Abstract
Background
Numerous studies suggest a positive association between physical activity and physical fitness in schoolchildren. However, little is known about some neglected forms of physical activity and their associations with physical fitness. This study was conducted via a self-reported questionnaire, owing to the COVID-19 pandemic in many regions in China.
Purpose
This study explores the associations between participating in sports, muscle-strengthening exercises, and active commuting with self-reported physical fitness assessed by the International Fitness Scale (IFIS).
Methods
A total of 3,807 study participants (ages 11–17) from 12 public schools in South-eastern China were recruited, with 2,407 providing valid data on variables for analysis. Study participants were asked to self-report their sociodemographic factors (i.e., sex, grade, age), participation in sports (never, 1–3 times per month, 1–2 times per week, and 3 or more times per week), muscle-strengthening exercise (0–7 days) and active commuting (0–5 days). Generalized linear models were used to explore the associations between sports participation, muscle-strengthening exercise, and active commuting with self-reported physical fitness (comprising general physical fitness, cardiorespiratory fitness, muscular strength, speed and agility, and flexibility). A total of 2,407 children and adolescents with a mean age of 13.82 (±2.1) years were included in the study's final analysis.
Results
The study found no significant association between active commuting and physical fitness. Regarding participating in sports and muscle-strengthening exercises, positive, significant associations were found, which showed that a higher frequency of participating in sports and more participation in muscle-strengthening exercises are associated with improved physical fitness.
Conclusion
This study offered evidence on the roles of some aspects of physical activity in physical fitness. To promote health in children and adolescents, they should be encouraged to participate in more sports and engage in muscle-strengthening exercises.
Keywords: sports participation, muscle strengthening exercise, active school travel, self-reported physical fitness, China
Highlights
- Physical fitness levels should be improved considerably in Chinese children and adolescents.
- Sports participation and muscle-strengthening exercise (MSE) were associated with higher levels of self-reported physical fitness.
- Active commuting might not be a contributor to self-reported physical fitness in Chinese children and adolescents.
Introduction
Physical fitness is defined as a set of attributes that people have or achieve while maintaining physical activity (1, 2). It is a well-recognised marker of an individual's health status (3–5). Physical fitness is classified as health-related and skill-related fitness (6). Five components compromise health-related physical fitness (HRPF): cardiorespiratory fitness, body composition, muscular strength, muscular endurance, and flexibility (6). Much evidence has demonstrated the importance and health benefits of higher levels of HRPF in children and adolescents (7, 8). For example, adolescents with higher levels of HRPF have a reduced risk of cardiovascular disease in later life (9). Cardiorespiratory fitness in adolescents is also directly associated with mental wellbeing and quality of life (10, 11). Also, higher cardiorespiratory fitness is positively associated with academic performance among adolescents (12). Muscular fitness (e.g., strength and endurance) is associated with lower risks of adiposity and cardiometabolic parameters and greater bone health in later life (13, 14). Because of the significance of HRPF, it is important to identify more effective ways to encourage it in children and adolescents. Nevertheless, synthesized data shows that lower levels of HRPF have been observed over the past two decades in children and adolescents (15).
Participating in regular and sufficient physical activity is associated with greater levels of HRPF in children and adolescents (7, 8). However, these studies focused on the overall levels of physical activity instead of different types of physical activity. According to earlier studies, adolescents can participate in many types of physical activity, including some that have been shown to be significantly associated with health outcomes and fitness components (8, 16, 17). For example, among the different types of physical activity, sports participation, muscle-strengthening exercise (MSE), and active commuting (AC) can all be organised frequently in school settings, while AC can happen daily. These two types are essential components of global surveillance of active lifestyles (18, 19). In terms of MSE, the World Health Organization recommends that young people (aged 11–17) should engage in it at least three times a week (20). Moreover, a large body of evidence indicates that participating in sports, MSE, and AC are associated with HRPF in adolescents (21–23).
Participating in sports is considered crucial to promoting positive health outcomes in children and adolescents (24, 25). Evidence has demonstrated higher levels of HRPF can be gained from participating in sports (26). A systematic review indicated that participating in organized sports was positively associated with muscular fitness among adolescents. AC plays a prominent role in preventing the risk of mental disorders (27, 28) and may reduce risks associated with poorer HRPF levels (21, 23). MSE is negatively associated with mental health disorders in adolescents and it can also promote muscular fitness (29). This evidence illustrates the importance of participating in sports, MSE, and AC for young people and promoting their health.
Studying the association between different types of physical activity and fitness helps design efficient and contextual fitness or health promotion plans. However, these associations remain rare in literature, limiting researchers' understanding of fitness promotion. It is, therefore, valuable to explore the associations of participating in sports, MSE, and AC with HRPF.
With the COVID-19 pandemic still active in many Chinese regions, assessing HRPF in adolescents using field-based assessment (such as a shuttle run for cardiorespiratory fitness) is unrealistic. Therefore, it is necessary to find an alternative to assess HRPF in adolescents. The International Fitness Scale (IFIS) is an option that can assess adolescents' HRPF simply and conveniently (30). The IFIS was developed in 2011 and much evidence has indicated that it is a reliable and valid instrument to assess HRPF in adolescents (30), with many studies confirming the psychometric properties of the IFIS in adolescents from various countries (31, 32). Unfortunately, evidence linking the benefits of participating in sports, MSE, and AC with self-reported HRPF is very rare, but this makes it worth studying.
To fill the research gap, this study, therefore, aims to explore the links between participating in sports, MSE, and AC (three different types of physical activity) with self-reported HRPF using a sample of Chinese adolescents.
Methods
Study design and participants
This study was a cross-sectional survey conducted between March and October in south-eastern China. 12 public schools in four cities in the South-eastern region were contacted, comprising 5 elementary schools, 5 middle schools and 2 high schools. In each school, 1–3 classes of each grade were randomly selected by a contact assigned to each school. This procedure recruited the initial sample comprising 3,807 children and adolescents (ages 11–17). Study participants providing information on variables of interest were included in this study, while those who did not report data on any variables (e.g., independents, outcomes and covariates) of interest that this study needed were excluded from the initial sample. For this study and further analysis, only 2,407 study participants were included as they provided valid data on variables this study needed. All the children and adolescents involved in the study, as well as their parents or guardians, were specifically advised that participation was completely voluntary. The study protocol and procedure were approved by the Institutional Review Board (IRB) of the Shanghai University of Sport with a Grant Number of 102772021RT071.
Measures
Independent variables (sports participation, MSE, AC)
Sports participation was measured by one question about the participation in organized sports and/or programs over the past 12 months. Participants were required to answer the frequency of sports participation in one week, with answer options of (1) Never, (2) 1–3 times per month, (3) 1–2 times per week, and (4) 3 or more times per week. This item has demonstrated good reliability and validity in assessing sports participation of children and adolescents (33).
MSE was assessed by the following question: “In the past week, how many days did you engage in exercise to strengthen or tone the muscle, such as push-ups, sit-ups, or lifting weights?” The possible responses were: 0 = none, 1 = 1 day, 2 = 2 days, 3 = 3 days, 4 = 4 days, 5 = 5 days, 6 = 6 days, and 7 = 7 days. This measure has been confirmed as reliable and valid in assessing MSE among Chinese children and adolescents (34). Based on the recommendation of the World Health Organization, participants who responded for 3 days or more were considered to meet the MSE guideline, otherwise, they were classified as not meeting the guideline (20).
AC was assessed by two independent questions: (1) On the weekdays, how many days did you go to school by walking, riding cycles, or other active ways? and (2) On the weekdays, how many days did go home after school by walking, riding cycles or other active ways?. The answer options for both the questions were 0–5 days.
Outcome variable (physical fitness)
The International Fitness Scale (IFIS) was used to evaluate the self-reported levels of HRPF, using a five-point Likert scale (very poor, poor, average, good, and very good). The IFIS contains five components, including general physical fitness, cardiorespiratory fitness, muscular strength, speed and agility, and flexibility. The scale has demonstrated acceptable reliability and validity in adolescents (32). In addition to the study sample for further analysis, 544 Chinese children and adolescents were also recruited, who took part in a reliability study. The unpublished results indicated that the IFIS had acceptable reliability (weighted kappa: 0.42–0.52; coefficient of internal consistency of 0.72) in Chinese children and adolescents (35). There has been convincing evidence to demonstrate the validity of the IFIS in children and adolescents (30). Hence, it was deemed that the IFIS can be used as a workable and valid instrument to assess HRPF in study participants of this study.
Controlling variables
Information on study participants' age, sex, siblings, living with parents or not, grade, residence, father and mother education level, and perceived family affluence (0–10 scale) were measured by a self-reported questionnaire. These sociodemographic factors were treated as covariates in further statistical analysis. Besides, study participants' moderate to vigorous physical activity and recreational screen time was assessed by the measures derived from the Health Behaviour in School-aged Children survey, with acceptable reliability and validity in Chinese children and adolescents (36). Sleep duration was measured by the Pittsburgh Sleep Scale. Moderate to vigorous physical activity, recreational screen time, and sleep duration was dichotomized as binary variable based on the Canadian 24-h Movement Guidelines (37, 38).
Statistical analysis
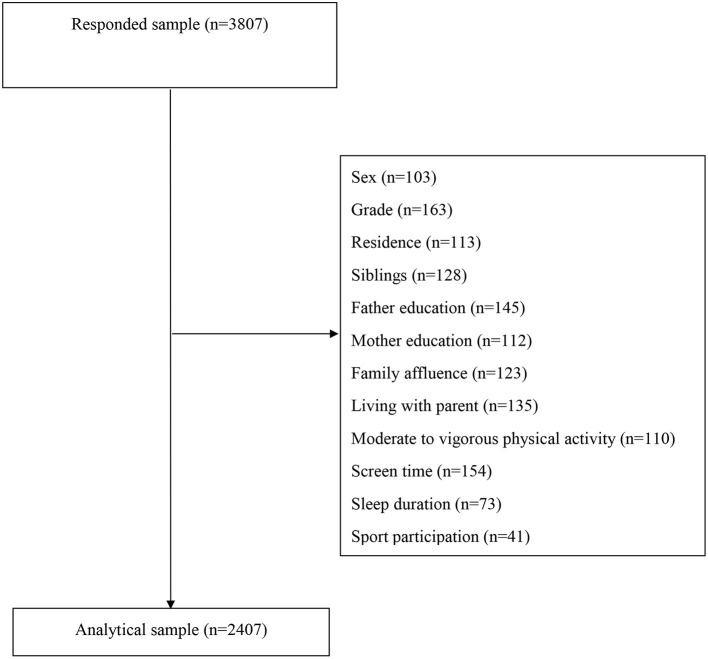
Prior to formal data analysis, missing data was coped with by using complete case analysis and the procedure can be found at Figure 1. All the statistical analysis was performed using SPSS 26.0 Version. Descriptive statistics (mean/standard deviation and percentage) were used to report sample characteristics. Mean with standard deviation was for continuous variables (e.g., age) while the percentage was for categorical variables (e.g., grade, residence). Partial correlation was used to explore the associations among sports participation, MSE, AC, and HRPF indicators after controlling for all the sociodemographic factors, moderate to vigorous physical activity, screen time, and sleep duration. To estimate the associations of sports participation (reference group: never), MSE (reference group: <3 times per week), and AC (0 days) with HRPF indicators, five separate models were established (model 1 for general physical fitness; model 2 for cardiorespiratory fitness; model 3 for muscular strength; model 4 for speed and agility; model 5 for flexibility). Entered in the model, sports participation, MSE, and AC were entered the model while controlling for all the other covariates. Generalized linear models with ordinal logistic regression were used to achieve the association estimation. The statistical significance was set up as p < 0.05.
Figure 1.
The procedure used for cleaning invalid and missing data in this study.
Results
Table 1 presents the sample characteristics. The mean age of all the study participants was 13.82 (±2.1), with boys accounting for 52.7%. More information on the study participants can be found in Table 1. In terms of sports participation, MSE, AC and self-reported HRPF indicators, 59.7% of the participants reported never engaging in any sports activities, whilst only 7.6% participated in sports more than three times per week. In addition, 23.4% met the MSE guideline. About 40% of study participants selected Active commuting for going to school or going home on weekdays.
Table 1.
Sample characteristics of this study.
| n/Mean | %/SD | |
|---|---|---|
| Age | 13.82 | 2.1 |
| Sex | ||
| Boy | 1,268 | 52.7 |
| Girl | 1,139 | 47.3 |
| Siblings | ||
| Yes | 1,184 | 49.2 |
| No | 1,223 | 50.8 |
| Living with parents | ||
| Yes | 2,018 | 83.8 |
| No | 389 | 16.2 |
| Grade | ||
| 4 | 355 | 14.7 |
| 5 | 334 | 13.9 |
| 7 | 353 | 14.7 |
| 8 | 415 | 17.2 |
| 10 | 515 | 21.4 |
| 11 | 435 | 18.1 |
| Residence | ||
| Rural | 277 | 11.5 |
| Suburban | 526 | 21.9 |
| Urban | 1,604 | 66.6 |
| Father education level | ||
| Middle school or below | 623 | 25.9 |
| High school | 595 | 24.7 |
| Undergraduate | 772 | 32.1 |
| Graduate | 137 | 5.7 |
| Unknown | 280 | 11.6 |
| Mother education level | ||
| Middle school or below | 770 | 32.0 |
| High school | 512 | 21.3 |
| Undergraduate | 732 | 30.4 |
| Graduate | 114 | 4.7 |
| Unknown | 279 | 11.6 |
| Family affluence | 5.09 | 1.5 |
| MVPA guideline | ||
| Not meet | 2,250 | 93.5 |
| Meet | 157 | 6.5 |
| Screen guideline | ||
| Not meet | 1,368 | 56.8 |
| Meet | 1,039 | 43.2 |
| Sleep guideline | ||
| Not meet | 1,674 | 69.5 |
| Meet | 733 | 30.5 |
| Sport participation | ||
| Never | 1,436 | 59.7 |
| 1-3 times per week | 370 | 15.4 |
| 1-2 times per week | 419 | 17.4 |
| 3 or more times per week | 182 | 7.6 |
| MSE guideline | ||
| Not meet | 1,844 | 76.6 |
| Meet | 563 | 23.4 |
| Active commuting on a weekday (go to school) | ||
| 0 | 1,077 | 44.7 |
| 1 day | 128 | 5.3 |
| 2 days | 132 | 5.5 |
| 3 days | 91 | 3.8 |
| 4 days | 80 | 3.3 |
| 5 days | 899 | 37.3 |
| Active commuting on a weekday (after school) | ||
| 0 | 970 | 40.3 |
| 1 day | 144 | 6.0 |
| 2 days | 129 | 5.4 |
| 3 days | 100 | 4.2 |
| 4 days | 67 | 2.8 |
| 5 days | 997 | 41.4 |
| Overall physical fitness | ||
| Very poor | 78 | 3.2 |
| Poor | 297 | 12.3 |
| Average | 1,254 | 52.1 |
| Good | 581 | 24.1 |
| Very good | 197 | 8.2 |
| Cardiorespiratory fitness | ||
| Very poor | 90 | 3.7 |
| Poor | 341 | 14.2 |
| Average | 1,140 | 47.4 |
| Good | 621 | 25.8 |
| Very good | 215 | 8.9 |
| Muscular strength | ||
| Very poor | 85 | 3.5 |
| Poor | 380 | 15.8 |
| Average | 1,239 | 51.5 |
| Good | 549 | 22.8 |
| Very good | 154 | 6.4 |
| Speed/Agility | ||
| Very poor | 63 | 2.6 |
| Poor | 305 | 12.7 |
| Average | 1,120 | 46.5 |
| Good | 667 | 27.7 |
| Very good | 252 | 10.5 |
| Flexibility | ||
| Very poor | 166 | 6.9 |
| Poor | 530 | 22.0 |
| Average | 1,031 | 42.8 |
| Good | 491 | 20.4 |
| Very good | 189 | 7.9 |
SD, standard deviation; MVPA, moderate to vigorous physical activity; MSE, muscle strengthening exercise.
The results from the partial correlation between sports participation, adherence to the MSE guideline, Active commuting, and HRPF indicators are shown in Table 2 after controlling for all the covariates. Specific results indicate that sports participation was correlated with all the indicators of self-reported HRPF (r ranged from 0.16–0.24, p < 0.001). Adherence to the MSE guideline was also associated with all the indicators of self-reported HRPF (r ranged from 0.13–0.23, p < 0.001). Active commuting was correlated with HRPF indicators, except for flexibility. This result is also displayed in the association between active commuting for home and HRPF indicators.
Table 2.
Partial correlation between sports participation, muscle strengthening exercise, active commuting and self-reported health-related physical fitness.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Sports participation | 1.00 | ||||||||
| 2. Muscle strengthening exercise | 0.25*** | 1.00 | |||||||
| 3. AC in weekday (school) | 0.10*** | 0.06** | 1.00 | ||||||
| 4. AC in weekday (home) | 0.08*** | 0.06** | 0.80*** | 1.00 | |||||
| 5. General physical fitness | 0.24*** | 0.21*** | 0.07*** | 0.06** | 1.00 | ||||
| 6. Cardiovascular fitness | 0.22*** | 0.20*** | 0.07*** | 0.07** | 0.57*** | 1.00 | |||
| 7. Muscular strength | 0.21*** | 0.23*** | 0.04 | 0.05* | 0.47*** | 0.43*** | 1.00 | ||
| 8. Speed and agility | 0.21*** | 0.19*** | 0.07*** | 0.05* | 0.51*** | 0.43*** | 0.43*** | 1.00 | |
| 9. Flexibility | 0.16*** | 0.13*** | 0.02 | 0.00 | 0.27*** | 0.24*** | 0.24*** | 0.27*** | 1.00 |
AC, active commuting.
p < 0.05,
p < 0.01,
p < 0.001.
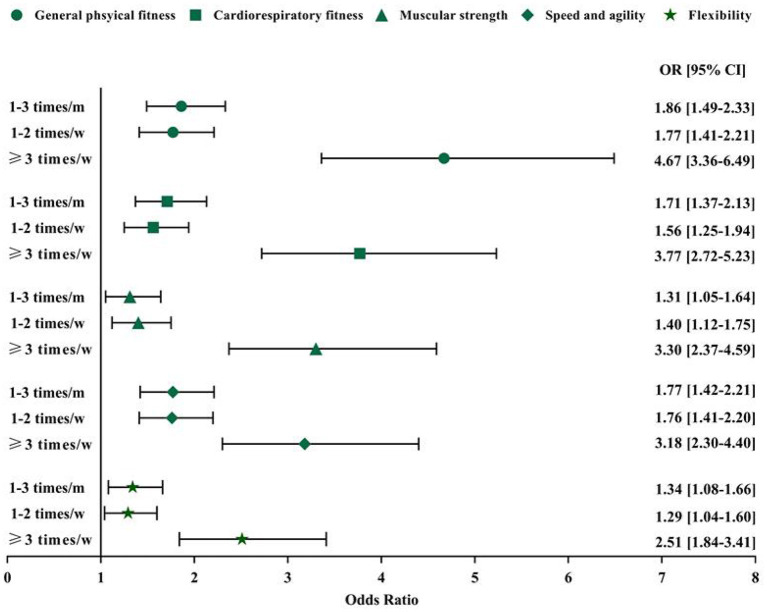
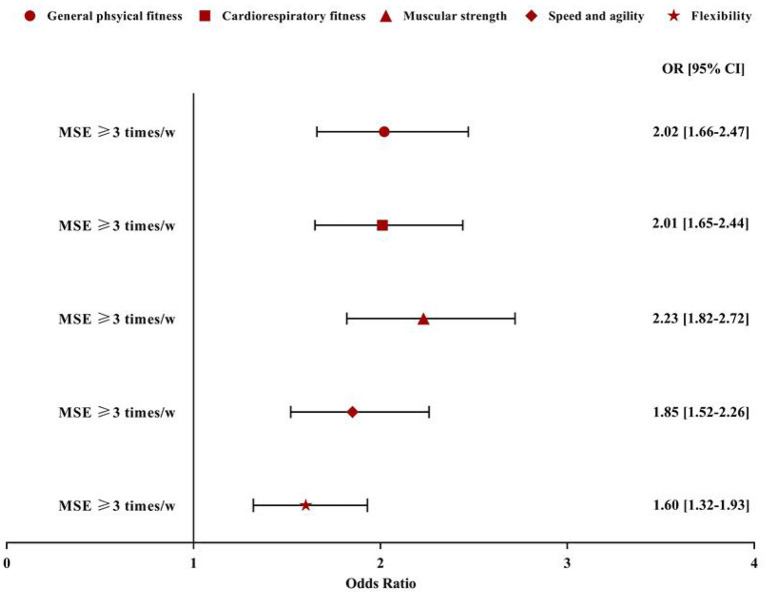
Following control of all the covariates in the current study results from the regression models suggested that sports participation (Figure 2) and adherence to the MSE guideline (Figure 3) were significantly associated with HRPF indicators in the study participants. Specifically, compared with participants who were never involved in sports participation, those reporting 1–3 times per month, 1–2 times per week, and 3 or more times per week had a greater likelihood of general physical fitness (OR = 1.86, 95% CI: 1.49–2.33; OR = 1.77, 95% CI: 1.41–2.21; OR = 4.67, 95% CI: 3.36–6.49). Similar results were also found in the association between sports participation and other HRPF indicators. However, no dose-dependent association was found between sports participation and HRPF indicators, except for muscular strength. As for the association between MSE and HRPF indicators, study participants meeting the MSE guideline were more likely to report higher levels of HRPF (OR for general physical fitness = 2.02, 95% CI: 1.66–2.47; OR for cardiorespiratory fitness = 2.01, 95% CI: 1.65–2.44; OR for muscular strength = 2.23, 95% CI: 1.82–2.72; OR for speed and agility = 1.85, 95%CI: 1.52–2.26; OR for flexibility = 1.60, 95% CI: 1.32–1.93). In the regression model, no significant association was found between Active commuting and HRPF indicators (all p > 0.05; data not shown) in the results.
Figure 2.
Association between frequency of sports participation and self-reported health-related physical fitness indicators. Model controlled for age, sex, siblings, living with parents or not, grade, residence, father and mother education level, and perceived family affluence, moderate to vigorous physical activity, recreational screen time and sleep duration. m, month; w, week; OR, odd ratio; CI, confidence interval. Reference group: never.
Figure 3.
Association between muscle strengthening exercise and self-reported health-related physical fitness indicators. Model controlled for age, sex, siblings, living with parents or not, grade, residence, father and mother education level, and perceived family affluence, moderate to vigorous physical activity, recreational screen time and sleep duration. MSE, muscle-strengthening exercise; w, week; OR, odd ratio; CI, confidence interval. Reference group: no more than 3 times/week.
Discussion
The primary aim of the current study is to examine the association between several types of physical activity and self-reported physical fitness (e.g., overall physical fitness, cardiorespiratory fitness) in adolescents aged 11–17. It was found that participating in sports and MSE are positively associated with higher levels of self-reported physical fitness indicators in adolescents. However, AC was not found to be associated with any self-reported physical fitness indicators.
A growing body of evidence has confirmed the positive associations between participating in sports and HRPF indicators in children and adolescents. For example, the Physical Activity Health Longitudinal (PAHL) study reported that adolescents who regularly participate in sports had higher levels of physical fitness (field-based assessments) (26). A longitudinal study suggested that those who participate in sports outperformed those who do not when measuring cardiorespiratory fitness (field-based assessments) (39). Participating in sports was also favourably associated with muscular strength (self-reported questionnaire) (40).
This convincing evidence supports the present research findings. It is, therefore, expected that children and adolescents who participate in sport more frequently can increase their PA levels (41), which in turn improves levels of physical fitness indicators. However, compared with some other studies that investigated the context of participating in sports (e.g., in school or out-of-school) (42), the present study failed to categorise the contexts in which participation occurred. This limits the current study to further explore the contextual health promotion effectiveness of participating in sports in children and adolescents. Future studies should fill the research gaps. Regarding the associations between participating in sports and physical fitness indicators (except for muscular strength), a no dose-response association was found, which may go beyond expectations. A possible reason for this may be due to measurement bias resulting from self-reported measures on sports participation and physical fitness indicators. Of note, odds ratios for the association between participating in sports three or more times and physical fitness indicators were larger than other levels of sports participation. This may imply that participating in sports at a specific frequency can help improve physical fitness indicators in children and adolescents.
As an important component of physical activity, MSE has been confirmed to be associated with a variety of health benefits (43, 44), including promoting mental health (45, 46) and physical fitness improvement (47, 48). It is, therefore, suggested that researchers encourage individuals to participate in more MSE. For children and adolescents, engaging in more muscle promoting activity contributes to higher levels of muscular fitness, including muscular strength and endurance (13). This supports the current study findings that MSE is associated with muscular strength. Moreover, evidence has suggested that MSE can increase other physical fitness indicators. Morrow et al. (49) found that adherence to the MSE guideline was more likely to produce greater levels of cardiorespiratory fitness. The present study also provides evidence for supporting previous, well-recognised guidelines that children and adolescents should engage in MSE at least three times a week, as this study is the very first to examine the association between meeting the MSE guidelines and various physical fitness indicators (albeit self-reported). Collectively, promoting MSE in children and adolescents should be a priority for future health promotion initiatives.
In addition to cardiorespiratory fitness and muscle strength, the current study also suggests that participating in sports and muscle-strengthening exercises are positively associated with speed, agility, and flexibility. Currently, there is no evidence concerning the associations between these two types of physical activity with speed, agility, and flexibility, so it is impossible to find comparable evidence. One explanation for the research findings is that participating in sports and muscle-strengthening exercises might make children and adolescents feel fitter, leading them to report higher levels of these two attributes.
Somewhat inconsistently with previous studies (21), the results found that AC was not associated with any self-reported HRPF indicators. Indeed, as AC is associated with higher levels of physical activity, it is likely that AC may lead to greater physical fitness among children and adolescents. A systematic review found that AC was positively associated with cardiorespiratory fitness in children and adolescents (21). In contrast, the present study does not support this review. Also, the current study suggests that AC is not associated with other HRPF indicators. We assumed several possible reasons to interpret why AC is not associated with HRPF indicators, including the lower intensity of AC (e.g., walking) in children and adolescents; and self-reported HRPF is subject to measurement and recalls bias; and that the measurement of AC is not well-validated. For example, in specific, although children and adolescent actively commuted between school and home, its duration and intensity may be restricted, which may not trigger the threshold of increasing children and adolescents' fitness level. Owing to the rare comparable evidence in this study, more observational and intervention studies are needed to explore and further confirm the roles of AC in physical fitness in children and adolescents.
Study limitations and strengths
This study has some limitations inherent in its design, measuring, and participants. First, owing to the study's cross-sectional design, the study could draw no causal conclusions. In other words, the directionality of the association between participating in sports and physical fitness indicators could not be determined. Second, this study employed self-reported measures to collect data on all the variables, which are subject to recall bias and social desirability of the participants. However, it should also be acknowledged that using objective measures would be offering a solution for studies with a large sample size. Third, as this study adopted a convenient and non-probabilistic sampling method, the research findings may be more regionally than nationally replicable. Finally, BMI was not included, which should be mentioned in the current study as a limitation. Given these limitations, future studies are encouraged to generate stronger evidence. Despite these limitations, this study still has some strengths. This study is the first to assess the associations between participating in sports and self-reported physical fitness indicators, which therefore broadens the literature. Also, the sample size in this study was large, so sufficient statistical power was achieved. Finally, this study controlled for many covariates to accurately estimate the association between participating in sports and self-rated physical fitness.
Practical implications
As self-reported physical fitness is recognised as an important marker of health status, a regular assessment or surveillance of self-reported physical fitness should be incorporated into a large health surveillance system.
Encouraging participation in sports and MSE is recommended.
Conclusion
This study offers some evidence concerning the associations between some types of physical activity and self-reported, health-related physical fitness in children and adolescents, highlighting the roles of participating in sports and muscle-strengthening exercises in improving self-reported physical fitness. Future studies should confirm or negate the present research findings.
Data availability statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author.
Ethics statement
The study protocol and procedure were approved by the Institutional Review Board (IRB) of the Shanghai University of Sport with a Grant Number of 102772021RT071. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
CS: writing—original draft. SC and JY: formal analysis. LW, KL, JH, HS, and SC: writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the National Social Science Fund of China (Grant No. 17BTY015).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Haskell WL, Kiernan M. Methodologic issues in measuring physical activity and physical fitness when evaluating the role of dietary supplements for physically active people. Am J Clin Nutr. (2000) 72:541S–50S. 10.1093/ajcn/72.2.541S [DOI] [PubMed] [Google Scholar]
- 2.Chen Z, Chi G, Wang L, Chen S, Yan J, Li S. The combinations of physical activity, screen time, and sleep, and their associations with self-reported physical fitness in children and adolescents. Int J Environ Res Public Health. (2022) 19:5783. 10.3390/ijerph19105783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ortega FB, Ruiz JR, Castillo MJ, Sjöström M. Physical fitness in childhood and adolescence: a powerful marker of health. Int J Obes. (2008) 32:1–11. 10.1038/sj.ijo.0803774 [DOI] [PubMed] [Google Scholar]
- 4.Van Andel GE, Austin DR. Physical fitness and mental health: a review of the literature. Adapt Phys Act Quart. (1984) 1:207–20. [Google Scholar]
- 5.Rauner A, Mess F, Woll A. The relationship between physical activity, physical fitness and overweight in adolescents: a systematic review of studies published in or after 2000. BMC Pediatr. (2013) 13:19. 10.1186/1471-2431-13-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. (1985) 100:126–31. [PMC free article] [PubMed] [Google Scholar]
- 7.Gray C, Gibbons R, Larouche R, Sandseter EBH, Bienenstock A, Brussoni M, et al. What is the relationship between outdoor time and physical activity, sedentary behaviour, and physical fitness in children? A systematic review. Int J Environ Res Public Health. (2015) 12:6455–74. 10.3390/ijerph120606455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Janssen I, LeBlanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. (2010) 7:40. 10.1186/1479-5868-7-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eisenmann JC, Wickel EE, Welk GJ, Blair SN. Relationship between adolescent fitness and fatness and cardiovascular disease risk factors in adulthood: the Aerobics Center Longitudinal Study (ACLS). Am Heart J. (2005) 149:46–53. 10.1016/j.ahj.2004.07.016 [DOI] [PubMed] [Google Scholar]
- 10.Eddolls WTB, McNarry MA, Lester L, Winn CON, Stratton G, Mackintosh KA. The association between physical activity, fitness and body mass index on mental well-being and quality of life in adolescents. Qual Life Res. (2018) 27:2313–20. 10.1007/s11136-018-1915-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bermejo-Cantarero A, Álvarez-Bueno C, Martínez-Vizcaino V, Redondo-Tébar A, Pozuelo-Carrascosa DP, Sánchez-López M. Relationship between both cardiorespiratory and muscular fitness and health-related quality of life in children and adolescents: a systematic review and meta-analysis of observational studies. Health Qual Life Outcomes. (2021) 19:127. 10.1186/s12955-021-01766-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marques A, Santos DA, Hillman CH, Sardinha LB. How does academic achievement relate to cardiorespiratory fitness, self-reported physical activity and objectively reported physical activity: a systematic review in children and adolescents aged 6–18 years. Br J Sports Med. (2018) 52:1039. 10.1136/bjsports-2016-097361 [DOI] [PubMed] [Google Scholar]
- 13.García-Hermoso A, Ramírez-Campillo R, Izquierdo M. Is muscular fitness associated with future health benefits in children and adolescents? A systematic review and meta-analysis of longitudinal studies. Sports Med. (2019) 49:1079–94. 10.1007/s40279-019-01098-6 [DOI] [PubMed] [Google Scholar]
- 14.Lin Y, Yan J. Muscle-strengthening activities and sociodemographic correlates among adults: findings from samples in mainland China. Int J Environ Res Public Health. (2020) 17:2266. 10.3390/ijerph17072266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fühner T, Kliegl R, Arntz F, Kriemler S, Granacher U. An update on secular trends in physical fitness of children and adolescents from 1972 to 2015: a systematic review. Sports Med. (2021) 51:303–20. 10.1007/s40279-020-01373-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haskell WL, Montoye HJ, Orenstein D. Physical activity and exercise to achieve health-related physical fitness components. Public Health Rep. (1985) 100:202. [PMC free article] [PubMed] [Google Scholar]
- 17.Vanhees L, De Sutter J, Geladas N, Doyle F, Prescott E, Cornelissen V, et al. Importance of characteristics and modalities of physical activity and exercise in defining the benefits to cardiovascular health within the general population: recommendations from the EACPR (Part I). Eur J Prev Cardiol. (2012) 19:670–86. 10.1177/2047487312437059 [DOI] [PubMed] [Google Scholar]
- 18.Aubert S, Barnes JD, Abdeta C, Abi Nader P, Adeniyi AF, Aguilar-Farias N, et al. Global matrix 30 physical activity report card grades for children and youth: results and analysis from 49 countries. J Phys Act Health. (2018) 15:S251–73. 10.1123/jpah.2018-0472 [DOI] [PubMed] [Google Scholar]
- 19.Huang C, Memon AR, Yan J, Lin Y, Chen S-T. The associations of active travel to school with physical activity and screen time among adolescents: do individual and parental characteristics matter? Front Public Health. (2021) 9:719742. 10.3389/fpubh.2021.719742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chaput J-P, Willumsen J, Bull F, Chou R, Ekelund U, Firth J, et al. WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: summary of the evidence. Int J Behav Nutr Phys Act. (2020) 17:141. 10.1186/s12966-020-01037-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lubans DR, Boreham CA, Kelly P, Foster CE. The relationship between active travel to school and health-related fitness in children and adolescents: a systematic review. Int J Behav Nutr Phys Act. (2011) 8:5. 10.1186/1479-5868-8-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Larouche R, Saunders TJ, John Faulkner GE, Colley R, Tremblay M. Associations between active school transport and physical activity, body composition, and cardiovascular fitness: a systematic review of 68 studies. J Phys Activity Health. (2014) 11:206–27. 10.1123/jpah.2011-0345 [DOI] [PubMed] [Google Scholar]
- 23.Henriques-Neto D, Peralta M, Garradas S, Pelegrini A, Pinto AA, Sánchez-Miguel PA, et al. Active commuting and physical fitness: a systematic review. Int J Environ Res Public Health. (2020) 17:2721. 10.3390/ijerph17082721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ren T, Yan J, Sun Q. Sociodemographic correlates of organized sports participation in a sample of middle school students in China. Front Public Health. (2021) 9:730555. 10.3389/fpubh.2021.730555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen S, Li X, Yan J, Ren Z. To be a sportsman? Sport participation is associated with optimal academic achievement in a nationally representative sample of high school students. Front Public Health. (2021) 9:730497. 10.3389/fpubh.2021.730497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Agata K, Monyeki MA. Association between sport participation, body composition, physical fitness, and social correlates among adolescents: the PAHL study. Int J Environ Res Public Health. (2018) 15:2793. 10.3390/ijerph15122793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen S-T, Guo T, Yu Q, Stubbs B, Clark C, Zhang Z, et al. Active school travel is associated with fewer suicide attempts among adolescents from low-and middle-income countries. Int J Clin Health Psychol. (2021) 21:100202. 10.1016/j.ijchp.2020.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gu J, Chen S-T. Association between active travel to school and depressive symptoms among early adolescents. Children. (2020) 7:41. 10.3390/children7050041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith JJ, Eather N, Weaver RG, Riley N, Beets MW, Lubans DR. Behavioral correlates of muscular fitness in children and adolescents: a systematic review. Sports Med. (2019) 49:887–904. 10.1007/s40279-019-01089-7 [DOI] [PubMed] [Google Scholar]
- 30.Ortega FB, Ruiz JR, España-Romero V, Vicente-Rodriguez G, Martínez-Gómez D, Manios Y, et al. The International Fitness Scale (IFIS): usefulness of self-reported fitness in youth. Int J Epidemiol. (2011) 40:701–11. 10.1093/ije/dyr039 [DOI] [PubMed] [Google Scholar]
- 31.Español-Moya MN, Ramírez-Vélez R. Psychometric validation of the International FItness Scale (IFIS) in Colombian youth. Rev Esp Salud Publica. (2014) 88:271–8. 10.4321/S1135-57272014000200009 [DOI] [PubMed] [Google Scholar]
- 32.Sánchez-López M, Martínez-Vizcaíno V, García-Hermoso A, Jiménez-Pavón D, Ortega FB. Construct validity and test–retest reliability of the International Fitness Scale (IFIS) in Spanish children aged 9–12 years. Scand J Med Sci Sports. (2015) 25:543–51. 10.1111/sms.12267 [DOI] [PubMed] [Google Scholar]
- 33.Howie EK, Guagliano JM, Milton K, Vella SA, Gomersall SR, Kolbe-Alexander TL, et al. Ten research priorities related to youth sport, physical activity, and health. J Phys Activity Health. (2020) 17:920–9. 10.1123/jpah.2020-0151 [DOI] [Google Scholar]
- 34.Xin F, Zhu Z, Chen S, Chen H, Hu X, Ma X, et al. Prevalence and correlates of meeting the muscle-strengthening exercise recommendations among Chinese children and adolescents: results from 2019 Physical Activity and Fitness in China—the youth study. J Sport Health Sci. (2022) 11:358–6. 10.1016/j.jshs.2021.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bao R, Chen S, Kastelic K, Drenowatz C, Li M, Zhang J, et al. Reliability of international fitness scale (IFIS) in Chinese children and adolescents. Children. (2022) 9:531. 10.3390/children9040531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu Y, Wang M, Tynjälä J, Lv Y, Villberg J, Zhang Z, et al. Test-retest reliability of selected items of Health Behaviour in School-aged Children (HBSC) survey questionnaire in Beijing, China. BMC Med Res Methodol. (2010) 10:1–9. 10.1186/1471-2288-10-73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tremblay MS, Carson V, Chaput J-P, Gorber SC, Dinh T, Duggan M, et al. Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metabol. (2016) 41(6 Suppl. 3):S311–27. 10.1139/apnm-2016-0151 [DOI] [PubMed] [Google Scholar]
- 38.Tremblay MS, Carson V, Chaput J-P. Introduction to the Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metabol. (2016) 41(6 Suppl. 3):iii–iv. 10.1139/apnm-2016-0203 [DOI] [PubMed] [Google Scholar]
- 39.Telford RM, Telford RD, Cochrane T, Cunningham RB, Olive LS, Davey R. The influence of sport club participation on physical activity, fitness and body fat during childhood and adolescence: the LOOK longitudinal study. J Sci Med Sport. (2016) 19:400–6. 10.1016/j.jsams.2015.04.008 [DOI] [PubMed] [Google Scholar]
- 40.Loprinzi PD, Cardinal BJ, Cardinal MK, Corbin CB. Physical education and sport: does participation relate to physical activity patterns, observed fitness, and personal attitudes and beliefs? Am J Health Promot. (2018) 32:613–20. 10.1177/0890117117698088 [DOI] [PubMed] [Google Scholar]
- 41.Hulteen RM, Smith JJ, Morgan PJ, Barnett LM, Hallal PC, Colyvas K, et al. Global participation in sport and leisure-time physical activities: a systematic review and meta-analysis. Prevent Med. (2017) 95:14–25. 10.1016/j.ypmed.2016.11.027 [DOI] [PubMed] [Google Scholar]
- 42.Silva G, Andersen LB, Aires L, Mota J, Oliveira J, Ribeiro JC. Associations between sports participation, levels of moderate to vigorous physical activity and cardiorespiratory fitness in children and adolescents. J Sports Sci. (2013) 31:1359–67. 10.1080/02640414.2013.781666 [DOI] [PubMed] [Google Scholar]
- 43.Bennie JA, Shakespear-Druery J, De Cocker K. Muscle-strengthening exercise epidemiology: a new frontier in chronic disease prevention. Sports Med Open. (2020) 6:40. 10.1186/s40798-020-00271-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bennie J, Smith J, Marvos Y, Biddle S, Kolbe-Alexander T. The neglected guideline: resistance exercise and public health. J Sci Med Sport. (2019) 22:S9. 10.1016/j.jsams.2019.08.051 [DOI] [Google Scholar]
- 45.Bennie JA, De Cocker K, Biddle SJH, Teychenne MJ. Joint and dose-dependent associations between aerobic and muscle-strengthening activity with depression: a cross-sectional study of 1.48 million adults between 2011 and 2017. Depress Anxiety. (2020) 37:166–78. 10.1002/da.22986 [DOI] [PubMed] [Google Scholar]
- 46.Bennie JA, Ding D, De Cocker K. Dose-dependent associations of joint aerobic and muscle-strengthening exercise with obesity: a cross-sectional study of 280,605 adults. J Sport Health Sci. (2021). 10.1016/j.jshs.2021.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bennie JA, De Cocker K, Pavey T, Stamatakis E, Biddle SJH, Ding D. Muscle strengthening, aerobic exercise, and obesity: a pooled analysis of 17 million US adults. Obesity. (2020) 28:371–8. 10.1002/oby.22673 [DOI] [PubMed] [Google Scholar]
- 48.Bennie JA, Ding D, Khan A, Stamatakis E, Biddle SJ, Kim J. Run, lift, or both? Associations between concurrent aerobic–muscle strengthening exercise with adverse cardiometabolic biomarkers among Korean adults. Eur J Prevent Cardiol. (2020) 27:738–48. 10.1177/2047487318817899 [DOI] [PubMed] [Google Scholar]
- 49.Morrow JR, Tucker JS, Jackson AW, Martin SB, Greenleaf CA, Petrie TA. Meeting physical activity guidelines and health-related fitness in youth. Am J Prev Med. (2013) 44:439–44. 10.1016/j.amepre.2013.01.008 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author.