Abstract
Loa loa microfilariae were found on thick blood smears (TBSs) from 8 of 300 (2.7%) residents of Bioko Island, Equatorial Guinea, during a Plasmodium falciparum sporozoite malaria vaccine clinical trial. Only one subject was found to have microfilaraemia on his first exam; parasites were not discovered in the other seven until subsequent TBSs were performed, at times many weeks into the study. All infected individuals were asymptomatic, and were offered treatment with diethylcarbamazine, per national guidelines. L. loa microfilaraemia complicated the enrolment or continued participation of these eight trial subjects, and only one was able to complete all study procedures. If ruling out loiasis is deemed to be important during clinical trials, tests that are more sensitive than TBSs should be performed.
Keywords: Loa loa, loiasis, malaria vaccine, microfilaraemia, microfilaria
Introduction
The filarial nematode Loa loa is common in West and Central Africa, with a reported prevalence of >20% on Bioko Island, Equatorial Guinea.1 Other than causing Calabar swellings2 and eye worm,3 loiasis has generally been regarded as a chronic, largely asymptomatic infection. However, serious cardiac, renal, pulmonary and neurologic complications have been reported4 and evidence suggests that high levels of L. loa microfilaraemia may be associated with an increase in all-cause mortality.5 Loiasis is of particular concern in areas endemic for onchocerciasis and lymphatic filariasis, since ivermectin used in mass treatment programs can cause potentially fatal encephalopathy in people with high levels of L. loa microfilaraemia.6 The World Health Organization recommends diethylcarbamazine (DEC) as the first-line treatment for loiasis,7 but it too can cause severe encephalopathy in patients with hypermicrofilaraemia.8,9 We report eight cases of asymptomatic L. loa microfilaraemia occurring in adult subjects in a clinical trial of two Plasmodium falciparum sporozoite (PfSPZ) malaria vaccines on Bioko Island, Equatorial Guinea, and the impact this had on the study.
Patients
Giemsa-stained thick blood smears (TBSs) were examined from 300 Equatoguinean residents of Bioko Island ages 6 months–65 y during a clinical trial of two malaria vaccines,10 the radiation-attenuated PfSPZ vaccine10–14 and the chemo-attenuated PfSPZ-CVac (PfSPZ chemoprophylaxis vaccine).15 Written informed consent was obtained from all study participants. Venous blood for TBSs was drawn at screening visits prior to enrolment in the trial and 5–20 additional times (depending on study group) during the subsequent vaccination and follow-up period in order to assess for malaria parasitaemia. Blood samples were generally drawn between 10:00 h and 14:00 h, which corresponds to the period of highest sensitivity for L. loa microfilaria detection.9L. loa microfilariae were found in 8 of 300 (2.7%) subjects tested (0 of 152 subjects ages 6 months–17 y and 8 of 148 subjects ages 18–65 y). Details of the eight cases are displayed in Table 1. All individuals with L. loa microfilaraemia were adults; there were seven males and one female, ranging in age from 21 to 61 y (median 24.5). All were asymptomatic and had unremarkable physical exams. Microfilariae (see Figure 1) were detected in one of the affected individuals (patient 4) on his first TBS, but were not seen in the other seven until their second (n=2), third (n=2), fifth (n=1), sixth (n=1) or fourteenth (n=1) (median 3) blood smears, 2–35 weeks (median 11.5) after the initial negative smear.
Table 1.
Characteristics and outcomes of eight cases of asymptomatic L. loa microfilaraemia in a malaria vaccine trial in Equatorial Guinea.
| Patient number | Gender | Age (years) | Number of smears before microfilariae detected | Microfilariae/mL at time of initial detection | qPCR at time of initial microscopic detection | Eosinophil count at time of initial detection (×103/mm3) | Treatment | Eosinophil count post-treatment (×103/mm3) | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 21 | 2 | 2500 | Positive | 0.81 | DEC ×2 | – | Cleared microfilariae |
| 2 | M | 61 | 3 | 3000 | Positive | 1.93 | DEC | 0.46 | Cleared microfilariae |
| 3 | M | 30 | 5 | 3000 | Positive | 1.21 | DEC | 0.42 | Cleared microfilariae |
| 4 | M | 25 | 1 | 15000 | ND | 0.83 | DEC | – | Cleared microfilariae |
| 5 | M | 23 | 2 | 1500 | ND | 1.36 | None | – | Lost to follow-up |
| 6 | M | 21 | 14 | 1500 | ND | 1.15 | None (DEC not taken) | – | Cleared microfilariae without treatment |
| 7 | F | 50 | 3 | 6000 | Negative | 0.48 | DEC ×2 | 0.16 | Cleared microfilariae, then recurred and was re-treated |
| 8 | M | 24 | 6 | 500 | ND | 1.1 | DEC | 0.64 | Cleared microfilariae, continued in trial |
ND: not done.
Eosinophilia was defined as an eosinophil count >0.5×103/mm3 in peripheral blood.
Figure 1.
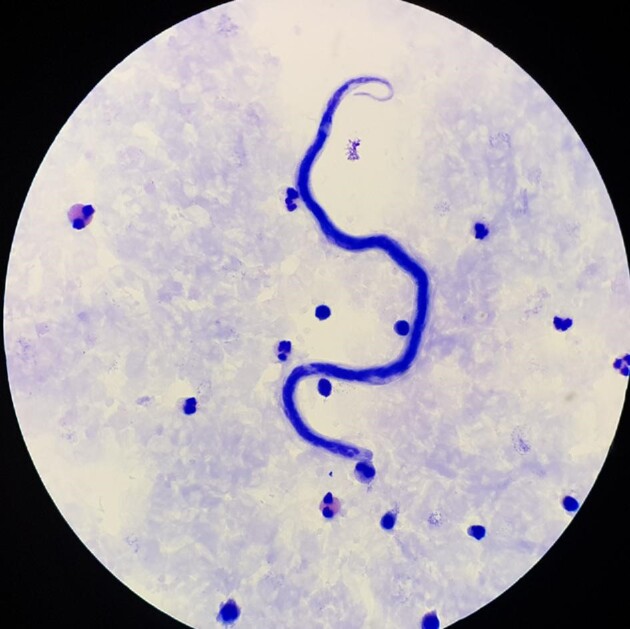
L. loa microfilaria seen on light microscopy of a TBS of one of the study subjects.
Eosinophil counts were measured with a Pentra C+ haematology analyser at the point of initial detection of microfilariae. Eosinophilia (defined as a peripheral blood eosinophil count >0.5×103/mm3) was seen in seven of eight of the affected subjects at the time of diagnosis, with counts ranging from 0.48 to 1.93×103/mm3 (median 1.13×103/mm3). By comparison, the eosinophil count for the 124 subjects enrolled in the study but not diagnosed with loiasis ranged from 0.09 to 4.54×103/mm3 (median 0.49×103/mm3) (p=0.011 by Wilcoxon rank sum test). Creatinine levels were determined with a COBAS Integra 400 plus analyser at the time of the first positive TBS. All creatinine levels were normal (mean = 0.81 mg/dL) and electrocardiograms were unremarkable.
The eight individuals were referred to the National Program for Onchocerciasis and Other Filariasis Control, where the diagnosis of loiasis was confirmed by repeat blood smear. The program prescribed a 21-d course of self-administered oral DEC, as per national guidelines; 12.5 mg on day 1, 25 mg on day 2, 50 mg on day 3, 50 mg twice daily on day 4 and 50 mg three times daily on days 5–21. Six of eight subjects reportedly completed treatment. Follow-up TBSs were free of microfilariae in five of these subjects (patients 2, 3, 4, 7 and 8) and the sixth cleared microfilariae after a second 21-d course of DEC (patient 1). One of these subjects (patient 7) completed treatment, was cleared of microfilariae and subsequently had a microfilaria-positive TBS. She was prescribed a second course of DEC. No known adverse effects of DEC were seen or reported. Eosinophil counts performed 4–10 weeks (median 7.5) after treatment were reduced to normal in three of the four subjects who were tested.
A pair of experienced microscopists on the research team retrospectively performed microfilaria counts on all eight of the TBS slides in which L. loa was first detected. In brief, 10 µL of blood collected in ethylenediaminetetraacetic acid was placed on a 10-mm×20-mm rectangle on a glass slide, dried and Giemsa stained and 2 µL of blood were examined (five to six passes across the width of the rectangle depending on the objective field number). Microfilaria counts ranged from 500 to 15 000 microfilaria/mL (Table 1). After conclusion of the trial, blood samples from the time of initial microscopic detection of microfilariae in four of the eight patients were also analysed for L. loa DNA by a published quantitative polymerase chain reaction (qPCR) assay.16L. loa DNA was found in blood samples from patients 1, 2 and 3, but not in patient 7 (Table 1).
The discovery of L. loa microfilaraemia in these otherwise healthy individuals had a significant impact on the conduct of the clinical trial and the retention of participants. The study protocol specified that all subjects be microscopically free from helminth infections at the time of enrolment. The protocol also mandated treatment of parasitic diseases in accordance with national guidelines, after which subjects could be allowed to continue in the study at the discretion of the investigators. Two subjects (patients 4 and 5) were found to have microfilaraemia before they were enrolled in the trial. They were prescribed DEC and given follow-up. Patient 4 completed treatment and cleared his microfilariae, but patient 5 never began treatment and was lost to follow-up. The remaining subjects had their first positive TBS for L. loa weeks into the trial, in the midst of a fixed study schedule. Three subjects (patients 1–3) who had received one or two doses of malaria vaccine prior to their diagnosis of loiasis were excluded from further vaccination since they were taking DEC at the time they were scheduled to be vaccinated. One subject (patient 6) was prescribed DEC, had a total of nine subsequent TBSs that were negative, received his final vaccine dose and later reported that he had never taken his treatment. Patient 7, whose vaccination was delayed due to treatment of microfilaraemia, eventually developed a separate medical condition that caused her to be withdrawn from the trial. In all, only one of the six enrolled adults diagnosed with L. loa was treated, cleared of microfilariae and able to participate in all remaining trial procedures (patient 8). Losing five subjects amounted to a significant reduction in sample size, as a total of 65 adults were enrolled in the trial.
Discussion
Eight (2.7%) of the 300 individuals who had TBSs performed during this vaccine trial10 were found to have L. loa microfilaraemia. Results were confirmed by a L. loa–specific qPCR in three of the four patients whose samples were retrospectively tested. The prevalence of loiasis on Bioko Island has previously been reported to be >20%,1 based on self-reported histories of ever having had eyeworm. This method may have overestimated the current prevalence of L. loa infection,17 particularly since mass administration of ivermectin for onchocerciasis control has occurred on Bioko Island since 1989.18 The microfilaricidal effects of ivermectin on L. loa are well established19 and the prevalence of L. loa microfilaraemia has been shown to decrease markedly in regions where ivermectin mass administration has been employed.19,20 Assessing the prevalence of loiasis is complicated by the fact that many individuals who harbour adult worms are amicrofilaremic21 and that some care is required to accurately distinguish L. loa from Mansonella perstans microfilariae by microscopy.22 Of interest, a recent cross-sectional study of 243 residents of Bioko Island found the prevalence of L. loa microfilaraemia to be 0.7% and M. perstans to be 8.8% by qPCR of whole blood.23
From a clinical standpoint, there was nothing extraordinary about the eight cases of L. loa microfilaraemia reported here. All were asymptomatic at the time of diagnosis, which is common among residents of endemic areas.24 A single course of DEC led to sustained clearance of microfilariae in four of six patients who were treated; one patient required a second course of DEC for persistent parasitaemia and another was re-treated when microfilaraemia recurred several weeks after demonstrated clearance. This is consistent with other reports.25,26 Typically, all patients had eosinophilia, which resolved in most cases with anti-filarial treatment.26,27 Although treatment with DEC has been associated with adverse reactions such as pruritus, Calabar swelling, dizziness, headache, arthralgias, fever and even encephalopathy,8,9,25,27,28 it was well tolerated in our patients.
What makes these cases relevant is their impact on the malaria vaccine trial. With respect to recruitment of participants, the protocol prescribed that all subjects be free from helminth infections at enrolment, as determined by microscopic examination of TBSs. This approach was taken due to concerns about a potential negative effect of these infections on vaccine-induced protective immunity.29 Because only one of the eight affected individuals was able to complete this trial, we could not assess the impact of L. loa microfilaraemia on the immune response to the vaccines studied. Still, it is clear that performing TBSs during screening visits was not adequate to rule out loiasis in this population. Only 1 of the 300 (0.3%) Equatoguinean potential participants had microfilariae on their initial TBS during screening. Another 7 of 300 (2.3%) were not found to have microfilaraemia until weeks later. In fact, a median of three negative TBSs were recorded among subjects who eventually displayed microfilaraemia.
It is known that the sensitivity of standard Giemsa-stained TBSs to detect loiasis is low; less than half of individuals who harbour adult worms have detectable microfilaraemia.21 Antibody tests could be used, but their inability to distinguish past from current infections30 would be likely to inflate the number of suspected active L. loa cases. Quantitative PCR has been shown to be more sensitive than microscopy for the detection of L. loa microfilariae16,23 and is a technology that is increasingly available in the field. In fact, in the current study, qPCR was used in tandem with microscopy to diagnose P. falciparum infection. In response to the detection of microfilariae in study subjects, after the trial, qPCR assays for L. loa and M. perstans were also established at the research site.
In summary, screening TBSs were likely inadequate to assess the true number of participants with loiasis in this study. If ruling out infection with L. loa is desired in early phase studies of vaccines against malaria and other pathogens, a more sensitive test such as qPCR could be done during initial screening to decrease the risk of enrolling individuals with occult loiasis that might later become patent by TBS.
An argument can be made against the need to detect and treat helminths prior to clinical trial enrolment in areas where they are endemic; the logic being that the drug or vaccine under investigation should be able to pass muster in a population where these parasitic infections are common. This may be a reasonable approach in larger later-phase trials, where randomization should balance the number of infected subjects in the comparison groups. In fact, TBS positivity for L. loa was removed as an exclusion criterion in a subsequent malaria vaccine trial conducted in the same population. In the current study, the incidental appearance of L. loa microfilariae on enrolled participants’ TBSs caused considerable disruption of the trial schedule. These subjects’ participation was effectively suspended for a minimum of 3 weeks while their diagnosis was confirmed, treatment provided and clearance of microfilariae verified. Four of the participants with loiasis were taking DEC at the time their vaccinations were scheduled; three were withdrawn from the trial and vaccination was delayed in the fourth. Some consideration was given to delaying treatment for asymptomatic loiasis until trial procedures were performed, but given this parasite's potential for significant morbidity and increased mortality,4,5,9 this approach was rejected. An alternative would have been to provide treatment without suspending trial procedures, although it would be important to ascertain that ongoing trial participation did not interfere with successful cure.
One issue that bears mentioning pertains to the safe treatment of loiasis. While this parasite has the potential to cause serious disease and should be treated, treatment is not without risk. Not all of the medical and laboratory personnel involved with the trial were initially familiar with this pathogen. As such, all microscopic diagnoses of L. loa microfilaraemia were confirmed by qualified personnel in the Equatoguinean National Program for Onchocerciasis and Other Filariasis Control. Treatment with DEC in accordance with national guidelines was offered to each patient and prescribed by National Program staff. Still, a later re-examination of the TBS slides in which L. loa was first detected showed microfilaria counts >2500/mL in four of the eight subjects with loiasis. Pretreatment with albendazole to decrease microfilarial load should have been considered in these patients prior to administration of DEC, given the risk of encephalopathy.8,9,31 Fortunately, none of the subjects treated for L. loa microfilaraemia experienced any adverse effects from DEC. Of note, although individuals with demonstrated L. loa microfilaraemia could not be enrolled and/or continue in the trial without evidence of parasitological cure (as was the case with other helminth infections), they were not compelled to accept treatment. In fact, two of the eight individuals diagnosed with loiasis opted to forgo treatment, although one of them initially claimed to have taken his DEC, then later confessed that he had not.
Conclusions
Although these eight cases of L. loa microfilaraemia were asymptomatic and generally responded well to treatment with DEC when it was accepted, what is relevant is the impact that this parasite had on the malaria vaccine trial. Based on published literature, loiasis could not reliably be ruled out by TBS during screening of participants. The incidental appearance of microfilariae on subsequent blood smears, weeks into the trial, led to the eventual exclusion of most affected participants, reducing the overall sample size. If L. loa microfilaraemia is deemed to be incompatible with clinical trial participation, a more sensitive method of diagnosis, such as qPCR, should be utilized.
Acknowledgements
The authors thank the study participants, the Bioko Island Malaria Elimination Project team for their work on the clinical trial, as well as Matilde Riloha Rivas, Director of the National Malaria Control Program of the Equatorial Guinea Ministry of Health and Social Welfare, and the Comité Ético Nacional de Guinea Equatorial for their oversight. We are grateful to members of the Data and Safety Monitoring Board for the clinical trial: James Campbell (chair), Feliciano Panades Shumad (local safety monitor), Alberto L. García-Basteiro, Brian Greenwood, and Mark Riddle. Kellie Boyd of the John S. Marietta Memorial Medical Library at JPS Health Network provided assistance with a literature search.
Contributor Information
Stephen R Manock, Sanaria Inc., Rockville, MD 20850, USA; Department of Family Medicine, John Peter Smith Hospital, Fort Worth, TX 76104, USA.
Vicente Urbano Nsue, National Malaria Control Program, Ministry of Health and Social Welfare, Malabo, Equatorial Guinea.
Ally Olotu, Department of Interventions & Clinical Trials, Ifakara Health Institute, Box 74, Bagamoyo, Tanzania; KEMRI Wellcome Trust Research Programme, P.O. Box 230-80108 Kilifi, Kenya.
Maximillian Mpina, Department of Interventions & Clinical Trials, Ifakara Health Institute, Box 74, Bagamoyo, Tanzania; Department of Medical Parasitology and Infection Biology, Clinical Immunology, Swiss Tropical and Public Health Institute, 4002 Basel, Switzerland; University of Basel, Petersplatz 1, 4001 Basel, Switzerland.
Elizabeth Nyakarungu, Department of Interventions & Clinical Trials, Ifakara Health Institute, Box 74, Bagamoyo, Tanzania.
José Raso, National Malaria Control Program, Ministry of Health and Social Welfare, Malabo, Equatorial Guinea.
Ali Mtoro, Department of Interventions & Clinical Trials, Ifakara Health Institute, Box 74, Bagamoyo, Tanzania.
Martín Eka Ondo Mangue, National Malaria Control Program, Ministry of Health and Social Welfare, Malabo, Equatorial Guinea.
Beltrán Ekua Ntutumu Pasialo, National Malaria Control Program, Ministry of Health and Social Welfare, Malabo, Equatorial Guinea.
Rufino Nguema, National Program for Onchocerciasis and Other Filariasis Control, Ministry of Health and Social Welfare, Malabo, Equatorial Guinea.
Pouria Riyahi, Sanaria Inc., Rockville, MD 20850, USA.
Tobias Schindler, Department of Medical Parasitology and Infection Biology, Clinical Immunology, Swiss Tropical and Public Health Institute, 4002 Basel, Switzerland; University of Basel, Petersplatz 1, 4001 Basel, Switzerland.
Claudia Daubenberger, Department of Medical Parasitology and Infection Biology, Clinical Immunology, Swiss Tropical and Public Health Institute, 4002 Basel, Switzerland; University of Basel, Petersplatz 1, 4001 Basel, Switzerland.
L W Preston Church, Sanaria Inc., Rockville, MD 20850, USA.
Peter F Billingsley, Sanaria Inc., Rockville, MD 20850, USA.
Thomas L Richie, Sanaria Inc., Rockville, MD 20850, USA.
Salim Abdulla, Department of Interventions & Clinical Trials, Ifakara Health Institute, Box 74, Bagamoyo, Tanzania.
Stephen L Hoffman, Sanaria Inc., Rockville, MD 20850, USA.
Authors’ contributions
SLH, SA, TLR and CD conceived and designed the malaria vaccine trial. SLH, SA, TLR, CD, AO, VUN, AM, MM, EN, TS, JR, MEOM, BENP, SRM, PFB and LWPC were responsible for study implementation. RN provided confirmation of microfilaraemia and prescribed treatment for participants with loiasis. PR was responsible for statistical analysis. SRM was responsible for writing the original draft. SLH, SA, TLR, CD, TS, LWPC and SRM were responsible for review and editing the article. All authors have read and agreed to the published version of the article. SRM and SLH are guarantors of the paper.
Funding
This work was supported by the government of Equatorial Guinea, Marathon E.G. Production, Noble Energy Equatorial Guinea and Atlantic Methanol Production Company. Funders did not contribute to the study design or to the collection, analysis or interpretation of data, the writing of the manuscript or the decision to submit it for publication.
Competing interests
SLH, TLR, PFB, PR and LWPC are employed by Sanaria Inc., which developed the PfSPZ vaccine and PfSPZ-CVac. SRM was employed by Sanaria Inc. at the time of the clinical trial but was not at the time the manuscript was prepared and submitted. AO was the recipient of a UK Medical Research Council African Research Leader award for work unrelated to this manuscript. All other authors declare no competing interests.
Ethical approval
The study was approved by the Comité Ético Nacional de Guinea Equatorial, additionally reviewed by the MaGil Institutional Review Board in Rockville, MD, the Ifakara Health Institute Institutional Review Board in Tanzania and the Ethics Committee of Northwestern and Central Switzerland.
Data availability
The data underlying this article are available in this published article.
References
- 1. Zouré HG, Wanji S, Noma Met al. . The geographic distribution of Loa in Africa: results of large-scale implementation of the Rapid Assessment Procedure for Loiasis (RAPLOA). PLoS Negl Trop Dis. 2011;5(6):e1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Negesse Y, Lanoie LO, Neafie RCet al. . Loiasis: “Calabar” swellings and involvement of deep organs. Am J Trop Med Hyg. 1985;34(3):537–46. [DOI] [PubMed] [Google Scholar]
- 3. Okonkwo ON, Hassan AO, Alarape Tet al. . Removal of adult subconjunctival Loa loa amongst urban dwellers in Nigeria. PLoS Negl Trop Dis. 2018;12(11):e0006920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Buell KG, Whittaker C, Chesnais CBet al. . Atypical clinical manifestations of loiasis and their relevance for endemic populations. Open Forum Infect Dis. 2019;6(11):ofz417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chesnais CB, Takougang I, Paguélé Met al. . Excess mortality associated with loiasis: a retrospective population-based cohort study. Lancet Infect Dis. 2017;17(1):108–16. [DOI] [PubMed] [Google Scholar]
- 6. Gardon J, Gardon-Wendel N, Demanga-Ngangueet al. . Serious reactions after mass treatment of onchocerciasis with ivermectin in an area endemic for Loa loa infection. Lancet 1997;350(9070):18–22. [DOI] [PubMed] [Google Scholar]
- 7. World Health Organization . WHO model prescribing information: drugs used in parasitic diseases, 2nd ed. Geneva: World Health Organization;1995. [Google Scholar]
- 8. Fain A. Les problèmes actuels de la loase [Current problems of loiasis]. Bull World Health Org. 1978;56(2):155–67. [PMC free article] [PubMed] [Google Scholar]
- 9. Metzger WG, Mordmüller B.. Loa loa-does it deserve to be neglected? Lancet Infect Dis. 2014;14(4):353–7. [DOI] [PubMed] [Google Scholar]
- 10. Jongo SA, Urbano V, Church LWPet al. . Immunogenicity and protective efficacy of radiation-attenuated and chemo-attenuated PfSPZ vaccines in Equatoguinean adults. Am J Trop Med Hyg. 2021;104(1):283–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Seder RA, Chang LJ, Enama MEet al. . Protection against malaria by intravenous immunization with a nonreplicating sporozoite vaccine. Science. 2013;341(6152):1359–65. [DOI] [PubMed] [Google Scholar]
- 12. Sissoko MS, Healy SA, Katile Aet al. . Safety and efficacy of PfSPZ vaccine against Plasmodium falciparum via direct venous inoculation in healthy malaria-exposed adults in Mali: a randomised, double-blind phase 1 trial. Lancet Infect Dis. 2017;17(5):498–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jongo SA, Church LWP, Mtoro ATet al. . Safety and differential antibody and T-cell responses to the Plasmodium falciparum sporozoite malaria vaccine, PfSPZ vaccine, by age in Tanzanian adults, adolescents, children, and infants. Am J Trop Med Hyg. 2019;100(6):1433–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Olotu A, Urbano V, Hamad Aet al. . Advancing global health through development and clinical trials partnerships: a randomized, placebo-controlled, double-blind assessment of safety, tolerability, and immunogenicity of PfSPZ vaccine for malaria in healthy Equatoguinean men. Am J Trop Med Hyg. 2018;98(1):308–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mordmüller B, Surat G, Lagler Het al. . Sterile protection against human malaria by chemoattenuated PfSPZ vaccine. Nature. 2017;542(7642):445–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fink DL, Kamgno J, Nutman TB.. Rapid molecular assays for specific detection and quantitation of Loa loa microfilaremia. PLoS Negl Trop Dis. 2011;5(8):e1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Emukah E, Rakers LJ, Kahansim Bet al. . In southern Nigeria Loa loa blood microfilaria density is very low even in areas with high prevalence of loiasis: results of a survey using the new LoaScope technology. Am J Trop Med Hyg. 2018;99(1):116–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Moya L, Herrador Z, Ta-Tang THet al. . Evidence for suppression of onchocerciasis transmission in Bioko Island, Equatorial Guinea. PLoS Negl Trop Dis. 2016;10(7):e0004829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pion SD, Tchatchueng-Mbougua JB, Chesnais CBet al. . Effect of a single standard dose (150–200 μg/kg) of Ivermectin on Loa loa microfilaremia: systematic review and meta-analysis. Open Forum Infect Dis. 2019;6(4):ofz019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chippaux JP, Bouchité B, Boussinesq Met al. . Impact of repeated large scale ivermectin treatments on the transmission of Loa loa. Trans R Soc Trop Med Hyg. 1998;92(4):454–8. [DOI] [PubMed] [Google Scholar]
- 21. Bouyou Akotet MK, Owono-Medang M, Mawili-Mboumba DPet al. . The relationship between microfilaraemic and amicrofilaraemic loiasis involving co-infection with Mansonella perstans and clinical symptoms in an exposed population from Gabon. J Helminthol. 2016;90(4):469–75. [DOI] [PubMed] [Google Scholar]
- 22. Mathison BA, Couturier MR, Pritt BS. Diagnostic identification and differentiation of microfilariae. J Clin Microbiol. 2019;57(10):e00706–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ta TH, Moya L, Nguema Jet al. . Geographical distribution and species identification of human filariasis and onchocerciasis in Bioko Island, Equatorial Guinea. Acta Trop. 2018;180:12–7. [DOI] [PubMed] [Google Scholar]
- 24. Herrick JA, Metenou S, Makiya MAet al. . Eosinophil-associated processes underlie differences in clinical presentation of loiasis between temporary residents and those indigenous to Loa-endemic areas. Clin Infect Dis. 2015;60(1):55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Saito M, Armstrong M, Boadi Set al. . Clinical features of imported loiasis: a case series from the Hospital for Tropical Diseases, London. Am J Trop Med Hyg. 2015;93(3):607–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gobbi F, Bottieau E, Bouchaud Oet al. . Comparison of different drug regimens for the treatment of loiasis-A TropNet retrospective study. PLoS Negl Trop Dis. 2018;12(11):e0006917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Puente S, Ramírez-Olivencia G, Lago Met al. . Loiasis in sub-Saharan migrants living in Spain with emphasis of cases from Equatorial Guinea. Infect Dis Poverty. 2020;9(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Herrick JA, Legrand F, Gounoue Ret al. . Posttreatment reactions after single-dose diethylcarbamazine or ivermectin in subjects with Loa loa infection. Clin Infect Dis. 2017;64(8):1017–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gazzinelli-Guimaraes PH, Nutman TB.. Helminth parasites and immune regulation. F1000Res. 2018;7:F1000 Faculty Rev-1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Akue JP, Eyang-Assengone ER, Dieki R.. Loa loa infection detection using biomarkers: current perspectives. Res Rep Trop Med. 2018;9: 43–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Klion A, Nutman TB, 2011. Loiasis and Mansonella infections. In: Guerrant R, Walker DH, Weller PF, editors. Tropical infectious diseases: principles, pathogens and practice, 3rd ed.Philadelphia: Saunders Elsevier; 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article are available in this published article.


