Abstract
Uninsured or underinsured individuals with cancer are likely to experience financial hardship, including forgoing healthcare or non-healthcare needs such as food, housing, or utilities. This study evaluates the association between health insurance coverage and financial hardship among cancer survivors during the COVID-19 pandemic. This cross-sectional analysis used Patient Advocate Foundation (PAF) survey data from May to July 2020. Cancer survivors who previously received case management or financial aid from PAF self-reported challenges paying for healthcare and non-healthcare needs during the COVID-19 pandemic. Associations between insurance coverage and payment challenges were estimated using Poisson regression with robust standard errors, which allowed for estimation of adjusted relative risks (aRR). Of 1,437 respondents, 74% had annual household incomes <$48,000. Most respondents were enrolled in Medicare (48%), 22% in employer-sponsored insurance, 13% in Medicaid, 6% in an Affordable Care Act (ACA) plan, and 3% were uninsured. Approximately 31% of respondents reported trouble paying for healthcare during the COVID-19 pandemic. Respondents who were uninsured (aRR 2.58, 95% confidence interval [CI] 1.83–3.64), enrolled in an ACA plan (aRR 1.86, 95% CI 1.28–2.72), employer-sponsored insurance (aRR 1.70, 95% CI 1.23–2.34), or Medicare (aRR 1.49, 95% CI 1.09–2.03) had higher risk of trouble paying for healthcare compared to Medicaid enrollees. Challenges paying for non-healthcare needs were reported by 57% of respondents, with 40% reporting trouble paying for food, 31% housing, 28% transportation, and 20% internet. In adjusted models, Medicare and employer-sponsored insurance enrollees were less likely to have difficulties paying for non-healthcare needs compared to Medicaid beneficiaries. Despite 97% of our cancer survivor sample being insured, 31% and 57% reported trouble paying for healthcare and non-healthcare needs during the COVID-19 pandemic, respectively. Greater attention to both medical and non-medical financial burden is needed given the economic pressures of the COVID-19 pandemic.
Introduction
Despite an increase in insurance coverage rates due to the passage of the Patient Protection and Affordable Care Act (ACA) [1], rates of underinsurance remain high among Americans with cancer [2]. Underinsurance, often characterized by spending >10% of household income on healthcare, is associated with cancer treatment delays and financial distress [3, 4]. Job layoffs and economic insecurity stemming from the COVID-19 pandemic are likely to increase rates of uninsurance and underinsurance [5]. For cancer survivors, these increases may be associated with financial hardship and result in forgone healthcare or non-healthcare purchases, such as food, housing, or utilities. This study examines the relationship between health insurance coverage and challenges paying for healthcare and non-healthcare needs during the COVID-19 pandemic in adults with cancer.
Materials and methods
This analysis used secondary, cross-sectional survey data from individuals who had previously received case management or financial aid from Patient Advocate Foundation (PAF), a non-profit organization that helps individuals with chronic illnesses access recommended care. Internet surveys were fielded from May 20 to July 12, 2020. Survey participation was incentivized via drawings for six individual $25 gift cards. Respondents provided written informed consent for all PAF survey communications. The University of Alabama at Birmingham Institutional Review Board approved this secondary analysis of the PAF survey data. Respondents reported challenges paying for healthcare and non-healthcare needs using the single-item survey question, “Have you had trouble paying for any of the following since the beginning of the COVID-19 pandemic?” Respondents were then asked to select all that applied, which included food, household supplies, housing (rent or mortgage), utilities, phone, internet/data, car/gas/transportation, childcare/eldercare/home health services, and healthcare/medical costs (e.g., prescription medications, doctor’s visits, clinical/hospital services, medical supplies).
Associations between insurance coverage and challenges affording healthcare or non-healthcare needs during the COVID-19 pandemic were estimated using adjusted relative risks (aRR) and 95% confidence intervals (CI) from modified Poisson models with robust standard errors [6]. Use of modified Poisson regression with sandwich errors for analysis of binary outcomes produces reliable estimates of relative risk, which is more easily interpretable than odds ratios produced by logistic regression [6]. Models were adjusted for age, sex, race and ethnicity, household income, education, employment, rurality, cancer type, and comorbidity count.
Results
Surveys were e-mailed to 15,857 PAF clients and completed by 4,108 (26% response rate; S1 Table). Of 1,437 respondents reporting a previous cancer diagnosis, 38% were aged <55 years, 23% were Black or African American, 74% had annual household incomes <$48,000, and 40% had a bachelor’s degree or higher (Table 1). Breast cancer was most common among respondents (35%), and 41% reported ≥3 additional comorbidities. Most respondents were enrolled in Medicare (48%), 22% in employer-sponsored insurance, 13% in Medicaid, 6% in an ACA plan, and 3% were uninsured.
Table 1. Respondent sociodemographic and clinical characteristics (N = 1437).
| Total N = 1437 | |
|---|---|
| Age | |
| 19–35 | 60 (4.2) |
| 36–55 | 490 (34.1) |
| 56–75 | 790 (55.0) |
| ≥ 76 | 97 (6.8) |
| Sex | |
| Male | 404 (28.1) |
| Female | 1033 (71.9) |
| Race and ethnicity | |
| White | 851 (59.2) |
| Black/African American | 336 (23.4) |
| Hispanic/Latino | 120 (8.4) |
| Other | 76 (5.3) |
| Unknown | 54 (3.8) |
| Education | |
| Less than high school | 41 (2.9) |
| High school degree | 321 (22.3) |
| Some college | 501 (34.9) |
| ≥ Bachelor’s degree | 569 (39.6) |
| Unknown | 5 (0.4) |
| Employment status | |
| Employed | 307 (21.4) |
| Retired | 397 (27.6) |
| Disabled | 535 (37.3) |
| Unemployed/other | 198 (13.8) |
| Household income | |
| ≤$47,999 | 1061 (73.8) |
| >$47,999 | 359 (25.0) |
| Unknown | 17 (1.2) |
| Rural-Urban Commuting Area | |
| Urban | 1083 (75.4) |
| Rural | 137 (9.5) |
| Unknown | 217 (15.1) |
| Cancer type | |
| Breast | 497 (34.6) |
| Genitourinary | 83 (5.8) |
| Gynecological | 38 (2.6) |
| Gastrointestinal | 75 (5.2) |
| Hematologic | 429 (29.9) |
| Other | 315 (21.9) |
| Comorbidity count* | |
| 0 | 583 (40.6) |
| 1–2 | 482 (33.5) |
| ≥3 | 372 (25.9) |
| Health insurance status | |
| Employer-sponsored | 322 (22.4) |
| ACA | 90 (6.3) |
| Medicare | 694 (48.3) |
| Medicaid | 185 (12.9) |
| Uninsured | 49 (3.4) |
| Other / unknown | 97 (6.8) |
*Count of comorbidities other than cancer
ACA = Affordable Care Act
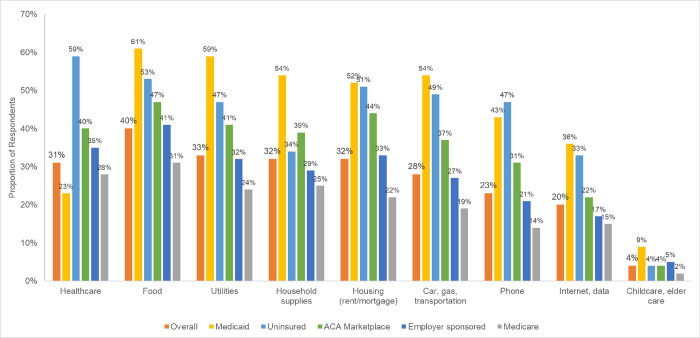
Overall, 31% of respondents reported challenges paying for healthcare during the COVID-19 pandemic (Fig 1). In adjusted models, respondents who were uninsured (aRR 2.58, 95% CI 1.83–3.64), enrolled in an ACA plan (aRR 1.86, 95% CI 1.28–2.72), employer-sponsored insurance (aRR 1.70, 95% CI 1.23–2.34), or Medicare (aRR 1.49, 95% CI 1.09–2.03) were more likely to report trouble paying for healthcare compared to Medicaid enrollees (Table 2).
Fig 1. Proportion of respondents reporting trouble paying for healthcare and non-healthcare needs during the COVID-19 pandemic by health insurance status (N = 1437).
Table 2. Adjusted model results estimating relative risk of trouble paying for healthcare or any non-healthcare need in cancer survivors (N = 1437).
| Trouble paying for healthcare | Trouble paying for any non-healthcare need | |
|---|---|---|
| Relative Risk | Relative Risk | |
| (95% Confidence Interval) | (95% Confidence Interval) | |
| Health insurance status | ||
| Medicaid | Ref. | Ref. |
| Affordable Care Act | 1.86 (1.28–2.72) | 0.88 (0.75–1.03) |
| Employer-sponsored | 1.70 (1.23–2.34) | 0.78 (0.69–0.87) |
| Medicare | 1.49 (1.09–2.03) | 0.76 (0.68–0.84) |
| Uninsured | 2.58 (1.83–3.64) | 0.91 (0.77–1.07) |
| Other / unknown | 1.44 (0.96–2.18) | 0.83 (0.71–0.98) |
| Age | ||
| 19–35 | Ref. | Ref. |
| 36–55 | 1.23 (0.82–1.85) | 0.98 (0.83–1.16) |
| 56–75 | 1.14 (0.75–1.73) | 0.83 (0.70–0.99) |
| ≥ 76 | 1.02 (0.57–1.82) | 0.61 (0.42–0.89) |
| Sex | ||
| Male | Ref. | Ref. |
| Female | 0.96 (0.78–1.19) | 1.04 (0.92–1.17) |
| Race and ethnicity | ||
| White | Ref. | Ref. |
| Black/African American | 0.99 (0.82–1.19) | 1.31 (1.20–1.43) |
| Hispanic/Latino | 1.19 (0.91–1.56) | 1.16 (1.02–1.32) |
| Other | 1.14 (0.83–1.57) | 1.00 (0.82–1.22) |
| Education | ||
| Less than high school | Ref. | Ref. |
| High school degree | 1.28 (0.71–2.30) | 0.91 (0.74–1.11) |
| Some college | 1.44 (0.81–2.55) | 0.93 (0.76–1.14) |
| ≥ Bachelor’s degree | 1.37 (0.77–2.45) | 0.86 (0.70–1.06) |
| Employment status | ||
| Employed | Ref. | Ref. |
| Retired | 0.81 (0.61–1.09) | 0.58 (0.47–0.70) |
| Disabled | 1.13 (0.90–1.41) | 1.13 (1.00–1.27) |
| Unemployed/other | 1.21 (0.94–1.56) | 1.08 (0.95–1.23) |
| Household income | ||
| ≤ $47,999 | Ref. | Ref. |
| > $47,999 | 1.00 (0.83–1.21) | 0.89 (0.80–1.00) |
| Rural-Urban Commuting Area | ||
| Urban | Ref. | Ref. |
| Rural | 1.25 (0.99–1.58) | 0.93 (0.80–1.07) |
| Cancer type | ||
| Breast | Ref. | Ref. |
| Genitourinary | 0.71 (0.43–1.16) | 0.84 (0.63–1.11) |
| Gynecological | 1.10 (0.74–1.66) | 0.89 (0.67–1.17) |
| Gastrointestinal | 0.87 (0.59–1.29) | 1.00 (0.84–1.18) |
| Hematologic | 0.78 (0.63–0.98) | 1.02 (0.91–1.14) |
| Other | 1.06 (0.86–1.30) | 0.99 (0.89–1.11) |
| Comorbidity count* | ||
| 0 | Ref. | Ref. |
| 1–2 | 1.10 (0.90–1.33) | 1.05 (0.94–1.16) |
| ≥ 3 | 1.50 (1.24–1.82) | 1.30 (1.18–1.44) |
*Count of comorbidities other than cancer
Challenges paying for non-healthcare needs during the COVID-19 pandemic were reported by 57% of respondents, with 40% reporting trouble paying for food, 32% for housing, 28% for transportation, and 20% for internet (Fig 1). In adjusted models, respondents enrolled in Medicare (aRR 0.76, 95% CI 0.68–0.84) or employer-sponsored insurance (aRR 0.78, 95% CI 0.69–0.87) were less likely to report challenges paying for non-healthcare needs compared to Medicaid enrollees (Table 2). In adjusted models of specific non-healthcare needs, Medicare beneficiaries and respondents enrolled in employer-sponsored plans were less likely to report trouble paying for food, household supplies, housing, utilities, a phone, internet or data, and transportation compared to Medicaid beneficiaries (S2 Table).
Discussion
Individuals with cancer are dealing with many financial challenges potentially associated with the COVID-19 pandemic, with 57% of our sample reporting trouble paying for non-healthcare needs and 31% reporting trouble paying for healthcare. Our results suggest the financial hardship experienced by cancer survivors may have been exacerbated during the COVID-19 pandemic when compared to pre-pandemic estimates, such as those in a recent study by Han and colleagues. Using the 2016 Medical Expenditures Panel Survey data, Han estimated 16% of cancer survivors experienced material financial hardship, which includes reduced spending on non-healthcare needs, and 27% experienced delayed or forgone health care due to cost [7]. Our study also showed risk of payment challenges differed by insurance coverage status. Medicaid beneficiaries were at lowest risk of challenges paying for healthcare, but highest risk of trouble affording non-healthcare needs. Conversely, respondents enrolled in an ACA plan, employer-sponsored insurance, or Medicare were more likely to report difficulties in paying for healthcare compared to Medicaid enrollees.
Our results suggest private insurance and Medicare coverage may not sufficiently protect against out-of-pocket medical costs in individuals with cancer. In our study, individuals with ACA, employer-sponsored, or Medicare insurance were at higher risk of trouble paying for healthcare during the COVID-19 pandemic compared to Medicaid enrollees. This is likely due to substantial cost sharing requirements posed by these insurance mechanisms. An estimated 47% of privately-insured patients are enrolled in high-deductible health plans [8]. In 2020, individual silver plan ACA deductibles averaged $4,450 and 26% of individuals with employer-sponsored insurance had annual deductibles of at least $2,000 [9, 10]. After deductibles are met, normal patient cost-sharing provisions such as copayments or coinsurance apply. Though the majority of Medicare beneficiaries are enrolled in supplemental coverage which offsets beneficiary Medicare Parts A and B cost sharing, Medicare Part D, which covers many oral anticancer medications, has no cap on patient out-of-pocket costs and imposes 25% co-insurance during the initial coverage period and in the coverage gap. Because the mean anticancer medication price was almost $14,000 in 2018, this benefit design commonly results in high out-of-pocket spending for enrollees with a cancer diagnosis [11]. Conversely, out-of-pocket costs for premium and cost sharing are capped at 5% of household income for all Medicaid enrollees [12]. Efforts towards increasing provider awareness of potential financial hardship in insured patients is needed during treatment and survivorship care planning.
On the other hand, over half of our study respondents reported trouble paying for non-healthcare needs during the COVID-19 pandemic, with similar risks of trouble found in respondents who were uninsured, ACA-insured, and enrolled in Medicaid. Difficulties in paying for non-medical necessities can affect cancer outcomes. Food-insecure cancer survivors have higher odds of forgone, delayed, or altered cancer treatment than those who are food secure [13]. Challenges paying for transportation, cited by almost one-third of our study respondents and half of Medicaid enrollees, can compound quickly and negatively impact receipt of care [14]. The pandemic-induced shifts to telehealth may not sufficiently offset access challenges stemming from transportation, as 53% of respondents in our study reporting transportation cost challenges also reported trouble affording internet [15]. While addressing food or housing insecurity may extend beyond the immediate scope of clinical practice, provider inquiry and accommodation of patient transportation and internet challenges, such as scheduling same-day appointments with cancer care team members, could reduce financial burden and improve receipt of recommended care. Of note, ACA-insured and Medicaid patients reported similar levels of difficulty in paying for non-healthcare necessities. However, there is no differentiation between ACA or employer-sponsored insurance in the electronic medical record. Patients with either type of coverage will appear as privately insured. Thus, providers should be aware that many of their privately insured patients face the same financial challenges as their Medicaid patients, and may wish to extend any discussions of financial burden or assistance to their privately insured patients as well.
The results of our study should be considered within limitations. The survey captures data from cancer survivors who previously received help accessing or paying for care from PAF and may not be representative of the larger cancer patient population. Information potentially associated with health insurance coverage and challenges paying for healthcare and non-healthcare needs, such as time since cancer diagnosis, current health care use or needs, and more detailed demographic information, was limited by use of secondary data. The results of our study could have been impacted by pandemic-related employment changes. However, this was uncommon in our study with only 2% of respondents reporting employment loss due to the COVID-19 pandemic. We had a low survey response rate, potentially due to the COVID-19 pandemic, which may result in selection bias. Our sample may also be biased towards individuals able to navigate services from a non-profit organization or access web-based surveys.
Conclusions
In this sample of cancer survivors, 31% and 57% reported trouble paying for healthcare and non-healthcare needs during the COVID-19 pandemic, respectfully. Those with private insurance or Medicare were more likely to report trouble paying for healthcare, while those enrolled in Medicaid most often reported trouble paying for non-healthcare needs. System-level efforts towards ensuring insurance coverage adequately addresses healthcare needs and provider-level efforts to incorporate financial information in clinical decision-making could aid in reducing patient-level financial hardship associated with the COVID-19 pandemic.
Supporting information
(DOCX)
(DOCX)
Acknowledgments
Previous presentations: This work was presented as a poster presentation at the virtual 2021 Academy Health Annual Research Meeting, June 14–17, 2021.
Data Availability
Data that support the findings of this study was collected for organizational and programmatic purposes by Patient Advocate Foundation and may be available upon request. Participants of this study did not agree for their data to be shared publicly. Use of data from Patient Advocate Foundation for analytic purposes requires a data use agreement that is reviewed by the external compliance officer prior to signature by both parties. Please contact PAF Compliance Officer Stephanie Trunk (Stephanie.trunk@patientadvocate.org) with inquiries.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Nipp RD, Shui AM, Perez GK, Kirchhoff AC, Peppercorn JM, Moy B, et al. Patterns in Health Care Access and Affordability Among Cancer Survivors During Implementation of the Affordable Care Act. JAMA Oncol. 2018;4(6):791–7. Epub 2018/03/30. doi: 10.1001/jamaoncol.2018.0097 ; PubMed Central PMCID: PMC5885177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collins SR, Rasmussen PW, Beutel S, Doty MM. The problem of underinsurance and how rising deductibles will make it worse. Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2014. Issue Brief (Commonw Fund). 2015;13:1–20. Epub 2015/06/03. . [PubMed] [Google Scholar]
- 3.Fletcher SA, Cole AP, Lu C, Marchese M, Krimphove MJ, Friedlander DF, et al. The impact of underinsurance on bladder cancer diagnosis, survival, and care delivery for individuals under the age of 65 years. 2020;126(3):496–505. doi: 10.1002/cncr.32562 [DOI] [PubMed] [Google Scholar]
- 4.Chino F, Peppercorn JM, Rushing C, Kamal AH, Altomare I, Samsa G, et al. Out-of-Pocket Costs, Financial Distress, and Underinsurance in Cancer Care. JAMA Oncol. 2017;3(11):1582–4. Epub 2017/08/11. doi: 10.1001/jamaoncol.2017.2148 ; PubMed Central PMCID: PMC5824215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garfield R CG, Damico A, Levitt L. Eligibility for ACA Health Coverage Following Job Loss 2020 [cited 2021 March 9].
- 6.Zou G. A Modified Poisson Regression Approach to Prospective Studies with Binary Data. American Journal of Epidemiology. 2004;159(7):702–6. doi: 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
- 7.Han X, Zhao J, Zheng Z, de Moor JS, Virgo KS, Yabroff KRJCE, et al. Medical financial hardship intensity and financial sacrifice associated with cancer in the United States. 2020;29(2):308–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen RAM, Michael E Zammitti; Emily P. Health Insurance Coverage: Early Release of Estimates From the National Health Interview Survey, January–March 2018. In: Services USDoHaH, editor. Centers for Disease Control and Prevention, National Center for Health Statistics 2018. [Google Scholar]
- 9.Claxton G, Damico A, Rae M, Young G, McDermott D, Whitmore HJHA. Health Benefits In 2020: Premiums In Employer-Sponsored Plans Grow 4 Percent; Employers Consider Responses To Pandemic: The annual Kaiser Family Foundation Employer Health Benefits Survey of the cost and coverage of US employer-sponsored health benefits. 2020;39(11):2018–28. doi: 10.1377/hlthaff.2020.01569 [DOI] [PubMed] [Google Scholar]
- 10.Cox C, Fehr R., Pollitz K., McDermott D., Claxton G., Damico A. Affordability in the ACA Marketplace Under a Proposal Like Joe Biden’s Health Plan: Kaiser Family Foundation; 2020. [February 17, 2021]. Available from: https://www.kff.org/health-reform/issue-brief/affordability-in-the-aca-marketplace-under-a-proposal-like-joe-bidens-health-plan/. [Google Scholar]
- 11.Dusetzina SB, Huskamp HA, Keating NL. Specialty Drug Pricing and Out-of-Pocket Spending on Orally Administered Anticancer Drugs in Medicare Part D, 2010 to 2019. JAMA. 2019;321(20):2025–8. doi: 10.1001/jama.2019.4492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brooks T, Roygardner L, Artiga S, Pham O, Dolan RJSFKFFAJ. Medicaid and CHIP eligibility, enrollment, and cost sharing policies as of January 2019: findings from a 50-State survey. 2019;22:2020. [Google Scholar]
- 13.McDougall JA, Anderson J, Adler Jaffe S, Guest DD, Sussman AL, Meisner AL, et al. Food insecurity and forgone medical care among cancer survivors. 2020;16(9):e922–e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Resio BJ, Chiu AS, Hoag JR, Brown LB, White M, Omar A, et al. Motivators, barriers, and facilitators to traveling to the safest hospitals in the United States for complex cancer surgery. 2018;1(7):e184595–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koonin LM, Hoots B, Tsang CA, Leroy Z, Farris K, Jolly B, et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic—United States, January–March 2020. 2020;69(43):1595. [DOI] [PMC free article] [PubMed] [Google Scholar]