Abstract
Objectives
The worldwide heart failure (HF) prevalence is 8.52 per 1000 inhabitants, with a global economic burden of 346.17 billion dollars. With the COVID-19 pandemic, the focus of medical care has changed to treating the morbidity and mortality of patients with COVID-19 and reducing medical procedures or visits to patients with HF, with the impact being greater in low- and middle-income countries.
Methods
We performed an interrupted time series analysis of HF to determine the changes in the trend of hospitalizations and in-hospital mortality of HF patients before and after the mandatory lockdown in Peru.
Results
A total of 18,514 adults were included in the analysis. Monthly hospital admissions immediately decreased by 599 (95% confidence interval [CI]: 113 to 1085) and the difference in slope before and after the lockdown was 6.4 hospital admissions (95% CI: −4 to 18). In-hospital mortality increased by 18% (95% CI: −8%–43%) and the difference in slope before and after the lockdown was −0.3% (95% CI: −0.9%–0.25%).
Conclusions
There was a reduction in hospitalizations and an increase in the in-hospital mortality of patients with HF before and after the mandatory lockdown due to the COVID-19 pandemic in Peru.
Keywords: COVID-19, Heart failure, Hospital mortality, Hospitalization, Trends, Peru
Introduction
Heart failure (HF) is a clinical manifestation of abnormal structure and/or cardiac function that leads to fluid retention.1 The worldwide prevalence of HF is 8.52 per 1000 people, with a global economic burden of $346.17 billion dollars.2 Some patients will develop chronic HF, which requires hospitalization to receive adequate control and treatment that contributes to their stabilization and prevents relapses.3 With the coronavirus disease 2019 (COVID-19) pandemic, the focus of health care has changed to treating the morbidity and mortality of patients with COVID-19, reducing medical procedures, limiting outpatient visits or visits to patients with HF, and requiring immediate medical attention.4
HF patients in high-income countries have been shown to have higher 30-day mortality during the COVID-19 pandemic compared to previous years.5 The pandemic's impact on patients with these pathologies in low- and middle-income countries, including Peru, has been greater due to a lack of medical personnel and scarcity of personal protective equipment and resources, making treatment more difficult.6 However, to date, little is known about the impact of the mandatory lockdown on health outcomes for patients with HF in Peru.
Therefore, this study examined the changes in the trend of hospitalizations and in-hospital mortality of HF patients before and after the mandatory lockdown in Peru.
Materials and Methods
This study used the anonymized database on hospitalizations from the Ministry of Health of Peru (MINSA), which provides patient-level information on hospital admissions due to any cause in any public medical and specialized institute of Peru belonging to the MINSA. Our sample included individuals (aged 18 years or older) admitted to the hospital with a diagnosis of HF (ICD-10: I50X).
We defined the following outcomes of interest: hospital admissions due to HF and the in-hospital mortality of patients with HF. Both variables were measured on a monthly basis. Hospital admissions was a continuous variable, whereas in-hospital mortality was a percentage variable measured as the ratio between hospital admissions and deaths. Lastly, we defined a dichotomous variable that measures the intervention as zero before implementing the mandatory lockdown in response to COVID-19 (January 2017 to February 2020), and as one otherwise (March 2020 to December 2020).
Statistical analyses
Stata 17 statistical software (Stata Corporation, College Station, TX, USA) was used for the data analyses. The intervention variable was used to perform a single-group interrupted time series analysis to assess the aggregate change in the outcomes of interest before and after the mandatory lockdown in Peru. We used the following equation to run the model:
| (1) |
where is the aggregate outcome of interest measured on a monthly basis, is the time measured every month that has passed since the start of the study (from month 1 to month 48), is the intervention variable, is an interaction term, is the mean value of the outcome of interest at the start of the study, is the value of the slope of the outcome of interest, is the change in the slope of the outcome of interest immediately after the intervention, is the difference of the slope after and before the intervention, and is the stochastic term of the statistical model. The coefficient is akin to a difference-in-difference slope.
The stationarity of the series was assessed using the Dickey–Fuller test for unit root7 and the Phillip–Perron test for unit root.8 In addition, the autocorrelation was assessed by plotting the correlogram and its 95% confidence bands and by estimating the Durbin–Watson test for autocorrelation.9 When autocorrelation of the first order was identified in any longitudinal series, we corrected it by estimating Prais-Winsten for AR(1) regression.10
Results
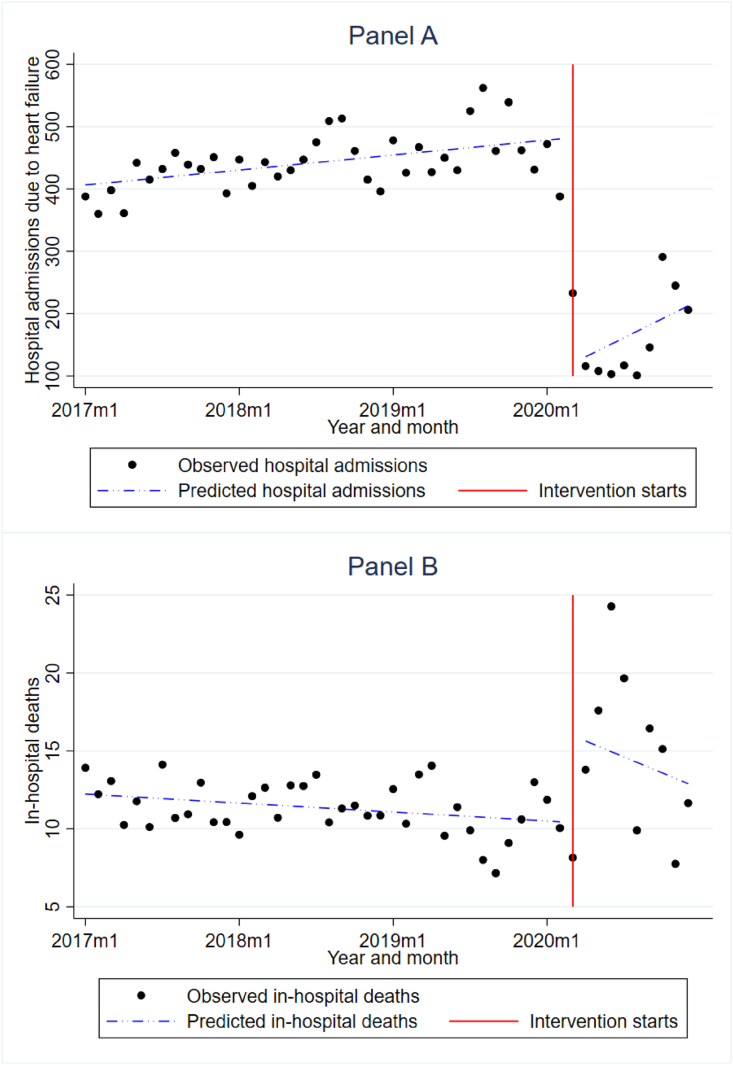
In total, 18,514 adults hospitalized with a diagnosis of HF were included for the analysis, of whom 53.7% were women; the median age was 73 years (interquartile range: 61–82). Overall, the average monthly hospital admissions immediately decreased by 599 (95% CI: 113 to 1085) after implementation of the mandatory lockdown (Figure 1A). The difference in slope before and after the lockdown was 6.4 hospital admissions (95% CI: −4 to 18).
Figure 1.
A. Hospitalizations of heart failure patients from 2017 to 2020. B. Percentage of in-hospital deaths/hospital admissions of patients with heart failure from 2017 to 2020.
On the other hand, the percentage of in-hospital deaths/hospital admissions of patients with HF increased by 18% (95% CI: −8%–43%) immediately after implementation of the mandatory lockdown (Figure 1B). The difference in slope before and after the lockdown was −0.3% (95% CI: −0.9%–0.25%).
Discussion
According to our results, reductions in HF hospitalizations were documented after lockdown, a finding similar to that reported in a study in Japan during the pandemic.11 This could be explained by several reasons; for example, patients with HF, knowing they are an at-risk group, may have been afraid to go to the hospital and get infected by COVID-19.12
Furthermore, because medical resources were shifted to prioritize COVID-19 patients, HF patients with less urgent conditions may have faced delays in treatment.11 This situation may have led to poor treatment and lack of follow-up for acute crises, causing patients to arrive decompensated at health centers, thus increasing mortality in these patients, as shown in our study.
The findings of our study suggest that HF mortality during hospitalization increased after the lockdown. This supports a Canadian study that showed a higher patient mortality and proportion of New York Heart Association functional class III/IV symptoms during the COVID-19 pandemic, caused by a lack of disease control.13 In addition, our study found the percentage of death/hospital admissions increased by 17%. This is supported by a Danish cohort study that found lower in-hospital mortality and higher out-of-hospital mortality during the lockdown compared with the same period in 2019.14 Several countries declined hospital admissions for cardiovascular diseases during the pandemic due to strategies to prevent the spread of SARS-CoV-2 and the reduced emergency hospitalization capacity of hospitals.4,15 Fewer hospital admissions reduce acute cardiovascular care settings and increase mortality during decompensated HF.
This study had some limitations. Our results were from secondary data, which may have had problems with registration and underreporting of cases. In addition, the database did not include relevant information on variables of interest, such as parameters directly linked with HF conditions (e.g., body mass index, family history, coexistence of other diseases, smoking behaviors), pre-hospitalization treatment history, and severity of HF, and there was no information on the causes of patient death. However, this study used a nationally representative database on hospital admissions from MINSA because it is the only one that allows the study of hospitalizations and mortality of patients with HF in the Peruvian population. This study can serve as a basis for future prospective research evaluating these associated factors.
Conclusions
In conclusion, there has been a reduction in hospital admissions and an increase in-hospital mortality of patients with HF before and after lockdown due to the COVID-19 pandemic in Peru.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
Approval by an ethics committee was not requested because this was a study with data in the public domain.
Authors contributions
Conceptualization, Data curation, Formal analysis, and Methodology: AHV. Writing – original draft: AHV, FJVL, RAC: Writing – review & editing: AHV, FJVL, RAC. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Acknowledgments
The authors are grateful to Carlos Rojas-Roque for his support in data analysis.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Kurmani S., Squire I. Acute heart failure: definition, classification and epidemiology. Curr Heart Fail Rep. 2017;14(5):385–392. doi: 10.1007/s11897-017-0351-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lippi G., Sanchis-Gomar F. Global epidemiology and future trends of heart failure. AME Med J. 2020;5:15. 15. [Google Scholar]
- 3.Ramani G.V., Uber P.A., Mehra M.R. Chronic heart failure: contemporary diagnosis and management. Mayo Clin Proc. 2010;85(2):180–195. doi: 10.4065/mcp.2009.0494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Filippo O., D’Ascenzo F., Angelini F., Bocchino P.P., Conrotto F., Saglietto A., et al. Reduced rate of hospital admissions for ACS during covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383(1):88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shoaib A., Van Spall H.G.C., Wu J., Cleland J.G.F., McDonagh T.A., Rashid M., et al. Substantial decline in hospital admissions for heart failure accompanied by increased community mortality during COVID-19 pandemic. Eur Heart J Qual Care Clin Outcomes. 2021;7(4):378–387. doi: 10.1093/ehjqcco/qcab040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bong C.-L., Brasher C., Chikumba E., McDougall R., Mellin-Olsen J., Enright A. The COVID-19 pandemic: effects on low- and middle-income countries. Anesth Analg. 2020;131(1):86–92. doi: 10.1213/ANE.0000000000004846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dickey D.A., Fuller W.A. Distribution of the estimators for autoregressive time series with a unit root. J Am Stat Assoc. 1979;74(366):427–431. [Google Scholar]
- 8.Phillips P.C.B., Perron P. Testing for a unit root in time series regression. Biometrika. 1988;75(2):335–346. [Google Scholar]
- 9.Durbin J., Watson G.S. Testing for serial correlation in least squares regression. II. Biometrika. 1951;38(1–2):159–178. [PubMed] [Google Scholar]
- 10.Fried R., Gather U. Robust trend estimation for AR(1) disturbances. Aust J Stat. 2016;34(2):139. [Google Scholar]
- 11.Morishita T., Takada D., Shin J.-H., Higuchi T., Kunisawa S., Fushimi K., et al. Effects of the COVID-19 pandemic on heart failure hospitalizations in Japan: interrupted time series analysis. ESC Heart Fail. 2022;9(1):31–38. doi: 10.1002/ehf2.13744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhatt A.S., Moscone A., McElrath E.E., Varshney A.S., Claggett B.L., Bhatt D.L., et al. Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol. 2020;76(3):280–288. doi: 10.1016/j.jacc.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Toner L., Koshy A.N., Ko J., Driscoll A., Farouque O. Clinical characteristics and trends in heart failure hospitalizations: an Australian experience during the COVID-19 lockdown. JACC Heart Fail. 2020;8(10):872–875. doi: 10.1016/j.jchf.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Andersson C., Gerds T., Fosbøl E., et al. Incidence of new-onset and worsening heart failure before and after the COVID-19 epidemic lockdown in Denmark: a Nationwide cohort study. Circ Heart Fail. 2020;13(6) doi: 10.1161/CIRCHEARTFAILURE.120.007274. [DOI] [PubMed] [Google Scholar]
- 15.Metzler B., Siostrzonek P., Binder R.K., Bauer A., Reinstadler S.J. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41(19):1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]