Abstract
Objectives: Based on the recommendations of the World Health Organization, we investigated the feasibility of oral health interventions (OHIs) as part of Health Promoting Schools (HPS) program in Karaj city elementary schools.
Materials and Methods: OHIs were accepted to be integrated into the components of HPS program by using the nominal group technique (NGT) and semi-structured interviews. Three NGT meetings were held with the faculty members of the School of Dentistry, Tehran University of Medical Sciences, and Karaj elementary school health care providers. Semi-structured interviews were held with school health executives of the Ministry of Health and Medical Education. The expert panel edited the OHIs and corrected the fragmentations, overlaps, and duplications. OHIs were sent to 24 individuals in six multi-stakeholder groups (faculty members of pediatric dentistry and community oral health departments, elementary school administrators, executive managers of Ministry of Health and Medical Education, elementary school dean and school healthcare providers). They were asked to score the feasibility of each intervention on a scale of 0 to 10.
Results : Based on the mean score of feasibility (threshold: 8) the OHIs were divided into two groups of feasible and infeasible. Eighty-six interventions were feasible, with a total mean score of 8.83±0.59 out of 10. The highest feasibility score was related to “comprehensive school health education”.
Conclusion: Integration of OHIs in HPS program is acceptable and feasible. The results can help policy-makers support the integration of OHIs in HPS program and encourage them to implement the program at the national level.
Key Words: Health Promotion, Public Policy, Health Care Reform, School Health Services, Public Health
Introduction
Childhood and adolescence are key periods of biological and social changes, and the effects of these periods on health have been documented in scientific resources [1]. Health in children is so important that the World Health Organization (WHO) acknowledges that positive childhood experiences related to health and education are keys to reducing global inequalities [2]. Moreover, oral and dental diseases in children adversely affect the developmental processes of life including socialization, communication, and self-confidence. Regarding the fact that during childhood and the school years, long-lasting beliefs, positive attitudes, and personal skills start to develop, paying special attention to oral health in this age group seems necessary [3]. Children with poor oral health have been reported to experience nearly 12 times more days with activity limitations [4]. Further-more, it has been indicated that improving the children's oral health can have positive effects on educational experiences as well [5].
There are more than one billion students throughout the world that spend a great deal of their time at schools; therefore, schools can play a paramount important role in health promotion, and school years in children's life ought to be regarded as an opportunity to teach them proper personal hygiene and preventive strategies in particular [6]. Since realizing the goal of health promotion in schools requires unified involvement and mutual collaboration of families, schools, health treatment centers, and the community, one of the most important ways to boost the students’ health is the implementation of various health education programs that guarantee their active participation in different healthcare activities [7]. Since early 1980s, a social perspective has been developed by the WHO for health promotion activities instead of focusing on individual health behaviors [8]. They formulated numerous health promotion programs like Health Promoting Schools (HPS) with the cooperation of health promotion, education and communication sectors, the school health workers, and the regional offices of the WHO in 1995 [9]. The HPS program has continuously enhanced potentials as a system in a healthy environment to promote health in everyday life, education, and work. Its primary objective is to enhance the potential of the schools to promote students’, families’ and community's health [10].The HPS program trains students in such a way that they can manage to take control of their health and therefore, prepares them to play their role as active responsible people in the future [11].
The program has eight components including (I) comprehensive school health education, (II) school health services, (III) nutritional services, (IV) healthy and safe school environments, (V) physical activity, (VI) school mental health, (VII) health promotion for school staff, and (VIII) student, family and community involvement [12].
A multitude of other investigations acknowl-edge that HPS programs can be beneficial and effective to promote students' health [13,14]. According to the evidence presented in a systematic review, in terms of nutritional services, the HPS program has managed to increase the consumption of high-fiber foods, healthy snacks, water, milk, fruits, and vegetables and reduce the consumption of red meat, high-fat foods, and sugary beverages [15].
The WHO developed the HPS program during the past two decades and it is currently running worldwide [8]. Iran is a country with a population of 80 million with 13 million students, where the program has been running since 2007, followed by programs on high-risk diseases such as diabetes and heart disease[16]. Initially, it was implemented as a pilot program in 2009-2010 in 36 elementary schools of East Azarbaijan Province and then expanded to include 700 elementary schools in the following year (2011-2012) [17].
Although this program covers different health-care fields, oral health interventions (OHIs) have not been incorporated into the HPS program. As recommended by the WHO, oral health diseases have a lot of common risk factors. Therefore, the integration of oral health promotion into broader health promotion programs should be noticed [18]. Some studies have investigated the feasibility of implementing health-based programs in HPS schools [17].
Despite the abundance of feasibility studies in general health using qualitative methods such as questionnaires and Delphi [19], there are few studies investigating the feasibility of OHIs in the HPS program, while the WHO has emphasized on its implementation in countries[20]. The aim of the present study was to investigate the feasibility of implementing OHIs as part of HPS program in the Iranian elementary schools.
MATERIALS AND METHODS
Ethical approval and consent to participate:
The Research Ethics Committee of Tehran University of Medical Sciences approved all procedures concerning humans in this study (Code: IR.TUMS.REC.1394.855). Verbal consent was obtained from each participant before the study was commenced. Additionally, the participants were allowed to withdraw at any time.
Procedural details:
First, we systematically searched the electronic databases including Cochrane, PubMed Central, Google Scholar, CINAHL, and EMBASE. Our exposures of interest were “Oral Health”, “Health Promoting Schools” and “Feasibility Assessment” from 2000 to 2018. After that, we defined the OHIs using the nominal group technique (NGT) and semi-structured interviews. Then, their feasibility was evaluated using the classic Delphi technique.
Three professional NGT meetings with school health experts were held to specify the OHIs that have the potential to be integrated into the HPS program. The faculty members of the community oral health and pediatric dentistry departments of Dental School of Tehran University of Medical Sciences and school health care providers of elementary schools of Karaj city participated in this study. All participants had at least three years of work experience in children's oral health field.
Karaj, a large city near Tehran, was selected for this study based on its experiences of HPS program and high population. The results of the 2016 “General Census of Population and Housing " showed that Karaj had more than 2.5 million population and was the destination of the largest number of immigrants in the country [21].
Based on the structure of the NGT, the sessions were managed by a facilitator who was a member of the research team. At the begging, the participants were asked to write all OHIs that could be integrated into the eight components of the HPS program on a white paper sheet and score the acceptability of any suggested intervention on a scale of 0-10 [22]. The OHI list of each participant was then presented to the other participants to score, and eventually the list was finalized.
Considering the role of MOHME in the community health planning, the opinions of seven school health administrators at the department of school health executives were also collected through semi-structured interviews. The interviewees were asked to announce their proposed OHIs for each component of HPS program which could be integrated into the HPS components. The statements of the interviewees were recorded after ensuring mutual proper understanding, and the conversations continued until saturation. After the interviews were done, the executive team listened to each recorded interview twice and typed the suggested interventions.
Interventions were organized into eight components of the HPS program and were sent back to the same interviewees for scoring and prioritizing the interventions using the Delphi method. They were asked to score the acceptability of intervention on a scale of 0-10 [23]. After completing the NGT and semi-structured interviews, reduction of fragmentation, overlap, and duplication of ideas were done by the expert panel [24]. The executive group of the project, namely the “expert panel” composed of 4 people: (I) a faculty member from the pediatric dentistry department, (II) a faculty member from the community oral health department, (III) a PhD candidate, and (IV) a senior dental student
Finally, the interventions were finalized. At the beginning of the study, OHIs were categorized into each of the eight components of the HPS program, and in NGT sessions and interviews, each of these interventions was scored separately. To determine the feasibility of the OHIs, we employed purposive sampling during which 24 individuals in 6 multi-stakeholder groups were selected as the study population [25]: (I) seven elementary school principals from Karaj, (II) three faculty members from the community oral health department, (III) three faculty members from the pediatric dentistry department, (IV) four executives and experts of the Ministry of Health and Medical Education, (V) four school health care providers, and (VI) three executives and experts of Ministry of Education. These participants were asked to score the feasibility of the mentioned interventions on a scale of 0-10 during March and April of 2019. The mean feasibility score of each intervention was calculated and divided into two groups based on the threshold of 8 out of 10: feasible and infeasible. However, given the wide range of quantitative scores for the suggested oral health interventions, quantitative analysis was done too to better understand the differences among the 8 components of the program (ANOVA and Tukey’s test).
Based on the results of the Kolmogorov-Smirnov test (SPSS 22), ANOVA and Tukey’s post hoc test with 95% confidence interval were applied. Although our study was a qualitative study, we used statistical tests like ANOVA and Tukey’s test to be able to distinguish between the components of the OHIs.
Results
According to the score given to each intervention, the interventions were divided into feasible and infeasible categories. A total of 86 interventions achieved scores higher than eight. The highest and the lowest rates of feasible interventions were related to "Comprehensive School Health Education" (31 interventions) and "Student, family and Community Involvement" (3 interventions) fields, respectively. The number and percentage of interventions with feasibility scores higher than eight (in each component of HPS program) are presented in Table 1.
Table 1.
Number of feasible and infeasible OHIs in all components of Health Promoting Schools (HPS) program
| HPS Components | Infeasible interventions |
Feasible interventions |
Total (100%) |
||
| N | % | N | % | N | |
| Comprehensive School Health Education |
1 | 3.1 | 31 | 96.9 | 32 |
| School Health Services | 5 | 29.4 | 12 | 70.6 | 17 |
| Healthy and Safe School Environments |
0 | 0 | 11 | 100 | 11 |
| Nutritional Services | 0 | 0 | 12 | 100 | 12 |
| Physical Activity | 0 | 0 | 5 | 100 | 5 |
| Health Promotion for School Staff | 0 | 0 | 8 | 100 | 8 |
| School Mental Health | 0 | 0 | 4 | 100 | 4 |
| Student, family and Community Involvement |
1 | 25 | 3 | 75 | 4 |
| Total | 7 | 7.5 | 86 | 92.5 | 93 |
The total mean score of feasibility was 8.83±0.59 out of 10. The highest and the lowest mean scores of feasible interventions were related to components of "Comprehensive School Health Education" (9.11±0.60) and "Student, Family and Community Involvement" (8.42±0.61), respectively. The mean score of feasibility of the interventions in all components of the HPS program is presented in Table 2.
Table 2.
Mean score of feasibility of the interventions in all components of the Health Promoting Schools (HPS) program
| Component of HPS program | Mean | SD |
|---|---|---|
|
Comprehensive school health
education |
9.11 | 0.6 |
| School health services | 8.43 | 0.59 |
|
Healthy and safe school
environments |
8.82 | 0.59 |
| Nutritional Services | 8.89 | 0.44 |
| Physical Activity | 9.06 | 0.29 |
|
Health Promotion for School
Staff |
8.70 | 0.3 |
| School mental health | 8.44 | 0.24 |
|
Student, family and community
involvement |
8.42 | 0.61 |
SD: standard deviation
The Kolmogorov-Smirnov test showed that all data were normally distributed (P<0.05); therefore, ANOVA and Tukey’s post hoc test with 95% confidence interval were applied. The results of ANOVA indicated that there was a significant difference in feasibility of the HPS program components (P<0.05).
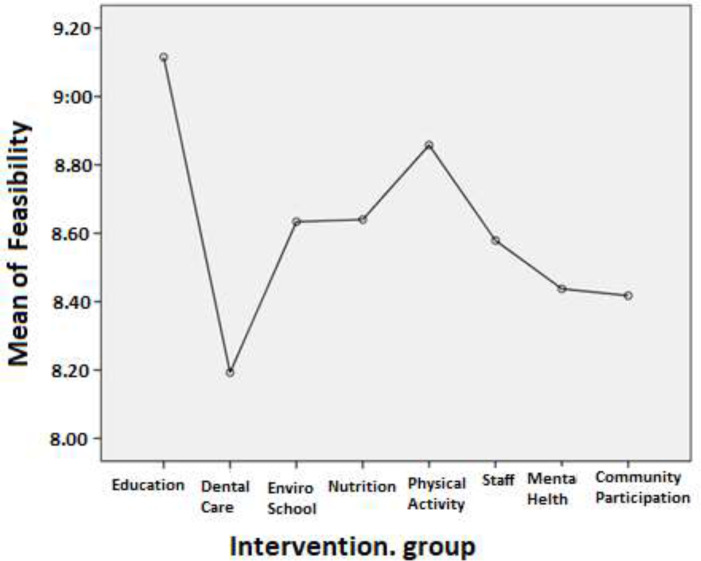
The Tukey’s post-hoc test results showed that variables were significantly correlated (P<0.001). Figure 1 shows the details. In spite of a significant difference between “Comprehensive School Health Education” and “School Health Services” (P<0.05), there was no significant difference between other HPS components (P>0.05). Figure 1 indicates the differences between the mean scores of feasibility of different components of the HPS program.
Fig. 1.
One-way ANOVA means plot of feasibility based on each of the eight components by the study groups
Discussion
Regarding the importance of oral health and necessity of its integration into holistic health programs like HPS, we tried to take advantage of all stakeholder groups at three levels: (I) scientific elite working in school health field (faculty members), (II) planners (policy-making executives at the Ministry of Health and Medical Education) and (III) people engaged in management and implementation of health programs (school healthcare providers).
In this study, we took advantage of different methods of data collection like NGT, classic Delphi method, and semi-structured interview approach. The feasibility of these interventions was scored by the multidisciplinary stakeholder groups. Another strength point of the present study was implementing the recommendations of the WHO to integrate oral health programs into other broader programs which has been taken into account in a multitude of other studies [18,26]. The WHO announced that since the conditions and challenges vary widely from one society to another, their recommendation can be adapted to the cultural context and the resources of a country [27]. Therefore, localization and customization of global health programs, and in particular HPS, is a must that has been addressed in many studies in some countries. In this study, we found the OHIs and customized them for our country.
In Canada, comprehensive School Health (CSH) has been demonstrated as an effective model for school-based health promotion. Roberts et al. [28] evaluated the essential conditions for the implementation of CSH to improve health behaviors of students and discovered the essential conditions of successful CSH implementation.
In Malaysia, a child-to-child health promotion approach called the Doktor Muda (Junior Doctors) Program (DMP) was introduced in 1980s to primary schools.
This program was considered as a HPS model. They compared the children’s oral health-related quality of life in schools with DMP program and in schools without it. The results indicated that in the DMP schools, 11–12-year-old children had significantly higher oral health-related quality of life compared with non-DMP school children. They were significantly better in some oral health behaviors and indices [10].
The results of statistical analysis showed that the feasibility of “Comprehensive School Health Education” component was significantly higher than other components and there was a significant difference between the mentioned component and “School Health Services” component. Besides, high cost of dental care procedures has been recognized as one of the most important barriers against the utilization of dental health services. It causes the infeasibility of interventions associated with these services. In 2014, Thompson et al. [29] announced that approximately 1 out of 5 Canadians reported the cost of dental services as a barrier against dental care service utilization. Moreover, Hardgraveset al. [30] stated that lack of accessibility to dental care services can impede optimal dental care. In Iran, Amiresmaili et al. [31] reported that low income and expensive dental procedures were the main reasons why people avoided dental treatment. Beigi et al. [32] stated that removing financial barriers by complementary dental insurance had a significant positive impact on dental visits of Tehran citizens. As pointed out in the results, unlike the oral health training interventions, feasibility of providing clinical services (healthcare services) in elementary schools achieved a low feasibility score. This may reflect the stakeholders' awareness of high costs of clinical services at schools (healthcare services). The results of the current study showed that school-based nutritional interventions earned high feasibility scores. Gannon et al. [33] investigated the effectiveness and feasibility of nutritional education for preschoolers who were provided with books on nutrition, food tasting experiences, useful nutritional activities, food safety training, food choices and nutrition-related physical activity. Their findings indicated that nutritional training in preschools is feasible and can influence the nutritional behaviors of children.
Kelishadi et al. [34] conducted a research to find barriers against the feasibility of physical activities in schools in Iran. Their findings indicated that lack of safe outdoor environment, lack of suitable places to do physical activities, and uncooperative families were the major barriers against physical activity at schools. Parents also pointed out that in addition to the priority of studying and doing homework, lack of safe and accessible places for exercise were the main obstacles. The findings of our study demonstrated that increasing the physical activity in elementary schools would occur by implementing interventions like "performing cultural activities to promote health during exercises". This intervention was one of the interventions perceived in the present study by stakeholders to help surmount major obstacles of students' physical activity.
Greaney et al, [35] at Harvard University devised an interdisciplinary curriculum to increase physical activity, decrease watching television, and increase the consumption of fruits and vegetables in middle schoolers in 2007. They explored acceptability and feasibility of the curriculum using 21 in-depth interviews with administrators, program coordinators, and teachers having experience with one or more of the intervention components. In line with our results, they indicated the feasibility of training programs during class sessions. Also, Barber et al. [36] indicated that the physical activity intervention was feasible at schools .
In Poland, Woynarowska-Sołdan [37] explored the results of implementation of school staff health promotion of the HPS program in 2018. Over 900 teachers and non-teaching employees from 21 schools took part in this project. They found that the implementation of the school staff health promotion program was successful; thus, programs related to the health of school staff were developed[37].
In agreement with our findings about the feasibility of mental health interventions and counseling services at schools, Lauria-Horner et al. [38] conducted a study to gauge feasibility and short-term effects of implementing a new curriculum to promote knowledge and attitude of primary school students concerning mental health. The research group prepared a curriculum regarding emotional development, depression, anxiety disorders, and attention-deficit hyperactivity disorder which was delivered by the school teachers. As in our study, emphasis on mental health education improved knowledge and attitudes towards mental health, and increased the feasibility of the project. Similarly, Evans et al, [39] in a study appraised the feasibility of a school mental health promotion program known as Mind Matters. The results demonstrated that the implementation of Mind Matters program was feasible and helped students feel safe and valued. The contribution of students, families and society to school health promotion plans is one of the ultimate goals of every health system.
Aydin [40] declared that the contribution and engagement of different groups of stakeholders (including schools, families, and society), guarantee the feasibility of collaborative programs and allow other people to contribute to this process and take their own responsibility. Despite the low scores of some interventions in our study, particular attention should be paid to the contribution of students, families and society to school health promotion plans in the HPS program in Iran.
CONCLUSION
Persistence in community-based educational programs, using combined training programs, follow-up and taking the underling argument in favor of theories and models of behavior change and provision of preventive services are the best ways to achieve optimal results. Although these issues have relatively been addressed in the HPS program, OHIs are ignored. After employing a wide variety of techniques and stakeholders, the findings of the present study resulted in 93 acceptable oral health related interventions; out of which, 86 interventions (92%) were also feasible. Therefore, as recommended by the WHO, OHIs should be integrated into HPS program. Our results showed that integration of OHIs in HPS program is acceptable and feasible. It can assist the policy makers to bolster and support the oral health integration in HPS program and encourage them to implement it at the national level.
Notes:
Cite this article as: Rostam Beigi M, Gholami M, Jafari A. Integration of Oral Health Interventions in the Health Promoting Schools Program in Iran: A Multi-Stakeholder Feasibility Assessment. Front Dent. 2021;18:43.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- 1.Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry. 2010 Nov;197(5):378–85. doi: 10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Langford R, Bonell CP, Jones HE, Pouliou T, Murphy SM, Waters E, et al. The WHO Health Promoting School framework for improving the health and well-being of students and their academic achievement. Cochrane Database Syst Rev. 2014 Apr;(4):Cd008958. doi: 10.1002/14651858.CD008958.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kwan SY, Petersen PE, Pine CM, Borutta A. Health-promoting schools: an opportunity for oral health promotion. Bulletin of the World Health organization. 2005 Sep;83:677–85. [PMC free article] [PubMed] [Google Scholar]
- 4.Offices UGA. Oral health: dental disease is a chronic problem among low-income populations. Washington, DC: Report to Congressional Requesters; 2000. Apr, [Google Scholar]
- 5.Jackson SL, Vann WF Jr, Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children's school attendance and performance. Am J Public Health. 2011 Oct;101(10):1900–6. doi: 10.2105/AJPH.2010.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vozza I, Guerra F, Marchionne M, Bove E, Corridore D, Ottolenghi L. A multimedia oral health promoting project in primary schools in central Italy. Annali di stomatologia. 2014 Jul;5(3):87. [PMC free article] [PubMed] [Google Scholar]
- 7.Honkala S. World Health Organization approaches for surveys of health behaviour among schoolchildren and for health-promoting schools. Med Princ Pract. 2014;23 Suppl 1(Suppl 1):24–31. doi: 10.1159/000354172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mukoma W, Flisher AJ. Evaluations of health promoting schools: a review of nine studies. Health Promot Int. 2004 Sep;19(3):357–68. doi: 10.1093/heapro/dah309. [DOI] [PubMed] [Google Scholar]
- 9.Jones JT, Furner Matthew. Health-promoting schools: a healthy setting for living, learning and working. World Health Organization; http://www.who.int/iris/handle/10665/63868 . [Google Scholar]
- 10.Yusof ZY, Jaafar N. Health promoting schools and children's oral health related quality of life. Health Qual Life Outcomes. 2013 Dec;11(1):1–9. doi: 10.1186/1477-7525-11-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Croucher R, Rodgers AI, Humpherson WA, Crush L. The "spread of effect' of a school based dental health education project. Community Dent Oral Epidemiol. 1985 Apr;13(4):205–7. doi: 10.1111/j.1600-0528.1985.tb01903.x. [DOI] [PubMed] [Google Scholar]
- 12.Kwan S, Petersen P WHO Information Series on School Health, Document Eleven. Oral Health Promotion: An Essential Element of a Health-Promoting School. Geneva: WHO; 2003. [Google Scholar]
- 13.Shahhosseini Z, Simbar M, Ramezankhani A. Characteristics of health-promoting schools from Iranian adolescents' point of view. Int J Adolesc Med Health. 2016 May;28(2):155–60. doi: 10.1515/ijamh-2014-0085. [DOI] [PubMed] [Google Scholar]
- 14.Nouri MFAB RP, Riyahi L. The effect of the impact of health promoting program on environmental indicators in elementary schools of Tabriz in academic year 2013-2014. Eur Online JNat. 2014 Dec;3(3 (s)):363. [Google Scholar]
- 15.Wang D, Stewart D. The implementation and effectiveness of school-based nutrition promotion programmes using a health-promoting schools approach: a systematic review. Public Health Nutr. 2013 Jun;16(6):1082–100. doi: 10.1017/S1368980012003497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sartipizadeh M, Yazdi-Feyzabadi V, Sakha MA, Zarrin A, Bazyar M, Moghadam TZ, Zandian H. Evaluating the health promoting schools in Iran: across-sectional study. Health Educ. 2021 Jan;121(2):125–139. [Google Scholar]
- 17.Fathi B, Allahverdipour H, Shaghaghi A, Kousha A, Jannati A. Challenges in developing health promoting schools' project: application of global traits in local realm. Health Promot Perspect. 2014 Jul;4(1):9–17. doi: 10.5681/hpp.2014.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. Integrated health services-what and why? Making Health Systems Work, Technical Brief No. 1. Geneva: World Health Organization; 2008. [Google Scholar]
- 19.Sahal N, Reintjes R, Eltayeb E, Aro A. Feasibility of implementing recommendations to improve communicable diseases surveillance-a modified Delphi study. Afr Health Sci. 2011;11 Suppl 1(Suppl 1):S93–9. doi: 10.4314/ahs.v11i3.70077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Organization WH. Oral health promotion: an essential element of a health-promoting school. 2003. [Google Scholar]
- 21.Alimondegari M, Banihashemi FS. The trend of changes in the unmarried population due to divorce in the general population and housing censuses of Iran: 1986-2016. Iran J Offic Statis Stud. 2020 Mar;30(2):503–18. [Google Scholar]
- 22.van Dijk PA, Miller D, Calder J, DiGiovanni CW, Kennedy JG, Kerkhoffs GM, et al. The ESSKA-AFAS international consensus statement on peroneal tendon pathologies. Knee Surg Sports Traumatol Arthrosc. 2018 Oct;26(10):3096–107. doi: 10.1007/s00167-018-4971-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Howell AM, Burns EM, Hull L, Mayer E, Sevdalis N, Darzi A. International recommendations for national patient safety incident reporting systems: an expert Delphi consensus-building process. BMJ Qual Saf. 2017 Feb;26(2):150–163. doi: 10.1136/bmjqs-2015-004456. [DOI] [PubMed] [Google Scholar]
- 24.Thapa B. Developing adolescent health-risk behavior instrument using Delphi method. Asian Pac. 2017;4:48–56. [Google Scholar]
- 25.Storms H, Claes N, Aertgeerts B, Van den Broucke S. Measuring health literacy among low literate people: an exploratory feasibility study with the HLS-EU questionnaire. BMC Public Health. 2017 Dec;17(1):475. doi: 10.1186/s12889-017-4391-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Petersen PE, Kwan S. Evaluation of community-based oral health promotion and oral disease prevention-WHO recommendations for improved evidence in public health practice. Community Dent Health. 2004 Dec;21(4):319–29. [PubMed] [Google Scholar]
- 27.World Health Organization. Local action: Creating health promoting schools. 2000 [Google Scholar]
- 28.Roberts E, McLeod N, Montemurro G, Veugelers PJ, Gleddie D, Storey KE. Implementing Comprehensive School Health in Alberta, Canada: the principal's role. Health Promot Int. 2016 Dec;31(4):915–24. doi: 10.1093/heapro/dav083. [DOI] [PubMed] [Google Scholar]
- 29.Thompson B, Cooney P, Lawrence H, Ravaghi V, Quinonez C. Cost as a barrier to accessing dental care: findings from a Canadian population-based study. J Public Health Dent. 2014 Aug;74(3):210–8. doi: 10.1111/jphd.12048. [DOI] [PubMed] [Google Scholar]
- 30.Hardgraves VM, MitchellTV , Hanson CC, Simmer-Beck M. A qualitative analysis of oral health care needs in arkansas nursing facilities: the professional role of the dental hygienist. J Dent Hyg. 2014 Dec;88(6):353–63. [PubMed] [Google Scholar]
- 31.Amiresmaili M, Amini S, Shahravan A, Goudarzi R, Saberi-Anari SH. Avoidance dental visit, the impact of predictor factors: A cross-sectional study in Kerman, Iran. J Oral Health Oral Epidemiol. 2017 Dec;7(1):39–46. [Google Scholar]
- 32.Beigi MR, Shamshiri AR, Asadi-Lari M, Hessari H, Jafari A. A crossectional investigation of the relationship between complementary health insurance and frequency of dental visits in 15 to 64 years old of Tehran population, Iran, a secondary data analysis (urban HEART-2) BMC Health Serv Res. 2019 Dec;19(1):678. doi: 10.1186/s12913-019-4526-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gannon A, Olson R, Cottrell L. Assessing the effectiveness of pre-school nutrition education: A pilot program. J Nutr Educ Behav. 2013 Sep;45(4):S11. [Google Scholar]
- 34.Kelishadi R, Ghatrehsamani S, Hosseini M, Mirmoghtadaee P, Mansouri S, Poursafa P. Barriers to physical activity in a population-based sample of children and adolescents in Isfahan, Iran. Int J Prev Med. 2010;1(2):131, 7. [PMC free article] [PubMed] [Google Scholar]
- 35.Greaney M, Hardwick CK, Mezgebu S, Lindsay AC, Roover ML, Peterson KE. Assessing the feasibility of a multi-program school-based intervention to promote physical activity and healthful eating in middle schools prior to wide-scale implementation. Am J Health Educ. 2007 Sep;38:250–7. [Google Scholar]
- 36.Barber SE, Jackson C, Hewitt C, Ainsworth HR, Buckley H, Akhtar S, et al. Assessing the feasibility of evaluating and delivering a physical activity intervention for pre-school children: a pilot randomised controlled trial. Pilot Feasibility Stud. 2016 Dec;2(1):1–13. doi: 10.1186/s40814-016-0052-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Woynarowska-Sołdan M. Implementation trial of school staff health promotion: Polish experiences. Health Promot Int. 2019 Oct;34(5):e47–58. doi: 10.1093/heapro/day068. [DOI] [PubMed] [Google Scholar]
- 38.Lauria-Horner BA, Kutcher S, Brooks SJ. The feasibility of a mental health curriculum in elementary school. Can J Psychiatry. 2004 Mar;49(3):208–11. doi: 10.1177/070674370404900309. [DOI] [PubMed] [Google Scholar]
- 39.Evans SW, Mullett E, Weist MD, Franz K. Feasibility of the MindMatters school mental health promotion program in American schools. J Youth Adolesc. 2005 Feb;34(1):51–8. [Google Scholar]
- 40.Aydin NG. A national study: School counselor involvement in school, family and community partnerships with linguistically diverse families(Doctoral dissertation, The University of Iowa) July 2011. [Google Scholar]