Graphical Abstract
Graphical Abstract.
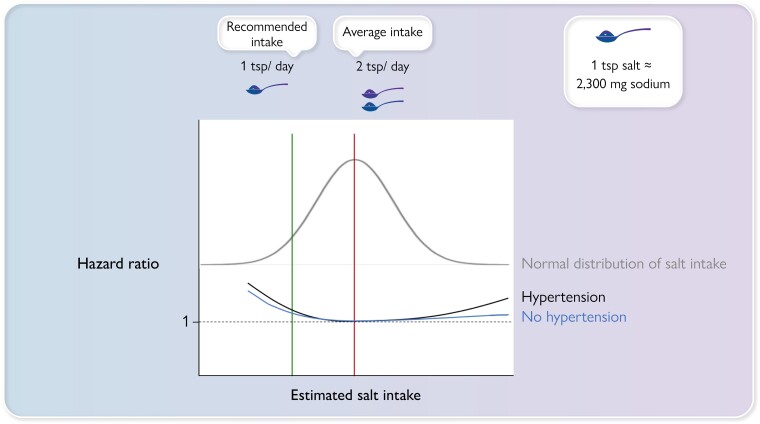
Schematic representation of the distribution of salt intake in the population (grey line) and hazard ratios for people with hypertension (black line) and with no hypertension (blue line).
This editorial refers to ‘Adding salt to foods and hazard of premature mortality’, by H. Ma et al., https://doi.org/10.1093/eurheartj/ehac208.
The World Heart Organization (WHO) recommends that adults consume no more than 5 g of salt per day (which corresponds to 2.3 g of sodium/day).1 The latest European Society of Cardiology guidelines, along with other national and international guidelines, characterizes a healthy diet as a daily salt intake below 5 g, or about a teaspoon, of salt per day,2 based on past recommendations and a recent meta-analysis.3 However, most of the available studies on sodium consumption in populations provide substantially higher estimates,4 with only a minor proportion meeting the WHO recommendation. The Prospective Urban Rural Epidemiology (PURE) study of 102 216 participants from 18 low-, middle-, and high-income countries found that 2.1% had an estimated sodium excretion of less than 3 g per day, and only 0.2% excreted less than 2.3 g per day, after adjustment for regression dilution bias.5 Accordingly, shifting the global population intake to the recommended level would represent a major change.
Because several recent studies show a U- or J-shaped association between salt and atherosclerotic cardiovascular disease, this major change may not be universally beneficial. For example, in a pooled analysis of >130 000 individuals from four large international studies, the association between sodium and a composite of death and major cardiovascular events differed between individuals with and without hypertension.6 Among individuals with hypertension, both high intakes, reflected in sodium excretion of ≥7 g/day but also low intake, <3 g/day were associated with higher risk, compared with sodium excretion of 4–5 g/day, with the latter corresponding to usual levels in many populations. In people without hypertension, higher sodium excretion was not associated with higher risk, whereas an excretion of <3 g/day was associated with a significantly increased risk. Of note, only 11% consumed <3 g of sodium per day. These data indicate that lowering sodium intake would be of most benefit among people with hypertension and high-sodium diets.
On the population level, a computer simulation model study from the USA7 estimated that a modest reduction in dietary salt by 3 g per day would reduce population levels of myocardial infarction and stroke substantially. However, there are several steps between a computational study on what might be beneficial on a group level, findings from observational studies, and advice directed to individuals. One teaspoon of salt per day is an easy metric to remember but going from approximately two teaspoons to one teaspoon per day represents a massive change and an intervention that, if observed, would lead to a drastic reduction in salt intake for most people, irrespective of their individual risk. In the absence of randomized controlled trials, the net effect of such a change remains controversial.8,9 Additionally, a recent ecological analysis in 181 countries found a positive correlation between sodium intake and healthy life expectancy at birth, with an inverse correlation between sodium and all-cause mortality.10
Given the various indications that a very low intake of sodium may not be beneficial, or may even be harmful, it is important to distinguish between recommendations on an individual basis and actions on a population level. Still, the medical profession, as well as people in general, will tend to read the recommendations as directed to individuals. In this issue of the European Heart Journal, Ma et al. describe the salt consumption issue from another angle that could be converted to advice:11 is adding salt to your food bad for your health? While ∼70% of sodium intake in western populations comes from processed and prepared foods, another 8–20% comes from salt added at the table.11 Translated into a question to the medical profession: is added extra salt associated with poorer survival, and, if so, is this because of higher death rates from cardiovascular disease?
Using data from the UK Biobank where a total of 501 379 participants had completed a questionnaire on the frequency of adding salt to foods at baseline, the authors found a graded relationship between higher frequency of adding salt to foods and higher hazard of all-cause premature mortality. During a median of 9.0 years of follow-up, 18 474 deaths were documented, with mortality increasing across groups with higher reported frequency of adding salt to food, with a hazard ratio of 1.28, 95% confidence interval (CI) 1.20–1.35 comparing those always adding salt to those who never, or only rarely, did. In addition, compared with the never/rarely group, always adding salt to foods was associated with 1.50 (95% CI 0.72–2.30) and 2.28 (95% CI) 1.66–2.90 years lower life expectancy at the age of 50 years in women and men, respectively. Even so, only 5% added salt frequently or always, while 12% said that they usually added salt. Importantly, the proportion of fruit and vegetables in the diet was essential, with a more pronounced effect of extra salt on mortality among individuals who ate little of these foods.
The authors conclude that adding salt to foods is associated with a higher hazard of all-cause premature mortality and lower life expectancy. This was true for cardiovascular mortality as well, which provides a biologically plausible link, given the strong evidence for a link between sodium intake and blood pressure.5 The effect on cardiovascular mortality was limited to stroke mortality.
So how does this translate into advice on the individual level? There is not a lot of evidence from randomized controlled trials. However, in support of the potential beneficial effects of a reduction in salt intake in high-risk individuals, a recent unblinded, cluster-randomized trial involving persons from 600 villages in rural China showed that the use of a salt substitute (75% sodium chloride and 25% potassium chloride, compared with regular salt) had a significant benefit on rates of stroke, major cardiovascular events, and death from any cause in high-risk persons with a history of stroke or who were 60 years of age or older, and had high blood pressure.12
Some health advice is straightforward; neither alcohol nor tobacco is necessary for survival, and the harmful effects of these substances are well established. However, with most dietary components, there is an optimal level which applies to salt as well as to many other substances. The evidence to reduce individual levels far below current consumption, if the current guidelines were followed, is close to non-existent and could cause harm in some people (Graphical Abstract). So far, what the collective evidence about salt seems to indicate is that healthy people consuming what constitutes normal levels of ordinary salt need not worry too much about their salt intake. Instead, to counterbalance potentially harmful effects of salt, and for many other reasons, a diet rich in fruit and vegetables should be a priority on the individual, as well as the population, level. People at high risk with a high salt intake are probably well advised to cut down, and not adding extra salt to already prepared foods is one way of achieving this. However, at the individual level, the optimal salt consumption range, or the ‘sweet spot’ remains to be determined.
Still, at the population level, there is no reason to be complacent about salt intake. There is a well-established link between salt consumption and population blood pressure levels. Public awareness about salt needs to be raised, but perhaps not in the shape of advice about target levels that are unlikely to be achieved, and which are possibly harmful in some. Hypertension is a major determinant of cardiovascular disease, with a population-attributable fraction of >20%, and a third of all strokes are attributable to this factor.13
Most of our salt consumption comes from salt added to food prepared by the industry, for example in common products such as bread and cheese, but also ready-made foods and other items. Adding salt is a source of profit by increasing preference for salty foods and making food products more palatable to people already used to a diet high in salt. A reduction in added salt in food produced by the industry is very unlikely to cause harm, while oversalting common products reduces the opportunity for people to choose for themselves and contributes to the development of hypertension.
Classic epidemiology argues that a greater net benefit is achieved by the population-wide approach (achieving a small effect in many people) than by targeting high-risk individuals (a large effect but only achieved in a small number of people).14 The obvious and evidence-based strategy with respect to preventing cardiovascular disease in individuals is early detection and treatment of hypertension, including lifestyle modifications, while salt reduction strategies at the societal level will lower population mean blood pressure levels, resulting in fewer people developing hypertension, needing treatment, and becoming sick. Not adding extra salt to food is unlikely to be harmful and could contribute to strategies to lower population blood pressure levels.
Funding
A.R. acknowledges support from the Swedish Research Council [2018-02527, VRREG 2019-00193], the Swedish Heart and Lung Foundation, and AFA Insurance
Conflicts of interest: None declared
References
- 1. WHO/Europe | Health policy—5 recommendations to reduce salt intake to live longer and healthier lives. 31 March 2022.
- 2. Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 2021;42:3227–3337. [DOI] [PubMed] [Google Scholar]
- 3. He FJ, Tan M, Ma Y, MacGregor GA. Salt reduction to prevent hypertension and cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol 2020;75:632–647. [DOI] [PubMed] [Google Scholar]
- 4. Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, et al. Global Burden of Diseases Nutrition and Chronic Diseases Expert Group (NutriCoDE). Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 2013;3:e003733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mente A, O’ MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A, et al. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med 2014;371:601–611. [DOI] [PubMed] [Google Scholar]
- 6. Mente A, O’Donnell M, Rangarajan S, Dagenais G, Lear S, McQueen M, et al. Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies. Lancet 2016;388:465–475. [DOI] [PubMed] [Google Scholar]
- 7. Bibbins-Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med 2010;362:590–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Graudal N. A radical sodium reduction policy is not supported by randomized controlled trials or observational studies: grading the evidence. Am J Hypertens 2016;29:543–548. [DOI] [PubMed] [Google Scholar]
- 9. O’Donnell M, Mente A, Alderman MH, Brady AJB, Diaz R, Gupta R, et al. Salt and cardiovascular disease: insufficient evidence to recommend low sodium intake. Eur Heart J 2020;41:3363–3373. [DOI] [PubMed] [Google Scholar]
- 10. Messerli FH, Hofstetter L, Syrogiannouli L, Rexhaj E, Siontis GCM, Seiler C, et al. Sodium intake, life expectancy, and all-cause mortality. Eur Heart J 2021;42:2103–2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ma H, Xue Q, Wang X, Li X, Franco OH, Li Y, et al. Adding salt to foods and hazard of premature mortality. Eur Heart J 2022;43:2879–2889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Neal B, Wu Y, Feng X, Zhang R, Zhang Y, Shi J, et al. Effect of salt substitution on cardiovascular events and death. N Engl J Med 2021;385:1067–1077. [DOI] [PubMed] [Google Scholar]
- 13. Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet 2020;395:795–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rose G. Sick individuals and sick populations. Int J Epidemiol 2001;30:427–432. [DOI] [PubMed] [Google Scholar]