Abstract
Background
Direct anterior approach total hip arthroplasty (DAA THA) traditionally involves a longitudinal incision, but a bikini incision may improve postoperative scar cosmesis and patient satisfaction while reducing wound complications. This systematic review compares the clinical outcomes and surgical complications in patients undergoing DAA THA via a bikini vs longitudinal incision.
Methods
A Preferred Reporting Items for Systematic Review and Meta-Analyses-compliant search of PubMed, Cochrane, and EMBASE was performed to identify original articles comparing patients undergoing DAA THA via a bikini vs longitudinal incision published from 2010 to 2021. Patient demographic data and postoperative outcomes (scar appearance, patient satisfaction, functional hip scores, and complications) were collected and qualitatively evaluated.
Results
A total of 8 double-armed studies were included, allowing comparison of clinical outcomes of a bikini incision (n = 952) vs a longitudinal incision (n = 1361). Three out of 4 (75.0%) studies comparing postoperative scar appearance and patient satisfaction reported improvements following bikini incision, while 1 study reported comparable results between incision types. Postoperative hip function was similar between incision types in 3 of 4 (75.0%) studies comparing this outcome. Lateral femoral cutaneous nerve injury was the most frequently reported complication following anterior THA, but rates were low overall, and most injuries resolved.
Conclusions
Bikini incision appears to be a safe alternative to the traditional longitudinal incision, with similar functional hip outcomes and potentially improved cosmesis and patient satisfaction while reducing wound complications. Current evidence suggests an elevated risk of lateral femoral cutaneous nerve injury with bikini incision, but this needs to be confirmed in further prospective randomized studies.
Keywords: Total hip arthroplasty, Direct anterior approach, Bikini incision, Oblique incision, Longitudinal incision, Outcomes
Introduction
Total hip arthroplasty (THA) is becoming increasingly common in the United States; the rate of THA procedures doubled from 2000 to 2010, with over 310,000 procedures being performed in patients aged 45 years and older [1]. The annual volume of THA procedures is predicted to increase to 850,000 in 2030, with the highest increase in the 45- to 54-year age group [2]. Recent studies have demonstrated that the direct anterior approach (DAA) for THA is associated with faster recovery, reduced muscle damage, reduced hospital length of stay, and improved postoperative pain and hip function [[3], [4], [5], [6], [7]]. Compared to traditional surgical approaches, the DAA is also associated with lower rates of complications including reoperation, dislocation, and infection [8].
DAA THA traditionally involves a longitudinal incision overlying the tensor fasciae latae, perpendicular to the tension lines of the skin. However, excessive scar formation and poor cosmesis with impaired wound healing can often result [[9], [10], [11]]. Alternatively, the bikini incision runs parallel to the anatomic skin tension lines, often resulting in decreased scar formation and improved cosmesis [12]. The incision is marked in line with the flexion crease approximately 6-8 cm in length, with two-thirds of the incision length being lateral to the anterosuperior iliac spine landmark and one-third medial; the incision and resultant cosmesis has been previously described in detail [13,14]. Both incisions are shown in Figure 1.
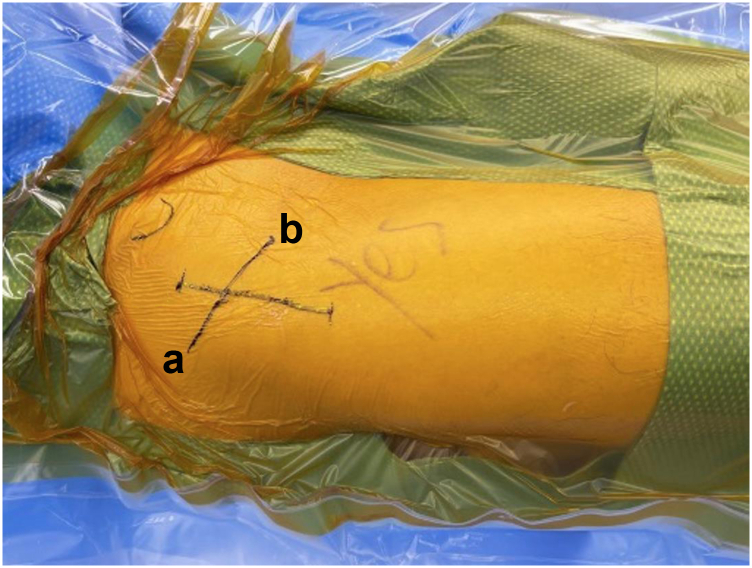
Figure 1.
Longitudinal (a) and bikini (b) incisions. Intraoperative photo of a right hip with anterosuperior iliac spine landmark on the left side of image with the caudal extent of the patient to the right side of image.
DAA with a bikini incision has been introduced fairly recently [12] and is generally utilized by experienced surgeons after achieving proficiency with the traditional anterior approach via a longitudinal incision. Thus, studies reporting the clinical outcomes of a bikini incision THA are limited. This study systematically reviewed the literature comparing clinical outcomes and/or complications of patients who underwent DAA THA via a bikini vs longitudinal incision.
Material and methods
Search protocol
A prospective registered systematic review (PROPSPERO-CRD42021249672) of the literature was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses checklist [15]. A comprehensive search was conducted in the PubMed, Cochrane, and EMBASE databases from January 1, 2010, through August 31, 2021, using an automated search tool (AutoLit; Nested Knowledge, Saint Paul, MN). The specific search strings used for the literature search are listed in Supplementary Table 1.
Study selection
Original studies comparing relevant clinical outcomes for patients who underwent DAA THA (direct anterior or anterior supine intermuscular approach) using a bikini vs longitudinal incision were included. Exclusion criteria were 1) non-English language studies; 2) studies published before January 1, 2010; 3) systematic/narrative reviews and meta-analyses; 4) opinion pieces, editorials, commentaries, letters, technical notes, and abstracts; 5) single-arm studies, case series, or case reports; 6) preclinical (in vitro, cadaveric, or animal) studies; 7) irrelevance to the study topic; and 8) insufficient surgical details (including any study that did not specify incision type).
Data extraction
Baseline data collected included age, sex, and body mass index (BMI, kg/m2). Primary outcomes of interest were scar cosmesis, patient satisfaction, functional hip outcomes, and postoperative complications, including lateral femoral cutaneous nerve (LFCN) injury (inclusive of neuropraxia, dysesthesia, and hypoesthesia), heterotopic ossification (HO), revision, superficial or deep infection, delayed wound healing, fracture, and dislocation. Follow-up period was extracted for each study.
Statistical analysis
This review presents a qualitative synthesis of data obtained from the included studies. Continuous variables, when available, are reported as frequency (count), mean, standard deviation, and range (minimum and maximum). Dichotomous/categorical variables are reported as a discrete number and percentage of subjects for each study arm.
Results
Search results
There were 480 unique studies identified in the literature search. One additional study was included via expert review and recommendation [16]. After screening based on titles/abstracts, 22 studies were selected for full-text review. Fourteen studies were excluded for a lack of comparison arm, irrelevance, not the bikini incision, or full texts unavailable, leaving 8 comparative studies eligible for final inclusion in this qualitative review (Fig. 2) [9,12,[16], [17], [18], [19], [20], [21]].
Figure 2.
Preferred Reporting Items for Systematic Review and Meta-Analyses flow diagram.
These 8 studies included 2 randomized controlled trials (RCTs) [16,21]. Two studies compared a singular complication between the incision types, 1 being HO and the other being LFCN injury [16,19].
Demographic and baseline characteristics
Table 1 summarizes study characteristics and patient demographics. The included studies reported a total of 2313 patients that underwent DAA THA using a bikini (n = 952) vs longitudinal incision (n = 1361). Seven studies reported mean age and sex proportion; in the bikini incision group, mean patient age ranged from 54.3 [20] to 70 [12] years, and the majority of reported patients were female (550/952; 57.8%). In the longitudinal incision group, the mean patient age ranged from 55 [20] to 67.4 [18] years, and the majority of reported patients were female (620/1132; 54.8%). Mean BMI data were available in 6 studies and ranged from 23.2 [16] to 25.6 [9] in the bikini group and from 23.8 [20] to 28 [12] in the longitudinal group.
Table 1.
Summary of studies included in the systematic review.
| Author, year | Study type | Incision type | Sample size | Sex (female) | Mean age (y) | Mean BMI (kg/m2) |
|---|---|---|---|---|---|---|
| Leunig et al., 2013 [12] | Retrospective cohort | Bikini | 26 | 20 (76.9) | 70.0 | 25.0 |
| Longitudinal | 33 | 10 (30.3) | 66.0 | 28.0 | ||
| Leunig et al., 2018 [9] | Retrospective cohort | Bikini | 398 | 227 (57.0) | 66.0 | 25.6 |
| Longitudinal | 556 | 256 (46.0) | 67.0 | 25.8 | ||
| Manrique et al., 2019 [17] | Retrospective case-control | Bikini | 86 | 76 (88.4) | 61.9 | 25.3 |
| Longitudinal | 230 | 200 (86.9) | 63.3 | 26.1 | ||
| Menzies-Wilson et al., 2020 [18] | Retrospective cohort | Bikini | 90 | 33 (36.7) | 65.5 | NR |
| Longitudinal | 124 | 54 (43.5) | 67.4 | NR | ||
| Rüdiger et al., 2020 [19] | Retrospective cohort | Bikini | 172 | 88 (51.2) | NR | NR |
| Longitudinal | 229 | NR | NR | NR | ||
| Sang et al., 2021 [16] | RCT | Bikini | 99 | 67 (67.7) | 60.7 | 23.2 |
| Longitudinal | 96 | 63 (65.6) | 61.4 | 24.7 | ||
| Wang et al., 2021a [20] | Retrospective cohort | Bikini | 32 | 16 (50.0) | 54.3 | 25.0 |
| Longitudinal | 43 | 18 (41.9) | 55.0 | 23.8 | ||
| Wang et al., 2021b [21] | RCT | Bikini | 49 | 23 (46.9) | 56.8 | 24.3 |
| Longitudinal | 50 | 19 (38.0) | 55.9 | 24.2 |
NR, not reported; RCT, Randomized controlled trial.
Data presented as frequency (n) or n (%).
Wound healing
Two studies compared wound healing between patients with bikini vs longitudinal incision following DAA THA [17,21]. A comparative study by Manrique et al. found that patients with bikini incisions (2.3%, 2/86) had lower rates of delayed wound healing than those with longitudinal incisions (6.1%, 14/230) at 20 days postoperatively although the difference was not found to be significant (P = .09) [17]. In patients with BMI >30 kg/m2, the difference in delayed wound healing was significant (bikini 0% [0/16] vs longitudinal 16.6% [8/48]; P < .05) [17]. Another recent RCT by Wang et al. found there was an increase in delayed wound healing with a longitudinal incision (12.0% [6/50]; P = .123) vs bikini (2.0% [1/49]) at 2 weeks postoperatively; however, this was not statistically significant [21]. Additional details are in Table 2.
Table 2.
Wound healing, cosmesis, and functional outcomes of included studies.
| Author, y | Follow-up (mo) | Would healing & scar cosmesis | Functional hip outcome |
|---|---|---|---|
| Leunig et al., 2013 [12] | 6 | NRS: similar between groups | WOMAC: similar scores; |
| Objective evaluation: narrower (P = .002) and shorter (P = .009) scars in bikini group. | OHS: similar scores (longitudinal 19.4 vs bikini 16.9; P = .240); | ||
| UCLA: similar scores (longitudinal 6.4 vs bikini 6.2; P = .516). | |||
| Leunig et al., 2018 [9] | 24-48 | UNC4P: lower mean total score in bikini group (P = .01); | OHS: similar between groups (longitudinal 45.3 ± 5.1 vs bikini 46.1 ± 3.9; P = .41). |
| Scar cosmesis: higher rate of “very satisfied” patients in the bikini group (P < .001). | |||
| Manrique et al., 2019 [17] | 6 | PSAS or the Vancouver scale: similar between groups. | NR |
| Menzies-Wilson et al., 2020 [18] | 6-24 | NR | OHS: lower in bikini group at 6 mo (longitudinal 36.2 ± 5.66 vs bikini 32.9 ± 4.56; P < .001); |
| Overall change in OHS: similar between groups at 6 mo. | |||
| Rüdiger et al., 2020 [19] | 3 | NR | NR |
| Sang et al., 2021 [16] | 6 | NR | NR |
| Wang et al., 2021a [20] | 3 | NR | OHS: |
| 1 mo (longitudinal 32.8 ± 4.1 vs bikini 31.7 ± 4.4), | |||
| 3 mo (longitudinal 43.1 ± 3.4 vs bikini 41.3 ± 4.3); | |||
| UCLA: | |||
| 1 mo (longitudinal 4.6 ± 0.8 vs bikini 4.8 ± 0.9), | |||
| 3 mo (longitudinal 6.2 ± 0.7 vs bikini 6.2 ± 0.5). | |||
| Wang et al., 2021b [21] | 6 | SCAR score: lower in bikini group (longitudinal 9.3 ± 2.0 vs bikini incision 7.4 ± 1.8; P < .001) | OHS: similar between groups (longitudinal vs bikini) |
| Satisfaction: higher in bikini group (longitudinal 38%, 19/50 vs bikini 63.3%, 31/40; P = .013). | 1 mo (32.3 ± 4.2 vs 32.1 ± 4.7; P = .880), 3 mo (42.2 ± 4.1 vs 42.0 ± 4.4; P = .854) |
||
| 6 mo (45.8 ± 1.6 vs 46.2 ± 1.1; P = .222) | |||
| UCLA: similar between groups (longitudinal vs bikini) | |||
| 1 mo (4.6 ± 0.8 vs 4.6 ± 0.6; P = .991) | |||
| 3 mo (6.2 ± 0.6 vs 6.1 ± 0.5; P = .836) | |||
| 6 mo (6.8 ± 0.7 vs 7.0 ± 0.5; P = .283) |
HHS, Harris Hip score; NR, not reported; NRS, Numeric Rating Scale; PSAS, Patient and Observer Scar Assessment Scale; SCAR, Scar cosmesis assessment & rating scale; UNC4P, The University of North Carolina “4P” scar scale.
Scar cosmesis
A total of 4 studies compared postoperative scar cosmesis and patient satisfaction among patients with bikini or longitudinal incision, 3 of which reported significant improvements in the bikini incision group and 1 reported high levels of satisfaction in both groups. An RCT by Wang et al. involving 100 patients (49 bikini; 50 longitudinal; 1 patient lost to follow-up) demonstrated that those with a bikini incision had significantly reduced Scar Cosmesis Assessment & Rating scale scores (bikini 7.4 ± 1.8 vs longitudinal 9.3 ± 2.0; P < .001) with more patients reporting moderate to high levels of satisfaction with the scar appearance (bikini 16.3% [8/49] vs longitudinal 10.0% [5/50]; P = .013) at 6-month follow-up [21]. Leunig et al. conducted a retrospective study of patients who underwent DAA THA (26 bikini; 33 longitudinal) and found that patients with bikini incision demonstrated improved subjective ratings related to scar cosmesis at 6 months compared to those with a longitudinal incision [12]. Moreover, the bikini incision group had shorter and narrower scars [12]. In a long-term study, Leunig et al. followed up 964 patients (398 bikini; 556 longitudinal) after DAA THA with up to 4-year follow-up, finding that patients in the bikini incision group had a lower mean University of North Carolina “4P” scar scale total score (bikini 0.2 vs longitudinal 0.4; P = .01), a lower incidence of peri-incisional numbness (7.5% vs 14.5%; P < .001), and more patients categorized as “very satisfied” with the scar (P < .001) than the longitudinal incision group [9].
In contrast, a case-control study of DAA THA (86 bikini; 230 longitudinal) investigated patient-reported scar cosmesis using either the Patient Scar Assessment Scale (bikini mean = 10, range 6-32 vs longitudinal mean = 11, range 6-32; P = .44) or the Vancouver Scale (bikini mean = 6, range 0-12 vs longitudinal mean = 7, range 0-13; P = .26) and found no significant difference in patient satisfaction between the 2 incision groups [17]. There were high levels of satisfaction in both groups with over 90% of patients reporting satisfactory appearance of the scar at 6 months [17]. Additional details are in Table 2.
Functional outcomes
Four studies directly compared postoperative functional hip outcomes between the bikini and longitudinal incisions [9,12,18,21], all of which reported no statistical functional difference. Wang et al. conducted an RCT involving 100 patients (49 bikini; 50 longitudinal; 1 patient lost to follow-up) and reported no significant difference in postoperative Oxford Hip Scores (OHS) or University of California Los Angeles (UCLA) activity-level rating scores when comparing bikini (OHS: 46.2 ± 1.1; UCLA: 7.0 ± 0.5) and longitudinal (OHS: 45.8 ± 1.6; UCLA: 6.8 ± 0.7) groups at 6 months (P = .222 and P = .283, respectively) [21]. Similarly, Leunig et al. reported no significant difference in either OHS, UCLA, or the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score between bikini (OHS: 16.9; UCLA: 6.2; WOMAC function: 11.0) and longitudinal (OHS: 19.4; UCLA: 6.5; WOMAC function: 9.1) incision groups at 6 months (P = .240) [12]. A similar finding was reported in a long-term follow-up study by Leunig et al. reporting no significant difference in 2- to 4-year postoperative OHS between bikini (46.1 ± 3.9) and longitudinal (45.3 ± 5.1; range 0-48) incision groups (P = .41) [9]. In contrast, a retrospective analysis by Menzies-Wilson et al. reported a statistically significant difference in 6-month OHS between bikini (n = 90) and longitudinal (n = 124) incision groups (32.89 ± 4.56 vs 36.2 ± 5.66, P = .000) [18]. However, overall change in the OHS was not statistically significant (bikini incision: 10.9 ± 6.4 vs longitudinal: 12.8 ± 6.6; P = .068) and was not considered clinically significant [18]. A retrospective study by Wang et al. reported improvement in functional hip outcomes over time in both incision types but made no conclusion as to the superiority of one over the other [20]. Additional details are in Table 2.
LFCN injury
LFCN injury was assessed in 6 studies [9,12,16,17,20,21], of which 5 studies compared LFCN injury among patients with bikini and longitudinal incisions [9,12,16,17,21]. A recent prospective randomized study of 99 bikini and 96 longitudinal incision DAA THA patients reported a significantly higher incidence of LFCN injury in the bikini group compared to the longitudinal group at 1.5 months postoperatively (36.4% [36/99] vs 21.9% [21/96], P < .05) [16]. However, the symptoms resolved over time, and at 6 months, there was no significant difference in the proportion of patients with LFCN symptoms between the incision types (bikini 7.1% [7/99] vs longitudinal 4.2% [4/96]; P = .380) [16]. Similarly, another RCT that compared outcomes between the bikini and longitudinal incision groups following DAA THA reported a higher incidence of LFCN dysesthesia in the bikini incision group (28.6%, 14/49) vs the longitudinal incision group (14.0%, 7/50) although this difference was not statistically significant (P = .076) [21]. Conversely, 2 retrospective studies reported no significant difference in the rates of postoperative LFCN injury between the 2 incision types [12,17]. Interestingly, a retrospective study by Leunig et al. (2018) found that patients with bikini incision had lower rates of LFCN hypoesthesia (P < .001) than those with longitudinal incision [9]. Additional details are in Table 3.
Table 3.
Complications reported in included studies.
| Author, y | Follow-up (mo) | Complications |
|---|---|---|
| Leunig et al., 2013 [12] | 6 | LFCN dysesthesia: similar rates (longitudinal 23% vs bikini 16%; P = .25) |
| LFCN hypesthesia: similar rates (longitudinal 60.6% vs bikini 61.5%; P = .942) | ||
| Leunig et al., 2018 [9] | 24-48 | LFCN hypoesthesia: lower rate in the bikini group (longitudinal 14.5% vs bikini 7.5%; P < .001) |
| HO: similar rates (P = .311) | ||
| Revision: similar rates (longitudinal 2.3%, 13/556 vs bikini 1.5%, 6/398). | ||
| Manrique et al., 2019 [17] | 6 | LFCN dysesthesia: similar rates (longitudinal 3.0%, 7/23 vs bikini 2.3%, 2/86; P = .37); |
| Delayed wound healing: similar rates at 20 d (longitudinal 6.1% vs bikini 2.3%; P = .37). | ||
| Menzies-Wilson et al., 2020 [18] | 6-24 | Superficial wound infection: “clinically irrelevant differences” between groups at 24 mo (longitudinal 0.8% vs bikini 1.1%). |
| Rüdiger et al., 2020 [19] | 3 | HO: lower incidence of Brooker grade 3-4 HO in bikini group (longitudinal 11.8%, 27/229 vs bikini 4.0%, 7/172; P = .00011); no Brooker grade 4 HO in bikini group. |
| Sang et al., 2021 [16] | 6 | LFCN injury: |
| 1.5 mo Higher rates in bikini group (longitudinal 21.9%, 23/96 vs bikini 36.4%, 36/99; P = .026) | ||
| 6 mo Similar rates (longitudinal 4.2%, 4/96 vs bikini 7.1%, 7/99; P = .380) | ||
| Wang et al., 2021a [20] | 3 | LFCN dysesthesia: longitudinal 14.0%, 6/43 vs bikini 15.6%, 5/32 |
| Venous thromboembolism: longitudinal 2.3%, 1/43 vs bikini 3.1%, 1/32 | ||
| Wang et al., 2021b [21] | 6 | LFCN injury: similar rates between groups; |
| Delayed wound healing: similar rates; | ||
| Infection: similar rates; | ||
| Venous thromboembolism: similar rates. |
NR, not reported.
Heterotopic ossification
Two studies directly compared the rate of severe HO (grade 3-4) between incision types [9,19]. Rudiger et al. retrospectively reviewed 401 THA patients (172 bikini; 229 longitudinal) to compare the incidence and severity of HO using the Brooker grade to evaluate anteroposterior and lateral radiographs at 3 months postoperatively [19]. Patients with a bikini incision demonstrated a significantly less Brooker grade 3/4 HO (4.0%, 7/172) than those with the longitudinal incision (11.8%, 27/229). Incision type did not affect functional outcomes in this study but significantly influenced the incidence of HO (P = .00013), which was independent of the surgeon’s experience [19]. Leunig et al. reported similar rates of HO between the incision types (P = .311); the rates of HO with Brooker ≥2 were 2.5% in the bikini and 6.7% in the longitudinal incision groups, which did not impact the OHS (P = .450) or result in additional surgery [9]. Additional details are in Table 3.
Reoperation and implant survival
Two studies compared revision rates between incision groups [9,17]. Leunig et al. reported no significant difference between bikini incision (1.5%, 6/398) and longitudinal incision (2.3%, 13/556) (P = .911) [9]; the reasons cited for revisions included dislocation, leg length discrepancy, and periprosthetic fracture. Manrique et al. reported 1 incidence of reoperation (0.4%, 1/230) in patients with bikini incision THA attributed to an acute periprosthetic joint infection [17]. Additional details are in Table 3.
Discussion
This study systematically reviewed clinical evidence reporting postoperative outcomes and complications following DAA THA using a bikini incision, finding that bikini incisions may result in improved scar cosmesis and decreased wound healing complications, without compromised hip functionality or reoperation rates. However, data reporting surgical complications of the bikini incision THA were heterogeneous and limited the ability to draw conclusions. These results indicate that bikini incision for THA should be further explored as an alternative to the traditional longitudinal incision.
A traditional longitudinal skin incision is performed perpendicular to the anatomic skin creases, resulting in increased skin edge tension and scar widening; however, an oblique bikini incision follows Langer’s lines and may lead to a narrower scar and improved appearance [12]. The improved wound healing observed among patients with bikini incisions is thought to be related to reduced tension around the skin edges of the incision compared to the traditional longitudinal incision, which causes constant tension around the skin edges [12,22]. In the 4 studies that compared postoperative scar appearance and patient satisfaction in this review, each used a different assessment method to evaluate scar appearance [9,12,17,21]. Additionally, these studies reported follow-up times ranging from 6 months [9,12] to 2-4 years [9], so it is difficult to draw strong conclusions about the potential benefits of the bikini incision for scar cosmesis. Taken together, however, the results of this review suggest benefits with the bikini incision in improving the postoperative appearance of the scar and improved scar-related satisfaction in patients following DAA THA. For reference, Figure 3 demonstrates 3-month scar appearances performed by the same author (B.N.).
Figure 3.
Longitudinal and bikini scars at 3 months performed by the same surgeon.
The relationship between bikini incision and risk of LFCN injury remains somewhat contested. Most of the retrospective studies included in this review demonstrated that the rate of LFCN injury following DAA THA did not vary significantly between patients with longitudinal and bikini incisions [12,17] although 2 included RCTs indicated that early LFCN outcomes were worse for bikini incision patients [16,21]. While the exact mechanism is unclear, bikini incision may raise the risk of injury to the LFCN branches due to greater medial extension over the tensor fasciae latae and reduced intraoperative field, sometimes requiring more forceful retraction [9,21,23]. Interestingly, evidence shows that LFCN symptoms improve significantly and spontaneously with time [[24], [25], [26], [27]], so early LFCN injury may not ultimately be an important indicator of surgical success. Further study of these outcomes in larger prospective trials is warranted.
THA is considered a reliable and valuable treatment. However, complications such as component loosening, instability, fracture, and leg length discrepancy may lead to revision surgery [22,28]. Unfortunately, few studies included in this review reported the specific complications leading to revision, making meaningful reoperation comparisons difficult. The only included study that directly compared revision rates between the 2 incision types reported minimal rates of leg length discrepancy, periprosthetic fracture, and dislocation [9]. The data remain unclear whether there is a difference in revision rates between the 2 incisions.
It is important to note that the clinical outcomes as well as the rate of postoperative complications of DAA THA, including revisions, are typically higher with surgeons in the initial stages of experience with a given technique. There is a steep learning curve for DAA THA, with 1 study noting that at least 50 procedures are required to obtain revision rates similar to those achieved by experienced surgeons [29,30]. Thus, outcome and complication data should be interpreted considering the experience of the surgeon performing the THA procedure. Additionally, Leunig et al. recommend that the oblique bikini incisions should be utilized only after mastering the DAA approach using the traditional longitudinal incision and in appropriately selected patients [9,12]. This strategy likely ensures that patients receive the most appropriate treatment while minimizing complications. The anterior approach of obtaining femoral exposure traditionally can be more difficult without the proper releases and appropriate incision placement. Figure 4 demonstrates adequate exposure during femoral preparation performed by the same author (C.D.) utilizing the bikini and longitudinal incisions. Another consideration with the bikini incision is distal and proximal extensibility; particularly, how to address intraoperative complications or when needed in complex primary or revision scenarios. Unfortunately, the limited data addressing this issue are purely anecdotal.
Figure 4.
Longitudinal and bikini femoral preparation performed by same surgeon demonstrating adequate exposure for femoral instrumentation.
Limitations
The primary limitation of this review was the small number of relevant studies identified for evaluation. There are few articles that discuss bikini incision with THA, so further study is needed to validate the results of this review and draw comparisons between bikini and longitudinal incisions. All the included studies were single-center studies, and the majority were also single-surgeon studies, which inherently limits the generalizability of the results. The rate of complications and outcomes is dependent on the experience of each surgeon with DAA THA and their preferences for a particular incision, but these factors could not be accounted for in this review. Additionally, many of the studies were retrospective in nature. Various assessments utilized patient-reported outcomes, which are subject to response style bias. Considerable heterogeneity existed among the studies regarding patient follow-up and data collection tools, preventing an appropriate meta-analysis assessment with inferential statistics.
Conclusions
Evidence suggests that the bikini incision utilized during the DAA THA may be associated with considerable improvement in scar cosmesis with increased patient satisfaction compared to the traditional longitudinal incision, with little to no observed differences in postoperative functional hip outcomes. A greater incidence of LFCN injury may be associated with bikini incision although symptoms can improve over time. Overall, limited and highly heterogeneous studies make it difficult to thoroughly compare bikini and longitudinal incisions; therefore, further prospective randomized studies are warranted.
Conflict of interest
Dr. Charles DeCook receives royalties from DePuy Synthes and is in the speakers’ bureau of or gave paid presentations for DePuy Synthes, Medtronic, and Mizuho.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2022.06.010.
Acknowledgments
The authors acknowledge Superior Medical Experts and Geeta Paranjape, PhD, for their assistance with literature research and manuscript drafting.
Appendix A. Supplementary Data
References
- 1.Wolford M.L.P.K., Bercovitz A. National Center for Health Statistics; Hyattsville, MD: 2015. Hospitalization for total hip replacement among inpatients aged 45 and over: United States, 2000–2010. NCHS data brief, no 186. [PubMed] [Google Scholar]
- 2.Singh J.A., Yu S., Chen L., Cleveland J.D. Rates of total joint replacement in the United States: future projections to 2020-2040 using the national inpatient sample. J Rheumatol. 2019;46:1134–1140. doi: 10.3899/jrheum.170990. [DOI] [PubMed] [Google Scholar]
- 3.Miller L.E., Gondusky J.S., Bhattacharyya S., Kamath A.F., Boettner F., Wright J. Does surgical approach affect outcomes in total hip arthroplasty through 90 days of follow-up? A systematic review with meta-analysis. J Arthroplasty. 2018;33:1296–1302. doi: 10.1016/j.arth.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 4.Taunton M.J., Mason J.B., Odum S.M., Springer B.D. Direct anterior total hip arthroplasty yields more rapid voluntary cessation of all walking aids: a prospective, randomized clinical trial. J Arthroplasty. 2014;29(9 Suppl):169–172. doi: 10.1016/j.arth.2014.03.051. [DOI] [PubMed] [Google Scholar]
- 5.Martin C.T., Pugely A.J., Gao Y., Clark C.R. A comparison of hospital length of stay and short-term morbidity between the anterior and the posterior approaches to total hip arthroplasty. J Arthroplasty. 2013;28:849–854. doi: 10.1016/j.arth.2012.10.029. [DOI] [PubMed] [Google Scholar]
- 6.Taunton M.J., Trousdale R.T., Sierra R.J., Kaufman K., Pagnano M.W. John charnley award: randomized clinical trial of direct anterior and miniposterior approach THA: which provides better functional recovery? Clin Orthop Relat Res. 2018;476:216–229. doi: 10.1007/s11999.0000000000000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao H.Y., Kang P.D., Xia Y.Y., Shi X.J., Nie Y., Pei F.X. Comparison of early functional recovery after total hip arthroplasty using a direct anterior or posterolateral approach: a randomized controlled trial. J Arthroplasty. 2017;32:3421–3428. doi: 10.1016/j.arth.2017.05.056. [DOI] [PubMed] [Google Scholar]
- 8.Miller L.E., Gondusky J.S., Kamath A.F., Boettner F., Wright J., Bhattacharyya S. Influence of surgical approach on complication risk in primary total hip arthroplasty. Acta Orthop. 2018;89:289–294. doi: 10.1080/17453674.2018.1438694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leunig M., Hutmacher J.E., Ricciardi B.F., Impellizzeri F.M., Rudiger H.A., Naal F.D. Skin crease ‘bikini’ incision for the direct anterior approach in total hip arthroplasty: a two- to four-year comparative study in 964 patients. Bone Joint J. 2018;100-B:853–861. doi: 10.1302/0301-620X.100B7.BJJ-2017-1200.R2. [DOI] [PubMed] [Google Scholar]
- 10.Christensen C.P., Karthikeyan T., Jacobs C.A. Greater prevalence of wound complications requiring reoperation with direct anterior approach total hip arthroplasty. J Arthroplasty. 2014;29:1839–1841. doi: 10.1016/j.arth.2014.04.036. [DOI] [PubMed] [Google Scholar]
- 11.Jahng K.H., Bas M.A., Rodriguez J.A., Cooper H.J. Risk factors for wound complications after direct anterior approach hip arthroplasty. J Arthroplasty. 2016;31:2583–2587. doi: 10.1016/j.arth.2016.04.030. [DOI] [PubMed] [Google Scholar]
- 12.Leunig M., Faas M., von Knoch F., Naal F.D. Skin crease 'bikini' incision for anterior approach total hip arthroplasty: surgical technique and preliminary results. Clin Orthop Relat Res. 2013;471:2245–2252. doi: 10.1007/s11999-013-2806-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Corten K., Holzapfel B.M. Direct anterior approach for total hip arthroplasty using the “bikini incision”. Oper Orthop Traumatol. 2021;33:318–330. doi: 10.1007/s00064-021-00721-y. [DOI] [PubMed] [Google Scholar]
- 14.Berry D.J., Lieberman J. Elsevier Health Sciences; Philadelphia, PA: 2019. Surgery of the hip E-book. [Google Scholar]
- 15.Page M.J., Moher D., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. doi: 10.1136/bmj.n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sang W., Xue S., Xu Y., Liu Y., Zhu L., Ma J. Bikini incision increases the incidence of lateral femoral cutaneous nerve injury in direct anterior approach hip arthroplasty: a prospective ultrasonic, electrophysiological, and clinical study. J Arthroplasty. 2021;36:3463–3470. doi: 10.1016/j.arth.2021.05.012. [DOI] [PubMed] [Google Scholar]
- 17.Manrique J., Paskey T., Tarabichi M., Restrepo C., Foltz C., Hozack W.J. Total hip arthroplasty through the direct anterior approach using a bikini incision can be safely performed in obese patients. J Arthroplasty. 2019;34:1723–1730. doi: 10.1016/j.arth.2019.03.060. [DOI] [PubMed] [Google Scholar]
- 18.Menzies-Wilson R., Marino I.T., Mahalingham K., Field R. Functional outcomes of direct anterior approach hip arthroplasty: oblique ‘bikini’ versus longitudinal skin incision. J Orthop Trauma Rehabilitation. 2020;27:52. [Google Scholar]
- 19.Rudiger H.A., Dittrich M., Robinson J., Mansour T., Schwab T., Stadelmann V.A., et al. The impact of heterotopic ossification on self-reported outcomes after total hip arthroplasty using the direct anterior approach. J Bone Joint Surg Am. 2020;102(Suppl 2):91–98. doi: 10.2106/JBJS.20.00071. [DOI] [PubMed] [Google Scholar]
- 20.Wang Q., Yang Y., Yang Z., Hu Y., Zhao X., Chen C., et al. Analgesic effects of ultrasound-guided iliohypogastric/ilioinguinal nerve block combined with lateral femoral cutaneous nerve block in total hip arthroplasty via direct anterior approach: a retrospective cohort study. Orthop Surg. 2021;13:920–931. doi: 10.1111/os.12795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang Q., Yue Y., Yang Z., Chen L., Li Q., Kang P. Comparison of postoperative outcomes between traditional longitudinal incision and bikini incision in total hip arthroplasty via direct anterior approach: a randomized controlled trial. J Arthroplasty. 2021;36:222–230. doi: 10.1016/j.arth.2020.07.047. [DOI] [PubMed] [Google Scholar]
- 22.Lee G.C., Marconi D. Complications following direct anterior hip procedures: costs to both patients and surgeons. J Arthroplasty. 2015;30(9 Suppl):98–101. doi: 10.1016/j.arth.2015.03.043. [DOI] [PubMed] [Google Scholar]
- 23.Rudin D., Manestar M., Ullrich O., Erhardt J., Grob K. The anatomical course of the lateral femoral cutaneous nerve with special attention to the anterior approach to the hip joint. J Bone Joint Surg Am. 2016;98:561–567. doi: 10.2106/JBJS.15.01022. [DOI] [PubMed] [Google Scholar]
- 24.Ozaki Y., Homma Y., Baba T., Sano K., Desroches A., Kaneko K. Spontaneous healing of lateral femoral cutaneous nerve injury and improved quality of life after total hip arthroplasty via a direct anterior approach. J Orthop Surg (Hong Kong) 2017;25 doi: 10.1177/2309499016684750. 2309499016684750. [DOI] [PubMed] [Google Scholar]
- 25.Patton R.S., Runner R.P., Lyons R.J., Bradbury T.L. Clinical outcomes of patients with lateral femoral cutaneous nerve injury after direct anterior total hip arthroplasty. J Arthroplasty. 2018;33:2919–2919.e1. doi: 10.1016/j.arth.2018.04.032. [DOI] [PubMed] [Google Scholar]
- 26.Nizam I., Alva A., Gogos S. The bikini incision anterior cemented total hip arthroplasty: assessment of radiological and clinical outcomes - a mid-term review. SICOT-J. 2021;7:3. doi: 10.1051/sicotj/2020050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alva A., Nizam I., Gogos S. Minimizing complications in bikini incision direct anterior approach total hip arthroplasty: a single surgeon series of 865 cases. J Exp Orthop. 2021;8:1. doi: 10.1186/s40634-020-00318-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eto S., Hwang K., Huddleston J.I., Amanatullah D.F., Maloney W.J., Goodman S.B. The direct anterior approach is associated with early revision total hip arthroplasty. J Arthroplasty. 2017;32:1001–1005. doi: 10.1016/j.arth.2016.09.012. [DOI] [PubMed] [Google Scholar]
- 29.de Steiger R.N., Lorimer M., Solomon M. What is the learning curve for the anterior approach for total hip arthroplasty? Clin Orthop Relat Res. 2015;473:3860–3866. doi: 10.1007/s11999-015-4565-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meermans G., Konan S., Das R., Volpin A., Haddad F.S. The direct anterior approach in total hip arthroplasty: a systematic review of the literature. Bone Joint J. 2017;99-B:732–740. doi: 10.1302/0301-620X.99B6.38053. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.