Abstract
Background
Action observation (AO) is a physical rehabilitation approach that facilitates the occurrence of neural plasticity through the activation of the mirror‐neural system, promoting motor recovery in people with stroke.
Objectives
To assess whether AO enhances upper limb motor function in people with stroke.
Search methods
We searched the Cochrane Stroke Group Trials Register (last searched 18 May 2021), the Cochrane Central Register of Controlled Trials (18 May 2021), MEDLINE (1946 to 18 May 2021), Embase (1974 to 18 May 2021), and five additional databases. We also searched trial registries and reference lists.
Selection criteria
Randomized controlled trials (RCTs) of AO alone or associated with physical practice in adults after stroke. The primary outcome was upper limb (arm and hand) motor function. Secondary outcomes included dependence on activities of daily living (ADL), motor performance, cortical activation, quality of life, and adverse effects.
Data collection and analysis
Two review authors independently selected trials according to the predefined inclusion criteria, extracted data, assessed risk of bias using RoB 1, and applied the GRADE approach to assess the certainty of the evidence. The reviews authors contacted trial authors for clarification and missing information.
Main results
We included 16 trials involving 574 individuals. Most trials provided AO followed by the practice of motor actions. Training varied between 1 day and 8 weeks of therapy, 10 to 90 minutes per session. The time of AO ranged from 1 minute to 10 minutes for each motor action, task or movement observed. The total number of motor actions ranged from 1 to 3. Control comparisons included sham observation, physical therapy, and functional activity practice. Primary outcomes: AO improved arm function (standardized mean difference (SMD) 0.39, 95% confidence interval (CI) 0.17 to 0.61; 11 trials, 373 participants; low‐certainty evidence); and improved hand function (mean difference (MD) 2.76, 95% CI 1.04 to 4.49; 5 trials, 178 participants; low‐certainty evidence). Secondary outcomes: AO did not improve ADL performance (SMD 0.37, 95% CI ‐0.34 to 1.08; 7 trials, 302 participants; very low‐certainty evidence), or quality of life (MD 5.52, 95% CI ‐30.74 to 41.78; 2 trials, 30 participants; very low‐certainty evidence). We were unable to pool the other secondary outcomes (motor performance and cortical activation). Only two trials reported adverse events without significant adverse effects.
Authors' conclusions
The effects of AO are small for arm function compared to any control group; for hand function the effects are large, but not clinically significant. For both, the certainty of evidence is low. There is no evidence of benefit or detriment from AO on ADL and quality of life of people with stroke; however, the certainty of evidence is very low. As such, our confidence in the effect estimate is limited because it will likely change with future research.
Keywords: Adult, Humans, Activities of Daily Living, Physical Therapy Modalities, Randomized Controlled Trials as Topic, Stroke, Stroke/complications, Stroke Rehabilitation, Upper Extremity
Plain language summary
Action observation for arm rehabilitation after stroke
Review question We sought to compare the effects of action observation on arm and hand function after stroke with an alternative intervention or no intervention. In addition, we observed the effects of this therapy on upper extremity performance, everyday activities, quality of life, and activation of brain areas.
Background Individuals who survive a stroke often have difficulty moving their arms, which can lead to problems with everyday activities and reduced participation in daily situations. Action observation is a physical rehabilitation approach proposed for arm rehabilitation, in which the person with stroke observes a healthy individual performing a task, either on video or in person, followed or not by execution of the same task. This safe technique can be performed without expensive and complicated equipment and requires minimal therapist supervision. Trials show that action observation activates brain areas similar to those activated when performing the same action, and may favor movement recovery after stroke.
Trial characteristics We identified 16 trials involving 574 individuals after stroke. Most used video sequences and action observation followed by some form of motor practice, using a range of activities, with task complexity increased over the course of training or when it was easy for the participant to carry out. The evidence is current to May 2021.
Key results Trials tested whether the use of action observation compared with an alternative intervention or no intervention resulted in participants' improved ability to use their arms and hands, and found that action observation might have a small effect on arm function (11 trials) and a large effect on hand function (five trials). There is no evidence of benefit or detriment from this therapy on everyday activities and quality of life of stroke patients. It was not possible to evaluate the results of upper extremity performance and activation of brain areas.
Certainty of the evidence The certainty of the evidence was low for arm function and hand function, and very low for everyday activities and quality of life. Participants could engage in this therapy safely, since adverse events were not significant in scale or magnitude. The certainty of the evidence for each outcome was limited due to the small number of study participants, low study quality, and poor reporting of study details.
Summary of findings
Summary of findings 1. Action observation versus control: effect on upper limb rehabilitation after stroke.
| Action observation versus control: effect on upper limb rehabilitation after stroke | ||||||
| Patient or population: upper limb rehabilitation after stroke Setting: hospital, clinic, research laboratory or home Intervention: action observation Comparison: control | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (trials) | Certainty of the evidence (GRADE) | Comments | |
| Risk with control | Risk with action observation | |||||
|
Arm function assessed by: Action Research Arm Test, Fugl‐Meyer Assessment, Wolf Motor Function Test Follow‐up: range 16 to 24 weeks |
The mean arm function was 0 SD | SMD 0.39 higher (0.17 higher to 0.61 higher) | ‐ | 373 (11 RCTs) | ⊕⊕⊝⊝ Lowa,b | Action observation may result in a slight increase in arm function. |
| Hand function assessed by: Box and Block Test Follow‐up: range 12 to 20 weeks | The mean hand function was 0 | MD 2.76 higher (1.04 higher to 4.49 higher) | ‐ | 178 (5 RCTs) | ⊕⊕⊝⊝ Low a,b | Action observation may result in a slight increase in hand function. |
| Dependence on ADL assessed by: Barthel Index, Functional Independence Measure Follow‐up: range 12 to 20 weeks | The mean dependence on activities of daily living was 0 | SMD 0.37 higher (0.34 lower to 1.08 higher) | ‐ | 302 (7 RCTs) | ⊕⊝⊝⊝ Very lowa,b,c | Action observation may increase/have little to no effect on dependence on activities of daily living but the evidence is very uncertain. |
| Quality of life assessed by: Stroke Impact Scale Follow‐up: range 8 to 12 weeks | The mean quality of life was 0 | SMD 0.13 higher (1.76 lower to 2.02 higher) | ‐ | 30 (2 RCTs) | ⊕⊝⊝⊝ Very lowa,b,c | The evidence is very uncertain about the effect of action observation on quality of life. |
|
Cortical activation assessed by: fMRI, MEP, EEG |
See comment | See comment | ‐ | 102 (4 RCTs) |
‐ | Trials could not be pooled due to the variety of measures and the absence of data in some groups. |
| Motor performance assessed by: Accelerometer, 3‐dimensional motion analysis system, number of acting Follow‐up: mean 1 week | See comment | See comment | ‐ | 91 (4 RCTs) | ‐ | Trials could not be pooled due to the variety of measures. Experimental groups showed improvements in movement time, peak acceleration and number of repetitions of a task in 1 minute. |
| Adverse effects | See comment | See comment | ‐ | 16 (2 RCTs) | ‐ | Trials could not be pooled due to subjectivity of the outcome assessment |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ADL: activities of daily living; CI: confidence interval; EEG: electroencephalography; fMRI: functional magnetic resonance imaging; MD: mean difference; MEP: motor evoked potential;RCTs: randomized controlled trials; SD: standard deviation; SMD: standardized mean difference. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level due to several ratings with 'unclear' or even 'high' risk of bias in allocation concealment, incomplete outcome data, blinding of outcome assessment or selective reporting. bDowngraded one level due to small total population size (< 400). cDowngraded one level due to moderate or high heterogeneity (> 50%).
Background
Description of the condition
Stroke is considered the second most common cause of death and the leading cause of adult neurological disability, according to the Global Burden of Diseases, Injuries and Risk factors study (GBD 2017; Katan 2018). It is predicted that in 2030 there will be 70 million stroke survivors worldwide (Feigin 2014).
People who survive the initial episode exhibit long‐term motor impairment, limited functional activities, and reduced participation in daily situations (Langhorne 2011). Motor damage to the upper limb has a significant impact on quality of life (Lieshout 2020). Even 12 months after the stroke, daily use of the affected upper limb is three times less than the unaffected one (Rand 2015). In addition, sensorimotor function and paretic upper limb capacity can predict increased use of the arm and hand in daily life (Lundquist 2021). Thus, upper limb recovery after stroke is crucial for executing activities of daily living (ADL).
Description of the intervention
Motor recovery after stroke occurs due to neural plasticity mechanisms, allowing for lost functions to be regained. Some mechanisms enable the person with stroke to relearn motor skills, leading to a permanent change in motor behavior. This rehabilitation process exemplifies motor learning (Gregor 2021). A range of neurorehabilitation techniques aim to facilitate neural plasticity to compensate for functional impairments in affected people. Recovery of upper limb function after stroke has been the subject of numerous studies using different treatment techniques and modalities (Pollock 2014).
In this sense, besides the physical practice of action, alternative methods can be used without movement execution, such as through action observation (AO). The visual perception of movement performed by others can stimulate the observer's motor areas. This cortical motor facilitation maintains some specific properties of the observed action, such as the temporal structure and muscular organization (Bassolino 2015).
Considered a multisensory approach encompassing motor somatosensory and cognitive rehabilitation (Johansson 2011), this approach has demonstrated an important role in stroke motor recovery by activating the mirror‐neural system of the brain (Buccino 2014). AO forms the basis of learning through imitation and consists of one person observing the performance of a motor task, either on a video or a real demonstration (Kim 2018). For example, the stroke patient is instructed to watch a video showing an adult stretching out their hand to pick up a cup, bringing the cup to their mouth, and then returning the cup to its initial position – the act of drinking. After observing the video sequence for a time, the individuals may or may not be asked to perform the same action.
AO can be performed from different perspectives. When it is done in a first‐person perspective it involves visual information that is seen by the person performing the movement and is related to the centrality of the subjective multidimensional and multimodal experience space in one’s own body. In contrast, from a third‐person perspective, action is observed as if another person is performing it or observing themselves moving in a mirror. In both perspectives, the same brain areas are activated, but the first‐person perspective causes more extensive and stronger activation than the other (Ge 2018).
AO has been applied alone or in association with other practices, such as imitation and engagement in motor practice and training of functional activities aimed at stimulating motor relearning (Bazzini 2022; Small 2012).
How the intervention might work
There is growing evidence that motor areas (including the primary motor cortex) can be recruited not only when actions are executed, but also when they are exercised mentally or simply observed (Zhu 2019). The neurophysiological basis for this finding is the mirror‐neuron system, formed by the rostral portion of the inferior parietal lobe, pars opercularis of the inferior frontal gyrus, and ventral portion of the premotor cortex (Garrison 2010; Kemmerer 2021).
For a long time, it was believed that the motor area engagement that occurs in the real execution of the action is the same that occurs during the observation of this action (Garrison 2013). However, a meta‐analysis found consistent activations in a bilateral premotor, parietal, and sensorimotor network across AO and movement execution (Hardwick 2018). AO recruited a mainly bilateral network of premotor, parietal, and occipital regions, while movement execution spanned a mainly bilateral cortical sensorimotor network.
Despite these differences in activated areas in movement execution and AO, some areas are activated in common. Added to this, mirror‐neuron system activation, given its distribution in the brain, provides multiple access to different brain areas; thus, AO might facilitate movement execution and motor learning by facilitating the excitability of the motor system (Huntley 2018; Small 2012) even in post‐stroke patients (Tani 2018). For this reason, it is suggested that this mirror‐neuron system activation may serve as an alternative means to rearrange damaged, but not completely lost, circuits, thereby rebuilding voluntary motor function. In addition, AO would therefore induce neural plasticity in people with stroke by promoting activation of the damaged motor circuits (Garrison 2013).
Why it is important to do this review
Stroke may lead to several neurological disorders, requiring long‐term restorative and rehabilitative treatment. It is important to seek cheap and easy‐to‐apply therapies that are accessible to this population, in addition to promoting better and shorter recovery. This review is important because it involves current therapy with easy access, whose neurophysiological basis is neural plasticity, to provide evidence of its effectiveness. Given the evidence of plasticity through mirror‐neural system activation during AO, it is necessary to determine the effect of this process on the acquisition of new motor skills or relearning of lost motor skills, resulting in improved upper limb performance in people with stroke.
Motor learning is a change in an individual's ability to perform a skill. The change emerges because of motor practice and is characterized by a relatively permanent improvement in performance (Krakauer 2019; Magill 1989). Motor skill acquisition occurs in three stages (cognitive, associative, and autonomous), during which cognitive demand decreases gradually, while physical demand is constant throughout the process (Fitts 1967; Krakauer 2019). Since learning a motor skill is conceptually dependent on motor practice, the question arises as to how AO (and its different applications) influences the learning process.
Thus, this review may clarify relevant aspects on how AO should be applied to promote significant improvements in upper limb motor function, whether it should be applied separately or in association with motor practice, in which stage of stroke, and the optimum dosage to be prescribed, among other questions. To that end, experimental trials that use this approach to promote motor learning in people with stroke must be pooled and systematically reviewed. Given that randomized clinical trials provide better evidence, the results of a number of investigations on the therapy in question must be carefully assessed, to assess the effectiveness and effects of this intervention. This would assist the rehabilitation therapist's decision making when treating upper limb motor function.
Objectives
To assess whether AO enhances upper limb motor function in people with stroke.
Methods
Criteria for considering studies for this review
Types of studies
We planned to review published and unpublished randomized controlled trials (RCTs), including those published only as abstracts. We also examined cluster‐RCTs and cross‐over trials with random allocation, analyzing data from the first period. We did not include quasi‐randomized or non‐randomized trials, but rather those where random allocation was accomplished by using a random‐number generator, referring to a random‐number table, and using sequentially‐numbered opaque sealed envelopes. We accepted trials in any language and from any year.
Types of participants
We included trials whose participants were clinically diagnosed with stroke and upper limb motor deficit. Participants were 18 years or older, any gender, with any degree of stroke impairment severity, and at any stage of the condition.
Types of interventions
We selected trials that included the following interventions.
AO alone or associated with motor practice, imitation or training of functional tasks versus other therapies.
AO alone or associated with motor practice, imitation or training of functional tasks versus conventional physiotherapy.
AO alone or associated with motor practice, imitation or training of functional tasks versus placebo.
AO alone or associated with motor practice, imitation or training of functional tasks versus no therapy.
We considered AO as the observation of an individual performing a motor action through videos or in real time. We did not include trials using mirror therapy in this review.
Types of outcome measures
We extracted the outcomes of interest from the baseline and the evaluation at the end of the intervention period (short term) and follow‐up (long term). Our list of outcome measures was not exhaustive; when we found trials with other relevant outcome measures, we included them and documented these findings. Moreover, when we identified a study in which more than one measurement instrument found the same outcome, we used the one included on our list.
Primary outcomes
-
Upper limb motor function, measured by the following.
-
Arm function
Motor Assessment Scale (upper limb component)
Frenchay Arm Test
Motor Activity Log
Wolf Motor Function Test
Action Research Arm Test
Fugl‐Meyer Assessment
-
Hand function
Motor Assessment scale (hand component)
Box and Block Test
Jebsen Test of Hand Function and Peg Test
-
Secondary outcomes
-
Dependence on activities of daily living (ADL), measured by the following.
Functional Independence Measure
Barthel Index
Rankin Scale
-
Motor performance, measured by kinematic analysis, e.g.
velocity
angular analysis of movement
-
Cortical activation, measured by the following.
Functional Magnetic Resonance
Transcranial Magnetic Stimulation
Electroencephalography
Positron Emission Tomography
-
Quality of life, restricted participation, or both, measured by the following.
London Handicap Scale
36‐Item Short Form Health Survey (SF‐36)
EuroQoL 5 dimensions (EQ‐5D)
Stroke Impact Scale
-
Adverse effects
pain
muscle weakness
fatigue
death
Search methods for identification of studies
See the Cochrane Stroke Group's search methods. We searched for trials in all languages and arranged for the translation of relevant articles where necessary.
Electronic searches
We searched the Cochrane Stroke Group Trials Register and the following electronic bibliographic databases and trial registers.
Cochrane Central Register of Controlled Trials (CENTRAL; 2021, Issue 5) in the Cochrane Library (searched May 2021; Appendix 1).
MEDLINE (Ovid) (from 1946 to May 2021; Appendix 2).
Embase (Ovid) (from 1980 to May 2021; Appendix 3).
CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature (from 1982 to May 2021; Appendix 4).
LILACS (Latin American and Caribbean Health Sciences Literature to May 2021; Appendix 5).
Allied and Complementary Medicine Database (AMED) (Ovid) (from 1985 to 18 May 2021; Appendix 6).
Physiotherapy Evidence Database (PEDro: www.pedro.org.au; searched May 2021; Appendix 7)
We developed the MEDLINE search strategy with the help of the Cochrane Stroke Group Information Specialist (Appendix 2), and adapted it for the other databases (Appendix 1; Appendix 3; Appendix 4; Appendix 5; Appendix 6; Appendix 7).
We searched the following trial registries for ongoing trials.
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov; searched May 2021; Appendix 8).
ISRCTN Registry (www.isrctn.com; searched May 2021 ‐ included on WHO International Clinical Trials Registry; Appendix 9).
Australian New Zealand Clinical Trials Registry (www.anzctr.org.au; searched May 2021 ‐ included on WHO International Clinical Trials Registry; Appendix 10).
World Health Organization (WHO) International Clinical Trials Registry Platform (trialsearch.who.int/Default.aspx; searched May 2021; Appendix 11).
Searching other resources
In an effort to identify further published, unpublished and ongoing trials, we:
screened reference lists of all relevant articles;
used Science Citation Index Cited Reference search for forward tracking of important articles;
contacted trialists, experts and researchers in our field of study;
handsearched journals (International Journal of Neurorehabilitation, Neurorehabilitation and Neural Repair, and Stroke);
searched for PhD and MSc theses (using Latin American and Caribbean Health Sciences Literature: LILACS).
Data collection and analysis
Selection of studies
Two review authors (JP and IR) independently screened the titles and abstracts of records obtained from the electronic searches and excluded those that were obviously irrelevant. We obtained the full text of the remaining records and the same two review authors selected trials for inclusion according to the predefined inclusion criteria. If any methodological question raised doubts about whether the study met the inclusion criteria, we contacted the study authors for clarification. If there was disagreement regarding the selection of trials, we attempted to reach a consensus through discussion. If this was impossible, we asked another review author (TC) to decide if the study should be included. We recorded reasons for exclusion and completed a PRISMA flowchart (Page 2021).
Data extraction and management
Two review authors (AF and LB) were responsible for data extraction. To record these data, we used a form we created, based on the Cochrane Consumers and Communication Group data extraction template for included studies (Ryan 2016), which we tested (piloted) in two trials. Where there was incomplete or unclear data, we contacted the study authors for clarification. The same two review authors discussed any disagreements encountered in order to reach a consensus; and if we could not reach consensus, another review author (TC) ruled on the issue. One review author (AF) entered all extracted data into Review Manager 5 (RevMan 5) (Review Manager 2020), and another (LB) working independently checked the data to confirm accuracy. These data refer to the following.
General information: title of the review, name of the review author who completed the form, and study ID.
Methods used: objectives, study design, instruments used, study duration, type of randomisation, allocation concealment, blind assessors, inclusion and exclusion criteria, institutions or study centers involved, study site, removal and abandonment of participants, and year of the study.
Participants: population description, sample size, age, sex, initial upper limb impairment, severity level of stroke and type of stroke, diagnostic criteria, phase (acute, subacute, and chronic), presence of communication or cognitive impairments.
Intervention: therapies used in association and in comparison, type of task, number and duration of the sessions and time of the sessions, methods used in the control group, and the profession of the person that applied the therapy.
Results: primary and secondary outcomes for each assessment and reassessment, methods and instrumentation for assessment, timing of outcome assessment, and adverse events.
Notes: contact with authors (information obtained or not), article in a language other than English, study financing and noteworthy conflicts of interest of study authors.
Assessment of risk of bias in included studies
We assessed risk of bias using the RoB 1 tool described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017). Two review authors (AF and LB) independently assessed the risk of bias and discussed disagreements and, if necessary, we asked another review author (TC) to come to a conclusion. We used a form containing the following risk of bias criteria.
Random sequence generation
Allocation concealment
Blinding of participants and personnel
Blinding of outcome assessment
Incomplete outcome data
Selective outcome reporting
Other bias
We classified each criterion, characterizing it as high, low, or uncertain risk of bias. We inserted this information into the risk of bias table produced for each study, along with the reason for each decision. We used Table 8.5.d from the Cochrane Handbook for Systematic Reviews of Interventions, which provides criteria for making judgements regarding risk of bias in each of the seven domains of the tool (Higgins 2017). We contacted trial authors for clarification and to request missing information. We considered the risk of bias of the trials and their contribution to the treatment effect.
Measures of treatment effect
We measured treatment effect using mean difference (MD) and standardized mean difference (SMD) for the continuous outcomes, with 95% confidence intervals (CIs). According to Higgins 2022, if trials are clinically diverse then a meta‐analysis may be meaningless, and genuine differences in effects may be obscured. Often it is nonsensical to combine all included trials in a single meta‐analysis: if there is a mix of comparisons of different treatments with different comparators, each combination may need to be considered separately (Higgins 2022). We performed a meta‐analysis using RevMan 5 only if there was clinical and methodological similarity between trials, so that they could be pooled for analysis (Review Manager 2020). One review author (LB) conducted this judgment. In case of doubt, a third review author (TC) made the final decision. We based clinical similarity on population characteristics, such as age range, type of stroke, stroke severity, and stage of stroke (acute, subacute and chronic). We considered similar methodology when the type of intervention and outcomes (motor function, dependence of daily living, and others), even if measured by different instruments, were repeated between trials. We used the random‐effects model in our analysis.
Unit of analysis issues
Cross‐over trials
We included one cross‐over study, using only the first period for analysis.
Cluster‐randomized trials
There were no cluster‐randomized trials.
Dealing with missing data
We contacted study authors when possible to verify key study characteristics and to obtain missing numerical outcome data. When this was not possible, and the missing data were thought to introduce serious bias, we performed a sensitivity analysis to explore the impact of including such trials in the overall assessment of results.
Assessment of heterogeneity
We assessed heterogeneity visually by observing the non‐overlapping of confidence intervals (CIs) in the forest plots. Once identified, we quantified heterogeneity by the I² statistic. When heterogeneity was caused by one or two trials with peripheral results that conflicted with the rest of the trials, we carried out analyses with and without these trials as part of the sensitivity analysis. We considered values of < 30% as low heterogeneity, from 30% to 60% moderate heterogeneity, 61% to 75%, representing substantial heterogeneity, and > 75% suggestive of considerable heterogeneity (Higgins 2022).
Assessment of reporting biases
The search for clinical trials registers helped in reducing publication bias. We compared the trial registry with the included trials methods. In the absence of registration, it was observed if the outcomes evaluated were surrogate or clinically relevant. We also investigated selective outcome reporting by the comparison of the methods section of papers with the results reported. We inspected the funnel plot for arm function analysis, the only one with more than 10 trials.
Data synthesis
We conducted a meta‐analysis when the trials could be combined. The review authors used the random‐effects model. We planned to do an analysis of AO (alone or associated with motor practice) versus any other control (active or inactive control). When it was not possible to perform a meta‐analysis, we demonstrated the results with tables and a narrative synthesis, where we presented outcomes and results or objectives, according to each treatment category.
Subgroup analysis and investigation of heterogeneity
We planned to carry out the following subgroup analyses.
Age
Type of stroke
Time poststroke: acute (< 1 month poststroke), subacute (1 month and ≤ 6 months poststroke) and chronic (> 6 months poststroke)
Length of treatment period or dose of treatment
Type of treatment: AO alone and associated with motor practice (activity, imitation or training of functional tasks)
Sensitivity analysis
As previously explained, we performed sensitivity analyses when we suspected that missing data could introduce important bias, and also to assess heterogeneity caused by trials with peripheral results. Furthermore we planned to carry out the following sensitivity analyses, excluding trials with a high risk of bias. We considered a study as having a high risk of bias if the following criteria were not met.
Allocation concealment
Blinding of outcome assessment
Summary of findings and assessment of the certainty of the evidence
We created a summary of findings table including the following outcomes: upper limb motor function (arm function and hand function), dependence on ADL, quality of life, cortical activation, motor performance, and adverse effects. We used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the certainty of a body of evidence as it relates to the trials contributing data to the review for the outcomes. In particular, we downgraded the certainty of evidence by one level when trials exhibited high risk of bias, the total sample size was small (n < 400), or when heterogeneity was inexplicably moderate or high (> 50%). Two review authors (LB and TC) independently assessed the certainty of the evidence.
We used the GRADEpro Guideline Development Tool to prepare the summary of findings table (GRADEpro GDT).
Results
Description of studies
See Characteristics of included studies; Characteristics of excluded studies
Results of the search
The searches of electronic databases and trial registers produced 8145 unique references for screening. After excluding non‐relevant citations, we obtained the full texts of 109 papers; of these, we included 16 trials in the qualitative analysis and 13 trials in the quantitative analysis of the review; Figure 1 shows the study flow diagram of the selected trials.
1.
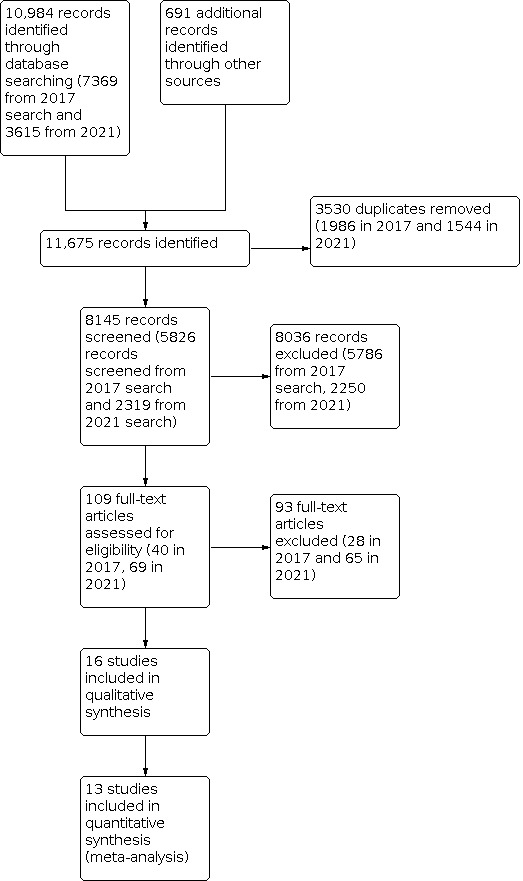
Study flow diagram
Included studies
We identified 16 randomized controlled trials (RCTs) with a total of 574 participants that met the inclusion criteria: 12 (478 participants) in the previous version (Celnik 2008; Cowles 2012; Dettmers 2014; Ertelt 2007; Franceschini 2012; Fu 2017; Harmsen 2015; Kim 2015; Kim 2016a; Kuk 2016; Lee 2013; Zhu 2015), and four (96 participants) in the updated review (Hsieh 2020; Jin‐Woo 2011; Mancuso 2021; Younghwa 2013). The trials were all randomized; one was a cross‐over trial (Celnik 2008). We contacted eight authors for clarification concerning methodology (how allocation concealment, random sequence generation, and blinding were performed) and results data; four authors replied.
We found two publications that we judged to be two reports of the same study (see study references for Franceschini 2012); while there were some differences in reported outcome measures and numbers of participants (Franceschini 2012 article with 102 participants; Sale 2012 article with 67 participants), we considered these were the same population of participants and therefore did not enter them as separate trials, since the use of duplicate data may lead to overestimating the intervention effects. We opted to use the study report with the largest sample size, considering this to provide the most comprehensive results.
Sample characteristics
We included 16 trials involving a total of 574 participants in the review. Samples ranged between nine (Celnik 2008), and 102 participants (Franceschini 2012), averaging approximately 35 participants per study. Only Kim 2015 did not characterize the sample. The mean age of participants ranged from 51.16 (±12.77) to 77.2 (±10.4) years. The sample consisted of 273 men and 208 women (Kim 2015 data not included). Seven trials included participants in the acute and/or subacute phase of stroke (Cowles 2012; Franceschini 2012; Fu 2017; Hsieh 2020; Kim 2016a; Mancuso 2021; Zhu 2015), and six in the chronic phase (Celnik 2008; Ertelt 2007; Harmsen 2015; Jin‐Woo 2011; Kuk 2016; Lee 2013). Dettmers 2014 and Younghwa 2013 included participants in the acute, subacute, and chronic phases. Initial upper limb impairment was severe (Cowles 2012; Franceschini 2012; Zhu 2015), and moderate (Ertelt 2007; Harmsen 2015; Hsieh 2020; Kim 2016a), but two trials included participants with mild, moderate, and severe paresis (Dettmers 2014; Mancuso 2021); the remaining trials did not specify initial upper limb impairment. Severity classification of upper limb impairment was performed using different instruments and methodologies, considering the Motricity Index, Fugl‐Meyer Assessment, Wolf Motor Function Test, and ability to move the upper limb.
Nine trials specified stroke etiology: two recruited only participants with ischemic stroke (Ertelt 2007; Fu 2017), and seven recruited participants with ischemic and hemorrhagic stroke (Franceschini 2012; Younghwa 2013; Harmsen 2015; Hsieh 2020; Jin‐Woo 2011; Kim 2016a; Kuk 2016). Five were carried out in a hospital setting or in rehabilitation centers (Cowles 2012; Ertelt 2007; Fu 2017; Kim 2016a; Zhu 2015); the others did not record treatment location.
Interventions
Intervention approaches
The following comparisons were used for the trials (Table 2).
1. Table of comparisons.
| Included trials | AO group | Control group |
| Celnik 2008 | 1. Congruent AO simultaneous to motor practice of thumb movements 2. Incongruent AO simultaneous to motor practice of thumb movements |
Motor practice of thumb movements |
| Cowles 2013 | Conventional physical therapy + AO with observation‐to‐imitate followed by motor practice | Conventional physical therapy |
| Dettmers 2014 | AO of typical ADL followed by motor practice (home‐based intervention) | 1. Placebo group: text observation followed by motor practice of typical ADL 2. Usual care: no specific training |
| Ertelt 2007 | AO of daily life hand and arm actions followed by motor practice | Placebo group: observation of geometric symbols and letters followed by motor practice of daily life hand and arm actions |
| Franceschini 2012 | Conventional physical therapy + AO of typical ADL followed by motor practice | Placebo group: conventional physical therapy + observation of objects followed by limb movements (exact order as experimental group) |
| Fu 2017 | Traditional rehabilitation treatment + drug treatment + action observation with observation‐to‐imitate | Traditional rehabilitation treatment + drug treatment + observation of geometric patterns and digit symbol and performed one action |
| Harmsen 2015 | AO of mirrored arm‐reaching activity from unaffected arm, alternated with affected arm‐reaching movements | Placebo group: observation of static photographs of landscapes, alternated with affected arm‐reaching movements |
| Hsieh 2020 | 1. AO of active range of motion exercises followed by motor practice 2. AO of reaching movement or one object manipulation task followed by motor practice 3. AO of one functional task (motor acts and complete action) followed by motor practice |
Motor practice of active range of motion exercises, reaching movement or object manipulation, and functional task action |
| Jin‐Woo 2011 | AO of functional tasks with objects followed by motor practice of the same movements with the objects | Motor practice of the functional task (verbally explained) |
| Kim 2015 | Occupational therapy + purposeful action observation program | Placebo group: occupational therapy + purposeful action observation program assignments without actually observing the purposeful actions |
| Kim 2016a | AO of functional tasks followed by motor practice of the same movements | Motor practice of functional tasks |
| Kuk 2016 | AO of an action similar to Box and Block test followed by motor practice of the same movements | Placebo group: observation of landscapes followed by motor practice of an action similar to Box and Block test |
| Lee 2013 | 1. AO: action observation of drinking behavior simultaneous to action imagination 2. AO + action: action observation of drinking behavior followed by motor practice |
1. Action: motor practice of drinking behavior 2. Control: no specific training |
| Mancuso 2021 | Physical therapy + AO of functional tasks followed by motor practice of the same movements | Task oriented training (verbal instructions and feedback) |
| Younghwa 2013 | AO of daily life hand and arm actions followed by motor practice | Task oriented training (verbal instructions and feedback) |
| Zhu 2015 | Physical therapy + occupational therapy + drug treatment + AO of upper limb movements followed by motor practice | Physical therapy + occupational therapy + drug treatment |
ADL: activities of daily living; AO: action observation
Participants in seven trials did not undergo physiotherapy or occupational therapy in addition to the procedures proposed for control and experimental groups (Celnik 2008; Ertelt 2007; Harmsen 2015; Jin‐Woo 2011; Kuk 2016; Lee 2013; Younghwa 2013). In all trials, AO was followed by some type of motor activity, largely functional tasks. Most of the investigations used variable practice, increasing the complexity of the tasks throughout training or when the participant demonstrated ease in carrying out the action. Constant practice of a motor activity was observed in two trials, practicing by repeating the same variant of the skill, one for upper limb reach and the other for water‐drinking action (Harmsen 2015; Lee 2013). Hsieh 2020 added to functional activities, observation and execution of upper limb range of motion exercises. In another study, after the observation, the execution of motor tasks was carrying wooden blocks from one box to another, similar to the Box and Block Test (Kuk 2016).
In one study, the individuals did not undergo functional task training but did perform thumb movements. Furthermore, the movements were carried out simultaneously to observation and considered congruent when performed in the same direction as the observed movement, and incongruent when the movement was in the opposite direction to that observed (Celnik 2008). Kim 2015 did not clearly explain whether the individuals performed the observed task after AO. However this likely occurred, since the study authors reported the experimental group as having undergone a training program ("purposeful action observation training program"), which can be understood as being some type of motor practice after the observed activity.
Comparison interventions
In some trials, the control group underwent rehabilitation treatment through conventional physical therapy and/or occupational therapy (Cowles 2013; Franceschini 2012; Fu 2017; Hsieh 2020; Kim 2015; Kim 2016a; Mancuso 2021; Zhu 2015), with or without other therapies. In all of these trials, physical therapy and occupational therapy was provided to the control and experimental group.
In Cowles 2013, the control group performed only conventional physical therapy. Some trials used activities other than conventional physical therapy (Hsieh 2020; Kim 2015; Kim 2016a; Mancuso 2021), such as the practice of functional tasks (Hsieh 2020; Kim 2015; Kim 2016a), in addition to active range of motion exercises, reaching movement or object manipulation (Hsieh 2020). Mancuso 2021 added Task‐oriented training to conventional physical. This intervention uses motor learning principles such as specificity of training, constrained use of impaired limbs, mass practice (repetition), shaping of skill, the saliency of a task, and knowledge of performance and result (Harvey 2009).
Some trials explored the content of conventional physical therapy applied. The control group in Cowles 2013 underwent soft tissue mobilization, joint mobilization, facilitating muscle activity, positioning, specific sensory input, splinting, exercise to increase strength, balance, mobility, upper limb functional tasks, and education. Franceschini 2012 used dexterity and gait training. Fu 2017 used Bobath/Brunnstrom, proprioceptive neuromuscular facilitation, and daily activity ability training. Mancuso 2021 submitted the control group to training for transfers, mobility, walking up and down steps, balance tasks, functional tasks for the upper limbs, joint and soft tissue mobilization, and specific sensory stimulation exercises to increase strength.
In two trials, patients received medication in addition to rehabilitation treatment (Fu 2017; Zhu 2015). In addition to rehabilitation, some control groups performed placebo observation plus some upper limb action or movement practice (Franceschini 2012; Fu 2017).
Placebo observation was the choice of several trials (Dettmers 2014; Ertelt 2007; Franceschini 2012; Fu 2017; Harmsen 2015; Kuk 2016). The observed content was text (Dettmers 2014), geometric symbols, letters or symbols (Ertelt 2007; Fu 2017), static images of objects (Franceschini 2012), and photographs and landscapes (Harmsen 2015; Kuk 2016). After this observation, the participants underwent some physical or motor training, such as functional activities training (Dettmers 2014; Ertelt 2007; Franceschini 2012), reach training (Harmsen 2015), upper limb movements (Fu 2017), and action training similar to Box and Block Test (Kuk 2016).
In a few trials, the control group practiced functional tasks (Jin‐Woo 2011; Lee 2013; Younghwa 2013), and specific movements, such as thumb movements (Celnik 2008). In only two trials (Dettmers 2014; Hsieh 2020), the exercises were individualized for the participants or the task was adjusted according to the participant's motor skills. In Franceschini 2012, the researcher provided physical help to support or mobilize the upper limb.
Two trials presented two control groups (Dettmers 2014; Lee 2013), one of which did not undergo specific training. To conduct the meta‐analysis, we did not use this group in order to reduce heterogeneity between trials.
Resources
The resources used to provide observation of action for the experimental group were television (TV) (Ertelt 2007; Fu 2017; Zhu 2015) and computer monitor (Harmsen 2015; Hsieh 2020; Jin‐Woo 2011; Kim 2016a; Kuk 2016; Younghwa 2013). The other authors did not specify the resource used for exposure (Celnik 2008; Cowles 2013; Dettmers 2014; Franceschini 2012; Kim 2015; Lee 2013; Mancuso 2021). Other resources used were objects, such as dish, towel, book, cup, coins, cubes, wooden blocks, clothes and others, materials used to carry out the training of tasks or functional activities, as detailed in seven trials (Ertelt 2007; Hsieh 2020; Jin‐Woo 2011; Kim 2016a; Kuk 2016; Lee 2013; Zhu 2015).
For the materials used for control groups, two trials referred to the use and manipulation of objects, such as towels, magazines, tables, drawers, bottles, and caps (Hsieh 2020; Kim 2016a). Others used more specific objects such as blocks and boxes (Kuk 2016), a cup (Lee 2013), clothes, and a wheelchair (Younghwa 2013). Another resource used was the TV or monitor (Kuk 2016) for the video presentation. The other trials did not specify the material used but reported that individuals watched videotapes and slide shows, possibly using TV or computer (Dettmers 2014; Ertelt 2007; Franceschini 2012; Fu 2017; Harmsen 2015).
Delivery
All the trials used video sequences to apply AO except Cowles 2012, which used real demonstrations of the task prescribed by the therapist, and the Kim 2015 trial, which did not report how therapy was applied. Six trials used first‐person perspective in applying AO (Celnik 2008; Cowles 2012; Franceschini 2012; Harmsen 2015; Hsieh 2020; Mancuso 2021), and three used third‐person perspective (Dettmers 2014; Fu 2017; Lee 2013). Two trials did not specify the perspective used (Kim 2015; Younghwa 2013). Other trials reported the position for the demonstration (in this case, third‐person perspective), which could be front, side, top, and back views of motor action. Kuk 2016 used two different views. Ertelt 2007, Jin‐Woo 2011, Kim 2016a; Zhu 2015 used three views.
In four trials, some type of verbal correction or feedback was provided after training in the experimental group (Cowles 2013; Franceschini 2012; Kim 2016a; Mancuso 2021). Other trials mentioned verbal instruction, explaining the motor task or movement (Franceschini 2012; Jin‐Woo 2011; Lee 2013; Mancuso 2021; Zhu 2015). In one study, the choice of activities was performed according to the physical capacity of the participants (Cowles 2013). In the Franceschini 2012 trial, the occupational therapist could offer physical help to complete the task or movement.
Two trials reported providing control therapy using video (Dettmers 2014; Harmsen 2015), and one using a slide show (Kuk 2016). Regarding the type of instruction, verbal instruction on the task or movement was used in five trials by the researchers or clinicians who applied the control intervention (Ertelt 2007; Franceschini 2012; Jin‐Woo 2011; Lee 2013; Younghwa 2013). The Younghwa 2013 trial included outcome feedback. Dettmers 2014 used textual instruction.
Setting
The clinical setting seems to have been the location of most trials, although only five reported this information. One trial carried out its research in an inpatient stroke unit (Cowles 2013), while four trials were carried out in rehabilitation centers (Ertelt 2007; Fu 2017; Kim 2016a; Zhu 2015). The Dettmers 2014 trial was carried out at the participants' home.
Amount of therapy provided
Intervention time in the experimental and control groups was 3 weeks in five trials (Cowles 2013; Ertelt 2007; Hsieh 2020; Jin‐Woo 2011; Lee 2013); 4 weeks, 5 times/week (Franceschini 2012; Kim 2016a; Mancuso 2021); 6 weeks, raging from four to six times/week (Dettmers 2014; Kim 2015; Younghwa 2013); and 8 weeks, six times/week (Fu 2017; Zhu 2015). Other trials performed the intervention in one day (Celnik 2008; Harmsen 2015; Kuk 2016).
The time of AO in the experimental group was variable between trials, ranging from a minimum of 1 minute (Cowles 2013; Kuk 2016), to a maximum of 10 minutes (Celnik 2008; Fu 2017), for each motor action, task or movement observed. The number of motor actions offered in each demonstration also varied between one (Celnik 2008; Lee 2013), two (Jin‐Woo 2011; Kim 2015; Younghwa 2013), and three (Ertelt 2007; Franceschini 2012; Mancuso 2021). Furthermore, in some trials, the observation of action was provided more than once: twice in the Ertelt 2007 trial, five times in Kuk 2016, and three times in the Hsieh 2020 and Celnik 2008 trials.
The time of one session in the experimental group lasted 10 minutes (Lee 2013), 20 minutes (Fu 2017), 30 minutes (Celnik 2008; Franceschini 2012; Jin‐Woo 2011; Kim 2015; Kim 2016a; Mancuso 2021; Younghwa 2013; Zhu 2015), 40 minutes (Ertelt 2007), and 60 minutes (Cowles 2013; Dettmers 2014; Hsieh 2020; Kuk 2016). One study did not specify the duration of the intervention (Harmsen 2015).
Training varied between 1 day and 8 weeks of therapy, with 10 to 90 minutes per session. Total treatment duration was 20 minutes in Kuk 2016, 30 minutes in Celnik 2008 and Harmsen 2015, 150 minutes in Lee 2013, 270 minutes in Jin‐Woo 2011, 600 minutes in Franceschini 2012 and Mancuso 2021, 720 minutes in Younghwa 2013, 800 minutes in Kim 2016a, 900 minutes in Cowles 2013, Kim 2015 and Hsieh 2020, 960 minutes in Fu 2017, 1440 minutes in Zhu 2015, 1620 minutes in Ertelt 2007, and 2520 minutes in Dettmers 2014. The protocol used in most of the trials divided the functional tasks into smaller parts and provided between 1 and 6 minutes of observation for each motor sequence, followed by two to six minutes of practice for the action observed. Other details regarding the intervention are presented in Table 3.
2. Action observation application to experimental group.
| Included trials | Time of AO of each motor action (min) | Time of exercise or imitation (min) of each motor action | Total AO (min) | Total exercise (min) | Total session (min) |
| Celnik 2008 | 10 | 10 | 30 | 30 | 30 |
| Cowles 2013 | 1 to 2 | 4 to 6 (2 to 4 rest) | 4 to 5 | 16 to 18 | 2 × 30‐min sessions (10 rest) |
| Dettmers 2014 | 5 + 4 after practice | Not reported | 9 | 20 | 60 |
| Ertelt 2007 | 6 | 6 | 36 | 36 | 90 |
| Franceschini 2012 | 3 | 2 | 9 | 6 | 2 × 15‐min sessions (60 rest) |
| Fu 2017 | 10 | 10 | 10 | 10 | 20 |
| Harmsen 2015 | 3 1 1 1 |
30 repetitions of reaching* 20 repetitions of reaching 20 repetitions of reaching |
6 | 60 repetitions* of reaching (time not informed) | Not reported |
| Hsieh 2020 | Phase 1: 2 to 3 Phase 2: 2 Phase 3: 2 + 2 (complete task) |
Phase 1: 2 to 4 minutes Phase 2: 3 minutes Phase 3: 3 minutes |
25 | 35 | 60 |
| Jin‐Woo 2011 | 5 | 10 | 10 | 20 | 30 |
| Kim 2015 | Not reported | Not reported | Not reported | Not reported | 30 |
| Kim 2016a | 9 (+1 to rest) | 30 | 9 | 30 | 40 |
| Kuk 2016 | 1 | 3 (10 rest) | 5 | 15 | 60 |
| Lee 2013 | 5 | 5 | 5 | 5 | 10 |
| Mancuso 2021 | 3 | 2 | 18 | 12 | 90 (60 of physical therapy and 30 of AO therapy) |
| Younghwa 2013 | 3 to 4 | 7 to 11 | 6 to 8 | 14 to 22 | 20 to 30 |
| Zhu 2015 | Not reported | Not reported | Not reported | Not reported | 30 |
Some of the trials did not provide all the values contained in the table, but based on those presented, it was possible to extrapolate the other values. AO: action observation
min: minutes *Not minutes
Session duration in the control group was 30 minutes in some trials (Celnik 2008; Franceschini 2012; Jin‐Woo 2011; Kim 2015; Kim 2016a; Mancuso 2021; Younghwa 2013). Three trials did not specify the exact duration of the session (Cowles 2013; Harmsen 2015; Zhu 2015). The others lasted: 10 minutes (Lee 2013); 20 minutes (Fu 2017; Kuk 2016); 60 minutes (Dettmers 2014); and 90 minutes (Ertelt 2007). Details on the timing of each component of control therapy are available in Table 4.
3. Interventions of control group.
| Included trials | Time of conventional physical therapy or occupational therapy/session | Time of control intervention | Session/day | Time of placebo video/session | Time of motor activity*/session |
| Celnik 2008 | Did not perform | 30 min | 1 | Did not perform | 30 min |
| Cowles 2013 | Not reported | Not reported | Not reported | Did not perform | Not reported |
| Dettmers 2014 | Did not perform | 60 min | 1 | Not reported | Not reported |
| Ertelt 2007 | Did not perform | 90 min | 1 | 36 min | 36 min |
| Franceschini 2012 | At least 3 hours/day of physiotherapy | 30 min | 2 | 9 min | 6 min |
| Fu 2017 | Not reported | 20 min | 1 | Not reported | Not reported |
| Harmsen 2015 | Did not perform | Not reported | 1 | 6 min | 70 repetitions of reaching |
| Hsieh 2020 | Not reported | 60 min | 1 | Did not perform | 60 min |
| Jin‐Woo 2011 | Did not perform | 30 min | 1 | Did not perform | 30 min |
| Kim 2015 | Not reported | 30 min | 1 | Did not perform | Not reported |
| Kim 2016a | Occupational therapy (1 hour/day) Physical therapy (2 hours/day) |
30 min | 1 | Did not perform | 30 min |
| Kuk 2016 | Did not perform | 20 min | 1 | 5 min | 15 min |
| Lee 2013 | Did not perform | 10 min | 1 | Did not perform | 10 min |
| Mancuso 2021 | 1 hour | 30 min | 1 | Did not perform | 30 min |
| Younghwa 2013 | Did not perform | 30 min | 1 | Did not perform | 30 min |
| Zhu 2015 | 2 to 5 hours | 2 to 5 hours | 1 | Did not perform | 2 to 5 hours |
*Motor activities refers to imitation, task practice, movement or functional training. min: minutes
Providers
Some authors mentioned that therapists provided the therapy without specifying the qualification or specialty of the professionals. Therefore, we used the same term as that provided by the study authors.
The professionals in charge of the control group therapy were therapists in seven trials (Cowles 2013; Ertelt 2007; Jin‐Woo 2011; Kim 2016a; Lee 2013; Mancuso 2021; Younghwa 2013), and occupational therapists in three trials (Dettmers 2014; Franceschini 2012; Hsieh 2020). Therapists applied the intervention in the experimental group in five trials (Cowles 2013; Jin‐Woo 2011; Kim 2016a; Mancuso 2021; Younghwa 2013). In three, the intervention was provided by occupational therapists (Dettmers 2014; Franceschini 2012; Hsieh 2020). In Ertelt 2007, individuals in this group were assisted by a psychologist. The remaining trials did not report who provided the intervention. One author recorded the time of professional experience of the therapist, from 5 to 8 years (Kim 2016a).
Outcomes
In relation to the outcomes used, 11 trials included upper limb motor function (Cowles 2012; Dettmers 2014; Ertelt 2007; Franceschini 2012; Fu 2017; Hsieh 2020; Jin‐Woo 2011; Kim 2015; Kim 2016a; Mancuso 2021; Zhu 2015); and only seven exhibited functional dependence for ADL as an outcome (Franceschini 2012; Fu 2017; Hsieh 2020; Kim 2016a; Mancuso 2021; Zhu 2015; Younghwa 2013). Motor performance was assessed in three trials involving several variables (Celnik 2008; Harmsen 2015; Lee 2013). Cortical activation was observed in four trials, using transcranial magnetic stimulation (TMS) (Celnik 2008; Fu 2017), functional magnetic resonance imaging (fMRI) (Ertelt 2007), and electroencephalography (EEG) (Kuk 2016).
Three trials included quality of life as an outcome (Dettmers 2014; Ertelt 2007; Hsieh 2020); one had adverse events, attention level, and fatigue as outcomes (Celnik 2008); while another monitored pain in the experimental group, but without quantifying it (Cowles 2013).
Some outcomes not foreseen in the review protocol were used. Mancuso 2021 evaluated spasticity. Jin‐Woo 2011 measured handgrip and specific pinch strength.
A number of instruments were used to quantify primary and secondary outcomes. With respect to the primary outcome (upper limb motor function), subdivided into the arm and hand, the following were used for the arm: Action Research Arm Test (Cowles 2012); Wolf Motor Function Test (Dettmers 2014; Ertelt 2007; Fu 2017; Jin‐Woo 2011; Kim 2015); Motor Activity Log (Dettmers 2014); Frenchay Arm Test (Ertelt 2007; Franceschini 2012); and Fugl‐Meyer Assessment (Franceschini 2012; Fu 2017; Kim 2016a; Hsieh 2020; Mancuso 2021; Zhu 2015). The motor function outcome of the hand was assessed by the Nine‐Hole Peg Test (Dettmers 2014), and Box and Block Test (Franceschini 2012; Hsieh 2020; Kuk 2016; Mancuso 2021).
All secondary outcomes specified in this review were present in the included trials. The following instruments were used to measure dependence in ADL: Functional Independence Measure ‐ motor items (Franceschini 2012; Hsieh 2020; Mancuso 2021), and Modified Barthel Index/Barthel Index (Fu 2017; Kim 2016a; Younghwa 2013; Zhu 2015). Motor performance, measured by kinematic analysis and an accelerometer was determined in the Celnik 2008 study, which considered angular difference, angular dispersion, and peak acceleration as measures. Harmsen 2015 also used an accelerometer to measure motor performance considering reaching time, whereas Kim 2015 considered average velocity, trajectory ratio, and motion angle, measured by a 3‐dimensional motion analysis system. In Lee 2013, the number of times the drinking task was performed in 1 minute was measured. Heterogeneity of the variables used to characterize motor performance precluded combining them in analysis and comparing them.
Cortical activation was determined by motor‐evoked potential (MEP) amplitudes, latency and center‐motion conduction time provoked by TMS (Celnik 2008; Fu 2017). Ertelt 2007 used fMRI to analyze the effects of AO. Kuk 2016 used EEG for investigating the mirror neuron system activation during AO. The Stroke Impact Scale was applied to measure quality of life (Dettmers 2014; Ertelt 2007; Hsieh 2020).
Spasticity was evaluated by the Modifed Ashworth Scale (Mancuso 2021), and handgrip strength was evaluated by manual dynamometer (Jin‐Woo 2011).
Adverse effects were quantified in one of the trials using the visual analogue scale, which focused on the level of attention and fatigue during the interventions (Celnik 2008). Other adverse effects, such as upper limb pain (overuse syndrome), were monitored for verbal or behavioral manifestations (e.g. grimacing, postural guarding), and for a decrease of at least two measurement levels in the Motricity Index, the scale that quantifies muscle weakness (Cowles 2012).
Three trials assessed the short‐term effects of AO, with assessment and reassessment on the same day (Celnik 2008; Harmsen 2015; Kuk 2016). Five trials assessed the effects after conclusion of therapy via follow‐up at 1 week (Lee 2013), 2 months (Ertelt 2007), 3 months (Hsieh 2020), 4 to 5 months (Franceschini 2012), and 6 months (Dettmers 2014). The Dettmers 2014 and Ertelt 2007 trials conducted follow‐up only for the experimental group.
Excluded studies
We excluded 25 trials for various reasons (Characteristics of excluded studies). Five trials are ongoing.
Risk of bias in included studies
Two review authors independently assessed the methodological quality of the included trials using RoB 1: see Characteristics of included studies, risk of bias summary (Figure 2), and risk of bias graph (Figure 3). Not all the trials followed CONSORT recommendations, a guideline for reporting randomized trials (Schulz 2010). For this reason, we emailed study authors for clarification in the event of questions concerning trial methodology.
2.

Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
3.

Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included trials.
Allocation
We judged random sequence generation as adequate in 10 trials (Celnik 2008; Cowles 2013; Franceschini 2012; Fu 2017; Harmsen 2015; Hsieh 2020; Kim 2016a; Kuk 2016; Mancuso 2021; Zhu 2015), while the other six exhibited unclear risk of bias for this criterion (Dettmers 2014; Ertelt 2007; Jin‐Woo 2011; Kim 2015; Lee 2013; Younghwa 2013).
Five of the 16 trials appropriately described the allocation concealment of participants to groups and we deemed these to be at low risk (Cowles 2013; Franceschini 2012; Hsieh 2020; Kim 2016a; Mancuso 2021); we considered only two trials at high risk (Fu 2017; Zhu 2015).
Blinding
No trials were able to blind participants or personnel. However, this type of blinding is impossible to apply with this therapy, and since therapist and participant were aware of the treatment they were performing, we considered there to be low potential to negatively influence the effect of the therapy and, therefore, judged them to be at low risk of bias.
Nine trials reported blinding the outcome assessor (Celnik 2008; Cowles 2013; Franceschini 2012; Fu 2017; Hsieh 2020; Kim 2016a; Lee 2013; Mancuso 2021; Zhu 2015); we considered the other trials to be at unclear risk of bias.
Incomplete outcome data
We deemed 13 trials to have low risk of bias in relation to this criterion (Cowles 2013; Dettmers 2014; Ertelt 2007; Harmsen 2015; Hsieh 2020; Jin‐Woo 2011; Kim 2015; Kim 2016a; Kuk 2016; Lee 2013; Mancuso 2021; Younghwa 2013; Zhu 2015), and considered three at high risk due to an imbalance in the number of participants in each group considered for analysis as well as the amount of losses in the sample (Celnik 2008; Franceschini 2012; Fu 2017).
Selective reporting
Three trials exhibited a high risk of selective reporting: Cowles 2013 and Hsieh 2020 did not include all outcomes and questionnaires provided in the trial registry, and Dettmers 2014 did not include data from a relevant questionnaire at follow‐up. We considered one study to be unclear (Lee 2013). The remaining 12 were at low risk of bias: five were recorded on trial registry sites and followed their registered protocol; the others had no trial record, but the outcomes were clinically relevant for the population.
Other potential sources of bias
Fifteen trials were free of other potential sources of bias and we considered these to be at low risk. We considered one study to be at high risk of bias (Kim 2015), related to the lack of clarity about outcome assessment time.
We evaluated funnel plots for Analysis 1.1, for arm function outcome. The graph appears slightly asymmetrical, with a greater concentration of trials in the center and top of the graph. Publication bias can lead to asymmetry. Some articles may not have been found in the search strategy used. In addition, as only seven trials had a study record, it may be that non‐significant results of some outcomes were not published by included trials that did not have a study registry. Furthermore, poor methodological quality can lead to spuriously inflated effects in smaller trials (Higgins 2022; Figure 4).
1.1. Analysis.

Comparison 1: Action observation versus control: effect on arm function, Outcome 1: Arm function
4.

Funnel plot of comparison: 1 Action observation therapy versus control: effect on arm function, outcome: Analysis 1.1. Arm function.
Effects of interventions
See: Table 1
See Table 1.
We could use data from 13 trials in meta‐analysis (Cowles 2013; Dettmers 2014; Ertelt 2007; Franceschini 2012; Fu 2017; Hsieh 2020; Jin‐Woo 2011; Kim 2015; Kim 2016a; Kuk 2016; Mancuso 2021; Younghwa 2013; Zhu 2015). The remaining trials evaluated parameters from the same outcome that were not comparable to each other in meta‐analysis (Celnik 2008; Harmsen 2015; Lee 2013).
Action observation versus control: effect on arm function
1.1 Arm function
Eleven trials (373 participants) provided postintervention assessment data for arm motor function (Cowles 2013; Dettmers 2014; Ertelt 2007; Fu 2017; Hsieh 2020; Jin‐Woo 2011; Kim 2015; Kim 2016a; Franceschini 2012; Mancuso 2021; Zhu 2015). Dettmers 2014 used two scales to assess upper limb motor function: Motor Activity Log and Wolf Motor Function Test. We could only use the Wolf Motor Function Test data (the only data provided by the study authors) for meta‐analysis. Ertelt 2007 used the measure of time for the Wolf Motor Function Test (lower values indicate better motor function), explaining the negative value in the analysis. We opted to use the Wolf Motor Function Test data instead of the Frenchay Arm Test because the first assesses upper limb motor function using 15 functional tasks (measuring the time to perform activities) and the score ranges from 0 to 30. The Frenchay Arm Test contains fewer tasks (5) and displays a lower range of scores (total score varies from 0 to 5).
Data used for meta‐analysis of this outcome refer to Action Research Arm Test (Cowles 2013), Wolf Motor Function Test (Jin‐Woo 2011; Kim 2015; Mancuso 2021), and Fugl‐Meyer Assessment (Franceschini 2012; Fu 2017; Hsieh 2020; Kim 2016a; Zhu 2015).
In the meta‐analysis, the impact of AO on arm function showed a small effect (standardised mean difference (SMD) 0.39, 95% confidence interval (CI) 0.17 to 0.61; P < 0.001, I² = 6%; 11 trials, 373 participants; low‐certainty evidence; Analysis 1.1).
1.2 Subgroup analysis: age
We analyzed the subgroups considering the mean age of the study participants. We compared trials in which the mean age was ≥ 60 years (5 trials, 210 participants) with those in which participants were < 60 years (6 trials, 163 participants). There was no difference between the groups (P = 0.95, I² = 0%; Analysis 1.2).
1.2. Analysis.

Comparison 1: Action observation versus control: effect on arm function, Outcome 2: Subgroup analysis: age
1.3 Subgroup analysis: type of stroke
We compared trials in which the sample consisted only of participants diagnosed with ischemic stroke (3 trials, 101 participants) to others with samples of participants with either ischemic or hemorrhagic stroke (4 trials, 139 participants), and with a group containing trials in which the study authors did not specify the type of stroke (4 trials, 133 participants). There was no difference between the groups (P = 0.32, I² = 12.7%; Analysis 1.3).
1.3. Analysis.

Comparison 1: Action observation versus control: effect on arm function, Outcome 3: Subgroup analysis: type of stroke
1.4 Subgroup analysis: time poststroke
We conducted subgroup analyses between trials that recruited participants in the acute or subacute (6 trials, 280 participants), chronic phases (3 trials, 43 participants), and those with any phase of the condition (1 trial, 38 participants). There was no intergroup difference (P = 0.74, I² = 0%; Analysis 1.4).
1.4. Analysis.

Comparison 1: Action observation versus control: effect on arm function, Outcome 4: Subgroup analysis: time poststroke
1.5 Subgroup analysis: treatment dose
We compared trials that provided ≥ 1000 minutes (5 trials, 161 participants) and < 1000 minutes of therapy (6 trials, 103 participants), and observed no intergroup difference (P = 0.55, I² = 0%; Analysis 1.5).
1.5. Analysis.

Comparison 1: Action observation versus control: effect on arm function, Outcome 5: Subgroup analysis: treatment dose
1.6 Subgroup analysis: type of control group
Concerning the groups used to compare AO, six trials (231 participants) compared this therapy with placebo — that is, the participants watched images of geometric figures and texts, among others (Dettmers 2014; Ertelt 2007; Franceschini 2012; Fu 2017; Kim 2015; Kim 2016a). Two trials (83 participants) used conventional physiotherapy for comparison purposes (Cowles 2012; Zhu 2015), and one compared AO only with movements like those performed in the experimental group (Celnik 2008). Three trials (59 participants) used observed functional activity practice (Hsieh 2020; Jin‐Woo 2011; Mancuso 2021). Thus, we decided to conduct subgroup analysis, comparing the types of control groups used. There was no intergroup difference (P = 0.57, I² = 0%; Analysis 1.6).
1.6. Analysis.

Comparison 1: Action observation versus control: effect on arm function, Outcome 6: Subgroup analysis: type of control group
Regarding the definition of the categories of control groups, we used the same terminology reported by study authors. Some study authors did not describe the conventional physical therapy protocol used. Furthermore, conventional physical therapy is a more global approach. The practice of the functional activity previously observed is more specific and, when used in the control group, makes this group more similar compared to the experimental group. Therefore, we chose to use different terms for conventional physical therapy and the observed functional activity practice.
1.7 Subgroup analysis: duration of observation
We compared trials that provided > 3 minutes of observation for each motor action (5 trials, 142 participants) with those that provided ≤ 3 minutes (4 trials, 158 participants). We observed a difference between the groups (P = 0.04, I² = 75.3%). Trials providing > 3 minutes of intervention had a greater effect on upper limb function (Analysis 1.7).
1.7. Analysis.

Comparison 1: Action observation versus control: effect on arm function, Outcome 7: Subgroup analysis: duration of observation
1.8. Subgroup analysis: upper limb impairment
We performed a subgroup analysis considering upper limb impairment. We compared three groups: trials that included individuals with severe upper limb impairment (3 trials, 173 participants), trials composed of individuals with moderate upper limb impairment (3 trials, 52 participants), and those that included individuals with mild, moderate, and severe upper limb impairment (2 trials, 70 participants). The test for subgroup differences did not indicate significance (P = 0.35, I² = 5.5%).
Arm function ‒ sensitivity analyses: without high risk of bias for allocation concealment
Two trials showed a high risk of bias for arm function, considering the allocation concealment criterion (Fu 2017; Zhu 2015). Thus we performed sensitivity analysis, considering this bias, as proposed in the protocol. The effect increased (SMD 0.46, 95% CI 0.15 to 0.76; P < 0.001, I2 = 27%; 9 trials, 268 participants; Table 5).
4. Arm function ‐ sensitivity analysis.
| Sensitivity analysis conducted | Trials included in analysis | Number of trials | Number of participants | Effect size | I2 |
| Without high risk of bias for allocation concealment |
Cowles 2013; Dettmers 2014; Ertelt 2007; Franceschini 2012; Hsieh 2020; Jin‐Woo 2011; Kim 2015; Kim 2016a; Mancuso 2021 |
9 | 268 | SMD 0.46, 95% CI 0.15 to 0.76, P < 0.001 |
27% |
| Without high risk of bias for incomplete outcome data |
Ertelt 2007; Jin‐Woo 2011; Kim 2016a; Mancuso 2021 |
4 | 83 | SMD 0.88, 95% CI 0.39 to 1.36, P < 0.001 | 8% |
| Home‐based action observation training (video‐therapy) | Cowles 2013; Ertelt 2007; Franceschini 2012; Fu 2017; Hsieh 2020; Jin‐Woo 2011; Kim 2015; Kim 2016a; Mancuso 2021; Zhu 2015 | 10 | 335 | SMD 0.41, 95% CI 0.16 to 0.66, P = 0.001 | 16% |
| Real demonstration | Dettmers 2014; Ertelt 2007; Franceschini 2012; Fu 2017; Hsieh 2020; Jin‐Woo 2011; Kim 2015; Kim 2016a; Mancuso 2021; Zhu 2015 | 10 | 351 | SMD 0.42, 95% CI 0.18 to 0.66, P < 0.001 | 13% |
CI: confidence interval; SMD: standardized mean difference
Arm function ‒ sensitivity analysis: without high risk of bias for incomplete outcome data
Additionally, two trials exhibited high risk of bias for incomplete outcome data (Franceschini 2012; Fu 2017), three for selective reporting (Cowles 2013; Dettmers 2014; Hsieh 2020), and one for other bias (Kim 2015). Thus we carried out sensitivity analysis to determine whether the effect of AO was influenced by these biases (including allocation concealment), and the effect increased (SMD 0.88, 95% CI 0.39 to 1.36; P < 0.001, I2 = 8%; 5 trials, 142 participants; Table 5).
Arm function ‒ sensitivity analysis: home‐based AO training (video therapy)
We conducted another sensitivity analysis excluding only Dettmers 2014, since it used a different methodology. In this study, treatment occurred at the participant's home (home‐based AO training with video therapy), without researcher supervision. Effect size increased slightly (SMD 0.41, 95% CI 0.16 to 0.66; P = 0.001, I2 = 16%; 10 trials, 335 participants; Table 5).
Arm function ‒ sensitivity analysis: real demonstration
Cowles 2013 was the only study in which AO was demonstrated live and not via video presentation. We conducted sensitivity analysis excluding this study to observe whether there was a change in effect size, noting a slight increase from 0.39 to 0.42 (SMD 0.42, 95% CI 0.18 to 0.66, P < 0.001, I2 = 13%; 10 trials, 351 participants; Table 5).
1.9 Arm function follow‐up
Four trials assessed the lasting effects of therapy on upper limb function at follow‐up (Dettmers 2014; Ertelt 2007; Franceschini 2012; Hsieh 2020). However, two trials were not included in meta‐analysis as they assessed only the experimental group (Dettmers 2014; Ertelt 2007).
In the Dettmers 2014 study, follow‐up was carried out 6 months after the end of treatment using questionnaires (Motor Activity Log and Wolf Motor Function Test) only for the group submitted to AO (video and placebo groups). Participants from the conventional care group could not be included in follow‐up analysis. Fourteen of 18 participants from the video group (AO) and 11 of 18 from the text group maintained their gains in quality and extent of movement, as measured by Motor Activity Log. Study authors did not record Wolf Motor Function Test data in follow‐up.
Ertelt 2007 applied two scales in the follow‐up, 8 weeks after treatment: Wolf Motor Function Test and Frenchay Arm Test. A comparison between the results of these clinical scales at the end of treatment and at follow‐up in a subgroup of seven participants (experimental) showed no decline in clinical status (P = 0.63 for Wolf Motor Function Test; P = 1 for Frenchay Arm Test).
Franceschini 2012 conducted follow‐up 4 to 5 months after treatment, and Hsieh 2020, 3 months. Both used Fugl‐Meyer Assessment and were included in a meta‐analysis with 93 participants. There was no effect of AO in follow‐up (MD 1.06, 95% CI ‐8.38 to 10.50, P = 0.83, I² = 17%; 2 trials, 93 participants; Analysis 1.9).
1.9. Analysis.

Comparison 1: Action observation versus control: effect on arm function, Outcome 9: Arm function follow‐up
Action observation versus control: effect on hand function
2.1 Hand function
Six trials assessed motor hand function after intervention (Dettmers 2014; Franceschini 2012; Hsieh 2020; Kim 2016a; Kuk 2016; Mancuso 2021), but Dettmers 2014 presented the data in graphs, making it difficult to establish the average and standard deviation (SD) and, even after contacting the author, we could not obtain the data related to this outcome.
We pooled the data presented by five study authors (Franceschini 2012; Hsieh 2020; Kim 2016a; Kuk 2016; Mancuso 2021; 178 participants). All used the Box and Block Test to assess this outcome. The impact of AO on hand function showed a large effect (mean difference (MD 2.76, 95% CI 1.04 to 4.49; P < 0.001, I² = 0%; 5 trials, 178 participants; low‐certainty evidence; Analysis 2.1).
2.1. Analysis.

Comparison 2: Action observation versus control: effect on hand function, Outcome 1: Hand function
2.2 Subgroup analysis: age
In subgroup analysis considering age, there was no intergroup difference between patients with a mean age ≥ 60 years (2 trials, 122 participants) with those in which participants were < 60 years (3 trials, 56 participants) (P = 0.94, I² = 0%; Analysis 2.2).
2.2. Analysis.

Comparison 2: Action observation versus control: effect on hand function, Outcome 2: Subgroup analysis: age
2.3 Subgroup analysis: time poststroke
In subgroup analysis of the effect of therapy on hand function, there was no intergroup difference in stroke phases: acute/subacute (3 trials, 144 participants) and chronic phase (2 trials, 34 participants) (P = 0.77, I² = 0%; Analysis 2.3).
2.3. Analysis.

Comparison 2: Action observation versus control: effect on hand function, Outcome 3: Subgroup analysis: time poststroke
2.4 Subgroup analysis: duration of observation
Regarding the duration of observation, there was no difference between subgroups that provided > 3 minutes of observation for each motor action (1 trial, 22 participants) with those that provided ≤ 3 minutes (4 trials, 156 participants) (P = 0.71, I² = 0%; Analysis 2.4).
2.4. Analysis.

Comparison 2: Action observation versus control: effect on hand function, Outcome 4: Subgroup analysis: duration of observation
Hand function ‒ sensitivity analysis: without high risk of bias for incomplete outcome data
We conducted sensitivity analysis for hand function, disregarding Franceschini 2012, which showed high risk of bias for incomplete outcome data. The effect of therapy decreased (MD 2.59, 95% CI 0.81 to 4.37; P < 0.001, I² = 0%; 4 trials, 88 participants; Table 6).
5. Hand function ‐ sensitivity analysis.
| Sensitivity analysis conducted | Trials included in analysis | Number of trials | Number of participants | Effect size | I2 |
| Without high risk of bias for incomplete outcome data |
Hsieh 2020; Kim 2016a; Kuk 2016; Mancuso 2021 |
4 | 88 | MD 2.59, 95% CI 0.81 to 4.37, P < 0.001 | 0% |
| Without high risk of bias for selective reporting |
Kim 2016a; Kuk 2016; Mancuso 2021 | 3 | 74 | MD 2.61, 95% CI 0.81, 4.41, P < 0.001 | 0% |
CI: confidence interval; MD: mean difference
Hand function ‒ sensitivity analysis: without high risk of bias for selective reporting
We performed another sensitivity analysis for hand function excluding Hsieh 2020, which showed high risk of bias for selective reporting and Franceschini 2012, which exhibited high risk of bias for incomplete outcome data. The effect of therapy decreased (MD 2.61, 95% CI 0.81, 4.41; P < 0.001, I² = 0%; 3 trials, 76 participants; Table 6).
2.5 Hand function ‒ follow‐up
Two trials with 93 participants examined the effects of AO on hand function at the end of the follow‐up, 4 months to 5 months (Franceschini 2012), and 3 months after the intervention (Hsieh 2020). This analysis reported no evidence of effect of AO on hand function in follow‐up (MD 5.19, 95% CI ‐1.82 to 12.21; P = 0.15, I² = 0%).
Action observation versus control: effect on ADL
3.1 Dependence on ADL
Seven trials (302 participants) presented dependence in ADL as an outcome using different scales: Functional Independence Measure (Franceschini 2012; Hsieh 2020; Mancuso 2021); Modified Barthel Index (Fu 2017; Kim 2016a; Younghwa 2013); and Barthel Index (Zhu 2015). There was no effect: SMD 0.37, 95% CI ‐0.34 to 1.08; P = 0.31, I² = 87%; very low‐certainty evidence; Analysis 3.1).
3.1. Analysis.

Comparison 3: Action observation versus control: effect on ADL, Outcome 1: Dependence on ADL
3.2 Subgroup analysis: age
There was no difference in subgroup analysis, considering the mean age of ≥ 60 years (4 trials, 205 participants) or < 60 years (3 trials, 97 participants) (P = 0.50, I² = 0%; Analysis 3.2).
3.2. Analysis.

Comparison 3: Action observation versus control: effect on ADL, Outcome 2: Subgroup analysis: age
3.3 Subgroup analysis: type of stroke
Subgroup analysis did not find any difference between subgroups of patients with ischemic stroke (2 trials, 85 participants) and subgroups with ischemic and hemorrhagic stroke (4 trials, 156 participants) (P = 0.21; I² = 35.9%; Analysis 3.3).
3.3. Analysis.

Comparison 3: Action observation versus control: effect on ADL, Outcome 3: Subgroup analysis: type of stroke
3.4 Subgroup analysis: time poststroke
There was a difference in subgroup analysis regarding post‐stroke time, considering the acute/subacute (5 trials, 258 participants) and chronic phase subgroups (2 trials, 44 participants). Patients in the acute/subacute phase had a greater impact of AO on the dependence on ADL; however, with considerable heterogeneity (SMD, 0.85, 95% CI 0.23 to 1.46, P < 0.001, I² = 91.2%; Analysis 3.4).
3.4. Analysis.

Comparison 3: Action observation versus control: effect on ADL, Outcome 4: Subgroup analysis: time poststroke
3.5 Subgroup analysis: treatment dose
The comparison between patients who underwent ≥ 1000 minutes (3 trials, 107 participants) and < 1000 minutes of therapy (4 trials, 195 participants) was not significant for this outcome (P = 0.85, I² = 0%; Analysis 3.5).
3.5. Analysis.

Comparison 3: Action observation versus control: effect on ADL, Outcome 5: Subgroup analysis: treatment dose
3.6 Subgroup analysis: type of control group
Three subgroups were considered to analyze the types of control groups: placebo (3 trials, 165 participants); conventional physical therapy (1 trial, 61 participants); and observed functional activity practice, including task‐oriented training, range of motion exercises, reaching, and object manipulation (3 trials, 76 participants). In Mancuso 2021, the control and experimental groups underwent conventional physical therapy; thus, this study was classified in the functional activities subgroup. There was no difference between the three subgroups (P = 0.29, I² = 20%).
3.7 Subgroup analysis: duration of observation
We compared trials that provided > 3 minutes of observation for each motor action (3 trials, 105 participants) with those that provided ≤ 3 minutes (3 trials, 136 participants). There was no difference (P = 0.70, I² = 0%; Analysis 3.7).
3.7. Analysis.

Comparison 3: Action observation versus control: effect on ADL, Outcome 7: Subgroup analysis: duration of observation
3.8 Subgroup analysis: upper limb impairment
Subgroup analysis found no difference between groups of patients with 1) severe impairment (2 trials, 151 participants ), 2) moderate impairment (2 trials, 36 participants), and 3) mild, moderate, and severe upper limb impairment (1 trial, 32 participants) (P = 0.22; I² = 34.6%; Analysis 3.6).
3.6. Analysis.

Comparison 3: Action observation versus control: effect on ADL, Outcome 6: Subgroup analysis: type of control group
Sensitivity analysis: without high risk of bias for allocation concealment
We performed sensitivity analysis for the dependence on ADL outcome, excluding trials with a high risk for allocation concealment (Fu 2017; Zhu 2015). The effect of the therapy increased (SMD 0.24, 95% CI ‐0.85 to 1.32; P = 0.67, I² = 90%; 5 trials, 188 participants; Table 7).
6. Dependence on ADL ‐ sensitivity analysis.
| Sensitivity analysis conducted | Trials included in analysis | Number of trials | Number of participants | Effect size | I2 |
| Without high risk of bias for allocation concealment | Franceschini 2012; Hsieh 2020; Kim 2016a; Mancuso 2021; Younghwa 2013 | 5 | 188 | SMD 0.24, 95% CI ‐0.85 to 1.32, P = 0.67 | 90% |
| Without high risk of bias for incomplete outcome data | Kim 2016a; Mancuso 2021; Younghwa 2013; Zhu 2015 | 4 | 145 | SMD 0.52, 95% CI ‐0.82 to 1.86, P = 0.45 | 92% |
| Removing peripheral trials | Franceschini 2012; Hsieh 2020; Zhu 2015 | 3 | 165 | SMD 0.13, 95% CI ‐0.25 to 0.51, P = 0.51 | 26% |
CI: confidence interval; SMD: standardized mean difference
Sensitivity analysis: without high risk of bias for incomplete outcome data
Two trials that assessed this outcome exhibited high risk of bias for incomplete outcome data (Franceschini 2012; Fu 2017) and one for selective reporting (Hsieh 2020). We carried out sensitivity analysis and observed that the effect of therapy increased (SMD 0.52, 95% CI ‐0.82 to 1.86; P = 0.452, I² = 92%; 4 trials, 145 participants; Table 7).
Sensitivity analysis: removing peripheral trials
In meta‐analysis related to this outcome, CIs did not overlap on the forest plots, which were quantified, showing considerable heterogeneity (I² = 87%). After removing the peripheral trials, heterogeneity decreased, becoming low (I² = 26%); however, no effect of therapy was observed (SMD 0.13, 95% CI ‐0.25 to 0.51; P = 0.51, I² = 26%; 3 trials, 165 participant; Table 7).
3.9 Dependence on ADL ‒ follow‐up
Two trials conducted a follow‐up for this outcome with 93 participants (Franceschini 2012; Hsieh 2020). There was no evidence of effect from the intervention (MD ‐0.77, 95% CI ‐5.43 to 3.88; P = 0.74; I² = 0%; Analysis 3.9).
3.9. Analysis.

Comparison 3: Action observation versus control: effect on ADL, Outcome 9: Dependence on ADL follow‐up
Action observation versus control: effect on motor performance
Three trials assessed motor performance (83 participants), but the fact that different kinematic variables were used precluded comparing them in analysis. One study assessed motor performance using the variable 'movement time' and was the only one that used the patient to make the video. Reaching movements from the unaffected arm were videotaped and mirrored. Thus, the filming and video demonstration methodology resembled the mirror therapy protocols. The authors found that the decrease in movement time was significantly more for the AO group compared with the control group (P = 0.026) (Harmsen 2015).
In Kim 2015, average velocity, trajectory ratio, and motion angle were the variables selected to measure the kinematic patterns of the upper limb before and after therapy. There was an improvement between pre and postintervention average velocity and trajectory ratio values in the experimental group. However, there was no intergroup difference.
One study assessed the number of times the drinking task was performed in 1 minute (Lee 2013). The experimental group watched a video of the task, the motor practice group performed the action, the combined group watched a video of the task and performed the action, and the control group performed neither AO nor physical execution. After the intervention, the number of drinking motions increased the most in the combination group.
Action observation versus control: effect on cortical activation
Four trials evaluated cortical activation after AO. Ertelt 2007 applied fMRI to analyze the effects of AO on motor system reorganization, using an independent sensorimotor task consisting of handling an object. The control group (placebo observation followed by hand and arm movements) showed practically no change in brain activity between pretest and post‐test treatment. By contrast, the experimental group exhibited numerous differences between pretreatment and post‐treatment brain activations on sensorimotor network (supplementary motor area, bilateral ventral premotor cortex, bilateral superior and inferior parietal areas, and bilateral cerebellum).
Celnik 2008 measured motor cortical excitability, recording the MEP amplitudes of muscles mediating movements in the trained (MEP agonist) and baseline (MEP antagonist) directions. The authors used two approaches to observe the action to be performed later: congruent (same direction) and incongruent (opposite direction). At postintervention, the MEP agonist showed a slight increase while the MEP antagonist decreased for the congruent group. This difference in excitability is reflected by a change in the MEP post/preintervention ratio. Thus the study authors found that observing another participant performing training motions in the same direction and in phase with physically trained individuals enhanced motor memory formation compared with physical training alone.
One study used the evaluation of MEP, which was determined using a transcranial magnetic stimulator (Fu 2017). The study author calculated latency, amplitude, and central motor conduction time (CMCT ‐ difference between cortex and spinal latency), finding an increase in amplitude and decrease in latency and CMCT. These changes were higher in the experimental than in the control group.
The MEP results reported by Celnik 2008 and Fu 2017 could not be pooled in meta‐analysis, because data from the first period of the cross‐over were not available for this outcome in the Celnik 2008 study.
Kuk 2016 analyzed cortical activation using EEG data from poststroke participants, only in the experimental group, in each session of AO, while they were watching the video clip. Sequential executions of the observed action after AO were not EEG‐monitored. The results revealed selective activation of the mirror‐neuron system, with the middle frontal gyrus less active.
Action observation versus control: effect on quality of life
4.1 Quality of life
Quality of life was assessed in three trials (30 participants) using the Stroke Impact Scale. We were unable to obtain data (mean and SD) from the Dettmers 2014 study to carry out analysis. However, the video group (video AO) improved on Stroke Impact Scale score (P < 0.001) from pre to post‐treatment. We conducted a meta‐analysis with the remaining two trials (Ertelt 2007; Hsieh 2020), with no evidence of benefit or detriment from the intervention (MD 5.52, 95% CI ‐30.74 to 41.78; P = 0.77, I² = 88%; very low‐certainty evidence; Analysis 4.1).
4.1. Analysis.

Comparison 4: Action observation versus control: effect on quality of life, Outcome 1: Quality of life
4.2 Quality of life follow‐up
In the Dettmers 2014 study, 14 of 18 participants from the video group and 11 of 18 from the text group completed the questionnaires after 6 months. Quality of life subjective self‐assessment improved further in the video group, but not in the text group (P value not reported).
Ertelt 2007 assessed the long‐term effects of AO only in the experimental group (seven participants). Follow‐up was conducted 8 weeks after the intervention and comparisons between the results at the end of treatment and at follow‐up in the subgroup of seven participants showed no decline in clinical status (P = 0.73).
In the Hsieh 2020 study, at 3‐month follow‐up, Stroke Impact Scale scores had been maintained in both groups, indicating retention effects.
Action observation versus control: adverse effects
This outcome was investigated in two trials (16 participants). The visual analogue scale was used in the Celnik 2008 trial to measure attention and fatigue levels, with scores varying from 1 to 7, where 1 equaled the worst response and 7 equaled the best response (least fatigue or best attention). The author reported that attention and fatigue level did not influence the findings, since there was no difference between attention (P = 0.17) or fatigue scores (P = 0.40) during the different intervention sessions. One participant did not conclude the experimental protocol due to a headache caused by TMS, not by the therapy.
In the Cowles 2012 study, participants were monitored during the experiment in order to detect the overuse syndrome. To that end participant accounts of upper limb pain — either verbal or behavioral, (e.g. grimacing, postural guarding) — and decreases of at least 2 measurement levels in the Motricity Index were recorded. No adverse events occurred in either group. Both groups (AO followed by motor practice and conventional physiotherapy) improved their Motricity Index score between baseline and outcome, but there was no intergroup difference.
Discussion
Summary of main results
The aim of this review was to evaluate the effect of AO on motor function and upper limb motor performance in poststroke patients. We included 16 trials with 574 participants in this review. Overall, the certainty of the evidence for outcomes was low to very low. The main results are presented in Table 1.
Overall, AO increased the arm function of individuals after stroke compared with other physiotherapy interventions or placebo. However, the effect size is small, and, considering the certainty of the GRADE evidence, AO may improve the arm motor function of patients with stroke (low certainty). The gain in arm motor function at the end of AO did not persist at follow‐up. We performed arm function analysis using multiple instruments. Accordingly, we were unable to consider the clinically‐important difference for this outcome.
Furthermore, the effect of therapy was not influenced by issues such as age, type of stroke, poststroke time, treatment dose, and type of control group. The evidence suggests that AO results in little to no difference in arm motor function in subgroups considering upper limb impairment. The use of > 3 minutes of observation, the supervision of a therapist/researcher, and the observation of a video presentation (not a real demonstration) increased the effect of the intervention.
The effect of AO on hand function was large. However, it does not appear to be clinically relevant, given that the minimum detectable difference is six blocks/minute for the Box and Block Test (Chen 2009). Furthermore, the evidence was considered low according to GRADE, that is, our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. The effect does not appear to be influenced by issues related to the stroke or the intervention.
There was no effect of AO on the performance of ADL when compared to control groups. According to GRADE, we considered the certainty of the evidence to be very low that AO may not improve this outcome in stroke patients. However, this therapy has a higher impact on patients in the acute/subacute phases in performing ADL, although with considerable heterogeneity. Younghwa 2013 results may have caused considerable heterogeneity because the control group protocol included aspects not addressed in the experimental group. These aspects are associated with larger effect sizes, such as distributed practice, feedback, random practice, and the use of clear functional goals (Timmermans 2010). The motor practice of the experimental group could address these aspects. Then, we can say that there was a discrepancy between the protocols used in the control and experimental groups. We observed no difference in the effect of AO on the performance of ADL considering upper limb impairment. That is, the fact that it is an applicable therapy for patients with a severe upper limb impairment will not necessarily promote the motor and functional improvement of this individual.
Only two trials were included in the quality of life meta‐analysis. There was no effect but considerable heterogeneity. According to GRADE, there is no evidence of benefit or detriment from AO in the quality of life of stroke patients.
We were unable to pool the results of motor performance, cortical activation, and adverse effects.
Despite being the outcome of a number of trials, the variables selected to measure motor performance were different between trials precluding intergroup comparison performing the meta‐analysis. A decline in movement time and rise in the number of drinking tasks completed in 1 minute were the motor performance gains obtained by the AO compared to control therapies. The following variables did not improve in the experimental intervention: average velocity, trajectory ratio, motion angle, angular difference, and angular dispersion. Despite the positive findings for some of the variables, there is not enough evidence to confirm that AO has an effect on motor performance.
Considering cortical activation and changes in the nervous system, trials demonstrated that AO: 1) improves motor performance by reactivation of motor areas containing the AO/action execution matching system, 2) could improve motor nerve excitability, 3) enhanced motor memory formation, and 4) might alter cortical activation patterns.
Only two trials considered adverse effects, which could not be pooled in the meta‐analysis. Nevertheless, these trials showed no adverse effects.
One of the causes of heterogeneity in this review refers to the different approaches to therapy application. The content offered in the AO was heterogeneous among the trials. In most trials, the content observed was functional tasks, composed of one to three motor actions, with or without increasing complexity of the tasks throughout training. Range of motion exercises, and performing active movements such as thumb movements were also offered for observation.
The time of AO was quite variable between trials, ranging from 1 minute to 10 minutes for each motor action, task, or movement observed. Adding a total observation time of 4 to 36 minutes per session.
The motor action performed after observing the action was the practice of the observed movement or task and ranged from 2 to 30 minutes of training for each motor action, totaling a minimum of 5 minutes and a maximum of 36 minutes of exercise per session.
Other causes of heterogeneity can be cited, such as duration of the treatment period, treatment frequency, and time points measured.
Overall completeness and applicability of evidence
We found only 16 RCTs that tested the effectiveness of AO; furthermore, the trials had a relatively small sample size. Since none of the trials included only participants with hemorrhagic stroke, we were unable to form a subgroup with only this population of participants. The mean age of the participants varied widely.
The most common outcome was arm motor function, and few trials assessed other important outcomes for people with stroke, such as hand motor function, dependence on ADL, quality of life, and adverse effects. Although cortical activation is not an outcome directly expressed by patients, it is particularly important to researchers and clinicians since it provides evidence that motor gains result from better brain activation. There is also a need to better monitor adverse effects such as pain, fatigue, and attention deficit, in order to determine the effectiveness of AO — that is, whether the benefits outweigh any adverse effect.
Nearly all the trials used motor practice after the observation of a task. This restricts the applicability of therapy for people with some degree of motricity in the affected upper limb; and although some trials included participants in the acute phase, it was not possible to observe the effect of AO on individuals who were unable to perform the movements. Therefore, it would be advisable to test whether applying AO alone, with no motor practice, would show any benefit for totally paralyzed patients. Moreover, the outcome of AO alone versus followed by motor practice should be compared, in order to determine whether the gains derive only from motor practice that occurs after observation.
Certainty of the evidence
The number of trials (only 13 trials in meta‐analyses) and sample sizes included in this review were small. Some trials showed a high risk of bias for allocation concealment, incomplete outcome data, selective reporting, and other types of bias related to lack of information. We observed unclear risk of bias in many trials with important criteria such as randomisation, allocation concealment, and blinded researchers, resulting from poor reporting and lack of clarification from the authors. The effect estimate was also inaccurate. Nevertheless, most of the results were consistent (low heterogeneity) and exhibited good external validity. According to the GRADE system, the certainty of evidence remains 'low' or 'very low' for most of the outcomes (Table 1).
Potential biases in the review process
Two review authors independently reviewed the trials, obtaining and extracting data, with a third review author available to resolve disagreements as needed, thereby minimizing bias. We are confident that we have identified all relevant trials; however, there is a small possibility that we failed to identify additional (published or unpublished) papers. Moreover, some analyses could not determine the effect of AO on adverse effects, since not all study authors could provide the required data. Another limitation of this review is that some of the trials had methodological shortcomings or even did not report important procedures in the manuscripts, such as allocation concealment, incomplete outcome data, and selective reporting. These biases can lead to underestimation or overestimation of the true intervention effect, according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2022).
Agreements and disagreements with other studies or reviews
We found four systematic reviews on AO for stroke patients. Sarasso 2015 analyzed trials investigating the effects of this therapy on different motor abilities in diseases such as stroke (upper and lower limb), Parkinson’s disease, cerebral palsy, and postsurgical orthopedic conditions, in 663 people (20 RCTs). This search included articles up to July 2015. Six trials involving stroke patients with upper limb impairment were also included in our review (Cowles 2012; Ertelt 2007; Franceschini 2012; Harmsen 2015; Kim 2015; Lee 2013). The conclusion of the Sarasso 2015 review suggested the efficacy of AO in improving motor functions both in neurological and orthopedic diseases. The study did not cover all the literature found in our review (only 6 of the 16 trials included) and did not pool the data in meta‐analyses. Despite this, Sarasso 2015 obtained similar conclusions regarding the overall effect of the therapy, but without estimating the effect size.
Peng 2019 summarized trials (17 RCTs, 600 participants) that investigated the effectiveness of AO in the arm and hand motor function, walking ability, gait performance, and ADL in stroke patients. The search included articles up to January 2019. Seven trials were also included in our review (Cowles 2012; Ertelt 2007; Franceschini 2012; Fu 2017; Kim 2015; Kim 2016a; Zhu 2015). Compared to control treatments, AO had a moderate effect size on arm and hand motor function and a moderate to large effect size on ADL performance. Peng 2019 concluded that AO is an effective approach for stroke patients to improve arm and hand motor function and daily activity performance. Effect sizes were different from our study, as was the outcome for ADL. This increase in effect size may have been due to: 1) only seven of the 16 articles included in our review were included, and these trials had more favorable results for the studied therapy; 2) the inclusion of Sale 2012 as a different study than Franceschini 2012 generated duplication of results (Sale's sample is a part of Franceschini's sample).
Zhang 2019 analyzed trials (7 RCTs, 276 participants) investigating the effects of AO on improving upper limb motor functions in people with stroke. The search included manuscripts up to March 2019. Seven trials were also included in our review (Cowles 2012; Ertelt 2007; Franceschini 2012; Fu 2017; Kim 2015; Kim 2016a; Zhu 2015). The results revealed an effect favoring the therapy over the control. Zhang 2019 concluded that AO is an effective method for improving upper limb motor function after stroke, corroborating our findings, despite having included few trials.
Ryan 2021 summarized trials (36 RCTs, 1405 participants) that investigated the effects of AO in amputees, orthopedic disorders, dementia, cerebral palsy, multiple sclerosis, Parkinson's disease, and stroke (upper and lower limb). The search included manuscripts up to July 2020. Seven trials involving AO therapy for upper limb impairment of stroke patients were also included in our review (Cowles 2012; Franceschini 2012; Fu 2017; Hsieh 2020; Kim 2015; Kim 2016a; Zhu 2015). In meta‐analyses, they observed an effect for hand function; and no effect for arm function. However, results related to Fugl‐Meyer Assessment and Modified Barthel Index are not comparable, and the authors included trials that performed lower limb training. The conclusion of Ryan 2021 suggested that the benefit of incorporating AO into rehabilitation programs is strongly supported in stroke patients. Our findings do not support such a strong recommendation.
We believe that due to our more recent and comprehensive search strategy, we identified more trials evaluating the effects of AO on upper limb function in poststroke patients than other systematic reviews already published.
Authors' conclusions
Implications for practice.
The results of this review show low‐certainty evidence that AO may improve arm motor function of poststroke patients compared with any control group. This effect seems to be increased by adopting observations > 3 minutes, professional supervision, and video presentations. AO improves hand motor function, but the evidence showed that the improvements were not clinically relevant.
There is no convincing evidence that the intervention affects dependence on ADL, motor performance, cortical activation, or quality of life after stroke. There is little evidence in the literature of any adverse effects.
The certainty of GRADE‐based evidence in this review varied from very low to low, due to the high risk of bias and small sample sizes. This means that our confidence in the estimated effect is limited and that the true effect may be substantially different. Thus, AO may improve arm and hand motor function. However, confidence in this effect is limited, mainly for arm function, but may be confirmed in future clinical trials.
Implications for research.
To improve the certainty of the evidence (GRADE) regarding the effect of AO on upper limb rehabilitation in people with stroke, new RCTs should be conducted, with greater methodological rigor in order to reduce the risk of bias, using a larger sample and standardized outcome assessment instruments to increase consistency. A guideline specifying the main evaluation tools for each outcome would be useful in standardizing the findings, given the variety of existing instruments. The Standardizing Measurement in Arm Rehabilitation Trials (SMART) Toolbox provides a selection of measures of importance to stroke survivors, carers, clinicians, and researchers in future RCTs, whilst considering psychometric properties, the ICF classification, and outcomes important to stroke survivors, carers, and clinicians (Millar 2021).
Furthermore, trials have exhibited methodological problems, such as lack of clarity, which hinders assessment of bias and quality. In order to minimize this shortcoming, research should follow the CONSORT recommendations (Schulz 2010), which contain guidelines for writing RCTs in the area of health. Data presentation should also be clear to allow easy interpretation and pooling of quantitative data.
It is important that the authors of future trials characterize their samples in more detail in order to attest the applicability of AO in specific situations, according to the etiology and phase of stroke, upper limb impairment, and brain hemisphere affected. Other information regarding the form of therapy application is also necessary for assessing its effects, such as whether therapy was administered through videos or live demonstrations, which perspective was used, treatment setting, and dose. Trials should include follow‐up assessment to determine if the effects are long‐lasting.
What's new
| Date | Event | Description |
|---|---|---|
| 18 November 2021 | New citation required but conclusions have not changed | The conclusions of the review have not changed. |
| 18 November 2021 | New search has been performed | We updated the searches to May 2021. We added four new trials, bringing the total number of included trials to 16, with a total of 574 particpiants. |
History
Protocol first published: Issue 9, 2015 Review first published: Issue 10, 2018
Acknowledgements
We thank Josh Cheyne for helping with search strategies and database searches; Hazel Fraser for resolving questions raised during the review; Alex Todhunter‐Brown, Gillian Mead and Richard Parker for their editorial review and recommendations.
Appendices
Appendix 1. The Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
#1MeSH descriptor: [Cerebrovascular Disorders] this term only #2MeSH descriptor: [Basal Ganglia Cerebrovascular Disease] this term only #3MeSH descriptor: [Brain Ischemia] explode all trees #4MeSH descriptor: [Carotid Artery Diseases] explode all trees #5MeSH descriptor: [Cerebral Small Vessel Diseases] explode all trees #6MeSH descriptor: [Intracranial Arterial Diseases] explode all trees #7MeSH descriptor: [Intracranial Embolism and Thrombosis] explode all trees #8MeSH descriptor: [Intracranial Hemorrhages] explode all trees #9MeSH descriptor: [Stroke] explode all trees #10MeSH descriptor: [Vasospasm, Intracranial] this term only #11MeSH descriptor: [Vertebral Artery Dissection] this term only #12(stroke* or poststroke or apoplex* or cerebral vasc* or brain vasc* or cerebrovasc* or cva* or SAH):ti,ab,kw (Word variations have been searched) #13((brain or cerebr* or cerebell* or vertebrobasil* or hemispher* or intracran* or intracerebral or infratentorial or supratentorial or middle cerebral artery or MCA* or anterior circulation or posterior circulation or basilar artery or vertebral artery or space‐occupying) near/5 (isch?emi* or infarct* or thrombo* or emboli* or occlus* or hypoxi*)):ti,ab,kw (Word variations have been searched) #14((brain* or cerebr* or cerebell* or intracerebral or intracran* or parenchymal or intraparenchymal or intraventricular or infratentorial or supratentorial or basal gangli* or putaminal or putamen or posterior fossa or hemispher* or subarachnoid) near/5 (h?emorrhag* or h?ematoma* or bleed*)):ti,ab,kw (Word variations have been searched) #15MeSH descriptor: [Hemiplegia] this term only #16MeSH descriptor: [Paresis] explode all trees #17MeSH descriptor: [Gait Disorders, Neurologic] explode all trees #18(hemipleg* or hemipar* or paresis or paraparesis or paretic):ti,ab,kw (Word variations have been searched) #19{or #1‐#18} 51283 #20MeSH descriptor: [Observation] this term only #21MeSH descriptor: [Psychomotor Performance] explode all trees #22MeSH descriptor: [Imitative Behavior] this term only #23MeSH descriptor: [Motion Perception] this term only #24MeSH descriptor: [Learning] this term only #25MeSH descriptor: [Anticipation, Psychological] this term only #26MeSH descriptor: [Photic Stimulation] this term only #27MeSH descriptor: [Mirror Neurons] this term only #28action observation or action‐observation or AO or AOT:ti,ab,kw (Word variations have been searched) #29((observ* or watch8) near/10 (action* or movement* or reach* or activit* or task* or motion* or motor train* or perform* or gestur* or demonstrat* or video* or TV screen or television screen or computer screen)):ti,ab,kw (Word variations have been searched) #30((visual or action or motion) near/5 perception):ti,ab,kw (Word variations have been searched) #31(visual‐motor matching):ti,ab,kw (Word variations have been searched) #32(mirror neur*):ti,ab,kw (Word variations have been searched) #33{or #20‐#32} #34MeSH descriptor: [Upper Extremity] explode all trees #35(upper limb* or upper extremit* or arm or arms or shoulder or shoulders or hand or hands or axilla* or elbow* or forearm* or finger* or wrist*):ti,ab,kw (Word variations have been searched) #36#34 or #35
Appendix 2. MEDLINE search strategy
Medline (Ovid) search strategy
1. cerebrovascular disorders/ or exp basal ganglia cerebrovascular disease/ or exp brain ischemia/ or exp carotid artery diseases/ or exp cerebral small vessel diseases/ or exp intracranial arterial diseases/ or exp "intracranial embolism and thrombosis"/ or exp intracranial hemorrhages/ or stroke/ or exp brain infarction/ or stroke, lacunar/ or vasospasm, intracranial/ or vertebral artery dissection/ or brain injuries/ or brain injury, chronic/ 2. (stroke$ or poststroke or apoplex$ or cerebral vasc$ or brain vasc$ or cerebrovasc$ or cva$ or SAH).tw. 3. ((brain or cerebr$ or cerebell$ or vertebrobasil$ or hemispher$ or intracran$ or intracerebral or infratentorial or supratentorial or middle cerebral artery or MCA$ or anterior circulation or posterior circulation or basilar artery or vertebral artery or space‐occupying) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$ or hypoxi$)).tw. 4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracran$ or parenchymal or intraparenchymal or intraventricular or infratentorial or supratentorial or basal gangli$ or putaminal or putamen or posterior fossa or hemispher$ or subarachnoid) adj5 (h?emorrhag$ or h?ematoma$ or bleed$)).tw. 5. hemiplegia/ or exp paresis/ 6. (hemipleg$ or hemipar$ or paresis or paretic or brain injur$).tw. 7. or/1‐6 8. exp upper extremity/ 9. (upper limb$ or upper extremit$ or arm or arms or shoulder or shoulders or hand or hands or axilla$ or elbow$ or forearm$ or finger$ or wrist$).tw. 10. 8 or 9 11. observation/ or psychomotor performance/ or imitative behavior/ or imagination/ 12. motion perception/ or visual perception/ or learning/ 13. anticipation, psychological/ or photic stimulation/ or mirror neurons/ 14. "Imagery (Psychotherapy)"/ 15. (action observation or action‐observation or AO or AOT).tw. 16. ((observ$ or watch$) adj10 (action$ or movement$ or reach$ or activit$ or task$ or motion$ or motor train$ or perform$ or gestur$ or demonstrat$ or video$ or TV screen or television screen or computer screen)).tw. 17. ((visual or action or motion) adj5 perception).tw. 18. visual‐motor matching.tw. 19. mirror neur$.tw. 20. 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 21. Randomized Controlled Trials as Topic/ 22. random allocation/ 23. Controlled Clinical Trials as Topic/ 24. control groups/ 25. clinical trials as topic/ or clinical trials, phase i as topic/ or clinical trials, phase ii as topic/ or clinical trials, phase iii as topic/ or clinical trials, phase iv as topic/ 26. double‐blind method/ 27. single‐blind method/ 28. Placebos/ 29. placebo effect/ 30. cross‐over studies/ 31. randomized controlled trial.pt. 32. controlled clinical trial.pt. 33. (clinical trial or clinical trial phase i or clinical trial phase ii or clinical trial phase iii or clinical trial phase iv).pt. 34. (random$ or RCT or RCTs).tw. 35. (controlled adj5 (trial$ or stud$)).tw. 36. (clinical$ adj5 trial$).tw. 37. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw. 38. (quasi‐random$ or quasi random$ or pseudo‐random$ or pseudo random$).tw. 39. ((control or experiment$ or conservative) adj5 (treatment or therapy or procedure or manage$)).tw. 40. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw. 41. (cross‐over or cross over or crossover).tw. 42. (placebo$ or sham).tw. 43. trial.ti. 44. (assign$ or allocat$).tw. 45. controls.tw. 46. or/21‐45 47. 7 and 10 and 20 and 46 48. exp animals/ not humans/ 49. 47 not 48
Appendix 3. Embase search strategy
1. cerebrovascular disease/ or brain disease/ or exp basal ganglion hemorrhage/ or exp brain hemangioma/ or exp brain hematoma/ or exp brain hemorrhage/ or exp brain infarction/ or exp brain ischemia/ or exp carotid artery disease/ or exp cerebral artery disease/ or exp cerebrovascular accident/ or exp cerebrovascular malformation/ or exp intracranial aneurysm/ or exp occlusive cerebrovascular disease/ or exp vertebrobasilar insufficiency/ 2. (stroke$ or poststroke or apoplex$ or cerebral vasc$ or brain vasc$ or cerebrovasc$ or cva$ or SAH).tw. 3. ((brain or cerebr$ or cerebell$ or vertebrobasil$ or hemispher$ or intracran$ or intracerebral or infratentorial or supratentorial or middle cerebral artery or MCA$ or anterior circulation or posterior circulation or basilar artery or vertebral artery or space‐occupying) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$ or hypoxi$)).tw. 4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracran$ or parenchymal or intraparenchymal or intraventricular or infratentorial or supratentorial or basal gangli$ or putaminal or putamen or posterior fossa or hemispher$ or subarachnoid) adj5 (h?emorrhag$ or h?ematoma$ or bleed$)).tw. 5. exp hemiplegia/ or exp paresis/ or neurologic gait disorder/ 6. (hemipleg$ or hemipar$ or paresis or paraparesis or paretic).tw. 7. or/1‐6 8. exp upper limb/ 9. (upper limb$ or upper extremit$ or arm or arms or shoulder or shoulders or hand or hands or axilla$ or elbow$ or forearm$ or finger$ or wrist$).tw. 10. 8 or 9 11. observation/ or psychomotor performance/ or exp imitation/ 12. movement perception/ or vision/ or learning/ 13. anticipation/ or photostimulation/ or mirror neuron/ 14. (action observation or action‐observation or AO or AOT).tw. 15. ((observ$ or watch$) adj10 (action$ or movement$ or reach$ or activit$ or task$ or motion$ or motor train$ or perform$ or gestur$ or demonstrat$ or video$ or TV screen or television screen or computer screen)).tw. 16. ((visual or action or motion) adj5 perception).tw. 17. visual‐motor matching.tw. 18. mirror neur$.tw. 19. or/11‐18 20. Randomized Controlled Trial/ or "randomized controlled trial (topic)"/ 21. Randomization/ 22. Controlled clinical trial/ or "controlled clinical trial (topic)"/ 23. control group/ or controlled study/ 24. clinical trial/ or "clinical trial (topic)"/ or phase 1 clinical trial/ or phase 2 clinical trial/ or phase 3 clinical trial/ or phase 4 clinical trial/ 25. Crossover Procedure/ 26. Double Blind Procedure/ 27. Single Blind Procedure/ or triple blind procedure/ 28. placebo/ or placebo effect/ 29. (random$ or RCT or RCTs).tw. 30. (controlled adj5 (trial$ or stud$)).tw. 31. (clinical$ adj5 trial$).tw. 32. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw. 33. (quasi‐random$ or quasi random$ or pseudo‐random$ or pseudo random$).tw. 34. ((control or experiment$ or conservative) adj5 (treatment or therapy or procedure or manage$)).tw. 35. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw. 36. (cross‐over or cross over or crossover).tw. 37. (placebo$ or sham).tw. 38. trial.ti. 39. (assign$ or allocat$).tw. 40. controls.tw. 41. (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 42. or/20‐40 43. 7 and 10 and 19 and 42
Appendix 4. CINAHL search strategy
S1(MH "Cerebrovascular Disorders") OR (MH "Basal Ganglia Cerebrovascular Disease+") OR (MH "Carotid Artery Diseases+") OR (MH "Cerebral Ischemia+") OR (MH "Cerebral Vasospasm") OR (MH "Intracranial Arterial Diseases+") OR ( (MH "Intracranial Embolism and Thrombosis") ) OR (MH "Intracranial Hemorrhage+") OR (MH "Stroke") OR (MH "Vertebral Artery Dissections") OR (MH "Stroke Patients") OR (MH "Stroke Units") S2TI ( stroke or poststroke or post‐stroke or cerebrovasc* or brain vasc* or cerebral vasc or cva or apoplex or SAH ) or AB ( stroke or poststroke or post‐stroke or cerebrovasc* or brain vasc* or cerebral vasc or cva or apoplex or SAH) S3TI ( brain* or cerebr* or cerebell* or intracran* or intracerebral ) or AB ( brain* or cerebr* or cerebell* or intracran* or intracerebral) S4TI ( ischemi* or ischaemi* or infarct* or thrombo* or emboli* or occlus* ) or AB ( ischemi* or ischaemi* or infarct* or thrombo* or emboli* or occlus*) S5S3 AND S4 S6TI ( brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid ) or AB ( brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid) S7TI ( haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed* ) or AB ( haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed*) S8S6 AND S7 S9TI transient ischaemic attack* or TI transient ischemic attack* or AB transient ischaemic attack* or AB transient ischemic attack* or TI TIA or TI TIA s or AB TIA or AB TIAs S10S1 OR S2 OR S3 OR S6 OR S9 OR S10 S11(MH "Upper Extremity+") S12TI ( upper limb* or upper extremit* or arm or arms or shoulder or shoulders or hand or hands or axilla* or elbow* or forearm* or finger* or wrist* ) OR AB ( upper limb* or upper extremit* or arm or arms or shoulder or shoulders or hand or hands or axilla* or elbow* or forearm* or finger* or wrist* ) S13S11 OR S12 S14(MH "Psychomotor Performance+") S15(MH "Imitative Behavior") S16(MH "Visual Perception+") S17(MH "Learning") S18(MH "Neurons+") S19TI ( (action observation or action‐observation or AO or AOT) ) OR AB ( (action observation or action‐observation or AO or AOT) ) S20TI ( ((observ* or watch*) N10 (action* or movement* or reach* or activit* or task* or motion* or motor train* or perform* or gestur* or demonstrat* or video* or TV screen or television screen or computer screen)) ) OR AB ( ((observ* or watch*) N10 (action* or movement* or reach* or activit* or task* or motion* or motor train* or perform* or gestur* or demonstrat* or video* or TV screen or television screen or computer screen)) ) S21TI ( (action observation or action‐observation or AO or AOT) ) OR AB ( (action observation or action‐observation or AO or AOT). ) S22TI ( ((visual or action or motion) N5 perception). ) OR AB ( ((visual or action or motion) N5 perception). ) S23TI (visual‐motor matching) OR AB (visual‐motor matching) S24TI mirror neur* OR AB mirror neur* S25S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 S26(MH "Randomized Controlled Trials") or (MH "Random Assignment") or (MH "Random Sample+") S27(MH "Clinical Trials") or (MH "Intervention Trials") or (MH "Therapeutic Trials") S28(MH "Double‐Blind Studies") or (MH "Single‐Blind Studies") or (MH "Triple‐Blind Studies") S29(MH "Control (Research)") or (MH "Control Group") or (MH "Placebos") or (MH "Placebo Effect") S30(MH "Crossover Design") OR (MH "Quasi‐Experimental Studies") S31PT (clinical trial or randomized controlled trial) S32TI (random* or RCT or RCTs) or AB (random* or RCT or RCTs) S33TI (controlled N5 (trial* or stud*)) or AB (controlled N5 (trial* or stud*)) S34TI (clinical* N5 trial*) or AB (clinical* N5 trial*) S35TI ((control or treatment or experiment* or intervention) N5 (group* or subject* or patient*)) or AB ((control or treatment or experiment* or intervention) N5 (group* or subject* or patient*)) S36((control or experiment* or conservative) N5 (treatment or therapy or procedure or manage*)) or AB ((control or experiment* or conservative) N5 (treatment or therapy or procedure or manage*)) S37TI ((singl* or doubl* or tripl* or trebl*) N5 (blind* or mask*)) or AB ((singl* or doubl* or tripl* or trebl*) N5 (blind* or mask*)) S38TI (cross‐over or cross over or crossover) or AB (cross‐over or cross over or crossover) S39TI (placebo* or sham) or AB (placebo* or sham) S40TI trial S41TI (assign* or allocat*) or AB (assign* or allocat*) S42TI controls or AB controls S43TI (quasi‐random* or quasi random* or pseudo‐random* or pseudo random*) or AB (quasi‐random* or quasi random* or pseudo‐random* or pseudo random*) S44S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 S45S10 AND S13 AND S25 AND S44
Appendix 5. LILACS search strategy
(TW:"Brain Vascular Disorders" OR TW:"Intracranial Vascular Disorders" OR TW:"Transtornos Vasculares do Cérebro" OR TW:"Transtornos Vasculares Intracranianos" OR TW:"Doenças Vasculares Intracranianas" OR TW:"Trastornos Vasculares del Cerebro" OR TW:"Trastornos Vasculares Intracraneales" OR TW:"Enfermedades Intracraneales Vasculares" OR MH:C10.228.140.300 OR MH:C14.907.253 OR TW:"Lenticulostriate Vasculopathy" OR TW:"Doença Cerebrovascular dos Gânglios Basais" OR TW:"Doenças Vasculares Lenticulostratais" OR TW:"Vasculopatia Lenticulostriatal" OR TW:"Vasculopatia Lenticuloestriatal" OR TW:"Enfermedad de los Ganglios Basales Cerebrovascular" OR TW:"Enfermedades Vasculares Lenticulostriatales" OR MH:C10.228.140.079.127$ OR MH:C10.228.140.300.100$ OR MH:C14.907.253.061$ OR TW:"Cerebral Ischemia" OR TW:"Ischemic Encephalopathy" OR TW:"Isquemia Cerebral" OR TW:"Encefalopatía Isquémica" OR MH:10.228.140.300.150$ OR MH:C14.907.253.092$ OR TW:"Carotid Atherosclerosis" OR TW:"Aterosclerosis de la Carótida " OR TW:"Aterosclerose Carotídea" OR TW:"Aterosclerose da Carótida" OR MH:C10.228.140.300.200$ OR MH:C14.907.253.123$ OR MH:C10.228.140.300.275$ OR MH:C14.907.253.329$ OR MH:C10.228.140.300.510$ OR MH:C14.907.253.560$ OR TW:"Cerebral Embolism and Thrombosis" OR TW:"Brain Embolism and Thrombosis" OR TW:"Embolia e Trombose Cerebral" OR TW:"Embolia e Trombose Encefálica" OR TW:"Embolia y Trombosis Cerebral" OR TW:"Embolia y Trombosis del Cerebro" OR MH:C10.228.140.300.525$ OR MH:C14.907.253.566$ OR MH:C14.907.355.590.213$ OR TW:"Brain Hemorrhage" OR TW:"Hemorragia Encefálica" OR TW:"Hemorragia Intracraniana" OR TW:"Hemorragia del Cerebro" OR TW:"Hemorragia Intracraneal" OR MH:C10.228.140.300.535$ OR MH:C14.907.253.573$ OR MH:C23.550.414.913$ OR TW:"Apoplexy" OR TW:"Cerebral Stroke" OR TW:"Cerebrovascular Accident" OR TW:"Cerebrovascular Apoplexy" OR TW:"Acidente Vascular Cerebral" OR TW:"Derrame Cerebral" OR TW:"Ictus Cerebral" OR TW:"AVC" OR TW:"Apoplexia" OR TW:"Acidente Cerebrovascular" OR TW:"Apoplexia Cerebral" OR TW:"Apoplexia Cerebrovascular" OR TW:"Icto Cerebral" OR TW:"Acidente Vascular Encefálico" OR TW:"AVE" OR TW:"Acidente Vascular do Cérebro" OR TW:"Acidente Cerebral Vascular" OR TW:"Acidentes Cerebrais Vasculares" OR TW:"Acidentes Cerebrovasculares" OR TW:"Acidentes Vasculares Cerebrais" OR TW:"Ataque" OR TW:"Ictus" OR TW:"Ictus Cerebral" OR TW:"Apoplejía" OR TW:"Ataque Cerebral" OR TW:"Apoplejía Cerebral" OR TW:"Apoplejía Cerebrovascular" OR TW:"Accidente Vascular Encefálico" OR TW:"Accidente Vascular del Cerebro" OR TW:"Accidente Vascular Cerebral" OR TW:"Accidente Cerebral Vascular" OR TW:"Accidentes Cerebrovasculares" OR MH:C10.228.140.300.775$ OR MH:C14.907.253.855$ OR TW:"Infarto Venoso Encefálico" OR TW:"Infarto Venoso Cerebral" OR TW:"Infarto Venoso do Encéfalo" OR TW:"Infarto do Encéfalo" OR TW:"Infarto Venoso del Encéfalo" OR TW:"Infarto del Encéfalo" OR MH:C10.228.140.300.150.477$ OR MH:C10.228.140.300.775.200$ OR MH:C14.907.253.092.477$ OR MH:C14.907.253.855.200$ OR TW:"Infarto Lacunar" OR TW:"Acidente Vascular Encefálico Lacunar" OR MH:C10.228.140.300.275.800$ OR MH:C10.228.140.300.775.600$ OR MH:C14.907.253.329.800$ OR MH:C14.907.253.855.600$ OR MH:C10.228.140.300.90$ OR MH:C14.907.253.951$ OR TW:"Cerebral Vasospasm" OR TW:"Intracranial Vasospasm" OR TW:"Angioespasmo Intracraniano" OR TW:"Angiospasmo Intracraniano" OR TW:"Vasoespasmo Cerebral" OR TW:"Vasospasmo Cerebral" OR TW:"Vasospasmo Intracraniano" OR TW:"Angioespasmo Intracraneal" OR TW:"Vasoespasmo Cerebral" OR TW:"Dissecting Vertebral Artery Aneurysm" OR MH:C10.228.140.300.350.875$ OR MH:C10.900.250.650$ OR MH:C14.907.055.050.575$ OR MH:C14.907.253.535.800$ OR MH:C26.915.200.600$ OR TW:"Aneurisma Disecante de la Arteria Vertebral" OR TW:"Dissecção da Artéria Vertebral" OR TW:"Aneurisma Dissecante da Artéria Vertebral" OR TW:"Brain Contusion" OR TW:"Brain Lacerations" OR TW:"Traumatic Brain Injury" OR MH:C10.228.140.199$ OR MH:C10.900.300.087$ OR MH:C26.915.300.200$ OR TW:"Lesión Cerebral" OR TW:"Lesiones Encefálicas" OR TW:"Traumatismo Cerebral" OR TW:"Traumatismos Cerebrales" OR TW:"Contusión Encefálica" OR TW:"Lesiones Traumáticas del Encéfalo" OR TW:"Lesiones Encefálicas Traumáticas" OR TW:"Laceraciones del Encéfalo" OR TW:"Laceraciones Encefálicas" OR TW:"Traumatismo Encefálico" OR TW:"Lesiones del Encéfalo Traumáticas" OR TW:"Lesão Cerebral" OR TW:"Lesões Encefálicas" OR TW:"Traumatismo Cerebral" OR TW:"Traumatismos Cerebrais" OR TW:"Contusão Encefálica" OR TW:"Lesões Encefálicas Traumáticas" OR TW:"Lacerações Encefálicas" OR TW:"Traumatismo do Encéfalo" OR TW:"Lesão Encefálica Traumática" OR MH:C10.228.140.140.127$ OR MH:C10.228.140.199.500$ OR MH:C10.900.300.087.250$ OR MH:C26.915.300.200.200$ OR tw:stroke* or tw:poststroke or tw:apoplex* or tw:cerebrovasc* or cva* or tw:SAH OR TW:Monoplegia OR MH:C10.597.622.295$ OR MH:C23.888.592.636.312$ OR TW:Hemiparesis OR TW:Muscle Paresis OR MH:C10.597.636$ OR MH:C23.888.592.643$ OR TW:"Hemiparesia" OR TW:"Paresia Muscular" OR TW:hemipleg* or TW:hemipar* or TW:paresis or TW:paretic) AND (MH:A01.378.800$ OR TW:"Extremidade Superior" OR TW:"upper limb" or TW:"upper extremity" or TW:arm or TW:arms or TW:shoulder or TW:shoulders or TW:hand or TW:hands or TW:axilla* or TW:elbow* or TW:forearm* or TW:finger* or TW:wrist*) AND (TW:Observation OR TW:Observación OR TW:Observação OR MH:E05.581.249 OR TW:"Perceptual Motor Performance" OR TW:"Visual Motor Coordination" OR TW:"Sensory Motor Performance" OR MH:F02.808 OR MH:G11.427.700 OR MH:G11.561.623 OR TW:"Desempenho Perceptual‐Motor" OR TW:"Coordenação Visiomotora" OR TW:"Desempenho Sensório‐Motor" OR TW:"Desempeño Motor Perceptual" OR TW:"Coordinación Motora Visual" OR TW:"Desempeño Motor Sensorial" OR TW:"Imitative Behavior" OR TW:"Conducta Imitativa" OR TW:"Comportamento Imitativo" OR MH:F01.145.510$ OR TW:"Motion Perception" OR TW:"Percepción de Movimiento" OR TW:"Percepção de Movimento" OR MH:F02.463.593.932.567 OR TW:"Percepción Visual" OR TW:"Percepção Visual" OR TW:"visual perception" OR MH:F02.463.593.932 OR TW:Learning OR TW:Aprendizaje OR TW:Aprendizagem OR TW:Phenomenography OR MH:F02.463.425 OR MH:F02.784.629.529 OR MH:SP4.006.047.453.604 OR TW:Aprendizado OR TW:Fenomenografia OR TW:"Psychological Anticipation" OR TW:"Anticipación Psicológica" OR TW:"Antecipação Psicológica" OR MH:F02.463.093 OR TW:"Photic Stimulation" OR TW:"Estimulación Luminosa" OR TW:"Estimulação Luminosa" OR TW:"Visual Stimulation" OR MH:E05.723.729 OR TW:"Estimulação Fótica" OR TW:"Estimulação Visual" OR TW:"Estimulación Fótica" OR TW:"Estimulación Visual" OR TW:"Mirror Neurons" OR TW:"Neurônios‐Espelho" OR TW:"Neuronas Espejo" OR MH:A08.675.500 OR MH:A11.671.487 OR TW:"action observation" OR TW:"action‐observation" OR TW:AO OR TW:AOT OR TW:"observación de la acción" OR TW:"observação da ação" OR TW:"visual‐motor matching" OR TW:"correspondência visual‐motora" OR TW:"coincidente visomotora") AND (((PT:"randomized controlled trial" OR PT:"controlled clinical trial" OR PT:"multicenter study" OR MH:"randomized controlled trials as topic" OR MH:"controlled clinical trials as topic" OR MH:"multicenter study as topic" OR MH:"random allocation" OR MH:"double‐blind method" OR MH:"single‐blind method") OR ((ensaio$ OR ensayo$ OR trial$) AND (azar OR acaso OR placebo OR control$ OR aleat$ OR random$ OR enmascarado$ OR simpleciego OR ((simple$ OR single OR duplo$ OR doble$ OR double$) AND (cego OR ciego OR blind OR mask))) AND clinic$)) AND NOT (MH:animals OR MH:rabbits OR MH:rats OR MH:primates OR MH:dogs OR MH:cats OR MH:swine OR PT:"in vitro"))
Update 2021:
(ti:(((stroke OR poststroke OR post‐stroke OR cerebrovasc* OR brain vasc* OR cerebral vasc* OR cva* OR apoplex* OR sah) OR ((brain* OR cerebr* OR cerebell* OR intracerebral OR intracranial OR subarachnoid) near/5 (haemorrhage* OR hemorrhage* OR haematoma* OR hematoma* OR bleed*)) OR ((brain* OR cerebr* OR cerebell* OR intracran* OR intracerebral) near/5 (isch*emi* OR infarct* OR thrombo* OR emboli* OR occlus*))))) AND ((action observation OR action‐observation OR ao OR aot) OR (observ* OR watch*) ) OR (action* OR learn* OR movement* OR reach* OR activit* OR task* OR motion* OR motor train* OR perform* OR gestur* OR demonstrat* OR video* OR tv screen OR television screen OR computer screen) AND ( db:("LILACS") AND type_of_study:("clinical_trials")) AND (year_cluster:[2016 TO 2021])
Appendix 6. Allied and Complementary Medicine Database (AMED) search strategy
1. cerebrovascular disorders/ or cerebral hemorrhage/ or cerebral infarction/ or cerebral ischemia/ or cerebrovascular accident/ or stroke/ 2. (stroke or poststroke or post‐stroke or cerebrovasc$ or brain vasc$ or cerebral vasc$ or cva$ or apoplex$ or SAH).tw. 3. ((brain$ or cerebr$ or cerebell$ or intracran$ or intracerebral) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$)).tw. 4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracranial or subarachnoid) adj5 (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$)).tw. 5. hemiplegia/ 6. (hemipleg$ or hemipar$ or paresis or paretic).tw. 7. or/1‐6 8. exp arm/ 9. (upper limb$ or upper extremit$ or arm or arms or shoulder or shoulders or hand or hands or axilla$ or elbow$ or forearm$ or finger$ or wrist$).tw. 10. 8 or 9 11. psychomotor performance/ or Movement/ or Motion/ 12. Visual perception/ 13. Learning/ 14. Photic stimulation/ 15. (action observation or action‐observation or AO or AOT).tw. 16. ((observ$ or watch$) adj10 (action$ or learn$ or movement$ or reach$ or activit$ or task$ or motion$ or motor train$ or perform$ or gestur$ or demonstrat$ or video$ or TV screen or television screen or computer screen)).tw. 17. ((visual or action or motion) adj5 perception).tw. 18. visual‐motor matching.tw. 19. mirror neur$.tw. 20. or/11‐19 21. 7 and 10 and 20
Appendix 7. PEDro search strategy
Abstract and Title: stroke*
Body part: upper arm, shoulder or shoulder girdle / forearm or elbow / hand or wrist.
Therapy: Neurodevelopmental therapy, neurofacilitation
Methods: Clinical trial
All search terms in the title or abstract were combined with body part descriptors using the AND operator.
Appendix 8. US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov)
action observation AND INFLECT EXACT "Interventional" [STUDY‐TYPES] AND ( Cerebrovascular Disorders OR Stroke OR Transient Ischaemic Attack OR Subarachnoid ) [DISEASE]
Appendix 9. ISRCTN Registry
Text search: stroke
Interventions: action observation
Appendix 10. Australian New Zealand Clinical Trials Registry
Search terms: cerebrovascular or cerebral or stroke or "transient ischemic attack or TIA or SAH" Description of intervention(s) / exposure: "action observation"
Appendix 11. WHO International Clinical Trials Registry Platform search strategy
Condition: stroke
Intervention: action observation
Data and analyses
Comparison 1. Action observation versus control: effect on arm function.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Arm function | 11 | 373 | Std. Mean Difference (IV, Random, 95% CI) | 0.39 [0.17, 0.61] |
| 1.2 Subgroup analysis: age | 11 | 373 | Std. Mean Difference (IV, Random, 95% CI) | 0.39 [0.17, 0.61] |
| 1.2.1 ≥ 60 years | 5 | 210 | Std. Mean Difference (IV, Random, 95% CI) | 0.39 [0.09, 0.69] |
| 1.2.2 < 60 years | 6 | 163 | Std. Mean Difference (IV, Random, 95% CI) | 0.41 [0.04, 0.78] |
| 1.3 Subgroup analysis: type of stroke | 11 | 373 | Std. Mean Difference (IV, Random, 95% CI) | 0.39 [0.17, 0.61] |
| 1.3.1 Ischemic stroke | 3 | 101 | Std. Mean Difference (IV, Random, 95% CI) | 0.56 [0.16, 0.96] |
| 1.3.2 Ischemic and hemorrhagic stroke | 4 | 139 | Std. Mean Difference (IV, Random, 95% CI) | 0.67 [‐0.04, 1.38] |
| 1.3.3 Type of stroke not stated | 4 | 133 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.13, 0.56] |
| 1.4 Subgroup analysis: time poststroke | 10 | 361 | Std. Mean Difference (IV, Random, 95% CI) | 0.41 [0.19, 0.64] |
| 1.4.1 Acute or subacute phase | 6 | 280 | Std. Mean Difference (IV, Random, 95% CI) | 0.39 [0.12, 0.66] |
| 1.4.2 Chronic phase | 3 | 43 | Std. Mean Difference (IV, Random, 95% CI) | 0.70 [‐0.06, 1.47] |
| 1.4.3 Acute, subacute and chronic phase | 1 | 38 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.27, 1.02] |
| 1.5 Subgroup analysis: treatment dose | 11 | 373 | Std. Mean Difference (IV, Random, 95% CI) | 0.39 [0.17, 0.61] |
| 1.5.1 ≥ 1000 minutes of therapy | 5 | 161 | Std. Mean Difference (IV, Random, 95% CI) | 0.34 [0.03, 0.65] |
| 1.5.2 < 1000 minutes of therapy | 6 | 212 | Std. Mean Difference (IV, Random, 95% CI) | 0.50 [0.07, 0.93] |
| 1.6 Subgroup analysis: type of control group | 11 | 373 | Std. Mean Difference (IV, Random, 95% CI) | 0.39 [0.17, 0.61] |
| 1.6.1 Placebo therapy | 6 | 231 | Std. Mean Difference (IV, Random, 95% CI) | 0.45 [0.13, 0.78] |
| 1.6.2 Conventional physical therapy | 2 | 83 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.23, 0.63] |
| 1.6.4 Functional activities training | 3 | 59 | Std. Mean Difference (IV, Random, 95% CI) | 0.56 [‐0.12, 1.24] |
| 1.7 Subgroup analysis: duration of observation | 9 | 300 | Std. Mean Difference (IV, Random, 95% CI) | 0.46 [0.21, 0.72] |
| 1.7.1 > 3 minutes of observation | 5 | 142 | Std. Mean Difference (IV, Random, 95% CI) | 0.72 [0.35, 1.10] |
| 1.7.2 ≤ 3 minutes of observation | 4 | 158 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.09, 0.54] |
| 1.8 Subgroup analysis: upper limb impairment | 8 | 295 | Std. Mean Difference (IV, Random, 95% CI) | 0.34 [0.11, 0.57] |
| 1.8.1 Severe impairment | 3 | 173 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.10, 0.50] |
| 1.8.2 Moderate impairment | 3 | 52 | Std. Mean Difference (IV, Random, 95% CI) | 0.75 [0.02, 1.49] |
| 1.8.3 Mild, moderate and severe impairments | 2 | 70 | Std. Mean Difference (IV, Random, 95% CI) | 0.41 [‐0.06, 0.88] |
| 1.9 Arm function follow‐up | 2 | 93 | Mean Difference (IV, Random, 95% CI) | 1.06 [‐8.38, 10.50] |
1.8. Analysis.

Comparison 1: Action observation versus control: effect on arm function, Outcome 8: Subgroup analysis: upper limb impairment
Comparison 2. Action observation versus control: effect on hand function.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Hand function | 5 | 178 | Mean Difference (IV, Random, 95% CI) | 2.76 [1.04, 4.49] |
| 2.2 Subgroup analysis: age | 5 | 178 | Mean Difference (IV, Random, 95% CI) | 2.76 [1.04, 4.49] |
| 2.2.1 ≥ 60 years | 2 | 122 | Mean Difference (IV, Random, 95% CI) | 3.00 [‐4.02, 10.02] |
| 2.2.2 < 60 years | 3 | 56 | Mean Difference (IV, Random, 95% CI) | 2.71 [0.91, 4.51] |
| 2.3 Subgroup analysis: time poststroke | 5 | 178 | Mean Difference (IV, Random, 95% CI) | 2.76 [1.04, 4.49] |
| 2.3.1 Acute or subacute phase | 3 | 144 | Mean Difference (IV, Random, 95% CI) | 2.67 [0.83, 4.51] |
| 2.3.2 Chronic phase | 2 | 34 | Mean Difference (IV, Random, 95% CI) | 3.46 [‐1.56, 8.47] |
| 2.4 Subgroup analysis: duration of observation | 5 | 178 | Mean Difference (IV, Random, 95% CI) | 2.76 [1.04, 4.49] |
| 2.4.1 > 3 minutes of observation | 1 | 22 | Mean Difference (IV, Random, 95% CI) | 2.60 [0.67, 4.53] |
| 2.4.2 ≤ 3 minutes of observation | 4 | 156 | Mean Difference (IV, Random, 95% CI) | 3.40 [‐0.45, 7.26] |
| 2.5 Hand function follow‐up | 2 | 93 | Mean Difference (IV, Random, 95% CI) | 5.19 [‐1.82, 12.21] |
2.5. Analysis.

Comparison 2: Action observation versus control: effect on hand function, Outcome 5: Hand function follow‐up
Comparison 3. Action observation versus control: effect on ADL.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Dependence on ADL | 7 | 302 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.34, 1.08] |
| 3.2 Subgroup analysis: age | 7 | 302 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.34, 1.08] |
| 3.2.1 ≥ 60 years | 4 | 205 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.83, 1.10] |
| 3.2.2 < 60 years | 3 | 97 | Std. Mean Difference (IV, Random, 95% CI) | 0.75 [‐0.73, 2.23] |
| 3.3 Subgroup analysis: type of stroke | 6 | 241 | Std. Mean Difference (IV, Random, 95% CI) | 0.38 [‐0.52, 1.27] |
| 3.3.1 Ischemic stroke | 2 | 85 | Std. Mean Difference (IV, Random, 95% CI) | 0.99 [0.54, 1.44] |
| 3.3.2 Ischemic and hemorrhagic stroke | 4 | 156 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐1.30, 1.44] |
| 3.4 Subgroup analysis: time poststroke | 7 | 302 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.34, 1.08] |
| 3.4.1 Acute or subacute phase | 5 | 258 | Std. Mean Difference (IV, Random, 95% CI) | 0.85 [0.23, 1.46] |
| 3.4.2 Chronic phase | 2 | 44 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.16 [‐2.16, ‐0.17] |
| 3.5 Subgroup analysis: treatment dose | 7 | 302 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.34, 1.08] |
| 3.5.1 ≥ 1000 minutes of therapy | 3 | 107 | Std. Mean Difference (IV, Random, 95% CI) | 0.33 [‐0.35, 1.01] |
| 3.5.2 < 1000 minutes of therapy | 4 | 195 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [‐0.78, 1.73] |
| 3.6 Subgroup analysis: type of control group | 7 | 302 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.34, 1.08] |
| 3.6.1 Placebo therapy | 3 | 165 | Std. Mean Difference (IV, Random, 95% CI) | 1.11 [‐0.03, 2.26] |
| 3.6.2 Conventional physical therapy | 1 | 61 | Std. Mean Difference (IV, Random, 95% CI) | 0.38 [‐0.12, 0.89] |
| 3.6.3 Functional activities training | 3 | 76 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐2.02, 1.17] |
| 3.7 Subgroup analysis: duration of observation | 6 | 241 | Std. Mean Difference (IV, Random, 95% CI) | 0.38 [‐0.52, 1.27] |
| 3.7.1 > 3 minutes of observation | 3 | 105 | Std. Mean Difference (IV, Random, 95% CI) | 0.64 [‐1.51, 2.79] |
| 3.7.2 ≤ 3 minutes of observation | 3 | 136 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.50, 0.90] |
| 3.8 Subgroup analysis: upper limb impairment | 5 | 219 | Std. Mean Difference (IV, Random, 95% CI) | 0.59 [‐0.10, 1.28] |
| 3.8.1 Severe | 2 | 151 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.11, 0.53] |
| 3.8.2 Moderate | 2 | 36 | Std. Mean Difference (IV, Random, 95% CI) | 0.98 [‐2.12, 4.09] |
| 3.8.3 Mild, moderate and severe | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | 0.90 [0.17, 1.63] |
| 3.9 Dependence on ADL follow‐up | 2 | 93 | Mean Difference (IV, Random, 95% CI) | ‐0.77 [‐5.43, 3.88] |
3.8. Analysis.

Comparison 3: Action observation versus control: effect on ADL, Outcome 8: Subgroup analysis: upper limb impairment
Comparison 4. Action observation versus control: effect on quality of life.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Quality of life | 2 | 30 | Mean Difference (IV, Random, 95% CI) | 5.52 [‐30.74, 41.78] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Celnik 2008.
| Study characteristics | ||
| Methods | Randomized cross‐over trial | |
| Participants | Methods of recruitment were not reported by authors 9 participants in a cross‐over design with 3 arms:
Inclusion criteria: stroke patients with single unilateral cortical or subcortical lesions Exclusion criteria: there were no exclusion criteria described in the study Mean (SD) age: not reported by authors Stroke details: not reported by authors Stroke phase: chronic |
|
| Interventions |
Physical training group: performed voluntary thumb movements Physical training and congruent AO group: observed a video displaying thumb movements in the same direction to that physically practiced simultaneously Physical training and incongruent AO group: observed a video displaying thumb movements in a direction opposite to that physically practiced simultaneously Sessions were 30 minutes, 3 blocks of 10 minutes each separated by 2‐minute rest |
|
| Outcomes | Outcomes recorded before and after intervention
|
|
| Notes | The authors declared no potential conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The allocation was generated randomly using Excel creating a random session order for each of the subjects and conditions." |
| Allocation concealment (selection bias) | Unclear risk | The author did not make it clear whether there was allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The outcome measures were analyzed by a blinded individual who did not participate in the data acquisition." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | One participant could not complete the protocol due to TMS‐related headache. The reasons were provided, but the exclusion of 1/9 participants in a cross‐over design, with 3 arms, may have affected the reliability of study results. |
| Selective reporting (reporting bias) | Low risk | There is no trial registration, but the outcomes are significant, and there is no selective reporting within the study. |
| Other bias | Low risk | No other potential risk of bias was found. |
Cowles 2013.
| Study characteristics | ||
| Methods | Randomized, controlled, observer‐blind efficacy trial | |
| Participants | All participants were recruited from an inpatient stroke unit 29 participants:
Inclusion criteria: adults who had suffered a stroke between 3 and 31 days before recruitment but with an intact premotor area (ability to encode observed human actions); able to produce some movement in a substantially paretic upper limb as assessed by a score of at least 18 on the Motricity Index but unable to produce a grip force of more than 65% of that of the ipsilesional side; free from observable contralesional upper limb movement deficits attributable to pathology other than stroke Exclusion criteria: patients who had no ability to imitate action with their ipsilesional limb. This ability was assessed by the research therapist who performed an upper limb activity 3 times, and potential participants were asked to observe and then perform the activity. This assessment was digitally filmed and saved onto a computer. An independent assessor viewed the recordings and judged the accuracy of imitation. Mean (SD) age: 77.2 (SD 10.4) years Stroke details: not reported by authors Stroke phase: acute |
|
| Interventions |
Experimental group: additionally watched functional tasks with intent to imitate for 1 to 2 minutes; and then for 4 to 6 minutes performed the activity simultaneously with the therapist Control group: received conventional physical therapy Sessions were 2 × 30‐minute sessions, with 10‐minute rest, for 15 working days |
|
| Outcomes | Outcomes recorded at baseline and within 3 working days of the end of intervention
|
|
| Notes | The authors declared no potential conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Group allocation was computer generated |
| Allocation concealment (selection bias) | Low risk | Details of group allocation were placed into sequentially‐numbered, opaque, sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All measures were made by an assessor blinded to treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 29 participants were randomized. Outcome measures were completed on 13 participants in the control group and 9 in the experimental group (22 participants). Reasons for attrition were provided: moved out of area (one in control group and 4 in experimental group); withdrew from trial (1 in experimental group); medically unwell (1 in experimental group); 1 of the participants in the control group failed to fully comprehend the instructions for the Motricity Index at baseline so this score was missing. Reasons for missing outcome data unlikely to be related to true outcome Where participants withdrew before outcome measured, they were not included in the analysis, and imputation was not used |
| Selective reporting (reporting bias) | High risk | The study protocol is available but not all of the study’s prespecified primary outcomes have been reported. Registered on the Current Controlled Trials Database — ISCRTN 51553998: www.controlled-trials.com/ISR CTN51553998/51553998 |
| Other bias | Low risk | No other potential risk of bias was found. |
Dettmers 2014.
| Study characteristics | ||
| Methods | Pilot randomized controlled trial | |
| Participants | Participants were recruited from 2 hospitals 56 participants:
Inclusion criteria: minimal function of the hand (ability to grip a small object and to release it (extension against gravity at wrist = 20° and at metacarpophalangeal and interphalangeal joints of each of the fingers = 10°), sufficient language abilities to complete the study’s questionnaires, and sufficient cognitive ability to understand and follow instructions for training, distance to the participant's home restricted to 300 km to allow for a follow‐up examination Exclusion criteria: prominent cognitive deficits (Mini Mental State Exam < 24), major depression (Beck Depression Index > 5), major aphasia (Token Test), apraxia (Florida Apraxia Screening Test), neglect (Albert’s Neglect Test), hemianopia, prior infarct, leucoencephalopathy and age below 18 or over 75 years, severe psychiatric disease, severe pulmonary or cardiovascular disease, epilepsy, severe joint deformity (neurological examination) and severe pain Mean (SD) age: video group: 62.79 (no SD reported), text group: 53.89 (14.74), usual care group: 58.83 (11.25). Stroke details:
Stroke phase: acute, subacute, and chronic |
|
| Interventions |
Video group: home‐based training. Participants received a DVD displaying 10 object‐related motor tasks of varying difficulty, each lasting 5 minutes and were requested to imitate the motor tasks, time not reported Text group: home‐based training. Participants performed the same tasks with written instructions without observation/imitation Usual care group: discharged without specific homework Participants were instructed to train 1 hour per day for 6 weeks (video and text groups) |
|
| Outcomes | Outcomes recorded at baseline, postintervention, and at 6 months from treatment conclusion
|
|
| Notes | The authors did not provide any declaration of interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization was done, but there was no information of how it was done |
| Allocation concealment (selection bias) | Unclear risk | There was no information about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but the outcome was not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Wolf Motor Function Test assessment was performed by a blind physiotherapist (low risk). There was no information about blinding other assessment instruments |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 participant was excluded during the intervention because of a recurrent stroke (video group). 1 participant from the text group was unwilling to come to the re‐evaluation. Another 2 participants refused to come to re‐evaluation (usual care group). Nevertheless, the reasons were provided and they had no direct relationship with the outcomes studied, and there was no substantial imbalance in final number of participants in each group considered for analysis. |
| Selective reporting (reporting bias) | High risk | Considering the description of the methodology, the follow‐up investigation was scheduled 12 months after the training, using Motor Activiy Log and Wolf Motor Function Test. However, the results concerning the follow‐up showed that the data were assessed 6 months after the end of the treatment and used as questionnaires the Stroke Impact Scale and Motor Activity Log, when the data of Wolf Motor Function Test were not available. |
| Other bias | Low risk | No other potential risk of bias was found. |
Ertelt 2007.
| Study characteristics | ||
| Methods | Randomized clinical trial | |
| Participants | Participants were recruited from the local Rehabilitation Center 16 participants:
Inclusion criteria: confirmed diagnosis of a first‐ever ischemic stroke in the territory of the medial cerebral artery, sustained more than 6 months prior to entering the study Exclusion criteria: patients older than 76 years, with hemorrhagic stroke or ischemic lesions in the territory of posterior or anterior cerebral artery, impaired level of consciousness (confusion, stupor, coma), severe to moderate aphasia, anosognosia or neglect, amnesia or dementia, depression Mean (SD) age: experimental group: 57.16 (8.73) years and control group: 55.40 (10.77) years Stroke details: first ischemic stroke in the territory of the medial cerebral artery Stroke phase: chronic |
|
| Interventions |
Experimental group: ("action observation therapy"): carefully watched video sequences containing daily life hand and arm actions for 6 minutes that were followed by repetitive practice of the observed actions for another 6 minutes using the same objects as shown in the video film Control group: matched the experimental treatment with the exception that the participants watched sequences of geometric symbols and letters instead of action sequences Sessions were 90 minutes, 18 rehabilitation sessions on consecutive working days |
|
| Outcomes | Outcomes recorded at baseline, postintervention, and 8 weeks after the end of intervention
|
|
| Notes | The authors did not provide any declaration of interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization was done, but no information of how it was done |
| Allocation concealment (selection bias) | Unclear risk | Authors did not report if there was allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Authors did not report if there was blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no exclusion of participants after randomisation. fMRI measurements were analyzed in 7 participants in the experimental group and 6 participants in the control group. |
| Selective reporting (reporting bias) | Low risk | There is no trial registration, but the outcomes were significant, and there was no selective reporting within the study. |
| Other bias | Low risk | No other potential risk of bias was found. |
Franceschini 2012.
| Study characteristics | ||
| Methods | Randomized controlled observer‐blind trial | |
| Participants | Eligible hemiparetic stroke survivors from 13 rehabilitation centers were recruited Franceschini 2012 paper: 102 participants:
Inclusion criteria: participants with first‐ever stroke, enrolled 30 days (±7) after the event onset with ischemia or primary hemorrhage, right‐handed prior to stroke Exclusion criteria: posterior circulation infarction, subarachnoid hemorrhage, severe forms of neglect and anosognosia (number of errors in Bell Barrage test ≥ 15), impaired comprehension (Token test score ≤ 17), history of endogenous depression or serious psychiatric disorders, and severe visual deficits (restricting the access to visual stimuli) Mean (SD) age: experimental group: 67.0 (12.4) years; control group: 65.7 (11.9) years Stroke details: etiology ‒ control group: 9 hemorrhagic, 40 ischemic; experimental group: 16 hemorrhagic, 37 ischemic. Lesion side: control group: 18 right, 24 left; experimental group: 22 right, 26 left Stroke phase: acute Sale 2014 paper: 67 participants:
Inclusion criteria: moderate‐to‐severe upper limb paresis, first‐ever ischemic stroke, 30 days (±7) after the event, right handed prior to stroke, unilateral brain lesions Exclusion criteria: posterior circulation infarction, subarachnoid hemorrhage, severe forms of neglect and anosognosia, impaired comprehension or dementia, history of endogenous depression or serious psychiatric disorders, severe visual deficits, bilateral motor impairment, severe sensory deficits in the paretic upper limb, refusal or inability to provide informed consent, other concomitant severe medical problems Mean (SD) age: 66.5 (12.7) years Stroke details: ischemic Stroke phase: acute |
|
| Interventions |
Experimental group: observation of 1 daily routine task (actions) carried out with the upper limb, each action consisted of 3 different meaningful motor sequences (3 minutes each). After observing the video, the participant should perform, with their paretic upper limb, the same movement (2 minutes each), with help when needed Control intervention: observation of 5 static images displaying objects, without any animal or human being (different 3‐minute sequences). Then, the participants had to perform limb movements for 2 minutes according to a standard sequence, simulating those performed by the other group Sessions were 2 × 15 minutes, daily (with 60‐minute interval), 5 days/week, for 4 consecutive weeks (in addition to 3 hours of standard rehabilitation) |
|
| Outcomes |
Franceschini 2012 paper: Outcomes recorded at baseline, postintervention and at 4 to 5 months from treatment conclusion
Sale 2014 paper: Outcomes recorded at baseline, postintervention and at 4 to 5 months from treatment conclusion
|
|
| Notes | There are 2 publications for this study. The authors declared no potential conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Central randomisation |
| Allocation concealment (selection bias) | Low risk | Participants and investigators enrolling participants could not foresee assignment because central allocation was used to conceal allocation |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All assessments were performed by trained professional not involved in the research treatment and blind to group allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 12 participants were excluded postrandomization, 5 from experimental group and 7 from control group. Reasons were not reported. There was an imbalance of 6 participants in final number of participants in each group considered for analysis |
| Selective reporting (reporting bias) | Low risk | There is no trial registration, but the outcomes are significant, and there is no selective reporting within the study |
| Other bias | Low risk | No other potential risk of bias was found. |
Fu 2017.
| Study characteristics | ||
| Methods | Randomized clinical trial | |
| Participants | Stroke patients who were hospitalized in Zhejiang Jiaxing Second Hospital Rehabilitation Center between June 2014 and September 2016 were recruited in this study 70 participants:
Inclusion criteria: unilateral hemiplegia, first‐episode of cerebral infarction determined by CT and MRI, stable vital signs, disease course of 2 to 6 months, age of 40 to 75 years; Mini Mental State Exam score ≥ 27 and treatment instructions can be performed, Fugl‐Meyer Assessment score ≥ 20 for upper extremity motor function, binocular vision or corrected visual acuity ≥ 1.0, everyday treatment can be tolerated, and providing informed consent and willingness to participate in the study Exclusion criteria: cerebral hemorrhage, subarachnoid hemorrhage, venous sinus thrombosis, transient ischemic attack, and progressive or reversible ischemic cerebral apoplexy; lesions located in bilateral cerebral hemisphere, cerebellum, or brain stem; joint and other diseases affecting patients sitting or active; heart, lung, liver, kidney, and other serious diseases; metal implantation in the body; a history of epilepsy; and skull defect Mean (SD) age: experimental group: 62.04 (9.93) years, control group: 59.76 (10.57) years Stroke details: etiology ‐ ischemic; hemiplegia: control group: 13 right, 12 left; experimental group: 12 right, 16 left Stroke phase: subacute |
|
| Interventions |
Experimental group: traditional rehabilitation treatment such as Bobath, Brunnstrom, proprioceptive neuromuscular facilitation, and daily activity ability training. In addition participants were requested to watch upper limbs motion video and required to imitate the action in the video. There were 30 actions in the video, including shoulder joint, elbow joint, wrist joints, forearm, and hand movements in all directions Control group: traditional rehabilitation treatment such as Bobath, Brunnstrom, proprioceptive neuromuscular facilitation, and daily activity ability training. In addition they watched different geometric patterns and digit symbol, and did the action picked from the 30 actions in the video. In both groups sessions were 20 minutes, 6 days/week, for 8 weeks |
|
| Outcomes | Outcomes recorded at baseline and postintervention
|
|
| Notes | The authors declared no potential conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | High risk | Authors did not report if there was allocation concealment, but randomisation type classifies the allocation concealment as high risk |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | There was no blinding of participants and personnel, but this item is not essential for this review |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessments were made by 2 trained professional therapists and the whole process was recorded. Subsequently, the average score from another 2 trained professional therapists was used for the analyses |
| Incomplete outcome data (attrition bias) All outcomes | High risk | There were 7 exclusions from the experimental group and 10 from the control group after randomisation, which corresponded to more than 10% and may compromise the results. Reasons were not reported |
| Selective reporting (reporting bias) | Low risk | There is no trial registration, but the outcomes are significant, and there is no selective reporting within the study. |
| Other bias | Low risk | No other potential risk of bias was found. |
Harmsen 2015.
| Study characteristics | ||
| Methods | Randomized clinical trial | |
| Participants | Patients were recruited from the outpatient clinic of Rijndam Rehabilitation Centre in Rotterdam, the Netherlands 37 participants:
Inclusion criteria: Brunnstrom score for upper‐extremity function between III and VI, a home‐dwelling status, and at least 6 months poststroke Exclusion criteria: presence of neglect, comorbidities that influence voluntary upper‐extremity function, or multiple strokes Mean (SD) age: experimental group: 57 (10.4) years, control group: 60 (8.8) years Stroke details: experimental group: 13 ischemic, 5 hemorrhagic; control group: 12 ischemic, 7 hemorrhagic Stroke phase: chronic |
|
| Interventions |
Experimental group (mirror therapy–based AO): sets of affected‐arm reaching movements, alternated with periods of observation. Participants observed mirrored video tapes (the video screen was positioned in the midsagittal plane) of reaching movements performed by their unaffected arm. Control group: sets of affected‐arm reaching movements, alternated with periods of observation. Participants observed static photographs of landscapes (the video screen was positioned in the midsagittal plane). Participants trained for 1 day: 3 minutes of AO, 30 repetitions of reaching, 1 minute of AO, 20 repetitions of reaching, 1 minute of AO, 20 repetitions of reaching, and 1 last minute of AO |
|
| Outcomes | Outcome recorded at baseline and postintervention
|
|
| Notes | The authors declared no potential conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random code using blocks of 20 participants |
| Allocation concealment (selection bias) | Unclear risk | Use of sealed envelopes. Authors did not report if envelopes were opaque or sequentially numbered. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Authors did not report if there was blinding of outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdraw was reported. There was no loss of data after intervention |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and the outcomes were reported in accordance with what has been proposed DOI 10.1186/ISRCTN40128145 |
| Other bias | Low risk | No other potential risk of bias was found. |
Hsieh 2020.
| Study characteristics | ||
| Methods | Pilot randomized clinical trial | |
| Participants | Subacute stroke patients (1 to 6 months from onset) 21 participants:
Inclusion criteria: diagnosis of cerebral ischemic or hemorrhagic stroke, 1 to 6 months since unilateral stroke onset, age between 20 and 80 years, baseline score of the Fugl‐Meyer Assessment between 20 and 60, ability to follow the study instructions (assessed by the Taiwan version of the Montreal Cognitive Assessment), and ability to participate in study therapy and assessment sessions Exclusion criteria: global or receptive aphasia, severe neglect, or major medical problems or comorbidities that influenced the usage of the upper limbs or caused severe pain Mean (SD) age: experimental group: 52.77 (11.25) years, control group: 54.30 (13.61) years Stroke details
Stroke phase: subacute |
|
| Interventions |
AO group: Phase 1 (10–15 minutes) ‐ patients watched upper limb active range of motion exercises and executed observed exercises with both arms and hands simultaneously. Phase 2 (15–20 minutes) ‐ patients watched one reaching movement or one object manipulation task for 2 minutes, and executed the movements that they had observed for 3 minutes; this sequence was repeated 3 times. Phase 3 (30 minutes) ‐ patients watched one functional task in each session (folding a towel, wiping a table, drinking water, opening a small drawer, and using a mobile phone) for 2 minutes and executed the action they had observed for 3 minutes; this sequence was repeated 3 times Mirror therapy group: patients were seated in front of a mirror box placed at their midsagittal plane. The affected arm of the participants was placed inside the mirror box, and the unaffected arm was in front of the mirror. The patient was instructed to watch the mirror reflection of the movement performed by his/her unaffected hand carefully and to imagine that the movement was performed by the affected hand. The participant was also encouraged to move the affected arm and hand as much as they could. In the mirror therapy group, treatment activities also contained active range of motion exercises (10–15 minutes), reaching movement or object manipulation (15–20 minutes), and functional task practice (30 minutes) Control group: dose‐matched bilateral arm training, but no video input or mirror box was provided for this group. The same 3 categories of movements and tasks as provided in the AO group were used. Treatment programs also included active range of motion exercises (10–15 minutes), reaching movement or object manipulation (15–20 minutes), and functional task practice (30 minutes). During training, patients were required to move both of their arms and hands simultaneously as possible In all groups sessions were 5 days/week, for 3 weeks |
|
| Outcomes | Outcomes recorded at baseline, postintervention, and 3 months follow‐up
|
|
| Notes | The authors declared no potential conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization was carried out using an online web‐based randomisation tool |
| Allocation concealment (selection bias) | Low risk | For concealment of allocation, randomisation procedure and assignment were managed by an independent research assistant who was not involved in participants' screening or evaluation. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All outcome measures were administered to the patients by the same rater, who was blinded to the group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts were recorded at follow‐up (3 months after treatment), but none after therapy. This study used an intention‐to‐treat analysis. For missing data, the last observation carried forward method was used. |
| Selective reporting (reporting bias) | High risk | This trial is registered with NCT02871700. Registry contains some outcomes not reported in manuscript: Modified Rankin scale, Wolf Motor function Test, Medical Research Council scale, Motor Activity Log, Chedoke Arm and Hand Activity Inventory, Revised Nottingham Sensory Assessment, ABILHAND questionnaire, Actigraphy, Magnetoencephalography, Visual Analogue Scale for pain and fatigue. Authors justified a lack of resources. However, some of the outcomes were questionnaires, which did not need resources. |
| Other bias | Low risk | No other potential risk of bias was found. |
Jin‐Woo 2011.
| Study characteristics | ||
| Methods | Randomized clinical trial | |
| Participants | Chronical stroke patients 13 participants:
Inclusion criteria: stroke diagnosis by a medical rehabilitation specialist; more than 6 months from the event; more than 24 points in Mini Mental State Examination; more than 34 points on the Motor‐Free Visual Perception Test; ability to pick up a 2.5 cm square with the affected hand, to communicate and follow instructions; not diagnosed with specific psychiatric findings of mental illness by a psychiatrist Exclusion criteria: not reported Mean (SD) age: experimental group: 63.2 (11.7) years, control group: 57.2 (10.2) years Stroke details
All right‐handed Stroke phase: chronic |
|
| Interventions |
Experimental group: participants sat in a quiet room, looking at a computer screen (13 inches) 30 cm ahead. The therapist provided verbal commands about the characteristics and movements needed to carry out the tasks. After observation (5 minutes), the subjects repeatedly imitated the movement observed with the object shown in the video for about 10 minutes. 2 tasks per session were included The tasks were upper limb movements related to a functional activity Control group: participants sat on chairs in front of a table. The therapist presented a functional activity task and verbally explained the characteristics and movements required for the task. Each task was repeated intensively for 15 minutes. 2 tasks were performed per session. The tasks were the same selected for the AO training In both groups sessions were 30 minutes/day, 3 times/week, for 3 weeks |
|
| Outcomes | Outcomes recorded at baseline and postintervention
|
|
| Notes | The authors did not provide any declaration of interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Authors do not describe how randomisation was done. |
| Allocation concealment (selection bias) | Unclear risk | Authors did not report if there was allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Authors did not report if there was blinding of outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdraw was reported. There was no loss of data after intervention. |
| Selective reporting (reporting bias) | Low risk | There is no trial registration. Outcomes are significant. There is no selective reporting within the study. |
| Other bias | Low risk | No other potential risk of bias was found. |
Kim 2015.
| Study characteristics | ||
| Methods | Non‐equivalent pretest/post‐test control group design | |
| Participants | Methods of recruitment were not reported by authors 12 participants:
Inclusion criteria: participants diagnosed as having hemiplegia due to stroke Exclusion criteria: there were no exclusion criteria described in the study Mean (SD) age: not reported by authors Stroke details: not reported by authors Stroke phase: not reported by authors |
|
| Interventions |
Control group: participants received traditional occupational treatment and topological treatment in which they performed purposeful AO program assignments without actually observing the purposeful actions Experimental group: participants received traditional occupational treatment and also performed a purposeful AO training program AO training was 30 minutes/session, 5 sessions/week for 6 weeks, a total of 30 sessions |
|
| Outcomes | Outcome recorded after and before intervention
|
|
| Notes | The authors did not provide any declaration of interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization was done, but there was no information of how it was done. |
| Allocation concealment (selection bias) | Unclear risk | Authors did not report if there was allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Authors did not report if there was blinding of outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no loss of outcome data or dropouts. |
| Selective reporting (reporting bias) | Low risk | There is no trial registration, but the outcomes are significant, and there is no selective reporting within the study. |
| Other bias | High risk | The article does not say how long after the evaluation the treatment began nor how long after the intervention the revaluation was performed. |
Kim 2016a.
| Study characteristics | ||
| Methods | Randomized clinical trial | |
| Participants | Methods of recruitment were not reported by authors 22 participants:
Inclusion criteria: aged between 18 and 70 years with a first‐time ischemic or hemorrhagic stroke; stroke experienced more than 1 month and less than 6 months before the study; sufficient cognition to participate in the study: a Mini Mental State Exam scores of 24 or higher; no excessive spasticity, defined as a grade of 3 or higher on the Modified Ashworth Scale Exclusion criteria: patients with any comorbidity or disability other than stroke that precluded upper‐extremity training; any uncontrolled health condition for which exercise was contraindicated Mean (SD) age: AO training group: 60.77 (7.03); task‐oriented training group: 59.11 (7.05) Stroke details: AO training group: 9 ischemic, 2 hemorrhagic; task‐oriented training group: 7 ischemic, 4 hemorrhagic Stroke phase: subacute |
|
| Interventions |
AO training group: participants watched video tasks for 9 minutes, had a 1‐minute break to organize their thoughts and practiced the task‐oriented training for 30 minutes Task‐oriented training group: participants performed tasks based on ADL for 30 minutes, without watching the video Sessions were 5 times/week for 4 weeks |
|
| Outcomes | Outcomes recorded after and before intervention
|
|
| Notes | The authors did not provide any declaration of interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated random number was used to allocate participants. |
| Allocation concealment (selection bias) | Low risk | Authors did not report if there was allocation concealment, but randomisation type classifies the allocation concealment as low risk. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The evaluator was not aware of the treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no exclusion of participants after randomisation. |
| Selective reporting (reporting bias) | Low risk | There is no trial registration, but the outcomes are significant, and there is no selective reporting within the study. |
| Other bias | Low risk | No other potential risk of bias was found. |
Kuk 2016.
| Study characteristics | ||
| Methods | Randomized clinical trial | |
| Participants | Methods of recruitment were not reported by authors 20 participants:
Inclusion criteria: > 6 months since stroke onset, no other neurological and orthopedic impairments, no cognitive impairment (> 24 points in Mini Mental State Exam ‒ Korean version) and ability to grasp a small cube (2.5 cm × 2.5 cm × 2.5 cm). Exclusion criteria: there were no exclusion criteria described in the study Mean (SD) age: experimental group: 60.00 (9.36) years; control group: 59.70 (6.58) years Stroke details: experimental group: 5 ischemic, 5 hemorrhagic; control group: 6 ischemic, 4 hemorrhagic Stroke phase: chronic |
|
| Interventions |
Experimental group: participants observed the action of placing wooden blocks from 1 side of the box to another for 1 minute followed by performing the same motor task for 3 minutes Control group: participants observed landscapes for 1 minute followed by performing motor task of placing wooden blocks from 1 box to another for 3 minutes 5 sessions with 10‐minute rest intervals between the sessions |
|
| Outcomes | Outcomes recorded at baseline and postintervention
|
|
| Notes | The authors declared no potential conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation was generated by flipping a coin |
| Allocation concealment (selection bias) | Unclear risk | Authors did not report if there was allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Authors did not report if there was blinding of outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was one exclusion for each group after randomisation; however, it was less than 10% of the sample, which did not compromise the results. |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were prespecified. |
| Other bias | Low risk | No other potential risk of bias was found. |
Lee 2013.
| Study characteristics | ||
| Methods | Randomized clinical trial | |
| Participants | Methods of recruitment were not reported by authors 33 participants:
Inclusion criteria: patients with stroke at least 6 months earlier who were assessed as having recovered to Brunnstrom stage 5, scored at least 20 points in the Korean Mini Mental State Exam, were able to understand and perform instructions, had visual acuity that was sufficient for watching videos, and right hemiplegic patients Exclusion criteria: there were no exclusion criteria described in the study Mean (SD) age: AO group: 63 (3.7) years, action practice group: 62 (1.5) years, combined Ao and action practice group: 61 (2.3) years, and control group: 60 (5.9) years Stroke details: not reported by authors Stroke phase: chronic |
|
| Interventions |
AO group: watched a drinking task video 20 times in 10 minutes and imagined they were performing the same task at the same time as they watched the video Action practice group: repeatedly practiced a drinking task for 10 minutes AO and action practice group: watched the task video for 5 minutes and practiced the actions for 5 minutes Control group: neither watched the video nor practiced the actions Sessions were 10 minutes/day for 3 weeks, 15 days total |
|
| Outcomes | Outcomes recorded at baseline, postintervention and 1 week after the end of intervention
|
|
| Notes | The authors did not provide any declaration of interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization was cited in abstract, but there was no information of how it was done |
| Allocation concealment (selection bias) | Unclear risk | Authors did not report if there was allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Physical therapist who conducted the assessments did not have any information about the experimental group of participants |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no exclusion of participants after randomisation and no loss of outcome data. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement of 'low risk' or 'high risk' |
| Other bias | Low risk | No other potential risk of bias was found. |
Mancuso 2021.
| Study characteristics | ||
| Methods | Randomized clinical trial | |
| Participants | Acute stroke patients (at a maximum of 30 days from onset) clinically evaluated by a neurologist and that underwent a CT brain scan 32 participants:
Inclusion criteria: both genders, any education level, aged from 18 to 90 years old, first‐ever stroke, unilateral cerebral lesion, upper limb impairment, and at a maximum of 30 days from onset, and ability to understand spoken language (Token Test score higher than 8) Exclusion criteria: subarachnoid hemorrhage, severe neglect at the Star Cancellation from the Behavioural Inattention Test (a score lower than 51), impaired comprehension (a score lower than 8 in the Token Test), ideomotor apraxia, cognitive decline (a score lower than 23.8 in the Mini Mental State Examination), history of endogenous depression or severe psychiatric disorders for which patients needed chronic pharmacotherapy, or severe visual deficits (eye field examination of the National Institutes of Health Stroke Scale) Median (IQR) age: experimental group: 76.5 (13.7) years, control group: 64.5 (15.75) Stroke details: Hemiparesis: experimental group: 7 right and 9 left; control group: 8 right and 8 left Stroke phase: acute |
|
| Interventions |
Experimental group: conventional therapy (60 minutes ‐ training for transfers, mobility, walking up and down steps, balance tasks, tailored functional tasks for the upper limbs (unimanual and bimanual), joint and soft tissue mobilization, and specific sensory stimulation) + AO (30 minutes). Participants were asked to carefully observe the videos for 3 minutes in order to prepare themselves to imitate the presented action. At the end of each sequence, participants performed the same movement with the paretic upper limb over a time period of 2 minutes. 3 minutes of sequence observation and 2 minutes of action performance for 3 motor sequences, repeated twice Control group: conventional therapy (60 minutes) + task oriented therapy (30 minutes). Participants performed functional activities with the upper limbs, using the same objects as AO, in both unimanual and bimanual modalities, without watching the video beforehand In both groups, each session was 190 minutes (60 minutes of conventional treatment + 30 minutes of AO or task oriented training), 5 days per week, for 4 weeks |
|
| Outcomes | Outcomes recorded at baseline and postintervention
|
|
| Notes | The authors declared no potential conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated random number was used to allocate participants arbitrarily to the AO training group or the control group. |
| Allocation concealment (selection bias) | Low risk | The randomisation procedure and assignment were managed by an independent researcher who was not involved in the evaluation of the participants. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All assessments were performed by trained researchers not involved in the treatment administration and blinded to the patient’s allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts were recorded during the treatment, and all participants fulfilled the protocol. |
| Selective reporting (reporting bias) | Low risk | The study was registered on ClinicalTrials.gov, with the number NCT04604171. Registry contains all reported outcomes |
| Other bias | Low risk | No other potential risk of bias was found. |
Younghwa 2013.
| Study characteristics | ||
| Methods | Randomized clinical trial | |
| Participants | Patients diagnosed with stroke by imaging (CT or MRI) who were admitted to Hospital D in Busan and received occupational therapy from January 2013 to April 2013 30 participants:
Inclusion criteria: patients who understood the purpose of this study and agreed to participate Exclusion criteria: no cognitive impairment with a score of 24 or greater on the Korean version of the Mini Mental State Examination, no other neurological disorders or orthopedic damage, and normal vision, hearing, and sensation Age. Experimental group: 30‐39 years – 2 patients, 40‐49 years – 1 patient, 50‐59 years – 3 patients, over 60 years – 8 patients. Control group: 30‐39 years – 2 patients, 40‐49 years – 3 patients, 50‐59 years – 3 patients, over 60 years – 7 patients Stroke details
Stroke phase: acute, subacute and chronic |
|
| Interventions |
Experimental group: participants watched a 3‐4 minute video. After observation, the movement was imitated by the participant, including: turning on a faucet, opening a bottle cap, folding a towel, moving around, putting on and taking off clothes, washing hands and applying lotion. 10‐15 minutes per movement (observing and imitating), 2 movements per day, totaling 20‐30 minutes per day Control group: training consisted of four tasks: putting on and taking off clothes, eating, decorating and moving the wheelchair. During execution, verbal commands and guidance on the activities were given and, after the completion of a movement, feedback on the activity was given. One task was applied at a time and repeated for 30 minutes. In both groups sessions were 4 days per week, for 6 weeks |
|
| Outcomes | Outcomes recorded at baseline and postintervention
|
|
| Notes | The authors did not provide any declaration of interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Authors do not describe how randomisation was done. |
| Allocation concealment (selection bias) | Unclear risk | Authors did not report if there was allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Authors did not report if there was blinding of outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdraw was reported. There was no loss of data after intervention. |
| Selective reporting (reporting bias) | Low risk | There is no trial registration. There is only one outcome, but significant, and there is no selective reporting within the study. |
| Other bias | Low risk | No other potential risk of bias was found. |
Zhu 2015.
| Study characteristics | ||
| Methods | Randomized clinical trial | |
| Participants | Stroke patients hospitalized in Jiaxing Rehabilitation Medical Center were recruited 70 participants:
Inclusion criteria: patients who met the diagnosis for stroke formulated in the 4th National Academic Conference on Cerebrovascular Disease in 1995, and were confirmed as having a stroke upon computed tomography or magnetic resonance imaging; first‐episode patients who began rehabilitation therapy within 6 months, for whom the sitting balance was ≥ Level 1, and the Fugl‐Meyer Assessment score was ≥ 15 for upper extremity motor function; patients with a stable condition; patients with a normal Kinesthetic and Visual Imagery Questionnaire score; patients who were 42 to 75 years of age; patients who provided informed consent and were willing to participate in the study Exclusion criteria: patients with cognitive impairment mini‐mental state examination score of < 24 in patients with a junior high school education or < 17 if illiterate; patients with severe upper limb spasticity; patients with severe bone joint malformation or myopathy; patients with severe diseases of the heart, lung, liver, or kidney Mean (SD) age: experimental group: 57.75 (15.57) years, control group: 56.89 (14.93) years Stroke details: not reported by authors Stroke phase: acute |
|
| Interventions |
Experimental group: additionally watched a video showing a specific action of the upper limb and then performed the same exercise after watching 30 videos Control group: received conventional drug treatment and traditional physical and occupational therapy Control group received conventional therapy 2 to 5 hours per day, 6 times/week for 8 weeks. Experimental group had additional 30 minutes/day, 6 times/week, for 8 weeks |
|
| Outcomes | Outcomes recorded at baseline and postintervention
|
|
| Notes | The authors declared no potential conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | High risk | Authors did not report if there was allocation concealment, but randomisation type classifies the allocation concealment as high risk. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Evaluators were unaware of the participant grouping status and did not participate in the treatment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 9 participants were excluded from analysis: 4 from experimental group and 5 from control group. Participants were excluded for absence on 3 consecutive days of intervention and aggravated condition of the participant. Nevertheless the reasons were reported and they have no direct relationship with the outcomes studied, and there is not a substantial imbalance in final number of participants in each group considered for analysis. |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were prespecified. |
| Other bias | Low risk | No other potential risk of bias was found. |
ADL: activities of daily living AO: action observation CT: computed tomography fMRI: functional magnetic resonance MEP: motor evoked potential MRI: magnetic resonance imaging SD: standard deviation TMS: transcranial magnetic stimulation IQR: interquartile range TMS: transcranial magnetic stimulation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Brunner 2014 | Study design: not a RCT |
| Cha 2015 | Study design: not a RCT |
| Chang 2017 | The intervention was mirror therapy |
| Emmerson 2017 | The intervention was home exercise programs including techniques, such as constraint‐induced movement therapy, repetitive task‐specific training, mirror therapy, and bilateral training |
| Ertelt 2012 | It is a protocol without results |
| Franceschini 2010a | Study design: not a RCT |
| Frenkel‐Toledo 2014 | Study design: not a RCT |
| Kim 2010 | Study design: not a RCT |
| Kim 2013a | Did not assess upper limb, but trunk and lower limb function |
| Kim 2013b | Did not assess upper limb, only lower limb |
| Kim 2014 | Study design: not a RCT |
| Kim 2016b | Used AO associated with interface‐based electrical stimulation |
| Ko 2014 | The control and experimental group performed AO |
| Lee 2016 | Irrelevant intervention: experimental group performed remote movement observation training based on telerehabilitation |
| Liepert 2014 | Study design: not a RCT |
| Lima 2020 | Study design: not a RCT |
| Lubart 2017 | The control and experimental group performed AO |
| Marangon 2014 | Study design: not a RCT |
| Sale 2012 | Study design: not a RCT |
| Shih 2017 | It is a protocol without results |
| Sugg 2015 | Study design: not a RCT |
| Sun 2016 | Used AO associated with motor imagery |
| Szameitat 2012 | Study design: not a RCT |
| Wright 2014 | Used AO associated with motor imagery |
| Yun 2011 | Study design: not a RCT |
AO: action observation; RCT: randomized controlled trial
Characteristics of ongoing studies [ordered by study ID]
NCT02235350.
| Study name | Study on the effectiveness of action observation treatment as a rehabilitation tool in acute stroke patients and in chronic stroke patients with apraxia: a randomized controlled trial |
| Methods | Randomized controlled trial |
| Participants | First‐ever ischemic or hemorrhagic stroke confirmed by CT/MRI, no later than 30 days from acute event, or chronic stroke patients (more than 3 months from the acute event) with apraxia. Aged 18 to 85 years. Upper limb plegia or paresis with muscle strength in grasping ‐ MRC < 4. Ability to understand and carry out simple verbal instruction. Mini Mental State Examination = 20 |
| Interventions |
Experimental group: AO Control group: observation of videos with no motor content |
| Outcomes |
|
| Starting date | June 2014 |
| Contact information | buccino@unicz.it |
| Notes | Date accessed: October 2017 The author did not provide any declaration of interests. |
NCT04015271.
| Study name | Feasibility of action observation and repetitive task practice on upper extremity outcomes in chronic stroke survivors |
| Methods | Randomized controlled trial |
| Participants | Aged 18 to 85 years. Experienced a stroke resulting in a Upper Extremity Fugl Meyer score >17 < 49; experienced a poststroke > 6 months; > 24 on the Folstein Mini Mental Status Examination Experienced only one stroke; discharged from all forms of physical rehabilitation intervention Visual acuity of 20/50 or greater with or without corrective lenses; > 19 on the Hooper Visual Organization Test Unilateral stroke only; cerebral stroke; age of onset of stroke greater than 18 years old |
| Interventions |
Experimental group: AO + repetitive task practice Placebo comparator: placebo video + repetitive task practice |
| Outcomes |
|
| Starting date | 27 June 2019 |
| Contact information | John Buford, PT, PhD, Ohio State University |
| Notes | Date accessed: May 2021 The author did not provide any declaration of interests. |
NCT04047134.
| Study name | Neuroimaging biomarkers toward a personalized upper limb action observation treatment in chronic stroke patients (BE‐TOP) |
| Methods | Randomized controlled trial |
| Participants | Aged 18 to 80 years; chronic stroke (never experienced AO treatment); first‐ever unilateral stroke due to ischemia provoking a clinically evident upper limb/hand deficit; diagnosis verified by brain imaging (MRI); cognitive function sufficient to understand the experimental instructions; Chedoke‐McMaster stroke Assessment Scale score greater than 1; informed written consent to participate in the study |
| Interventions |
Experimental group: AO treatment Control group: observation of videos with non‐motor contents |
| Outcomes |
|
| Starting date | 1 July 2019 |
| Contact information | Francesco Infarinato, PhD |
| Notes | Date accessed: May 2021. The author did not provide any declaration of interests. |
NCT04574687.
| Study name | Effects of action observation therapy on fine motor skills of upper limb functions in chronic stroke patients |
| Methods | Randomized controlled trial |
| Participants | Aged 30 to 70 years, first‐ever stroke, enroled 6 months after the event onset with ischemia or primary hemorrhage. All patients were right handed prior to stroke |
| Interventions |
Experimental group: AO Control group: neurodevelopmental techniques |
| Outcomes |
|
| Starting date | 15 September 2019 |
| Contact information | Maryam Shabbir, PhD, Riphah International University |
| Notes | Date accessed: May 2021 The author did not provide any declaration of interests. |
NCT04943601.
| Study name | Action observation therapy for stroke |
| Methods | Randomized controlled trial |
| Participants | Male and female aged 40‐75 years; acute phase of stroke (< 3 months); without cognitive impairments (Mini‐Mental State Examination > 23); no visual or auditory abnormalities; preserved visual acuity; middle cerebral artery infarction; Fugl‐Meyer assessment score ≥ 20 for upper extremity status Dominant hand |
| Interventions |
Experimental: AO training group Active comparator: conventional therapy group |
| Outcomes |
|
| Starting date | 1 December 2020 |
| Contact information | Imran Amjad, PhD imran.amjad@riphah.edu.pk Ayesha Afridi, PhD ayesha.afridi@riphah.edu.pk |
| Notes | Date accessed: November 2021. The author did not provide any declaration of interests. |
AO: action observation CT: computed tomography EEG: electroencephalography fMRI: Functional Magnetic Resonance MEG: magnetoencephalography MRC: Medical Research Council MRI: magnetic resonance imaging sEMG: surface electromyography
Differences between protocol and review
There were a number of differences between what we planned in the protocol and the final review. Sensitivity analysis should be conducted after removing trials with high risk of allocation concealment and blinding of outcome assessment. We did this, disregarding only two trials that exhibited high risk of bias for allocation concealment. Furthermore we carried out two sensitivity analyses to determine whether the effect of AO changed with the mode of application: one removing trials in which therapy took place in the participants’ home, and the other in which the action was demonstrated by the therapist and not through video.
We also intended to conduct subgroup analysis considering the type of treatment, as follows: one subgroup in which therapy was based on AO alone and another where observation was followed by physical exercise. However, there were no trials that applied AO alone to upper limb motor function; and therefore we decided to conduct subgroup analysis considering the types of control groups (placebo, conventional physiotherapy, and with no specific therapy). We performed another subgroup analysis considering the duration of observation.
Although not foreseen in the protocol, we also conducted a subgroup analysis based on upper limb motor impairment.
When updating this review, the search of other resources did not include conference proceedings, as the search in databases, newspapers, and citation indexes captured abstracts published in relevant events. We decided not to update Rehabdata due to the small number of trials found on this database in the first version of this review. It was necessary to use another search strategy for the Lilacs database (Latin American and Caribbean Health Sciences Literature; Appendix 5) to complete the search for theses, dissertations, and other records.
Contributions of authors
Lorenna Borges (LB): conducted the review, assessed risk of bias and certainty of the evidence, performed statistical analyses, interpreted the results, and was responsible for writing the review.
Aline Fernandes (AF): data extraction and assessment of risk of bias. She also helped in methodological planning and contributed to writing the review.
Jacilda Passos (JP): study selection and data extraction. She also revised the manuscript.
Tania Campos (TC): was the reviewing judge, helped interpret the results. She also revised the manuscript.
Isabelle Rego (IR): study selection and data extraction. She also revised the manuscript.
Sources of support
Internal sources
Department of Physical Therapy, Federal University of Rio Grande do Norte, Brazil
External sources
No sources of support provided
Declarations of interest
Lorenna RDM Borges: none known Aline Fernandes: none known Jacilda Passos: none known Isabelle Rego: none known Tania F Campos: none known
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Celnik 2008 {published and unpublished data}
- Celnik P, Webster B, Glasser DM, Cohen LG. Effects of action observation on physical training after stroke. Stroke 2008;39(6):1814-20. [DOI: 10.1161/STROKEAHA.107.508184] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cowles 2013 {published and unpublished data}
- Cowles T, Clark A, Mares K, Peryer G, Stuck R, Pomeroy V. Observation-to-imitate plus practice could add little to physical therapy benefits within 31 days of stroke: translational randomized controlled trial. Neurorehabilitation and Neural Repair 2013;27(2):173-82. [DOI: 10.1177/1545968312452470] [DOI] [PubMed] [Google Scholar]
Dettmers 2014 {published and unpublished data}
- Dettmers C, Nedelko V, Hassa T, Starrost K, Schoenfeld MA. Video therapy: promoting hand function after stroke by action observation training – a pilot randomized controlled rial. International Journal of Physical Medicine and Rehabilitation 2014;2(189):2. [2329-9096] [Google Scholar]
Ertelt 2007 {published and unpublished data}
- Ertelt D, Hemmelmann C, Dettmers C, Ziegler A, Binkofski F. Observation and execution of upper-limb movements as a tool for rehabilitation of motor deficits in paretic stroke patients: protocol of a randomized clinical trial. BMC Neurology 2012;12(1):42. [DOI: 10.1186/1471-2377-12-42] [DOI] [PMC free article] [PubMed] [Google Scholar]
Franceschini 2012 {published and unpublished data}
- Franceschini M, Ceravolo MG, Agosti M, Cavallini P, Bonassi S, Dall’Armi V, et al. Clinical relevance of action observation in upper-limb stroke rehabilitation a possible role in recovery of functional dexterity. A randomized clinical trial. Neurorehabilitation and Neural Repair 2012;26(5):456-62. [DOI: 10.1177/1545968311427406] [DOI] [PubMed] [Google Scholar]
- Sale P, Ceravolo MG, Franceschini M. Action observation therapy in the subacute phase promotes dexterity recovery in right-hemisphere stroke patients. BioMed Research International 2014;2014:1-7. [DOI: 10.1155/2014/457538] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fu 2017 {published data only}
- Fu J, Zeng M, Shen F, Cui Y, Zhu M, Gu X, et al. Effects of action observation therapy on upper extremity function, daily activities and motion evoked potential in cerebral infarction patients. Medicine 2017;96(42):1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harmsen 2015 {published and unpublished data}
- Harmsen WJ, Bussmann JB, Selles RW, Hurkmans HL, Ribbers GM. A mirror therapy-based action observation protocol to improve motor learning after stroke. Neurorehabilitation and Neural Repair 2015;29(6):509-16. [DOI: 10.1177/1545968314558598] [DOI] [PubMed] [Google Scholar]
Hsieh 2020 {published data only}
- Hsieh Y-W, Lin Y-H, Zhu J-D, Wu C-Y, Lin Y-P, Chen C-C. Treatment effects of upper limb action observation therapy and mirror therapy on rehabilitation outcomes after subacute stroke: a pilot study. Behavioural Neurology 2020;2020:1-9. [DOI: 10.1155/2020/6250524] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jin‐Woo 2011 {published data only}
- Jin-Woo J, Soon BY, Lee MK. The effect of action observation training on upper extremity function in chronic stroke patients. Journal of Korean Society of Occupational Therapy 2011;19:15–24. [Google Scholar]
Kim 2015 {published data only}
- Kim E, Kim K. Effect of purposeful action observation on upper extremity function in stroke patients. Journal of Physical Therapy Science 2015;27(9):2867-9. [DOI: 10.1589/jpts.27.2867] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim E, Kim K. Effects of purposeful action observation on kinematic patterns of upper extremity in individuals with hemiplegia. Journal of Physical Therapy Science 2015;27(6):1809-11. [DOI: 10.1589/jpts.27.1809] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2016a {published data only}
- Kim C, Bang D. Action observation training enhances upper extremity function in subacute stroke survivor with moderate impairment: a double-blind, randomized controlled pilot trial. Journal of the Korean Society of Physical Medicine 2016;11(1):133-40. [10.13066/kspm.2016.11.1.133] [Google Scholar]
Kuk 2016 {published data only}
- Kuk E, Kim J, Oh D, Hwang H. Effects of action observation therapy on hand dexterity and EEG-based cortical activation patterns in patients with post-stroke hemiparesis. Topics in Stroke Rehabilitation 2016;23(5):318-25. [DOI: 10.1080/10749357.2016.1157972] [DOI] [PubMed] [Google Scholar]
Lee 2013 {published and unpublished data}
- Lee D, Roh H, Park J, Lee S, Han S. Drinking behavior training for stroke patients using action observation and practice of upper limb function. Journal of Physical Therapy Science 2013;25(5):611-4. [DOI: 10.1589/jpts.25.611] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mancuso 2021 {published and unpublished data}
- Mancuso M, Di Tondo S, Costantini E, Damora A, Sale P, Abbruzzese L. Action observation therapy for upper limb recovery in patients with stroke: a randomized controlled pilot study. Brain Sciences 2021;11(3):1-12. [DOI: 10.3390/brainsci11030290] [DOI] [PMC free article] [PubMed] [Google Scholar]
Younghwa 2013 {published data only}
- Younghwa G, Bora K. An impact of action-observation training and task-oriented training on activities of daily living of stroke patients. Journal of Korean Integrative Medicine 2013;1(3):19-28. [Google Scholar]
Zhu 2015 {published and unpublished data}
- Zhu MH, Wang J, Gu XD, Shi MF, Zeng M, Wang CY, et al. Effect of action observation therapy on daily activities and motor recovery in stroke patients. International Journal of Nursing Sciences 2015;2(3):279-82. [DOI: 10.1016/j.ijnss.2015.08.006] [DOI] [Google Scholar]
References to studies excluded from this review
Brunner 2014 {published data only}
- Brunner IC, Skouen JS, Ersland L. Plasticity and response to action observation: a longitudinal FMRI study of potential mirror neurons in patients with subacute stroke. Neurorehabilitation and Neural Repair 2014;28(9):874-84. [DOI: 10.1177/1545968314527350] [DOI] [PubMed] [Google Scholar]
Cha 2015 {published data only}
- Cha Y, Yoo E, Jung M, Park S, Park J, Lee J. Effects of mental practice with action observation training on occupational performance after stroke. Journal of Stroke and Cerebrovascular Diseases 2015;24(6):1405-13. [DOI] [PubMed] [Google Scholar]
Chang 2017 {published data only}
- Chang M, Kim H, Kim K, Oh J, Jang C, Yoon T. Effects of observation of hand movements reflected in a mirror on cortical activation in patients with stroke. Journal of Physical Therapy Science 2017;29(1):38-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Emmerson 2017 {published data only}
- Emmerson K, Harding K, Taylor N. Home exercise programmes supported by video and automated reminders compared with standard paper-based home exercise programmes in patients with stroke: a randomized controlled trial. Clinical Rehabilitation 2017;31(8):1068-77. [DOI] [PubMed] [Google Scholar]
Ertelt 2012 {published data only}
- Ertelt D, Hemmelmann C, Dettmers C, Ziegler A, Binkofsk F. Observation and execution of upper-limb movements as a tool for rehabilitation of motor deficits in paretic stroke patients: protocol of a randomized clinical trial. BMC Neurology 2012;12(1):42. [DOI: 10.1186/1471-2377-12-42] [DOI] [PMC free article] [PubMed] [Google Scholar]
Franceschini 2010a {published data only}
- Franceschini M, Agosti M, Cantagallo A, Sale P, Mancuso M, Buccino G. Mirror neurons: action observation treatment as a tool in stroke rehabilitation. European Journal of Physical and Rehabilitation Medicine 2010;46(4):517-23. [MEDLINE: ] [PubMed] [Google Scholar]
Frenkel‐Toledo 2014 {published data only}
- Frenkel-Toledo S, Bentin S, Perry A, Liebermann D, Soroker N. Mirror-neuron system recruitment by action observation: effects of focal brain damage on mu suppression. NeuroImage 2014;87:127-37. [DOI] [PubMed] [Google Scholar]
Kim 2010 {published data only}
- Kim J, Yang B, Lee M. The effect of action observational physical training on manual dexterity in stroke patients. Physical Therapy Korea 2010;17(2):17-24. [Google Scholar]
Kim 2013a {published data only}
- Kim J, Chung E, Lee B. A study of analysis of the brain wave with respected to action observation and motor imagery: a pilot randomized controlled trial. Physical Therapy Science 2013;25(7):779-82. [DOI: 10.1589/jpts.25.779] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2013b {published data only}
- Kim JH, Lee BH. Action observation training for functional activities after stroke: a pilot randomized controlled trial. NeuroRehabilitation 2013;33(4):565-74. [DOI: 10.3233/NRE-130991] [DOI] [PubMed] [Google Scholar]
Kim 2014 {published data only}
- Kim SS, Kim TH, Lee BH. Effects of action observational training on cerebral hemodynamic changes of stroke survivors: a fTCD study. Journal of Physical Therapy Science 2014;26(3):331-4. [10.1589/jpts.26.331] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2016b {published data only}
- Kim T, Kim S, Lee B. Effects of action observational training plus brain-computer interface-based functional electrical stimulation on paretic arm motor recovery in patient with stroke: a randomized controlled trial. Occupational Therapy International 2016;23(1):39-47. [DOI: 10.1002/oti.1403] [DOI] [PubMed] [Google Scholar]
Ko 2014 {published data only}
- Ko H-E, Park J-J, Lee K-J, Lee E-H, Oh M-H. The effect of action-observational physical training based on mirror neuron system on upper extremity function and activities of daily living in stroke patient. Journal of the Korea Institute of Electronic Communication Sciences 2013;9(1):123-30. [Google Scholar]
Lee 2016 {published data only}
- Lee H, Kim H, Kwon H, Cho Y, Lee S. Effects of the distant action observation training program on function restorations of chronic stroke patients. Journal of Korean Society of Occupational Therapy 2016;24(1):1-13. [DOI: 10.14519/jksot.2016.24.1.01] [DOI] [Google Scholar]
Liepert 2014 {published data only}
- Liepert J, Greiner J, Dettmers C. Motor excitability changes during action observation in stroke patients. Journal of Rehabilitation Medicine 2014;46(5):400-5. [DOI: 10.2340/16501977-1276] [DOI] [PubMed] [Google Scholar]
Lima 2020 {published data only}
- Lima AC, Christofoletti G. Exercises with action observation contribute to upper limb recovery in chronic stroke patients: a controlled clinical trial. Motriz 2020;26(1):e10200148. [Google Scholar]
Lubart 2017 {published data only}
Marangon 2014 {published data only}
- Marangon M, Priftis K, Fedeli M, Masiero S, Tonin P, Piccione F. Lateralization of motor cortex excitability in stroke patients during action observation: a TMS study. BioMed Research International 2014;2014. [DOI] [PMC free article] [PubMed]
Sale 2012 {published data only}
- Sale P, Franceschini M. Action observation and mirror neuron network: a tool for motor stroke rehabilitation. European Journal of Physical and Rehabilitation Medicine 2012;48(2):313-8. [PMID: ] [PubMed] [Google Scholar]
Shih 2017 {published data only}
- Shih TY, Wu CY, Lin KC, Cheng CH, Hsieh YW, Chen CL, et al. Effects of action observation therapy and mirror therapy after stroke on rehabilitation outcomes and neural mechanisms by MEG: study protocol for a randomized controlled trial. Trials 2017;18((1 CC-Stroke)):459. [DOI: 10.1186/s13063-017-2205-z] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sugg 2015 {published data only}
- Sugg K, Muller S, Winstein C, Hathorn D, Dempsey A. Does action observation training with immediate physical practice improve hemiparetic upper-limb function in chronic stroke? Neurorehabilitation and Neural Repair 2015;29(9):807-17. [DOI: 10.1177/1545968314565512] [DOI] [PubMed] [Google Scholar]
Sun 2016 {published data only}
- Sun Y, Wei W, Luo Z, Gan H, Hu X. Improving motor imagery practice with synchronous action observation in stroke patients. Topics in Stroke Rehabilitation 2016;23(4):245-53. [DOI] [PubMed] [Google Scholar]
Szameitat 2012 {published data only}
- Szameitat A, Shen S, Conforto A, Sterr A. Cortical activation during executed, imagined, observed, and passive wrist movements in healthy volunteers and stroke patients. NeuroImage 2012;62(1):266-80. [DOI] [PubMed] [Google Scholar]
Wright 2014 {published data only}
- Wright D, Williams J, Holmes P. Combined action observation and imagery facilitates corticospinal excitability. Frontiers in Human Neuroscience 2014;8:951. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yun 2011 {published data only}
- Yun TW, Lee MK. The change of mu rhythm during action observation in people with stroke. Journal of the Korean Society of Physical Medicine 2011;6(3):361-8. [Google Scholar]
References to ongoing studies
NCT02235350 {published data only}
- NCT02235350. Study on the effectiveness of action observation treatment (AOT) as a rehabilitation tool in acute stroke patients and in chronic stroke patients with apraxia: a randomized controlled trial. clinicaltrials.gov/ct2/show/study/NCT02235350 (first received 9 September 2014). [NCT02235350]
NCT04015271 {published data only}
- NCT04015271. Feasibility of action observation and repetitive task practice on upper extremity outcomes in chronic stroke survivors. clinicaltrials.gov/show/NCT04015271 (first received 10 July 2019).
NCT04047134 {published data only}
- NCT04047134. Neuroimaging biomarkers toward a personalized upper limb action observation treatment in chronic stroke patients. clinicaltrials.gov/show/NCT04047134 (first received 6 August 2019).
NCT04574687 {published data only}
- NCT04574687. Effects of action observation therapy on fine motor skills of upper limb functions in chronic stroke patients. clinicaltrials.gov/show/NCT04574687 (first received 5 October 2020).
NCT04943601 {published data only}
- NCT04943601. Action observation therapy for stroke [Effect of action observation exercises with complex tasks on upper limb function in acute stroke]. clinicaltrials.gov/show/NCT04943601 (first received 29 June 2021). [REC/00816]
Additional references
Bassolino 2015
- Bassolino M, Sandini G, Pozzo T. Activating the motor system through action observation: is this an efficient approach in adults and children? Developmental Medicine & Child Neurology 2015;57(Suppl 2):42-5. [DOI: 10.1111/dmcn.12686] [DOI] [PubMed] [Google Scholar]
Bazzini 2022
- Bazzini MC, Nuara A, Scalona E, De Marco D, Rizzolatti G, Avanzini P, et al. The proactive synergy between action observation and execution in the acquisition of new motor skills. Frontiers in Human Neuroscience 2022;16 :793849 . [DOI: 10.3389/fnhum.2022.793849] [DOI] [PMC free article] [PubMed] [Google Scholar]
Buccino 2014
- Buccino G. Action observation treatment: a novel tool in neurorehabilitation. Philosophical Transactions of the Royal Society B: Biological Sciences 2014;369(1644):20130185. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2009
- Chen HM, Chen CC, Hsueh IP, Huang SL, Hsieh CL. Test-retest reproducibility and smallest real difference of 5 hand function tests in patients with stroke. Neurorehabilitation and Neural Repair 2009;23(5):435-40. [DOI] [PubMed] [Google Scholar]
Cowles 2012
- Cowles T, Clark A, Mares K, Peryer G, Stuck R, Pomeroy V. Observation-to-imitate plus practice could add little to physical therapy benefits within 31 days of stroke: translational randomized controlled trial. Neurorehabilitation and Neural Repair 2012;27(2):173-82. [DOI] [PubMed] [Google Scholar]
Feigin 2014
- Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 2014;383(9913):245-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fitts 1967
- Fitts PM, Posner MI. Human Performance. Belmont: Brooks/Colemann, 1967. [Google Scholar]
Garrison 2010
- Garrison KA, Winstein CJ, Aziz-zadeh L. The mirror neuron system: a neural substrate for methods in stroke rehabilitation. Neurorehabilitation and Neural Repair 2010;24(5):404-12. [DOI] [PubMed] [Google Scholar]
Garrison 2013
- Garrison KA, Aziz-zadeh L, Wong SW, Liew SL, Winstein CJ. Modulating the motor system by action observation after stroke. Stroke 2013;44(8):2247-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
GBD 2017
- GBD 2015 Neurological Disorders Collaborator Group. Global, regional, and national burden of neurological disorders during 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurology 2017;16:877–97. [DOI: 10.1016/ S1474-4422(17)30299-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ge 2018
- Ge S, Liu H, Lin P, Gao J, Xiao C, Li Z. Neural basis of action observation and understanding from first- and third-person perspectives: an fMRI study. Frontiers in Behavioral Neurosciences 2018;12:283. [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Hamilton (ON): McMaster University (developed by Evidence Prime), (accessed prior to 15 June 2022). Available at gradepro.org.
Gregor 2021
- Gregor S, Saumur TM, Crosby LD, Powers J, Patterson KK. Study paradigms and principles investigated in motor learning research after stroke: a scoping review. Archives of Rehabilitation Research and Clinical Translation 2021;3(2):100-11. [DOI: 10.1016/j.arrct.2021.100111] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hardwick 2018
- Hardwick RM, Caspers S, Eickhoff SB, Swinnen SP. Neural correlates of action: comparing meta-analyses of imagery, observation, and execution. Neuroscience & Biobehavioral Reviews 2018;94:31-44. [DOI: 10.1016/j.neubiorev.2018.08.003] [DOI] [PubMed] [Google Scholar]
Harvey 2009
- Harvey RL. Improving poststroke recovery: neuroplasticity and task-oriented training. Current Treatment Options in Cardiovascular Medicine 2009;11(3):251-9. [DOI] [PubMed] [Google Scholar]
Higgins 2017
- Higgins JP, Altman DG, Sterne JA, (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Churchill R, Chandler J, Cumpston MS editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.2.0 (updated June 2017). Cochrane, 2017. Available from www.training.cochrane.org/handbook/archive/v5.2.
Higgins 2022
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
Huntley 2018
- Huntley MK, Muller S, Vallence AM. Corticospinal excitability is modulated by distinct movement patterns during action observation. Experimental Brain Research 2018;236 (4):1067-75 . [DOI: 10.1007/s00221-018-5199-1] [DOI] [PubMed] [Google Scholar]
Johansson 2011
- Johansson BB. Current trends in stroke rehabilitation. A review with focus on brain plasticity. Acta Neurologica Scandinavica 2011;123(3):147-59. [DOI] [PubMed] [Google Scholar]
Katan 2018
- Katan M, Luft A. Global burden of stroke. Seminars in Neurology 2018;38(02):208-11. [DOI: 10.1055/s-0038-1649503] [DOI] [PubMed] [Google Scholar]
Kemmerer 2021
- Kemmerer D. What modulates the Mirror Neuron System during action observation? Multiple factors involving the action, the actor, the observer, the relationship between actor and observer, and the context. Progress in Neurobiology 2021;205:102-28. [DOI: 10.1016/j.pneurobio.2021.102128] [DOI] [PubMed] [Google Scholar]
Kim 2018
- Kim D-H, An D-H, Yoo W-G. Effects of live and video form action observation training on upper limb function in children with hemiparetic cerebral palsy. Technology and Health Care 2018 ;26 (3):437-43. [DOI: 10.3233/THC-181220] [DOI] [PubMed] [Google Scholar]
Krakauer 2019
- Krakauer JW, Hadjiosif AM, Xu J, Wong AL, Haith AM. Motor learning. Comprehensive Physiology 2019;14(9):613-63 . [DOI: 10.1002/cphy.c170043] [DOI] [PubMed] [Google Scholar]
Langhorne 2011
- Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet 2011;377(9778):1693-702. [DOI: 10.1016/S0140-6736(11)60325-5] [DOI] [PubMed] [Google Scholar]
Lieshout 2020
- Lieshout EC, de Port IG, Dijkhuizen RM, Visser-Meily JM. Does upper limb strength play a prominent role in health-related quality of life in stroke patients discharged from inpatient rehabilitation? Topics in Stroke Rehabilitation 2020;27(7):525-33. [DOI: 10.1080/10749357.2020.1738662] [DOI] [PubMed] [Google Scholar]
Lundquist 2021
- Lundquist CB, Nielsen JF, Brunner IC. Predicting hand motor recovery in severe stroke: the role of motor evoked potentials in relation to early clinical assessment. Journal of Stroke and Cerebrovascular Diseases 2021;30(11):106025. [DOI: 10.1016/j.jstrokecerebrovasdis.2021.106025] [DOI] [PubMed] [Google Scholar]
Magill 1989
- Magill RA. Motor Learning: Concepts and Applications. 3rd edition. Dubuque: Wm C Brown, 1989. [Google Scholar]
Millar 2021
- Millar JD, Van Wijck F, Pollock A, Ali M. International consensus recommendations for outcome measurement in post-stroke arm rehabilitation trials. European Journal of Physical and Rehabilitation Medicine 2021;57(1):61-8. [DOI] [PubMed] [Google Scholar]
Page 2021
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLOS Medicine 2021;18(3):e1003583. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peng 2019
- Peng T, Zhu J, Chen C, Tai R, Lee C, Hsieh Y. Action observation therapy for improving arm function, walking ability, and daily activity performance after stroke: a systematic review and meta-analysis. Clinical Rehabilitation 2019;33(8):1277-85. [DOI: 10.1177/0269215519839108] [DOI] [PubMed] [Google Scholar]
Pollock 2014
- Pollock A, Farmer SE, Brady MC, Langhorne P, Mead GE, Mehrholz J, et al. Interventions for improving upper limb function after stroke. Cochrane Database of Systematic Reviews 2014, Issue 11. Art. No: CD010820. [DOI: 10.1002/14651858.CD010820.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rand 2015
- Rand D, Eng JJ. Predicting daily use of the affected upper extremity 1 year after stroke. Journal of Stroke and Cerebrovascular Diseases 2015;24(2):274-83. [DOI: 10.1016/j.jstrokecerebrovasdis.2014.07.039] [DOI] [PubMed] [Google Scholar]
Review Manager 2020 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.4. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2020.
Ryan 2016
- Ryan R, Synnot A, Prictor M, Hill S. Cochrane Consumers and Communication Group Data Extraction Template for Included Studies. cccrg.cochrane.org/author-resources. [DOI: 10.26181/5b57cfd711743] [DOI]
Ryan 2021
- Ryan D, Fullen B, Rio E, Segurado R, Stokes D, O’Sullivan C. Effect of action observation therapy in the rehabilitation of neurologic and musculoskeletal conditions: a systematic review. Archives of Rehabilitation Research and Clinical Translation 2021;3:1-33. [DOI: 10.1016/j.arrct.2021.100106] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sarasso 2015
- Sarasso E, Gemma M, Agosta F, Filippi M, Gatti R. Action observation training to improve motor function recovery: a systematic review. Archives of Physiotherapy 2015;5(1):14. [DOI: 10.1186/s40945-015-0013-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Medicine 2010;8:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Small 2012
- Small SL, Buccino G, Solodkin A. The mirror neuron system and treatment of stroke. Developmental Psychobiology 2012;54(3):293-310. [DOI] [PubMed] [Google Scholar]
Tani 2018
- Tani M, Ono Y, Matsubara M, Ohmatsu S, Yukawa Y, Kohno M, Tominaga T. Action observation facilitates motor cortical activity in patients with stroke and hemiplegia. Neurosci Res 2018;133:7-14. [DOI] [PubMed] [Google Scholar]
Timmermans 2010
- Timmermans AA, Spooren AI, Kingma H, Seelen HA. Influence of task-oriented training content on skilled arm-hand performance in stroke: a systematic review. Neurorehabilitation and Neural Repair 2010;24(9):858-70. [DOI] [PubMed] [Google Scholar]
Zhang 2019
- Zhang B, Kan L, Dong A, Zhang J, Bai Z, Xie Y, et al. The effects of action observation training on improving upper limb motor functions in people with stroke: A systematic review and meta-analysis. PLOS ONE 2019;14(8):1-13. [DOI: 10.1371/journal.pone.0221166] [e0221166] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhu 2019
- Zhu JD, Cheng CH, Tseng YJ, Chou CC, Chen CC, Hsieh YW, et al. Modulation of motor cortical activities by action observation and execution in patients with stroke: an MEG study. Neural Plasticity 2019;30:8481371 . [DOI: 10.1155/2019/8481371] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Borges 2015
- Borges LR, Melo LP, Fernandes AB, Guerra RO, Campos TF. Action observation for upper limb rehabilitation after stroke. Cochrane Database of Systematic Reviews 2015, Issue 9. Art. No: CD011887. [DOI: 10.1002/14651858.CD011887] [DOI] [PMC free article] [PubMed] [Google Scholar]
Borges 2018
- Borges LR, Fernandes AB, Melo LP, Guerra RO, Campos TF. Action observation for upper limb rehabilitation after stroke. Cochrane Database of Systematic Reviews 2018, Issue 10. Art. No: CD011887. [DOI: 10.1002/14651858.CD011887.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


