed] [Google Scholar]
- MacLean KA, Johnson MW, Griffiths RR. (2011) Mystical experiences occasioned by the hallucinogen psilocybin lead to increases in the personality domain of openness. Journal of Psychopharmacology 25(11): 1453–1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nayak S, Gukasyan N, Barrett FS, et al. (2021) Classic psychedelic coadministration with lithium, but not lamotrigine, is associated with seizures: An analysis of online psychedelic experience reports. Pharmacopsychiatry 54: 240–245. [DOI] [PubMed] [Google Scholar]
- Nicholas CR, Henriquez KM, Gassman MC, et al. (2018) High dose psilocybin is associated with positive subjective effects in healthy volunteers. Journal of Psychopharmacology 32(7): 770–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichols DE. (2016) Psychedelics. Pharmacological Reviews 68(2): 264–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutt DJ, King LA, Phillips LD. (2010) Drug harms in the UK: A multicriteria decision analysis. The Lancet 376(9752): 1558–1565. [DOI] [PubMed] [Google Scholar]
- Peden NR, Macaulay K, Bissett AF, et al. (1981) Clinical toxicology of ‘magic mushroom’ ingestion. Postgraduate Medical Journal 57(671): 543–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petranker R, Anderson T, Maier L, et al. (2020) Microdosing psychedelics: Subjective benefits and challenges, substance testing behavior, and the relevance of intention. Journal of Psychopharmacology 36: 85–96. [DOI] [PubMed] [Google Scholar]
- Riley SC, Blackman G. (2008) Between prohibitions: Patterns and meanings of magic mushroom use in the UK. Substance Use & Misuse 43(1): 55–71. [DOI] [PubMed] [Google Scholar]
- Rucker JJ, Iliff J, Nutt DJ. (2018) Psychiatry & the psychedelic drugs. Past, present & future. Neuropharmacology 142: 200–218. [DOI] [PubMed] [Google Scholar]
- Satora L, Goszcz H, Ciszowski K. (2005) Poisonings resulting from the ingestion of magic mushrooms in Kraków. Przeglad Lekarski 62(6): 394–396. [PubMed] [Google Scholar]
- Spear LP. (2000) The adolescent brain and age-related behavioral manifestations. Neuroscience & Biobehavioral Reviews 24(4): 417–463. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Albert D, Cauffman E, et al. (2008) Age differences in sensation seeking and impulsivity as indexed by behavior and self-report: Evidence for a dual systems model. Developmental Psychology 44(6): 1764. [DOI] [PubMed] [Google Scholar]
- Strassman RJ. (1984) Adverse reactions to psychedelic drugs. A review of the literature. Journal of Nervous and Mental Disease 172(10): 577–595. [DOI] [PubMed] [Google Scholar]
- Studerus E, Gamma A, Kometer M, et al. (2012) Prediction of psilocybin response in healthy volunteers. PLoS ONE 7(2): e30800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Third Wave (2015) LSD vs psilocybin mushrooms. Available at: https://thethirdwave.co/lsd-vs-shrooms/
- Van Amsterdam J, Opperhuizen A, van den Brink W. (2011) Harm potential of magic mushroom use: A review. Regulatory Toxicology and Pharmacology 59(3): 423–429. [DOI] [PubMed] [Google Scholar]
- Van Amsterdam J, Opperhuizen A, Koeter M, et al. (2010) Ranking the harm of alcohol, tobacco and illicit drugs for the individual and the population. European Addiction Research 16(4): 202–207. [DOI] [PubMed] [Google Scholar]
- Vollenweider FX, Vollenweider-Scherpenhuyzen MF, Babler A, et al. (1998) Psilocybin induces schizophrenia-like psychosis in humans via a serotonin-2 agonist action. Neuroreport 9: 3897–3902. [DOI] [PubMed] [Google Scholar]
- Williams LM, Brown KJ, Palmer D, et al. (2006) The mellow years? Neural basis of improving emotional stability over age. Journal of Neuroscience 26(24): 6422–6430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittmann M, Carter O, Hasler F, et al. (2007) Effects of psilocybin on time perception and temporal control of behaviour in humans. Journal of Psychopharmacology 21(1): 50–64. [DOI] [PubMed] [Google Scholar]
- Yaden DB, Yaden ME, Griffiths RR. (2021) Psychedelics in psychiatry – Keeping the renaissance from going off the rails. JAMA Psychiatry 78: 469–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jop-10.1177_02698811221084063 for Adverse experiences resulting in emergency medical treatment seeking following the use of magic mushrooms by Emma I Kopra, Jason A Ferris, Adam R Winstock, Allan H Young and James J Rucker in Journal of Psychopharmacology