Abstract
Purpose:
To review the principles, advantages, and disadvantages of asynchronous and synchronous delivery models of home-based cardiac rehabilitation (HBCR).
Methods:
We reviewed recently published systematic reviews and other publications of randomized studies of asynchronous and synchronous HBCR to assess principles, outcomes, and limitations of those delivery methods compared with center-based cardiac rehabilitation (CBCR).
Summary:
While most studies prior to 2016 involved asynchronous HBCR approaches to care, studies since 2016 have included asynchronous or synchronous delivery models. Both delivery models have been shown to help provide core components of cardiac rehabilitation (CR). Studies using either method have been shown to have similar short-term patient outcomes as CBCR, at least in low- to moderate-risk patients who have been studied. Asynchronous HBCR offers greater flexibility for patients and CR staff, while synchronous HBCR provides greater real-time oversight and feedback to patients.
Asynchronous and synchronous HBCR is an option to consider for patients eligible for CR. Additional research is needed for both delivery models, applied separately or in combination, to compare their impact on shorter- and longer-term patient outcomes and to assess their impact in patient subgroups (referral diagnosis, women, elderly, underrepresented racial and ethnic minority groups, patients at a higher cardiovascular disease risk, patients with multiple comorbid conditions, etc).
Keywords: asynchronous, cardiac rehabilitation, home-based, models, synchronous
Home-based cardiac rehabilitation (HBCR) has gained significant interest in recent years as a potential option to expand the reach of cardiac rehabilitation (CR).1 Studies suggest similar short-term benefits from HBCR as compared with center-based cardiac rehabilitation (CBCR) at least in the patient groups included in those studies. The hope of HBCR is that it will help reduce current gaps in CR participation, improve the cost-effectiveness of CR, expand the reach of CR, and increase the longer-term benefits of CR for patients.1,2
Especially during the worldwide SARS-CoV-2 pandemic, there has been a growing need to implement HBCR options for patients.3 One important consideration in implementing HBCR is the communication strategy to be used to connect CR staff and patients. Studies of HBCR have generally used two communication approaches, one that links staff and patients at flexible times other than when the patient is carrying out an exercise training session (asynchronous communication) and another that links staff and patients in real time when the patient is exercising (synchronous communication).2,4,5 The purpose of this article is to review the principles, evidence, advantages, and disadvantages of both models and to discuss future research directions of these delivery approaches for HBCR.
DEFINITIONS OF ASYNCHRONOUS AND SYNCHRONOUS HBCR
The use of the terms “asynchronous” and “synchronous” for purposes of HBCR is unique and differs from the common use of these terms with general communication strategies.6 In common usage, “asynchronous” usually refers to communication strategies in which there is a delay or lag between the time a message is sent and when it is received and acted upon. In contrast, “synchronous” communication strategies, in the general sense, usually involve live communication strategies that allow people to communicate and exchange information with each other in real time.
In HBCR delivery models, asynchronous communication refers to a system in which the patient and CR staff members communicate at times other than when the patient is carrying out exercise training (Figure).2 Communications in asynchronous HBCR originate from either the CR staff or the patient and occur at scheduled or unscheduled times as needed. On the contrary, synchronous HBCR utilizes communication strategies between the patient and CR staff that occur in real time when the patient is actively carrying out an exercise training session. Communications in synchronous HBCR typically originate from the CR staff at scheduled times.
Figure.
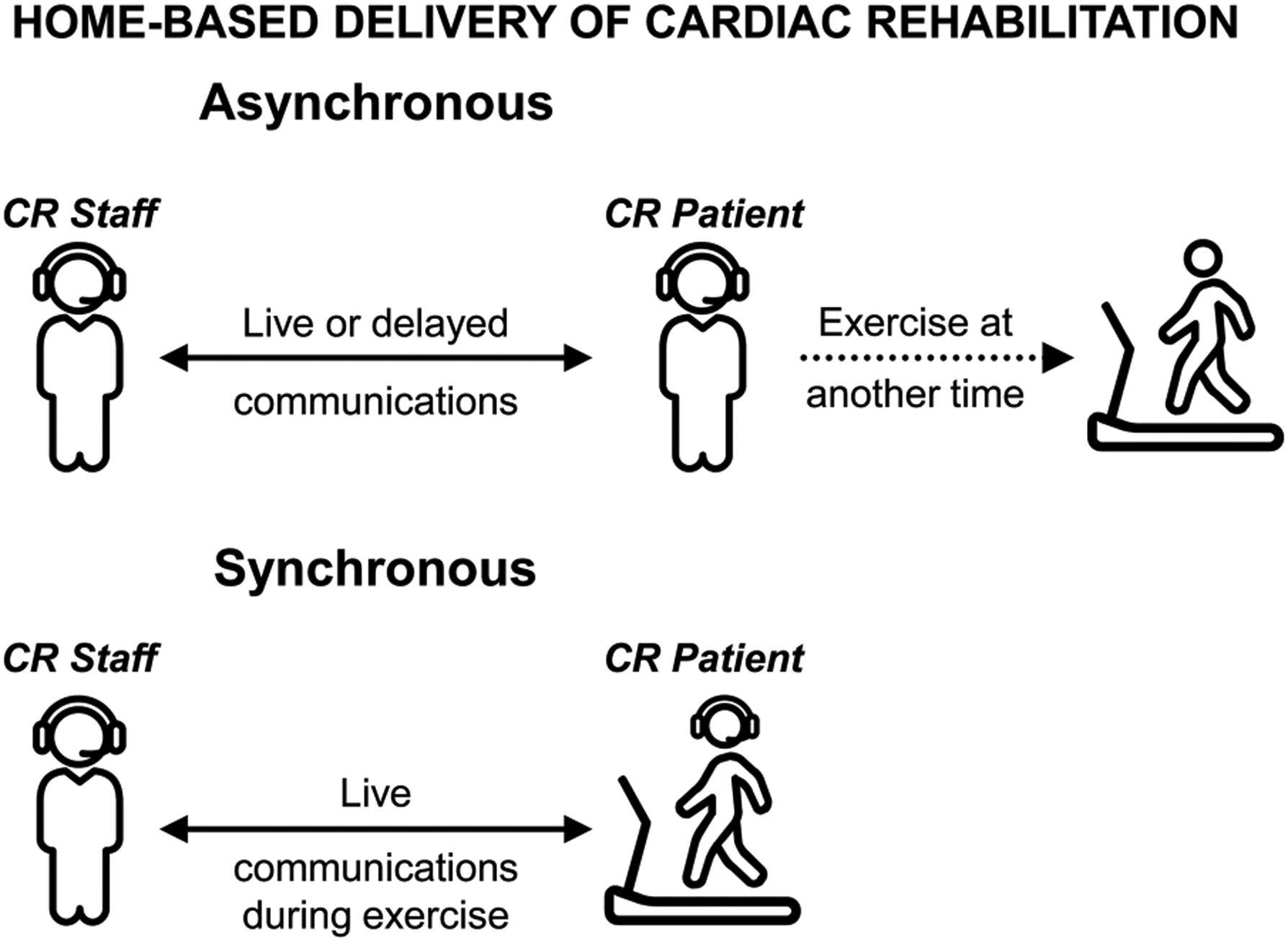
Asynchronous and synchronous models of communication for home-based cardiac rehabilitation. Abbreviation: CR, cardiac rehabilitation.
Both communication approaches—asynchronous and synchronous—can be carried out using a variety of messaging techniques, such as telephone calls, text messaging, videoconferencing, or even in-person home visits. However, asynchronous HBCR studies have generally used telephone calls as the primary communication tool7,8 while synchronous HBCR studies have typically used live video calls as the primary communication tool.9,10 Likewise, both approaches can include a variety of additional tools including internet-based, streaming, or virtual reality patient education tools11 and remote physiologic monitoring such as electrocardiography, blood pressure, and weight monitoring.
Components of clinical CR care that are delivered to patients are similar in asynchronous and synchronous HBCR delivery models. These components include patient communications, patient evaluations, goal setting, counseling, education, treatment, data collection/management, and follow-up.12 In other words, the components of CR care are common between the two delivery models (and between HBCR and CBCR), but the key difference between asynchronous and synchronous HBCR strategies is whether or not the patient and CR staff members are connected in real time during their HBCR exercise training sessions. Of note, most HBCR models—both asynchronous and synchronous—include in-person assessment visits at program entry and graduation, and some include a small number of CBCR sessions at the outset to prepare patients for implementation of HBCR.
REVIEW OF RELEVANT LITERATURE
While CBCR is typically discussed as being separate from HBCR, most CBCR programs include an informal component of asynchronous HBCR. During conventional CBCR, patients are usually encouraged to carry out their own CR therapies (exercise training, nutritional therapy, medication adherence strategies, stress management, etc) at home in an unsupervised, asynchronous manner and then to return to the CR center, reporting regularly on their home-based activities. Starting in the 1990s, research studies on HBCR strategies began to sprout roots.7,13 Communication strategies for HBCR were studied, using the communication techniques that were available at the time, primarily telephone communications between the patient and CR staff. With advances over the past 30 yr in communication strategies and health-related remote monitoring technologies, additional asynchronous and synchronous communication strategies have been developed and tested to determine their efficacy in carrying out HBCR care.
HOW DO CLINICAL OUTCOMES IN ASYNCHRONOUS HBCR COMPARE WITH CBCR?
Randomized controlled studies of HBCR have commonly used asynchronous communication strategies, dating back to the 1990s.7,8 These studies have generally shown that asynchronous models of HBCR have high levels of patient utilization and satisfaction and that they have similar short-term improvements in intermediate outcomes as with CBCR (eg, in functional capacity, quality of life, cardiovascular disease risk factor control).14 Studies have primarily included patients with low-to-moderate cardiovascular disease risk, but some have included higher-risk patients with heart failure with reduced ejection fraction (HFrEF).15 Studies are lacking in patients with multiple comorbid conditions, those aged ≥75 yr, women, and individuals from underserved racial and ethnic groups. Based largely on the results of randomized studies of asynchronous HBCR, the 2019 American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR)/American College of Cardiology (ACC)/American Heart Association (AHA) Scientific Statement on HBCR suggested that HBCR could be considered a reasonable alternative to CBCR in low- to moderate-risk individuals who are not able to participate in CBCR.2
EXAMPLES OF ASYNCHRONOUS HBCR RANDOMIZED CONTROLLED STUDIES
A large percentage of early studies of HBCR have involved the use of asynchronous delivery of HBCR. For example, in the 22 randomized controlled trials of HBCR versus CBCR/usual care that were published between 1984–2016 and that were included in the 2019 AACVPR/ACC/AHA Scientific Statement on HBCR,2 20 of the 22 studies involved asynchronous strategies, seven included synchronous strategies, and six included both synchronous and asynchronous strategies. A growing number of randomized trials of HBCR have been published in recent years, with ≥ 9 published just since January 2020.9,16–23 More recent studies of HBCR have included studies of asynchronous HBCR,20,21,23 as well as a growing number of synchronous HBCR.9,24
The following section contains brief descriptions of a representative sample of randomized studies of asynchronous HBCR.
One of the first published studies of asynchronous HBCR was the MULTIFIT study, published by DeBusk et al7 in 1994. In that study, patients recovering from myocardial infarction were randomized to either usual care or HBCR under the guidance of a nurse case manager who utilized telephone-based interactions with patients at regular intervals that were asynchronous with their home-based exercise sessions. At follow-up, smoking cessation rates, functional capacity improvements, and low-density lipoprotein cholesterol control were all superior in the HBCR intervention group compared with the usual care group.
A more recent study from Varnfield et al8 tested a smartphone-based application that linked patients with CR staff for guiding, assessing, and adjusting treatment goals and related activities in an asynchronous manner. Compared with patients randomized to a CBCR program, patients randomized to the intervention group had similar improvements in functional capacity, healthy dietary habits, lipid control, and psychological health both at 6 wk and at 6 mo. Adherence to CR sessions was superior in the HBCR group, with 80% of participants completing CR in the HBCR group while only 47% of participants completed CR in the CBCR arm. However, while the use of remote technological tools in HBCR may be viewed as an efficient and effective way to help promote patient engagement and participation, it is admittedly difficult to compare adherence between CBCR and HBCR since patients in CBCR must come in person to a central location to be considered adherent while patients in HBCR may be considered adherent if they simply connect via telephone with CR staff. Nonetheless, the study by Varnfield et al8 was a critical advance in the field as it helped validate and update the findings from the MULTIFIT study using up-to-date communication technologies.
Another recent study, involving a straightforward approach to asynchronous HBCR, has been implemented in the Department of Veterans Affairs health care system. A nonrandomized, prospective, observational study compared HBCR outcomes with those of CBCR in patients following myocardial infarction, percutaneous coronary intervention, and/or coronary artery bypass graft surgery.20 Participants in the HBCR arm met in person with CR staff members at the time of program initiation, to undergo assessments, derive an individualized treatment plan, and receive guidance on how to participate in the HBCR program. Participants were provided a physical activity tracker, exercise bands, and a stepper to help promote engagement in their exercise program. In addition, participants were asked to keep track of physical activity in a logbook to encourage self-management and monitoring skills. Participants were contacted by telephone each week for the first 6 wk, followed by three biweekly telephone calls, during which their progress was assessed and treatment plans adjusted to stimulate progressive advances in their exercise training. Participants in the HBCR arm were found to improve functional capacity and quality-of-life measures as much as or better than those in the CBCR arm. However, several limitations were noted in the study, including a greater loss to follow-up in the HBCR arm, which may have affected the results of the study in favor of the HBCR arm. In addition, a recent report from a registry of 923 veterans participating in HBCR at 25 Veterans Affairs hospitals nationally demonstrated significant improvements in functional capacity and health status measures.25 Notably, the registry, which included many patients with high clinical complexity and risk, reported no safety issues related to HBCR participation.
Asynchronous HBCR has been studied in a lower-income country using a simplified asynchronous delivery approach.23 The intervention started with an in-hospital CR class for participating patients, after which they received a locally developed educational booklet that helped them implement CR at home. The participants received a monthly telephone call for 12 mo that allowed CR staff to evaluate, educate, and encourage patient progress. The intervention improved cardiovascular disease risk factor control, quality of life, and exercise capacity more in the participants randomized to the intervention group than in the group of participants randomized to usual care. This study demonstrated that a relatively low-cost, simplified but longer-term HBCR program can help patients with cardiovascular disease make significant longer-term improvements in their cardiovascular health.
Another study of asynchronous HBCR recently assessed its impact in a group of individuals who had previously refused participation in traditional CBCR, a common finding in most countries of the world.21 Of 966 patients identified who had refused traditional CBCR, 179 (19%) met entry criteria and agreed to be included in the study. The intervention was a 6-mo program in which participants received educational training about HBCR, a treatment plan, a smartphone, and a heart rate monitor. Motivational telephone calls were made by CR staff to the participants once per week for the first month, then once every other week in the second month, and then once a month from the third month to the end of the sixth month. Patients in the intervention group demonstrated significantly greater exercise capacity at follow-up than the control group, with no difference in the incidence of adverse events between groups. This study suggests that asynchronous HBCR may help expand the reach of CR and provide care to those who would normally not participate in CBCR.
Finally, while most asynchronous HBCR studies have included low- to moderate-risk patients, the REACH-HF trial was a recently published randomized trial of asynchronous HBCR in patients with HFrEF.15,26–28 The 12-wk intervention was codeveloped by patients, caregivers, and clinicians and included exercise training, self-management tools, social support opportunities, and facilitation by nurses or physiotherapists. Outcomes were assessed out to 12 mo after the initiation of the intervention. Approximately 90% of participants in the intervention group completed the study. Heart failure–specific quality of life improved significantly in the intervention group compared with those participants randomized to the usual care group. No significant differences were noted in functional capacity, possibly due to a relatively low level of engagement in exercise training by participants in the intervention group. The cost per participant of delivering the intervention was calculated to be approximately £400 (~US $550) and the cost per quality of life year gained was £1720 (~US $2400). This study not only highlights the well-known challenge of engaging patients with HFrEF in exercise training but also suggests that asynchronous HBCR may help increase overall program participation in this patient group in a cost-effective manner.
HOW DO CLINICAL OUTCOMES IN SYNCHRONOUS HBCR COMPARE WITH CBCR?
As has been pointed out for studies of asynchronous HBCR, studies of synchronous HBCR have reported similar shorter-term clinical outcomes compared with the outcomes in patients cared for in CBCR. Studies have largely included low- to moderate-risk patients,24 although some studies of synchronous HBCR have been conducted in higher-risk patients with stable HFrEF.11 However, studies of synchronous HBCR have not been conducted in significant numbers of individuals with multiple comorbid conditions, in those who are ≥75 yr, in women, or in individuals from underserved racial and ethnic minority groups.
The following section contains brief descriptions of synchronous HBCR randomized controlled studies.
As mentioned earlier, a relatively small number of early studies of HBCR used synchronous delivery models. A small number of studies in the 1990s examined the role of simultaneous voice and electrocardiographic (ECG) trans-telephonic transmission for home-based exercise training in CR patients.13,29,30 These early studies supported the feasibility and probable safety of such an approach. In more recent years, advances in monitoring and communication technology have led to an increase in the number of randomized studies of HBCR that have tested the utility of synchronous communications methods.9,24
An example of synchronous HBCR is the study by Maddison et al,24 which assessed the impact of a 12-wk telerehabilitation synchronous HBCR model on patient outcomes, compared with a traditional CBCR model of care in patients with coronary artery disease. The impact on functional capacity was similar in both groups. Waist circumference decreased more in the CBCR group, while the HBCR group was less sedentary than the CBCR group. Nonhospital costs were nearly 50% lower in the HBCR group than in the CBCR group. This study suggests that a telerehabilitation HBCR program is as effective as a CBCR program in most short-term outcomes and that it can be delivered at a significantly lower cost than CBCR.
Another recent randomized study of synchronous HBCR versus CBCR was conducted in patients with stable HFrEF.10 Intervention patients were provided a laptop computer, a mobile broadband device connected to a wireless broadband internet, an automatic sphygmomanometer, a finger pulse oximeter, and strength training equipment (resistance bands and free weights). The telerehabilitation sessions were held in real time twice weekly for 12 wk and were delivered by a physiotherapist who interacted directly with up to four patients/session. At 6 mo of follow-up, quality of life was similar in the HBCR and CBCR groups, but total health care costs were approximately 40% lower in the HBCR group than in the CBCR group, suggesting that HBCR may offer an equally effective therapy to patients at a lower cost than in CBCR.
Finally, the TELEREH-HF trial, a randomized trial of synchronous telerehabilitation in HFrEF patients, utilized ECG monitoring and remote monitoring with cardiac implantable electronic devices over a 9-wk intervention period.9 Adherence was excellent in the patients included in the HBCR group, with nearly 90% of participants considered adherent to the intervention at 9 wk. No deaths or other serious adverse events occurred during the HBCR sessions or directly afterward (within 1 hr of the session). While there were significant improvements at 9 wk in functional capacity and quality of life, there was no difference in longer-term outcomes observed after 24 mo, including days alive and out of hospital, all-cause hospitalizations, and all-cause mortality rates when compared with usual care. This suggests that in patients with HFrEF, a short-term telerehabilitation intervention provides shorter-term intermediate benefits and is safe, but that it may not translate into longer-term clinical improvements. Longer-term interventions may be needed to produce longer-term clinical benefits, particularly in patients with HFrEF.
HOW DO CLINICAL OUTCOMES COMPARE IN ASYNCHRONOUS VERSUS SYNCHRONOUS HBCR?
To our knowledge, no head-to-head comparison studies between asynchronous and synchronous HBCR have been published. However, it is worth noting that some studies use a combination of asynchronous and synchronous communication strategies.9
DISCUSSION
As noted in the 2019 AACVPR/ACC/AHA Scientific Statement on HBCR,2 and supported by additional research since that time, evidence for and interest in HBCR are growing. Several factors are likely contributing to the growing interest in HBCR. First, the important benefits of CR services are recognized perhaps now more than ever, as reflected in the high level of recommendation for CR in national cardiovascular clinical guidelines and quality performance measures.31,32 Second, new strategies are being sought to help bridge the gap in delivery of CR around the world, since only a small percentage of eligible patients are currently receiving CR.33–36 Third, advances in technology and communication tools are helping accelerate the options on how to provide HBCR and may help increase the reach and cost-effectiveness of CR.5,8,37 Finally, the limitations that have been thrust upon CR programs during the SARS-CoV-2 pandemic have produced a sense of urgency worldwide for the need to more fully develop and implement effective HBCR strategies.3
Results of randomized studies of asynchronous and synchronous HBCR suggest that it is safe and reasonable to consider these models of HBCR in individuals who qualify for CR but are not able to or choose not to participate in conventional CBCR. While many of the asynchronous HBCR studies have been conducted in low- to moderate-risk individuals, some have been conducted in higher-risk groups. In contrast, the predominance of studies on the use of synchronous HBCR has been collected in moderate- to high-risk patients with stable HFrEF, while some have been conducted in lower-risk groups. Should asynchronous HBCR be used primarily in lower-risk patients and synchronous HBCR in higher-risk individuals? Should all HBCR patients start with synchronous methods and then transition to asynchronous methods after 2–4 wk? And what are the optimal dose, frequency, and content of HBCR intervention sessions, for both asynchronous and synchronous approaches? Additional studies are clearly needed to help clarify these and other questions about the relative and possibly complementary roles of asynchronous and synchronous HBCR in various patient subgroups.
ADVANTAGES AND DISADVANTAGES OF ASYNCHRONOUS AND SYNCHRONOUS HBCR
Potential advantages and disadvantages of asynchronous HBCR are noted in the Table. Convenience and flexibility for patients and CR staff are important advantages of asynchronous HBCR. Patients have more flexibility to exercise from day to day during times that are most convenient to them and then connect with the CR staff for reporting and assessment purposes at another time that is convenient for both parties. In addition, both live and/or delayed communications can be used for asynchronous HBCR, utilizing a variety of methods, including chats/text messaging, secure e-mail messaging, video calls, or telephone calls. This flexibility may help explain why adherence has been reported to be higher in asynchronous HBCR than in CBCR.8
Table.
Potential Advantages and Disadvantages of Asynchronous and Synchronous Home-Based Cardiac Rehabilitation
| Advantages | Disadvantages | |
|---|---|---|
| Asynchronous HBCR |
|
|
| Synchronous HBCR |
|
|
Abbreviations: CR, cardiac rehabilitation; HBCR, home-based cardiac rehabilitation.
One disadvantage to asynchronous HBCR is the lack of direct, real-time supervision of patients by CR staff during exercise sessions. This absence of direct supervision raises concerns regarding the lack of guidance that many patients need to initiate and advance their exercise training, as well as concerns about the safety and medicolegal liabilities of unsupervised exercise training outside of the CR center. However, to date, HBCR studies have reported that HBCR and CBCR have similar effects on improvements in exercise capacity, and similar safety profiles, at least in the patients who have been included in studies of HBCR. Moreover, integration of objective monitoring technologies (eg, heart rate straps or smartwatches with heart rate/ECG measurement) may allow for visualization of adherence to exercise training and identification of important dysrhythmias. In addition, there are concerns that social support and psychological health parameters may be inferior with asynchronous HBCR compared with CBCR. However, there is evidence that psychological health parameters for patients in HBCR improve to a similar level as for those in CBCR.8,18
Advantages and disadvantages of synchronous HBCR are also listed in the Table. A primary advantage of synchronous HBCR is that CR staff members can visually connect in real time with patients while they are carrying out their HBCR sessions, at least theoretically helping optimize safety and personalization of exercise training for patients. While not yet shown in head-to-head comparison studies, this advantage of synchronous HBCR may then lead to greater improvements in functional capacity and patient outcomes associated with those improvements. In addition, some synchronous HBCR programs provide virtual group exercise sessions, involving more than one patient at a time. While this may lead to logistical challenges for CR staff, it does offer the possibility of increased efficiency compared with asynchronous communications, which are generally one-on-one interactions between CR staff and patients.
A significant disadvantage of synchronous HBCR is the reduced flexibility that patients may experience due to the fact that exercise training sessions must be carried out at times that coincide with the availability of the CR staff members to connect with them virtually to supervise their activities. Another potential disadvantage of synchronous HBCR is the need for advanced video connection and technological literacy, which may be problematic for some patients in CR, particularly those individuals who lack resources, training, or experience to be able to comfortably participate.
OTHER ISSUES
While this article has focused on the scientific evidence, advantages, and disadvantages for asynchronous and synchronous approaches to HBCR, it is readily apparent that other issues are also critically important as CR programs ascertain if, how, and when they might implement HBCR services, including issues of medicolegal requirements and concerns, staffing, home/community provision of exercise equipment for participating patients, and sustainable reimbursement strategies. While coverage by the Centers for Medicare and Medicaid Services of asynchronous and synchronous HBCR beyond the time of the current public health emergency is uncertain, coverage has been in place in some health care systems, including asynchronous HBCR that is offered through Kaiser Permanente Southern California38 and the US Department of Veterans Affairs.39 In addition, coverage of synchronous HBCR is provided through Blue Cross-Blue Shield Michigan.40 As evidence continues to accumulate on the safety, efficacy, and efficiency of both asynchronous and synchronous approaches to HBCR, a broadening of coverage options for HBCR will be warranted.
FUTURE DIRECTIONS
Future research studies will need to address several questions. Does asynchronous HBCR lead to outcomes that are as good as or better than synchronous HBCR? Is one approach preferred in lower-risk patients? Is one approach preferred in higher-risk patients? Does the use of combined asynchronous and synchronous delivery options result in better patient outcomes than the use of either modality alone? Which modality leads to the best longer-term adherence and outcomes? How can either modality avoid the potential negative effects of the digital divide, potentially increasing the gap in HBCR delivery in underserved populations with limited resources who are at highest risk for gaps in their health care services?
SUMMARY
There is a growing body of evidence suggesting an important role for HBCR in the delivery of CR services. Randomized studies suggest that asynchronous and synchronous HBCR services have similar shorter-term outcomes in low- to moderate-risk individuals. Asynchronous models of HBCR have greater flexibility for CR patients and CR staff, while synchronous models of HBCR provide greater real-time evaluation and guidance for CR patients from CR staff. Challenges that are not science based may potentially influence the feasibility and application of asynchronous and synchronous HBCR, including medicolegal issues, staffing requirements, and the need for reimbursement. Important scientific questions need to be addressed by future research studies to clarify the roles and impact of asynchronous and synchronous HBCR models of CR care.
Footnotes
Dr Beatty was formerly employed at Apple Inc from 2018–2019 and held stock in Apple Inc from 2018–2021. The other authors declare no conflicts of interest.
REFERENCES
- 1.Balady GJ, Ades PA, Bittner VA, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. 2011;124(25):2951–2960. [DOI] [PubMed] [Google Scholar]
- 2.Thomas RJ, Beatty AL, Beckie TM, et al. Home-based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. J Cardiopulm Rehab Prev. 2019;39(4):208–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scherrenberg M, Wilhelm M, Hansen D, et al. The future is now: a call for action for cardiac telerehabilitation in the COVID-19 pandemic from the secondary prevention and rehabilitation section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2021;28(5):524–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nakayama A, Takayama N, Kobayashi M, et al. Remote cardiac rehabilitation is a good alternative of outpatient cardiac rehabilitation in the COVID-19 era. Environ Health Prev Med. 2020;25:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rawstorn JC, Gant N, Rolleston A, et al. End users want alternative intervention delivery models: usability and acceptability of the REMOTE-CR exercise-based cardiac telerehabilitation program. Arch Phys Med Rehabil. 2018;99(11):2373–2377. [DOI] [PubMed] [Google Scholar]
- 6.Synchronous vs. asynchronous communication: a guide for managers. https://fellow.app/blog/remote/synchronous-vs-asynchronous-communication-guide-for-managers. Published 2021. Accessed July 9, 2021.
- 7.DeBusk RF, Miller NH, Superko HR, et al. A case-management system for coronary risk factor modification after acute myocardial infarction. Ann Intern Med. 1994;120(9):721–729. [DOI] [PubMed] [Google Scholar]
- 8.Varnfield M, Karunanithi M, Lee CK, et al. Smartphone-based home care model improved use of cardiac rehabilitation in post-myocardial infarction patients: results from a randomised controlled trial. Heart. 2014;100(22):1770–1779. [DOI] [PubMed] [Google Scholar]
- 9.Piotrowicz E, Pencina MJ, Opolski G, et al. Effects of a 9-week hybrid comprehensive telerehabilitation program on long-term outcomes in patients with heart failure: the telerehabilitation in heart failure patients (TELEREH-HF) randomized clinical trial. JAMA Cardiol. 2020;5(3):300–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hwang R, Morris NR, Mandrusiak A, et al. Cost-utility analysis of home-based telerehabilitation compared with centre-based rehabilitation in patients with heart failure. Heart Lung Circ. 2019;28(12):1795–1803. [DOI] [PubMed] [Google Scholar]
- 11.Brewer LC, Kaihoi B, Schaepe K, et al. Patient-perceived acceptability of a virtual world-based cardiac rehabilitation program. Digit Health. 2017;3:2055207617705548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Balady GJ, Williams MA, Ades PA, et al. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. J Cardiopulm Rehab Prev. 2007;27(3):121–129. [DOI] [PubMed] [Google Scholar]
- 13.Sparks KE, Shaw DK, Eddy D, Hanigosky P, Vantrese J. Alternatives for cardiac rehabilitation patients unable to return to a hospital-based program. Heart Lung. 1993;22(4):298–303. [PubMed] [Google Scholar]
- 14.Anderson L, Sharp GA, Norton RJ, et al. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev. 2017;6(6):CD007130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dalal HM, Taylor RS, Wingham J, et al. A Facilitated Home-Based Cardiac Rehabilitation Intervention for People With Heart Failure and Their Caregivers: A Research Programme Including the REACH-HF RCT. Southampton, England: NIHR Journals Library; 2021. [PubMed] [Google Scholar]
- 16.Avila A, Claes J, Goetschalckx K, et al. Home-based rehabilitation with telemonitoring guidance for patients with coronary artery disease (Short-Term Results of the TRiCH Study): randomized controlled trial. J Med Internet Res. 2018;20(6):e225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Batalik L, Dosbaba F, Hartman M, Batalikova K, Spinar J. Benefits and effectiveness of using a wrist heart rate monitor as a telerehabilitation device in cardiac patients: a randomized controlled trial. Medicine (Baltimore). 2020;99(11):e19556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bravo-Escobar R, Gonzalez-Represas A, Gomez-Gonzalez AM, Heredia-Torres A. Effectiveness of e-Health cardiac rehabilitation program on quality of life associated with symptoms of anxiety and depression in moderate-risk patients. Sci Rep. 2021;11(1):3760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Claes J, Cornelissen V, McDermott C, et al. Feasibility, acceptability, and clinical effectiveness of a technology-enabled cardiac rehabilitation platform (Physical Activity Toward Health-I): randomized controlled trial. J Med Internet Res. 2020;22(2):e14221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schopfer DW, Whooley MA, Allsup K, et al. Effects of home-based cardiac rehabilitation on time to enrollment and functional status in patients with ischemic heart disease. J Am Heart Assoc. 2020;9(19):e016456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Snoek JA, Prescott EI, van der Velde AE, et al. Effectiveness of home-based mobile guided cardiac rehabilitation as alternative strategy for nonparticipation in clinic-based cardiac rehabilitation among elderly patients in Europe: a randomized clinical trial. JAMA Cardiol. 2021;6(4):463–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Song Y, Ren C, Liu P, Tao L, Zhao W, Gao W. Effect of smartphone-based telemonitored exercise rehabilitation among patients with coronary heart disease. J Cardiovasc Transl Res. 2020;13(4):659–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Uddin J, Joshi VL, Moniruzzaman M, et al. Effect of home-based cardiac rehabilitation in a lower-middle income country: results from a controlled trial. J Cardiopulm Rehabil Prev. 2020;40(1):29–34. [DOI] [PubMed] [Google Scholar]
- 24.Maddison R, Rawstorn JC, Stewart RAH, et al. Effects and costs of real-time cardiac telerehabilitation: randomised controlled non-inferiority trial. Heart. 2019;105(2):122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Drwal KR, Wakefield BJ, Forman DE, Wu WC, Haraldsson B, El Accaoui RN. Home-based cardiac rehabilitation: experience from the Veterans Affairs. J Cardiopulm Rehabil Prev 2021;41(2): 93–99. [DOI] [PubMed] [Google Scholar]
- 26.Dalal HM, Taylor RS, Jolly K, et al. The effects and costs of home-based rehabilitation for heart failure with reduced ejection fraction: the REACH-HF multicentre randomized controlled trial. Eur J Prev Cardiol. 2019;26(3):262–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frost J, Wingham J, Britten N, et al. Home-based rehabilitation for heart failure with reduced ejection fraction: mixed methods process evaluation of the REACH-HF multicentre randomised controlled trial. BMJ Open. 2019;9:e026039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wingham J, Frost J, Britten N, et al. Caregiver outcomes of the REACH-HF multicentre randomized controlled trial of home-based rehabilitation for heart failure with reduced ejection fraction. Eur J Cardiovasc Nurs. 2019;18(7):611–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fletcher GF, Chiaramida AJ, LeMay MR, Johnston BL, Thiel JE, Spratlin MC. Telephonically-monitored home exercise early after coronary artery bypass surgery. Chest. 1984;86(2):198–202. [DOI] [PubMed] [Google Scholar]
- 30.Squires RW, Miller TD, Harn T, Micheels TA, Palma TA. Transtelephonic electrocardiographic monitoring of cardiac rehabilitation exercise sessions in coronary artery disease. Am J Cardiol. 1991;67(11):962–964. [DOI] [PubMed] [Google Scholar]
- 31.O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127(4):e362–e425. [DOI] [PubMed] [Google Scholar]
- 32.Thomas RJ, Balady G, Banka G, et al. 2018 ACC/AHA clinical performance and quality measures for cardiac rehabilitation: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J Am Coll Cardiol 2018;71(16):1814–1837. [DOI] [PubMed] [Google Scholar]
- 33.Beatty AL, Doll JA, Schopfer DW, et al. Cardiac rehabilitation participation and mortality after percutaneous coronary intervention: insights from the Veterans Affairs Clinical Assessment, Reporting, and Tracking Program. J Am Heart Assoc. 2018;7(19):e010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Beatty AL, Truong M, Schopfer DW, Shen H, Bachmann JM, Whooley MA. Geographic variation in cardiac rehabilitation participation in Medicare and Veterans Affairs populations: opportunity for improvement. Circulation. 2018;137(18):1899–1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li S, Fonarow GC, Mukamal K, et al. Sex and racial disparities in cardiac rehabilitation referral at hospital discharge and gaps in long-term mortality. J Am Heart Assoc. 2018;7(8):e008088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Turk-Adawi K, Supervia M, Lopez-Jimenez F, et al. Cardiac rehabilitation availability and density around the globe. EClinicalMedicine. 2019;13:31–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Falter M, Scherrenberg M, Dendale P. Digital health in cardiac rehabilitation and secondary prevention: a search for the ideal tool. Sensors (Basel). 2020;21(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Funahashi TBL, Joshi N. Saving lives with virtual cardiac rehabilitation. NEJM Catalyst. 2019:1–14. [Google Scholar]
- 39.Schopfer DW, Krishnamurthi N, Shen H, Duvernoy CS, Forman DE, Whooley MA. Association of Veterans Health Administration home-based programs with access to and participation in cardiac rehabilitation. JAMA Intern Med. 2018;178(5):715–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Berry R, Brawner CA, Kipa SG, Stevens C, Bloom C, Keteyian SJ. Telemedicine home-based cardiac rehabilitation: a case series. J Cardiopulm Rehabil Prev. 2020;40(4):245–248. [DOI] [PMC free article] [PubMed] [Google Scholar]


