Abstract
Introduction:
Patient satisfaction has been found to be a determinant of patient compliance to medical advice and treatment, medical service utilisation, the doctor—patient relationship, and continuity of care. Assessment of patient satisfaction can be used to evaluate health care services and identify areas to target for quality improvement.
Methods:
A cross-sectional study was conducted to determine the satisfaction level of patients attending a primary care clinic and its associated factors. Participants’ experience of time at the clinic, socio-demographic data, and personal health information were collected. The 18-Item Patient Satisfaction Questionnaire was used to determine patient satisfaction. Univariate and multivariate analyses were employed to identify the factors associated with patient satisfaction.
Results:
We recruited 327 participants and 50.46% reported satisfaction. The highest satisfaction was reported in the communication domain (80.80% of the maximum score) and the lowest score was reported in the accessibility and convenience domain (66.40%). The only significant positive correlation with total patient satisfaction score was the difference between perceived and expected length of consultation.
Conclusion:
The only independently associated factor was the difference between perceived and expected length of consultation; therefore, changing how time is spent during consultations may prove useful in improving patient satisfaction.
Keywords: Patient Satisfaction, Primary Care, Length of Consultation
Introduction
Patient satisfaction with health care services is an important issue as patients are the recipients and consumers of these services. Satisfaction is an important determinant of patient compliance to the medical advice and treatment rendered, medical service utilisation, the doctor-patient relationship, and continuity of care.1'4
Generally, factors that influence patient satisfaction can be categorised: (a) patient-related factors (e.g., age, race, gender, education level, and socioeconomic status), (b) medical personnel-related factors (e.g., technical skills, time spent during visit, communication skills, bedside manners), and (c) system-related factors (e.g., accessibility, facilities, appointments, referrals, and continuity of care).5
Length of time spent with the doctor is one of the strongest determinants of patient satisfaction.6 The duration of time spent in consultations has shortened over the years, mainly due to increasing administrative work load of the physician and the emphasis on cost effectiveness of health services.7 Many studies have shown that when the time spent with the physician in ambulatory encounters is shortened, it may decrease both patient and physician satisfaction.8 Time is a key element in the formation of the patient—doctor relationships and should be regarded as a valuable resource in health care.
In Malaysia, patient satisfaction studies in primary care settings have been conducted over the last 10 years and have involved both government and private primary care clinics in different populations (i.e., urban, suburban, and rural populations). Several different instruments have been employed to evaluate patient satisfaction, such as SERVQUAL, Modified Patient Satisfaction Questionnaire III (PSQ III), Patient Satisfaction Questionnaire II (PSQ II), and different cut-off points for satisfied patients have been used.9-12 Generally, most of the studies reported a high level of satisfaction (78.8–93.1% satisfied patients)5,9,12; two studies from Aizuddin et al. and Haliza et al. reported the proportion of satisfied patients as 27.5% and 19.4%, respectively.10,13
Studies specifically investigating patient satisfaction and the time spent with physicians as a resource remain scarce,8 especially in the local setting. The aim of this study was to determine the patient satisfaction level and its association with the experience of time spent in the clinic and other factors for patients attending an academic primary care clinic.
Methods
Study design and setting
A cross-sectional study was conducted over 3 weeks from July 18, 2016, to August 5, 2016, in an academic primary care clinic in Kuala Lumpur, Malaysia. University Malaya Medical Centre (UMMC) Primary Care Clinic is a unique primary health care setting where the primary health care providers can order inhospital investigations, as the clinic is attached to the UMMC, a tertiary care hospital.
Study population
The participants eligible for this study were all adult patients attending the UMMC primary care clinic (General Clinic)-Klinik Rawatan Utama (RUKA) during the study period. The General Clinic was chosen because the patients attending general clinics are more diverse and representative of the general population. Exclusion criteria were patients younger than 18 years of age, patients requiring emergency care, and patients who could not understand both English and Malay.
Sample size calculation
Sample size calculation was performed using 0pen Epi, a sample size calculator for finite populations. Based on a recent local study conducted by Aizuddin et al. in a primary care setting, the proportion of satisfied patients was 27.5%10; therefore, a sample size of 285 patients with a 95% confidence interval was used. Considering a 20% drop-out rate, the sample size was estimated to be 342. The study enrolled a total of 357 patients.
Sampling method
Participants were recruited using a systematic random sampling method. The first participant was selected randomly from a digit starting from 0 to 9. Subsequently, every tenth patient was sampled based on the last digit of a fourdigit queue number.
Study instruments
The study instrument was a structured data collection form consisting of two sets of questionnaires (Pre-consultation Questionnaire and Post-consultation Questionnaire) and one set of data collection forms for the actual consultation time.
The Pre-consultation Questionnaire consisted of two sections: the socio-demographic profile and the personal health and visit information of the participants. The Postconsultation Questionnaire consisted of two sections, including the perceived length of the consultation and a Short-form Patient Satisfaction Questionnaire (PSQ-18). Both questionnaires were self-administered.
The PSQ-18 was chosen because the instrument is clinically relevant to the study setting and population. The PSQ-18 was originally developed by Marshall and Hays and was derived from the PSQ-III.14 The PSQ-18 comprises 18 items answered on a five-point Likert scale ranging from 1 (‘strongly agree’) to 5 (‘strongly disagree’). These items include general satisfaction (2 items), technical quality (4 items), interpersonal manners (2 items), communication (2 items), financial aspects (2 items), time spent with the doctor (2 items), and accessibility and convenience (4 items).14 The PSQ-18 subscales correlate well with their full-scale counterparts in the PSQ-III, with a generally acceptable internal consistency coefficient of 0.64-0.77.14 Moreover, the PSQ-III has been used extensively in patient satisfaction surveys and is validated for use in Malaysia.15-17
The data collection form for actual consultation time consists of a 2 x 5 table where the first column records the ‘time in’ and second column records the ‘time out’. There are five rows indicating first to fifth time consultations for the same patient in the clinic on the same day. The attending doctors were directed to fill in the start time of consultation in the ‘Time in’ column and end time of consultation in the ‘Time out’ column in the first row of the table. If the attending doctor ordered investigations (e.g., x-ray, FBC) when the patient entered the consultation room for the second time, the attending doctors were directed to fill in the start time of the consultation in the ‘Time in’ column and end time of consultation in the ‘Time out’ column on the second row of the table. The attending doctors were directed to follow the same procedure if the patient left and reentered the consultation room for the third, fourth, fifth, or subsequent times. The form was collected at the end of the clinic session by the investigator. The investigator calculated the time spent in the consultation room by subtracting the ‘time out’ from the ‘time in’ for each row of the table. Then, the time spent for each consultation was summated to determine the actual length of the consultation.
Definition of the experience of time spent by patients in clinic variables
-
Expected length of consultation
This is the patient’s expectation of the length of time that would be spent in consultation. This was determined before the patient consulted with the attending doctor.
-
Perceived length of consultation
This is the patient’s perception of the time spent in consultation. This was determined after the patient consulted with the attending doctor.
-
Actual length of consultation
This is the actual duration of the consultation and was calculated by subtracting the ‘time out’ from the ‘time in’. Then, the time spent in each consultation on the same day were summated to determine the actual length of consultation (in minutes).
-
Difference between perceived and expected length of consultation
This variable was calculated by subtracting the perceived length of consultation from the expected length of consultation (in minutes).
-
Difference between actual and expected length of consultation
This variable was calculated by subtracting the actual length of consultation from the expected length of consultation (in minutes).
Statistical analysis
All statistical analyses were performed using Statistical Package for Social Science (SPSS) version 23. Descriptive analysis was performed for all the variables in this study.
Outliers were checked for continuous data. A formal assessment for normality using the Kolmogorov—Smirnov test was performed for all continuous variables. If this formal method showed that the variables were not normally distributed, other methods of assessing normality were carried out, including comparing the mean and median, constructing a histogram overlaid with a normal curve, constructing a normal probability plot, and constructing a box and whisker plot. All the continuous variables were normally distributed, except for the total monthly household income variable.
The independent t-test or ANOVA test were used to compare the total patient satisfaction scores for categorical variables. Pearson’s correlation test was employed to evaluate the association of the total patient satisfaction score with the continuous variables (normally distributed variables). Spearman’s correlation test was employed to evaluate the association of the total patient satisfaction scores with total monthly household income (non-normally distributed variable).
A multiple regression model was employed to study the relationship between the total patient satisfaction score and the actual length of consultation, waiting time, the difference between the perceived and expected length of consultation, and the sociodemographic variables with a p-value <0.25 (age, gender, marital status, job status, and type of occupation). The ‘job status’ variable was recategorised into ‘working’ and ‘not working’, and the ‘type of occupation’ variable was recategorised into ‘government sector’ and ‘non-government sector’ in the multiple regression model.
Data collection
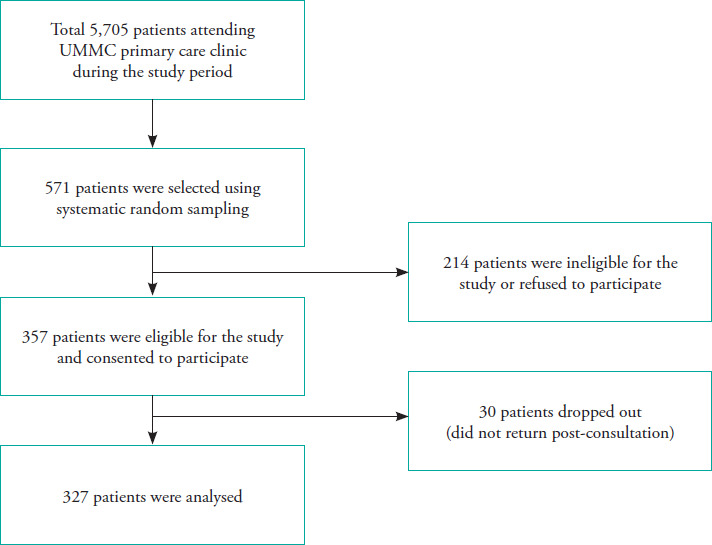
Data collection was conducted with the assistance of the triage nurses, clerks, enumerator, and doctors. The flow chart of the recruitment process is illustrated in Figure 1. The recruitment rate was 62.5%. From those patients recruited in the study, a total of 30 patients did not return after the consultation and were considered to have dropped out, making the drop-out rate 8.4%. The final total number of participants analysed was 327.
Figure 1. Flowchart of participant recruitment.
Ethical approval
This study was approved by the UMMC Ethics Committee (reference number 20163-2278) on April 15, 2016, before the commencement of the study.
Results
Socio-demographic profiles of the participants
The mean age of this study’s participants was 52 years, with a standard deviation of 17 years. There were slightly more female participants (n=184) than male participants (n=143), and more than two-thirds of the participants were married. Most of the participants were Malay (48.0%), followed by Chinese (25.1%), Indian (24.2%), and others (2.8%). Regarding employment, 45% of the participants were working and most of them worked in the private sector. Almost 90% of the participants had obtained at least a secondary level of education. The median total monthly household income was RM 2500 (Table 1).
Table 1. Socio-demographic characteristics of participants.
|
Participant profile |
Number of participants, n |
Percentage, % |
|---|---|---|
|
Age (years) |
|
|
|
Mean + SD# Range |
51.95 ± 17.32 18-87 |
|
|
Gender |
|
|
|
Male |
143 |
43.7 |
|
Female |
184 |
56.3 |
|
Race |
|
|
|
Malay |
157 |
48.0 |
|
Chinese |
82 |
25.1 |
|
Indian |
79 |
24.2 |
|
Other |
9 |
2.8 |
|
Marital Status |
|
|
|
Single |
74 |
22.6 |
|
Married |
253 |
77.4 |
|
Job Status |
|
|
|
Working |
147 |
45.0 |
|
Not working |
92 |
28.1 |
|
Student |
18 |
5.5 |
|
Retired |
70 |
21.4 |
|
Type of Occupation |
|
|
|
Government sector |
51 |
15.6 |
|
Private sector |
82 |
25.1 |
|
Self-employed |
14 |
4.3 |
|
Unrelated |
180 |
55.0 |
|
Highest Education Level |
|
|
|
Primary school |
39 |
11.9 |
|
Secondary school |
147 |
45.0 |
|
Diploma |
55 |
16.8 |
|
Degree |
62 |
19.0 |
|
Postgraduate degree |
17 |
5.2 |
|
No formal education |
7 |
2.1 |
|
Total Monthly Household Income (RM) Median (IQR*) Range |
2500 (750-5000) 0-30000 |
|
standard deviation
interquartile range
Patient total satisfaction score and its domains
The mean total patient satisfaction score was 67.18, which was almost three-quarters (74.64%) of the maximum score (90). In this study, all the domains achieved >75% of the maximum score, except for the ‘time spent with doctor’ domain and ‘accessibility and convenience’ domain, which only achieve 68.4% and 66.4% of the maximum score, respectively.
Table 2. Patient total satisfaction score and its domains.
|
Variables |
Mean score ± SD |
Range |
Maximum score |
|---|---|---|---|
|
Total Satisfaction Score |
67.18 ± 6.76 |
40-87 |
90 |
|
General Satisfaction |
7.97 ± 1.16 |
2-10 |
10 |
|
Technical Quality |
15.28 ± 1.94 |
8-20 |
20 |
|
Interpersonal Manner |
7.87 ±1.20 |
3-10 |
10 |
|
Communication |
8.08 ± 1.19 |
2-10 |
10 |
|
Financial Aspect |
7.53 ± 1.34 |
4-10 |
10 |
|
Time Spent with Doctor |
6.84 ± 1.26 |
4-10 |
10 |
|
Accessibility and Convenience |
13.28 ± 2.23 |
6-20 |
20 |
Experience of time spent by patients in the clinic
The mean expected length of consultation and perceived length of consultation were 15.85 minutes and 14.39 minutes, respectively, while the actual length of consultation was 16.43 minutes. The mean waiting time was 81.13 minutes, with a standard deviation of 3.25 minutes. The difference between perceived and expected length of consultation ranged from -110 minutes to 50 minutes, with a mean score of -1.46 minutes. The difference between the actual and expected length of consultation ranged from -101 minutes to 61 minutes, with a mean score of 0.58 minutes.
Relationship between experience of time spent by patients in the clinic and total patient satisfaction score
The difference between perceived and expected length of consultation demonstrated a significant positive linear relationship with total patient satisfaction score (correlation coefficient: 0.151, p=0.006). Although the perceived length of consultation, actual length of consultation, and difference between the actual and expected length of consultation showed a positive linear relationship with total patient satisfaction score, these findings were not significant (Table 3).
Table 3. Relationship between the experience of time spent by patients in the clinic and total patient satisfaction score.
|
|
Correlation coefficient value |
p-value |
|---|---|---|
|
Expected Length of Consultation* |
-0.059 |
0.287 |
|
Perceived Length of Consultation |
0.097 |
0.081 |
|
Actual Length of Consultation# |
0.065 |
0.245 |
|
Waiting Time |
-0.034 |
0.539 |
|
Difference Between Perceived and Expected Length of Consultation+ |
0.151 |
0.006 |
|
Difference Between Actual and Expected Length of Consultation+ |
0.094 |
0.089 |
one of the cases with outliers was excluded from data analysis (n=326)
one of the cases with outliers was excluded from data analysis (n=326)
two of the cases with outliers were excluded from data analysis (n=325)
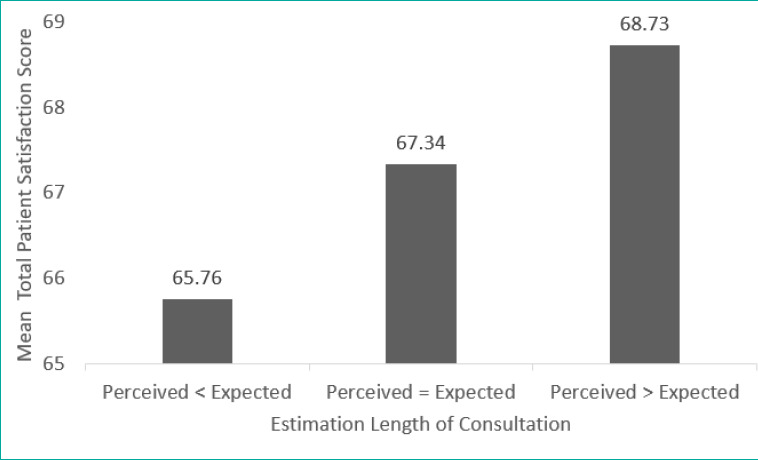
Association between total patient satisfaction score and estimated length of consultation
The patients who perceived the length of consultation to be longer than the expected length of consultation had a significantly higher mean total satisfaction score as compared with the patients who perceived the length of consultation to be equal to or shorter than the expected length of consultation (Figure 2).
Figure 2. Association between total patient satisfaction score and estimated length of consultation.
Association between total patient satisfaction score and socio-demographic characteristics, personal health, and visit information of participants
There was no significant association between total patient satisfaction score and the sociodemographic characteristics, personal health and visit information of the participants, except marital status (p=0.026). Married participants had a significantly higher mean total patient satisfaction score as compared with single participants (Table 4).
Table 4. Association between total patient satisfaction score and socio-demographic characteristics of participants.
|
Participant profile |
Number of participants, n (%) |
Mean total satisfaction score |
p-value |
|---|---|---|---|
|
Gender |
|
|
|
|
Male |
143 (43.7) |
67.22 |
0.173# |
|
Female |
184 (56.3) |
67.15 |
|
|
Race |
|
|
|
|
Malay |
157 (48.0) |
67.88 |
0.257* |
|
Chinese |
82 (25.1) |
66.37 |
|
|
Indian |
79 (24.2) |
66.49 |
|
|
Other |
9 (2.8) |
68.56 |
|
|
Marital Status |
|
|
|
|
Single |
74 (22.6) |
66.05 |
0.026 # |
|
Married |
253 (77.4) |
67.51 |
|
|
Job Status |
|
|
|
|
Working |
147 (45.0) |
67.20 |
0.100* |
|
Not working |
92 (28.1) |
66.47 |
|
|
Student |
18 (5.5) |
64.94 |
|
|
Retired |
70 (21.4) |
68.64 |
|
|
Type of Occupation |
|
|
|
|
Government sector |
51 (35.2) |
68.12 |
0.211* |
|
Private sector |
82 (55.1) |
66.44 |
|
|
Self-employed |
14 (9.7) |
68.36 |
|
|
Highest Education Level |
|
|
|
|
Primary school |
39 (11.9) |
68.00 |
0.735* |
|
Secondary school |
147 (45.0) |
66.62 |
|
|
Diploma |
55 (16.8) |
67.04 |
|
|
Degree |
62 (19.0) |
67.65 |
|
|
Postgraduate degree |
17 (5.2) |
68.29 |
|
|
No formal education |
7 (2.1) |
68.86 |
|
Independent t-test
ANOVA test
Association between total patient satisfaction score and associated factors
By using a multiple regression model, we determined that the only factor with significant positive correlation with total patient satisfaction score was the difference between perceived and expected length of consultation (regression coefficient: 0.110, p=0.02). The VIF of all examined factors was less than 5, showing no evidence of multicollinearity problems (Table 5).
Table 5. Association between total patient satisfaction score and associated factors (multiple regression model).
|
Variables |
Regression Coefficient (b) |
p-value |
95% Confidence Interval |
Collinearity Statistics (VIF) |
|---|---|---|---|---|
|
Constant |
69.326 |
|
|
|
|
Age |
0.047 |
0.119 |
-0.012-0.106 |
1.962 |
|
Gender |
-0.013 |
0.986 |
-1.535-1.509 |
1.068 |
|
Marital Status |
-0.158 |
0.887 |
-2.350-1.528 |
1.583 |
|
Job Status |
-0.358 |
0.709 |
-2.244-0.106 |
1.648 |
|
Type of Occupation |
-1.827 |
0.126 |
-4.173-0.519 |
1.342 |
|
Actual Length of Consultation |
0.021 |
0.685 |
-0.079-0.120 |
1.140 |
|
Waiting Time |
-0.007 |
0.531 |
-0.030-0.016 |
1.029 |
|
Difference Between Perceived and Expected Length of Consultation |
0.110 |
0.020 |
0.018-0.202 |
1.148 |
Final Model Equation
Total Patient Satisfaction Score = 69.326 + 0.110* (Difference Between Perceived and Expected Length of Consultation)
Discussion
The only significant positive correlation with total patient satisfaction score in this study using the multiple regression model was the difference between perceived and expected length of consultation. This finding was consistent with a study conducted by Lin et al. where the patients perception of time spent with the physician that met or exceeded the expected time was associated with a significantly higher patient satisfaction score.18 Another study by Cape et al. showed that patients who overestimated the time spent with their physician had a higher satisfaction score, suggesting that patients’ perception of time spent with their physician had a greater bearing on patient satisfaction than the actual time spent with the physician.19 Therefore, patient satisfaction is dependent on how long the patient perceives the consultation to have lasted and their expectation of the length of consultation.
The patient’s experience with the consultation is crucial for the length of consultation perceived by the patient. If the consultation experienced by patients is positive, they perceive the length of the consultation to be longer than it actually is.19 This observation brought about the concept of ‘perceived quality of consultation’. The perceived quality of consultation is influenced by the setting of the clinic and both the verbal and nonverbal behaviour of the treating physician.20 The expectation of the length of consultation may represent the expectation of how the consultation takes place indirectly. A study by Ogden et al. reported that dissatisfaction with the emotional aspects of the consultation and lower intention to comply with doctors’ recommendations were significantly correlated with the patient’s preference for more time during the consultation. Therefore, changing how the time is spent in consultation (e.g., by listening to patients and trying to understand their needs) could improve the patient’s satisfaction with consultation length rather increasing the actual length of the consultation.21 This hypothesis is further supported by a meta-analysis by Lemon and Smith suggesting that actual length of consultation was not the variable responsible for improving patient satisfaction, but rather the exploration of the patient’s psychosocial factors.22 Therefore, it is crucial to ascertain the expectations and psychosocial needs of the patient during each consultation and to manage them accordingly to achieve higher patient satisfaction.
The mean total patient satisfaction score in this study was 67.18, which was 74.64% of the maximum score (90). The proportion of satisfied patients was 50.46% when using mean total satisfaction score as the cut-off, which was much lower than most local studies with reported proportions of satisfied patients ranging from 78.8% to 93.1%.5,9,12 However, several local studies on patient satisfaction reported lower satisfied patient rates, ranging from 19.4% to 27.5%.10,13 The differences can partly be attributed to the different patient satisfaction study instruments used, such as SERVQUAL, PSQ III, PSQ II, and different cut-off points for satisfied patients. The lower reported satisfaction score could also be a result of issues in the health care delivery, especially in the domains of accessibility, convenience, and time spent with the doctor.
In this study, the communication domain had the highest satisfaction score, with 80.80% of the maximum score. In contrast, the accessibility and convenience domain had the lowest score, with only 66.40% of the maximum score. These findings are consistent with the findings of another study conducted in a university clinic, Universiti Kebangsaan Malaysia Medical Centre (UKMMC) Primary Care Clinic, where 96.5% of the respondents were satisfied with the ‘doctors’ domain, which mainly examined the doctors’ communication skills (i.e., social skills, information gathering skills, and information giving skills); in contrast, only 68.1% of the respondents were satisfied with the ‘accessibility’ domain.5 Another study conducted in a government primary care clinic reported contradicting results: 61.1% of the respondents were satisfied with the ‘accessibility’ domain, 35.1% of the respondents were satisfied with the ‘interpersonal manner’ domain, and only 6.7% of the respondents satisfied with the ‘continuity of care’ domain.11 Both UMMC Primary Care Clinic and UKMMC Primary Care Clinic are training facilities for postgraduate trainees in Family Medicine; most of the doctors at these two facilities are master students trained to communicate effectively with patients. This may have contributed to the higher satisfaction score in the ‘communication’ and ‘doctors’ domains as compared with the scores of the government primary care clinic of the Ministry of Health. In terms of accessibility, the government primary care clinic achieved a higher satisfaction score as these clinics are located within the community and are therefore close to the patients’ homes.
Appointment intervals are also usually shorter as these clinics. Both the UMMC Primary Care Clinic and UKMMC Primary Care Clinic are located in busy city areas and appointment intervals are much longer due to high patient load.
This study examined the association of expected, perceived, and actual length of consultation with patient satisfaction in a primary care clinic. The difference between perceived and expected length of consultation had a significant positive correlation with patient satisfaction and highlights the importance of focusing on ways to improve the patient’s perception of the consultation time and managing the patient’s expectations of consultations. By doing so, the patient’s satisfaction will be improved and thus a better quality of health care service can be rendered. The limitations of this study are its low recruitment rate of 62.5 % and that its results are not generalisable to the entire population. There may also have been observation bias, as the doctors who participated were aware that they were being studied. The data collection was completed in 2016, therefore the results are not recent.
Further studies should examine factors that influence patients’ expectations and perceptions of consultation quality and duration. Our findings showed that quality of time in consultation is important in clinical practice; therefore, we recommend that communication with patients be improved by implementing skill workshops for doctors.
The proportion of satisfied patients using the mean as the cut-off point was lower than in comparable studies. This indicates that there are issues that must be corrected, especially in the domain of accessibility and convenience. The perceived length of consultation exceeding the expected length of consultation was the only significant factor associated with high patient satisfaction. Therefore, changing the way the time is spent in consultation might be a more feasible way to improve patient satisfaction rather than increasing the actual length of the consultation.
Acknowledgments
This study was funded by the University Malaya Postgraduate Research Fund (PO036-2016A).
Conflicts of Interest
The authors declare no conflicts of interest.
How does this paper make a diffrence in general practice?
Based on this study, the perceived length of consultation exceeding the expected length of consultation was significantly associated with a higher satisfaction score. Changing how the time is spent in consultation (e.g., by listening to patients and trying to understand their needs) rather than increasing the length of the consultation might be a more feasible way to improve patient satisfaction in view of time constraints during busy clinic sessions.
The development of a system where the patients can record the expected length of consultation before their consultation might be useful.
References
- 1.Weiss GL. Patient satisfaction with primary medical care evaluation of sociodemographic and predispositional factors. Med Care. 1988;26:383–92. doi: 10.1097/00005650-198804000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Cleary PD. The increasing importance of patient surveys. QHC. 1999;8:212. doi: 10.1136/qshc.8.4.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pascoe GC. Patient satisfaction in primary health care: a literature review and analysis. EvalProgram Plann. 1983;6:185–210. doi: 10.1016/0149-7189(83)90002-2. [DOI] [PubMed] [Google Scholar]
- 4.Ganasegeran K, Perianayagam W, Abdul Manaf R, Ali Jadoo SA, Al-Dubai SAR. Patient satisfaction in Malaysia’s busiest outpatient medical care. Sci World J. 2015:2015. doi: 10.1155/2015/714754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hizlinda T, Teoh S, Siti Nurbaiyah K, et al. A cross-sectional study on patient satisfaction with Universiti Kebangsaan Malaysia Medical Centre (UKMMC) primary care clinic. Med Health. 2012;7:12–23. [Google Scholar]
- 6.Anderson RT, Camacho FT, Balkrishnan R. Willing to wait? The influence of patient wait time on satisfaction with primary care. BMC Health Serv Res. 2007;7:1. doi: 10.1186/14726963-7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dugdale DC, Epstein R, Pantilat SZ. Time and the patient—physician relationship. J Gen Intern Med. 1999;14:34–40. doi: 10.1046/j.1525-1497.1999.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davidoff F. Time. Ann Intern Med. 1997;127:483–5. doi: 10.7326/0003-4819127-6-199709150-00011. [DOI] [PubMed] [Google Scholar]
- 9.Sharifa Ezat W, Jamsiah M, Malka S, Azimatun Noor A, Tuti Ningseh NIA. Customers’ satisfaction among urban and rural public health clinics in state of Selangor, Malaysia. Malays J Public Health Med. 2010;10:52–67. [Google Scholar]
- 10.Aizuddin AN, Salmiah B, Ahamad J. Kajian keratan rentas perbandingan kepuasan pelanggan di antara klinik-klinik kesihatan primer luar bandar dan bandar di daerah hulu langat dan faktor-faktor yang mempengaruhi. Malays J Public Health Med. 2012;12:52–67. [Google Scholar]
- 11.Haliza A, Rizal A, Jamaluddin RR, Noorhaida U. Kepuasan pelanggan di kalangan pesakit luar klinik kerajaan dan klinik swasta di Seremban, Negeri Sembilan. J Kesihat Masy. 2005;11:1–11. [Google Scholar]
- 12.Aniza I, Suhaila A. Clients satisfactions in ISO certified health clinic in Klinik Kesihatan Bandar Baru Bangi, Selangor and its associated factors. J Kesihat Masy. 2011;17:18–25. [Google Scholar]
- 13.Haliza A, Rizal A, Jamaluddin RR. Kajian kepuasan pelanggan di kalangan pesakit klinik swasta di Seremban, Negeri Sembilan. J Kesihat Masy. 2003;9:45–51. [Google Scholar]
- 14.Marshall GN, Hays RD. The patient satisfaction questionnaire short-form (PSQ-18). Rand Santa Monica, CA: 1994. [Google Scholar]
- 15.Narimah AHH, Shahril Rizwan O, Nadhrah NR, Adlina S, Hakimi ZA, Nuraliza AS. A descriptive cross-sectional study on patient satisfaction in a private hospital in Selangor. Malays J Public Health Med. 2006;6:6–12. [Google Scholar]
- 16.Chan C, Azman W. Attitudes and role orientations on doctor-patient fit and patient satisfaction in cancer care. Singapore Med J. 2012;53:52. [PubMed] [Google Scholar]
- 17.Lim B, Hamid M, Khoo S, Yusof A. Patient satisfaction in the treatment of acute hamstring strain injury. IJKSS. 2014;2:9. doi: 10.7575/aiac.ijkss.v.2n.2p.9. [DOI] [Google Scholar]
- 18.Lin C-T, Albertson GA, Schilling LM, et al. Is patients' perception of time spent with the physician a determinant of ambulatory patient satisfaction? Arch Intern Med. 2001;161:1437–42. doi: 10.1001/archinte.161.11.1437. [DOI] [PubMed] [Google Scholar]
- 19.Cape J. Consultation length, patient-estimated consultation length, and satisfaction with the consultation. Br J Gen Pract. 2002;52:1004–6. [PMC free article] [PubMed] [Google Scholar]
- 20.Lussier M-T, Richard C. Time flies: patients’ perceptions of consultation length and actual duration. Can Fam Physician. 2007;53:46–7. [PMC free article] [PubMed] [Google Scholar]
- 21.Ogden J, Bavalia K, Bull M, et al. “I want more time with my doctor”: a quantitative study of time and the consultation. Fam Pract. 2004;21:479–83. doi: 10.1093/fampra/cmh502. [DOI] [PubMed] [Google Scholar]
- 22.Lemon TI, Smith RH. Consultation content not consultation length improves patient satisfaction. J Fam Med Prim Care. 2014;3:333–9. doi: 10.4103/2249-4863.148102. [DOI] [PMC free article] [PubMed] [Google Scholar]


