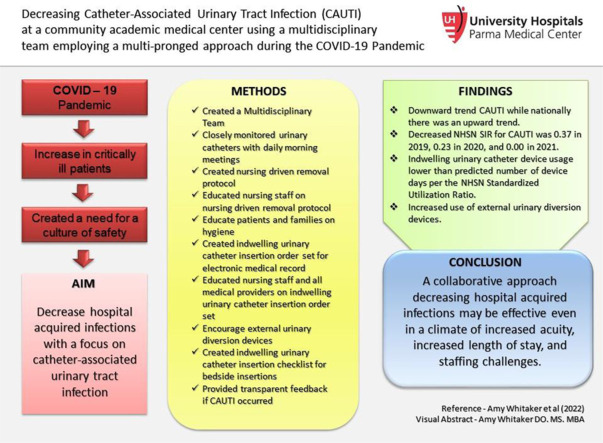
Graphical abstract
Key words: Indwelling Urinary Catheter (IUC), External urinary diversion device, Hospital Acquired Infection (HAI), National Healthcare Safety Network (NHSN), Standardized Infection Ratio (SIR), Standard Utilization Ratio (SUR)
Abstract
In the midst of the COVID – 19 pandemic, a multidisciplinary team implemented evidence-based strategies to eliminate catheter associated urinary tract infections (CAUTI), as defined by the National Healthcare Safety Network (NHSN) surveillance definition for those units included in the NHSN standardized infection ratio. The team evaluated indwelling urinary catheters daily for indication, implemented a urinary catheter order set, established a urinary catheter insertion checklist, and promoted use of external urinary diversion devices. The facility NHSN standardized infection ratio for CAUTI was 0.37 in 2019, 0.23 in 2020, and 0.00 in 2021. A collaborative approach decreasing hospital acquired infections may be effective even in a climate of increased acuity, increased length of stay, and staffing challenges.
University Hospitals Parma Medical Center (UHPMC) in Parma, Ohio is an adult suburban hospital with 247 licensed beds that is striving to reach a goal of zero harm for all patients. Many hospital systems nationally are aiming to decrease hospital acquired infection (HAI) such as catheter associated urinary tract infections (CAUTI).1, 2, 3, 4 CAUTIs result in thousands of deaths each year and billions of dollars in added costs to the US health care system, yet these infections are preventable.5 It is estimated that approximately 12%-16% of adult hospital inpatients will have an indwelling urinary catheter (IUC) at some time during their hospitalization and each day the IUC remains, a patient has a 3%-7% increased risk of acquiring a CAUTI.6 When nurse-driven hospital protocols are set in place to ensure an IUC is appropriately placed, maintained, and removed promptly when no longer needed, the number of CAUTI are dramatically decreased.7 Additionally, literature has shown evidence behind daily meetings between hospital leadership and nursing may reduce the CAUTI Standard Infection Rate (SIR).8 As critically ill patients began to fill the hospital during the beginning of the COVID-19 pandemic leading to increased IUC use, UHPMC took a multidisciplinary approach to avoid HAIs during the COVID-19 pandemic, including CAUTIs, to create a culture of safety.9 This approach to HAI prevention during the COVID-19 Pandemic, January 2019 to December 2021, was unique due to combined use of the nurse driven IUC removal protocol, the inclusion of a bedside nursing IUC checklist, and an IUC insertion order set that was created in the electronic medical record (EMR).
Materials and methods
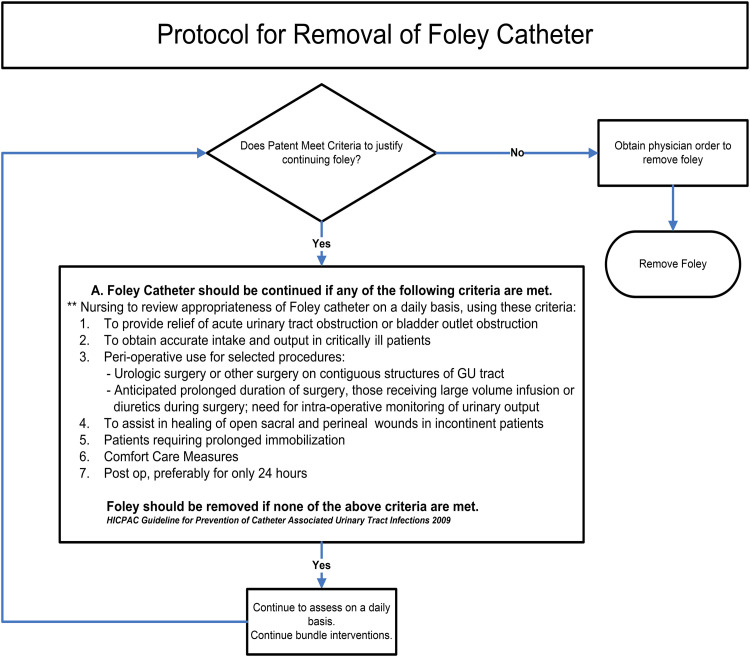
In an effort to reduce CAUTIs, a quality improvement project was developed by a multidisciplinary team including the chief operating officer, chief medical officer, chief nursing officer, intensivists, nurse managers, bedside registered nurses, patient care assistants, nursing education staff, medical residents, and quality staff including infection prevention nurses was assembled. This team created a culture of safety throughout the hospital around avoiding use of IUCs in order to avoid the patient harm of a CAUTI. From the top leaders to physicians and bedside nurses, urinary catheters were tracked, discussed daily at morning nursing huddles, and made a focus throughout all areas of the hospital. The quality team monitored IUCs daily to ensure the proper use and prompt removal when no longer indicated per the Nurse-Driven Indwelling Urinary Catheter Removal Protocol that was established (Fig 1 ).
Fig 1.
Nurse-driven indwelling urinary catheter removal protocol. IUC appropriateness was emphasized prompting removal when criteria weren't met.
Nurses reviewed the removal protocol when an IUC was ordered and were educated on removal and maintenance by unit managers and informational handouts. Infection prevention nurses met in person with patients who were resistant to catheter removal to educate them on the importance of removal to decrease infection risk. This education was individualized to the patient's needs. Per CDC guidelines, hand hygiene for staff, patients, and visitors was emphasized to reduce contamination rates as well.10 Medical staff were educated on the preference for external catheter use over IUC for bedbound patients without retention during regular staff meetings.
This quality project included an IUC insertion order set that was created in the EMR. Strict clinical criteria were incorporated into the order set to help drive providers to critically evaluate the need for an IUC prior to insertion. The order set has the provider give the exact reason for insertion and triggered the ability for the nurses to remove the foley per the removal protocol. Male and female external urinary diversion devices were emphasized along with bladder scanner re-training for staff to quantify urinary retention. Intermittent catheterization and hourly toilet prompts were recommended as the initial intervention for post-void residual or urinary retention cases. If a urinary catheter was kept in use for urinary retention, a urology consult was recommended by the team to the attending physician. Urologists were not part of the initial team but a urology consult was encouraged for all patients with retention. External catheters were emphasized as an option for bedbound patients when IUC wasn't necessary. The product representatives for the external catheters trained the nurses on indications and proper use.
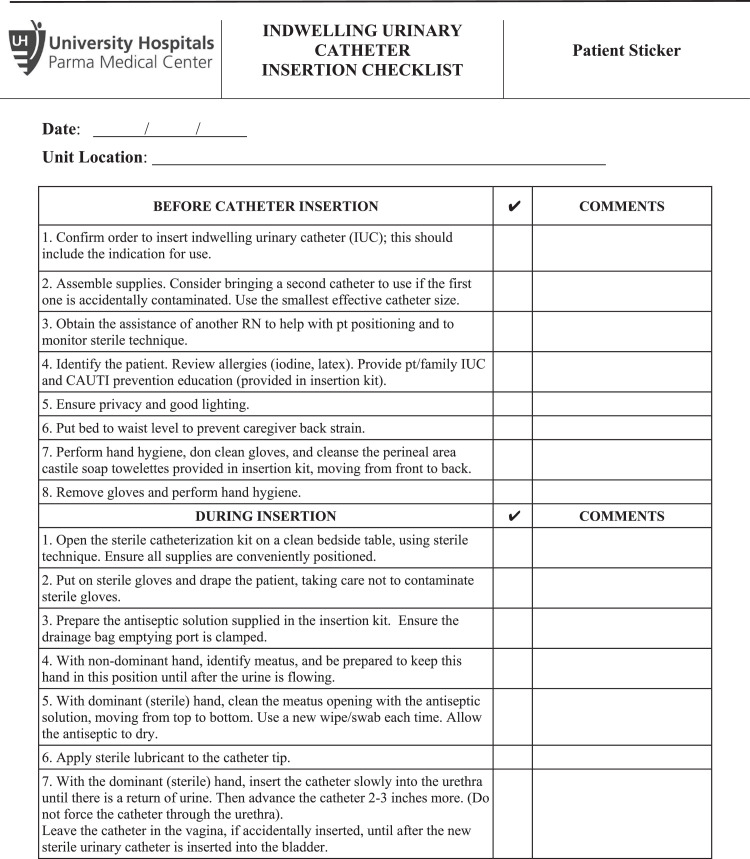
When an IUC was deemed necessary, a standardized kit was employed and aseptic insertion and maintenance techniques were enforced through the use of an insertion checklist. (See Fig 2 ).
Fig 2.
Indwelling urinary catheter insertion checklist used bedside during placement of IUCs. This is used at the bedside by a second RN in order to improve aseptic insertion.
Two nurses are required for the placement of an IUC to ensure aseptic technique. The insertion checklist was the idea of a bedside nurse who cared for a patient who developed a CAUTI. The nurse identified concerns about urinary catheter insertion without another registered nurse to call out breaches in technique or to provide additional support or supplies while the inserter is donned for a sterile procedure.
Daily morning huddles of the multidisciplinary team ensured prompt removal of IUCs and the use of the Nurse-Driven IUC Removal Protocol was emphasized in these daily meetings (Fig 1). When the criteria in Figure 1 are no longer met, that prompts removal of the IUC. Catheter maintenance was monitored closely by quality staff through daily review of nursing documentation.
If a hospital acquired CAUTI did occur, the team conducted a root cause analysis to identify any causes or practice gaps, while providing transparent feedback to the providers and staff directly involved in the patient's care. All HAI CAUTIs were logged by the quality department and reported to the NHSN.
This Quality Improvement Initiative was reviewed and determined to not meet the criteria for human subjects’ research by the University Hospitals Cleveland Medical Center Institutional Review Board.
Results
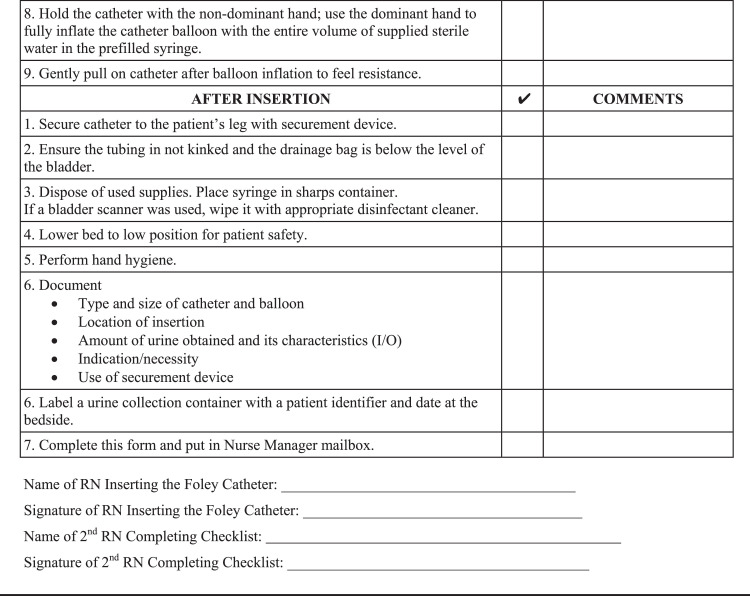
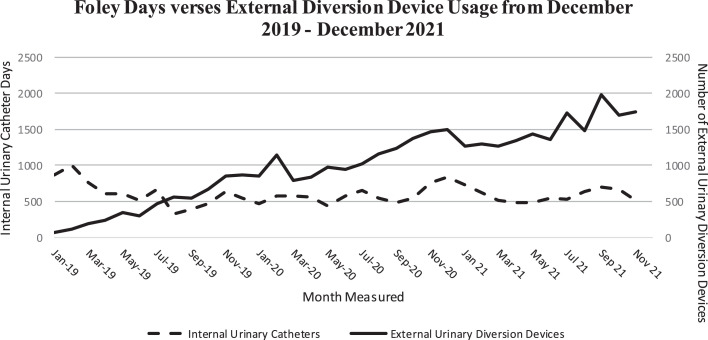
After the implementation of the multidisciplinary team, there was a remarkable downward trend in the number of hospital acquired CAUTIs while upward trends were noted during the same time period nationally.11 This sustained decrease occurred despite the COVID-19 surge, when the national CAUTI NHSN SIR steadily increased in 2020, ranging from 0.59 in Q1 to 0.82 in Q4.11 In contrast, at UHPMC the CAUTI NHSN SIR decreased from 0.37 in 2019 to 0.23 in 2020. This was sustained into 2021 with a 0.00 CAUTI NHSN SIR. Also, the facility maintained an IUC device usage that was statistically lower than the predicted number of device days per the NHSN Standardized Utilization Ratio (SUR) with a P value < .05. IUC use remained stable as an upward trend in external urinary diversion devices was noted (Fig 3 ). Per the UHPMC Purchasing Manager, the use of the external urinary diversion devices used increased from 6,114 devices for the entire year of 2019, to 12,704 devices in 2020, and 18,102 in 2021.
Fig 3.
Foley days verses external diversion devices used from December 2019 to December 2021. This graph demonstrates trending of increased usage of external urinary diversion devices.
Discussion
CAUTIs remain a significant concern in health care. CAUTIs cause significant morbidity and mortality for patients, but also have quality and financial consequences for health care entities. Impactful reduction in CAUTIs has been difficult to achieve during the COVID-19 pandemic, due to the high acuity and longer length of stay associated with severe COVID-19.11 Our community hospital adopted increased focus on necessity of IUC placement, enhanced sterility with a bedside IUC checklist, and daily assessment of IUC necessity. Through these interventions, the CAUTI NHSN SIR for our facility continued to decrease while the CAUTI NHSN SIR increased nationally.11 Particular focus included educating the physicians and nurses on appropriate indications for IUCs and available alternative urinary diversion devices. Urology engagement was key to managing IUC that met clinical indications. All IUC were under surveillance by the quality department. These interventions showed a significant decrease in CAUTI within the community hospital setting that other institutions could implement during surges to decrease known HAIs.
Reduction in the number of IUC insertions and the number of days IUCs are in use removes the source of infection. A robust checklist performed by 2 licensed providers placing the IUC helps to guarantee sterility in performing the procedure thereby minimizing the chances of pathogen introduction at the time of placement. Studies have shown the benefit of a multidisciplinary team approach with CAUTI reduction in surgical units, and the results from this study highlight the importance of the creation of a multi-tiered approach to tackle CAUTI no matter where the patient is located in the hospital.12 The implementation of a nurse driven protocol was unique to our approach to decreasing CAUTIs. Gauron and Bigand implemented reports created by charge nurses to discuss continuation or removal of IUC devices with primary nurses. While this was beneficial for them, we found that a strict protocol would enhance removal of unnecessary IUCs. While UHPMC saw an increase in overall census, case mix index, and admissions during the reference period, the number of CAUTIs were significantly reduced. An institutional commitment to external urinary diversion devices, while financially more costly in the short term, showed to be superior for patient safety in avoidance of adverse events.
The process above may be implemented at other health care entities. Robust surveillance by quality, nursing, and physician teams allows for early intervention opportunities to eliminate or prevent the placement of IUC prior to development of an infection. A limitation of this protocol was implementation in the setting of a high acuity suburban inpatient facility excluding pediatric and obstetric services. This study does not represent patient populations in an academic tertiary or rural community hospital. Reported data reflects the units included in NHSN SIR Reports only. A notable challenge existed around the increase length of stay and acuity of patients during waves of the COVID-19 pandemic. Longitudinal study of the patients did not occur after discharge. Challenges existed in achieving buy in with some members of the medical staff, which required increased communication from the members of the administration, quality, and nursing teams.
Reduction in CAUTI is critical work for any organization who places priority on zero harm to patients. Reducing CAUTI leads to better patient/family, financial, and operational outcomes for health care entities. While time intensive, an opportunity may exist to create an electronic solution to aid in surveillance and prompt removal of urinary catheters. Future reduction in CAUTI may occur through implementation of a urinary culture stewardship program and reducing the need for unnecessary antibiotics in asymptomatic bacteriuria. Similar methodology could be employed in a variety of areas of defects in quality such as patient safety indicators.
To conclude, with the implementation of a multidisciplinary team that is dedicated to reducing the number of HAI including CAUTI, a suburban hospital may be able to see the number of CAUTI decrease hospital-wide regardless of the acuity and length of stay.
Footnotes
Conflicts of interest: All authors listed above have no conflict of interest including employment, consultancies, stock ownership, honoraria, paid expert testimony, patent applications/registrations, and grants or other funding.
References
- 1.Nickel W, Saint S, Olmsted RN, et al. The Interdisciplinary Academy for Coaching and Teamwork (I-ACT): a novel approach for training faculty experts in preventing healthcare-associated infection. Am J Infect Control. 2014 Oct;42(suppl 10):S230–S235. doi: 10.1016/j.ajic.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 2.Saint S, Greene MT, Fowler KE, et al. What US hospitals are currently doing to prevent common device-associated infections: results from a national survey. BMJ Qual Saf. 2019;28:741–749. doi: 10.1136/bmjqs-2018-009111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McAlearney AS, Hefner JL, Sieck CJ, et al. Searching for management approaches to reduce HAI transmission (SMART): a study protocol. Implement Sci. 2017;12:82. doi: 10.1186/s13012-017-0610-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krocová J, Prokešová R. Aspects of prevention of urinary tract infections associated with urinary bladder catheterisation and their implementation in nursing practice. Healthcare (Basel) 2022;10:152. doi: 10.3390/healthcare10010152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hollenbeak CS, Schilling AL. The attributable cost of catheter-associated urinary tract infections in the United States: a systematic review. Am J Infect Control. 2018;46:751–757. doi: 10.1016/j.ajic.2018.01.015. [DOI] [PubMed] [Google Scholar]
- 6.US. Centers for Disease Control and Prevention. The National Healthcare Safety Network (NHSN) Component. 2022 Jan. Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases.
- 7.Dy S, Major-Joynes B, Pegues D, Bradway C. A nurse-driven protocol for removal of indwelling urinary catheters across a multi-hospital academic healthcare system. Urol Nurs. 2016;36:243–250. [PubMed] [Google Scholar]
- 8.Allen B., Culbertson J., Eyherabide S., Geca M. A Multifaceted approach to CAUTI reduction. Am J Infect Contr. 2019;47:S40. [Google Scholar]
- 9.Lastinger L, Alvarez C, Kofman A, et al. Continued increases in the incidence of healthcare-associated infection (HAI) during the second year of the coronavirus disease 2019 (COVID-19) pandemic. Infect Contr Hosp Epidemiol. 2022:1–5. doi: 10.1017/ice.2022.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Indwelling urinary catheter Insertion and maintenance presentation. Centers for Disease Control and Prevention. Atlanta, GA: US. Department of Health and Human Services, Centers for Disease Control and Prevention. Accessed May 7, 2022. https://www.cdc.gov/infectioncontrol/pdf/strive/CAUTI104-508.pdf
- 11.Weiner-Lastinger L, Pattabiraman V, Konnor R, et al. The impact of coronavirus disease 2019 (COVID-19) on healthcare-associated infections in 2020: A summary of data reported to the National Healthcare Safety Network. Infect Contr Hosp Epidemiol. 2022;43:12–25. doi: 10.1017/ice.2021.362. [DOI] [PubMed] [Google Scholar]
- 12.Gauron G, Bigand T. Implementation of evidence-based strategies to reduce catheter-associated urinary tract infections among hospitalized, post-surgical adults. Am J Infect Control. 2021;49:843–845. doi: 10.1016/j.ajic.2020.11.016. [DOI] [PubMed] [Google Scholar]