Abstract
Objectives
To assess the economic and mental health impacts of COVID-19 in the presence of previous exposure to flooding events.
Methods
Starting in April 2018, the Texas Flood Registry (TFR) invited residents to complete an online survey regarding their experiences with Hurricane Harvey and subsequent flooding events. Starting in April 2020, participants nationwide were invited to complete a brief online survey on their experiences during the pandemic. This study includes participants in the TFR (N = 20,754) and the COVID-19 Registry (N = 8568) through October 2020 (joint N = 2929).
Logistic regression and generalized estimating equations were used to examine the relationship between exposure to flooding events and the economic and mental health impacts of COVID-19.
Results
Among COVID-19 registrants, 21% experienced moderate to severe anxiety during the pandemic, and 7% and 12% of households had difficulty paying rent and bills, respectively. Approximately 17% of Black and 15% of Hispanic households had difficulty paying rent, compared to 5% of non-Hispanic white households. The odds of COVID-19 income loss are 1.20 (1.02, 1.40) times higher for those who previously had storm-related home damage compared to those who did not and 3.84 (3.25–4.55) times higher for those who experienced Harvey income loss compared to those who did not. For registrants for whom Harvey was a severe impact event, the odds of having more severe anxiety during the pandemic are 5.14 (4.02, 6.58) times higher than among registrants for whom Harvey was a no meaningful impact event.
Conclusions
Multiple crises can jointly and cumulatively shape health and wellbeing outcomes. This knowledge can help craft emergency preparation and intervention programs.
Keywords: Climate change, COVID-19, Mental health, Socioeconomic factors
1. Introduction
Climate change has increased the number and severity of extreme weather events in the United States and globally. Nationally, the annual average of billion-dollar weather and climate events has steadily increased from 3.1 events per year in the 1980s to 12.8 events per year in the 2010s. In 2021, 20 billion-dollar weather and climate disasters affected the United States (NOAA National Centers for Environmental Information, 2022). Southeast Texas is especially vulnerable to effects of climate change in the form of extreme storms and flooding events. In Texas, the number of billion-dollar flood disasters, including inland (non-tropical) flooding events, severe storms, and tropical cyclone events, increased from a total of 37 events between 1980 and 2009 to 51 events between 2010 and 2019 (NOAA National Centers for Environmental Information, 2022).
Many studies have linked flooding to adverse economic and health impacts (Harville et al., 2011, 2018; Jacobs and Harville, 2015; Lowe et al., 2016, 2019). Economic and social stressors that emerge in the aftermath of flooding events, including disaster-related income and property loss, and symptoms of stress and anxiety in the short-term post-disaster context, may worsen long-term mental health impacts (Stephenson et al., 2014; Bonanno et al., 2010; Cerdá et al., 2013; Lowe et al., 2013). Individuals affected by repeated flooding may cumulate stressors even before they are able to recover from a previous flooding event (Stephenson et al., 2014). Low-income and minority populations, as well as the elderly and those with pre-existing health conditions, are especially vulnerable to cumulating effects (Benevolenza and DeRigne, 2019).
In cohorts of US gulf coast residents in Mississippi and Louisiana, exposure to at least one hurricane (for example, Hurricane Katrina) led to exacerbation of mental health outcomes in a subsequent hurricane or disaster like the Deepwater Horizon oil spill (Covert et al., 2020). Additionally, residents exposed to both Hurricane Katrina and the Deepwater Horizon oil spill tended to experience worse mental and physical health outcomes compared to those who experienced just one or neither of the disasters. Cumulative or dose response effects in mental health were also observed in residents exposed to more than one storm. Outside of studies on multiple flood exposures, cumulative health effects have also been observed in persons exposed to multiple wildfires and persons exposed to traumatic events following the World Trade Center attack and collapse (Silveira et al., 2021; Fernandez et al., 2005; Caramanica et al., 2015). In the Houston Metropolitan Statistical Area, increasing frequency of hazard exposure, including exposure to extreme weather and explosions and chemical releases at industrial facilities, has been associated with declines in mental health (Sansom et al., 2022). The economic and mental health impacts of natural disasters also vary by duration, severity, and mode of onset (Bonanno et al., 2010; Yamori and Goltz, 2021). In a cohort of US Gulf Coast residents exposed to multiple disasters, risk of adverse mental health outcomes, including stress, anxiety, depression, and post-traumatic stress disorder (PTSD), increased with increasing duration and severity of the cumulative exposure (Hu et al., 2021). The current literature focuses on the effects of repeated exposure to large-scale disasters of sudden onset and short duration (identifiable beginning and end) which are characterized by acute impacts. Few studies have incorporated gradual-onset disasters which are slowly evolving, not constrained by time, and characterized by chronic impacts (Yamori and Goltz, 2021; Adepoju et al., 2021; Siegel et al., 2003; Schafer et al., 2021).
The COVID-19 pandemic is an ongoing, long-term disaster. Early studies on mental health impacts of the pandemic report increased symptoms of anxiety and depressive disorders in the first year and increased disruptions in mental health services (Jia et al., 2021; Vahratian et al., 2021; World Health Organization, 2022). Women, young adults, adults with less than high school education, individuals with pre-existing health conditions, and low-income and minority communities were disproportionately impacted (World Health Organization, 2022; Kearney et al., 2021; Panchal et al., 2021). Leveraging the infrastructure of a community registry launched in Southeast Texas in response to Hurricane Harvey during the year 2018, this study aims to understand whether previous flood-related stressors, controlling for socio-demographic factors, increase susceptibility and vulnerability to economic and mental health impacts during the COVID-19 pandemic. This investigation concentrates on the registry's focal geography: Southeast Texas.
2. Materials and methods
The Texas Flood Registry is the first of its kind registry to track the health and housing impacts of a natural disaster (Miranda et al., 2021). The TFR is a collaborative project led by Rice University, the Environmental Defense Fund, and the University of Notre Dame with input from local health and emergency management organizations in Texas. In the months after Hurricane Harvey made landfall, the TFR implemented a survey to collect health, location, and exposure information from residents of Harvey-impacted areas, capturing data on both short- and long-term effects of the storm. The underlying technical infrastructure of the registry was designed to flexibly adapt to any type of disaster allowing for the rapid deployment of surveys related to severe storms after Harvey, such as the May 2019 and Tropical Storm Imelda flooding events.
The emergence of COVID-19 presented a call to action to leverage technical resources from the TFR to help local health departments in their response efforts and interventions related to the global pandemic. Using the technical backbone of the TFR, the TFR team deployed the COVID-19 Registry, an ongoing data gathering and sharing platform designed to track the spread and impact of the COVID-19 pandemic over time and across geographies. For the COVID-19 Registry, participants completed a brief online survey of their experiences during the pandemic, including changes in their health, behavior, and economic status.
2.1. Survey methods
To deploy surveys, the registry's technical infrastructure organizes individual storms or events as separate modules in the database to allow for the easy addition of new modules and multiple surveys in a module. Survey respondents are recruited through email and social media marketing, media interviews, radio and television ads, community contacts, and Public Service Announcements that direct community members to the registry website. Prior to COVID-19, participants were also recruited using tablets or paper forms at in-person events and community centers, particularly to assist in the recruitment of residents who might not have access to personal computers or wireless connections.
New participants are directed to a survey selection page where they read explanatory information and consent to participate. They then select the weather event about which they would like to answer questions. Based on the participant's selection, the website populates a core survey with key questions on health, location, and exposures as a result of the weather event (Disaster Research Response (DR2) Resources Portal, 2021). Existing participants who agreed to be re-contacted and live in an affected area (determined using the address provided in their most recently completed storm survey), receive an email invitation to complete the new survey. Multiple surveys completed by a participant are linked by a user ID. We built on this infrastructure to deploy the COVID-19 Registry one month after the first known case of COVID-19 was reported in Texas (Texas Department of State Health Services, 2020).
The COVID-19 Registry implements a survey designed to supplement surveillance data collected by health departments and also captures data on the economic and mental health impacts of the pandemic as experienced by the general public. It was launched as a national registry on April 10, 2020 at registry. rice.edu/covid_19. Recruitment consisted of Facebook advertising in the Greater Houston area, TV and radio ads, and online referrals (email and social media marketing) from health departments and community partners. TFR registrants who agreed to be re-contacted also received an email link to complete the survey online. After giving informed consent, participants were asked questions regarding their experience since January 1, 2020 (the month when the first case of COVID-19 was confirmed in the United States) (Holshue et al., 2020). The survey consists of four sections: 1) symptoms and accessing health care; 2) exposures; 3) behaviors; and 4) economic and household impacts (Disaster Research Response (DR2) Resources Portal, 2022). The first section included questions on baseline health, COVID-19 related symptoms, and measures of anxiety. The exposures section asked questions about contact with confirmed COVID-19 cases and recent travel history. The third section (behaviors) focused on participation in exposure mitigation behaviors (e.g., masking, physical distancing). The fourth section (impacts) covered a variety of economic and household experiences such as loss of income. Follow-up surveys were launched in June 2020 to track changes in health outcomes, mitigation behaviors, and economic impacts over the duration of the pandemic. Respondents received an email every two weeks reminding them of the opportunity to complete the follow-up survey. The follow-up survey was configured so that respondents could login at any time to update their health or economic situation. A public summary dashboard is available (https://registry.rice.edu/covid19_dashboard). Data are stored on the Kinder Institute Urban Data Platform (https://www.kinderudp.org) servers that meet the requirements of the Health Insurance Portability and Accountability Act. This work was undertaken under the auspices of human subjects research protocols approved by the IRB at Rice University. If a researcher wishes to access registry data, they may apply through the Urban Data Platform provided they have IRB approval from their home institution.
2.2. Statistical methods
In this study, we examined the economic and mental health impacts of the COVID-19 pandemic in a group of respondents who lived in areas affected by Hurricane Harvey (and other flooding events in sensitivity analysis) – although they may or may not have personally experienced flooding. This analysis used TFR data collected between April 2018 and October 2020 and COVID-19 Registry data collected between April 2020 and October 2020. This analysis was restricted to registrants who lived in the impact zone of a major storm in Texas when the storm hit, as determined by a federal disaster declaration or local emergency notification and the address provided in their completed storm survey. The study includes 2929 respondents who completed both surveys. Registrants with missing responses to questions pertaining to the exposures or outcomes of interest or demographic characteristics were excluded from any analysis involving that data.
2.3. Exposures of interest
In this analysis, explanatory variables used to characterize exposure included home flooding, home damage, income loss due to Harvey, and the respondent's stress reaction to Hurricane Harvey. The Texas Flood Registry core survey includes questions on registrants' experiences during and after a storm, covering a variety of sections including their living environment, their physical and mental health, and an open-ended response question. Responses to questions on home flooding, home damage, and income loss due to Harvey were dichotomous yes/no responses. To measure distress associated with Hurricane Harvey, the survey used the Impact of Event Scale, a 15-item self-report questionnaire (Horowitz et al., 1979; Joseph, 2000). Respondents were asked how often, during the past week, they experienced symptoms of stress related to the storm event. Participants answered the questions using a 4-point frequency scale, ranging from 0 (Not at all) to 4 (Often). A total IES score was calculated using the sum of all items and categorized to represent increasing severity of impact, with cutoff points of 0–8 (No meaningful impact), 9–25 (Impact event), 26–43 (Powerful impact event), and 44–75 (Severe impact event).
2.4. Outcomes of interest
Outcomes of interest in this analysis included household income loss due to COVID-19, anxiety severity, and economic difficulties experienced due to the COVID-19 pandemic. Registrants were asked to indicate whether they or any member of their household lost incomes as a consequence of the COVID-19 pandemic using the answer choices 1) Yes, I have, 2) Yes, a member of my household has, 3) Yes, I have and a member of my household has, and 4) No. Household income loss was recoded as a dichotomous yes/no variable.
Anxiety severity was calculated from the Generalized Anxiety Disorder Scale (GAD-7). The GAD-7 is a 7-item self-report questionnaire (Lowe et al., 2008). Respondents were asked how often, during the last 2 weeks, they were bothered by symptoms of generalized anxiety disorder. Participants answered the questions using a 4-point scale, ranging from 0 (Not at all) to 4 (Nearly every day). A total GAD-7 score was calculated using the sum of all items, with scores of ≥5, ≥10, and ≥15 representing mild, moderate, and severe anxiety, respectively. The GAD-7 is clinically validated (Lowe et al., 2008). A cut point of 10 is consistent with GAD diagnoses made by mental health professionals using DSM-IV criteria (Spitzer et al., 2006).
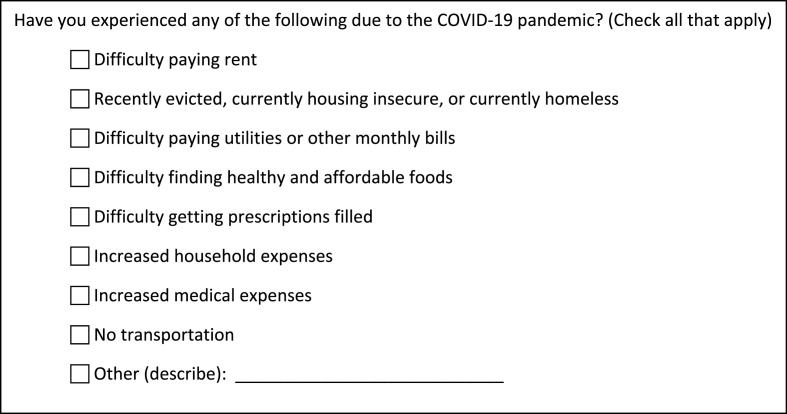
Economic difficulties due to COVID-19 were captured using a check-all-that-apply question format with nine items or answer choices (Fig. 1 ).
Fig. 1.
COVID-19 Registry question on economic difficulties due to the pandemic.
In the raw data, each item was formatted as a separate dichotomous variable. For registrants who selected at least one item, the selected items were coded as 1, and the unselected items were coded as 0. All variables were coded as missing if the registrant did not select any item.
2.5. Statistical models
Summary statistics were calculated for variables of interest. The relationship between COVID-19 income loss and exposure to Hurricane Harvey was examined using binomial logistic regression, while ordinal logistic regression was used to model anxiety severity. For the model
| (1) |
π denotes the probability of reporting COVID-19 income loss or higher anxiety severity. Thus, is the odds and the log odds ratio. All models were adjusted for individual-level age, education level, gender, and race/ethnicity (1). Modeling anxiety severity provided an opportunity to examine the potential cumulative effects of Hurricane Harvey and COVID-19, particularly the economic fallout, on mental health. In addition to fitting single exposure models for each Hurricane Harvey exposure, a single exposure model was fit with COVID-19 income loss as a predictor variable. Double exposure models were also constructed for each Harvey exposure with COVID-19 income loss.
For responses to the check-all-that-apply question on COVID-19 economic difficulties, generalized estimating equations (GEE) with logit link function, as suggested by Agresti and Liu, were used to examine the relationship between COVID-19 economic outcomes and experiences during Harvey (Agresti and Liu, 1999, 2001). An unstructured covariance structure was specified at the individual level to estimate the within-subject dependence among responses. For a respondent with exposure i, let πj|i denote the probability of responding “yes” on the jth item where i = 1, 0 and j = 1–8 (2).
| (2) |
This model permits different marginal probabilities for each combination of item j and i. Effects are constant across levels of demographic variables. This model includes an item indicator variable with a category for each answer choice to the check-all-that-apply question (Fig. 1). The item ‘recently evicted, currently housing insecure, or currently homeless’ was combined with ‘Other’ due to a small number of responses. ‘Difficulty paying rent’ was set as the reference category. Therefore, the model provides information on the probability that an item is selected more or less commonly than “difficulty paying rent.” The addition of an exposure of interest to the model provided information on how that exposure influences the probability that any economic difficulty is selected (or the response is 1). GEEs were fit with an interaction term between exposures of interest and the item indicator variable to determine the effect of each exposure on the selection of each economic difficulties item. QIC was used to assess goodness of fit for the GEEs. In a nested model comparison, model (2) had the lowest QIC.
Separate models were fit for each combination of COVID-19 outcome and storm-related exposure. As a result of data sparseness, models were not developed to examine the relationship between economic difficulties and distress related to Hurricane Harvey. All models were adjusted for individual-level age, education level, gender, and race/ethnicity. Although impacts of COVID-19 vary geographically, an exploratory analysis showed that adding a random intercept at the county level or fixed effects for county did not improve model fit, and the variance between counties in the data was found to be near zero. Odds ratios were generated from these models and are presented with 95% confidence intervals.
2.6. Sensitivity analysis
In addition to Hurricane Harvey, we collected data on exposures and impacts of the May 2019 storms, the first severe storms to impact the Greater Houston area after Hurricane Harvey, and Tropical Storm Imelda. All storm surveys in the Texas Flood Registry include yes-no questions on home flooding and income loss. Leveraging data available from all three storm surveys, we performed a sensitivity analysis to examine the relationship between COVID-19 related outcomes and exposure to any storm. The sensitivity analysis includes 2964 respondents who completed the core COVID-19 survey and at least one storm survey. We reran the logistic regression models and GEEs for COVID-19 related income loss, anxiety severity, and economic difficulties using home flooding and income loss due to any storm as explanatory variables for COVID-19 outcomes. Home flooding was defined as responding “yes” at least once across the three storm surveys. Income loss was similarly defined.
All analyses were conducted in SAS. The analysis code is available upon request. Follow-up data were not included as part of this study but can be found summarized on the public dashboard and on the Kinder Institute Urban Data Platform (https://www.kinderudp.org) servers.
3. Results
As of October 1, 2020, a total of 20,754 registrants have enrolled in the Texas Flood Registry and 8568 registrants have enrolled in the COVID-19 Registry.
Of the 20,754 registrants of the Texas Flood Registry, 15,093 are non-Hispanic white (72.7%), 3045 are Hispanic (14.7%), and 1662 are non-Hispanic Black (8.0%). TFR registrants are predominantly female (77.9%), which is common in voluntary registries. Age is relatively evenly distributed: 5914 (28.5%) registrants are 40 years older or younger, 9290 (44.8%) between 41 and 60 years old, and 5463 (26.3%) are 61 years or older.
Of the 8568 COVID-19 registrants, 6643 (77.5%) are non-Hispanic white, 1053 (12.3%) are Hispanic, and 388 (4.5%) are non-Hispanic Black. COVID-19 registrants are also predominantly female (75.1%). Age distribution is spread out evenly: 1862 registrants (21.6%) are 40 years old or younger, 5204 (39.0%) are between 41 and 60 years old, and 3364 (39.3%) are 61 years or older. Results from the GAD-7 items indicated 21% of registrants experienced moderate to severe anxiety.
Economically, 569 (7%) and 1040 (12%) of all COVID-19 registrants say their household has had difficulty paying rent or bills due to COVID-19, respectively. Broken down by race (Table 1 ), approximately 17% of Black households and 15% of Hispanic households say they have difficulty paying their rent, compared to 5% of non-Hispanic white households. Similarly, 28% of Black households and 23% of Hispanic households say they are having difficulty paying bills, compared to 9% of non-Hispanic white households.
Table 1.
Select economic impacts by race/ethnicity of COVID-19 registrants: April 10, 2020 – October 1, 2020.
| Registry N (%) | Non-Hispanic White N (%) | Non-Hispanic Black N (%) | Hispanic N (%) | |
|---|---|---|---|---|
| Total Population | 8568 | 6643 | 388 | 1053 |
| Economic Impact | ||||
| Difficulty paying rent | 569 (7) | 312 (5) | 67 (17) | 157 (15) |
| Difficulty paying bills | 1040 (12) | 628 (9) | 108 (28) | 238 (23) |
| Difficulty finding food | 1524 (18) | 1132 (17) | 85 (22) | 210 (20) |
| Difficulty getting prescriptions filled | 535 (6) | 407 (6) | 34 (9) | 64 (6) |
| Increased household expenses | 2101 (25) | 1438 (22) | 152 (39) | 379 (36) |
| Increased medical expenses | 409 (5) | 283 (4) | 28 (7) | 71 (7) |
| No transportation | 137 (2) | 85 (1) | 17 (4) | 27 (3) |
| Lost health insurance | 120 (1) | 73 (1) | 14 (4) | 26 (2) |
| Difficulty buying household supplies | 2335 (27) | 1742 (26) | 143 (37) | 320 (30) |
| Other | 345 (4) | 265 (4) | 10 (3) | 48 (5) |
A total of 2929 respondents completed both the Hurricane Harvey and COVID-19 core surveys. Compared to respondents in the COVID-19 Registry as a whole, respondents completing both surveys were more likely to be non-Hispanic white (81.8%) and between 41 and 60 years old (42.9%). 75.9% of respondents completing both surveys were female, which is comparable to the overall gender distribution of the COVID-19 Registry. Among joint respondents, 1182 (40.4%) reported home flooding due to Harvey, 1525 (54.1%) reported home damage, and 1037 (35.4%) reported income loss due to Harvey. Responses to the Impact of Event Scale questionnaire indicate that for 441 (18.3%) respondents, Hurricane Harvey was a severe impact event.
Results of the binomial logistic regression predicting household income loss due to COVID-19 are shown in Table 2 .
Table 2.
COVID-19 income loss by Hurricane Harvey exposure.
| Exposure model | OR (95% CI) | p-value |
|---|---|---|
| Flooding due to Harvey (N = 2897) | ||
| Home flooded | 1.10 (0.94, 1.28) | 0.2515 |
| Home not flooded | Ref | |
| Gender | ||
| Male | 0.95 (0.79, 1.14) | 0.5777 |
| Female | Ref | |
| Race/ethnicity | ||
| Non-Hispanic Other | 1.72 (1.02, 2.93) | 0.0097 |
| Non-Hispanic Asian | 1.40 (0.80, 2.46) | |
| Hispanic | 1.38 (1.06, 1.80) | |
| Non-Hispanic Black | 1.44 (1.01, 2.05) | |
| Non-Hispanic White | Ref | |
| Education group | ||
| High school graduate or less | 1.66 (1.21, 2.28) | <.0001 |
| Some college or associates | 1.44 (1.22, 1.71) | |
| Bachelors or higher | Ref | |
| Age group | ||
| 61+ | 0.49 (0.40, 0.61) | <.0001 |
| 41–60 | 0.97 (0.79, 1.20) | |
| 18–40 | Ref | |
| Damage due to Harvey (N = 2790) | ||
| Home damaged | 1.20 (1.02, 1.40) | 0.0260 |
| Home not damaged | Ref | |
| Gender | ||
| Male | 0.95 (0.79, 1.14) | 0.5587 |
| Female | Ref | |
| Race/ethnicity | ||
| Non-Hispanic Other | 1.83 (1.06, 3.15) | 0.0097 |
| Non-Hispanic Asian | 1.34 (0.75, 2.39) | |
| Hispanic | 1.39 (1.07, 1.81) | |
| Non-Hispanic Black | 1.43 (0.99, 2.06) | |
| Non-Hispanic White | Ref | |
| Education group | ||
| High school graduate or less | 1.63 (1.18, 2.24) | <.0001 |
| Some college or associates | 1.42 (1.19, 1.69) | |
| Bachelors or higher | Ref | |
| Age group | ||
| 61+ | 0.48 (0.38, 0.59) | <.0001 |
| 41–60 | 0.96 (0.77, 1.19) | |
| 18–40 | Ref | |
| Income loss due to Harvey (N = 2897) | ||
| Income lost | 3.84 (3.25, 4.55) | <.0001 |
| No income lost | Ref | |
| Gender | ||
| Male | 1.06 (0.87, 1.27) | 0.5723 |
| Female | Ref | |
| Race/ethnicity | ||
| Non-Hispanic Other | 1.48 (0.85, 2.57) | 0.3878 |
| Non-Hispanic Asian | 1.28 (0.71, 2.31) | |
| Hispanic | 1.17 (0.88, 1.54) | |
| Non-Hispanic Black | 1.20 (0.83, 1.74) | |
| Non-Hispanic White | Ref | |
| Education group | ||
| High school graduate or less | 1.29 (0.92, 1.80) | 0.1207 |
| Some college or associates | 1.17 (0.97, 1.40) | |
| Bachelors or higher | Ref | |
| Age group | ||
| 61+ | 0.55 (0.43, 0.69) | <.0001 |
| 41–60 | 0.95 (0.76, 1.18) | |
| 18–40 | Ref | |
| Impact of Event Scale (N = 2391) | ||
| Severe Impact Event | 1.78 (1.38, 2.30) | <.0001 |
| Powerful Impact Event | 1.37 (1.09, 1.73) | |
| Impact Event | 1.09 (0.87, 1.36) | |
| No Meaningful Impact | Ref | |
| Gender | ||
| Male | 1.02 (0.83, 1.25) | 0.8650 |
| Female | Ref | |
| Race/ethnicity | ||
| Non-Hispanic Other | 1.79 (0.98, 3.28) | 0.1417 |
| Non-Hispanic Asian | 1.13 (0.60, 2.12) | |
| Hispanic | 1.32 (0.99, 1.76) | |
| Non-Hispanic Black | 1.15 (0.77, 1.71) | |
| Non-Hispanic White | Ref | |
| Education group | ||
| High school graduate or less | 1.49 (1.05, 2.10) | 0.0004 |
| Some college or associates | 1.43 (1.18, 1.73) | |
| Bachelors or higher | Ref | |
| Age group | ||
| 61+ | 0.47 (0.37, 0.60) | <.0001 |
| 41–60 | 0.97 (0.77, 1.22) | |
| 18–40 | Ref |
In models adjusted for age, education level, gender, and race/ethnicity, home damage and income loss due to Harvey are significant predictors of COVID-19 income loss but not home flooding due to Harvey (OR 1.10 (0.94–1.28), p = 0.25). The odds of COVID-19 income loss are 1.20 (1.02, 1.40) for those who had home damage due to Harvey compared to those who did not. The effect size is greater for income loss due to Harvey. The odds of COVID-19 income loss are 3.84 (3.25, 4.55) for those who lost income due to Harvey compared to those who did not. An increasing probability of COVID-19 income loss is also observed with increasing severity of distress or stress reaction related to Hurricane Harvey. For registrants for whom Harvey was a severe impact event, the odds of COVID-19 income loss are 1.78 (1.38, 2.30) times higher than among registrants for whom Harvey was a no meaningful impact event. In the models with home flooding and damage due to Harvey as the exposures of interest, respondents who were non-white, younger or had lower educational attainment had significantly greater odds of COVID-19 income loss. The effects of age and education level were sustained in the model with Harvey-related distress as the exposure of interest but not in the model with income loss due to Harvey, where only the effect of age was significant.
The results of the ordinal logistic regression showing the odds of higher severity of anxiety show a similar trend (Table 3 ).
Table 3.
Odds of higher anxiety severity during the COVID-19 pandemic by Hurricane Harvey exposure.
| Exposure model | Single exposure |
Double exposure |
||
|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Flooding due to Harvey (N = 2760) | ||||
| Home flooded | 1.15 (0.99, 1.33) | 0.0662 | 1.14 (0.98, 1.32) | 0.0812 |
| Home not flooded | Ref | Ref | ||
| COVID-19 income loss | ||||
| Income lost | – | – | 1.72 (1.49, 2.00) | <.0001 |
| No income lost | – | Ref | ||
| Gender | ||||
| Male | 0.45 (0.38, 0.54) | <.0001 | 0.45 (0.38, 0.54) | <.0001 |
| Female | Ref | Ref | ||
| Race/ethnicity | ||||
| Non-Hispanic Other | 1.13 (0.69, 1.85) | 0.8988 | 1.06 (0.65, 1.75) | 0.8310 |
| Non-Hispanic Asian | 0.87 (0.51, 1.48) | 0.84 (0.49, 1.43) | ||
| Hispanic | 1.02 (0.80, 1.31) | 0.98 (0.76, 1.25) | ||
| Non-Hispanic Black | 0.88 (0.63, 1.24) | 0.84 (0.60, 1.18) | ||
| Non-Hispanic White | Ref | Ref | ||
| Education group | ||||
| High school graduate or less | 1.28 (0.96, 1.72) | 0.0411 | 1.21 (0.90, 1.63) | 0.1728 |
| Some college or associates | 1.20 (1.02, 1.42) | 1.14 (0.97, 1.35) | ||
| Bachelors or higher | Ref | Ref | ||
| Age group | ||||
| 61+ | 0.29 (0.23, 0.35) | <.0001 | 0.31 (0.25, 0.38) | <.0001 |
| 41-60 | 0.68 (0.56, 0.82) | 0.67 (0.55, 0.81) | ||
| 18-40 | Ref | Ref | ||
| Damage due to Harvey (N = 2660) | ||||
| Home damaged | 1.22 (1.05, 1.41) | 0.0098 | 1.20 (1.03, 1.39) | 0.0188 |
| Home not damaged | Ref | Ref | ||
| COVID-19 income loss | ||||
| Income lost | – | – | 1.66 (1.43, 1.93) | <.0001 |
| No income lost | – | Ref | ||
| Gender | ||||
| Male | 0.45 (0.38, 0.55) | <.0001 | 0.46 (0.38, 0.55) | <.0001 |
| Female | Ref | Ref | ||
| Race/ethnicity | ||||
| Non-Hispanic Other | 1.12 (0.67, 1.85) | 0.9569 | 1.05 (0.63, 1.74) | 0.9493 |
| Non-Hispanic Asian | 0.91 (0.53, 1.58) | 0.89 (0.51, 1.54) | ||
| Hispanic | 1.05 (0.82, 1.34) | 1.00 (0.78, 1.28) | ||
| Non-Hispanic Black | 0.93 (0.65, 1.31) | 0.88 (0.62, 1.25) | ||
| Non-Hispanic White | Ref | Ref | ||
| Education group | ||||
| High school graduate or less | 1.26 (0.94, 1.69) | 0.0447 | 1.20 (0.89, 1.61) | 0.1591 |
| Some college or associates | 1.21 (1.02, 1.43) | 1.16 (0.98, 1.37) | ||
| Bachelors or higher | Ref | Ref | ||
| Age group | ||||
| 61+ | 0.29 (0.23, 0.36) | <.0001 | 0.31 (0.25, 0.38) | <.0001 |
| 41-60 | 0.67 (0.55, 0.82) | 0.66 (0.54, 0.81) | ||
| 18-40 | Ref | Ref | ||
| Income loss due to Harvey (N = 2760) | ||||
| Income lost | 1.60 (1.37, 1.87) | <.0001 | 1.39 (1.18, 1.63) | <.0001 |
| No income lost | Ref | Ref | ||
| COVID-19 income loss | ||||
| Income lost | – | – | 1.58 (1.36, 1.85) | <.0001 |
| No income lost | – | Ref | ||
| Gender | ||||
| Male | 0.46 (0.38, 0.55) | <.0001 | 0.46 (0.38, 0.55) | <.0001 |
| Female | Ref | Ref | ||
| Race/ethnicity | ||||
| Non-Hispanic Other | 1.05 (0.64, 1.73) | 0.8179 | 1.02 (0.62, 1.68) | 0.7585 |
| Non-Hispanic Asian | 0.84 (0.49, 1.43) | 0.83 (0.48, 1.41) | ||
| Hispanic | 0.96 (0.75, 1.23) | 0.94 (0.74, 1.21) | ||
| Non-Hispanic Black | 0.83 (0.59, 1.17) | 0.82 (0.58, 1.15) | ||
| Non-Hispanic White | Ref | Ref | ||
| Education group | ||||
| High school graduate or less | 1.18 (0.88, 1.59) | 0.2936 | 1.17 (0.87, 1.57) | 0.3937 |
| Some college or associates | 1.12 (0.94, 1.32) | 1.10 (0.93, 1.30) | ||
| Bachelors or higher | Ref | |||
| Age group | ||||
| 61+ | 0.30 (0.25, 0.38) | <.0001 | 0.32 (0.26, 0.39) | <.0001 |
| 41-60 | 0.67 (0.55, 0.82) | 0.67 (0.55, 0.81) | ||
| 18-40 | Ref | Ref | ||
| Impact of Event Scale (N = 2288) | ||||
| Severe Impact Event | 5.14 (4.02, 6.58) | <.0001 | 4.95 (3.87, 6.34) | <.0001 |
| Powerful Impact Event | 2.55 (2.04, 3.19) | 2.49 (1.99, 3.12) | ||
| Impact Event | 1.55 (1.25, 1.93) | 1.55 (1.25, 1.92) | ||
| No Meaningful Impact | Ref | Ref | ||
| COVID-19 income loss | ||||
| Income lost | – | – | 1.45 (1.23, 1.70) | <.0001 |
| No income lost | – | Ref | ||
| Gender | ||||
| Male | 0.53 (0.43, 0.64) | <.0001 | 0.53 (0.43, 0.64) | <.0001 |
| Female | Ref | Ref | ||
| Race/ethnicity | ||||
| Non-Hispanic Other | 0.99 (0.57, 1.74) | 0.3062 | 0.94 (0.53, 1.64) | 0.2678 |
| Non-Hispanic Asian | 0.71 (0.39, 1.30) | 0.70 (0.38, 1.28) | ||
| Hispanic | 0.97 (0.74, 1.27) | 0.94 (0.72, 1.23) | ||
| Non-Hispanic Black | 0.68 (0.46, 1.01) | 0.67 (0.46, 0.99) | ||
| Non-Hispanic White | Ref | Ref | ||
| Education group | ||||
| High school graduate or less | 0.93 (0.68, 1.28) | 0.9024 | 0.90 (0.65, 1.24) | 0.7923 |
| Some college or associates | 1.00 (0.83, 1.20) | 0.97 (0.81, 1.17) | ||
| Bachelors or higher | Ref | Ref | ||
| Age group | ||||
| 61+ | 0.26 (0.21, 0.33) | <.0001 | 0.28 (0.22, 0.35) | <.0001 |
| 41-60 | 0.60 (0.49, 0.75) | 0.60 (0.48, 0.74) | ||
| 18-40 | Ref | Ref | ||
In models adjusted for age, education level, gender, and race/ethnicity, home damage and income loss due to Harvey are significant predictors of having more severe anxiety related to COVID-19. The odds of having higher anxiety related to COVID-19 is 1.22 (1.05, 1.41) for respondents who had home damage compared to those who did not. The odds of higher anxiety are 1.60 (1.37, 1.87) times greater for those who lost income due to Harvey compared to those who did not. Additionally, the odds of having higher anxiety increases in a dose response manner as severity of stress reaction to Harvey increases. For registrants for whom Harvey was a severe impact event, the odds of having more severe anxiety are 5.14 (4.02, 6.58) times higher than among registrants for whom Harvey was a no meaningful impact event. This effect is also observed when comparing respondents whose homes flooded to those who did not and trends toward significance (OR 1.15 (0.99, 1.33), p = 0.07). The significant effects observed in the single exposure models were sustained when COVID-19 income loss was added as a confounder (Table 3). When the effect of COVID-19 income loss on anxiety severity is examined alone, the odds of having higher anxiety are 1.73 (1.49, 2.01). In the double exposure models, COVID-19 income loss continues to be a significant predictor. The effect size of COVID-19 income loss decreases when added to models for Harvey-related income loss and distress but remains stable when added to models for home flooding and damage due to Harvey. These results suggest a cumulative effect of more severe anxiety in the doubly exposed group. Lower educational attainment is a significant predictor of higher anxiety severity in the single exposure models for home flooding and damage due to Harvey but not in the other models. In all single and double exposure models, both male gender and older age have a significant protective effect on the odds of experiencing anxiety severity.
The results of the GEE analysis show a significant positive effect for Harvey-related impacts (Table 4 ).
Table 4.
Economic difficulty during the COVID-19 pandemic by Hurricane Harvey exposure.
| Exposure model | OR (95% CI) | p-value |
|---|---|---|
| Flooding due to Harvey (N = 1620) | ||
| COVID-19 economic difficulty x Flooding due to Harvey | ||
| Difficulty paying rent by flooding due to Harvey | ||
| Home flooded | 2.04 (1.52, 2.73) | <.0001 |
| Home not flooded | Ref | |
| COVID-19 economic difficultyamong respondents who did not experience home flooding | ||
| Difficulty filling prescriptions, Home not flooded | 1.54 (1.16, 2.04) | <.0001 |
| Difficulty finding food, Home not flooded | 6.02 (4.68, 7.75) | |
| Difficulty paying bills, Home not flooded | 2.52 (2.07, 3.07) | |
| Increased household expenses, Home not flooded | 9.46 (7.34, 12.20) | |
| Increased medical expenses, Home not flooded | 1.02 (0.75, 1.38) | |
| No transportation, Home not flooded | 0.30 (0.20, 0.46) | |
| Other, Home not flooded | 1.02 (0.74, 1.41) | |
| Difficulty paying rent, Home not flooded | Ref | |
| COVID-19 economic difficultyamong respondents who experienced home flooding | ||
| Difficulty filling prescriptions, Home flooded | 0.67 (0.34, 1.34) | <.0001 |
| Difficulty finding food, Home flooded | 2.63 (1.44, 4.80) | |
| Difficulty paying bills, Home flooded | 2.33 (1.47, 3.67) | |
| Increased household expenses, Home flooded | 4.84 (2.64, 8.87) | |
| Increased medical expenses, Home flooded | 0.54 (0.26, 1.10) | |
| No transportation, Home flooded | 0.20 (0.07, 0.55) | |
| Other, Home flooded | 0.48 (0.22, 1.05) | |
| Difficulty paying rent, Home flooded | Ref | |
| Gender | ||
| Male | 0.98 (0.86, 1.12) | 0.7821 |
| Female | Ref | |
| Race/ethnicity | ||
| Non-Hispanic Other | 1.39 (1.05, 1.84) | 0.0073 |
| Non-Hispanic Asian | 1.26 (0.85, 1.86) | |
| Hispanic | 1.21 (1.03, 1.43) | |
| Non-Hispanic Black | 1.35 (1.09, 1.67) | |
| Non-Hispanic White | Ref | |
| Education group | ||
| High school graduate or less | 1.72 (1.41, 2.10) | <.0001 |
| Some college or associates | 1.43 (1.28, 1.61) | |
| Bachelors or higher | Ref | |
| Age group | ||
| 61+ | 0.68 (0.59, 0.79) | <.0001 |
| 41–60 | 0.94 (0.83, 1.08) | |
| 18–40 | Ref | |
| Damage due to Harvey (N = 1620) | ||
| COVID-19 economic difficulty x Damage due to Harvey | ||
| Difficulty paying rent by damage due to Harvey | ||
| Home damaged | 2.12 (1.53, 2.93) | <.0001 |
| Home not damaged | Ref | |
| COVID-19 economic difficultyamong respondents who did not experience home damage | ||
| Difficulty filling prescriptions, Home not damaged | 1.54 (1.08, 2.20) | <.0001 |
| Difficulty finding food, Home not damaged | 6.59 (4.80, 9.06) | |
| Difficulty paying bills, Home not damaged | 2.54 (1.99, 3.24) | |
| Increased household expenses, Home not damaged | 9.81 (7.12, 13.50) | |
| Increased medical expenses, Home not damaged | 0.92 (0.63, 1.36) | |
| No transportation, Home not damaged | 0.26 (0.15, 0.46) | |
| Other, Home not damaged | 1.00 (0.66, 1.52) | |
| Difficulty paying rent, Home not damaged | Ref | |
| COVID-19 economic difficulty among respondents who experienced home damage | ||
| Difficulty filling prescriptions, Home damaged | 0.81 (0.37, 1.77) | 0.0009 |
| Difficulty finding food, Home damaged | 3.03 (1.51, 6.10) | |
| Difficulty paying bills, Home damaged | 2.32 (1.36, 3.94) | |
| Increased household expenses, Home damaged | 5.53 (2.73, 11.18) | |
| Increased medical expenses, Home damaged | 0.63 (0.27, 1.48) | |
| No transportation, Home damaged | 0.23 (0.07, 0.78) | |
| Other, Home damaged | 0.56 (0.22, 1.39) | |
| Difficulty paying rent, Home damaged | Ref | |
| Gender | ||
| Male | 0.99 (0.87, 1.13) | 0.8671 |
| Female | Ref | |
| Race/ethnicity | ||
| Non-Hispanic Other | 1.38 (1.05, 1.81) | 0.0101 |
| Non-Hispanic Asian | 1.37 (0.92, 2.03) | |
| Hispanic | 1.18 (1.01, 1.39) | |
| Non-Hispanic Black | 1.35 (1.08, 1.69) | |
| Non-Hispanic White | Ref | |
| Education group | ||
| High school graduate or less | 1.69 (1.38, 2.07) | <.0001 |
| Some college or associates | 1.42 (1.26, 1.60) | |
| Bachelors or higher | Ref | |
| Age group | ||
| 61+ | 0.68 (0.59, 0.79) | <.0001 |
| 41–60 | 0.94 (0.82, 1.08) | |
| 18–40 | Ref | |
| Income loss due to Harvey (N = 1620) | ||
| COVID-19 economic difficulty x Income loss due to Harvey | ||
| Difficulty paying rent by income loss due to Harvey | ||
| Income lost | 5.72 (3.99, 8.21) | <.0001 |
| No income lost | Ref | |
| COVID-19 economic difficulty among respondents who did not experience income loss | ||
| Difficulty filling prescriptions, No income lost | 2.93 (2.01, 4.26) | <.0001 |
| Difficulty finding food, No income lost | 11.31 (8.06,15.87) | |
| Difficulty paying bills, No income lost | 3.28 (2.45, 4.38) | |
| Increased household expenses, No income lost | 16.73 (11.95, 23.43) | |
| Increased medical expenses, No income lost | 1.40 (0.93, 2.11) | |
| No transportation, No income lost | 0.45 (0.26, 0.79) | |
| Other, No income lost | 2.41 (1.65, 3.52) | |
| Difficulty paying rent, No income lost | Ref | |
| COVID-19 economic difficulty among respondents who experienced income loss | ||
| Difficulty filling prescriptions, Income lost | 0.55 (0.24, 1.26) | <.0001 |
| Difficulty finding food, Income lost | 2.18 (1.04, 4.58) | |
| Difficulty paying bills, Income lost | 2.31 (1.25, 4.29) | |
| Increased household expenses, Income lost | 4.22 (2.01, 8.88) | |
| Increased medical expenses, Income lost | 0.54 (0.22, 1.33) | |
| No transportation, Income lost | 0.18 (0.05, 0.60) | |
| Other, Income lost | 0.30 (0.12, 0.72) | |
| Difficulty paying rent, Income lost | Ref | |
| Gender | ||
| Male | 0.99 (0.87, 1.13) | 0.8654 |
| Female | Ref | |
| Race/ethnicity | ||
| Non-Hispanic Other | 1.29 (0.97, 1.71) | 0.0305 |
| Non-Hispanic Asian | 1.26 (0.85, 1.86) | |
| Hispanic | 1.17 (1.00, 1.38) | |
| Non-Hispanic Black | 1.32 (1.06, 1.63) | |
| Non-Hispanic White | Ref | |
| Education group | ||
| High school graduate or less | 1.64 (1.35, 2.00) | <.0001 |
| Some college or associates | 1.34 (1.19, 1.52) | |
| Bachelors or higher | Ref | |
| Age group | ||
| 61+ | 0.74 (0.63, 0.85) | <.0001 |
| 41–60 | 0.95 (0.83, 1.08) | |
| 18–40 | Ref |
Home flooding, home damage, and income loss due to Harvey increase the odds that difficulty paying rent due to the COVID-19 pandemic is reported. Furthermore, interaction terms were significant for home flooding, home damage, and income loss due to Harvey, suggesting Harvey-related impacts differentially influence the probability that a specific economic difficulty due to the COVID-19 pandemic is selected (p < 0.001). In models adjusting for age, education level, gender and race/ethnicity, the odds of difficulty paying rent due to the COVID-19 pandemic are 2.04 (1.52, 2.73) times greater for respondents who experienced home flooding compared to those who did not. Among respondents who did not experience home flooding due to Harvey, the odds of reporting difficulty filling prescriptions (OR 1.54 (1.16, 2.04)), difficulty finding food (OR 6.02 (4.68, 7.75)), difficulty paying bills (OR 2.52 (2.07, 3.07)), and increased household expenses (OR 9.46 (7.34, 12.20)) in comparison to difficulty paying rent were significantly greater. Among respondents who experienced home flooding, odds of reporting difficulty finding food (OR 2.63 (1.44, 4.80)), difficulty paying bills (OR 2.33 (1.47, 3.67)), and increased household expenses (OR 4.84 (2.64, 8.87)) in comparison to difficulty paying rent remained significantly greater but with smaller effect size. The odds of reporting difficulty filling prescriptions (OR 0.67 (0.34, 1.34)), increased medical expenses (OR 0.54 (0.26, 1.10)), and other economic difficulties (OR 0.48 (0.22, 1.05)) in comparison to difficulty paying rent were lower but not significantly different. The odds of reporting no transportation in comparison to difficulty paying rent remained significantly lower (OR 0.20 (0.07, 0.55)).
Similarly, the odds of difficulty paying rent due to the pandemic are 2.12 (1.53, 2.93) times greater for respondents who had home damage compared to those who did not. Among respondents who did not experience home damage due to Harvey, the odds of reporting difficulty filling prescriptions (OR 1.54 (1.08, 2.20)), difficulty finding food (OR 6.59 (4.80, 9.06)), difficulty pay bills (OR 2.54 (1.99, 3.24)), and increased household expenses (OR 9.81 (7.12, 13.50)) in comparison to difficulty paying rent were significantly greater. Additionally, there was no significant difference in the odds of reporting increased medical expenses (OR 0.92 (0.63, 1.36)) and other economic difficulties (OR 1.00 (0.66, 1.52)) in comparison to difficulty paying rent. The odds of reporting no transportation in comparison to difficulty paying rent were 0.23 (0.07, 0.78) times lower. Among respondents who experienced home damage, odds of difficulty finding food (OR 3.03 (1.51, 6.10)), difficulty paying bills (OR (2.32 (1.36, 3.94)), and increased household expenses (OR 5.53 (2.73, 11.18)) remained significantly greater but with smaller effect size. The odds of reporting difficulty filling prescriptions (OR 0.81 (0.37, 1.77)), increased medical expenses (OR 0.63 (0.27, 1.48)), and other economic difficulties (OR 0.56 (0.22, 1.39)) in comparison to difficulty paying rent were lower but not significantly different. The odds of reporting no transportation in comparison to difficulty paying rent remained significantly lower (OR 0.23 (0.07, 0.78)).
The odds of experiencing difficulty paying rent due to the COVID-19 pandemic are more than five times greater (OR 5.72 (3.99, 8.21)) for those who lost income to due Harvey compared to those who did not. Among respondents who did not experience income loss due to Harvey, respondents were significantly more likely to report difficulty filling prescriptions (OR 2.93 (2.01, 4.26)), difficulty finding food (OR 11.31 (8.06, 15.87)), difficulty pay bills (OR 3.28 (2.45, 4.38)), increased household expenses (OR 16.73 (11.95, 23.43)), and other economic difficulties (2.41 (1.65, 3.52)) in comparison to difficulty paying rent. The odds of reporting increased medical expenses in comparison to difficulty paying rent were greater but not significant (OR 1.40 (0.93, 2.11)). The odds of reporting no transportation in comparison to difficulty paying rent were 0.45 (0.26, 0.79) times lower. Among respondents who experienced income loss, odds of difficulty finding food (OR 2.18 (1.04, 4.58)), difficulty paying bills (OR (2.31 (1.25, 4.29)), and increased household expenses (OR 4.22 (2.01, 8.88)) in comparison to difficulty paying rent remained significantly greater but with smaller effect size. The odds of reporting difficulty filling prescriptions (OR 0.55 (0.24, 1.26)) and increased medical expenses (OR 0.54 (0.22, 1.33)) in comparison to difficulty paying rent were lower but not significantly different. The odds of reporting no transportation (OR 0.18 (0.05, 0.60)) and other economic difficulties (OR 0.30 (0.12, 0.72)) in comparison to difficulty paying rent were significantly lower. Across all models, non-white respondents and respondents who had lower educational attainment had increased odds of reporting any economic difficulty. Older age had a significant protective effect on the odds of reporting any economic difficulty.
For the sensitivity analysis, a total of 2964 respondents completed the core COVID-19 survey and at least one storm survey. Results show the odds of COVID-19 income loss are 1.11 (0.95, 1.30) times higher for those who experienced home flooding due to any storm (p = 0.18) (Supplementary Table 1). In comparison to the effect of home flooding due to Harvey alone (p = 0.25), the effect trends more towards significance. When examining the relationship between COVID-19 income loss and income loss due to any storm, adding data from the other storms maintained the effects observed when looking at Harvey alone. The odds of COVID-19 income loss are 3.92 (3.32, 4.63) times higher for income loss due to any storm compared to no income loss for any storm. Home flooding and income loss due to any storm also increase the odds of reporting economic difficulties due to COVID-19 (Supplementary Table 2). These results are comparable to the effects observed for home flooding and income loss due to Harvey. Similarly, home flooding and income loss due to any storm are significant predictors of having more severe anxiety. In models examining the cumulative effect of exposure to any storm and COVID-19 income loss on mental health during the pandemic, home flooding and income loss due to any storm were significant predictors of more severe anxiety (Supplementary Table 3), as was COVID-19 income loss.
4. Discussion
As a result of climate change, the United States has experienced more flooding events in recent years (NOAA National Centers for Environmental Information, 2022). Previous studies have shown that repeated disaster exposure reduces resilience to future events (Bonanno et al., 2010). This effect is often mediated by economic and social factors that intensify and prolong the impacts on individuals and communities (Stephenson et al., 2014). These studies, however, typically focus on the effects of repeated exposure to large-scale disasters of short duration. This investigation is the first of its kind to examine how stressors related to a large-scale, short-duration disaster influence economic and mental health outcomes in an evolving, long-term disaster. This study found that previous flood-related economic and mental health stressors influence COVID-19 outcomes more than acute impacts like home flooding and damage. Additionally, COVID-19 income loss and previous flood-related stressors cumulatively affect anxiety severity during the pandemic.
Results of the analysis examining economic and mental health outcomes in the group of respondents exposed to Hurricane Harvey are consistent with previous research on the compounding effects of multiple disasters (Harville et al., 2011, 2018; Jacobs and Harville, 2015; Lowe et al., 2016, 2019). The results suggest respondents adversely affected by Harvey were more likely to experience economic and mental health difficulties due to COVID-19. On its own, COVID-19 income loss is a significant predictor of anxiety severity during the pandemic. When modeled with Hurricane Harvey exposures, both COVID-19 income loss and the storm exposures contribute significantly to the odds of having higher anxiety, suggesting a cumulative effect. Furthermore, results of the sensitivity analysis show respondents impacted by any storm were more likely to experience worse outcomes during the COVID-19 pandemic.
Previous studies of hurricane survivors have shown that property damage, hurricane-related housing insecurity, and hurricane-related unemployment are associated with poor mental health (Galea et al., 2007; Adeola, 2009). Recovery from a disaster can take anywhere from six months to a year or even longer depending on the severity of the incident and the pre-disaster vulnerability of the population (Finch et al., 2010). Additionally, psychological reactions to natural disasters occur in waves of emotional highs and lows that take place well beyond the one-year anniversary of an event (Kessler et al., 2008; Neria and Shultz, 2012; Ruggiero et al., 2012). In a study of particularly vulnerable Katrina-survivors, hurricane-related stressors were associated with high rates of mental and physical illness one year later (Rhodes et al., 2010). Nearly half of study participants exhibited probable PTSD (Rhodes et al., 2010). Three or more years after Katrina, psychological distress remained high enough in 30% of this study population to indicate probable mental illness (Paxson et al., 2012). In March 2020, Southeast Texas was less than three years post-Harvey and less than one year past the severe storms of May 2019 and Tropical Storm Imelda. A preliminary assessment of mental health impacts three weeks after Harvey found a positive association between hurricane exposures and mental health symptoms, particularly PTSD and anxiety symptoms (Schwartz et al., 2018). When the pandemic hit, it is likely vulnerable populations were still in the midst of recovery from previous storms. In this study, economic and mental stressors caused by Harvey have a larger effect size and appear to influence COVID-19 outcomes more than home flooding and damage, highlighting the differential effects of acute impacts versus long-term stressors (Lichtveld, 2018).
The effect of both previous storms and the pandemic on mental health is consequential. The higher IES and GAD-7 scores documented in the registry are associated with functional impairment and depression (Spitzer et al., 2006), as well as panic disorder, social anxiety disorder, and posttraumatic stress disorder (Joseph, 2000; Kroenke et al., 2007). Both disasters are likely to have a long-term impact on the mental health and well-being of the population (Torales et al., 2020) indicating the need to have longitudinal studies designed to better analyze ongoing mental health impacts.
Public health disasters amplify existing vulnerabilities in our communities. Results from the COVID-19 Registry show that in every measure of economic impact tested, non-Hispanic Blacks and Hispanics are experiencing economic difficulties due to COVID-19 at higher rates than non-Hispanic whites. Previous findings from the Texas Flood Registry show that in the year following Harvey, self-reported floodwater exposure increased the odds of adverse health outcomes including shortness of breath, skin rash, problems concentrating, headaches, and general allergic response (runny nose, itchy eyes, and dry skin) (Miranda et al., 2021). Low income and minority registrants, as well as those with pre-existing health conditions, were more likely to report adverse health outcomes (Miranda et al., 2021). This is concerning given that low income and minority populations are at higher risk of exposure to COVID-19 and face poorer health outcomes when infected with the virus (Raifman and Raifman, 2020). Those with pre-existing health conditions are also more likely to get severely ill from COVID-19 (Centers for Disease Control and Prevention, 2021).
These findings are subject to important limitations. First, the data are a convenience sample of those who elected to join the registries. Thus, respondents are not representative of the population of Southeast Texas. Low income and minority populations are more vulnerable to COVID-19 and flooding events. A population-based SARS-CoV-2 prevalence study conducted in Houston demonstrated the disproportionate impact of COVID-19 on minority populations (Symanski et al., 2021). This study population, however, is mostly white. This may limit the generalizability of the results. However, the strength of our findings in this disproportionately white, non-random sample suggests that the effects may be even stronger among minority populations. Second, the check-all-that-apply question for economic difficulties experienced due to the COVID-19 pandemic does not include a ‘Not applicable’ or ‘None of the above’ answer choice. As a result, it is not possible to identify respondents who did not experience economic difficulties. This reduced the number of observations used in the GEE analysis and may have created nonresponse bias. Third, the analysis uses self-reported exposure and health information rather than environmental data and diagnosis of mental health conditions by a medical professional, introducing potential for misclassification and self-report bias. Finally, although the models in this analysis are adjusted for demographic characteristics, the registry lacks information on factors that could provide additional insights to the economic and mental health impacts observed in the study population. Specifically, pre-existing mental health disorders, medication history, history of traumatic events, and the loss of loved ones due to a disaster have been associated with long-term continuing distress and less resilience compared to others (Bonanno et al., 2010; Chan and Rhodes, 2014). Nevertheless, we see important evidence of the high and disparate impact of both disasters in Southeast Texas.
5. Conclusions
The Texas Flood Registry and COVID-19 Registry are web-based community registries designed to track the impacts of public health disasters. The TFR team continues to work with health departments and community partners to contextualize results in the context of larger community concerns. Registries can provide an important mechanism for rapidly collecting important information in the midst of public health crises.
Past flooding events may have made certain people more susceptible and vulnerable to mental health and economic impacts during the pandemic. In planning COVID-19 response efforts, considering exposure to previous disasters, particularly major storms like Hurricane Harvey, may help identify communities and individuals at greatest risk for adverse economic and mental health outcomes during the pandemic. Identifying high risk populations and persistent stressors of people who lived through Harvey will help develop evidence-based interventions. Given recent efforts by the Biden Administration to address health disparities, this work could help assist in prioritizing resources and in guiding policies such as the Justice-40 initiative (Young et al., 2021). To reduce vulnerability to future disasters, storm recovery efforts should prioritize interventions that address mental health and social and economic stability.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We thank members of the Children's Environmental Health Initiative (CEHI) for their contributions to this project. We thank Pierre Martin Dominique Zéphyr and Julia Gohlke for their feedback on the analysis. This project was supported by the Cullen Trust for Health Care, the Environmental Defense Fund, and the National Institutes of Health (Award Number R21ES029461).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2022.114020.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Data availability
The authors do not have permission to share data.
References
- Adeola F.O. Mental health & psychosocial distress sequelae of Katrina: an empirical study of survivors. Hum. Ecol. Rev. 2009;16(2):16. [Google Scholar]
- Adepoju O.E., Han D., Chae M., et al. Health disparities and climate change: the intersection of three disaster events on vulnerable communities in Houston, Texas. Int. J. Environ. Res. Publ. Health. 2021;19(1) doi: 10.3390/ijerph19010035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agresti A., Liu I.M. Modeling a categorical variable allowing arbitrarily many category choices. Biometrics. 1999;55(3):936–943. doi: 10.1111/j.0006-341x.1999.00936.x. [DOI] [PubMed] [Google Scholar]
- Agresti A., Liu I. Strategies for modeling a categorical variable allowing multiple category choices. Socio. Methods Res. 2001;29(4):403–434. [Google Scholar]
- Benevolenza M.A., DeRigne L. The impact of climate change and natural disasters on vulnerable populations: a systematic review of literature. J. Hum. Behav. Soc. Environ. 2019;29(2):266–281. [Google Scholar]
- Bonanno G.A., Brewin C.R., Kaniasty K., Greca A.M. Weighing the costs of disaster: consequences, risks, and resilience in individuals, families, and communities. Psychol. Sci. Publ. Interest. 2010;11(1):1–49. doi: 10.1177/1529100610387086. [DOI] [PubMed] [Google Scholar]
- Caramanica K., Brackbill R.M., Stellman S.D., Farfel M.R. Posttraumatic stress disorder after hurricane sandy among persons exposed to the 9/11 disaster. Int. J. Emerg. Ment. Health. 2015;17(1):356–362. doi: 10.4172/1522-4821.1000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerdá M., Bordelois P.M., Galea S., Norris F., Tracy M., Koenen K.C. The course of posttraumatic stress symptoms and functional impairment following a disaster: what is the lasting influence of acute versus ongoing traumatic events and stressors? Soc. Psychiatr. Psychiatr. Epidemiol. 2013;48(3):385–395. doi: 10.1007/s00127-012-0560-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan C.S., Rhodes J.E. Measuring exposure in Hurricane Katrina: a meta-analysis and an integrative data analysis. PLoS One. 2014;9(4) doi: 10.1371/journal.pone.0092899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covert H.H., Sherman M., Le D., Lichtveld M.Y. Environmental health risk relationships, responsibility, and sources of information among Vietnamese Americans in coastal Mississippi. Health Risk Soc. 2020;22(5–6):362–376. doi: 10.1080/13698575.2020.1840528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Texas Flood Registry Resource Details. Disaster Research Response (DR2) Resources Portal; 2021. https://tools.niehs.nih.gov/dr2/index.cfm/resource/24267 [Google Scholar]
- Disaster Research Response (DR2) Resources Portal; 2022. COVID-19 Registry Resource Details.https://tools.niehs.nih.gov/dr2/index.cfm/resource/24285 [Google Scholar]
- Fernandez W.G., Galea S., Miller J., et al. Health status among emergency department patients approximately one year after consecutive disasters in New York City. Acad. Emerg. Med. 2005;12(10):958–964. doi: 10.1197/j.aem.2005.06.005. [DOI] [PubMed] [Google Scholar]
- Finch C., Emrich C.T., Cutter S.L. Disaster disparities and differential recovery in New Orleans. Popul. Environ. 2010;31:179–202. [Google Scholar]
- Galea S., Brewin C.R., Gruber M., et al. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Arch. Gen. Psychiatr. 2007;64(12):1427–1434. doi: 10.1001/archpsyc.64.12.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harville E.W., Xiong X., Smith B.W., Pridjian G., Elkind-Hirsch K., Buekens P. Combined effects of Hurricane Katrina and Hurricane Gustav on the mental health of mothers of small children. J. Psychiatr. Ment. Health Nurs. 2011;18(4):288–296. doi: 10.1111/j.1365-2850.2010.01658.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harville E.W., Shankar A., Dunkel Schetter C., Lichtveld M. Cumulative effects of the Gulf oil spill and other disasters on mental health among reproductive-aged women: the Gulf Resilience on Women's Health study. Psychol Trauma. 2018;10(5):533–541. doi: 10.1037/tra0000345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holshue M.L., DeBolt C., Lindquist S., et al. First case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz M., Wilner N., Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom. Med. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Hu M.D., Lawrence K.G., Gall M., et al. Natural hazards and mental health among US Gulf Coast residents. J. Expo. Sci. Environ. Epidemiol. 2021;31(5):842–851. doi: 10.1038/s41370-021-00301-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs M.B., Harville E.W. Long-term mental health among low-income, minority women following exposure to multiple natural disasters in early and late adolescence compared to adulthood. Child Youth Care Forum. 2015;44(4):511–525. doi: 10.1007/s10566-015-9311-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia H., Guerin R.J., Barile J.P., et al. National and state trends in anxiety and depression severity scores among adults during the COVID-19 pandemic — United States, 2020–2021. MMWR Morb. Mortal. Wkly. Rep. 2021;70:1427–1432. doi: 10.15585/mmwr.mm7040e3. [DOI] [PubMed] [Google Scholar]
- Joseph S. Psychometric evaluation of horowitz's impact of event scale: a review. J. Trauma Stress. 2000;13(1):101–113. doi: 10.1023/A:1007777032063. [DOI] [PubMed] [Google Scholar]
- Kearney A., Hamel L., Brodie M. Kaiser Family Foundation; 2021. Mental Health Impact of the COVID-19 Pandemic: an Update.https://www.kff.org/coronavirus-covid-19/poll-finding/mental-health-impact-of-the-covid-19-pandemic/ [Google Scholar]
- Kessler R.C., Galea S., Gruber M.J., Sampson N.A., Ursano R.J., Wessely S. Trends in mental illness and suicidality after Hurricane Katrina. Mol. Psychiatr. 2008;13(4):374–384. doi: 10.1038/sj.mp.4002119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B., Monahan P.O., Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Lichtveld M. Disasters through the lens of disparities: elevate community resilience as an essential public health service. Am. J. Publ. Health. 2018;108(1):28–30. doi: 10.2105/AJPH.2017.304193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe B., Decker O., Muller S., et al. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med. Care. 2008;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Lowe S.R., Tracy M., Cerdá M., Norris F.H., Galea S. Immediate and longer-term stressors and the mental health of Hurricane Ike survivors. J. Trauma Stress. 2013;26(6):753–761. doi: 10.1002/jts.21872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe S.R., Sampson L., Gruebner O., Galea S. Community unemployment and disaster-related stressors shape risk for posttraumatic stress in the longer-term aftermath of hurricane sandy. J. Trauma Stress. 2016;29(5):440–447. doi: 10.1002/jts.22126. [DOI] [PubMed] [Google Scholar]
- Lowe S.R., McGrath J.A., Young M.N., et al. Cumulative disaster exposure and mental and physical health symptoms among a large sample of gulf coast residents. J. Trauma Stress. 2019;32(2):196–205. doi: 10.1002/jts.22392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization; Geneva: 2022. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact. [Google Scholar]
- Miranda M.L., Callender R., Canales J.M., et al. The Texas flood registry: a flexible tool for environmental and public health practitioners and researchers. J. Expo. Sci. Environ. Epidemiol. 2021;31(5):823–831. doi: 10.1038/s41370-021-00347-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neria Y., Shultz J.M. Mental health effects of Hurricane Sandy: characteristics, potential aftermath, and response. JAMA. 2012;308(24):2571–2572. doi: 10.1001/jama.2012.110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billion-dollar weather and climate disasters. NOAA National Centers for Environmental Information (NCEI) U.S. 2022 https://www.ncei.noaa.gov/access/monitoring/billions/ [Google Scholar]
- Panchal N., Kamal R., Cox C., Garfield R. Kaiser Family Foundation; 2021. The Implications of COVID-19 for Mental Health and Substance Use.https://www.kff.org/report-section/the-implications-of-covid-19-for-mental-health-and-substance-use-issue-brief/#endnote_link_510918-4 [Google Scholar]
- Paxson C., Fussell E., Rhodes J., Waters M. Five years later: recovery from post traumatic stress and psychological distress among low-income mothers affected by Hurricane Katrina. Soc. Sci. Med. 2012;74(2):150–157. doi: 10.1016/j.socscimed.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- People with Certain Medical Conditions. Centers for Disease Control and Prevention (CDC); 2021. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html [Google Scholar]
- Raifman M.A., Raifman J.R. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am. J. Prev. Med. 2020;59(1):137–139. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes J., Chan C., Paxson C., Rouse C.E., Waters M., Fussell E. The impact of hurricane Katrina on the mental and physical health of low-income parents in New Orleans. Am. J. Orthopsychiatry. 2010;80(2):237–247. doi: 10.1111/j.1939-0025.2010.01027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggiero K.J., Gros K., McCauley J.L., et al. Mental health outcomes among adults in Galveston and Chambers counties after Hurricane Ike. Disaster Med. Public Health Prep. 2012;6(1):26–32. doi: 10.1001/dmp.2012.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sansom G.T., Thompson C., Sansom L., Fawkes L., Boerlin E. Compounding impacts of hazard exposures on mental health in Houston, TX. Nat. Hazards. 2022;111:2809–2818. [Google Scholar]
- Schafer L., Jorks P., Seck E., Koulibaly O., Diouf A. Germanwatch; Bonn, Germany: 2021. Slow-onset Processes and Resulting Loss and Damage - an Introduction. [Google Scholar]
- Schwartz R.M., Tuminello S., Kerath S.M., Rios J., Lieberman-Cribbin W., Taioli E. Preliminary assessment of hurricane Harvey exposures and mental health impact. Int. J. Environ. Res. Publ. Health. 2018;15(5) doi: 10.3390/ijerph15050974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DSHS Annouces First Case of COVID-19 in Texas . 2020. Texas Department of State Health Services.https://www.dshs.texas.gov/news/releases/2020/20200304.aspx [Google Scholar]
- Siegel J.M., Shoaf K.I., Afifi A.A., Bourque L.B. Surviving two disasters: does reaction to the first predict response to the second? Environ. Behav. 2003;35(5):637–654. [Google Scholar]
- Silveira S., Kornbluh M., Withers M.C., Grennan G., Ramanathan V., Mishra J. Chronic mental health sequelae of climate change extremes: a case study of the deadliest californian wildfire. Int. J. Environ. Res. Publ. Health. 2021;18(4) doi: 10.3390/ijerph18041487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stephenson J., Vaganay M., Cameron R., Joseph P. The long-term health impacts of repeated flood events. WIT Trans. Ecol. Environ. 2014;184:12. [Google Scholar]
- Symanski E., Ensor K.B., Piedra P.A., et al. Population-based estimates of SARS-CoV-2 seroprevalence in Houston, Texas as of september 2020. J. Infect. Dis. 2021;224(10):1649–1657. doi: 10.1093/infdis/jiab203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torales J., O'Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatr. 2020;66(4):317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- Vahratian A., Blumberg S.J., Terlizzi E.P., Schiller J.S. Symptoms of anxiety or depressive disorder and use of mental health care among adults during the COVID-19 pandemic — United States, august 2020–february 2021. MMWR Morb. Mortal. Wkly. Rep. 2021;70:490–494. doi: 10.15585/mmwr.mm7013e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamori K., Goltz J.D. Disasters without borders: the coronavirus pandemic, global climate change and the ascendancy of gradual onset disasters. Int. J. Environ. Res. Publ. Health. 2021;18(6) doi: 10.3390/ijerph18063299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S., Mallory B., McCarthy G. The White House; 2021. The Path to Achieving Justice 40.https://www.whitehouse.gov/omb/briefing-room/2021/07/20/the-path-to-achieving-justice40/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors do not have permission to share data.