Abstract
Background
Open wedge high tibial osteotomy (OWHTO) and total knee arthroplasty (TKA) alter the ankle joint line obliquity (AJLO) to be more horizontal relative to the ground and aligns the valgus subtalar joint (SJ) neutrally. A previous study of the hindfoot alignment angle (HAA) showed that lower limb alignment after OWHTO becomes under-corrected because of abnormal compensation by the SJ. However, because TKA can exclude effects of femorotibial joint instability, analysis of a post-TKA cohort enables a more accurate evaluation of SJ compensation than analysis of a post-OWHTO cohort. In the present study, we performed radiographic evaluations before and after TKA to analyze SJ compensation.
Methods
Lower limb and hindfoot alignment were measured on plain radiographs in 46 patients (48 knees) who underwent TKA in our department. The patients were divided into Group A (postoperative AJLO within ±1°) and Group B (postoperative AJLO greater than ±1°), and various parameters were compared between the groups. The preoperative HAA that resulted in an abnormal postoperative AJLO was investigated.
Results
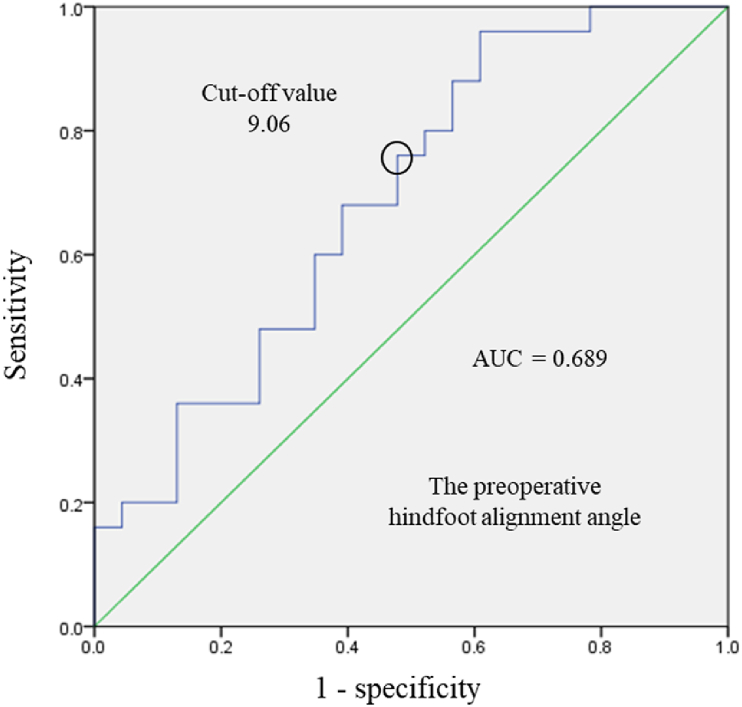
Group A had a significantly smaller preoperative HAA (p = 0.03) and postoperative HAA (p < 0.01) than Group B. Differences in the preoperative HAA between the two groups showed a cut-off value of 9.06°.
Conclusion
Patients with an HAA of more than 9.06° are likely to have abnormal hindfoot compensation.
Keywords: Total knee arthroplasty, Hindfoot alignment angle, Subtalar joint, Compensation
1. Introduction
Varus or valgus deformities of the knee joint may be caused by osteoarthritis (OA).1 Lower limb malalignment along with subtalar joint (SJ) compensation allows the proximal tibial articular surface to be horizontal to the ground.1, 2, 3, 4 Therefore, varus knees develop a valgus hindfoot, and valgus knees develop a varus hindfoot.4, 5, 6 In addition, after open wedge high tibial osteotomy (OWHTO) or total knee arthroplasty (TKA) for varus OA, the talus joint surface becomes horizontal to the ground with a valgus hindfoot.1, 2, 3, 4,7, 8, 9, 10, 11, 12, 13, 14 The compensatory ability and alignment changes of the SJ are then attributed to the mobility of the SJ.8,14, 15, 16, 17, 18 A previous study used the hindfoot alignment angle (HAA) to evaluate SJ compensation and showed that lower limb alignment after OWHTO was under-corrected because of abnormal SJ compensation.14 Thus, the SJ is an important factor in determining lower limb alignment. However, SJ compensation may be affected by the complicated structure of the joint, and the pathophysiology has not been clarified.
A previous study of SJ compensation included patients who had undergone OWHTO.14 The lower limb alignment became valgus after surgery; therefore, the varus and valgus mobility of the femorotibial (FT) joint and the influence of postoperative valgus alignment on the hindfoot could not be excluded. In contrast to OWHTO, TKA highly constrains the FT joint and the target alignment is close to neutral, making it possible to exclude the influence of FT joint mobility on hindfoot alignment. Furthermore, if SJ compensation is normal, the talus should be horizontal to the ground in patients with OA with neutral lower limb alignment after TKA. Therefore, the compensatory ability of the SJ could be evaluated more accurately by comparing hindfoot alignment before and after TKA rather than OWHTO.
In the present study, we evaluated SJ mobility using imaging before and after TKA. We hypothesized that investigating the impact of TKA on hindfoot alignment may clarify the pathophysiology of the compensatory ability of the SJ.
2. Patients and methods
2.1. Patients
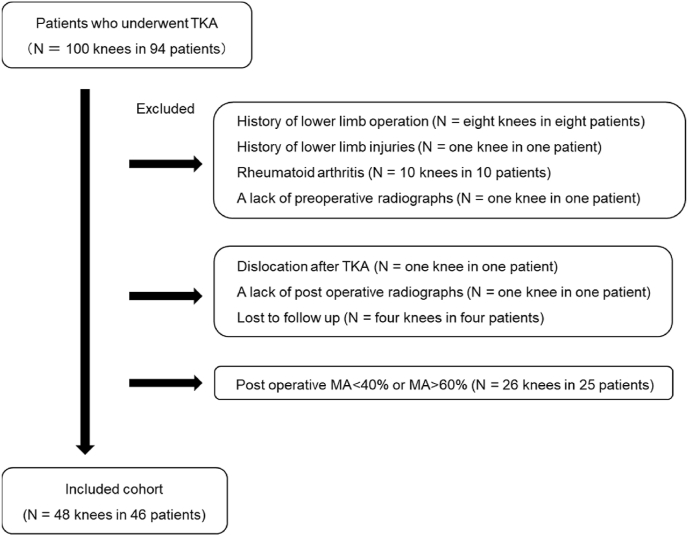
We identified 94 patients (100 knees) with OA who had undergone TKA performed by one of our senior surgeons between April 2019 and July 2021. Patients with Kellgren–Lawrence grade III or IV knee OA refractory to conservative therapy were indicated for surgery. The exclusion criteria were lower limb injury (8 knees), lower limb fracture (1 knee), rheumatoid arthritis (10 knees), postoperative implant dislocation (1 knee), lack of preoperative and postoperative radiographs (2 knees), and loss to follow-up (4 knees). The inclusion criterion was a mechanical axis (MA) of 40%–60% on anteroposterior weight-bearing whole-leg radiographs obtained at 3 months after TKA. Forty-eight knees of 46 patients were analyzed (Fig. 1).
Fig. 1.
Study flowchart. MA: mechanical axis; TKA: total knee arthroplasty.
2.2. Surgical procedure and postoperative rehabilitation
We performed TKA using a posterior stabilized type of Persona® (Zimmer Biomet, Warsaw, IN, USA) or Triathlon® (Stryker, Mahwah, IN, USA). The patients were permitted to begin range-of-motion training 1 day after surgery and gait training 2 days after surgery.
2.3. Radiographic measurements
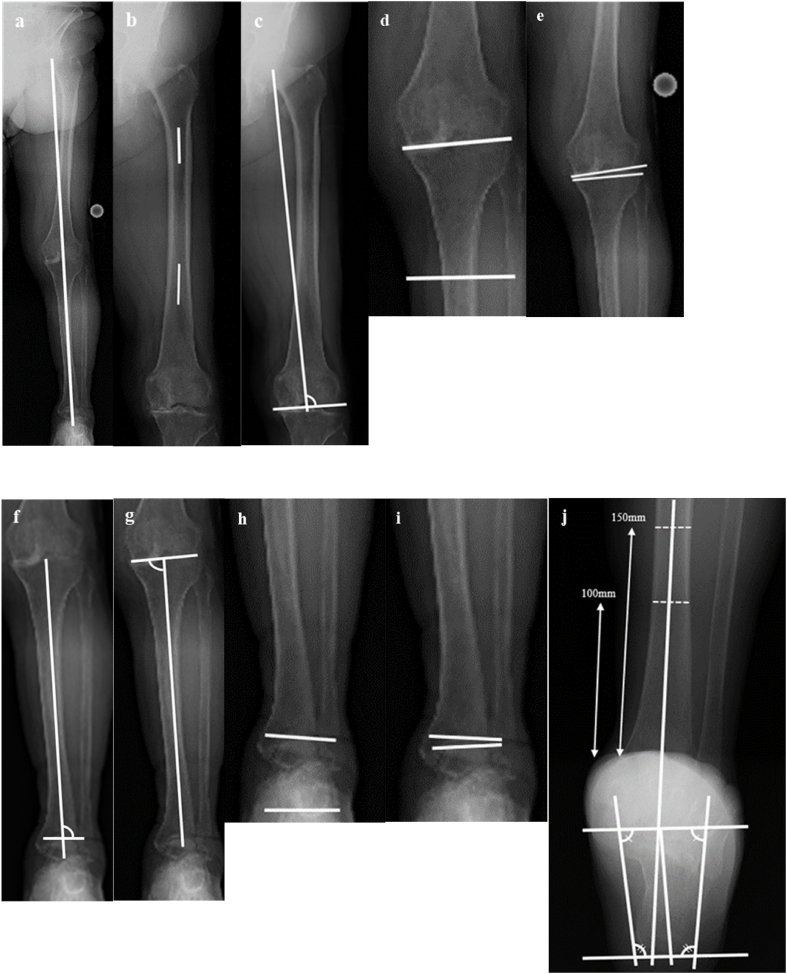
Radiographs of the entire length of the lower limb taken before and 3 months after TKA with the patella facing straight ahead and the knee joint in extension were evaluated. The assessment items were the MA, hip-knee-ankle angle (HKA), lateral bowing angle of the femoral shaft (BFS), mechanical lateral distal femoral angle (mLDFA), knee joint line obliquity relative to the ground (KJLO10; valgus shift of the proximal knee joint surface was indicated by a negative value), joint line convergence angle (JLCA), mechanical lateral distal tibial angle (mLDTA), mechanical medial proximal tibial angle (mMPTA), ankle joint line obliquity relative to the ground (AJLO10; valgus shift of the talus surface was indicated by a negative value), and talar tilt. The hindfoot angle was measured using hindfoot angle view radiographs (Fig. 2).19, 20, 21
Fig. 2.
Radiographic parameters evaluated preoperatively and postoperatively for total knee arthroplasty. The hindfoot angle was measured on hindfoot alignment views, and frontal alignment of the ankle and knee joints was measured on weight-bearing whole-leg radiographs. (a) Mechanical axis. (b) Lateral bowing angle of the femoral shaft. (c) Mechanical lateral distal femoral angle. (d) Knee joint line obliquity relative to the ground (valgus shift of the proximal knee joint surface was indicated by a negative value). (e) Joint line convergence angle. (f) Mechanical lateral distal tibial angle. (g) Mechanical medial proximal tibial angle. (h) Ankle joint line obliquity relative to the ground (valgus shift of the talus surface was indicated by a negative value). (i) Talar tilt. (j) Hindfoot angle. The angle at which the tibial and calcaneal axes intersect is the hindfoot angle. The tibial axis is the line bisecting the shaft cortex and drawn approximately 100 mm from the tibial surface, and the calcaneal axis is the line bisecting the osteogenic contours of the calcaneus.
In accordance with a previous study,14 the hindfoot angle plus the AJLO was used as an index of hindfoot alignment. Compensation of the SJ was then assessed indirectly as the pre-to post-TKA difference in the HAA.
3. Statistical analysis
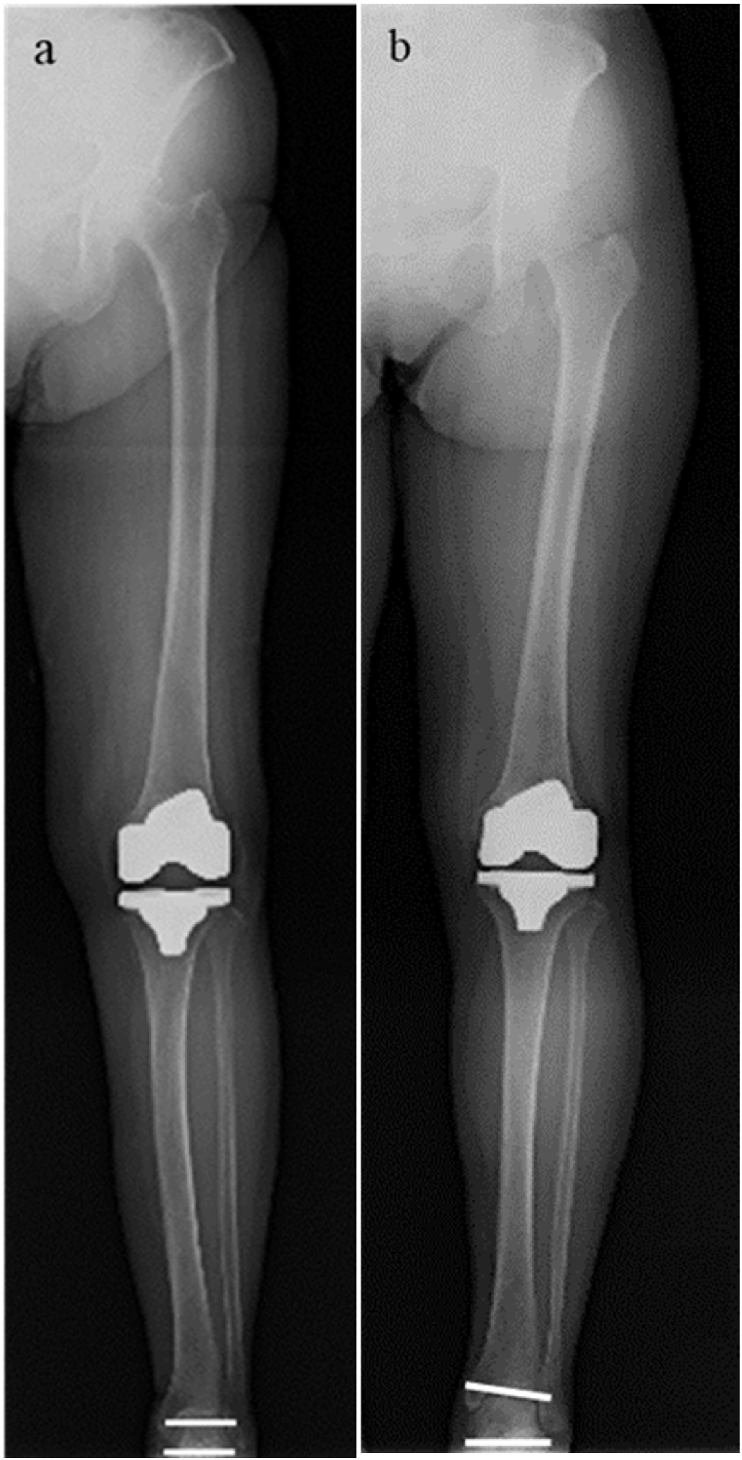
Patient background characteristics (age, sex, right and left side, body mass index [BMI], and Kellgren-Lawrence grade) are expressed as mean ± standard deviation. Preoperative and postoperative differences in the MA, HKA, BFS, mLDFA, KJLO, JLCA, mLDTA, mMPTA, AJLO, and talar tilt were evaluated using the paired t-test. Radiographic parameters were compared using the Mann–Whitney U test between patients with postoperative AJLO within ±1° (Group A) and those with AJLO greater than ±1° (Group B) (Fig. 3).
Fig. 3.
Whole-leg radiograph of the lower limb taken 3 months after TKA with the patella facing straight ahead and the knee joint in extension. (a) Patients with a postoperative ankle joint line obliquity relative to the ground (AJLO) within ±1° (Group A). (b) Patients with a postoperative AJLO of greater than ±1° (Group B).
Binomial and multivariate logistic regression analyses were performed between the explanatory variables (age, sex, BMI, and preoperative radiographic parameters) and the criterion variable of postoperative AJLO within ±1°. Results were considered significant at a p-value of <0.05. Cut-off values for each parameter were determined using receiver operating characteristic (ROC) curves based on the results of the logistic regression analysis. The estimated area, sensitivity, and specificity were also obtained from the ROC curves. A post-hoc power analysis was conducted to confirm that the number of knees examined provided sufficient statistical power to detect significance. The results showed that examining 42 knees resulted in 80% power with significance at 5%, validating our sample size of 48 knees.
Radiographic measurements were performed by two orthopedic surgeons, independently. The intraclass correlation coefficient ranged from 0.81 to 1.00 for both intraobserver and interobserver variances. Statistical analyses were performed using SPSS software version 23.0 (IBM Corporation, Armonk, NY, USA).
4. Results
The patients’ background characteristics (age, sex, right and left side, BMI, and Kellgren-Lawrence grade) are presented in Table 1. Of the 48 knees analyzed, 23 were in Group A and 25 were in Group B.
Table 1.
Patients’ background characteristics (n = 48).
| Patient characteristics | |
|---|---|
| Age (years) | 76.4 ± 7.7 (range 58–89) |
| Sex (male/female) | 6/42 |
| Right/left | 29/19 |
| BMI (kg/m2) | 26.0 ± 3.4 (range 19.3–34.5) |
| Kellgren - Lawrence grade (Ⅰ/Ⅱ/Ⅲ/Ⅳ) | 0/0/5/43 |
Data are presented as the mean ± standard deviation (range) or number of patients unless otherwise noted.
BMI: body mass index.
Table 2 shows the differences in mean radiographic parameters. From preoperatively to postoperatively, significant improvement was observed in the MA (p < 0.01) and HKA (p < 0.01), a significant increase was observed in the mMPTA (p < 0.01), and a significant decrease was observed in the KJLO (p = 0.01), JLCA (p < 0.01), AJLO (p = 0.01), hindfoot angle (p < 0.01), and HAA (p < 0.01).
Table 2.
Differences in mean radiographic parameters as determined by the paired-t test.
| Pre - TKA | Post - TKA | Difference | p value | |
|---|---|---|---|---|
| MA (%) | 26.4 ± 35.8 | 47.9 ± 4.9 | - 21.5 ± 35.4 | <0.01 |
| HKA (°) | - 5.4 ± 9.5 | - 0.2 ± 1.3 | - 5.2 ± 9.2 | <0.01 |
| BFS (°) | - 0.8 ± 2.7 | - 0.9 ± 2.8 | 0.1 ± 0.1 | 0.36 |
| mLDFA (°) | 89.1 ± 3.0 | 89.7 ± 1.7 | −0.6 ± 3.4 | 0.20 |
| KJLO (°) | 2.9 ± 4.6 | 0.3 ± 1.8 | 2.5 ± 4.9 | 0.01 |
| JLCA (°) | 3.2 ± 5.6 | 0.1 ± 0.7 | 3.1 ± 5.7 | < 0.01 |
| mLDTA (°) | 90.8 ± 3.8 | 90.5 ± 3.2 | 0.3 ± 0.3 | 0.49 |
| mMPTA (°) | 85.1 ± 3.5 | 89.8 ± 1.3 | -4.7 ± 3.7 | < 0.01 |
| AJLO (°) | 3.7 ± 6.3 | - 0.4 ± 2.9 | 4.1 ± 8.4 | 0.01 |
| Talar tilt (°) | 0.1 ± 1.1 | 0 ± 1.1 | - 0.1 ± 0.8 | 0.36 |
| Hindfoot angle (°) | 5.3 ± 4.8 | 2.7 ± 4.6 | 2.6 ± 4.3 | <0.01 |
| HAA (°) | 11.8 ± 6.6 | 6.4 ± 4.0 | 5.4 ± 5.5 | <0.01 |
Data are presented as the mean ± standard deviation.
TKA: total knee arthroplasty; MA: mechanical axis; HKA: hip-knee-ankle angle; BFS: lateral bowing angle of the femoral shaft; mLDFA: mechanical lateral distal femoral angle; KJLO: knee joint line obliquity relative to the ground; JLCA: joint line convergence angle; mLDTA: mechanical lateral distal tibial angle; mMPTA: mechanical medial proximal angle; AJLO: ankle joint line obliquity relative to the ground; HAA: hindfoot alignment angle.
The preoperative HAA (p = 0.03) and postoperative HAA (p < 0.01) were significantly smaller in Group A than Group B (Table 3).
Table 3.
Comparison of preoperative and postoperative radiographic parameters between Groups A and B.
| Group A (n = 23) | Group B (n = 25) | p value | |
|---|---|---|---|
| Preoperative | |||
| MA (%) | 20.9 ± 28.6 | 31.1 ± 41.2 | 0.32 |
| HKA (°) | - 7.5 ± 7.8 | - 3.4 ± 10.6 | 0.14 |
| BFS (°) | - 0.4 ± 3.1 | - 1.1 ± 2.3 | 0.35 |
| mLDFA (°) | 89.1 ± 2.7 | 89.1 ± 3.3 | 0.96 |
| KJLO (°) | 2.4 ± 2.3 | 3.3 ± 6.0 | 0.48 |
| JLCA (°) | 3.7 ± 4.0 | 2.7 ± 6.9 | 0.53 |
| mLDTA (°) | 90.4 ± 3.1 | 91.1 ± 4.3 | 0.52 |
| mMPTA (°) | 84.4 ± 4.0 | 85.7 ± 2.8 | 0.20 |
| AJLO (°) | 3.7 ± 3.4 | 3.7 ± 8.2 | 0.97 |
| Talar tilt (°) | - 0.3 ± 1.3 | 0.1 ± 1.0 | 0.25 |
| Hindfoot angle (°) | 5.6 ± 4.0 | 5.1 ± 5.5 | 0.71 |
| HAA (°) | 9.7 ± 6.2 | 13.8 ± 6.4 | 0.03 |
| Postoperative | |||
| MA (%) | 48.5 ± 4.9 | 47.3 ± 4.9 | 0.38 |
| HKA (°) | - 0.1 ± 1.3 | - 0.3 ± 1.3 | 0.58 |
| BFS (°) | - 0.4 ± 3.1 | - 1.3 ± 2.4 | 0.24 |
| mLDFA (°) | 89.6 ± 1.7 | 89.8 ± 1.7 | 0.70 |
| KJLO (°) | 0.8 ± 1.5 | - 0.1 ± 2.1 | 0.12 |
| JLCA (°) | 0.1 ± 0.7 | 0 ± 0.6 | 0.66 |
| mLDTA (°) | 89.9 ± 2.0 | 91.1 ± 3.9 | 0.22 |
| mMPTA (°) | 89.9 ± 1.2 | 89.7 ± 1.4 | 0.59 |
| AJLO (°) | 0 ± 0.7 | 1.5 ± 3.8 | 0.06 |
| Talar tilt (°) | - 0.1 ± 1.2 | 0.2 ± 0.9 | 0.48 |
| Hindfoot angle (°) | 2.2 ± 4.2 | 3.2 ± 5.0 | 0.47 |
| HAA (°) | 4.4 ± 2.9 | 8.2 ± 4.1 | <0.01 |
Data are presented as the mean ± standard deviation. Parameters were compared using paired t-tests.
MA: mechanical axis; HKA: hip-knee-ankle angle; BFS: lateral bowing angle of the femoral shaft; mLDFA: mechanical lateral distal femoral angle; KJLO: knee joint line obliquity relative to the ground; JLCA: joint line convergence angle; mLDTA: mechanical lateral distal tibial angle; mMPTA: mechanical medial proximal angle; AJLO: ankle joint line obliquity relative to the ground; HAA: hindfoot alignment angle.
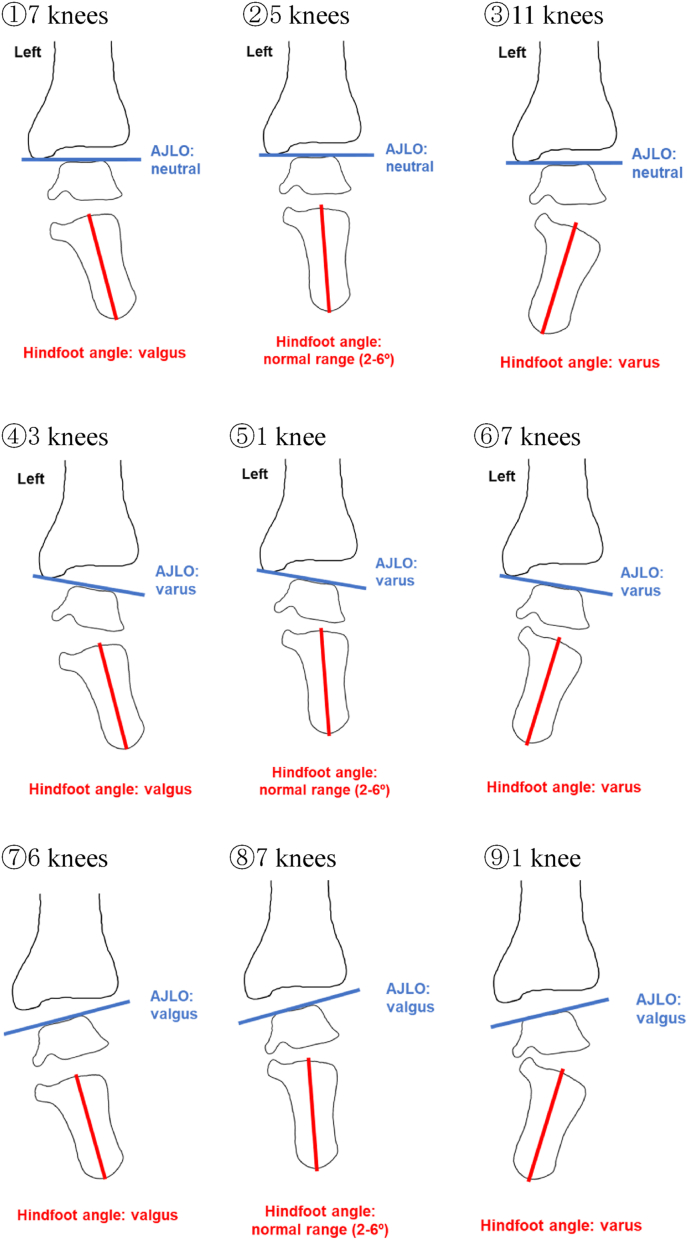
Nine postoperative hindfoot angle and AJLO combinations were observed (Fig. 4). Patients with neutral AJLO had varus-tilted hindfoot angles (11 of 48 knees), valgus-tilted hindfoot angles (7 knees), and normal hindfoot angles (5 knees). Patients with varus-tilted AJLO had valgus-tilted hindfoot angles (3 knees), normal hindfoot angles (1 knee), and varus-tilted hindfoot angles (7 knees). Patients with valgus-tilted AJLO had valgus-tilted hindfoot angles (6 knees), normal hindfoot angles (7 knees), and varus-tilted hindfoot angles (1 knee).
Fig. 4.
Nine combinations of the postoperative hindfoot angle and ankle joint line obliquity relative to the ground (AJLO).
We used binomial logistic regression analysis to identify preoperative parameters that predict a postoperative AJLO within ±1° (Table 4). The only predictor significantly associated with a postoperative AJLO within ±1° was the preoperative HAA (odds ratio [OR] = 0.90, 95% confidence interval [CI] = 0.82–0.99, p = 0.04). We used multivariate logistic regression analysis to identify preoperative parameters that predict a postoperative AJLO within ±1° (Table 5). There was a significant association between the preoperative HAA (OR = 0.69, 95% CI = 0.54–0.89, p = 0.01) and a postoperative AJLO within ±1°.
Table 4.
Binomial logistic regression analysis to identify the preoperative parameters that predict a postoperative AJLO of within ±1°.
| Variables | Odds ratio (95% Cl) | p value |
|---|---|---|
| Age | 0.99 (0.92–1.07) | 0.84 |
| Sex (female = 0, male = 1) | 0.41 (0.07–2.51) | 0.34 |
| BMI (kg/m2) | 0.98 (0.83–1.16) | 0.78 |
| Preoperative | ||
| MA (%) | 0.95 (0.89–1.02) | 0.14 |
| HKA (°) | 0.99 (0.98–1.01) | 0.32 |
| BFS (°) | 1.11 (0.89–1.38) | 0.34 |
| mLDFA (°) | 1.01 (0.83–1.22) | 0.96 |
| KJLO (°) | 0.95 (0.83-1.09) | 0.49 |
| JLCA (°) | 1.04 (0.93-1.15) | 0.52 |
| mLDTA (°) | 0.95 (0.81–1.11) | 0.51 |
| mMPTA (°) | 0.89 (0.75-1.06) | 0.87 |
| AJLO (°) | 1.00 (0.92-1.10) | 0.97 |
| Talar tilt (°) | 0.73 (0.43–1.25) | 0.25 |
| Hindfoot angle (°) | 1.04 (0.92–1.17) | 0.56 |
| HAA (°) | 0.90 (0.82–0.99) | 0.04 |
AJLO: ankle joint line obliquity relative to the ground; Cl: confidence interval; BMI: body mass index; MA: mechanical axis; HKA: hip-knee-ankle angle; BFS: lateral bowing angle of the femoral shaft; mLDFA: mechanical lateral distal femoral angle; KJLO: knee joint line obliquity relative to the ground; JLCA: joint line convergence angle; mLDTA: mechanical lateral distal tibial angle; mMPTA: mechanical medial proximal angle; HAA: hindfoot alignment angle.
Table 5.
Multivariate logistic regression analysis to identify the preoperative parameters that predict a postoperative ankle joint line obliquity relative to the ground of within ±1°.
| Variables | Odds ratio (95% Cl) | p value |
|---|---|---|
| Preoperative HAA (°) | 0.69 (0.54–0.89) | 0.01 |
Cl: confidence interval; HAA: hindfoot alignment angle.
Analysis using ROC curves showed that the cut-off value for the preoperative HAA at which the postoperative AJLO after TKA was greater than ±1° was 9.06°. The sensitivity was 76.0%, the specificity was 52.2%, and the area under the curve was 0.689 (Fig. 5).
Fig. 5.
Receiver operating characteristic curve showing the preoperative hindfoot alignment angle necessary to determine the cut-off value at which the ankle joint line obliquity relative to the ground after total knee arthroplasty becomes greater than ±1° after total knee arthroplasty. AUC: area under the curve.
5. Discussion
This is the first study to evaluate the relationship between various parameters and SJ mobility using the HAA before and after TKA. A significant difference between the preoperative and postoperative HAA was noted when the postoperative AJLO was not within ±1°, even when the postoperative lower limb alignment was neutral. Our results show that patients with a preoperative HAA of more than 9.06° are predicted to have abnormal SJ compensation.
The relationship between TKA and hindfoot alignment has been studied previously. Mullaji and Shetty13 evaluated preoperative and postoperative deviations in the HKA, MA, and MA including the hindfoot. They reported a decrease in hindfoot valgus alignment after TKA.13 However, they did not evaluate the AJLO. Previous reports suggest that ankle symptoms may occur postoperatively when the valgus-tilted AJLO does not improve after osteotomy and TKA.8,10,15,22,23 In addition, the mobility of the SJ cannot be evaluated only by evaluating hindfoot alignment. Therefore, when evaluating the SJ, it is necessary to evaluate both the hindfoot and the AJLO. Diao et al.2 evaluated changes in the HKA and hindfoot angle before and after TKA and showed a correlation between postoperative HKA improvement and the hindfoot angle. However, they did not evaluate SJ mobility. Norton et al.4 reported that post-TKA foot and ankle joint pain and dysfunction may be exacerbated and hindfoot symptoms may worsen if patients undergoing TKA also have SJ stiffness. Therefore, the SJ mobility should be evaluated before and after TKA. However, their report included only varus knees.4 Cho et al.3 compared the severity of preoperative knee deformity between patients with <10 and ≥ 10° of varus and reported no significant difference in postoperative hindfoot alignment. However, they did not evaluate the perioperative AJLO and SJ mobility.3 Takenaka et al.1 evaluated the perioperative hindfoot alignment. They evaluated hindfoot compensatory ability and reported that hindfoot valgus improves over time because of the hindfoot compensatory ability after TKA.1 However, they did not evaluate the perioperative AJLO. Attention should be paid to the AJLO from the viewpoint of foot and ankle pain and disability after TKA. Okamoto et al.24 reported that patients with severe OA who had insufficient correction of hindfoot alignment after TKA still complained of foot pain. Their study differed from ours in that hindfoot alignment was measured on lateral weight-bearing radiographs. In addition, they evaluated postoperative pain but not the mobility of the SJ.
In the present study, the preoperative HAA cut-off value that distinguished a postoperative AJLO of greater than ±1° from a postoperative AJLO within ±1° was 9.06°. In contrast, a previous study showed that the cut-off value after OWHTO was 15.9°.14 However, OWHTO adjusts the lower limb alignment to be more valgus, and the effects of the KJLO and JLCA cannot be excluded. Therefore, evaluating SJ mobility in patients undergoing TKA can exclude the influence of FT joint instability and evaluate SJ mobility more accurately. In this study, we assessed the mobility of the SJ in patients undergoing TKA and calculated the cut-off value for abnormal SJ mobility. Our results suggest that patients with OA and an HAA of >9.06° have abnormal compensation in the hindfoot and are likely to develop hindfoot malalignment and pain after osteotomy and TKA. Therefore, assessing the preoperative HAA is clinically significant for prediction of foot pain and malalignment after osteotomy and TKA.
This study has two main limitations: one is its retrospective design and the other is its relatively small sample size, although the power analysis indicated an adequate number of patients to achieve 80% power. Another limitation is that the SJ and its mobility were not directly assessed by radiography or other methods; rather, the HAA was evaluated as a measure of hindfoot mobility. The final limitation is that clinical variables were not evaluated. Further research is needed to determine whether patients with OA and an HAA of >9.06° have associated changes in clinical variables after TKA.
6. Conclusion
SJ mobility affects postoperative AJLO after TKA. Patients with OA and an HAA of >9.06° have abnormal compensation in the hindfoot and are predicted to develop hindfoot malalignment and pain after osteotomy or TKA. Thus, the preoperative HAA should be assessed before osteotomy or TKA.
Ethical review committee statement
This retrospective study was approved by the Institutional Review Board of Fukuoka University Hospital (U21-11-010). Informed consent was obtained from all patients.
CRediT authorship contribution statement
Yutaro Yamasaki: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft. Akira Maeyama: Conceptualization, Methodology, Writing – review & editing. Kotaro Miyazaki: Conceptualization, Investigation, Methodology, Writing – review & editing. Tetsuro Ishimatsu: Writing – review & editing. Ichiro Yoshimura: Writing – review & editing. Takuaki Yamamoto: Supervision, Writing – review & editing.
Declarations of competing interest
None.
Acknowledgments
We thank Kelly Zammit, BVSc, from Edanz Group (https://en-author-services.edanzgroup.com/), for editing a draft of this manuscript.
References
- 1.Takenaka T., Ikoma K., Ohashi S., et al. Hindfoot alignment at one year after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24(8):2442–2446. doi: 10.1007/s00167-015-3916-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diao N., Yu F., Yang B., Ma L., Yin H., Guo A. Association between changes in hip-knee-ankle angle and hindfoot alignment after total knee arthroplasty for varus knee osteoarthritis. BMC Muscoskel Disord. 2021;22(1):610. doi: 10.1186/s12891-021-04488-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cho W.S., Cho H.S., Byun S.E. Changes in hindfoot alignment after total knee arthroplasty in knee osteoarthritic patients with varus deformity. Knee Surg Sports Traumatol Arthrosc. 2017;25(11):3596–3604. doi: 10.1007/s00167-016-4278-8. [DOI] [PubMed] [Google Scholar]
- 4.Norton A.A., Callaghan J.J., Amendola A., et al. Correlation of knee and hindfoot deformities in advanced knee OA: compensatory hindfoot alignment and where it occurs. Clin Orthop Relat Res. 2015;473(1):166–174. doi: 10.1007/s11999-014-3801-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reilingh M.L., Beimers L., Tuijthof G.J.M., Stufkens S.A.S., Maas M., Dijk C.N. Measuring hindfoot alignment radiographically: the long axial view is more reliable than the hindfoot alignment view. Skeletal Radiol. 2010;39(11):1103–1108. doi: 10.1007/s00256-009-0857-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saltzman C.L., el-Khoury G.Y. The hindfoot alignment view. Foot Ankle Int. 1995;16(9):572–576. doi: 10.1177/107110079501600911. [DOI] [PubMed] [Google Scholar]
- 7.Chandler J.T., Moskal J.T. Evaluation of knee and hindfoot alignment before and after total knee arthroplasty: a prospective analysis. J Arthroplasty. 2004;19(2):211–216. doi: 10.1016/j.arth.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 8.Choi G.W., Yang J.H., Park J.H., et al. Changes in coronal alignment of the ankle joint after high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2017;25(3):838–845. doi: 10.1007/s00167-015-3890-3. [DOI] [PubMed] [Google Scholar]
- 9.Choi J.Y., Song S.J., Kim S.J., Kim S.H., Park J.S., Suh J.S. Changes in hindfoot alignment after high or low tibial osteotomy. Foot Ankle Int. 2018;39(9):1097–1105. doi: 10.1177/1071100718773767. [DOI] [PubMed] [Google Scholar]
- 10.Lee K.M., Chang C.B., Park M.S., Kang S.B., Kim T.K., Chung C.Y. Changes of knee joint and ankle joint orientations after high tibial osteotomy. Osteoarthritis Cartilage. 2015;23(2):232–238. doi: 10.1016/j.joca.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 11.Takeuchi R., Saito T., Koshino T. Clinical results of a valgus high tibial osteotomy for the treatment of osteoarthritis of the knee and the ipsilateral ankle. Knee. 2008;15(3):196–200. doi: 10.1016/j.knee.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Yoshimoto K., Noguchi M., Yamada A., Nasu Y. Compensatory function of the subtalar joint for lower extremity malalignment. Adv Orthop. 2019 doi: 10.1155/2019/7656878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mullaji A., Shetty G.M. Persistent hindfoot valgus causes lateral deviation of weightbearing axis after total knee arthroplasty. Clin Orthop Relat Res. 2011;469(4):1154–1160. doi: 10.1007/s11999-010-1703-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miyazaki K., Maeyama A., Yoshimura I., Kobayashi T., Ishimatsu T., Yamamoto T. Influence of hindfoot alignment on postoperative lower limb alignment in medial opening wedge high tibial osteotomy. Arch Orthop Trauma Surg. 2021 doi: 10.1007/s00402-021-04001-z. [DOI] [PubMed] [Google Scholar]
- 15.Lee J.H., Jeong B.O. Radiologic changes of ankle joint after total knee arthroplasty. Foot Ankle Int. 2012;33(12):1087–1092. doi: 10.3113/FAI.2012.1087. [DOI] [PubMed] [Google Scholar]
- 16.Pagenstert G.I., Hintermann B., Barg A., Leumann A., Valderrabano V. Realignment surgery as alternative treatment of varus and valgus ankle osteoarthritis. Clin Orthop Relat Res. 2007;462:156–168. doi: 10.1097/BLO.0b013e318124a462. [DOI] [PubMed] [Google Scholar]
- 17.Tanaka Y., Takakura Y., Hayashi K., Taniguchi A., Kumai T., Sugimoto K. Low tibial osteotomy for varus-type osteoarthritis of the ankle. J Bone Joint Surg Br. 2006;88(7):909–913. doi: 10.1302/0301-620X.88B7.17325. [DOI] [PubMed] [Google Scholar]
- 18.Burssens A., De Roos D., Barg A., et al. Alignment of the hindfoot in total knee arthroplasty: a systematic review of clinical and radiological outcomes. Bone Joint Lett J. 2021;103(1):87–97. doi: 10.1302/0301-620X.103B1.BJJ-2020-0143.R1. [DOI] [PubMed] [Google Scholar]
- 19.Haight H.J., Dahm D.L., Smith J., Krause D.A. Measuring standing hindfoot alignment: reliability of goniometric and visual measurements. Arch Phys Med Rehabil. 2005;86(3):571–575. doi: 10.1016/j.apmr.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 20.Strash W.W., Berardo P. Radiographic assessment of the hindfoot and ankle. Clin Podiatr Med Surg. 2004;21(3):295–304. doi: 10.1016/j.cpm.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 21.Williamson E.R., Chan J.Y., Burket J.C., Deland J.T., Ellis S.J. New radiographic parameter assessing hindfoot alignment in stage II adult-acquired flatfoot deformity. Foot Ankle Int. 2015;36(4):417–423. doi: 10.1177/1071100714558846. [DOI] [PubMed] [Google Scholar]
- 22.Kim J.G., Suh D.H., Choi G.W., Koo B.M., Kim S.G. Change in the weight-bearing line ratio of the ankle joint and ankle joint line orientation after knee arthroplasty and high tibial osteotomy in patients with genu varum deformity. Int Orthop. 2021;45(1):117–124. doi: 10.1007/s00264-020-04799-0. [DOI] [PubMed] [Google Scholar]
- 23.Graef F., Falk R., Tsitsilonis S., Perka C., Zahn R., Hommel H. Correction of excessive intraarticular varus deformities in total knee arthroplasty is associated with deteriorated postoperative ankle function. Knee Surg Traumatol Arthrosc. Knee Surg Sports Traumatol Arthrosc. 2020;28(12):3758–3765. doi: 10.1007/s00167-019-05812-9. [DOI] [PubMed] [Google Scholar]
- 24.Okamoto Y., Otsuki S., Jotoku T., Nakajima M., Neo M. Clinical usefulness of hindfoot assessment for total knee arthroplasty: persistent post-operative hindfoot pain and alignment in pre-existing severe knee deformity. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2632–2639. doi: 10.1007/s00167-016-4122-1. [DOI] [PubMed] [Google Scholar]