Abstract
Objective:
Childhood trauma exacts a lasting toll on one’s own mental health and the health of one’s offspring; however, limited research has examined the pathways through which this intergenerational transmission occurs. This study aimed to identify the transactions and mechanisms that link maternal early life trauma, maternal depressive symptoms, and children’s internalizing symptoms.
Method:
A pregnancy cohort of N = 1462 mothers (66% Black, 32% White, 2% Other race) reported their childhood trauma exposure and depressive symptoms during pregnancy. Maternal depressive and children’s internalizing symptoms were measured repeatedly when offspring were 12, 24, 36, and 48–60 months of age. A path model tested the transactional associations between maternal and child symptomatology and mediation of maternal childhood trauma on offspring symptoms via maternal depressive symptoms.
Results:
Mothers’ childhood trauma history was related to greater prenatal and postnatal (12 and 24 months) maternal depressive symptoms, which were prospectively associated with offspring internalizing problems at 36 and 48–60 months. Child-directed effects on maternal depressive symptoms were not observed. The association of maternal trauma on children’s internalizing at 36 months was mediated by maternal depressive symptoms at 24 months.
Limitations:
Assessments of the key study variables were provided by mothers. Childhood trauma was evaluated retrospectively.
Conclusion:
Women’s experiences of adversity in childhood have persistent and cumulative effects on their depression during the transition to parenthood, which is associated with risk for children’s internalizing. Given the two-generation influence of maternal childhood trauma exposure, attending to its impact may protect both caregivers and their children.
Keywords: Adverse childhood experiences, intergenerational trauma transmission, prenatal programming, maternal depression, child internalizing
Exposure to traumatic and stressful early life experiences occur with alarming frequency. In a nationally representative sample, approximately one-quarter of adults experienced three or more adversities in childhood (Mersky et al., 2021), with some evidence that individuals who identify as Black or female are more frequently exposed (Merrick et al., 2018). The negative sequelae of childhood traumas span multiple domains of health (i.e., physical, social, emotional; Hughes et al., 2017), extend across the lifespan (Herzog and Schmahl, 2018), and may be transmitted from one generation to the next (Plant et al., 2018). This latter point, referring to the intergenerational transmission of trauma, describes the risk conferred by mothers’ own experiences of adversity on their children’s emotional and behavioral problems. In a growing research program, mothers’ exposure to childhood traumatic events (CTE; e.g., physical, sexual, or emotional abuse; neglect; exposure to domestic violence) has been associated with a range of socioemotional, behavioral, and neurodevelopmental outcomes among offspring (Plant et al., 2018). Following this consistent documentation of which child outcomes are influenced by maternal early life adversity, empirical investigations have turned to examining how such associations emerge. The mechanistic pathways that link maternal CTE to child outcomes are complex and likely interactive, including biological factors (Jones et al., 2019), negative life events (Negriff et al., 2020), attachment styles (Cooke et al., 2019), and maternal mental health (Browne et al., in press; Doi et al., 2020). The present study focuses on the potential mediating role of maternal depressive symptoms, given the high prevalence of such symptomatology among women who have experienced early trauma (Letourneau et al., 2019). For example, a meta-analysis of more than 16 epidemiological studies found that adults who experienced childhood maltreatment or abuse were twice as likely to develop persistent and recurrent depression (Nanni et al., 2012).
Depressive symptoms among mothers, in turn, serve as a risk factor for children’s emotional problems, particularly internalizing symptoms (Goodman, 2020). Evidence for these separate pathways (i.e., maternal childhood trauma to maternal depressive symptoms; maternal depressive symptoms to children’s internalizing problems) has prompted tests (albeit limited) of comprehensive mediation models. In a study of mother-child dyads, Letourneau and colleagues found that maternal perinatal depressive symptoms mediated the relation between maternal adverse childhood experiences (ACEs) and internalizing behavior when children were 2 years of age (Letourneau et al., 2019). Though compelling, the Letourneau study recruited a sample of predominantly White, university-educated, Canadian mothers with higher incomes. Studies that explore these relations in racially and ethnically diverse samples and/or those with lower socioeconomic status are essential yet limited, which significantly detracts from the inclusivity and generalizability of intergenerational research on maternal adversity and mother/child emotional symptomatology (Henrich et al., 2010). Given racial disparities in adversity-related perinatal health outcomes and the provision of maternal child healthcare services (Lorch and Enlow, 2016), and the need for broad representation of all groups in psychological science (Roberts et al., 2020), it is essential to test these associations in diverse samples. Moreover, extant mechanistic research has generally been methodologically limited by cross-sectional designs and/or single assessments of maternal and child mental health during the early postpartum period (Doi et al., 2020).
Notably, research examining the consequences of maternal depression largely focuses on unidirectional parent-to-child effects, omitting consideration of an essential component of the processes through which parent and child symptoms develop and maintain over time: child-to-parent effects (Paschall and Mastergeorge, 2016). Transactional frameworks capture these dynamic reciprocal processes by modeling how parents and children influence (and are influenced by) each other in a continuous process of development (Paschall and Mastergeorge, 2016). In this way, developmental outcomes are not reduced to a sole cause (i.e., individual or environmental context), but are the product of continuous, interdependent interactions between the child and the family context (Sameroff, 2000). One longitudinal study of ethnically diverse, low-income children and their mothers observed transactional relations such that heightened levels of maternal depressive symptoms at 18 months were positively associated with internalizing symptoms among children at 4 years of age, while heightened levels of children’s internalizing at 18 months were associated with greater maternal depressive symptoms at 4 years (Roubinov et al., 2019). Despite the logical appeal and widespread acceptance of transactional models, such approaches continue to be underutilized when compared to models of parent-directed effects (Paschall and Mastergeorge, 2016). Moreover, prior transactional research has not examined the bidirectionality between maternal-child symptoms that may emerge from a backdrop of mothers’ CTE.
The present study examined longer-term direct and indirect associations among maternal CTE, maternal depressive symptoms, and children’s internalizing symptoms collected from pregnancy through age 5 in a longitudinal cohort of socioeconomically and racially diverse women and their offspring. In order to address the gaps in prior research, the current study tested the following four hypotheses:
Higher levels of prenatal and postpartum maternal depressive symptoms would predict higher child internalizing symptoms at subsequent timepoints.
Higher levels of child internalizing symptoms would predict higher maternal depressive symptoms at subsequent timepoints.
Mothers’ experiences of CTE would exert repeated, cumulative effects on maternal depressive symptoms over time such that maternal CTE could predict outcomes for mothers and children at multiple points in time, even when controlling for previous associations.
Maternal depressive symptoms would mediate the effect of mothers’ CTE on offspring internalizing symptoms.
Method
Participants.
The sample included mothers and their biological children who participated in the Conditions Affecting Neurocognitive Development and Learning in Early Childhood (CANDLE) Study, a prospective study of the effects of environmental exposures on maternal and child health among families in Shelby County, Tennessee (LeWinn et al., 2020). Women were recruited prenatally and followed during their offspring’s childhood years; the present study includes data from follow-up assessments through child age 5. Criteria for inclusion in the study were: (1) Shelby County resident, (2) between 16 and 28 weeks gestation, (3) between 16 and 40 years of age, (4) could speak and understand English, (5) had a singleton pregnancy, (6) low medical-risk pregnancy, and (7) planned to deliver at one-of-five participating health care settings in Shelby County. The Institutional Review Board at the University of Tennessee Health Science Center approved all study procedures prior to recruitment and data collection.
There were 5,228 women who were screened for eligibility. Of the 3,320 (63.5%) who met inclusion, 1,503 (45.3%) enrolled in the study. Sample descriptives for participants who were included in the present analyses are displayed in Table 1.
Table 1.
Sample demographics and descriptive statistics (n = 1462)
| Maternal race/ethnicity (n, %) | |
| Black | 961 (65.8%) |
| White | 472 (32.3%) |
| Other race (Asian, American Indian/Alaska Native, Native Hawaiian/Pacific Islander or Other) | 27 (1.8%) |
| Child sex (n, %) | |
| Male | 736 (50.3%) |
| Household income (M, SD) | $20,567 ($18,863) |
| Maternal childhood traumatic event types (n, %) | |
| 0 traumatic event types | 852 (63.0%) |
| 1 traumatic event types | 341 (25.2%) |
| 2 traumatic event types | 122 (9.0%) |
| 3 traumatic event types | 38 (2.8%) |
| Maternal depressive symptoms (M, SD) | |
| 3rd trimester of pregnancy | 0.24 (0.4) |
| 1 year | 0.21 (0.2) |
| 2 years | 0.20 (0.4) |
| 3 years | 0.21 (0.5) |
| 4–5 years | 0.19 (0.4) |
| Children’s internalizing symptoms (M, SD)a | |
| 12 months | 2.01 (1.6) |
| 24 months | 2.20 (1.7) |
| 36 months | 6.71 (6.2) |
| 48–60 months | 6.21 (6.1) |
Note.
Children’s internalizing symptoms were measured by the BITSEA at 12 and 24 months and the CBCL at 3 and 4–5 years.
Procedures
Women were recruited from university medical group clinics and through community outreach. For any woman under 18 years old, a legally authorized representative co-signed the written informed consent. Prenatal data were collected from women during a third trimester clinic visit (when women were between 27 and 42 weeks pregnant). Subsequent study assessments were conducted in the homes or during children’s clinic visits: 12 months (clinic visit), 24 months (clinic or home visit), 36 month (clinic visit), and 48–60 months (clinic visit).
Measures
Maternal childhood traumatic events (CTE).
Three items from Traumatic Life Events Questionnaire (TLEQ) were used to assess women’s exposure to CTE. The TLEQ is a 23-item measure that evaluates lifetime exposure to traumatic events across varied stressor types (Kubany et al., 2000). Prior research has found the measure to have high reliability and validity (Peirce et al., 2009). Three of the items on the TLEQ are specific to childhood traumas and thus, were used for the current study: 1) physically punished growing up, 2) witnessed violence growing up, and 3) sexual molestation before 13th birthday. As in prior published studies using the CANDLE cohort, affirmative responses were summed to create a count of CTE (0–3) (Adgent et al., 2019; Ahmad et al., 2021; Pilkay et al., 2020; Shih et al., 2020; Slopen et al., 2018; Steine et al., 2020).
Maternal depressive symptoms.
At all five study timepoints (prenatal; 12, 24, 36, and 48–60 months postpartum), mothers completed the Brief Symptom Inventory (BSI). The BSI is one of the most widely used and accepted measures of psychiatric symptoms that was adapted from the longer Symptom Checklist-90-R (Derogatis and Melisaratos, 1983). It has good construct validity, concurrent validity, internal consistency, and test-retest reliability (Derogatis & Fitzpatrick; Urbán et al., 2014). The present study used the Depression subscale from the BSI, which evaluates the severity of six symptoms during the prior 7 days on a 5-point Likert scale (0 = never to 5 = almost always). Higher scores indicate greater depressive symptoms.
Child internalizing symptoms.
Offspring internalizing symptoms were evaluated with two different measures in accordance with children’s age/developmental stage. At 12 and 24 months, mother’s reported on child internalizing symptoms using the 8-item Internalizing subscale of the Brief Infant Toddler Social Emotional Assessment (BITSEA; Briggs-Gowan et al., 2004). Example items include “cries or hangs onto you when you try to leave,” “seems very unhappy, sad, depressed, or withdrawn,” and “worries a lot or is very serious.” At 36 and 48–60 months, mothers completed the 36-item Internalizing subscale of the Child Behavior Checklist (Achenbach and Rescorla, 2000). The CBCL evaluates a number of the same internalizing symptoms as the BITSEA (e.g., “unhappy, sad, or depressed,” “worries,” “withdrawn, doesn’t get involved with others,” “gets too upset when separate from parents”), as well as other developmentally-appropriate internalizing symptoms that may emerge in later toddlerhood (e.g., “doesn’t answer when people talk to him/her,” “acts too young for age”).
Covariates.
All models were adjusted for child sex (0 = female, 1 = male), maternal race (0 = Black and Other Race, 1 = White), and household income adjusted for family size when children were 12 months old (see Table 1). Note, we did not also control for education in models since the correlation between income and education in this sample was very high (r = 0.70, p < 0.001).
Data Analysis
Cross-lagged panel model (CLPM) analysis was used to examine the association among maternal CTE, maternal depressive symptoms, and child internalizing symptoms when mothers were in their third trimester of pregnancy, and when offspring were 12, 24, 36, and 46–60 months old.1 Models of this type permit simultaneous examination of autoregressive paths within variables over time and directional associations between variables controlling for previous levels (i.e., the association of maternal depression at time 1 to child internalizing at time 2 and vice versa). We also included paths from maternal CTE to maternal depression and child internalizing at every time point. In addition to the standard autocorrelations among repeated measures, pathways were also permitted linking observations across two time points (e.g., 24 months maternal depression with 3rd trimester maternal depression, 36 months maternal depression with 12 months maternal depression, 48–60 months maternal depression with 24 months maternal depression). Such “time minus two timepoints” correlations were included to account for the high stability in our repeated measures of maternal depression and child internalizing. Model fit was evaluated using a) root mean squared error of the approximation (RMSEA; cutoff value < 0.06), b) comparative fit index (CFI; cutoff value > 0.95), c) standardized root mean square residual (SRMR < .08), d) Tucker-Lewis index (TLI; cutoff value > 0.95), and e) chi-square with degrees of freedom and p (Hu and Bentler, 1999; West, Taylor, & Wu, 2012). Maternal race, child sex, and income were included as covariates in all adjusted models, and scores were standardized given that different measures of child internalizing problems were used in the present analyses (BITSEA at the 12 and 24 month assessments and CBCL at the 36 and 48 month assessments, as described above). All analyses were conducted in Mplus version 8.1 (Muthén, L.K. & Muthén, B.O., 1998) with maximum likelihood estimation with robust standard errors (MLR) as our estimation method since it is robust to non-normality. Standardized estimates are reported. Effect sizes were evaluated as small (β < 0.1), medium (β∈ [0.1, 0.5], or large (β ≥ 0.5) (Cohen, 1988).
Missing data.
In accordance with the recommended standard missing data handling procedures (Graham, 2009), hypothesis testing was carried out with full information maximum likelihood (FIML) procedures supplemented by auxiliary variables. Of the full sample N = 1,503 women recruited in the study, the present analytic sample of N = 1,462 women included those with a living child who provided data during the prenatal assessment and at least one postnatal visit. Women who were missing all postnatal data were excluded. Women who were retained did not differ from those who were excluded on the basis of race (p = 0.41), exposure to childhood trauma (p = 0.69), or prenatal depressive symptoms (p = 0.57). Simulation studies for complex mediation suggest that our sample size is larger than the minimum sample size required (N>640) to detect small indirect effects with power > .80 (Thoemmes, MacKinnon, & Reiser, 2010).
Results
As shown in Table 1, over one-third of mothers reported exposure to at least one type of traumatic event during childhood: 25% experienced one type, 9% experienced two types, and 2.8% experienced all three types of traumatic events. Zero-order correlations are provided in Table 2.
Table 2.
Zero-order correlations among study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Maternal childhood traumatic exposures | -- | |||||||||||
| 2. Prenatal maternal depressive symptoms | .19*** | -- | ||||||||||
| 3. 12 month maternal depressive symptoms | .19*** | .51*** | -- | |||||||||
| 4. 24 month maternal depressive symptoms | .15*** | .44*** | .45*** | -- | ||||||||
| 5. 36 month maternal depressive symptoms | .14*** | .38*** | .41*** | .55*** | -- | |||||||
| 6. 48–60 month maternal depressive symptoms | .16*** | .40*** | .45*** | .50*** | .41*** | -- | ||||||
| 7. 12 month child internalizing symptoms | .19*** | .10** | .16*** | .08* | .004 | .10** | -- | |||||
| 8. 24 month child internalizing symptoms | .07* | .11*** | .10*** | .21*** | .11*** | .11*** | .36*** | -- | ||||
| 9. 36 month child internalizing symptoms | .07* | .11*** | .20*** | .17*** | .24*** | .14*** | .27*** | .37*** | -- | |||
| 10. 48–60 month child internalizing symptoms | .10** | .17*** | .23*** | .26*** | .22*** | .35*** | .21*** | .32*** | .48*** | -- | ||
| 11. Child sex | −.03 | −.04 | −.04 | .01 | .008 | .01 | −.02 | .03 | −.03 | −.003 | -- | |
| 12. Household income at 12 months | −.19*** | −.11*** | −.09** | −.09** | −.08* | −.10** | −.25*** | −.21*** | −.13*** | −.09** | −.03 | -- |
| 13. Maternal race/ethnicity | −.09** | −.01 | .03 | −.02 | −.01 | −.02 | −.21*** | −.17*** | −.004 | −.01 | −.03 | .50*** |
Notes. Child sex coded as 0 = Female, 1 = Male. Maternal race coded as 0 = Black or Other Race, 1 = White.
p < .05,
p < .01,
p < .001
Fit indices for the cross-lagged model presented in Figure 1 indicated a good fit of the model to the data (RMSEA = 0.05 (90% CI = 0.04, 0.06), CFI = 0.95, SRMR = .04; TLI = 0.80; χ2(72) = 1518, p = 0.00). Although the TLI was below the recommended cut-off, the RMSEA, CFI, and SRMR of the current model suggest good fit. Prior research states that a combination of RMSEA < .06 and SRMR < .08 indicates good model fit (Hu & Bentler, 1999); the present model meets these criteria. Autoregressive paths for both maternal depression and child internalizing indicated significant stability from the prenatal period through child age 5 across both constructs (all ps < 0.05). Below, we organize our primary results by hypothesis.
Figure 1.
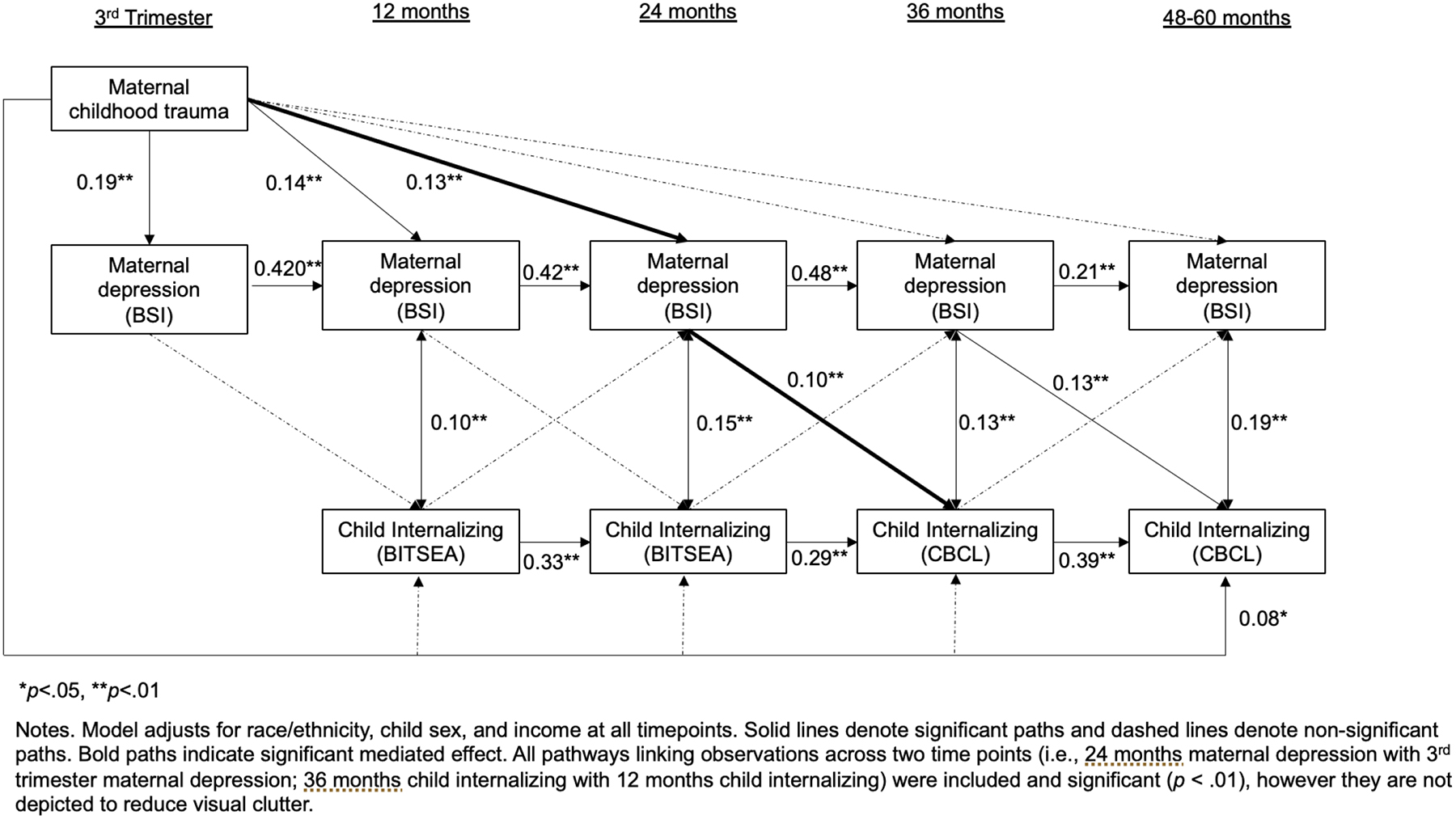
Cross lagged panel model with standardized estimates linking maternal exposure to childhood trauma, maternal depressive symptoms, and children’s internalizing symptoms.
Hypothesis 1: Evidence of transactional associations emerged at two timepoints during the early childhood period. Higher levels of maternal depressive symptoms at 24 months were associated with higher child internalizing symptoms at 36 months (β = 0.097, SE = 0.037, p < 0.01) and similarly, maternal depressive symptoms at 36 months were positively associated with child internalizing at 48–60 months (β = 0.126, SE = 0.05, p < 0.01), reflecting small and medium sized effects, respectively. Notably, such relations emerged even after accounting for the stability of children’s internalizing symptoms and the concurrent relations between the residuals of the maternal depressive symptoms and children’s internalizing symptoms.
Hypothesis 2: The paths representing child-directed effects were not significant from infancy through early childhood. Thus, there was no evidence that children’s internalizing symptoms predicted maternal depressive symptoms during the study period after adjusting for prior relations across time.
Hypothesis 3: Mothers’ exposure to childhood trauma was associated with maternal depressive symptoms during the perinatal through early toddlerhood periods. More specifically, maternal CTE was associated with depressive symptoms during the third trimester of pregnancy (β = 0.194, SE = 0.42, p < 0.01), and when children were 12 months (β = 0.138, SE = 0.04, p < 0.01) and 24 months old (β = 0.131, SE = 0.05, p < 0.01), reflecting medium sized effects. After accounting for these prior relations and the stability of depression, mothers’ childhood trauma was not significantly associated with maternal depressive symptoms when children were between 36 and 60 months of age.
Hypothesis 4: Maternal childhood trauma exposure predicted her depressive symptoms during the postpartum period, which in turn, predicted internalizing symptoms in her offspring. We tested three indirect effects suggested by the significant paths in Figure 1. The effect of maternal childhood trauma on offspring internalizing at 36 months was significantly mediated by maternal depressive symptoms at 24 months (β = 0.013, 95% CI 0.001 to 0.025, p = 0.04), a small effect. Two additional serial mediation paths were not significant: 1. Maternal CTE to maternal depressive symptoms from 12 to 24 months to children’s internalizing symptoms at 36 months (β = 0.006, 95% CI 0.0 to 0.012, p = 0.052) and 2. Maternal childhood trauma to maternal depressive symptoms from 24 to 36 months to children’s internalizing symptoms at 48–60 months (β = 0.008, 95% CI −0.002 to 0.018, p = 0.10).
Discussion
An individual with a history of traumatic experiences in childhood may endure effects of such exposures across their lifespan and potentially transmit such impacts to subsequent generations. However, studies rarely consider the complexities of such relations, including how caregiver and offspring mental health are reciprocally related over time. Integrating intergenerational transmission of trauma and parent-child transactional frameworks, the current study examined how risk initiated by mothers’ early CTE generated subsequent reciprocal associations between maternal and child mental health. In a large, prospective, longitudinal cohort study of predominantly Black and White families, mothers’ childhood trauma was associated with maternal depressive symptoms from the perinatal period through 24 months postpartum, but it did not continue to add predictive value to maternal depressive symptoms in later toddlerhood. During toddlerhood, maternal depressive symptoms were associated with children’s internalizing symptoms, however child-directed effects of internalizing on subsequent maternal depressive symptoms were not found. A mechanistic pathway was observed whereby the association of maternal childhood trauma on child internalizing at 36 months operated through maternal depressive symptoms at 24 months. This study represents a rigorous test of intergenerational transmission and directionality of effects, as all pathways controlled for previous levels of the predictors and outcome variables and all directions and timings of association were considered from pregnancy to 60 months postpartum.
In the present study, heightened levels of depressive symptoms were observed among mothers with early trauma exposure, confirming prior empirical associations (Choi et al., 2019). A unique feature of the current research is its intensive, repeated measures longitudinal design, which provides for a nuanced exploration of timing. Illustratively, we observed persistent, cumulative effects of maternal CTE on prenatal, 12, and 24 month postnatal maternal depressive symptoms, but no significant relations between CTE and maternal depression when children were 36 through 60 months of age. In general, the perinatal and infancy periods place women at risk for the development of depressive symptoms given normative bodily changes, physical discomfort, identity/role changes, and lack of sleep (Davis and Narayan, 2020). Women with a history of early adversity exposure may be particularly vulnerable because infant and child distress may cue her own early trauma, exacerbating the stressors that typically emerge during this time (Davis and Narayan, 2020). Originating in attachment theory (Bowlby, 2008), the metaphors “ghosts in the nursery” (Fraiberg et al., 1975) and “voices from the past” (Bernard et al., 2012) describe the ways in which mothers’ own experiences of abuse, neglect, or other childhood trauma may powerfully influence her adjustment during the transition to parenthood. For mothers in current study, it appears that the legacy of CTE exerts a particularly pronounced effect during pregnancy and in offspring’s first two years of life compared to later in childhood.
Transactional paths revealed that maternal depressive symptoms at 24 and 36 months were prospectively associated with children’s internalizing problems at the subsequent timepoint (36 and 48–60 months, respectively). However, maternal depression measured during pregnancy or the earlier postpartum periods (12 and 24 months) was not associated with children’s later internalizing symptoms. Exposure to perinatal maternal depression has been strongly implicated in the development of offspring behavior problems (Goodman, 2020), thus the lack of significant predictive associations for this time period in the current study is surprising, though not without precedent. In a nationally representative sample, children exposed to maternal depression between the ages of 2 to 3 years and 4 to 5 years were at greater odds for developing behavior problems, however risk was not elevated among children exposed to maternal depression during the first postpartum year (Naicker et al., 2012). It may be the case children experience greater negative effects from cumulative exposure to maternal depression, which would be reflected by an association with later maternal depression (when children are 3 to 5 years of age) that persists from earlier postpartum depression (when children are 1 to 2 years of age; Halligan et al., 2007). While such findings may suggest a substantive rationale for our pattern of findings, potential methodological reasons may also play a role. In particular, it is harder to discriminate or identify internalizing problems among younger children who have less developed verbal skills compared to when children are older such that there may be limitations in the measurement of this construct at earlier ages.
Similarly surprising was the lack of child-directed effects of early internalizing problems on subsequent maternal depressive symptoms. In other words, maternal depressive symptoms in the current study increased risk for offspring maladjustment, but evidence for the opposing relation was not observed. Although reciprocal relations are less commonly observed during infancy (Hanington et al., 2010), emerging evidence of bidirectionality between maternal depression and children’s behavior problems has been found in prior longitudinal studies of older children (Roubinov et al., 2019). Notably, prior transactional models of maternal and child mental health have not attended to mothers’ experiences of adversity during the childhood period and it is possible that a relatively stable factor, such as the influence of CTE, could operate as confound (Dora and Baydar, 2020). Our inclusion of maternal childhood adversity in our predictive models may thus explain the small/nonsignificant reciprocal relations found in our models. Depressive disorders among adults with and without exposure to childhood abuse have also been suggested to represent two distinct subgroups of depression given differences in neurobiological underpinnings (Teicher and Samson, 2013) and responsiveness to treatment (Nanni et al., 2012). For women with a history of childhood trauma, it may be the case that factors other than their children’s behavior problems exert a more marked impact on depressive symptoms, compared to women without such a history. However, it is also possible that significant associations from children’s behavior problems to maternal depression did not emerge due to a lack of statistical power.
Broadening and strengthening prior research that has examined these associations among samples with higher socioeconomic status and using cross-sectional designs (Plant et al., 2018), we observed an indirect pathway of maternal CTE on child internalizing problems via a pathway of maternal depressive symptoms in our socioeconomically and racially diverse sample. Results of this explanatory pathway in the present longitudinal study suggests specificity in the timing of such effects: Maternal CTE was associated with maternal depressive symptoms at 24 months postpartum, which was associated with internalizing when offspring were 36 months of age. Thus, maternal depression during offspring’s early years of life appeared to serve as a mechanism linking a mother’s own childhood trauma exposure to her child’s internalizing problems. However, there was no evidence that mothers’ childhood trauma influenced children’s behavior problems through a mechanism of maternal mental health in pregnancy. It is interesting to speculate why we observed postnatal (but not prenatal) programming effects. Some studies of fetal programming suggest a stronger influence of prenatal anxiety (Glover, 2011) and prenatal stress (Bush et al., 2021) than prenatal depression on children’s development, thus our focus on the latter may have precluded significant findings. Moreover, behavior problems among older offspring appear to be more strongly influenced by depression exposure during the postpartum and later childhood periods rather than prenatal exposure (Hay et al., 2008). Finally, other findings from this cohort indicate that maternal CTE predicts the level and rise of placental Corticotrophin-Releasing Hormone (pCRH; Steine et al., 2020) a hormone only detectable only during pregnancy that is associated with both risk for maternal postpartum depression (Glynn and Sandman, 2014) and children’s neurodevelopmental outcomes (Howland et al., 2016). It may be that effects of maternal CTE on maternal and child mental health are operating, at least in part, through effects on maternal biology during pregnancy. This is an area ripe for further study.
Strengths and Limitations
Strengths of the current study include its prospective, longitudinal design and repeated measures that allow for examination of both timing and directionality of associations among maternal childhood trauma, maternal depressive symptoms, and child internalizing problems during a salient period of child development. However, there are a number of limitations that must also be considered. Assessments of the three primary study constructs (maternal CTE, maternal depressive symptoms, child internalizing problems) were provided by mothers, introducing depression-related negative perceptual biases that may contribute to overreporting of child adjustment problems (Chilcoat and Breslau, 1997). Future research would be strengthened by evaluations of child behavior by other informants (e.g., preschool teacher, other primary caregivers) and/or observational measures, although this is not typical in studies of young child internalizing and often not feasible to collect within large cohorts. Although depressive and internalizing symptoms were assessed in a prospective manner, maternal CTE was evaluated retrospectively. Questions have been raised about the validity of retrospective reports, however prospective and retrospective reports of adversity show moderate agreement and the latter is more strongly predictive of subjectively measured adult outcomes than the former (Reuben et al., 2016). Heritability is a mechanism for the transmission of depression from parents to offspring (Goodman, 2020), though we did not measure genetic factors in the present study. Statistically significant mother-child paths are likely partly due to heritability and partly due to environmental influences. Finally, the present study focused on maternal depression given its prevalence during the childbearing years and its well-established associations with children’s internalizing symptoms (Goodman, 2020). Yet, empirical studies suggest parents’ symptoms of posttraumatic stress may be a stronger mechanism linking parental history of childhood trauma and offspring adjustment than parental depressive symptoms (Narayan et al., 2021). Future research should examine a broad range of maternal distress and/or psychopathology when evaluating pathways of intergenerational transmission.
Conclusions
Findings from this study support the position that the psychological scars of childhood trauma may not be bound within a single generation. A comprehensive understanding of the intergenerational transmission of trauma necessitates consideration of the timing and mechanisms of such effects. Results of the present study support a model in which mothers with a history of childhood trauma experienced heightened depressive symptoms from the prenatal period through early toddlerhood; maternal depressive symptoms, in turn, were associated with offspring internalizing problems in later toddlerhood and early childhood. The effect of mothers’ early trauma to children’s internalizing at 36 months operated via a pathway of maternal depressive symptoms at 24 months. Awareness that maternal depression and its sequelae may have roots in women’s exposure to early adverse experiences is important for trauma-informed prevention and intervention efforts that support mothers during the transition to parenthood. Specifically, comprehensive models of care that support maternal mental health in concert with child mental health and parent-child relationship quality (e.g., Healthy Steps; Piotrowski, Talavera, & Mayer, 2009) are essential (yet underutilized) evidence-based models (Hagan et al., 2017). That said, meaningful improvements to population health will also necessitate socioeconomic and policy changes that redress the longstanding systemic inequities that contribute substantially to adverse exposures and their mental health sequelae.
Highlights.
Maternal childhood trauma was persistently associated with her depressive symptoms
Maternal depressive symptoms prospectively predicted children’s internalizing symptoms
Children’s internalizing symptoms did not predict subsequent maternal depression
Maternal depressive symptoms mediated the impact of maternal trauma on internalizing
Childhood trauma may exert a two-generation impact on caregivers and their children
Acknowledgements:
The CANDLE study data used in this paper was funded by the Urban Child Institute and the NIH (R01 HL109977). We are grateful for the participation of families enrolled in the CANDLE cohort, as well as the dedication of CANDLE research staff and investigators. Some coauthors on this paper received support from the ECHO PATHWAYS consortium, funded by the NIH (grants 1UG3OD023271-01 and 4UH3OD023271-03). Dr. Bush is the Lisa and John Pritzker Distinguished Professor of Developmental and Behavioral Health and receives support from the Lisa Pritzker Foundation and the Tauber Family Foundation. Dr. Roubinov is supported by the National Institute of Mental Health (K23MH1137019).
Footnotes
Prior to running CLPM, we attempted to fit a random-intercept cross-lagged panel model (RI-CLPM) in accordance with prevailing recommendations.(Hamaker et al., 2015) All attempts were unsuccessful and led to model non-convergence due to negative variance components. Consultation with statistical experts advised a less complex model (i.e., CLPM; Personal communication with Linda Muthén, 2020)
References
- Achenbach TM, Rescorla LA, 2000. Manual for the ASEBA preschool forms and profiles. Burlington, VT: University of Vermont, Research center for children, youth, and families. [Google Scholar]
- Adgent MA, Elsayed‐Ali O, Gebretsadik T, Tylavsky FA, Kocak M, Cormier SA, … & Carroll KN (2019). Maternal childhood and lifetime traumatic life events and infant bronchiolitis. Paediatric and perinatal epidemiology, 33(4), 262–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad SI, Rudd KL, LeWinn KZ, Mason WA, Murphy L, Juarez PD, … & Bush NR (2021). Maternal childhood trauma and prenatal stressors are associated with child behavioral health. Journal of developmental origins of health and disease, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernard K, Dozier M, Bick J, Lewis‐Morrarty E, Lindhiem O, Carlson E, 2012. Enhancing Attachment Organization Among Maltreated Children: Results of a Randomized Clinical Trial. Child Development 83, 623–636. 10.1111/j.1467-8624.2011.01712.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowlby J, 2008. A Secure Base: Parent-Child Attachment and Healthy Human Development. Basic Books. [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Irwin JR, Wachtel K, Cicchetti DV, 2004. The Brief Infant-Toddler Social and Emotional Assessment: Screening for Social-Emotional Problems and Delays in Competence. Journal of Pediatric Psychology 29, 143–155. 10.1093/jpepsy/jsh017 [DOI] [PubMed] [Google Scholar]
- Browne DT, LeWinn KZ, May SS, Tylavsky F, & Bush NR (in press). Maternal Childhood Trauma, Psychopathology, and Child Adaptive Functioning: Pre- and Postnatal Programming. Pediatric Research. [DOI] [PubMed] [Google Scholar]
- Bush NR, Savitz J, Coccia M, Jones-Mason K, Adler N, Boyce WT, Laraia B, Epel E, 2021. Maternal Stress During Pregnancy Predicts Infant Infectious and Noninfectious Illness. The Journal of Pediatrics 228, 117–125.e2. 10.1016/j.jpeds.2020.08.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chilcoat HD, Breslau N, 1997. Does Psychiatric History Bias Mothers’ Reports? An Application of a New Analytic Approach. Journal of the American Academy of Child & Adolescent Psychiatry 36, 971–979. 10.1097/00004583-199707000-00020 [DOI] [PubMed] [Google Scholar]
- Choi KW, Houts R, Arseneault L, Pariante C, Sikkema KJ, Moffitt TE, 2019. Maternal Depression in the Intergenerational Transmission of Childhood Maltreatment and Psychological Sequelae: Testing Postpartum Effects in a Longitudinal Birth Cohort. Dev Psychopathol 31, 143–156. 10.1017/S0954579418000032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences, 2nd edition. Hillsdale, NJ: Erlbaum. [Google Scholar]
- Cooke JE, Racine N, Plamondon A, Tough S, Madigan S, 2019. Maternal adverse childhood experiences, attachment style, and mental health: Pathways of transmission to child behavior problems. Child abuse & neglect 93, 27–37. [DOI] [PubMed] [Google Scholar]
- Davis EP, Narayan AJ, 2020. Pregnancy as a period of risk, adaptation, and resilience for mothers and infants. Development and Psychopathology 32, 1625–1639. 10.1017/S0954579420001121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, & Fitzpatrick M (2004). The SCL-90-R, the Brief Symptom Inventory (BSI), and the BSI-18. In Maruish ME (Ed.), The use of psychological testing for treatment planning and outcomes assessment: Instruments for adults (pp. 1–41). Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Derogatis LR, Melisaratos N, 1983. The Brief Symptom Inventory: an introductory report. Psychological Medicine 13, 595–605. 10.1017/S0033291700048017 [DOI] [PubMed] [Google Scholar]
- Doi S, Fujiwara T, Isumi A, 2020. Association between maternal adverse childhood experiences and mental health problems in offspring: An intergenerational study. Development and Psychopathology 1–18. 10.1017/S0954579420000334 [DOI] [PubMed] [Google Scholar]
- Dora B, Baydar N, 2020. Transactional associations of maternal depressive symptoms with child externalizing behaviors are small after age 3. Development and Psychopathology 32, 293–308. 10.1017/S0954579419000075 [DOI] [PubMed] [Google Scholar]
- Fraiberg S, Adelson E, Shapiro V, 1975. Ghosts in the Nursery: A Psychoanalytic Approach to the Problems of Impaired Infant-Mother Relationships. Journal of the American Academy of Child Psychiatry 14, 387–421. 10.1016/S0002-7138(09)61442-4 [DOI] [PubMed] [Google Scholar]
- Glover V, 2011. Annual Research Review: Prenatal stress and the origins of psychopathology: an evolutionary perspective. Journal of Child Psychology and Psychiatry 52, 356–367. 10.1111/j.1469-7610.2011.02371.x [DOI] [PubMed] [Google Scholar]
- Glynn LM, Sandman CA, 2014. Evaluation of the Association Between Placental Corticotrophin-Releasing Hormone and Postpartum Depressive Symptoms. Psychosomatic Medicine 76, 355–362. 10.1097/PSY.0000000000000066 [DOI] [PubMed] [Google Scholar]
- Goodman SH, 2020. Intergenerational Transmission of Depression. Annual Review of Clinical Psychology 16, 213–238. [DOI] [PubMed] [Google Scholar]
- Graham JW, 2009. Missing Data Analysis: Making It Work in the Real World. Annual Review of Psychology 60, 549–576. 10.1146/annurev.psych.58.110405.085530 [DOI] [PubMed] [Google Scholar]
- Hagan MJ, Browne DT, Sulik M, Ippen CG, Bush N, Lieberman AF, 2017. Parent and Child Trauma Symptoms During Child–Parent Psychotherapy: A Prospective Cohort Study of Dyadic Change. Journal of Traumatic Stress 30, 690–697. 10.1002/jts.22240 [DOI] [PubMed] [Google Scholar]
- Halligan SL, Murray L, Martins C, Cooper PJ, 2007. Maternal depression and psychiatric outcomes in adolescent offspring: A 13-year longitudinal study. Journal of Affective Disorders 97, 145–154. 10.1016/j.jad.2006.06.010 [DOI] [PubMed] [Google Scholar]
- Hamaker EL, Kuiper RM, Grasman RPPP, 2015. A critique of the cross-lagged panel model. Psychological Methods 20, 102–116. 10.1037/a0038889 [DOI] [PubMed] [Google Scholar]
- Hanington L, Ramchandani P, Stein A, 2010. Parental depression and child temperament: Assessing child to parent effects in a longitudinal population study. Infant Behavior and Development 33, 88–95. 10.1016/j.infbeh.2009.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hay DF, Pawlby S, Waters CS, Sharp D, 2008. Antepartum and postpartum exposure to maternal depression: different effects on different adolescent outcomes. Journal of Child Psychology and Psychiatry 49, 1079–1088. 10.1111/j.1469-7610.2008.01959.x [DOI] [PubMed] [Google Scholar]
- Henrich J, Heine SJ, Norenzayan A, 2010. Most people are not WEIRD. Nature 466, 29–29. 10.1038/466029a [DOI] [PubMed] [Google Scholar]
- Herzog JI, Schmahl C, 2018. Adverse Childhood Experiences and the Consequences on Neurobiological, Psychosocial, and Somatic Conditions Across the Lifespan. Front. Psychiatry 9. 10.3389/fpsyt.2018.00420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howland MA, Sandman CA, Glynn LM, Crippen C, Davis EP, 2016. Fetal exposure to placental corticotropin-releasing hormone is associated with child self-reported internalizing symptoms. Psychoneuroendocrinology 67, 10–17. 10.1016/j.psyneuen.2016.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM, 1999. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal 6, 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, Jones L, Dunne MP, 2017. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet Public Health 2, e356–e366. 10.1016/S2468-2667(17)30118-4 [DOI] [PubMed] [Google Scholar]
- Jones CW, Esteves KC, Gray SA, Clarke TN, Callerame K, Theall KP, Drury SS, 2019. The transgenerational transmission of maternal adverse childhood experiences (ACEs): Insights from placental aging and infant autonomic nervous system reactivity. Psychoneuroendocrinology 106, 20–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubany ES, Leisen MB, Kaplan AS, Watson SB, Haynes SN, Owens JA, Burns K, 2000. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment 12, 210–224. 10.1037/1040-3590.12.2.210 [DOI] [PubMed] [Google Scholar]
- Letourneau N, Dewey D, Kaplan BJ, Ntanda H, Novick J, Thomas JC, Deane AJ, Leung B, Pon K, Giesbrecht GF, Team, the Ap.S., 2019. Intergenerational transmission of adverse childhood experiences via maternal depression and anxiety and moderation by child sex. Journal of Developmental Origins of Health and Disease 10, 88–99. 10.1017/S2040174418000648 [DOI] [PubMed] [Google Scholar]
- LeWinn KZ, Bush NR, Batra A, Tylavsky F, Rehkopf D, 2020. Identification of Modifiable Social and Behavioral Factors Associated With Childhood Cognitive Performance. JAMA Pediatrics 174, 1063–1072. 10.1001/jamapediatrics.2020.2904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorch SA, Enlow E, 2016. The role of social determinants in explaining racial/ethnic disparities in perinatal outcomes. Pediatric Research 79, 141–147. 10.1038/pr.2015.199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrick MT, Ford DC, Ports KA, Guinn AS, 2018. Prevalence of Adverse Childhood Experiences From the 2011–2014 Behavioral Risk Factor Surveillance System in 23 States. JAMA Pediatr 172, 1038. 10.1001/jamapediatrics.2018.2537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mersky JP, Choi C, Plummer Lee C, Janczewski CE, 2021. Disparities in adverse childhood experiences by race/ethnicity, gender, and economic status: Intersectional analysis of a nationally representative sample. Child Abuse & Neglect 117, 105066. 10.1016/j.chiabu.2021.105066 [DOI] [PubMed] [Google Scholar]
- Muthén LK & Muthén BO, 1998. Mplus User’s Guide. Eighth Edition. Muthén & Muthén, Los Angeles, CA. [Google Scholar]
- Naicker K, Wickham M, Colman I, 2012. Timing of First Exposure to Maternal Depression and Adolescent Emotional Disorder in a National Canadian Cohort. PLOS ONE 7, e33422. 10.1371/journal.pone.0033422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanni V, Uher R, Dr MU, Danese A, 2012. Childhood Maltreatment Predicts Unfavorable Course of Illness and Treatment Outcome in Depression: A Meta-Analysis. American Journal of Psychiatry 169, 1–11. 10.1176/appi.ajp.2011.11020335 [DOI] [PubMed] [Google Scholar]
- Narayan AJ, Lieberman AF, Masten AS, 2021. Intergenerational transmission and prevention of adverse childhood experiences (ACEs). Clinical Psychology Review 85, 101997. 10.1016/j.cpr.2021.101997 [DOI] [PubMed] [Google Scholar]
- Negriff S, Palmer Molina A, Hackman DA, 2020. Parental Exposure to Childhood Maltreatment and Offspring’s Mental Health: Investigating Pathways Through Parental Adversity and Offspring Exposure to Maltreatment. Child maltreatment 1077559520912342. [DOI] [PubMed] [Google Scholar]
- Paschall KW, Mastergeorge AM, 2016. A review of 25 years of research in bidirectionality in parent–child relationships: An examination of methodological approaches. International Journal of Behavioral Development 40, 442–451. [Google Scholar]
- Peirce JM, Burke CK, Stoller KB, Neufeld KJ, Brooner RK, 2009. Assessing Traumatic Event Exposure: Comparing the Traumatic Life Events Questionnaire to the Structured Clinical Interview for DSM-IV. Psychol Assess 21, 210–218. 10.1037/a0015578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piotrowski CC, Talavera GA, & Mayer JA (2009). Healthy Steps: a systematic review of a preventive practice-based model of pediatric care. Journal of Developmental & Behavioral Pediatrics, 30(1), 91–103. [DOI] [PubMed] [Google Scholar]
- Personal communication with Linda Muthén, 2020.
- Pilkay SR, Combs-Orme T, Tylavsky F, Bush N, Smith AK. 2020. Maternal trauma and fear history predict BDNF methylation and gene expression in newborns. PeerJ, 8, e8858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plant DT, Pawlby S, Pariante CM, Jones FW, 2018. When one childhood meets another – maternal childhood trauma and offspring child psychopathology: A systematic review. Clin Child Psychol Psychiatry 23, 483–500. 10.1177/1359104517742186 [DOI] [PubMed] [Google Scholar]
- Reuben A, Moffitt TE, Caspi A, Belsky DW, Harrington H, Schroeder F, Hogan S, Ramrakha S, Poulton R, Danese A, 2016. Lest we forget: comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. Journal of Child Psychology and Psychiatry 57, 1103–1112. 10.1111/jcpp.12621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts SO, Bareket-Shavit C, Dollins FA, Goldie PD, Mortenson E, 2020. Racial Inequality in Psychological Research: Trends of the Past and Recommendations for the Future. Perspect Psychol Sci 15, 1295–1309. 10.1177/1745691620927709 [DOI] [PubMed] [Google Scholar]
- Roubinov DS, Epel ES, Adler NE, Laraia BA, Bush NR, 2019. Transactions between maternal and child depressive symptoms emerge early in life. Journal of Clinical Child & Adolescent Psychology 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sameroff AJ, 2000. Developmental systems and psychopathology. Development and psychopathology 12, 297–312. [DOI] [PubMed] [Google Scholar]
- Slopen N, Roberts AL, LeWinn KZ, Bush NR, Rovnaghi CR, Tylavsky F, Anand KJS, 2018. Maternal experiences of trauma and hair cortisol in early childhood in a prospective cohort. Psychoneuroendocrinology 98, 168–176. 10.1016/j.psyneuen.2018.08.027 [DOI] [PubMed] [Google Scholar]
- Steine IM, LeWinn KZ, Lisha N, Tylavsky F, Smith R, Bowman M, Sathyanarayana S, Karr CJ, Smith AK, Kobor M, Bush NR, 2020. Maternal exposure to childhood traumatic events, but not multi-domain psychosocial stressors, predict placental corticotrophin releasing hormone across pregnancy. Soc Sci Med 266, 113461. 10.1016/j.socscimed.2020.113461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shih EW, Ahmad SI, Bush NR, Roubinov D, Tylavsky F, Graff C, … & LeWinn KZ (2021). A path model examination: maternal anxiety and parenting mediate the association between maternal adverse childhood experiences and children’s internalizing behaviors. Psychological Medicine, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Roberts AL, LeWinn KZ, Bush NR, Rovnaghi CR, Tylavsky F, & Anand KJ (2018). Maternal experiences of trauma and hair cortisol in early childhood in a prospective cohort. Psychoneuroendocrinology, 98, 168–176. [DOI] [PubMed] [Google Scholar]
- Steine IM, LeWinn KZ, Lisha N, Tylavsky F, Smith R, Bowman M, … & Bush NR (2020). Maternal exposure to childhood traumatic events, but not multi-domain psychosocial stressors, predict placental corticotrophin releasing hormone across pregnancy. Social Science & Medicine, 266, 113461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teicher MH, Samson JA, 2013. Childhood Maltreatment and Psychopathology: A Case for Ecophenotypic Variants as Clinically and Neurobiologically Distinct Subtypes. AJP 170, 1114–1133. 10.1176/appi.ajp.2013.12070957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoemmes F, MacKinnon DP, & Reiser MR (2010). Power analysis for complex mediational designs using Monte Carlo methods. Structural Equation Modeling, 17(3), 510–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbán R, Kun B, Farkas J, Paksi B, Kökönyei G, Unoka Z, … & Demetrovics Z (2014). Bifactor structural model of symptom checklists: SCL-90-R and Brief Symptom Inventory (BSI) in a non-clinical community sample. Psychiatry Research, 216(1), 146–154. [DOI] [PubMed] [Google Scholar]
- West SG, Taylor AB, & Wu W (2012). Model fit and model selection in structural equation modeling. Handbook of structural equation modeling, 1, 209–231. [Google Scholar]


