Abstract
Background and aims
The COVID-19 pandemic affected the processes of routine care for chronic patients due to disrupted delivery care. The aim of the present study is to verify the COVID-19 pandemic effects on diabetes control and management.
Methods and results
The study was designed as a retrospective observational study, performed on two cohorts of patients with diabetes in 2019 and 2020. Data used for the analyses were gathered from administrative and laboratory databases, which do not include any sensible information on COVID-19. The Tuscany Regional Health Agency is data controller for current administrative databases and has been working to produce available information for policy decision-making.
In 2020, in comparison with 2019, a relevant reduction of the number of patients measuring HbA1c was observed during the March–April lockdown, and again during the second pandemic wave in Autumn. A similar pattern was observed for specialist visits for diabetes, for which the introduction of televisits only partly compensated for the reduction of traditional office visits. The number of patients receiving drugs for diabetes each week in 2020 was very similar to 2019. The mean HbA1c values and the proportion of HbA1c values > 8% for each week, were higher during the 2020 Spring and Autumn lockdown.
Conclusion
COVID-19 pandemic negatively impacts diabetes management, reducing specialist visits and HbA1c determinations during the first and second pandemic wave. Despite a satisfactory continuity in pharmacological treatment, short-term impairment of average glycemic control was detected, particularly in Autumn.
Keywords: COVID-19, Diabetes mellitus, HbA1c
1. Introduction
The COVID-19 pandemic affected the processes of routine care for chronic patients due to disrupted delivery care [1]. In-person physical face-to-face visits had ceased due to government restriction, greater instilled fear, and focus shifted toward COVID care. In addition, patients have less chance for community-based support and care [1,2]. Worldwide, the pandemic adversely affected clinical decision-making by limiting laboratory testing and physical examination [3,4]. During the outbreak of the pandemic, hospitalization rate, emergency department visits and inpatient clinic visits of chronic diseases were significantly reduced [2].
For people with diabetes, the lockdown can be expected to exert a negative impact on the management of diabetes due to the anxiety and depression that can be generated by the concern about the risk of infection, the uncertainties for medical and pharmacologic supply and the impossibility to access regularly consultation with health care providers. Available data in people with type 1 diabetes [5,6](T1DM) have been reassuring, showing no worsening of glycemic control. A recent meta-analysis of trials on the effects of confinement due to lockdown measures on glycemic control, failed to detect significant detrimental effects on HbA1c in either T1DM or T2DM [7]. Most patients with type 2 diabetes avoided a deterioration of HbA1c and body weight during the lockdown. Telemedicine could have mitigated the negative impact of lockdown [8].
The COVID-19 epidemic and the lockdown measures have significantly reduced healthcare quality standards, such as control of LDL cholesterol and blood pressure. The indicators with the greatest negative effect were those of screening, e.g. for diabetic foot [9].
During the first pandemic wave, in March 2020, lockdown measures adopted in Italy restricted the access to specialist visits, general practitioners, and the collection of blood samples for laboratory measurements to urgent cases [10]. Later during the year, the second pandemic wave forced many specialists to dedicate part of their working hours to COVID-19 wards, limiting the availability of specialist care.
The Tuscany Regional Health Agency (TRHA) has a long-standing epidemiological experience in monitoring the main chronic conditions affecting people living in the Italian Region of Tuscany. Since the first beginning of the COVID-19 epidemic in Italy, the Agency has been working to produce available information for policy decision-making and citizens. The aim of the present study is to verify the COVID-19 pandemic effects on diabetes control and management.
2. Methods
The study was designed as a retrospective observational study, performed on two cohorts of patients with diabetes in 2019 and 2020. Patients were included if on January 1st, 2019 or 2020, they were residents in Tuscany and aged over 40 years, and they had a diagnosis of diabetes. Diabetes was identified either by a previous diagnosis of diabetes (ICD-9-CM code 250∗) in hospital discharge records, two or more prescriptions of drugs for diabetes (ATC2 code A10) in the same year, a certified diagnosis of diabetes for full reimbursement of diabetes-related healthcare services, and/or a previous determination of HbA1c over 6.5% (see Table 1 of Supplementary Material for greater detail). Separate analyses were performed in sub-cohort of subjects with at least one determination of HbA1c during the following year (both for 2019 and 2020).
For each of the two cohorts (2019 and 2020), for each week of the following year, the proportion of subjects with at least one specialist visit for diabetes, the dispensation of drugs for diabetes and the determination of HbA1c were assessed. Televisits for diabetes were also retrieved. In addition, mean HbA1c values and proportion of patients with HbA1c>8% for each week were determined.
Individual information about diabetes status was gathered from the TRHA database called “MaCro”, an Italian acronym for “chronic diseases”. In the MaCro system, a validated algorithm identifies subjects as diabetic by the use of administrative data, including records from hospital discharges, drugs prescriptions, outpatient services, exemptions, home and residential care, health registry. All these sources are linked one to each other by the anonymized ID IDUNI, which is associated to every subject living in Tuscany. The algorithm loops on calendar periods from 1 January to 31 December, starting from the first past moment of data availability up to the present day. An individual is classified as affected by diabetes on 1 January of a year of interest (index date) if:
-
●
he is living in Tuscany on the index date;
-
●
he satisfied at least one identification criteria during one year or more before the index date.
Once the selection happens, the chronic status is kept until censoring for death or change of residence.
The values of HbA1c were obtained from laboratory data available for the whole region. Descriptive data are reported, without any formal statistical comparison.
Data used for the analyses were gathered from administrative and laboratory databases, which do not include any sensible information on CoViD-19. The Tuscany Regional Health Agency is data controller for current administrative databases, with the institutional mission of processing them to support policy decision-making and to produce available information for citizens. In addition, the Agency was given the responsibility for using laboratory data in order to produce healthcare indicators. For the above-described reasons, there was no need for specific ethical approval.
3. Results
Out of 229,939 patients with diabetes on January 1st, 2019, 157,598 (68%) had at least one determination of HbA1c during 2019. The corresponding figure for 2020 was 135,558 out of 230,162 patients (59%). The age distribution and geographic distribution of the two cohorts and of the sub-cohorts with at least one determination of HbA1c are reported in Tables 1 and 2 of supplementary material.
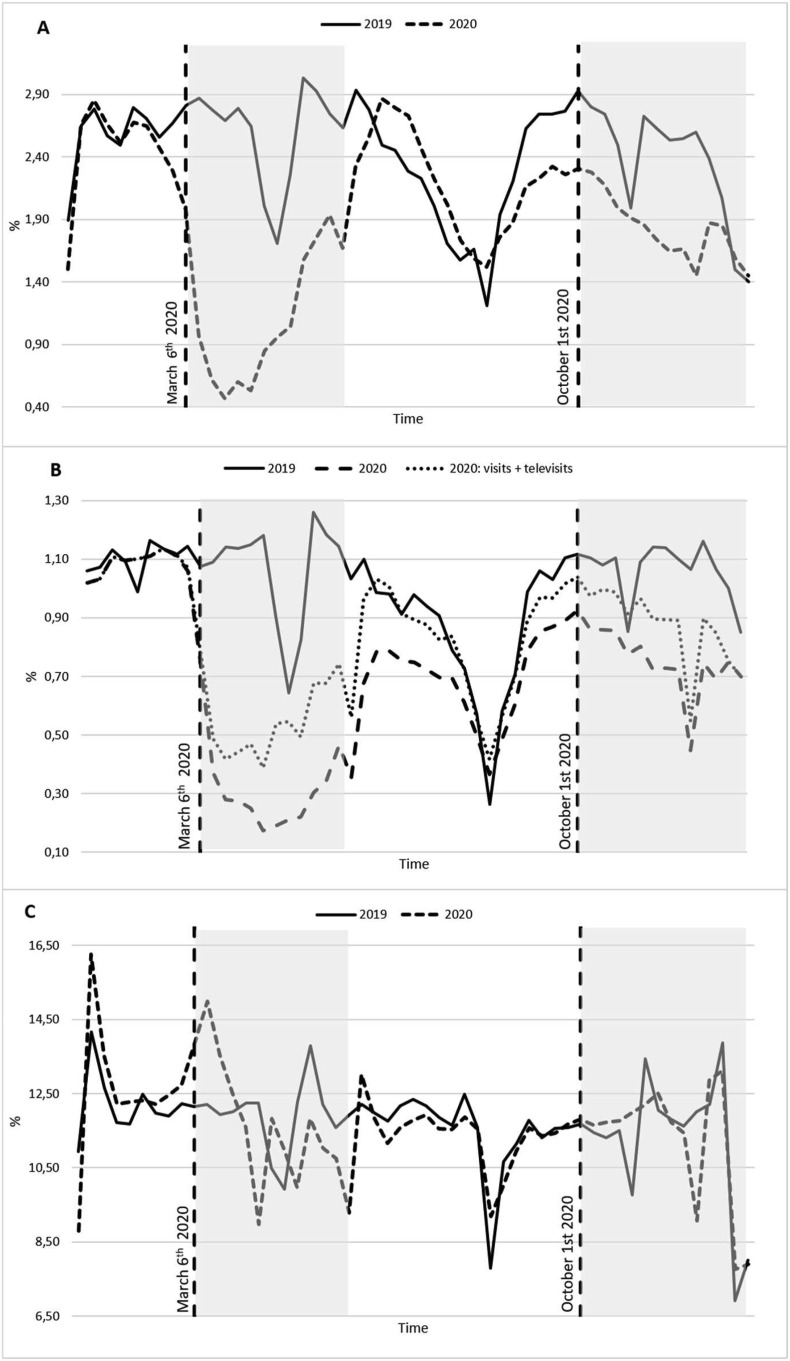
The proportion of patients with at least one determination of HbA1c for each week of 2019 and 2020 is reported in Fig. 1 , panel A, showing a reductionduring the March–April lockdown, and again during the second pandemic wave in Autumn. The proportion of patients with at least one determination of HbA1c in 2019 and 2020 was 68.5% and 58.5%, respectively; the corresponding figures for the proportion of patients receiving at least one specialist visit and/or televisit during the year was 41.7 and 47.7%. Among patients performing at least one determination of HbA1c during the year 2019, 58.4% had not received a specialist visit during the year; the corresponding figure for 2020 was 57.9%. The total number of specialist visits in 2019 was 117,247, whereas the number of visits (regular visits + televists) in 2020 was 96,814, with a reduction of patients receiving a specialist visit particularly during the first pandemic wave and, to a lesser extent, during the second wave in Autumn, and with no relevant recovery during the Summer interval. Conversely, the number of patients receiving drugs for diabetes each week in 2020 was very similar to 2019, with the only exception of the first week of the March lockdown, showing an increased dispensation of drugs (Fig. 1, panel C). Results observed in the sub-cohorts with at least one determination of HbA1c during the year were similar to those of the whole cohorts (Fig. 1, supplementary material).
Figure 1.
Weekly proportion of patients with diabetes and at least one HbA1C determination (A); withat least one visit for diabetes (B); withat least one delivery of diabetes medication (C). The x-axis represents time expressed in weeks.
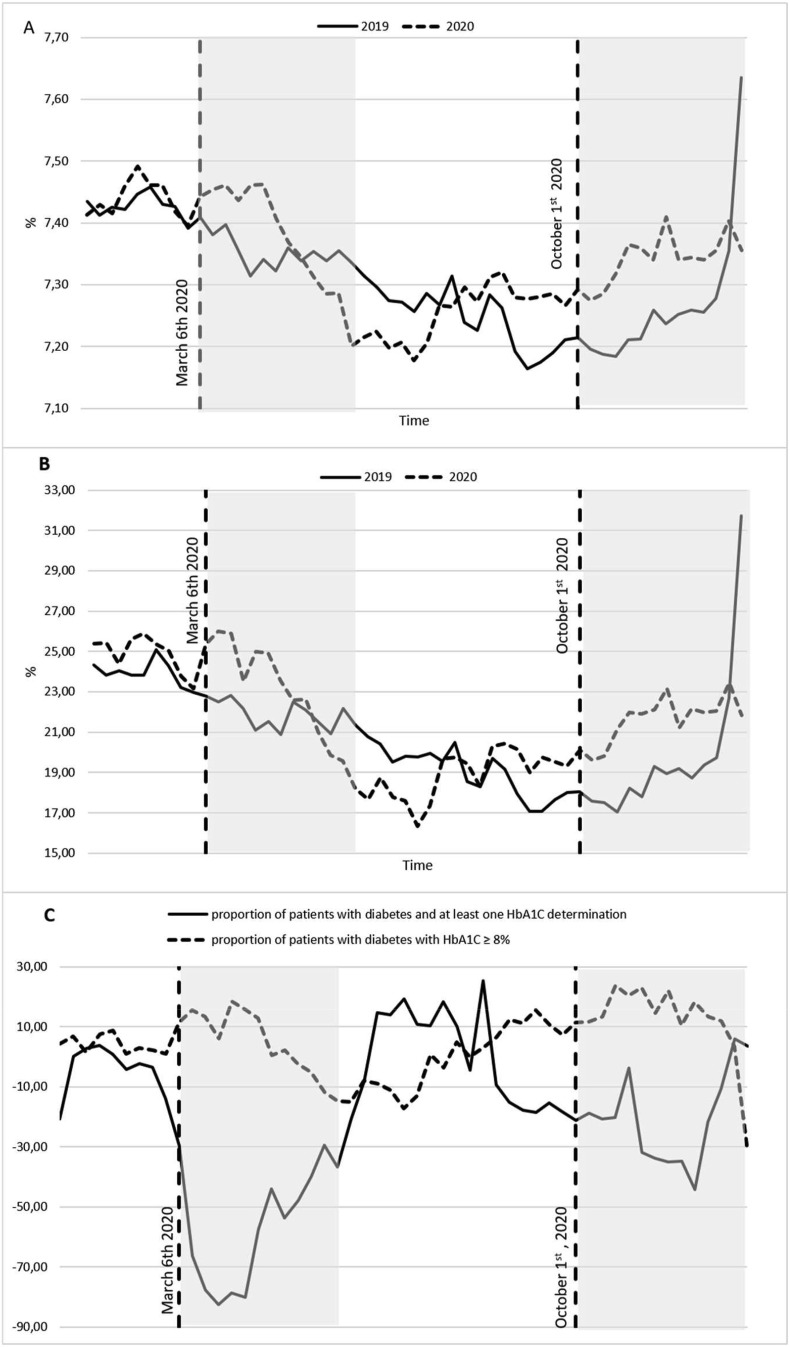
Panel A and B of Fig. 2 summarize the mean HbA1c values and the proportion of HbA1c values > 8% for each week, in 2019 and 2020. In comparison with the corresponding weeks of 2019, higher HbA1c values were observed during the 2020 Spring lockdown, and again during the Autumn pandemic wave; conversely, mean HbA1c in 2020 was lower at the beginning of Summer. Fig. 2, panel C, shows percent variations in 2020 (versus 2019) of the proportion of patients with at least one HbA1c determination and of those with HbA1c >8%, for each week. The fraction of patients with high HbA1c rises when the overall number of determinations is lower, and vice versa. In comparison with 2019, the difference in the proportion of HbA1c measures over 8% shows two distinct peaks in March and November, with an increase from 5 to 15%; the reduction in the number of weekly determinations of HbA1c reaches 57% in March and 30% in November. Overall, in 2020 mean HbA1c increased (by at least 0.1%) in 51.0% of patients, decreased in 44.1%, and remained stable in 4.9%.The proportion of patients measuring HbA1c and mean HbA1c levels were similar in men and women (suppl. Fig. 2), and in subjects aged up to or over 65 years (suppl. Figure 3).
Figure 2.
Mean HbA1c values in the 2019 and 2020 cohort (A); Weekly proportion of HbA1c determinations ≧ 8% (B); Percentage weekly variations in 2020 (versus 2019) of the proportion of patients with at least one HbA1c determination and of those with HbA1c > 8% (C).
4. Discussion
The COVID-19 pandemic appeared to have a relevant impact on the management of diabetes. In 2020, from March onwards, the number of patients performing determinations of HbA1c decreased dramatically, particularly in Spring and Autumn. In March and April, this reduction was probably the direct effect of restrictive measures which, during lockdown, imposed the suspension of non-urgent medical procedures, including the collection of blood samples for laboratory determinations. No such restriction was adopted in Autumn, when the reduction of patients measuring HbA1c was more plausibly attributable to the attitude of many patients to avoid any contact with healthcare facilities for fear of contagion. It is also possible that the regular measurement of HbA1c for assessing diabetes control was disrupted in Autumn because of the reduction in the number of specialist visits in Diabetes Outpatient Clinics; in fact, many patients measure HbA1c shortly before a specialist visit. However, a similar reduction in the frequency of HbA1c determinations was observed also in patients who never attended Specialist care.
The local healthcare system provides comprehensive integrated care for patients with diabetes, which is managed by both general practitioners and diabetes specialists. Regular specialist visits are offered to all patients with type 1 diabetes and to those with type 2 diabetes on basal-bolus insulin therapy, whereas those with type 2 diabetes not on basal bolus insulin are generally managed by general practitioners, with specialist visits performed in case of diabetic complications and whenever glycemic control as considered inadequate. In addition, before the pandemic outbreak, specialists were in charge of control visits on stable, uncomplicated patients with type 2 diabetes treated with DPP4 inhibitors, GLP1 agonists and/or SGLT2 inhibitors, since the reimbursement of those drugs was limited to specialist prescription. From March 2020 onward, and for all 2020, Regional and National determinations allowed the renewal of those prescriptions by general practices, without specialist certification, thus reducing the need for patients to access specialist facilities for non-clinical purposes. The COVID-19 pandemic interfered with this organization, determining a relevant reduction of the number of visits during the Spring lockdown, when only urgent visits could be performed. During the second pandemic wave, peaking in November, no restriction of access to Outpatient Clinics was imposed; however, a wide reduction in the number of visited patients was observed. This could be partly due to the hesitancy of some patients in approaching Outpatient Clinics; in addition, as a consequence of the admission of a large number of COVID-19 patients, many specialists were diverted from their usual occupation and transferred to support COVID-19 or non-COVID-19 Internal Medicine wards, leading to the cancellation of many planned visits in Diabetes Outpatient Clinics. Notably, despite the reduction in the number of specialist visits (which was not entirely compensated by televisits), the overall number of patients receiving at least one visit or televisit was reduced. The pandemic appears to have reduced the frequency of visits, more than the overall number of patients receiving specialist care.
Some measures were taken in order to reduce the impact of the pandemic on the management of chronic conditions. These included the development of telemedicine, with televisits (approved in Tuscany on March 16th, 2020) [11], and the introduction of the electronic prescription for drugs (from April 6th, 2020) [12]. Televisits were an effective means to substitute part of the traditional office control visits [8], overcoming restriction to physical access to Clinics and fears of patients approaching Outpatient facilities. However, the overall number of televisits did not entirely compensate for the number of lost visits: the reduced number of available specialists, particularly in Autumn, probably played a role. As a consequence, the overall number of visits (visits and televisits) in 2020 was lower than in 2019. Conversely, electronic prescription allowed for good preservation of therapeutic continuity: the number of patients receiving drugs for diabetes remained substantially stable throughout the first and second pandemic wave.
Data on measured HbA1c values are more difficult to interpret. During the epidemic peaks, when the number of determinations is lower, recorded mean values are higher. As a consequence, the mean HbA1c levels in the year increased in 2020 in a majority of patients, in comparison with 2019. This could be largely explained by a selection bias: when there are greater obstacles to routine care, patients with acute problems, who are expected to show higher mean HbA1c levels, have a greater chance of performing laboratory exams. Differences between 2020 and 2019 could therefore be interpreted as the effect of selection of more severe cases. Conversely, the impact on glycemic control of lockdown measures and home confinement per se could have been negligible, as suggested by previous studies [7,8]. However, the comparison of HbA1c levels during the first and the second wave suggests other possible mechanisms. In fact, in Autumn mean HbA1c levels were similar to those observed during the Spring lockdown, but the reduction of the number of determinations (and the related effect of selection) was wider in Spring than in Autumn. It can be speculated that a sustained reduction in specialist care during many months in 2020 produced a negative effect on glycemic control in many patients in the last months of the year. In fact, HbA1c reflects glucose levels of the previous 3–4 months, and the effect of specialist visits (with drug prescription, dietary intervention, patient education, etc.) on glucose may develop well after the visit; as a consequence, the full effect of the reduction of specialist visits on glucose control (if any) would be easier to detect in the first months of 2021, which were not included in this study. In addition, part of traditional specialist visits were replaced by televisits, without a formal assessment of their efficacy in this specific organizational context. Available evidence suggests that telemedicine in diabetes, when integrated in a well-planned healthcare pathway, can impove outcomes, but the emergency substitution of office visits with remote contacts could have had diverging effects. The design of the present study does not allow any reliable estimation of the efficacy of televisits during the 2020 pandemic outbreaks.
Several further limitations of this study should be considered when interpreting results. The sample, although wide, does not include all residents in Tuscany Region; included areas are not necessarily representative of the whole regional territory. In addition, the database includes only laboratory determinations performed in public laboratories; non-reimbursed measurements performed in private laboratories remain undetected, leading to an underestimation of the completeness of follow-up for diabetes management. Furthermore, the database captures all totally or partially reimbursed drugs dispensed in public or private pharmacies; there is no information on the actual use of dispensed drugs by patients. Adherence to pharmacological treatment could therefore have been overestimated. In addition, administrative data do not allow to discriminate between type 1, type 2, and other forms of diabetes. Furthermore, the database contains administrative data and laboratory results, but no other clinical data; for this reason, we cannot retrieve information on diabetic complications, body weight, blood pressure control, etc.
Based on data from Tuscany, the COVID-19 pandemic had a negative impact on the management of diabetes, with a reduction of specialist visits and HbA1c determinations during the first and second pandemic wave. Despite a satisfactory continuity in pharmacological treatment, a possible short-term impairment of average glycemic control was detected, particularly in Autumn. Further studies with a longer follow-up are needed to assess the effects of the impairment of quality of care on glycemic control in the medium term.
Declaration of competing interest
BB, BN, PF declare no conflict of interest that could be perceived as prejudicing the impartiality of the research reported. EM has received consultancy fees from Boehringer Ingelheim, Eli Lilly and Novo Nordisk speaking fees from Abbott, EliLilly, Sanofi, and research grants from Abbott, AstraZeneca Boehringer Ingelheim and Molteni.
Handling Editor: S. Piro
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.numecd.2022.07.017.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Danhieux K., Buffel V., Pairon A., Benkheil A., Remmen R., Wouters E., et al. The impact of COVID-19 on chronic care according to providers: a qualitative study among primary care practices in Belgium. BMC Fam Pract. 2020;21(1):1–6. doi: 10.1186/s12875-020-01326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kendzerska T., Zhu D.T., Gershon A.S., Edwards J., Peixoto C., Robillard R., et al. Vol. 14. Dovepress; 2021. The effects of the health system response to the COVID-19 pandemic on chronic disease management: a narrative review; p. 575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kouri A., Gupta S., Yadollahi A., Clodagh R., Gershon A., To T., et al. Chest; 2020. CHEST reviews: addressing reduced laboratory-based pulmonary function testing during a pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams S., TsiligianniIJNpcrm . Nature Publishing Group; 2020. COVID-19 poses novel challenges for global primary care; pp. 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fernández E., Cortazar A., Bellido V. Impact of COVID-19 lockdown on glycemic control in patients with type 1 diabetes. Diabetes Res Clin Pract. 2020;166:108348. doi: 10.1016/j.diabres.2020.108348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Verma A., Rajput R., Verma S., Balania V.K.B., Jangra B. Impact of lockdown in COVID 19 on glycemic control in patients with type 1 Diabetes Mellitus. Diabetes Metabol Syndr: Clin Res Rev. 2020;14(5):1213–1216. doi: 10.1016/j.dsx.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Silverii G.A., Delli Poggi C., Dicembrini I., Monami M., Mannucci E. Glucose control in diabetes during home confinement for the first pandemic wave of COVID-19: a meta-analysis of observational studies. Acta Diabetol. 2021;58(12):1603–1611. doi: 10.1007/s00592-021-01754-2. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scoccimarro D., Giove G., Silverii A., Dicembrini I., Mannucci E. Effects of home confinement during COVID-19 outbreak on glycemic control in patients with type 2 diabetes receiving telemedicine support. Acta Diabetol. 2021:1–4. doi: 10.1007/s00592-021-01817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coma E., Mora N., Méndez L., Mència B., Hermosilla E., Mireia F., et al. Primary care in the time of COVID-19: monitoring the effect of the pandemic and the lockdown measures on 34 quality of care indicators calculated for 288 primary care practices covering about 6 million people in Catalonia. BMC Fam Pract. 2020;21(1):208. doi: 10.1186/s12875-020-01278-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Italian Ministry of Health COVID-19 report. http://www.salute.gov.it/portale/nuovocoronavirus/ (Available online:
- 11.Region T. Telemedicne approval. http://www301.regione.toscana.it/bancadati/atti/DettaglioAttiG.xml?codprat=2020DG00000000530
- 12.Region T. Electronic prescription Tuscan Region. 2020. https://mcusercontent.com/5227a0b53753ead404d5efed1/files/6313a60d-c47d-4b98-a77f-e1fa274575af/LETTERA_REGINE_TOSCANA.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.