Abstract
Objectives: This study aimed to compare the marginal fit of temporary restorations fabricated by the conventional chairside method, 3D printing, and milling.
Materials and Methods: In this in vitro, experimental study, 14 temporary restorations were conventionally fabricated over an implant abutment and analog that had been mounted in a phantom model at the site of canine tooth, using auto-polymerizing acrylic resin and putty index. In digital manufacturing, the original model was scanned, and the final restoration was designed. Fourteen temporary restorations were milled out of polymethyl methacrylate (PMMA) blocks, and 14 others were printed by a 3D printer. Temporary crowns were placed on the abutment, and images were obtained from specific areas under a stereomicroscope at x100 magnification to measure the amount of marginal gap. Data were analyzed using one-way ANOVA and Tukey’s test (α=0.05).
Results: The mean marginal gap values for the temporary crowns in the 3D printing, milling, and chairside groups were 91.40, 75.28 and 51.23 µm, respectively. The crowns that were conventionally fabricated chairside exhibited the lowest marginal gap, and the difference in this respect was significant among the three groups (P<0.05).
Conclusion: Temporary crowns fabricated by the chairside method showed significantly smaller marginal gap; however, the marginal gap of all three groups was within the clinically acceptable range.
Key Words: Dental Marginal Adaptation; Printing, Three-Dimensional; Computer-Aided Design; Dental Restoration, Temporary
Introduction
Temporary restorations are fabricated to protect the pulp and periodontium of the prepared teeth, and also to restore esthetics and function [1,2]. In order to achieve these goals, temporary crowns should have optimal contour and precise marginal fit [1,3]. Marginal fit of temporary restorations highly depends on their fabrication technique [1,4]. Temporary crowns can be fabricated directly or indirectly [5,6]. In the direct method, the temporary restoration is fabricated directly on the prepared tooth using a previously made index. However, in the indirect method, the restoration is fabricated on a dental cast and is then transferred into the oral cavity [5]. Although the direct method is faster, it has some drawbacks. For instance, the residual monomer has the potential to irritate the adjacent tissue and cause allergic stomatitis and lichenoid reactions [7,8]. Polymerization shrinkage of acrylic resin is another drawback of the direct method, which would result in marginal, interproximal, and occlusal discrep-ancy [9,10]. Many of these drawbacks can be overcome by indirect fabrication of temporary restorations [5].
The computer-aided design/computer-aided manufacturing (CAD/CAM) technique has been recently employed for the fabrication of temporary restorations [11]. The majority of CAD/CAM systems use a milling machine. In this method, the temporary crown is milled out of resin blocks using burs specifically designed for this purpose [12]. Due to the polymerization of these resin blocks with high degree of conversion, the restorations fabricated by this technology often have higher strength and precision than the directly fabricated restora-tions [13-15]. However, the range of movement and the size of burs can cause some limitations in this technique [12,16].
The additive manufacturing, also known as the 3D printing, can be used to produce 3D objects by laying down successive layers of material. In this method, less material is used than the milling technique. Also, this technology can produce more complex structures compared with the milling technique [12,17,18]. The 3D printing technology can be divided into several groups, depending on the material used. The types commonly used in dentistry include stereo lithography, photopolymer jetting (Poly Jet), and fused deposition modeling [12,15,18]. Digital light processing enables the fabrication of high-resolution restorations [19].
The use of 3D printers for the fabrication of temporary restorations has been previously studied, and only a small number of these studies have assessed the marginal fit of restorations fabricated as such [20-22]. Marginal adaptation of temporary crowns fabricated by different methods has not been well investigated so far. Therefore, this study aimed to compare the marginal gap of temporary restorations fabricated by the conventional chairside method, milling, and 3D printing. The null hypothesis was that no difference would be found in the marginal fit of temporary restorations fabricated by the abovementioned three techniques.
MATERIALS AND METHODS
In this in vitro, experimental study, the sample size was calculated to be 14 in each of the three groups according to a previous study by Mai et al, [2] assuming alpha=0.05, beta=0.1, and power of 90%.
For the fabrication of the original model, an implant fixture analog (SIC lab implant 3.4 mm; SIC invent AG, Basel, Switzerland) was mounted in a phantom model (Dental Typodont model 200; Plutusdental Supply Inc., Orlando, FA, USA) of the maxilla at the site of maxillary right canine. An abutment was then placed over it. This abutment served as a bridge abutment to assess the effect of presence of the adjacent tooth on the accuracy of abutment scanning and fabrication of temporary restoration in interproximal areas. The adjacent lateral incisor was present and the first premolar was missing.
For the fabrication of temporary restorations by the conventional putty (Coltene Iberia S.L. Madrid, Spain) index method, before replacing the canine with an analog and abutment, a putty index was made from the canine tooth. A total of 14 temporary restorations were fabricated on the respective abutment using polymethyl methacrylate (PMMA; GC Tempron, GC America Inc., USA). In order to minimize the polymerization shrink-age, the temporary restoration remained on the abutment and was not removed until the final setting was accomplished.
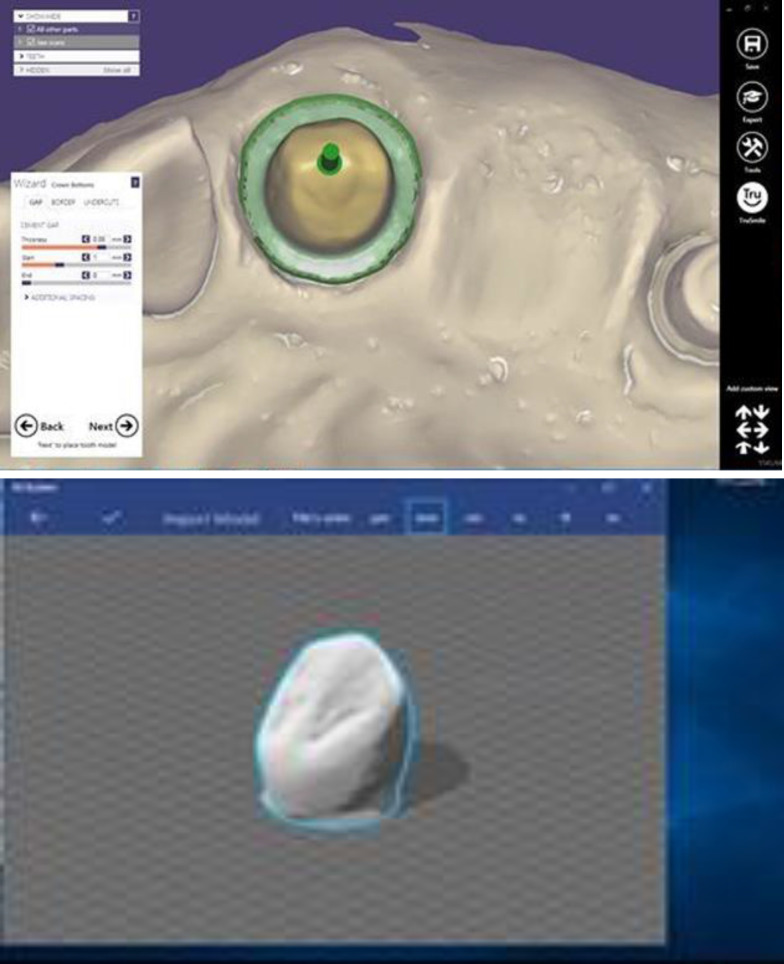
For digital fabrication of temporary restora-tions, the original model was scanned by 3Shape Trios scanner (3Shape Trios; 3Shape, Denmark), and the restoration was finally designed by the Exocad 2016 software (Exocad GmbH, Darmstadt, Germany) (Fig. 1).
Fig. 1.
Temporary restoration design using Exocad
All restorations had the same size, thickness, and design. To match the size with the first group, the sample was first scanned for the fabrication of a pre-op model, and the remaining samples were designed according to this model. The designed files were transferred to a digital light processing printer (Prodent Labx, Product Bonyan Mecatronic, Tabriz, Iran), and the samples were printed using UV resin (Freeprint Temp UV, Detax, Germany) at 385nm wave-length, with 4s of curing for each layer, and post curing for 300 s at 30mw/cm2.
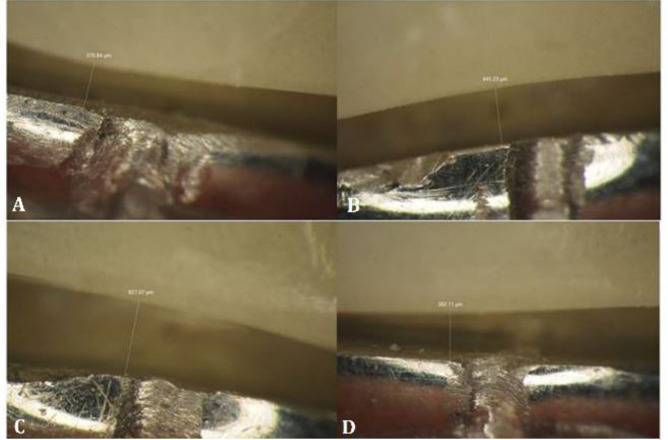
For the last group, the designed files were milled out of PMMA blocks (Yamahachi Dental MFG. Co., Aichi Pref, Japan), using a milling machine (rainbow TM mill, Dentium, South Korea). In order to assess the marginal fit of the crowns, the abutment and fixture were removed from the model and mounted in acrylic resin. Their midbuccal, midpalatal, midmesial and middistal surfaces were then marked by a notch on the finish line of the abutment. Each crown was seated on the abutment, and the amount of marginal gap was measured under a stereomicroscope (SZX16, Olympus, Tokyo, Japan) at ×100 magnification at the marked areas in the buccal, lingual, mesial and distal surfaces. A C-clamp was used to prevent the movement of the crowns during imaging.
A Neubauer chamber with the same magnification was used under the microscope for software scaling and calibration. Finally, the gap at the two sides of the notch was quantified with MIP4 Student software (Nahamin Pardazan Asia, Mashhad, Iran), and mean value was reported as the marginal gap (vertical discrepancy) of the samples in micrometers (µm) (Fig. 2).
Fig. 2.
Stereomicroscopic images showing the marginal gap at ×100 magnification
Data were analyzed using SPSS version 16 (SPSS Inc., IL, USA). The amount of marginal gap was compared among the 3 groups of fabrication of temporary restorations using one-way ANOVA followed by the Tukey’s test for pairwise comparisons (α=0.05).
Results
Table 1 shows the mean, standard deviation, and standard error of the marginal gap in the three groups in micrometers (µm). ANOVA showed a significant difference in marginal gap among the three methods of fabrication of temporary crowns (P<0.05).
Table 1.
Mean and standard deviation (SD) of the marginal gap (µm) in the three groups (n=14)
| Method | Mean | SD |
|---|---|---|
| Milling | 75.28 | 22.14 |
| 3D printing | 91.4 | 36.07 |
| Chairside method | 51.23 | 21.7 |
The Tukey’s post hoc test indicated significant differences between the chairside method and 3D printing (P<0.001).
There were no significant differences between the milling and 3D printing (P=0.278), and milling and chairside methods (P=0.065).
Discussion
This study compared the marginal gap of temporary restorations fabricated by the conventional chairside method with putty index, digital light processing 3D printing, and milling. The results revealed significant differences in marginal gap in the buccal, mesial and distal surfaces among the three groups.
Studies on the efficacy of 3D printing for the fabrication of temporary restorations are limited. Eftekhar Ashtiani et al. [23] assessed the dimensional accuracy of intra-coronal restorations fabricated by the digital and conventional methods, and showed that the conventional resin pattern method was more accurate than 3D printing, which was in agreement with our results. Some factors can affect the marginal fit of restorations fabricated by 3D printing such as type of printer, type of resin, resin and device calibration in terms of environmental moisture and temperature, and complexity of restoration shape [11,24]. Also, restoration preparation design, accuracy of scanning, type of software program, restoration materials, and reproducibility of milling can affect the accuracy of temporary restorations. However, it should be noted that the dimensional accuracy of all restorations in their study and ours was within the clinically acceptable range. The clinically acceptable marginal gap of restorations is reportedly 20 to 150 µm [25-27] . Thus, all these techniques can be successfully used in the clinical setting. Mai et al. [2] assessed the marginal fit of interim crowns fabricated by 3D printing, milling, and selective-pressure impression techniques and reported that 3D printing increased the marginal fit of interim crowns, especially in the occlusal surface. Lee et al. [28] assessed the internal fit of crowns fabricated by 3D printing and CAD/CAM milling machine, and reported that the internal fit and marginal adaptation of interim restorations fabricated by the 3D printing method were higher compared with restorations fabricated by the CAD/CAM milling machine. Peng et al. [22] assessed the internal fit and marginal integrity of temporary crowns made by different manufacturing methods and showed that digitally fabricated temporary crowns had better internal fit and smaller marginal discrepancy. In the study by Mai et al, [2] maximum distortion of crowns occurred in the conventional impression group. They explained that polymerization shrinkage of auto-polymerizing resin was responsible for such a high level of distortion. In this study, we did not remove the putty index and Tempron until the completion of polymerization in order to reduce polymerization shrinkage.
Marginal discrepancy is one problem associated with the fabrication of temporary restorations by the putty index method, which occurs as the result of polymerization shrinkage [29,30]. This problem is more significant in use of PMMA restoration material, and is relatively less common in use of acrylic-based composite resins. The volumetric polymerization shrinkage of acrylic resin is around 6%; it decreases the retention and leads to deformation of restoration [31]. In fabrication of temporary restorations using the CAD/CAM technology, the restorations are milled out of pre-polymerized blocks. Thus, polymerization shrinkage does not occur.
In the milling manufacturing technique, restorations are fabricated by the subtractive manufacturing technique using the cutting burs. Thus, the size of bur and its range of cutting movements can limit the process of fabrication [18]. This technique enables mass production of different forms of restorations by milling pre-polymerized blocks of different materials with variable geometries. Rayyan et al. [32] discussed that the CAD/CAM temporary restorations made from acrylic resin had more accurate margins than restorations made from resin. However, in case of presence of sharp edges and harder surfaces, fabrication of restorations by the milling method would be difficult and may cause some problems. In such conditions, the shape of restorations should be altered to facilitate the milling process. Liu et al. [33] showed that sharp edges, bulges, and depressions cannot be easily fabricated by 3D printing. Also, in restoration milling by the CAD/CAM system, the errors related to the diameter of bur should also be taken into account [34].
All three fabrication techniques tested in this study yielded restorations with clinically acceptable marginal fit. In this study, the methodology adopted for measurement of marginal gap was similar to that of Eftekhar Ashtiani et al [23]. No consensus has been reached on a standard method for measurement of marginal gap. Thus, studies on this topic have reported variable results due to differences in methodologies [35,36].
It should be noted that in vitro studies on marginal fit of temporary restorations often over-estimate the marginal fit of restorations compared with the clinical setting [37]. Factors present in the oral environment such as the saliva, gingival crevicular fluid, blood, patient movement, and space shortage often contribute to inaccuracy and marginal misfit of restorations. These factors also affect prosthetic restorations fabricated by the use of intraoral scanners and CAD/CAM technology. However, digital systems can magnify the scanned teeth on the display monitor and allow for re-scanning of faulty areas to minimize errors in digital impressions. Considering the current findings, clinical trials are required to further confirm the results of this study. On the other hand, other factors such as the mechanical and esthetic properties and cost-effectiveness of 3D printing fabrication technique should be evaluated in the clinical setting. Future studies on a larger sample size are required to assess other types of 3D printers and scanners and their effect on marginal fit of temporary restorations.
CONCLUSION
Within the limitations of this in vitro study, the results showed that the marginal fit of restorations fabricated by all three methods was within the acceptable range. The putty index technique yielded the highest and the 3D printing yielded the lowest marginal fit.
Notes:
Cite this article as: Mohajeri M, Khazaei S, Vafaee F, Firouz F, Ghorbani Gholiabad S, Shisheian A. Marginal Fit of Temporary Restorations Fabricated by the Conventional Chairside Method, 3D Printing and Milling. Front Dent. 2021:18:31.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- 1.Burns DR, Beck DA, Nelson SK, Committee on Research in Fixed Prosthodontics of the Academy of Fixed P. A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: report of the Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. J Prosthet Dent. 2003 Nov;90(5):474–97. doi: 10.1016/s0022-3913(03)00259-2. [DOI] [PubMed] [Google Scholar]
- 2.Mai HN, Lee KB, Lee DH. Fit of interim crowns fabricated using photopolymer-jetting 3D printing. J Prosthet Dent. 2017 Aug;118(2):208–15. doi: 10.1016/j.prosdent.2016.10.030. [DOI] [PubMed] [Google Scholar]
- 3.Gratton DG, Aquilino SA. Interim restorations. Dent Clin North Am. 2004 Apr;48(2):vii,487–97. doi: 10.1016/j.cden.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 4.Mously HA, Finkelman M, Zandparsa R, Hirayama H. Marginal and internal adaptation of ceramic crown restorations fabricated with CAD/CAM technology and the heat-press technique. J Prosthet Dent. 2014 Aug;112(2):249–56. doi: 10.1016/j.prosdent.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 5.Regish KM, Sharma D, Prithviraj DR. Techniques of fabrication of provisional restoration: an overview. Int J Dent. 2011 Jan;2011:134659. doi: 10.1155/2011/134659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vahidi F. The provisional restoration. Dent Clin North Am. 1987 Jul;31(3):363–81. [PubMed] [Google Scholar]
- 7.Michalakis K, Pissiotis A, Hirayama H, Kang K, Kafantaris N. Comparison of temperature increase in the pulp chamber during the polymerization of materials used for the direct fabrication of provisional restorations. J Prosthet Dent. 2006 Dec;96(6):418–23. doi: 10.1016/j.prosdent.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 8.Syed M, Chopra R, Sachdev V. Allergic reactions to dental materials-a systematic review. J Clin Diagn Res. 2015 Oct;9(10):ZE04–9. doi: 10.7860/JCDR/2015/15640.6589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kelvin Khng KY, Ettinger RL, Armstrong SR, Lindquist T, Gratton DG, Qian F. In vitro evaluation of the marginal integrity of CAD/CAM interim crowns. J Prosthet Dent. 2016 May;115(5):617–23. doi: 10.1016/j.prosdent.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 10.Kim SH, Watts DC. Polymerization shrinkage-strain kinetics of temporary crown and bridge materials. Dent Mater. 2004 Jan;20(1):88–95. doi: 10.1016/s0109-5641(03)00101-5. [DOI] [PubMed] [Google Scholar]
- 11.Alharbi N, Osman R, Wismeijer D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J Prosthet Dent. 2016 Jun;115(6):760–7. doi: 10.1016/j.prosdent.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 12.van Noort R. The future of dental devices is digital. Dent Mater. 2012 Jan;28(1):3–12. doi: 10.1016/j.dental.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 13.Park JM, Hong YS, Park EJ, Heo SJ, Oh N. Clinical evaluations of cast gold alloy, machinable zirconia, and semiprecious alloy crowns: A multicenter study. J Prosthet Dent. 2016 Jun;115(6):684–91. doi: 10.1016/j.prosdent.2015.10.018. [DOI] [PubMed] [Google Scholar]
- 14.hamseddine L, Mortada R, Rifai K, Chidiac JJ. Marginal and internal fit of pressed ceramic crowns made from conventional and computer-aided design and computer-aided manufacturing wax patterns: An in vitro comparison. J Prosthet Dent. 2016 Aug;116(2):242–8. doi: 10.1016/j.prosdent.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 15.Stansbury JW, Idacavage MJ. 3D printing with polymers: Challenges among expanding options and opportunities. Dent Mater. 2016 Jan;32(1):54–64. doi: 10.1016/j.dental.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 16.Koch GK, Gallucci GO, Lee SJ. Accuracy in the digital workflow: From data acquisition to the digitally milled cast. J Prosthet Dent. 2016 Jun;115(6):749–54. doi: 10.1016/j.prosdent.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 17.Ebert J, Ozkol E, Zeichner A, Uibel K, Weiss O, Koops U, et al. Direct inkjet printing of dental prostheses made of zirconia. J Dent Res. 2009 Jul;88(7):673–6. doi: 10.1177/0022034509339988. [DOI] [PubMed] [Google Scholar]
- 18.Sun J, Zhang FQ. The application of rapid prototyping in prosthodontics. J Prosthodont. 2012 Dec;21(8):641–4. doi: 10.1111/j.1532-849X.2012.00888.x. [DOI] [PubMed] [Google Scholar]
- 19.Kim SY, Shin YS, Jung HD, Hwang CJ, Baik HS, Cha JY. Precision and trueness of dental models manufactured with different 3-dimensional printing techniques. Am J Orthod Dentofacial Orthop. 2018 Jan;153(1):144–53. doi: 10.1016/j.ajodo.2017.05.025. [DOI] [PubMed] [Google Scholar]
- 20.Berman B. 3-D printing: The new industrial revolution. Bus Horiz. 2012 Mar;55(2):155–62. [Google Scholar]
- 21.Joo HS, Park SW, Yun KD, Lim HP. Complete-mouth rehabilitation using a 3D printing technique and the CAD/CAM double scanning method: a clinical report. J Prosthet Dent. 2016 Jul;116(1):3–7. doi: 10.1016/j.prosdent.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 22.Peng CC, Chung KH, Yau HT. Assessment of the internal fit and marginal integrity of interim crowns made by different manufacturing methods. J Prosthet Dent . 2020 Mar;123(3):514–22. doi: 10.1016/j.prosdent.2019.02.024. [DOI] [PubMed] [Google Scholar]
- 23.Eftekhar Ashtiani R, Nasiri Khanlar L, Mahshid M, Moshaverinia A. Comparison of dimensional accuracy of conventionally and digitally manufactured intracoronal restorations. J Prosthet Dent. 2018 Feb;119(2):233–8. doi: 10.1016/j.prosdent.2017.03.014. [DOI] [PubMed] [Google Scholar]
- 24.Puebla K, Arcaute K, Quintana R, Wicker RB. Effects of environmental conditions, aging, and build orientations on the mechanical properties of ASTM type I specimens manufactured via stereolithography. Rapid Prototyp J. 2012 Jul;18(5):374–88. [Google Scholar]
- 25.Felton DA, Kanoy BE, Bayne SC, Wirthman GP. Effect of in vivo crown margin discrepancies on periodontal health. J Prosthet Dent. 1991 Mar;65(3):357–64. doi: 10.1016/0022-3913(91)90225-l. [DOI] [PubMed] [Google Scholar]
- 26.Sulaiman F, Chai J, Jameson LM, Wozniak WT. A comparison of the marginal fit of In-Ceram, IPS Empress, and Procera crowns. Int J Prosthodont. 1997 Sep;10(5):478–84. [PubMed] [Google Scholar]
- 27.Vanlioglu BA, Evren B, Yildiz C, Uludamar A, Ozkan YK. Internal and marginal adaptation of pressable and computer-aided design/computer-assisted manufacture onlay restorations. Int J Prosthodont. 2012 May;25(3):262–4. [PubMed] [Google Scholar]
- 28.Lee WS, Lee DH, Lee KB. Evaluation of internal fit of interim crown fabricated with CAD/CAM milling and 3D printing system. J Adv Prosthodont. 2017 Aug;9(4):265–70. doi: 10.4047/jap.2017.9.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ehrenberg D, Weiner GI, Weiner S. Long-term effects of storage and thermal cycling on the marginal adaptation of provisional resin crowns: a pilot study. J Prosthet Dent. 2006 Mar;95(3):230–6. doi: 10.1016/j.prosdent.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 30.Nejatidanesh F, Lotfi HR, Savabi O. Marginal accuracy of interim restorations fabricated from four interim autopolymerizing resins. J Prosthet Dent. 2006 May;95(5):364–7. doi: 10.1016/j.prosdent.2006.02.030. [DOI] [PubMed] [Google Scholar]
- 31.Patras M, Naka O, Doukoudakis S, Pissiotis A. Management of provisional restorations' deficiencies: a literature review. J Esthet Restor Dent. 2012 Feb;24(1):26–38. doi: 10.1111/j.1708-8240.2011.00467.x. [DOI] [PubMed] [Google Scholar]
- 32.Rayyan MM, Aboushelib M, Sayed NM, Ibrahim A, Jimbo R. Comparison of interim restorations fabricated by CAD/CAM with those fabricated manually. J Prosthet Dent. 2015 Sep;114(3):414–9. doi: 10.1016/j.prosdent.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 33.Liu Q, Leu MC, Schmitt SM. Rapid prototyping in dentistry: technology and application. Int J Adv Manuf Tech. 2006 Jun;29(3):317–35. [Google Scholar]
- 34.Ortorp A, Jonsson D, Mouhsen A, Vult von Steyern P. The fit of cobalt-chromium three-unit fixed dental prostheses fabricated with four different techniques: a comparative in vitro study. Dent Mater. 2011 Apr;27(4):356–63. doi: 10.1016/j.dental.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 35.Katsoulis J, Mericske-Stern R, Rotkina L, Zbaren C, Enkling N, Blatz MB. Precision of fit of implant-supported screw-retained 10-unit computer-aided-designed and computer-aided-manufactured frameworks made from zirconium dioxide and titanium: an in vitro study. Clin Oral Implants Res. 2014 Feb;25(2):165–74. doi: 10.1111/clr.12039. [DOI] [PubMed] [Google Scholar]
- 36.Park JY, Kim HY, Kim JH, Kim JH, Kim WC. Comparison of prosthetic models produced by traditional and additive manufacturing methods. J Adv Prosthodont. 2015 Aug;7(4):294–302. doi: 10.4047/jap.2015.7.4.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boeddinghaus M, Breloer ES, Rehmann P, Wostmann B. Accuracy of single-tooth restorations based on intraoral digital and conventional impressions in patients. Clin Oral Investig. 2015 Nov;19(8):2027–34. doi: 10.1007/s00784-015-1430-7. [DOI] [PubMed] [Google Scholar]