Abstract
Purpose
To report a 56-year-old male in Saudi Arabia who developed signs of aberrant facial nerve regeneration after recovering from Bell's palsy associated with COVID-19 infection.
Observations
The patient presented, months following recovery from Bell's palsy associated with COVID-19, with symptoms of aberrant seventh nerve regeneration in the form of tearing with eating “crocodile tears” and synchronous right eyelid closure with the jaw movement.
Conclusions and Importance
Case reports of Bell's palsy associated with COVID-19 are emerging, but association does not mean causation. That said, we need to report these cases to draw attention to the possible neuroinvasive propensity of this virus. It is also imperative to recognize Bell's palsy as a possible symptom of COVID-19.
Keywords: COVID-19, Infection, Ophthalmology, Peripheral nerve disease, Bell's palsy
1. Introduction
Bell's palsy is considered an acute idiopathic facial nerve palsy. Although the majority of patients with Bell's palsy achieve complete recovery without medical interventions, a subset of patients develop long-term sequelae, such as aberrant nerve regeneration where axons of regenerating nerve fibers reach different muscle targets than their original targets during the recovery process.1, 2, 3 The incidence rate of this aberrant nerve regeneration after Bell's palsy ranged from 8.6% to 28%,1,4 and there is a potential correlation between the severity of Bell's palsy and this sequelae.4 Several reports have linked Bell's palsy with Coronavirus disease (COVID-19), caused by a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).5, 6, 7 The first Bell's palsy case after COVID-19 was reported early in the pandemic in the month of April 2020.8 However, the hypothesis regarding the neuropathogenesis of COVID-19 is still debatable.9
We present a case of a COVID-19 patient who developed Bell's palsy and signs of aberrant nerve regeneration as long-term sequelae.
2. Case report/findings
A 56-year-old patient with type 2 diabetes and hypertension -both well controlled with medications-, developed right-sided Bell's palsy three days after the confirmation of COVID-19 using nasopharyngeal swab polymerase chain reaction (PCR) in the summer of 2020. Initially, the patient exhibited a sore throat and fever; afterward, his sense of smell and taste was lost. Eventually, the patient developed right facial weakness with an uneven smile that prompted him to get a teleconsultation with a neurologist who diagnosed the patient with Bell's palsy via video chat. However, due to the patient's uncomplicated and mild course of COVID-19, he was never hospitalized and was only managed on an outpatient basis. Approximately less than a month later the patient had an in-office visit with an otolaryngologist, who confirmed Bell's palsy diagnosis and referred the patient to a physiotherapist without pharmacological interventions.
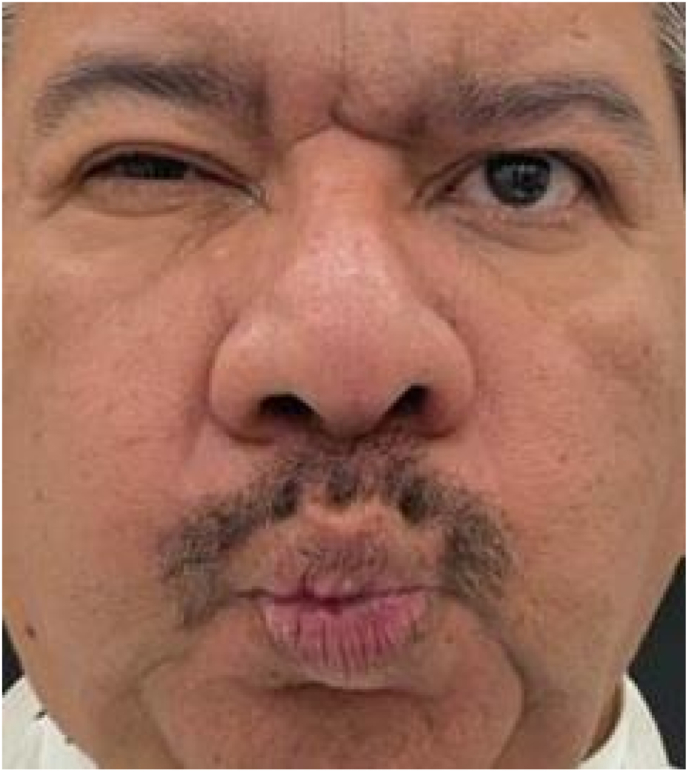
Ten months after recovery from COVID-19, the patient presented to the ophthalmology clinic with symptoms of aberrant seventh nerve regeneration in the form of tearing while eating “crocodile tears” and synchronous right eyelid closure with jaw movement. After conducting a general examination, the patient showed a fairly symmetrical face with more dermatochalasis on the right side. The marginal reflex distance 1 of the right eye was 2 mm, and for the left eye was 5 mm. The palpebral fissure height of the right eye was 7 mm, and for the left eye was 10 mm. Levator function was excellent in the right eye and the left eye at 15 mm and 17 mm, respectively. The tear breakup time for the right eye was 2 seconds and for the left eye was 3 seconds. When asked to move the jaw sideways (Fig. 1) or purse the lips (Fig. 2), the palpebral fissure of the right eyelid involuntary narrowed. (video).
Fig. 1.
Image showing right palpebral fissure narrowing with lateral jaw movement to the right and normal right eyelid with lateral jaw movement to the left.
Fig. 2.
Image showing the involuntary narrowing of the right palpebral fissure upon contraction of orbicularis oris muscle.
A few months after Bell's palsy and due to persistent right facial weakness, the neurologist ordered a magnetic resonance imaging (MRI) of the brain to rule out vascular and tumoral causes of seventh nerve palsy. The MRI revealed inflammatory changes of paranasal sinuses accompanied by nonspecific subcortical flat-attenuated inversion recovery signs on the white matter, but no significant intracranial findings were found.
As for the management, the patient was managed conservatively at the start of Bell's palsy with physiotherapy. Then, he continued the recommended exercises at home and exhibited significant improvement in the degree of facial weakness.
3. Discussion
Bell's palsy is currently the most common disorder affecting the seventh cranial nerve. The mechanism of Bell's palsy is still unclear, but viral, ischemic, and immune-mediated mechanisms have been postulated.10,11 Moreover, it is known that coronaviruses have neuroinvasive propensity and COVID-19 patients have presented with central and peripheral nervous system disorders “including Bell's palsy”.12 In a recent retrospective study, an estimated incidence of Bell's palsy was 0.08% higher in patients with COVID-19, which translates to approximately 82 per 100 000 patients with COVID-19.13 Multiple hypotheses regarding the pathogenesis of Bell's palsy in COVID-19 patients have been proposed. One of the most accepted hypotheses is molecular mimicry, where mimicry between microbial and nerve antigens is thought to be a major driving force behind the development of the disorder.14 The other hypothesis of neural ischemia cannot be ruled out in this case, especially since hypercoagulability has been demonstrated in some patients with COVID-19.15 Additionally, our patient already has vasculopathic risk factors; hence, the exact cause of the Bell's palsy in our patient cannot be pinpointed.
Aberrant seventh nerve regeneration can be a sequela of Bell's palsy and can present as an involuntary synchronous narrowing of the palpebral fissure with pursing of the lips due to the abnormal intrafacial connections between the orbicularis oculi and orbicularis oris both of which supplied by the seventh cranial nerve.11,14 This connection has been termed Marin-Amat syndrome in the previous literature.16 However, it has been heavily argued by Wartenberg et al. that this is solely an intrafacial associated movement that commonly occurs after facial paralysis.17 The argument made by Wartenberg et al. was supported by the available electromyography studies found in some case reports.18 Moreover, our patient exhibited tearing with eating, which can happen when the regenerating nerve redirects and reaches the lacrimal gland. This abnormal innervation will cause tearing with the taste or smell of food instead of causing salivation.19
Further studies regarding the surge in cases of Bell's palsy associated with COVID-19 are necessary to understand this connection, which also can shed a light on the possible emerging relationship between Bell's palsy and the COVID-19 vaccine as depicted in some published articles.20
4. Conclusions
A causal relationship between COVID-19 and Bell's palsy still cannot be proven, but it is imperative to report these cases. With the reports of Bell's palsy are emerging during the pandemic, larger observational studies are needed to investigate this connection and the possible neuroinvasive propensity of this virus.
Patient consent
The patient provided consent to use his images and clinical history for education and publication.
Funding
No funding was received for this work.
Author agreement statement
The submission, or parts of it, is not currently submitted elsewhere for publication. All coauthors and acknowledged parties have read and approved the final revised manuscript.
Author’s contributions
Furat Alrajhi and Hadeel Seraj performed the literature review and writing of the manuscript. Nada Taher and Ahmed Alnabihi obtained pertinent clinical data and clinical images as well as editing of the manuscript.
Declaration of competing interest
The authors have no disclosures to report.
Acknowledgments
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajoc.2022.101679.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
https://drive.google.com/file/d/1trllKw-GBN1bW9QKOcn5hIrYEqep6_zo/view?usp=sharing.
Video: Video showing the involuntary narrowing of the right palpebral fissure upon contraction of orbicularis oris muscle.
References
- 1.Peitersen E. Bell's palsy: the spontaneous course of 2,500 peripheral facial nerve Palsies of different etiologies. Acta Otolaryngol. 2002 Jan 1;122(7):4–30. [PubMed] [Google Scholar]
- 2.Crumley R.L. Mechanisms of synkinesis. Laryngoscope. 1979;89(11):1847–1854. doi: 10.1288/00005537-197911000-00020. [DOI] [PubMed] [Google Scholar]
- 3.Wu Z.B., Silverman C.A., Linstrom C.J., Tessema B., Cosetti M.K. Objective computerized versus subjective analysis of facial synkinesis. Laryngoscope. 2005;115(12):2118–2122. doi: 10.1097/01.mlg.0000182811.49686.76. [DOI] [PubMed] [Google Scholar]
- 4.Ramsey D.J., Haas L.P., Tucker S.M. Long-term outcome after acute peripheral facial palsy. Ophthalmic Plast Reconstr Surg. 2022 Aug;38(4):381–386. doi: 10.1097/IOP.0000000000002134. [DOI] [PubMed] [Google Scholar]
- 5.Guan W jie, Ni Z yi, Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 Apr 30;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nath A. Neurologic complications of coronavirus infections. Neurology. 2020 May 12;94(19):809–810. doi: 10.1212/WNL.0000000000009455. [DOI] [PubMed] [Google Scholar]
- 7.Mao L., Jin H., Wang M., et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020 Jun 1;77(6):683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wan Y., Cao S., Fang Q., Wang M., Huang Y. https://europepmc.org/article/PPR/PPR152025 Coronavirus disease 2019 complicated with Bell’s palsy: a case repor [Internet]. 2020 [cited 2022 Jul 29]. Available from:
- 9.Gupta S., Jawanda M.K., Taneja N., Taneja T. A systematic review of Bell's Palsy as the only major neurological manifestation in COVID-19 patients. J Clin Neurosci. 2021 Aug 1;90:284–292. doi: 10.1016/j.jocn.2021.06.016. [DOI] [PubMed] [Google Scholar]
- 10.Zhang W., Xu L., Luo T., Wu F., Zhao B., Li X. The etiology of Bell's palsy: a review. J Neurol. 2020 Jul 1;267(7):1896–1905. doi: 10.1007/s00415-019-09282-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dahl E.H., Mosevoll K.A., Cramariuc D., Vedeler C.A., Blomberg B. COVID-19 myocarditis and postinfection Bell's palsy. BMJ Case Rep CP. 2021 Jan 1;14(1) doi: 10.1136/bcr-2020-240095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sepehrinezhad A., Shahbazi A., Negah S.S. COVID-19 virus may have neuroinvasive potential and cause neurological complications: a perspective review. J Neurovirol. 2020 Jun 1;26(3):324–329. doi: 10.1007/s13365-020-00851-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tamaki A., Cabrera C.I., Li S., et al. Incidence of Bell palsy in patients with COVID-19. JAMA Otolaryngol Head Neck Surg. 2021 Aug 1;147(8):767–768. doi: 10.1001/jamaoto.2021.1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nepal G., Rehrig J.H., Shrestha G.S., et al. Neurological manifestations of COVID-19: a systematic review. Crit Care. 2020 Jul 13;24(1):421. doi: 10.1186/s13054-020-03121-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee S.G., Fralick M., Sholzberg M. Coagulopathy associated with COVID-19. CMAJ (Can Med Assoc J) 2020 May 25;192(21) doi: 10.1503/cmaj.200685. E583–E583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rana P.V., Wadia R.S. The Marin-Amat syndrome: an unusual facial synkinesia. J Neurol Neurosurg Psychiatr. 1985 Sep 1;48(9):939–941. doi: 10.1136/jnnp.48.9.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wartenberg R. Inverted marcus gunn phenomenon”: (So-Called Marin Amat syndrome) Arch Neurol Psychiatr. 1948 Dec 1;60(6):584–596. [Google Scholar]
- 18.Frueh B.R. Associated facial contractions after seventh nerve palsy Mimicking jaw-winking. Ophthalmology. 1983 Sep 1;90(9):1105–1109. doi: 10.1016/s0161-6420(83)80053-0. [DOI] [PubMed] [Google Scholar]
- 19.Modi P., Arsiwalla T. StatPearls [Internet]. Treasure Island (FL) StatPearls Publishing; 2022. Crocodile Tears Syndrome.http://www.ncbi.nlm.nih.gov/books/NBK525953/ [cited 2022 Jun 8]. Available from: [Google Scholar]
- 20.Colella G., Orlandi M., Cirillo N. Bell's palsy following COVID-19 vaccination. J Neurol. 2021 Oct 1;268(10):3589–3591. doi: 10.1007/s00415-021-10462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.