Abstract
Objectives
This study reports the prevalence of anemia and investigates its associated correlates and outcomes among elderly hospitalized patients in a single hospital in Bahrain.
Methods
A retrospective study was conducted on 227 consecutive elderly patients admitted under general internal medicine in the biggest tertiary hospital in Bahrain. Medical records were reviewed for all patients, including clinical characteristics, laboratory results, and outcomes.
Results
Anemia was highly prevalent among hospitalized elderly patients (71.6%). Males were significantly more affected than females (p = 0.031). In terms of severity, the most common type was moderate anemia (56.1%); with regards to etiology, the most common type was anemia associated with chronic disease (48.1%). Anemia was as common as other comorbidities, including hypertension (71.4%) and diabetes mellitus (53.7%). When comparing anemic to non-anemic patients, the length of hospital stay was significantly longer (p < 0.001) and inversely correlated to the level of hemoglobin; furthermore, 1-year mortality was significantly higher (p < 0.001). When compared to those with mild anemia, patients with moderate/severe anemia were more likely to die (odds ratio [OR] = 2.2, 95% confidence interval [CI]: 1.27–4.92).
Conclusion
The prevalence of anemia in our study was higher than previously reported. Even so, anemia receives minimal attention and is usually seen as a minor problem. Our results reiterate the need to recognize the high importance of anemia especially when diagnosing and treating older patients. This, in turn, could positively affect a number of outcomes such as mortality, length of stay, and the functional decline of admitted individuals.
Keywords: Anemia, Anemia of chronic disease, Elderly, Internal medicine, Iron deficiency anemia
الملخص
أهداف البحث
تشير هذه الدراسة إلى كمية انتشار فقر الدم وتدرس الارتباطات والنتائج المرتبطة به بين المرضى المسنين في المستشفى.
طرق البحث
تم إجراء دراسة بأثر رجعي على 227 مريضا مسنا متتاليا تم تنويمهم في قسم الطب الباطني العام في أكبر مستشفى ثانوي في البحرين. تمت مراجعة السجلات الطبية للمرضى بما في ذلك الخصائص والنتائج المختبرية والمرضية.
النتائج
كان فقر الدم منتشرا بشكل كبير بين المرضى المسنين في المستشفى (71.6٪). بالإضافة إلى ذلك كان الذكور أكثر تأثرا من الإناث. أكثر الأنواع شيوعا هو فقر الدم المتوسط من حيث الشدة (56.1٪) وفقر الدم الناجم عن الأمراض المزمنة من حيث المسببات (48.1٪). كان فقر الدم شائعا مثل الأمراض المصاحبة الأخرى مثل ارتفاع ضغط الدم (71.4٪) وداء السكري (53.7٪). عند مقارنة المصابين وغير المصابين بفقر الدم، كانت مدة الإقامة في المستشفى أطول وترتبط عكسيا بتركيز الهيموجلوبين وكان معدل الوفيات لمدة عام أعلى. بالإضافة إلى ذلك، عند المقارنة مع المصابين بفقر الدم الخفيف، كان المرضى الذين يعانون من فقر الدم المتوسط / الحاد أكثر عرضة للوفاة (نسبة الأرجحية = 2.2 ، فاصل الثقة 95٪ من 1.27 إلى 4.92).
الاستنتاجات
انتشار فقر الدم في دراستنا أعلى مما تم الإبلاغ عنه سابقا. ومع ذلك، لا يحظى فقر الدم باهتمام كبير وعادة ما ينظر إليه على أنه مشكلة يسيرة. تؤكد نتائجنا على الحاجة إلى التعرف على الأهمية الكبيرة لفقر الدم خاصة عند تشخيص المرضى الأكبر سنا وعلاجهم. وهذا يمكن أن يؤثر بشكل إيجابي على النتائج مثل نسبة الوفاة، ومدة الإقامة، والتدهور الوظيفي للأفراد اللذين تم إدخالهم إلى المستشفى.
الكلمات المفتاحية: فقر الدم, كبار السن, فقر الدم الناجم عن الأمراض المزمنة, فقر الدم الناجم عن نقص الحديد, الطب الباطني
Introduction
Anemia poses a significant health burden globally with an overall prevalence of 27% among populations worldwide.1 In addition, the prevalence of anemia is higher in female subjects, from 15 years of age to adulthood, and in older subjects of both genders.1 In community dwelling individuals aged 65 years and above, anemia is present in 10% of women and 11% of men.2 Hospitalized patients show an even higher prevalence of anemia (40–50%).3 In the elderly, multifactorial anemia is the most common type.4 The National Health and Nutrition Examination Survey III study demonstrated that in elderly anemic patients, one third of cases are due to nutritional deficiencies while two thirds are due to chronic disease (ACD) or unexplained reasons for anemia (UA).2
Anemia has been associated with multiple different adverse outcomes in the general population. In older adults specifically, the presence of anemia, as well as low hemoglobin (Hb) levels, were found to be independent risk factors for increased frailty, reduced physical performance, and an increased risk of falls.5 Anemia has also been linked to an increased risk of hospitalization and mortality.6 In addition, a systematic review, including over 30 years of published data, identified a possible association between anemia in the elderly and cognitive performance.7 Despite these significant consequences, anemia in the elderly population is often overlooked, as concluded by Randi et al.8 This is possibly due to the high number of comorbidities and the complexity of diagnosing and treating this population.
Anemia of chronic disease has a complex pathophysiology and is generally related to and aggravated by multiple factors including hemolysis, blood loss, drug related adverse events, and vitamin deficiencies.9 The Baltimore Longitudinal Study on Aging demonstrated that serum erythropoietin increases as an individual ages; this may serve as compensation for increased red blood cell turnover, subclinical blood loss, or the increased erythropoietin resistance of red cell precursors.10 This supports the idea that anemia occurs when such compensatory mechanisms becomes inadequate such as in very advanced age or those affected by renal impairment.10
Anemia research from Bahrain is scarce, particularly in older individuals. Some studies have focused on specific population samples and demonstrated that anemia affects 30% of children aged 3 years and 51% of pregnant women.11,12 Currently, no local data is available regarding the prevalence of anemia in the elderly. Hence, our aims were three-fold. First to determine the prevalence of anemia among elderly hospitalized patients. Second, to describe the characteristics of anemic patients, and third, to investigate the relationship between anemia and different outcomes.
Materials and Methods
Study design, population, and samples
This retrospective observational study was carried out in a 1200-bed tertiary hospital in Bahrain. All patients admitted to the hospital between January and June 2018 were assessed for eligibility. The inclusion criteria were as follows: (1) patients admitted under General Internal Medicine and (2) patients aged 60 years or more. Of these, we excluded patients with incomplete medical electronic records or laboratory investigations. After applying our selection criteria, 227 eligible patients were identified.
Study measures and outcomes
The electronic health system was used to extract information about the patients, including baseline characteristics, such as age, gender, chronic illnesses, regular medications, laboratory results, and the reason for admission. Laboratory workup for anemia is generally requested for all anemic patients admitted under general medicine and was extracted retrospectively. The Katz Index of Independence in Activities of Daily Living13 was calculated to identify the level of function prior to admission. The primary outcomes were the length of stay for patients who survived the hospital admission and the 1-year mortality after the admission.
Anemia was defined according to hemoglobin cut-off levels defined by the World Health Organization (WHO) (<12.0 g/dL for females, <13.0 g/dL for males).14 Severity was defined as mild with Hb ≥ 11 g/dL, moderate with Hb 8.0–10.9 g/dL and severe with Hb < 8.0 g/dL). In addition, the following laboratory results were recorded for all 227 patients: serum iron (Fe), ferritin, transferrin saturation (TSAT), cobalamin (B12), folic acid, and c-reactive protein (CRP).
Causes of anemia were classified based on the following criteria: Iron deficiency anemia (IDA) in the presence of ferritin <30 μg/L and/or TSAT <20% and CRP ≤5 mg/L, ACD in the presence of CRP >5 mg/L, ferritin >100 μg/L and TSAT <20%, B12 and folic acid deficiency in the presence of vitamin B12 < 200 pg/mL, and/or folic acid <2 ng/mL and TSAT ≥20%. Anemia of Chronic kidney Disease (ACKD) was defined as anemia combined with an estimated glomerular filtration rate (eGFR) < 30 mL/min/1.73 m2. Anemia secondary to other etiologies was defined as UA.
Statistical analysis
Data analysis was conducted using Statistical Package for the Social Sciences (SPSS -24) software (IBM, Armonk, NY, USA). The number and percentage of patients in different categories were reported for categorical variables. For continuous variables, summary statistics (including mean and standard deviation) were used to describe the variables. Means were compared using the Chi-square (χ2) or Fisher's exact test for categorical variables, and the t-test or Mann–Whitney U test for continuous variables. P-values < 0.05 were deemed significant.
Abbreviations
ACD, Anemia of chronic disease; B12, Cobalamin; CRP, C-reactive protein (CRP); DM, Diabetes Mellitus; eGFR, Estimated glomerular filtration rate; Fe, Iron; Hb, Hemoglobin; IDA, Iron deficiency anemia; SPSS -24, Statistical Package for the Social Sciences 24; TSAT Transferrin saturation (TSAT); UA, Unexplained anemia; WHO, World Health Organization.
Results
Baseline characteristics
Our study included 227 patients aged 60 years and above; The mean age was 76.6 ± 9.4 years and female gender comprised 56.8% (129) of the sample (Table 1). Most admissions were due to infectious causes (n = 156, 68.7%) with a mean length of stay of 13.5 ± 14.7 days. Inpatient mortality rate was 31.7% (72) increasing to 50.7% (115) at 1-year follow up. Over half the patients (59.9%, n = 136) had 4 or more comorbidities, with diabetes mellitus (DM) and hypertension being the most common. Polypharmacy, defined as taking 5 or more medications, was observed in 71.4% (n = 162) of the patients. In addition, the mean level of hemoglobin was 10.9 ± 2.2 g/dL.
Table 1.
Baseline characteristics of the patients.
| Baseline characteristics | Total number = 227 n (%) |
|
|---|---|---|
| Age, mean ± SD | 76.6 ± 9.4 | |
| Age groups | 60–69 | 65 (28.6) |
| 70–79 | 65 (28.6) | |
| 80–89 | 78 (34.4) | |
| ≥90 | 19 (8.4) | |
| Nationality, Bahrain | 215 (94.7) | |
| Gender | Male | 98 (43.2) |
| Female | 129 (56.8) | |
| Comorbidities | Hypertension | 162 (71.4) |
| Diabetes Mellitus | 122 (53.7) | |
| Ischemic Heart Disease | 58 (25.6) | |
| Dyslipidemia | 63 (27.8) | |
| Chronic Kidney Disease | 25 (11.0) | |
| Regular Medications | Aspirin | 100 (44.1) |
| Diuretics | 79 (34.8) | |
| Iron | 56 (24.7) | |
| Insulin | 50 (22.0) | |
| Folate | 16 (7.0) | |
| Vitamin B12 | 4 (1.8) | |
| Number of chronic diseases, mean ± SD | 2.8 ± 1.6 | |
| Number of regular medications, mean ± SD | 6.0 ± 3.5 | |
| Admission Diagnosis | Infectiousa | 156 (68.7) |
| Non-infectiousb | 71 (31.3) | |
| Katz score, mean ± SD | 3.63 ± 2.39 | |
| Hemoglobin, mean ± SD (g/dL) | 10.9 ± 2.2 | |
| Length of Stay, mean ± SD (Days) | 13.5 ± 14.7 | |
| 1 year mortality |
115 (50.7) |
|
| Causes of anemia |
Total number = 164 n (%) |
|
| Anemia of Chronic Disease | 79 (48.2) | |
| Iron Deficiency Anemia | 46 (28.0) | |
| Chronic Kidney Disease | 23 (14.0) | |
| Unexplained Anemia | 9 (5.5) | |
| Folate/B12 Deficiency | 7 (4.3) | |
Urinary tract infection, respiratory tract infection, gastroenteritis, and skin and soft tissue infection.
Myocardial infarction, gastrointestinal bleeding, renal failure, and cerebrovascular accident.
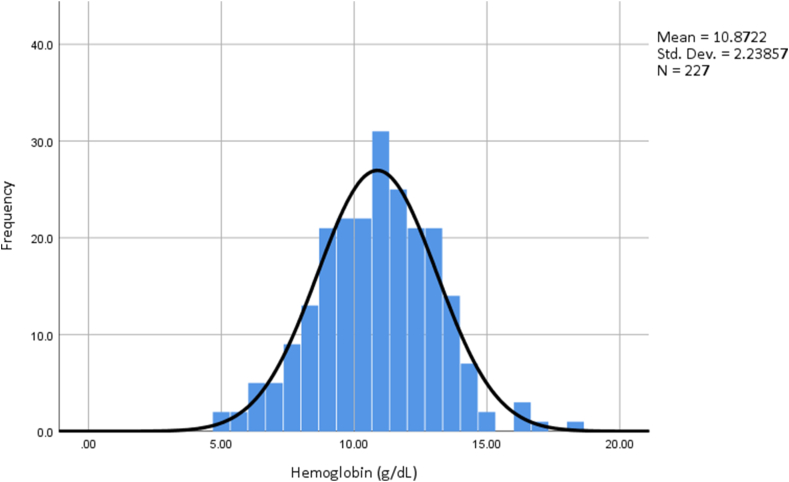
Prevalence and etiology
The prevalence of anemia was 72.2% (164) with a significantly higher occurrence in males than females at 79.6% and 66.7%, respectively (p = 0.031) (Table 2). According to our severity cutoffs, of all anemic patients, 31.1% (51) had mild anemia, 56.1% (92) had moderate anemia, and 12.8% (21) had severe anemia. Hemoglobin levels were normally distributed among all the patients (Figure 1). The minimum hemoglobin level was 4.8 and the maximum was 18.2. Tests of normality, carried out with the Kolmogorov–Smirnov and Shapiro–Wilk tests, were non-significant, with p-values of 0.2 and 0.67, respectively. More than half of anemic patients were female (52.4%), with a mean age of 76.5 ± 9.4 years. Most admissions were due to infective causes; the two most common infections being urinary tract infections and respiratory tract infections which together accounted for over half of the admissions. Following admission, 59.1% of anemic patients were discharged home and 60.4% died within one year of admission. Of all 164 anemic patients, 47 were receiving iron or vitamin supplementation on admission (28.6%).
Table 2.
Comparison of characteristics between anemic and non-anemic patients.
| Non-anemic total = 63 n (%)a |
Anemic total = 164 n (%)a |
P value | ||
|---|---|---|---|---|
| Age, mean ± SD | 76.8 ± 9.6 | 76.5 ± 9.4 | 0.928 | |
| Age groups | 60–69 | 19 (29.2) | 46 (70.8) | 0.793 |
| 70–79 | 15 (23.1) | 50 (76.9) | ||
| 80–89 | 23 (29.5) | 55 (70.5) | ||
| ≥90 | 6 (31.6) | 13 (68.4) | ||
| Gender | Male | 20 (20.4) | 78 (79.6) | 0.031 |
| Female | 43 (33.3) | 86 (66.7) | ||
| Comorbidities | Hypertension | 42 (25.9) | 120 (74.0) | 0.332 |
| Diabetes Mellitus | 27 (22.1) | 95 (77.9) | 0.041 | |
| Dyslipidemia | 21 (33.3) | 42 (66.7) | 0.245 | |
| Ischemic Heart Disease | 12 (20.7) | 46 (79.3) | 0.164 | |
| Chronic Kidney Disease | 2 (8.0) | 23 (92.0) | 0.019 | |
| Regular Medications | Aspirin | 27 (27.0) | 73 (73.0) | 0.822 |
| Insulin | 7 (14.0) | 43 (86.0) | 0.014 | |
| Diuretics | 17 (21.5) | 62 (78.5) | 0.125 | |
| Iron | 9 (16.1) | 47 (83.9) | 0.024 | |
| Folate | 1 (6.3) | 15 (93.8) | 0.046 | |
| Vitamin B12 | 1 (25.0) | 3 (75.0) | 0.901 | |
| Number of chronic diseases, mean ± SD | 2.6 ± 1.4 | 2.9 ± 1.7 | 0.803 | |
| Number of regular medications, mean ± SD | 5.1 ± 3.4 | 6.3 ± 3.5 | 0.932 | |
| Admission Diagnosis | Infectiousb | 45 (28.8) | 111 (71.2) | 0.586 |
| Non-infectiousc | 28 (39.4) | 43 (60.6) | ||
| Hb, mean ± SD (g/dL) | 13.5 ± 1.2 | 9.9 ± 1.7 | <0.001 | |
| Katz Index, mean ± SD | 3.81 ± 2.42 | 3.57 ± 2.38 | 0.495 | |
| Length of Stay, mean ± SD (Days) | 8.2 ± 5.3 | 15.5 ± 16.6 | <0.001 | |
| 1 year Mortality | 16 (13.9) | 99 (86.1) | <0.001 | |
Percentages represent a comparison between anemic and non-anemic groups.
Urinary tract infection, respiratory tract infection, gastroenteritis, and skin and soft tissue infection.
Myocardial infarction, gastrointestinal bleeding, renal failure, and cerebrovascular accident.
Figure 1.
The distribution of hemoglobin levels.
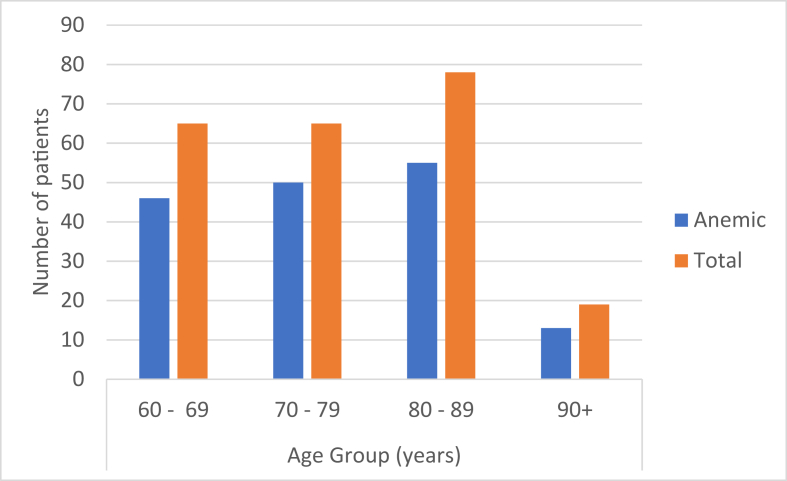
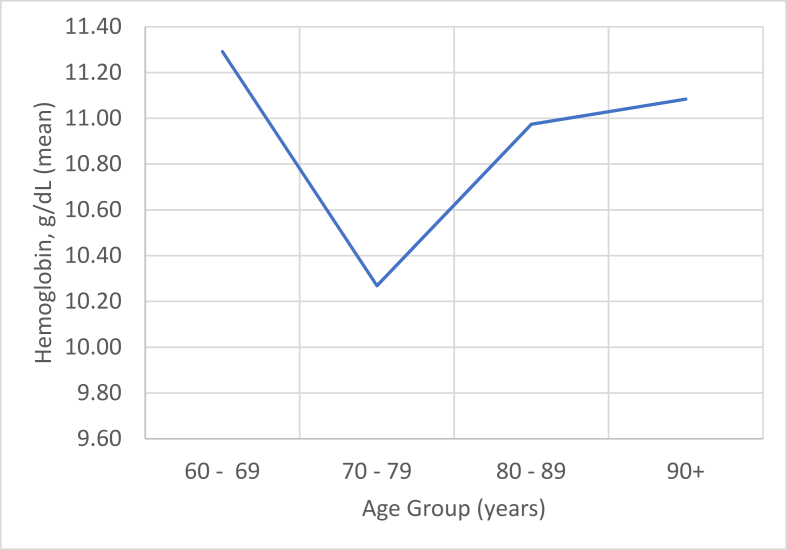
The commonest type of anemia among our patients was ACD (48.2%, n = 79) followed by IDA (28.0%, n = 46) (Table 1). Only 7 (4.3%) patients had low folate and/or vitamin B12 levels as the underlying cause. Patients between the ages of 70 and 79 years had the highest prevalence of anemia (76.9%) (Figure 2) and the lowest mean hemoglobin level (10.3 g/dL) (Figure 3).
Figure 2.
The prevalence of anemia among different age groups.
Figure 3.
Mean hemoglobin level trends among different age groups.
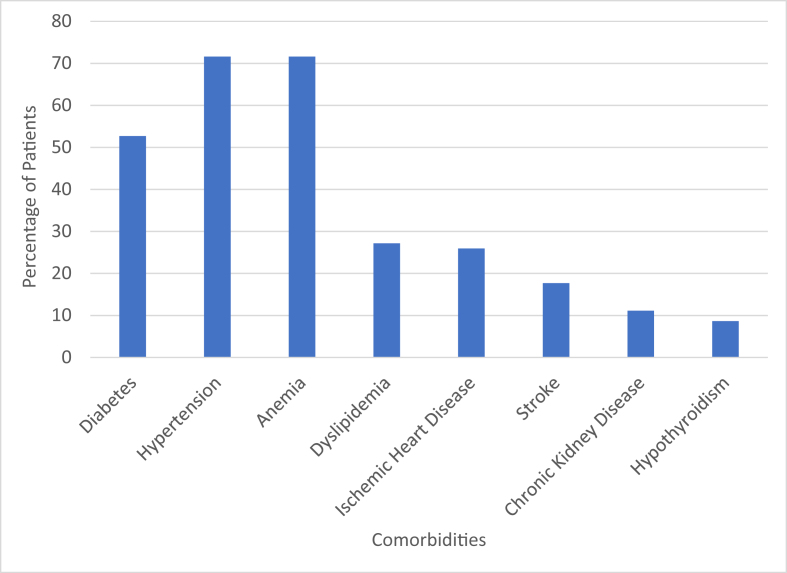
Anemia was the most common comorbidity among hospitalized elderly patients (72.2%) followed by hypertension (71.4%) and DM (53.7%) (Figure 4). Other conditions included dyslipidemia, ischemic heart disease, stroke, and chronic kidney disease.
Figure 4.
The prevalence of different comorbidities among all patients.
Outcomes of anemia
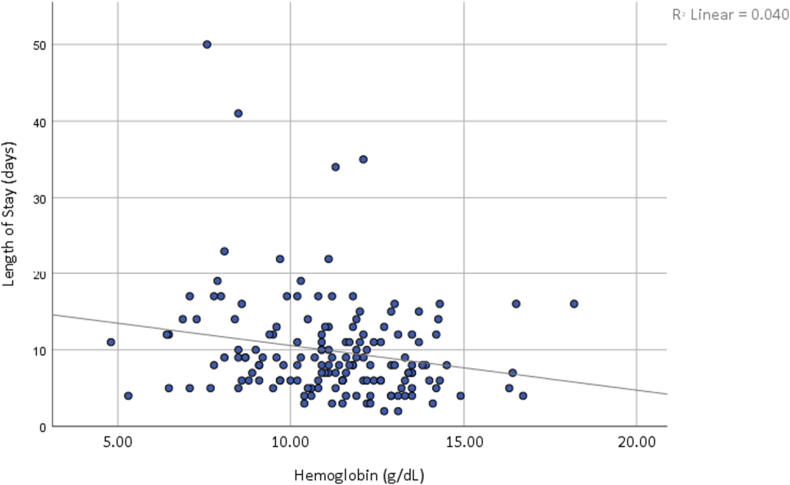
There were significant differences in health outcomes when comparing anemic with non-anemic patients. The length of stay for anemic patients was significantly longer (p < 0.001) (Table 2). As opposed to mild and moderate anemia, patients with severe anemia had a 129% higher likelihood of staying in the hospital for more than 9 days (odds ratio [OR] = 2.29; 95% confidence interval [CI]: 1.309–3.986). Pearson's correlation coefficient was calculated to assess the correlation between the length of hospital stay and hemoglobin levels; there was a negative correlation between these parameters (r(168) = −0.2, p < 0.05; Figure 5). Outliers (length of stay >80 days) and patients who died in hospital were excluded from this part of the analysis. In addition, there was a significant difference in 1-year mortality between the two groups (P < 0.001). There was, however, no significant difference in premorbid Katz index, the number of chronic illnesses, and the number of regular medications.
Figure 5.
The correlation between the length of hospital stay and hemoglobin levels.
Binary logistic regression analysis was used to predict independent risk factors for 1-year mortality. Higher Katz scores reduced the odds of 1-year mortality (OR = 0.77; p = 0.003). When compared to those with mild anemia, patients with moderate/severe anemia were more likely to die (OR = 2.2; 95% CI 1.27–4.92). Other significant risk factors for mortality within 1 year included age (OR = 1.14, p < 0.001) and length of stay (OR = 1.034, p = 0.046). Other parameters, including polypharmacy, comorbidities, and hemoglobin levels, were not found to be statistically significant as risk factors.
Discussion
Overview and prevalence
According to the criteria set by the WHO, our study demonstrated a very high prevalence of anemia among older adults admitted to hospital. Worldwide, several studies have reported the prevalence of anemia in elderly patients admitted in an acute setting; this prevalence ranged from 43.9% to 71.0%.8,15, 16, 17, 18, 19 Our high-end prevalence could be due to the severity of illness in our population who had mean Katz scores of moderate dependence and a relatively high 1-year mortality rate (50.7%) compared to other similar studies, such as Abrahamsen et al.20 (17%) and Joosten et al.21 (21%). In addition, most other studies have examined older adults in the community or ambulant patients.2,22 Anemia was also found to be significantly more prevalent among elderly males as compared to females. A similar trend of male predominance has been reported in the literature.23, 24, 25 This could be in part due to the different sex-specific criteria for defining anemia set by the WHO. It should also be noted that the males in our study did not have significantly higher rates of chronic illnesses, polypharmacy, or a lower functional status compared to females. However, they did have a higher mean age than females (77.03 and 76.24 years respectively, p = 0.014); 42.9% of patients were aged 80 years or above (p = 0.024).
The existing literature demonstrates a correlation between increasing age and a reduction in hemoglobin level.2 Patel et al. reported that the prevalence of anemia increases with advancing age after the age of 50 and exceeds 20% in those ≥85 years of age among community dwelling individuals.24 Our results, however, did not show any statistically significant difference with advancing age. This may be related to our specifically selected cohort. Since our study subjects all had serious issues that required admission to hospital, it is presumed that they are at high risk of comorbidities including anemia, regardless of age. Studies performed in the community would include all elderly patients with variable serious health issues whereas our study included those with severe health issues and therefore an increased risk of anemia, even in younger age groups.
With regards to the severity of anemia, our study demonstrated that most elderly hospitalized patients had moderate anemia. This is contrary to other similar studies where mild anemia was most predominant.3,19,26 Our findings, however, were similar to those reported by Joshi et al. and Randi et al., who reported moderate anemia in 58.8% and 49% of patients, respectively.8,23 This could be related to the fact that elderly patients requiring hospital admission are acutely unwell with multiple chronic illnesses, leading to a lower proportion of admissions of mild as compared to moderate anemia. This is further supported by the fact that most studies examining older adults in community dwellings demonstrated a higher proportion of mild anemia among their cohorts.2,24,27 In our study, mild anemia was present in one out of three patients. Even in its mild forms, anemia is commonly associated with unwanted outcomes with regards to morbidity and mortality in older individuals.28 This stresses the fact that even milder degrees of anemia can have a negative impact and should not be considered a normal physiological change of aging.
Multiple etiologies
Given the negative impact anemia has on desired outcomes, clinicians must identify the etiological origins of anemia in “all” cases to facilitate the selection of optimal therapy.
In the elderly, multiple factors can contribute to the pathogenesis of anemia. Clinically, it can be challenging to understand the contributing factors and underlying causes that result in anemia; this can make it even more difficult to decide on the correct management. Anemia in older adults can be categorized into four major types: 1) anemia due to chronic inflammation or chronic disease, 2) anemia due to Iron, B12, or folic acid deficiencies, 3) anemia due to renal insufficiency and, 4) unexplained anemia.2 While most of the studies investigating the etiological profile of anemia in older individuals were performed on community dwelling patients, only a few were performed on hospitalized patients.3,8,23,26,29 Comparing our results to these previous studies could prove difficult due to the variable classification methods used. However, ACD appears to be the most predominant type. In fact, ACD in addition to IDA are the most common types in hospitalized and community dwelling geriatric patients.27 In our cohort, 3 out of 4 patients either had IDA or ACD. ACD results from chronic illnesses, recurrent infections, inflammatory disorders, and malignancies.9 All of those conditions increase in prevalence with advancing age and are more likely to be encountered in an acute hospital setting as opposed to the community. This is evidenced by the characteristics of our patients, including a high number of comorbidities, polypharmacy, and the fact that most admissions were due to infections. Other studies have also demonstrated that folic acid and vitamin B12 deficiencies are the least common causes of anemia.8,26
Clinical impact
According to the literature, anemia in the elderly is usually mild with hemoglobin levels being around 11–12 g/dL.2,24,27 Being mild usually creates a misleading perception of low importance. On the contrary, anemia in older individuals has been associated with a magnitude of negative outcomes, including decreased functional status,20 recurrent falls,5 cognitive decline and dementia,2,7 prolonged hospital stay,6,8,15,19 and increased mortality.6,8 In this study, we investigated the relationship between anemia and the length of hospital stay, 1-year mortality, and functional status.
In agreement with the literature, the level of hemoglobin in our patients was inversely proportional to the length of stay.8,15,19 This reinforces the importance of addressing anemia in the geriatric population. In addition, higher mortality rates are usually observed in patients with anemia.6,8 This was noted in our study upon comparison of both groups. Moreover, moderate/severe anemia was associated with greater odds of 1-year mortality compared to mild anemia.
In addition to its correlation with mortality, anemia plays a role in morbidity.28 In fact, anemia is considered a major comorbidity in itself. Our study demonstrated that anemia is as prevalent as major comorbid conditions such as DM and hypertension. Even though anemia is highly prevalent and leads to poor outcomes, it is usually underreported and undertreated.8,28
Several studies have reported a significant difference in functional status between both groups favoring non-anemic patients.1,20 The reduced level of function in anemic individuals could be due to chronic suboptimal delivery of oxygen to organs that are ageing and possibly already damaged.4 While the premorbid Katz index in our study was found to be an independent risk factor for 1-year mortality for all patients, there was no significant association found between this index and hemoglobin levels. Similarly, Joosten et al. reported no significant difference in premorbid Katz index when compared between anemic and non-anemic older adults admitted to an acute geriatric ward.21 This is possibly due to the characteristics of our patients. Most of our participants, whether they were anemic or not, were severely unwell with a poor baseline condition, as evidenced by the high mortality rate and high prevalence of anemia.
Limitations
Our study has several limitations. The study included subjects who were selected from patients admitted under general medicine service in hospital which may not represent all patients in other services or treatment settings. Also, the rates of readmission were not included; these data may have been of value in determining prognostic features. Specific treatment given during the hospital admission to target anemia (or lack thereof) was not included in the data collection, so it is not known whether that influenced the outcomes being studied. Moreover, data was not available for the dietary habits of patients, nutritional supplementation, and socio-economic and living arrangements of the patients. Future studies with longer follow-up are recommended. These could include comparisons between younger and older adults and between the different etiologies of anemia and prognostic outcomes. In addition, further research is now needed to better understand the mechanisms and treatment benefits of ACD given its very high prevalence among older individuals.
Conclusion
The global prevalence of anemia in the elderly is high. It is even higher among the hospitalized. Our results showed higher values than previously reported, thus reiterating the significance of anemia. In addition, our findings demonstrate the unquestionable role of anemia in developing poorer health outcomes including prolonged hospitalization and mortality. Overall, there is no doubt about the significance of hemoglobin levels. Physicians should pay close attention in addressing anemia as a chronic disease with significant impact on the patient's health including early recovery and clinical improvement from several pathological conditions. Hence, the appropriate therapeutic option has to be taken into account by considering the cause of anemia. It is imperative that anemic older adults receive adequate clinical attention and that anemia is not simply considered a normal part of the ageing process. Therefore, implementing preventative strategies, early detection, and the treatment of anemia in older adults should be of utmost importance to clinicians and administrators alike. Our study is the first of its kind locally demonstrating the impact of anemia on elderly hospitalized patients. Further studies, preferably longitudinal, are now needed to study its impact on function, disease progression, and quality of life.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
The study was conducted after approval from the secondary health care research committee at the Ministry of Health in Bahrain [Approval number 14-19 dated 19/11/2019].
Authors contributions
MA conceptualized the study and proofread the final draft; AJA and ASA collected the data, contributed to the introduction, and proofread the draft; SSA and KS contributed to data analysis, methodology, and formulation of the graphics. KA conceptualized the study, contributed to the discussion and conclusion, and proofread the draft. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Kassebaum N.J., GBD 2013 Anemia Collaborators The global burden of anemia. Hematol Oncol Clin N Am. 2016 Apr;30(2):247–308. doi: 10.1016/j.hoc.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Guralnik J.M., Eisenstaedt R.S., Ferrucci L., Klein H.G., Woodman R.C. Prevalence of anemia in persons 65 years and older in the United States: evidence for a high rate of unexplained anemia. Blood. 2004 Oct 15;104(8):2263–2268. doi: 10.1182/blood-2004-05-1812. [DOI] [PubMed] [Google Scholar]
- 3.Petrosyan I., Blaison G., Andrès E., Federici L. Anaemia in the elderly: an aetiologic profile of a prospective cohort of 95 hospitalised patients. Eur J Intern Med. 2012 Sep;23(6):524–528. doi: 10.1016/j.ejim.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 4.Girelli D., Marchi G., Camaschella C. Anemia in the elderly. Hemasphere. 2018 Apr 17;2(3):e40. doi: 10.1097/HS9.0000000000000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Penninx B.W., Pluijm S.M., Lips P., Woodman R., Miedema K., Guralnik J.M., et al. Late-life anemia is associated with increased risk of recurrent falls. J Am Geriatr Soc. 2005 Dec;53(12):2106–2111. doi: 10.1111/j.1532-5415.2005.00491.x. [DOI] [PubMed] [Google Scholar]
- 6.Culleton B.F., Manns B.J., Zhang J., Tonelli M., Klarenbach S., Hemmelgarn B.R. Impact of anemia on hospitalization and mortality in older adults. Blood. 2006 May 15;107(10):3841–3846. doi: 10.1182/blood-2005-10-4308. [DOI] [PubMed] [Google Scholar]
- 7.Andro M., Le Squere P., Estivin S., Gentric A. Anaemia and cognitive performances in the elderly: a systematic review. Eur J Neurol. 2013 Sep;20(9):1234–1240. doi: 10.1111/ene.12175. [DOI] [PubMed] [Google Scholar]
- 8.Randi M.L., Bertozzi I., Santarossa C., Cosi E., Lucente F., Bogoni G., et al. Prevalence and causes of anemia in hospitalized patients: impact on diseases outcome. J Clin Med. 2020 Mar 30;9(4):950. doi: 10.3390/jcm9040950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poggiali E., Migone De Amicis M., Motta I. Anemia of chronic disease: a unique defect of iron recycling for many different chronic diseases. Eur J Intern Med. 2014 Jan;25(1):12–17. doi: 10.1016/j.ejim.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 10.Ershler W.B., Sheng S., McKelvey J., Artz A.S., Denduluri N., Tecson J., et al. Serum erythropoietin and aging: a longitudinal analysis. J Am Geriatr Soc. 2005 Aug;53(8):1360–1365. doi: 10.1111/j.1532-5415.2005.53416.x. [DOI] [PubMed] [Google Scholar]
- 11.Al Haddad L., Al-Dubaib R., Al-Najem W., Al-Shaikh Z., Al-Ghawi A. Iron deficiency anemia among 3-year-old children and its management in primary health care in Bahrain. J Bahrain Med Soc. 2017;29(3):35–40. doi: 10.26715/jbms.29.3.2017.44a. [DOI] [Google Scholar]
- 12.Merza R., Alekri R., Alekri S., Alsaleh A., Alnasir F. The prevalence and factors associated with iron deficiency anemia in anemic pregnant women. Bahrain Med Bull. 2014;36(3):172–176. doi: 10.12816/0008112. [DOI] [Google Scholar]
- 13.Katz S., Foed A.B., Moskowitz R.W., Jackson B.A., Jaffe M.W. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization . vol. 405. 1968. pp. 1–40. (Nutritional anemia: report of a WHO scientific group). Technical Report Series. [Google Scholar]
- 15.Migone De Amicis M., Poggiali E., Motta I., Minonzio F., Fabio G., Hu C., et al. Anemia in elderly hospitalized patients: prevalence and clinical impact. Intern Emerg Med. 2015 Aug;10(5):581–586. doi: 10.1007/s11739-015-1197-5. [DOI] [PubMed] [Google Scholar]
- 16.Hamid M., Naz A., Alawattegama L.H., Steed H. The prevalence of anaemia in a district general hospital in the United Kingdom. Cureus. 2021;13(5) doi: 10.7759/cureus.15086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tay M.R.J., Ong Y.Y. Prevalence and risk factors of anaemia in older hospitalised patients. Proc Singapore Healthc. 2011;20(2):71–79. doi: 10.1177/201010581102000202. [DOI] [Google Scholar]
- 18.Bashir F., Nageen A., Kidwai S.S., Zulfikar S., Shiraz S., Ara J. Anemia in hospitalized patients: prevalence, etiology and risk factors. J Liaquat Univ Med Health Sci. 2017;16(2):80–85. doi: 10.22442/jlumhs.171620511. [DOI] [Google Scholar]
- 19.Zaninetti C., Klersy C., Scavariello C., Bastia R., Balduini C.L., Invernizzi R. Prevalence of anemia in hospitalized internal medicine patients: correlations with comorbidities and length of hospital stay. Eur J Intern Med. 2018;51:11–17. doi: 10.1016/j.ejim.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 20.Abrahamsen J.F., Monsen A.L., Landi F., Haugland C., Nilsen R.M., Ranhoff A.H. Readmission and mortality one year after acute hospitalization in older patients with explained and unexplained anemia - a prospective observational cohort study. BMC Geriatr. 2016;16:109. doi: 10.1186/s12877-016-0284-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joosten E., Detroyer E., Milisen K. Effect of anaemia on hand grip strength, walking speed, functionality and 1 year mortality in older hospitalized patients. BMC Geriatr. 2016 Aug 19;16(1):153. doi: 10.1186/s12877-016-0326-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Inelmen E.M., D'Alessio M., Gatto M.R., Baggio M.B., Jimenez G., Bizzotto M.G., et al. Descriptive analysis of the prevalence of anemia in a randomly selected sample of elderly people living at home: some results of an Italian multicentric study. Aging (Milano) 1994;6(2):81–89. doi: 10.1007/BF03324220. [DOI] [PubMed] [Google Scholar]
- 23.Joshi I., Thakur S., Bhawani R., Kaushal V., Mahajan A. Clinical profile and etiology of anaemia in elderly: a hospital based study at a tertiary care in the Sub-Himalayan region. JIAG. 2017;13:18–22. doi: 10.35262/jiag.v13i1.18-22. [DOI] [Google Scholar]
- 24.Patel K.V. Epidemiology of anemia in older adults. Semin Hematol. 2008 Oct;45(4):210–217. doi: 10.1053/j.seminhematol.2008.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sanford A.M., Morley J.E. Editorial: anemia of old age. J Nutr Health Aging. 2019;23(7):602–605. doi: 10.1007/s12603-019-1214-x. [DOI] [PubMed] [Google Scholar]
- 26.Geisel T., Martin J., Schulze B., Schaefer R., Bach M., Virgin G., et al. An etiologic profile of anemia in 405 geriatric patients. Anemia. 2014;2014:932486. doi: 10.1155/2014/932486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tettamanti M., Lucca U., Gandini F., Recchia A., Mosconi P., Apolone G., et al. Prevalence, incidence and types of mild anemia in the elderly: the “Health and Anemia” population-based study. Haematologica. 2010;95(11):1849–1856. doi: 10.3324/haematol.2010.023101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nissenson A.R., Goodnough L.T., Dubois R.W. Anemia: not just an innocent bystander? Arch Intern Med. 2003;163(12):1400–1404. doi: 10.1001/archinte.163.12.1400. [DOI] [PubMed] [Google Scholar]
- 29.Bhasin A., Rao M.Y. Characteristics of anemia in elderly: a hospital based study in South India. Indian J Hematol Blood Transfus. 2011 Mar;27(1):26–32. doi: 10.1007/s12288-011-0056-4. [DOI] [PMC free article] [PubMed] [Google Scholar]