Abstract
In some instances, unsuppressed HIV has been associated with severe COVID-19 disease, but the mechanisms underpinning this susceptibility are still unclear. Here, we assessed the impact of HIV infection on the quality and epitope specificity of SARS-CoV-2 T cell responses in the first wave and second wave of the COVID-19 epidemic in South Africa. Flow cytometry was used to measure T cell responses following peripheral blood mononuclear cell stimulation with SARS-CoV-2 peptide pools. Culture expansion was used to determine T cell immunodominance hierarchies and to assess potential SARS-CoV-2 escape from T cell recognition. HIV-seronegative individuals had significantly greater CD4+ T cell responses against the Spike protein compared to the viremic people living with HIV (PLWH). Absolute CD4 count correlated positively with SARS-CoV-2-specific CD4+ and CD8+ T cell responses (CD4 r=0.5, p=0.03; CD8 r=0.5, p=0.001), whereas T cell activation was negatively correlated with CD4+ T cell responses (CD4 r=−0.7, p=0.04). There was diminished T cell cross-recognition between the two waves, which was more pronounced in individuals with unsuppressed HIV infection. Importantly, we identify four mutations in the Beta variant that resulted in abrogation of T cell recognition. Taken together, we show that unsuppressed HIV infection markedly impairs T cell responses to SARS-Cov-2 infection and diminishes T cell cross-recognition. These findings may partly explain the increased susceptibility of PLWH to severe COVID-19 and also highlights their vulnerability to emerging SARS-CoV-2 variants of concern.
Research organism: Human
Introduction
Despite measures to contain the spread of SARS-CoV-2 infection, the pandemic is persisting, with a devastating impact on healthcare systems and the world economy (Verma et al., 2021). The research community rapidly mobilized and developed vaccines and therapeutics at unprecedented speed (Polack et al., 2020; Ball, 2021). COVID-19 vaccines have prevented serious illness and death and have in some cases interrupted chains of transmission at community level (Kampf, 2021). However, the COVID-19 pandemic remains a major concern in Africa due to dismal vaccine coverage (WHO, 2021a) and the emergence of variants of concern that may be more transmissible, cause more severe illness, or have the potential to evade immunity from prior infection or vaccination (Shinde et al., 2021).
The interaction of HIV-1 infection, common in sub-Saharan Africa (H. The Lancet, 2020), with COVID-19 remains understudied. Initial small studies reported that people living with HIV (PLWH) had similar or better COVID-19 outcomes (Calza et al., 2020; Lee et al., 2021). Larger epidemiological studies have demonstrated increased hospitalization and higher rates of COVID-19-related deaths among PLWH compared with HIV-negative individuals (Davies, 2020a; Geretti et al., 2020; Bhaskaran et al., 2021; Vizcarra et al., 2020). Other studies have linked HIV-mediated CD4+ T cell depletion to suboptimal T cell and humoral immune responses to SARS-CoV-2 (Riou, 2021). A recent study showed prolonged shedding of high titer SARS-CoV-2 and emergence of multiple mutations in an individual with advanced HIV and antiretroviral treatment (ART) failure (Karim et al., 2021b).
Although B cells have repeatedly been shown to play a pivotal role in immune protection against SARS-CoV-2 infection and antibody responses and are typically used to evaluate immune responses to currently licensed COVID-19 vaccines (Sahin et al., 2020; Khoury et al., 2021), mounting evidence suggest that T cell responses are equally important. For instance, strong SARS-CoV-2-specific T cell responses are associated with milder disease (Riou, 2021; Sette and Crotty, 2021; Liao et al., 2020; Schub et al., 2020; Rydyznski Moderbacher et al., 2020). Moreover, T cell responses can confer protection even in the absence of humoral responses, given that patients with inherited B cell deficiencies or hematological malignancies are able to fully recover from SARS-CoV-2 infection (Bange et al., 2021). In some instances, COVID-19 disease severity has been attributed to poor SARS-CoV-2-specific CD4+ T cell polyfunctionality potential, reduced proliferation capacity, and enhanced HLA-DR expression (Riou, 2021). Importantly, a recent study identified nonsynonymous mutations in known MHC-1-restricted CD8+ T cell epitopes following deep sequencing of SARS-CoV-2 viral isolates from patients, demonstrating the capacity of SARS-CoV-2 to escape from CTL recognition (Agerer et al., 2021). Regarding vaccine-induced T cell responses, it was recently shown that mRNA vaccines can stimulate Th1 and Th2 CD4+ T cell responses that correlate with post-boost CD8+ T cell responses and neutralizing antibodies (Painter et al., 2021). The cited examples, herein, highlight the need to gain more insight into T cell-mediated protection against COVID-19 (Altmann and Boyton, 2020).
This study used a cohort of PLWH and HIV-seronegative individuals diagnosed with COVID-19 during the first wave dominated by the wild-type (wt) D614G virus (Tegally et al., 2021c), and the second wave dominated by the Beta variant. Peripheral blood mononuclear cells (PBMCs) were used to determine the impact of HIV infection on SARS-CoV-2-specific T cell responses and to assess T cell cross-recognition. Our data showed impaired SARS-CoV-2-specific T cell responses in individuals with unsuppressed HIV infection and highlighted poor cellular cross-recognition between variants, which was more pronounced than those with unsuppressed HIV. The muted responses in unsuppressed HIV infection may be attributable to low absolute CD4 count and immune activation. Importantly, we identified mutations in the Beta variant that could potentially reduce T cell recognition. Taken together, these data highlight the need to ensure uninterrupted access to ART for PLWH during the COVID-19 pandemic.
Results
Study participants were drawn from a longitudinal observational cohort study that enrolled and tracked patients with a positive COVID-19 qPCR test presenting at three hospitals in the greater Durban area. Study participants were recruited into this study based on HIV status and sample availability. They include 25 participants recruited during the first wave (wt) of the pandemic in KwaZulu-Natal from June to December 2020 (Karim et al., 2021a). Twenty-three second wave (Beta variant) participants were recruited from January to June 2021. All study participants were unvaccinated because the COVID-19 vaccine was not readily available in South Africa at the time. Study participants were stratified into three groups, namely HIV-seronegative (HIV-neg), people living with HIV (PLWH) with viral load below 50 copies/ml, here termed (suppressed), and PLWH with detectable viral load of ≥1000 copies/ml (viremic). Study participants included HIV-seronegative (HIV-neg) (n=17). PLWHs (n=31) were subdivided into suppressed (n=17) and viremic (n=14). The male-to-female ratio and age distribution were comparable between PLWH and HIV-seronegative groups (Table 1). The median CD4 count for PLWH (suppressed 661 and viremic 301) (p=0.0002, Table 1). Study participants had predominantly mild COVID-19 disease that did not require supplemental oxygen or ventilation (Table 1).
Table 1. Donor characteristics stratified by HIV status.
| All (n=48) | HIV-neg (N=17) | HIV+suppressed (n=17) | HIV+viremics (N=14) | Statistics | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age years, median (IQR) | 40.5 (30–51.75) | 45 (27–53.5) | 45 (39.5–54) | 31.5 (26.5–42) | 0.036* (KW) |
| Male sex, n (%) | 14 (29.16) | 8 (47.05) | 3 (17.64) | 3 (21.42) | 0.2 (0.82–10) (F) |
| HIV-associated parameters | |||||
| HIV viral load copies/ml |
19,969 (2335–43,568) | ||||
| CD4 cells/µl median (IQR) | 661 (398.5–836.5) | 834.5 (739.3–1029) | 661 (494–789.5) | 301 (113.8–568) | 0.0002** (KW) |
| Disease severity | |||||
| Asymptomatic, n (%) | 9 (18.75) | 4 (23.52) | 3 (17.64) | 2 (14.28) | 0.6 (0.32–9.53) (F) |
| Mild | 29 (60.42) | 12 (70.59) | 10 (58.82) | 7 (50) | 0.01* (0.13–0.84) (F) |
| Severe/oxygen supplementation | 8 (16.67) | 1 (5.88) | 4 (23.52) | 3 (21–42) | 0.33 (0.48–49.67) (F) |
| Death, n (%) | 1 (2.1) | 0 | 0 | 1 (7.1) | 0.46 (F) |
P values calculated by Kruskal-Wallis test for unpaired three groups (KW) or Fischer’s exact test (F).
Unsuppressed HIV infection is associated with altered SARS-CoV-2-specific CD4+ and CD8+ T cell responses
Immunity to SARS-CoV-2 typically induces robust T cell responses, but the impact of HIV infection on these responses has not been fully elucidated (Bange et al., 2021; Riou et al., 2021; Grifoni et al., 2020). Thus, we sought to determine the impact of HIV infection on SARS-CoV-2-specific CD4+ and CD8+ T cell responses. PBMCs were stimulated with PepTivater 15 mer megapools purchased from Miltenyi Biotec. The pools contained predicted CD4 and CD8 epitopes spanning the entire Spike coding sequence (aa5-1273). Intracellular cytokine staining of peptide-stimulated PBMCs was followed by flowcytometric analyses described in the Materials and methods section. The samples used for these analyses were collected between 2 and 4 weeks after COVID-19 PCR positive diagnosis. The time points were selected based on longitudinal T cell analysis that showed SARS-CoV-2-specific T cell responses peaked between 14 and 30 days after PCR positive diagnosis (data not shown), consistent with other studies (Keeton et al., 2021; Keeton et al., 2022). Representative flow plots for each group and aggregate data show viremic PLWH had significantly lower frequencies of SARS-CoV-2-specific IFN-γ/TNF-α-producing CD4+ T cells compared to suppressed PLWH (p=0.002) and HIV-seronegative individuals (p=0.0006) (Figure 1B). There was no significant difference in SARS-CoV-2-specific IFN-γ/TNF-α-producing CD8+ T cells among the groups (Figure 1B), and no significant differences in SARS-CoV-2-specific CD4+ or CD8+ T cell frequencies were observed between the suppressed PLWH and HIV-seronegative individuals (Figure 1B).
Figure 1. The impact of unsuppressed HIV infection on SARS-CoV-2-specific CD4+ and CD8+ T cell responses.
(A) Representative flowplots gated on IFN-γ/TNF-α dual positive CD4+ and CD8+ T cells. (B) Aggregate data for IFN-γ/TNF-α dual positive CD4+ and CD8+ T cells are shown (HIV-neg, n=14; suppressed, n=16: viremic, n=13). SARS-CoV-2-specific CD4+ and CD8+ T cells producing IFN-γ, TNF-α, and IL-2 cells in various combinations are shown. Pie chart and dot plots for (C) SARS-CoV-2-specific CD4+ and (D) CD8+ T cells. Pie chart represents the mean distribution across subjects of mono-functional, bi-functional, and poly-functional cytokine producing SARS-CoV-2-specific T cells. Size of each pie segment relates to the frequency of a mono-functional, bi-functional, and triple-functional response. Dot plot represents the frequency of combinations of cytokines produced. Wilcoxon test was done among the dot plots using SPICE software (significant p values are highlighted).
Simultaneous production of cytokines, commonly referred to as polyfunctionality, which is regarded as a measure of the quality of the T cell response, has been shown to correlate with viral control (Betts et al., 2006). Thus, we evaluated the quality of the CD4+ and CD8+ T cell responses among the groups by enumerating cells producing three (IFN-γ, TNF-α, and IL-2) cytokines in various combinations. Consistent with dual IFN-γ, TNF-α cytokine secretion data (Figure 1B), the patterns of cytokine production of HIV-seronegative was mostly similar to HIV suppressed individuals (pie charts, Figure 1C and D). Analysis of single cytokine production revealed that HIV-seronegative individuals and suppressed PLWH predominantly produced IFN-γ responses (green sectors of the pie chart, Figure 1C and D), whereas viremic PLWH predominantly produced TNF-α responses for both CD4+ and CD8+ T cells (magenta sectors of the pie chart, Figure 1C and D). Cells co-producing all three cytokines were very rare regardless of HIV status (red sectors of the pie chart, Figure 1C and D). Nonetheless, HIV-seronegative had greater frequencies of dual cytokine secreting cells compared to viremic PLWH (p=0.0330 for CD4, Figure 1C; p=0.0330 for CD8, Figure 1D). Taken together, the data show that uncontrolled HIV infection lowers the magnitude and alters the quality of SARS-CoV-2 T cell responses. Importantly, complete plasma HIV suppression preserves the capacity to mount high magnitude, dual-functional SARS-CoV-2-specific T cell responses.
T cell responses against the major SARS-CoV-2 structural proteins
Having observed differences in magnitude and quality of SARS-CoV-2 spike-specific T responses, we next measured responses directed against major structural proteins, the nucleocapsid (N), the membrane (M), and Spike (S), again using PepTivater peptide pools from Miltenyi biotec. Our data show all three major SARS-CoV-2 proteins are targeted by SARS-CoV-2-specific CD4+ and CD8+ T cells (Figure 2A and B), with a preponderance for greater S-specific CD8+ T cell responses relative to M (Figure 2A). These data suggest that most SARS-CoV-2 structural proteins can be targeted by T cells, consistent with previous reports (Tarke et al., 2021).
Figure 2. Comparison of SARS-CoV-2 protein targeting by T cell responses among HIV-negatives, suppressed and viremic donors.
Magnitude of (A) CD4+ T and (B) CD8+ T cell responses targeting the Membrane (M), Nucleocapsid (N), and Spike (S) SARS-CoV-2 proteins among study groups. P values for differences among the groups are *<0.05; as determined by the Wilcoxon matched-pairs signed rank test (GraphPad Prism version 9.3.0).
Uncontrolled HIV infection abrogates SARS-CoV-2 T cell cross-recognition between wild-type D614G and Beta variant
To evaluate the impact of uncontrolled HIV infection on cross-reactive T cell responses between wt and the Beta variant, we compared the breadth of responses and the ability to cross-recognize SARS-CoV-2 Beta variant peptides among the three study groups. These studies were conducted using two sets of 15 mer overlapping peptides (OLPs). Set 1 was comprised of 16 wt peptides, spanning the receptor-binding domain (RBD) and non-RBD regions of spike (S) that are known hotspots for mutations (Tegally et al., 2021c). Set 2 consisted of corresponding peptides that included all the major mutations that define the Beta variant lineage (Wibmer et al., 2021). A detailed description of the peptides is contained in Supplementary file 1.
We first sought to determine cross-reactivity of SARS-CoV-2-specific CD4+ and CD8+ T cells induced following infection with the wt (D614G, wave 1) and Beta variant (wave 2), between each other. We found that wave 1 donors had significantly lower CD8+ (p=0.0312) and CD4+ T cell responses (p=0.0078) to Beta variant relative to corresponding wt responses (Figure 3A). Wave 2 donors had no significant differences in T cells responses to Beta and wt (Figure 3B). Using a 12-day cultured stimulation assay, we were able to massively expand the magnitude of SARS-CoV-2-specific CD4+ and CD8+ T cells (Figure 3C) and (Figure 3—figure supplement 1), and this allowed us to hone in on single peptide responses (Table 1). Representative data for a wave 1 donor shows three CD8+ and two CD4+ wt responses (red circles), that did not cross-recognize corresponding Beta variants (blue bars) (Figure 3D). Contrariwise, a representative wave 2 donor had one CD8+ and one CD4+T cell response to the Beta variant that did not cross-react to the wt version of the peptide (Figure 3E). Intra-donor comparison revealed significantly more CD8+ (p=0.0156) and CD4+ T cell responses (p=0.0312) to wt peptides compared to the corresponding Beta variant peptides in wave 1 donors (Figure 3F). Conversely, unlike the ex vivo data (Figure 3B), wave 2 donors had significantly more CD8+ T cell responses to Beta variant peptides relative to wt peptides (p=0.0312), and a trend toward increased CD4+ T cells against Beta peptides (p=0.0625), highlighting the increased sensitivity of expanded cells (Figure 3G). Taken together, these data show poor cross-recognition of wt and Beta variant epitopes.
Figure 3. Poor cross-recognition of SARS-CoV-2-specific CD4+ and CD8+ T cell responses between wt and beta variants in wave 1 and wave 2 COVID-19 participants.
Ex vivo assessment of T cell cross-recognition between the two waves. (A) Intra-donor SARS-CoV-2-specific T cell responses to wt and corresponding Beta variant peptides by wave 1 participants. (B) Intra-donor SARS-CoV-2-specific T cell responses to wt and corresponding Beta variant peptides in wave 2 participants. Next, PBMCs were expanded for 12 days in the presence of S1S2 SARS-CoV-2 peptide pools and tested against wt and corresponding Beta variants at single peptide level. (C) Representative flow plots showing the frequency of SARS-CoV-2-specific CD4+ and CD8+ T cells before and after cultured expansion. (D) T cell responses to single wt (red bars) and corresponding Beta (blue bars) peptide stimulation for a representative donor from wave 1. (E) T cell responses to single wt and corresponding Beta peptide stimulation for a representative donor from wave 2 (positive responses are circled). A response was deemed positive if ≥1% or higher. (F) Number of expanded wt and corresponding Beta responses for each wave 1 donor. (G) Number of expanded wt and corresponding Beta responses for each wave 2 donor. P values calculated using Wilcoxin matched-pairs signed rank T test. PBMC, peripheral blood mononuclear cell; wt, wild-type.
Figure 3—figure supplement 1. Cross-recognition of SARS-CoV-2 CD4+ T cell responses between wt and Beta variants in wave 1 and wave 2 COVID-19 donors: PBMCs were expanded for 12 days in the presence of S1S2 SARS-CoV-2 peptide pools.
We then assessed the impact of HIV infection on cross-recognition of wt and Beta variant epitopes. Representative data for an HIV-seronegative individual from the first wave had six wt and five Beta variant CD8+ T cell responses, one was cross-recognized (circled) (Figure 4A). The same individual had five wt and five Beta variant CD4+ T responses, one was cross-recognized (Figure 4B). Similarly, a representative suppressed wave 1 donor had five wt and two Beta variant CD8+ T cell responses, one of which was cross-recognized (Figure 4C). This same donor had six wt and zero Beta variant CD4+ T cell responses (Figure 4D). A representative viremic individual had four weak wt CD8+ T cell responses and three borderline CD4 responses, none of which were cross-recognized (Figure 4E and F). Summary data showed viremic PLWH had significantly narrow breadth of SARS-CoV-2-specific CD8+ (p=0.039) and CD4+ T cell responses (p=0.033) compared to suppressed PLWH and HIV-seronegative individuals (Figure 4G and H). Collectively, these data show that SARS-CoV-2-specific T cell responses in viremic PLWH have limited breadth and subsequently poor cross-recognition potential.
Figure 4. The effects of unsuppressed HIV infection on T cell breadth and ability to cross-recognize the Beta variant.
Representative data for a negative donor showing greater, (A) CD8+ and (B) CD4+ T cell breadth. A cross-recognized responses between wt and Beta is circled. Representative data for a suppressed donor showing greater, (C) CD8+ and (D) CD4+ T cell breadth. A cross-recognized response is circled. Representative data for a viremic donor showing greater, (E) CD8+ and (F) CD4+ T cell breadth. (G) Aggregate data comparing breath of SARS-CoV-2-specific CD8+, and (H) CD4+ T cell response between HIV-negative and suppressed versus viremics. Breadth here is simply the number of positive responses among the individual peptides tested.
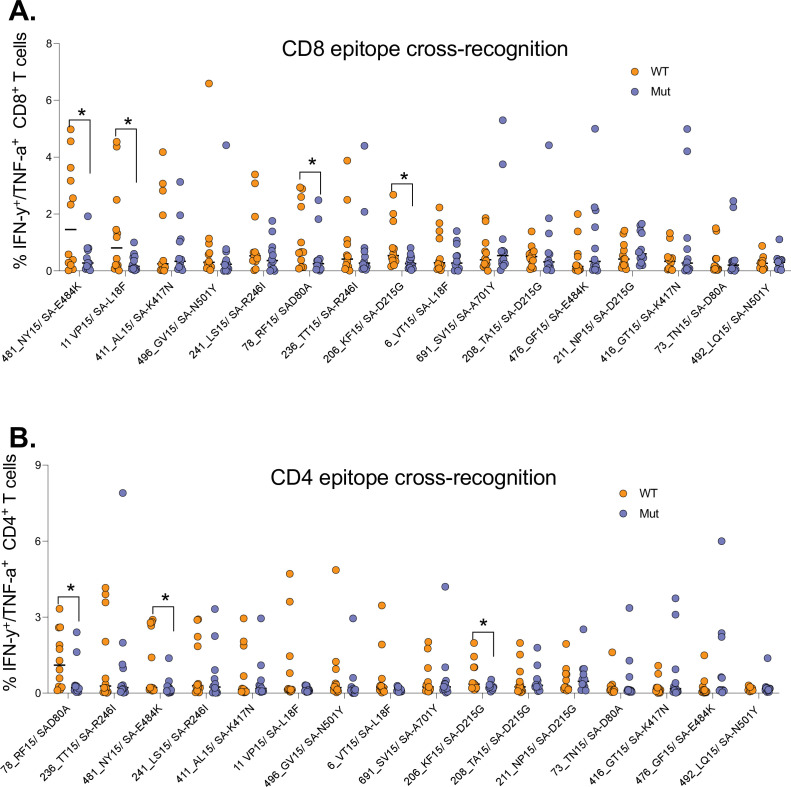
Identification of mutations in the Beta variant that are associated with reduced cross-recognition
Having shown poor T cell cross-recognition of SARS-CoV-2 epitopes between wt and Beta variant, we next sought to identify mutations that might be responsible for the loss of recognition. We combined all the T cell data for the 12 (4 HIV-negatives, 4 HIV-suppressed, and 4 HIV-viremics) donors used for cultured epitope screening studies. All the samples were culturally expanded using wt peptides from the first wave. This analysis identified four Beta variant peptides (listed in Supplementary file 1) that had significant reduction in CD8+ T cell recognition relative to wt peptides (Figure 5A). Three of these peptides were also poorly recognized by CD4+ T cells (Figure 5B). The amino acid sequences for wt and corresponding mutations include the E484K mutation, a key Beta variant spike residual change also associated with loss antibody binding (Wibmer et al., 2021). Taken together, these data identified mutations in the Beta variant that may abrogate T cell recognition, suggesting that they may be potential T cell escape mutations and warrant further investigation.
Figure 5. Identification of Beta mutations associated with reduced cross-recognition between wt and Beta variant.
(A) Side-by-side comparison of SARS-CoV-2-specific CD8+ T cell response between wt and Beta. (B) Side-by-side comparison of SARS-CoV-2-specific CD4+ T cell response between wt. The analysis combined all the 12 participants. P values calculated by Mann-Whitney U-test. wt, wild-type.
Immunodominance hierarchy of SARS-CoV-2 CD8+ and CD4+ T cell responses targeting the spike protein
Virus-specific CD8+ and CD4+ T cells typically target viral epitopes in a distinct hierarchical order (Streeck et al., 2009; Laher et al., 2017). Identifying SARS-CoV-2 epitopes that are most frequently targeted by T cells is important for the design of vaccines that can induce protective T cell responses. To determine the immunodominance hierarchy of SAR-CoV-2 specific T cell responses targeting the spike protein, OLPs were ranked based on magnitude and frequency of recognition. This analysis revealed the most immunodominant wt peptides targeted by CD8+ T cell responses (Figure 6A). The Beta variant resulted in dramatic shift in the immunodominance hierarchy whereby, three of five most dominant wt CD8+ T cell responses (Figure 6A), their Beta variant versions were subdominant (downward arrows) (Figure 6B). Contrariwise, three subdominant wt responses were among the most dominant Beta variant responses (upward arrows) (Figure 6B). A similar trend was observed for CD4+ T cell responses (Figure 6C and D). These data demonstrated a shift in the immunodominant hierarchy between wt and Beta variant responses, which partly explains poor T cell cross-recognition between successive SARS-CoV-2 variants.
Figure 6. Immunodominance hierarchy of SARS-CoV-2 CD8+ and CD4+ T cell responses targeting wt and Beta.
Immunodominance hierarchy of CD8+ T cell responses to, (A) wt and (B) the corresponding Beta variant peptides. Similarly, Immunodominance hierarchy of CD4+ T cell responses to, (C) wt and (D) the corresponding Beta variant. Arrows indicate responses that changed hierarchical position (among the six most dominant responses) between the two waves. Data arranged in descending order of magnitude of responses to wt peptide stimulation. wt, wild-type.
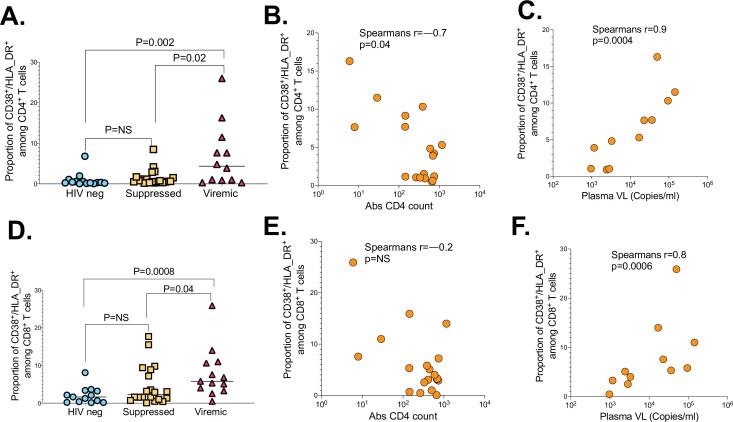
The impact of HIV markers of diseases progression on SARS-CoV-2-specific T cell responses
To gain more insight into why viremic PLWH responded poorly to SARS-CoV-2 infection, we investigated if T cell activation defined here as co-expression of CD38 and HLA-DR, absolute CD4 count and plasma viral load, impacted immune responses (Du et al., 2009). The proportion of activated (CD38/HLA-DR) CD4+ T cells was higher in viremic PLWH compared to suppressed (p=0.02) and HIV-seronegative individuals (p=0.002; Figure 7A). Moreover, proportion of activated (CD38/HLA-DR) CD4+ T cells among viremic PLWH negatively correlated with absolute CD4 counts (r=–0.7, p=0.04; Figure 7B), and positively correlated with HIV plasma viral loads (r=0.9, p=0.0004; Figure 7C). Similarly, proportion of activated (CD38/HLA-DR) CD8+ T cells were significantly higher in viremic PLWH relative to suppressed PLWH (p=0.04) and HIV-seronegative individuals (p=0.0008; Figure 7D). The negative relationship between proportion of activated (CD38/HLA-DR) CD8+ T cells and CD4 counts did not reach statistical significance (Figure 7E), but proportion of activated (CD38/HLA-DR) CD8+ T cells were positively correlated with HIV plasma viral loads among viremic PLWH (r=0.8, p=0.0006; Figure 7F).
Figure 7. The impact of HIV markers of diseases progression on SARS-CoV-2 T cell immunity.
(A) CD4+ T cell activation graphed based on the frequency of CD38/HLA-DR co-expressing cells. (B) Correlation between CD4+ T cell activation and absolute CD4 counts of viremic PLWH. (C) Correlation between CD4+ T cell activation and HIV plasma viral load of viremic PLWH. (D) CD8+ T cell activation measured by CD38/HLA-DR. (E) Correlation between CD8+ T cell activation and absolute CD4 counts of viremic PLWH. (F) Correlation between CD8+ T cell activation and HIV plasma viral load of viremic PLWH. P values calculated by Mann-Whitney U-test and Pearson correlation test. PLWH, people living with HIV.
Figure 7—figure supplement 1. Assessment of the effect of COVID-19 disease severity on, (A) SARS-CoV-2-specific CD4+, and (B) CD8+ T cell responses.
Taken together, these data suggest that hyper immune activation driven by uncontrolled HIV infection impacts CD4+ and CD8+ T cell responses.
Finally, we interrogated the relationship between SARS-CoV-2-specific responses and disease severity, stratified into asymptomatic, mild, and severe diseases requiring oxygen supplementation, as previously defined (Karim et al., 2021a). We found no significant differences between the magnitude of CD4+ or CD8+ T cell responses and disease severity among the groups (Figure 7—figure supplement 1A,B). We next, examined sex differences and found no difference in CD4+ and CD8+T cell responses to SARS-CoV-2 infection (Figure 7—figure supplement 1C,D). Age is a risk factor for severe COVID-19 (WHO, 2021a); thus, we examined the relationship between age and T cell responses. There was a negative relationship between age and magnitude of CD8+ T cell responses (CD8 r=−0.6, p=0.002) (Figure 7—figure supplement 1E), and a similar trend for CD4+ T cell responses (CD4 r=−0.3, P=0.15) (Figure 7—figure supplement 1F). These data show that younger people had greater responses compared to older people, whereas disease severity and sex did not have discernible effect on SARS-CoV-2 T cell responses.
Discussion
The greater burden of HIV in sub-Saharan Africa makes investigating the impact of HIV infection on COVID-19 immunity and disease outcomes critical for bringing the epidemic under control in the region. Recent studies have documented strong cellular responses following SARS-CoV-2 infection and vaccination, but the effects of HIV on SARS-CoV-2-specific T cell responses are not well characterized. Here, we investigated the antigen-specific CD4+ and CD8+ T cell responses in a cohort of SARS-CoV-2- infected individuals with and without HIV infection. Our results show that unsuppressed HIV infection is associated with reduced cellular responses to SARS-CoV-2 infection. We also show that low absolute CD4 count and hyper immune activation are associated with diminution of SARS-CoV-2-specific T cell responses. Importantly, we identify spike mutations in the Beta variant that abrogate recognition by memory T cells raised against wt epitopes. Similarly, immune responses targeting Beta variant epitopes poorly cross-recognize corresponding wt epitopes. These data reveal the potential for emerging SARS-CoV-2 variants to escape T cell recognition. Importantly, our data highlight the potential for unsuppressed HIV infection to attenuate vaccine-induced T cell immunity.
HIV-induced immune dysregulation is well documented (Klatt et al., 2013). Unsuppressed HIV infection is associated with profound dysfunction of virus-specific T cell immunity partly caused by immune activation (Klatt et al., 2013; Ndhlovu et al., 2015). Recent studies have reported strong association between unsuppressed HIV infection and poor COVID disease outcomes, for instance, a large cross-section study found a link between severe HIV disease and poor COVID-19 outcomes including COVID-19-associated death (Chanda et al., 2020). This study showed that individuals with unsuppressed HIV infection mount weak responses to SARS-CoV-2 infection and poorly recognize SARS-CoV-2 Beta variant mutations. We also examined several mechanisms by which unsuppressed HIV can impact SARS-CoV-2-specific T cell responses and found that HIV-induced immune defects such as low CD4+ T cell counts, higher HIV plasma viral loads, and elevated immune activation were invariably associated with diminished SARS-CoV-2 responses. These findings are consistent with several recent reports, such as a case of one HIV-positive patient with low CD4 count that had prolonged CIVID-19 disease (Wang et al., 2020). The ability of unsuppressed HIV to cause severe immune activation was also recently documented by others (d’Ettorre et al., 2020; Sharov, 2021). Taken together, these data suggest that HIV-induced immune dysregulation negatively impacts the potential to mount robust T cell responses to SARS-CoV-2 infection.
Furthermore, although ART-mediated HIV suppression rarely results in complete immune reconstitution (Henrich et al., 2017), sustained complete plasma HIV suppression was associated with robust SARS-CoV-2 responses that were mostly similar in magnitude and quality to responses mounted by HIV-seronegative individuals. Given reduced levels of CD38 and HLA-DR dual positive cells and near normal absolute CD4 counts in suppressed individuals, it is reasonable to speculate that reduced immune activation and superior CD4+ T helper function were partly responsible for improved immune responses in suppressed individuals.
The emergence of several SARS-CoV-2 variants with mutations in the viral Spike (S) protein such as mutations in the RBD, N-terminal domain (NTD), and furin cleavage site region (Tarke, 2021) continue to fuel the epidemic. These mutations have been shown to directly affect ACE2 receptor binding affinity, infectivity, viral load, and transmissibility (Tarke, 2021; Greaney et al., 2021; Starr et al., 2021). The variants of concern identified since the start of the COVID-19 pandemic include the Alpha (Davies, 2020b), Beta (Tegally et al., 2021b), Gamma (Voloch et al., 2020), and Delta (Mallapaty, 2021), and now the Omicron variant. Most of these have been shown to attenuate neutralization but the impact of these mutations on T cell responses has not been extensively explored (Riou et al., 2022). However, a recent report demonstrating the potential for SARS-CoV-2 to evade cytolytic T lymphocyte (CTL) surveillance, highlight the need for more investigations regarding the potential CTL-driven immune pressure to shape emerging variants (Agerer et al., 2021). To this end, our study provides new evidence that SARS-CoV-2 has the potential to evade T cell recognition. Moreover, our data suggest that spike mutations in the Beta variant that were associated with antibody escape may also escape T cell recognition.
Southern Africa has had at least four epidemic waves of COVID-19. The first was a mixture of SARS-CoV-2 lineages (with D614G), the second wave was driven by the Beta variant (Tegally et al., 2021a), and the third by the Delta variant (Callaway, 2021). The fourth wave dominated by the highly mutated Omicron variant (WHO, 2021b; Viana et al., 2021). Intriguingly, there was some evidence that PLWH in South Africa had increased disease severity in the second wave compared to the first wave (Karim et al., 2021a). The precise mechanisms responsible for increased severity are not fully understood, but low CD4+ T cell counts and high neutrophil-to-lymphocyte ratio (NLR) showed strong association with disease severity (Karim et al., 2021a). Our data suggest that diminished T cell responses to the Beta variant even in previously exposed individuals may have contributed to severe disease in the second wave.
Here, we report poor cross-recognition of the Beta variant by individuals infected with wt and vice versa, which was exacerbated by unsuppressed HIV infection. However, others have reported better cross-recognition between variants and vaccines. Possible explanation for the apparent discrepancy include, (1) unlike other studies that compared responses to the entire spike protein using peptide pools to stimulate cells (Keeton et al., 2022; Gao et al., 2022), our cross-recognition studies focused on head-to-head comparisons of single wt peptides with corresponding variants peptides containing a lineage defining mutation (Keeton et al., 2022). We may have picked up fewer cross-reactive responses because we used dual section of IFN-γ and TNF-α as a readout for antigen-specific responses, which is more stringent than single cytokine producing cells. (3) We used cultured expansions prior to ICS assays which amplifies the response several folds above background and therefore more specific. In fact, our ex vivo cross-recognition data are comparable to other studies which also showed diminution of responses across variants (Keeton et al., 2022). Future studies should apply our cultured expansion and the dual cytokine secretion readout to assess cross-recognition among other variants and different vaccine regimens.
Although, we repeatedly showed robust in vitro T cell expansion following ex vivo peptide stimulation but limited expansion against mutant versions of the peptides, there is need to identify optimal peptides that were targeted by CD8+ and CD4+ T cells in the context of restricting MHC class I and II alleles. SARS-CoV-2 responses are generally very broad (Grifoni et al., 2020); thus, it is not clear from these studies how the loss of T cell cross-recognition in Spike affects the overall protective immunity. Furthermore, investigating if the observed poor T cell cross-recognition between wave 1 and wave 2 is generalizable to the Delta and the Omicron variants is clearly warranted. Importantly, our data raise the question of whether CTL selection pressure plays a significant role in shaping emerging variants. This concept should be investigated using larger longitudinal studies with longer durations of follow-up.
Previous work in this cohort examined the relationship T cell and B cell responses and found a positive association between CD8+ T cells frequency and several CD19 B cell subsets, which was attenuated in PLWH (Karim et al., 2021a), suggesting that both arms of the immune system are impacted by HIV/SARS-CoV-2 coinfection. However, the current study did not examine this relationship at antigen-specific level due to sample limitations. Future work is required to understand the relationship between T cell and humoral immunity and the impact of unsuppressed HIV infection on long-term protection.
In conclusion, we show that uncontrolled HIV infection is associated with low magnitude, reduced polyfunctionality, and diminished cross-recognition of SARS-CoV-2-specific CD4+ and CD8+ T cell responses. Importantly, fully suppressed PLWH had comparable SARS-CoV-2-specific T cell responses with HIV-seronegative individuals. These findings may partly explain high propensity for severe COVID-19 among PLWH and also highlight their vulnerability to emerging SARS-CoV-2 variants of concern, especially those with uncontrolled HIV infection. Hence, there is need to ensure uninterrupted access to ART for PLWH during the COVID-19 pandemic.
Materials and methods
Ethical declaration
The study protocol was approved by the University of KwaZulu-Natal Biomedical Research Ethics Committee (BREC) (approval BREC/00001275/2020). Consenting adult patients (>18 years old) presenting at King Edward VIII, Inkosi Albert Luthuli Central Hospital, and Clairwood Hospital in Durban, South Africa, between July 29 and August November 2021 with PCR confirmed SARS-CoV-2 infection were enrolled in the study.
Sample collection and laboratory testing
Blood samples used in this study were collected between 1 and 3 weeks after COVID-19 PCR positive diagnosis. HIV testing was done using a rapid test and viral load quantification was performed from a 4-ml EDTA by a commercial lab (Molecular Diagnostic Services, Durban, South Africa) using the Real-Time HIV-negative1 viral load test on an Abbott machine. CD4 counts were performed by a commercial lab (Ampath, Durban, South Africa). PLWHs were categorized into suppressed and unsuppressed based on viral load measurements of <50 and >1000 copies/ml, respectively, at the time of sample collection.
T lymphocyte phenotyping
PBMCs were isolated from blood samples by density gradient method and cryopreserved in liquid nitrogen as previously described (Karim et al., 2021b). Frozen PBMCs were thawed, rested, and stimulated for 14 hr at 37°C, 5% CO2 with either staphylococcal enterotoxin B (SEB, 0.5 µg/ml), SARS-CoV-2 wt peptide pool (8 µg/ml), 501Y.V2 variant peptide pool (4 µg/ml), or the Control Spike peptide pool (Miltenyi, Bergisch Gladbach, Germany, 2 µg/ml). Brefeldin A (BioLegend, CA) and CD28/CD49d (BD Biosciences, Franklin Lakes, NJ) were also added ahead of the 14-hr incubation at 5 and 1 µg, respectively. The cells were stained with an antibody cocktail containing: Live/Dead fixable aqua dead cell stain, anti-CD3 PE-CF594 (BD), anti-CD4 Brilliant Violet (BV) 650, anti-CD8 BV 786 (BD), anti-CD38 Alexa Fluor (AF) 700 (BD), anti-human leukocyte antigen (HLA) – DR Allophycocyanin (APC) Cy 7 (BD), and anti-programmed cell death protein 1 (PD) BV 421 (BD). After a 20-min incubation at room temperature, the cells were washed, fixed, and permeabilized using the BD Cytofix/Cytoperm fixation permeabilization kit. Thereafter, the cells were stained for 40 min at room temperature with an intracellular antibody cocktail containing: anti-IFN-γ BV 711 (BD), anti-IL-2 PE (BD), and anti-TNF-α PE-Cy 7 (BD). Finally, the cells were washed and acquired on an LSR Fortessa and analysed on FlowJo v10.7.2. Differences between groups were considered to be significant at a p value of <0.05. Statistical analyses were performed using GraphPad Prism 8.0 (GraphPad Software, Inc, San Diego, CA).
Ex-vivo cultured expansion of SARS-COV-2-specific T cells
PBMCs at a concentration of 2 million cells per well in a 24-well plate in R10 medium were stimulated with 10 μg/ml of SARS-COV-2 of OLP pools spanning the entire spike protein. The cells were incubated at 37°C in 5% CO2. After 2 days, the cells were washed and fresh R10 medium supplemented with 100 U/ml recombinant IL-2 was added. Cultured cells were fed twice weekly with regular medium replenishment. On day 14, the cells were washed three times with fresh R10 medium and rested at 37°C in 5% CO2 overnight in fresh R10 medium. On the following day, the cells were restimulated with individual peptides for 16 hr followed by ICS. Peptides that induced IFN-γ/TNF-α dual production above background (No stimulation control) were deemed reactive. Meaning that the expanded cells contained a subset of cells that were specific for that particular peptide.
Statistical analyses
All statistical analyses were conducted with GraphPad Prism 9.3.1 (GraphPad Software, La Jolla, CA) and p values were considered significant if less than 0.05. Specifically, the Mann-Whitney U- and Kruskal-Wallis H-tests were used for group comparisons. Additional post hoc analyses were performed using the Dunn’s multiple comparisons test. Correlations between variables were defined by the Spearman’s rank correlation test. Categorical data were analysed using the Fisher’s exact test.
Acknowledgements
The authors would like to thank our study participants, the laboratory and clinic staff at Africa Health Research Institute for collecting the samples and compiling the clinical demographic data for the study. The authors would like to thank Drs Wendy Burgers, Catherine Riou, and Robert Wilkinson for designing and providing us the SARS-CoV-2 wt and Beta variant peptides. The authors thank Ms Anele Mbata and Mr Mza Nsimbi for their assistance with sample processing and cryopreservation.
Funding Statement
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Contributor Information
Andrea O Papadopoulos, Email: andrea.papadopoulos@ahri.org.
Zaza M Ndhlovu, Email: zndhlovu@mgh.harvard.edu.
Joshua T Schiffer, Fred Hutchinson Cancer Research Center, United States.
Tadatsugu Taniguchi, Institute of Industrial Science, The University of Tokyo, Japan.
Funding Information
This paper was supported by the following grants:
Howard Hughes Medical Institute 55008743 to Zaza M Ndhlovu.
Bill and Melinda Gates Foundation INV-018944 to Alex Sigal.
South Africa Medical Research Council 31026 to Willem Hanekom.
Sub-Sahara African Network for TB and HIV Research Excellence COL016 to Zaza M Ndhlovu.
Africa Health Research Institute LoA R82 to Zaza M Ndhlovu.
Additional information
Competing interests
No competing interests declared.
No competing interests declared.
Author contributions
Investigation, Writing - original draft, Writing – review and editing.
Investigation, Writing - original draft.
Resources, Formal analysis, Investigation, Writing - original draft, Project administration, Writing – review and editing.
Investigation, Methodology, Writing - original draft.
Data curation, Project administration.
Resources, Investigation, Project administration, Writing – review and editing.
Data curation, Project administration.
Formal analysis, Writing – review and editing.
Data curation, Investigation, Project administration.
Conceptualization, Funding acquisition, Writing – review and editing.
Data curation, Project administration, Writing – review and editing.
Conceptualization, Formal analysis, Validation, Investigation, Writing - original draft, Project administration, Writing – review and editing.
Ethics
Human subjects: Ethical Declaration: The study protocol was approved by the University of KwaZulu-Natal Biomedical Research Ethics Committee (BREC) (approval BREC/00001275/2020). Consenting adult patients (>18 years old) presenting at King Edward VIII, Inkosi Albert Luthuli Central Hospital, and Clairwood Hospital in Durban, South Africa, between 29 July to August November 2021 with PCR confirmed SARS-CoV-2 infection were enrolled into the study.
Additional files
The table contains a list of peptides spanning the receptor-binding domain (RBD) and non-RBD regions of spike with known hotspots for mutations, and a corresponding list of peptides with Beta variant lineage defining mutations. The Beta variants mutations are highlighted in red. The two sets of peptides were used for cultured expansion studies.
Data availability
All source data files for the figures are now publicly available on our institutional website (Africa Health Research Institute database). The data can be accessed using this link: https://doi.org/10.23664/AHRI.SARS.CoV.2.
The following dataset was generated:
Nkosi K, Charasa C, Papadopoulos AO, Nguni TZ, Karim F, Moosa MYS, Gazy I, Jambo K, Hanekom W, Sigal A, Ndhlovu ZM. 2022. Unsuppressed HIV infection impairs T cell responses to SARS-CoV-2 infection and abrogates T cell cross-recognition. AHRI Data Repository.
References
- Agerer B, Koblischke M, Gudipati V, Montaño-Gutierrez LF, Smyth M, Popa A, Genger JW, Endler L, Florian DM, Mühlgrabner V, Graninger M, Aberle SW, Husa AM, Shaw LE, Lercher A, Gattinger P, Torralba-Gombau R, Trapin D, Penz T, Barreca D, Fae I, Wenda S, Traugott M, Walder G, Pickl WF, Thiel V, Allerberger F, Stockinger H, Puchhammer-Stöckl E, Weninger W, Fischer G, Hoepler W, Pawelka E, Zoufaly A, Valenta R, Bock C, Paster W, Geyeregger R, Farlik M, Halbritter F, Huppa JB, Aberle JH, Bergthaler A. SARS-CoV-2 mutations in MHC-I-restricted epitopes evade CD8+ T cell responses. Science Immunology. 2021;6:eabg6461. doi: 10.1126/sciimmunol.abg6461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altmann DM, Boyton RJ. SARS-CoV-2 T cell immunity: Specificity, function, durability, and role in protection. Science Immunology. 2020;5:eabd6160. doi: 10.1126/sciimmunol.abd6160. [DOI] [PubMed] [Google Scholar]
- Ball P. The lightning-fast quest for COVID vaccines - and what it means for other diseases. Nature. 2021;589:16–18. doi: 10.1038/d41586-020-03626-1. [DOI] [PubMed] [Google Scholar]
- Bange EM, Han NA, Wileyto P, Kim JY, Gouma S, Robinson J, Greenplate AR, Hwee MA, Porterfield F, Owoyemi O, Naik K, Zheng C, Galantino M, Weisman AR, Ittner CAG, Kugler EM, Baxter AE, Oniyide O, Agyekum RS, Dunn TG, Jones TK, Giannini HM, Weirick ME, McAllister CM, Babady NE, Kumar A, Widman AJ, DeWolf S, Boutemine SR, Roberts C, Budzik KR, Tollett S, Wright C, Perloff T, Sun L, Mathew D, Giles JR, Oldridge DA, Wu JE, Alanio C, Adamski S, Garfall AL, Vella LA, Kerr SJ, Cohen JV, Oyer RA, Massa R, Maillard IP, Maxwell KN, Reilly JP, Maslak PG, Vonderheide RH, Wolchok JD, Hensley SE, Wherry EJ, Meyer NJ, DeMichele AM, Vardhana SA, Mamtani R, Huang AC. CD8+ T cells contribute to survival in patients with COVID-19 and hematologic cancer. Nature Medicine. 2021;27:1280–1289. doi: 10.1038/s41591-021-01386-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betts MR, Nason MC, West SM, De Rosa SC, Migueles SA, Abraham J, Lederman MM, Benito JM, Goepfert PA, Connors M, Roederer M, Koup RA. HIV nonprogressors preferentially maintain highly functional HIV-specific CD8+ T cells. Blood. 2006;107:4781–4789. doi: 10.1182/blood-2005-12-4818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhaskaran K, Rentsch CT, MacKenna B, Schultze A, Mehrkar A, Bates CJ, Eggo RM, Morton CE, Bacon SCJ, Inglesby P, Douglas IJ, Walker AJ, McDonald HI, Cockburn J, Williamson EJ, Evans D, Forbes HJ, Curtis HJ, Hulme WJ, Parry J, Hester F, Harper S, Evans SJW, Smeeth L, Goldacre B. HIV infection and COVID-19 death: a population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. The Lancet. HIV. 2021;8:e24–e32. doi: 10.1016/S2352-3018(20)30305-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaway E. Delta coronavirus variant: scientists brace for impact. Nature. 2021;595:17–18. doi: 10.1038/d41586-021-01696-3. [DOI] [PubMed] [Google Scholar]
- Calza L, Bon I, Borderi M, Colangeli V, Viale P. No Significant Effect of COVID-19 on immunological and virological parameters in pImmunological and Virological Parameters in Patients With HIV-1 Infection. Journal of Acquired Immune Deficiency Syndromes. 2020;85:e6–e8. doi: 10.1097/QAI.0000000000002427. [DOI] [PubMed] [Google Scholar]
- Chanda D, Minchella PA, Kampamba D, Itoh M, Hines JZ, Fwoloshi S, Boyd MA, Hamusonde K, Chirwa L, Nikoi K, Chirwa R, Siwingwa M, Sivile S, Zyambo KD, Mweemba A, Mbewe N, Mutengo KH, Malama K, Agolory S, Mulenga LB. Covid-19 severity and covid-19–associated deaths among hospitalized patients with hiv infection — zambia, march–december 2020. MMWR. Morbidity and Mortality Weekly Report. 2020;70:807–810. doi: 10.15585/mmwr.mm7022a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies MA. HIV and Risk of COVID-19 Death: A Population Cohort Study from the Western Cape Province, South Africa. medRxiv. 2020a doi: 10.1101/2020.07.02.20145185. [DOI]
- Davies NG. Estimated Transmissibility and Severity of Novel SARS-CoV-2 Variant of Concern 202012/01 in England. medRxiv. 2020b doi: 10.1101/2020.12.24.20248822. [DOI]
- Du J, Wei L, Li G, Hua M, Sun Y, Wang D, Han K, Yan Y, Song C, Song R, Zhang H, Han J, Liu J, Kong Y. Persistent high percentage of HLA-DR+CD38high CD8+ T Cells associated with immune disorder and disease severity of COVID-19. Frontiers in Immunology. 2009;12:735125. doi: 10.3389/fimmu.2021.735125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- d’Ettorre G, Recchia G, Ridolfi M, Siccardi G, Pinacchio C, Innocenti GP, Santinelli L, Frasca F, Bitossi C, Ceccarelli G, Borrazzo C, Antonelli G, Scagnolari C, Mastroianni CM. Analysis of type I IFN response and T cell activation in severe COVID-19/HIV-1 coinfection. Medicine. 2020;99:e21803. doi: 10.1097/MD.0000000000021803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Y, Cai C, Grifoni A, Müller TR, Niessl J, Olofsson A, Humbert M, Hansson L, Österborg A, Bergman P, Chen P, Olsson A, Sandberg JK, Weiskopf D, Price DA, Ljunggren H-G, Karlsson AC, Sette A, Aleman S, Buggert M. Ancestral SARS-CoV-2-specific T cells cross-recognize the Omicron variant. Nature Medicine. 2022;28:472–476. doi: 10.1038/s41591-022-01700-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geretti AM, Stockdale AJ, Kelly SH, Cevik M, Collins S, Waters L, Villa G, Docherty A, Harrison EM, Turtle L, Openshaw P, Baillie JK, Sabin C, Semple M, Group CS. Outcomes of COVID-19 related hospitalisation among people with HIV in the ISARIC WHO clinical characterisation protocol UK protocol: Prospective observational study. SSRN Electronic Journal. 2020;1:3666248. doi: 10.2139/ssrn.3666248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greaney AJ, Loes AN, Crawford KHD, Starr TN, Malone KD, Chu HY, Bloom JD. Comprehensive mapping of mutations in the SARS-CoV-2 receptor-binding domain that affect recognition by polyclonal human plasma antibodies. Cell Host & Microbe. 2021;29:463–476. doi: 10.1016/j.chom.2021.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grifoni A, Weiskopf D, Ramirez SI, Mateus J, Dan JM, Moderbacher CR, Rawlings SA, Sutherland A, Premkumar L, Jadi RS, Marrama D, de Silva AM, Frazier A, Carlin AF, Greenbaum JA, Peters B, Krammer F, Smith DM, Crotty S, Sette A. Targets of t cell responses to sars-cov-2 coronavirus in humans with covid-19 disease and unexposed individuals. Cell. 2020;181:1489–1501. doi: 10.1016/j.cell.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- H. The Lancet When pandemics collide. The Lancet. HIV. 2020;7:e301. doi: 10.1016/S2352-3018(20)30113-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henrich TJ, Hatano H, Bacon O, Hogan LE, Rutishauser R, Hill A, Kearney MF, Anderson EM, Buchbinder SP, Cohen SE, Abdel-Mohsen M, Pohlmeyer CW, Fromentin R, Hoh R, Liu AY, McCune JM, Spindler J, Metcalf-Pate K, Hobbs KS, Thanh C, Gibson EA, Kuritzkes DR, Siliciano RF, Price RW, Richman DD, Chomont N, Siliciano JD, Mellors JW, Yukl SA, Blankson JN, Liegler T, Deeks SG. HIV-1 persistence following extremely early initiation of antiretroviral therapy (ART) during acute HIV-1 infection: An observational study. PLOS Medicine. 2017;14:e1002417. doi: 10.1371/journal.pmed.1002417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampf G. The epidemiological relevance of the COVID-19-vaccinated population is increasing. The Lancet Regional Health. Europe. 2021;11:100272. doi: 10.1016/j.lanepe.2021.100272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karim F, Gazy I, Cele S, Zungu Y, Krause R, Bernstein M, Khan K, Ganga Y, Rodel H, Mthabela N, Mazibuko M, Muema D, Ramjit D, Ndung’u T, Hanekom W, Gosnell B, Lessells RJ, Wong EB, de Oliveira T, Moosa MYS, Lustig G, Leslie A, Kløverpris H, Sigal A, COMMIT-KZN Team HIV status alters disease severity and immune cell responses in Beta variant SARS-CoV-2 infection wave. eLife. 2021a;10:e67397. doi: 10.7554/eLife.67397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karim F, Moosa M, Gosnell B, Cele S, Giandhari J, Pillay S, Tegally H, Wilkinson E, San J, Msomi N, Mlisana K, Khan K, Bernstein M, Manickchund N, Singh L, Ramphal U, Hanekom W, Lessells R, Sigal A, de Oliveira T, COMMIT-KZN Team Persistent SARS-CoV-2 Infection and Intra-Host Evolution in Association with Advanced HIV Infection. medRxiv. 2021b doi: 10.1101/2021.06.03.21258228. [DOI]
- Keeton R, Richardson SI, Moyo-Gwete T, Hermanus T, Tincho MB, Benede N, Manamela NP, Baguma R, Makhado Z, Ngomti A, Motlou T, Mennen M, Chinhoyi L, Skelem S, Maboreke H, Doolabh D, Iranzadeh A, Otter AD, Brooks T, Noursadeghi M, Moon JC, Grifoni A, Weiskopf D, Sette A, Blackburn J, Hsiao N-Y, Williamson C, Riou C, Goga A, Garrett N, Bekker L-G, Gray G, Ntusi NAB, Moore PL, Burgers WA. Prior infection with SARS-CoV-2 boosts and broadens Ad26.COV2.S immunogenicity in a variant-dependent manner. Cell Host & Microbe. 2021;29:1611–1619. doi: 10.1016/j.chom.2021.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keeton R, Tincho MB, Ngomti A, Baguma R, Benede N, Suzuki A, Khan K, Cele S, Bernstein M, Karim F, Madzorera SV, Moyo-Gwete T, Mennen M, Skelem S, Adriaanse M, Mutithu D, Aremu O, Stek C, du Bruyn E, Van Der Mescht MA, de Beer Z, de Villiers TR, Bodenstein A, van den Berg G, Mendes A, Strydom A, Venter M, Giandhari J, Naidoo Y, Pillay S, Tegally H, Grifoni A, Weiskopf D, Sette A, Wilkinson RJ, de Oliveira T, Bekker L-G, Gray G, Ueckermann V, Rossouw T, Boswell MT, Bhiman JN, Moore PL, Sigal A, Ntusi NAB, Burgers WA, Riou C. T cell responses to SARS-CoV-2 spike cross-recognize Omicron. Nature. 2022;603:488–492. doi: 10.1038/s41586-022-04460-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury DS, Cromer D, Reynaldi A, Schlub TE, Wheatley AK, Juno JA, Subbarao K, Kent SJ, Triccas JA, Davenport MP. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nature Medicine. 2021;27:1205–1211. doi: 10.1038/s41591-021-01377-8. [DOI] [PubMed] [Google Scholar]
- Klatt NR, Chomont N, Douek DC, Deeks SG. Immune activation and HIV persistence: implications for curative approaches to HIV infection. Immunological Reviews. 2013;254:326–342. doi: 10.1111/imr.12065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laher F, Ranasinghe S, Porichis F, Mewalal N, Pretorius K, Ismail N, Buus S, Stryhn A, Carrington M, Walker BD, Ndung’u T, Ndhlovu ZM. HIV controllers exhibit enhanced frequencies of major histocompatibility complex class II Tetramer+ gag-specific CD4+ T cells in chronic clade C HIV-1 Infection. Journal of Virology. 2017;91:e02477-16. doi: 10.1128/JVI.02477-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee KW, Yap SF, Ngeow YF, Lye MS. COVID-19 in people living with HIV: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health. 2021;18:3554. doi: 10.3390/ijerph18073554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao M, Liu Y, Yuan J, Wen Y, Xu G, Zhao J, Cheng L, Li J, Wang X, Wang F, Liu L, Amit I, Zhang S, Zhang Z. Single-cell landscape of bronchoalveolar immune cells in patients with COVID-19. Nature Medicine. 2020;26:842–844. doi: 10.1038/s41591-020-0901-9. [DOI] [PubMed] [Google Scholar]
- Mallapaty S. India’s massive COVID surge puzzles scientists. Nature. 2021;592:667–668. doi: 10.1038/d41586-021-01059-y. [DOI] [PubMed] [Google Scholar]
- Ndhlovu ZM, Kamya P, Mewalal N, Kløverpris HN, Nkosi T, Pretorius K, Laher F, Ogunshola F, Chopera D, Shekhar K, Ghebremichael M, Ismail N, Moodley A, Malik A, Leslie A, Goulder PJR, Buus S, Chakraborty A, Dong K, Ndung’u T, Walker BD. Magnitude and kinetics of CD8+ T Cell activation during hyperacute HIV infection impact viral set point. Immunity. 2015;43:591–604. doi: 10.1016/j.immuni.2015.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Painter MM, Mathew D, Goel RR, Apostolidis SA, Pattekar A, Kuthuru O, Baxter AE, Herati RS, Oldridge DA, Gouma S, Hicks P, Dysinger S, Lundgreen KA, Kuri-Cervantes L, Adamski S, Hicks A, Korte S, Giles JR, Weirick ME, McAllister CM, Dougherty J, Long S, D’Andrea K, Hamilton JT, Betts MR, Bates P, Hensley SE, Grifoni A, Weiskopf D, Sette A, Greenplate AR, Wherry EJ. Rapid induction of antigen-specific CD4+ T cells is associated with coordinated humoral and cellular immunity to SARS-CoV-2 mRNA vaccination. Immunity. 2021;54:2133–2142. doi: 10.1016/j.immuni.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, Perez JL, Pérez Marc G, Moreira ED, Zerbini C, Bailey R, Swanson KA, Roychoudhury S, Koury K, Li P, Kalina WV, Cooper D, Frenck RW, Jr, Hammitt LL, Türeci Ö, Nell H, Schaefer A, Ünal S, Tresnan DB, Mather S, Dormitzer PR, Şahin U, Jansen KU, Gruber WC, C4591001 Clinical Trial Group Safety and efficacy of the bnt162b2 mrna covid-19 vaccine. The New England Journal of Medicine. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riou C. Profile of SARS-CoV-2-Specific CD4 T cell response: relationship with disease severity and impact of HIV-1 and active mycobacterium tuberculosis co-infection. medRxiv. 2021 doi: 10.1101/2021.02.16.21251838. [DOI]
- Riou C, du Bruyn E, Stek C, Daroowala R, Goliath RT, Abrahams F, Said-Hartley Q, Allwood BW, Hsiao N-Y, Wilkinson KA, Arlehamn CSL, Sette A, Wasserman S, Wilkinson RJ, HIATUS consortium Relationship of SARS-CoV-2-specific CD4 response to COVID-19 severity and impact of HIV-1 and tuberculosis coinfection. The Journal of Clinical Investigation. 2021;131:149125. doi: 10.1172/JCI149125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riou C, Keeton R, Moyo-Gwete T, Hermanus T, Kgagudi P, Baguma R, Valley-Omar Z, Smith M, Tegally H, Doolabh D, Iranzadeh A, Tyers L, Mutavhatsindi H, Tincho MB, Benede N, Marais G, Chinhoyi LR, Mennen M, Skelem S, du Bruyn E, Stek C, de Oliveira T, Williamson C, Moore PL, Wilkinson RJ, Ntusi NAB, Burgers WA, South African cellular immunity network Escape from recognition of SARS-CoV-2 variant spike epitopes but overall preservation of T cell immunity. Science Translational Medicine. 2022;14:eabj6824. doi: 10.1126/scitranslmed.abj6824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rydyznski Moderbacher C, Ramirez SI, Dan JM, Grifoni A, Hastie KM, Weiskopf D, Belanger S, Abbott RK, Kim C, Choi J, Kato Y, Crotty EG, Kim C, Rawlings SA, Mateus J, Tse LPV, Frazier A, Baric R, Peters B, Greenbaum J, Ollmann Saphire E, Smith DM, Sette A, Crotty S. Antigen-specific adaptive immunity to sars-cov-2 in acute covid-19 and associations with age and disease severity. Cell. 2020;183:996–1012. doi: 10.1016/j.cell.2020.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahin U, Muik A, Derhovanessian E, Vogler I, Kranz LM, Vormehr M, Baum A, Pascal K, Quandt J, Maurus D, Brachtendorf S, Lörks V, Sikorski J, Hilker R, Becker D, Eller A-K, Grützner J, Boesler C, Rosenbaum C, Kühnle M-C, Luxemburger U, Kemmer-Brück A, Langer D, Bexon M, Bolte S, Karikó K, Palanche T, Fischer B, Schultz A, Shi P-Y, Fontes-Garfias C, Perez JL, Swanson KA, Loschko J, Scully IL, Cutler M, Kalina W, Kyratsous CA, Cooper D, Dormitzer PR, Jansen KU, Türeci Ö. COVID-19 vaccine BNT162b1 elicits human antibody and TH1 T cell responses. Nature. 2020;586:594–599. doi: 10.1038/s41586-020-2814-7. [DOI] [PubMed] [Google Scholar]
- Schub D, Klemis V, Schneitler S, Mihm J, Lepper PM, Wilkens H, Bals R, Eichler H, Gärtner BC, Becker SL, Sester U, Sester M, Schmidt T. High levels of SARS-CoV-2-specific T cells with restricted functionality in severe courses of COVID-19. JCI Insight. 2020;5:142167. doi: 10.1172/jci.insight.142167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sette A, Crotty S. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell. 2021;184:861–880. doi: 10.1016/j.cell.2021.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharov KS. HIV/SARS-CoV-2 co-infection: T cell profile, cytokine dynamics and role of exhausted lymphocytes. International Journal of Infectious Diseases. 2021;102:163–169. doi: 10.1016/j.ijid.2020.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinde V, Bhikha S, Hoosain Z, Archary M, Bhorat Q, Fairlie L, Lalloo U, Masilela MSL, Moodley D, Hanley S, Fouche L, Louw C, Tameris M, Singh N, Goga A, Dheda K, Grobbelaar C, Kruger G, Carrim-Ganey N, Baillie V, de Oliveira T, Lombard Koen A, Lombaard JJ, Mngqibisa R, Bhorat AE, Benadé G, Lalloo N, Pitsi A, Vollgraaff P-L, Luabeya A, Esmail A, Petrick FG, Oommen-Jose A, Foulkes S, Ahmed K, Thombrayil A, Fries L, Cloney-Clark S, Zhu M, Bennett C, Albert G, Faust E, Plested JS, Robertson A, Neal S, Cho I, Glenn GM, Dubovsky F, Madhi SA, 2019nCoV-501 Study Group Efficacy of nvx-cov2373 covid-19 vaccine against the b.1.351 variant. The New England Journal of Medicine. 2021;384:1899–1909. doi: 10.1056/NEJMoa2103055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starr TN, Greaney AJ, Addetia A, Hannon WW, Choudhary MC, Dingens AS, Li JZ, Bloom JD. Prospective mapping of viral mutations that escape antibodies used to treat COVID-19. Science. 2021;371:850–854. doi: 10.1126/science.abf9302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streeck H, Jolin JS, Qi Y, Yassine-Diab B, Johnson RC, Kwon DS, Addo MM, Brumme C, Routy J-P, Little S, Jessen HK, Kelleher AD, Hecht FM, Sekaly R-P, Rosenberg ES, Walker BD, Carrington M, Altfeld M. Human immunodeficiency virus type 1-Specific CD8 + T-Cell responses during primary infection are major determinants of the viral set point and loss of CD4 + T Cells. Journal of Virology. 2009;83:7641–7648. doi: 10.1128/JVI.00182-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarke A. Negligible Impact of SARS-CoV-2 Variants on CD4+ and CD8+ T Cell Reactivity in COVID-19 Exposed Donors and Vaccinees. bioRxiv. 2021 doi: 10.1101/2021.02.27.433180. [DOI]
- Tarke A, Sidney J, Kidd CK, Dan JM, Ramirez SI, Yu ED, Mateus J, da Silva Antunes R, Moore E, Rubiro P, Methot N, Phillips E, Mallal S, Frazier A, Rawlings SA, Greenbaum JA, Peters B, Smith DM, Crotty S, Weiskopf D, Grifoni A, Sette A. Comprehensive analysis of T cell immunodominance and immunoprevalence of SARS-CoV-2 epitopes in COVID-19 cases. Cell Reports. Medicine. 2021;2:100204. doi: 10.1016/j.xcrm.2021.100204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tegally H, Wilkinson E, Giovanetti M, Iranzadeh A, Fonseca V, Giandhari J, Doolabh D, Pillay S, San EJ, Msomi N, Mlisana K, von Gottberg A, Walaza S, Allam M, Ismail A, Mohale T, Glass AJ, Engelbrecht S, Van Zyl G, Preiser W, Petruccione F, Sigal A, Hardie D, Marais G, Hsiao N, Korsman S, Davies MA, Tyers L, Mudau I, York D, Maslo C, Goedhals D, Abrahams S, Laguda-Akingba O, Alisoltani-Dehkordi A, Godzik A, Wibmer CK, Sewell BT, Lourenço J, Alcantara LCJ, Kosakovsky Pond SL, Weaver S, Martin D, Lessells RJ, Bhiman JN, Williamson C, de Oliveira T. Detection of a SARS-CoV-2 variant of concern in South Africa. Nature. 2021a;592:438–443. doi: 10.1038/s41586-021-03402-9. [DOI] [PubMed] [Google Scholar]
- Tegally H, Wilkinson E, Giovanetti M, Iranzadeh A, Fonseca V, Giandhari J, Doolabh D, Pillay S, San EJ, Msomi N, Mlisana K, von Gottberg A, Walaza S, Allam M, Ismail A, Mohale T, Glass AJ, Engelbrecht S, Van Zyl G, Preiser W, Petruccione F, Sigal A, Hardie D, Marais G, Hsiao M, Korsman S, Davies MA, Tyers L, Mudau I, York D, Maslo C, Goedhals D, Abrahams S, Laguda-Akingba O, Alisoltani-Dehkordi A, Godzik A, Wibmer CK, Sewell BT, Lourenço J, Alcantara LCJ, Pond SLK, Weaver S, Martin D, Lessells RJ, Bhiman JN, Williamson C, de Oliveira T. Emergence and Rapid Spread of a New Severe Acute Respiratory Syndrome-Related Coronavirus 2 (SARS-CoV-2) Lineage with Multiple Spike Mutations in South Africa. medRxiv. 2021b doi: 10.1101/2020.12.21.20248640. [DOI]
- Tegally H, Wilkinson E, Lessells RJ, Giandhari J, Pillay S, Msomi N, Mlisana K, Bhiman JN, von Gottberg A, Walaza S, Fonseca V, Allam M, Ismail A, Glass AJ, Engelbrecht S, Van Zyl G, Preiser W, Williamson C, Petruccione F, Sigal A, Gazy I, Hardie D, Hsiao NY, Martin D, York D, Goedhals D, San EJ, Giovanetti M, Lourenço J, Alcantara LCJ, de Oliveira T. Sixteen novel lineages of SARS-CoV-2 in South Africa. Nature Medicine. 2021c;27:440–446. doi: 10.1038/s41591-021-01255-3. [DOI] [PubMed] [Google Scholar]
- Verma P, Dumka A, Bhardwaj A, Ashok A, Kestwal MC, Kumar P. A statistical analysis of impact of covid19 on the global economy and stock index returns. SN Computer Science. 2021;2:27. doi: 10.1007/s42979-020-00410-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viana R, Moyo S, Amoako DG, Tegally H, Scheepers C, Althaus CL, Anyaneji UJ, Bester PA, Boni MF, Chand M, Choga WT, Colquhoun R, Davids M, Deforche K, Doolabh D, Engelbrecht S, Everatt J, Giandhari J, Giovanetti M, Hardie D, Hill V, Hsiao NY, Iranzadeh A, Ismail A, Joseph C, Joseph R, Koopile L, Pond SLK, Kraemer MU, Kuate-Lere L, Laguda-Akingba O, Lesetedi-Mafoko O, Lessells RJ, Lockman S, Lucaci AG, Maharaj A, Mahlangu B, Maponga T, Mahlakwane K, Makatini Z, Marais G, Maruapula D, Masupu K, Matshaba M, Mayaphi S, Mbhele N, Mbulawa MB, Mendes A, Mlisana K, Mnguni A, Mohale T, Moir M, Moruisi K, Mosepele M, Motsatsi G, Motswaledi MS, Mphoyakgosi T, Msomi N, Mwangi PN, Naidoo Y, Ntuli N, Nyaga M, Olubayo L, Pillay S, Radibe B, Ramphal Y, Ramphal U, San JE, Scott L, Shapiro R, Singh L, Smith-Lawrence P, Stevens W, Strydom A, Subramoney K, Tebeila N, Tshiabuila D, Tsui J, van Wyk S, Weaver S, Wibmer CK, Wilkinson E, Wolter N, Zarebski AE, Zuze B, Goedhals D, Preiser W, Treurnicht F, Venter M, Williamson C, Pybus OG, Bhiman J, Glass A, Martin DP, Rambaut A, Gaseitsiwe S, von Gottberg A, de Oliveira T. Rapid Epidemic Expansion of the SARS-CoV-2 Omicron Variant in Southern Africa. medRxiv. 2021 doi: 10.1101/2021.12.19.21268028. [DOI] [PMC free article] [PubMed]
- Vizcarra P, Pérez-Elías MJ, Quereda C, Moreno A, Vivancos MJ, Dronda F, Casado JL, COVID-19 ID Team Description of COVID-19 in HIV-infected individuals: a single-centre, prospective cohort. The Lancet. HIV. 2020;7:e554–e564. doi: 10.1016/S2352-3018(20)30164-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voloch CM, Silva F R, de Almeida LGP, Cardoso CC, Brustolini OJ, Gerber AL, Guimarães A, Mariani D, Costa R, Ferreira OC, Cavalcanti AC, Frauches TS, de Mello CMB, Galliez RM, Faffe DS, Castiñeiras T, Tanuri A, de Vasconcelos ATR, Covid19-UFRJ Workgroup. LNCC-Workgroup Genomic Characterization of a Novel SARS-CoV-2 Lineage from Rio de Janeiro, Brazil. bioRxiv. 2020 doi: 10.1101/2020.12.23.20248598. [DOI] [PMC free article] [PubMed]
- Wang M, Luo L, Bu H, Xia H. One case of coronavirus disease 2019 (COVID-19) in a patient co-infected by HIV with a low CD4+ T-cell count. International Journal of Infectious Diseases. 2020;96:148–150. doi: 10.1016/j.ijid.2020.04.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . Update on Omicron. WHO DASH board. WHO; 2021a. [Google Scholar]
- WHO . Update on Omicron. WHO DASH board; 2021b. [Google Scholar]
- Wibmer CK, Ayres F, Hermanus T, Madzivhandila M, Kgagudi P, Oosthuysen B, Lambson BE, de Oliveira T, Vermeulen M, van der Berg K, Rossouw T, Boswell M, Ueckermann V, Meiring S, von Gottberg A, Cohen C, Morris L, Bhiman JN, Moore PL. SARS-CoV-2 501Y.V2 escapes neutralization by South African COVID-19 donor plasma. Nature Medicine. 2021;27:622–625. doi: 10.1038/s41591-021-01285-x. [DOI] [PubMed] [Google Scholar]