Abstract
Objective
The objective of the study was to determine and compare flexural strength and microhardness of Cention N with Glass ionomer cement (GIC) (GC Gold Label Type IX Extra) and Zirconomer improved at a distinctive time period in artificial saliva.
Materials and methods
Cention N, GC Gold Label Type IX Extra, Zirconomer improved for the fabrication of samples. To determine the physical properties such as flexural strength and microhardness, test samples (n-30) of dimensions 12 mm (length)*4 mm (breadth)*2 mm (thickness) were made and divided into three groups. Every sample was dipped for 28 days in a plastic tube containing 5 mL of artificial saliva. Statistical analysis was done using one-way ANOVA with a post hoc test, intergroup and intragroup analyses were carried out.
Results
In an intergroup analysis, flexural strength and microhardness of Cention N were substantially higher than Zirconomer improved and GIC (GC Gold Label Type IX Extra), respectively. In intragroup analysis found that there was a significant decrease (p < 0.001) in the level of flexural strength as well as microhardness after samples were immersed in artificial saliva of group A (Cention N), group B (GC Gold Label Type IX Extra), and group C (Zirconomer improved) from 1st day to 28th day in artificial saliva.
Conclusion
It can be concluded that Cention N had the highest flexural strength and microhardness of the three materials tested. Zirconomer improved can be used as a basic filling material in various restorative procedures due to good comparable mechanical properties and is economical for patients.
How to cite this article
Adsul PS, Dhawan P, Tuli A, et al. Evaluation and Comparison of Physical Properties of Cention N with Other Restorative Materials in Artificial Saliva: An In Vitro Study. Int J Clin Pediatr Dent 2022;15(3):350-355.
Keywords: Artificial saliva, Cention N, Conventional glass-ionomer cement, Flexural strength, Microhardness, Zirconomer improved
Introduction
Prevention and eradication of caries have been the greatest challenge faced by dentists. The tooth is typically restored by a coronal restoration material in the case of dental carious lesions, which often requires retreat due to conditions such as the progression of dental caries around the restoration or the falling out of dental restoration.1
Developments in evolutionary research have focused primarily on reducing stresses and improving physical properties2 by manipulating filler factors such as filler particle size, shape, and concentration.3 Research on the physical properties of the material is clinically important especially if they are to be applied in high-masticatory stress-bearing regions.4
Glass ionomer cement (GIC) has always been regarded as a gold standard for the restoration of teeth in pediatric patients because it has certain unique properties, such as the release of anticariogenic fluoride into adjacent tooth structures, and chemical bonding to enamel and dentin.5 However, they are susceptible to fracture and have low wear resistance. These deficiencies have restricted their usage and have made them unsuitable for areas of high stress. Another generation of glass ionomer is GC Fuji type IX, which has been developed specifically for geriatric and pediatric patients, to address the disadvantage of traditional GIC.6
The recently released “alkaline” restorative material Cention N (Ivoclar Vivadent) is a new form of tooth-colored, restorative filling material for bulk placement in retentive preparations. Cention N is a urethane dimetacrylate (UDMA)—based, self-curing powder/liquid restorative with optional additional light curing. The liquid consists of dimethacrylates and initiators, while the powder includes a mixture of glass fillers, initiators, and pigments. It is radio-opaque and contains alkaline glass fillers capable of releasing ions of fluoride, calcium, and hydroxide. Due to the single-use of cross-linking methacrylate monomers in combination with a stable, effective self-curing initiator, Cention N shows a high polymer network density and polymerization degree over the complete depth of restoration.7
Zirconomer (Shofu Inc.) has produced a newer formulation of GIC according to the manufacturer's statement that it uses a robust processing method to demonstrate strength consistent with that of silver amalgam. To achieve optimum particle size and characteristics, the glass portion of the formulation is subjected to finely controlled micronization. Homogeneous zirconia particles are added to further strengthen the content for higher occlusal load resistance and longer durability.8–11
This research was therefore done to assess and compare the physical properties of Cention N with other restorative materials such as GIC (GC Gold Mark Type IX Extra) and Zirconomer improved at different time intervals in artificial saliva.
Materials and Methods
Materials
The restorative materials used in this study were: Cention N (Ivoclar, Vivadent, Liechtenstein), GC Gold Label Type IX Extra (GC International Corp, Japan), and Zirconomer improved (Shofu Inc.), as shown in Table 1.
Table 1.
Test materials used in the study
| Sl. no. | Materials | Manufacturer | Batch no. | Powder/liquid ratio (g) |
|---|---|---|---|---|
| 1. | Group A (Cention N) | Ivoclar vivadent, Liectenstein | X 53,840 | 1:1 |
| 2. | Group B (GC Gold Label 9 Extra) | GC corporation Tokyo, Japan | 201,976 | 1:1 |
| 3. | C (Zirconomer improved) | Shofu inc. Japan | 091,91882 | 2:1 |
Preparation of Sample
The study consists of 30 specimens with dimensions of 12 mm (length) × 4 mm (breadth) × 2 mm (thickness) according to ADA Specification No. 6612 for testing flexural strength and microhardness. Specimens were made with the aid of Affinis Super Soft Putty customized silicone mould (Coltene Whaledent Pvt Ltd). Samples are divided into three groups, each of which has 10 specimens. Group A includes samples of Cention N, group B includes samples of GC Gold Label Type IX Extra, and group C includes samples of Zirconomer improved. The restorative materials used in this analysis have been chemically cured. The test material was mixed and manipulated as per the manufacturer's instructions and put in a modified silicone mould using a plastic filling instrument. The compression firming was carried out by a plastic filling instrument to allow proper adaptation of the material. It was permitted to set the material and after setting, the samples were removed from the mould. The samples were then visually inspected for imperfections and to ensure that the conditions for inclusion and exclusion of the sample are met (Fig. 1).
Fig. 1.

Distribution of test samples according to material
Flexural Strength Test
Samples were mounted on the test machine (Universal Testing Machine; Model 5567, Instron, United Kingdom)24 and a load of one KN was applied using a three-point bending test (I = 20 mm) at a crosshead speed of 1 mm/min until the specimen was fractured (Fig. 2). The maximum fracture load (F in Newton) for each sample was registered at 24 hours. After that, the samples were submerged in 5 mL of artificial saliva (Wet Mouth ICPA Health Products Ltd) with a pH of 5 and kept in the incubator at 37°C for 28 days, and test specimens have recorded the change in flexural strength on 28th day. The flexural intensity was automatically determined using a computerized program based on the following formula:
Fig. 2.

Universal Testing Machine; Model 5567, Instron
F–Maximum load (Newton),
l–Distance between the supports (millimeter),
b–Width of the specimen (millimeter),
h–Height of the specimen (millimeter).
Microhardness Test
Samples used to measure the flexural strength are the same as those used to test the microhardness of the Vickers microhardness measuring tool (HMV Microhardness Tester, Shimadzu, Japan)25 (Fig. 3). The indenter conducted this test, which was pyramidal in shape with a pointed tip and a square base. Test samples were forced against the indenter at a particular load (P) of 300 gm for 15 seconds. The microhardness indenter started at the center of the sample and three indentations linear to four cardinal points with a distance of 4 mm between each other. The mean diagonal length (L) of the resulting indentation on the test specimen was measured at 24 hours. After that, all samples were submerged in 5 mL of artificial saliva (Wet Mouth ICPA Health Products Ltd) for 28 days, and after 28 days, the specimens tested showed an improvement in microhardness. The hardness number of Vickers was determined by the equation given below.
Fig. 3.
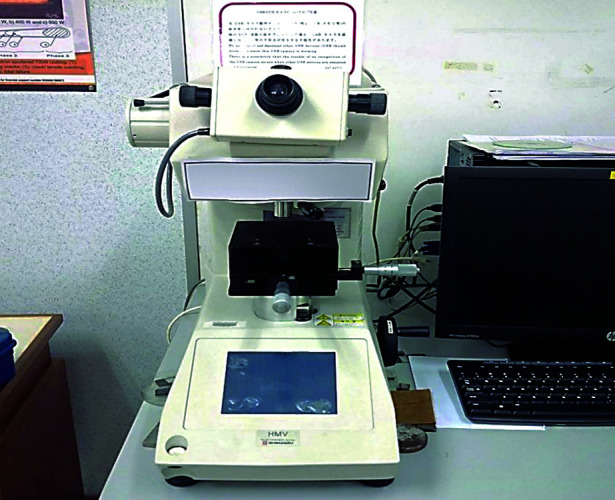
HMV microhardness tester
Vicker's Hardness = KP*L/d2
The value of K is 1.854,
L = applied load (kg),
d is the mean diagonal length (mm).
Statistical Analyses
Data analysis was conducted using SPSS version 18. Intergroup analysis was conducted using one-way ANOVA with the post hoc Tukey test, while a one-way ANOVA with the post hoc Bonferroni test was performed for intragroup comparison. A p-value (p < 0.001) was found to be statistically important.
Results
Intergroup analysis (Table 2) showed that flexural strength in group A (Cention N) was significantly higher (p < 0.001) than in other groups on day 1 and day 28. Group C (Zirconomer improved) was lower than group A (Cention N) but slightly higher than group B (GC Gold Mark Type IX Extra) on day 1 and day 28. Group B (GC Gold Mark Form IX Extra) showing the lowest flexural intensity on day 1 and 28.
Table 2.
Intergroup analysis for flexural strength at different time intervals
| Time interval | Group A | Group B | Group C | p-value* | Post hoc test | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |||
| 1 day | 81.6801 | 0.7580 | 54.1839 | 7.0863 | 76.6781 | 0.8296 | <0.001 | A>C>B |
| 28 day | 72.6101 | 0.6909 | 46.2685 | 4.7673 | 65.5885 | 0.8963 | <0.001 | A>C>B |
*non-significant
Intragroup analysis (Table 3) showed a substantial decrease (p < 0.001) in the flexural intensity of group A (Cention N), group B (GC Gold Mark Type IX Extra), and group C (Zirconomer improved) from day 1 to day 28 in artificial saliva.
Table 3.
Intragroup analysis for flexural strength at different time intervals
| Groups | Day | Mean | SD | p-value* |
|---|---|---|---|---|
| Group A | 1 day | 87.28 | 1.169,797703 | <0.001 |
| 28 day | 79.424 | 1.149,600897 | ||
| Group B | 1 day | 41.581 | 0.583,675138 | <0.001 |
| 28 day | 32.3307 | 0.645,368981 | ||
| Group C | 1 day | 68.527 | 0.464,878718 | <0.001 |
| 28 day | 48.65 | 0.530,056601 |
*non-significant
Comparitive evaluation (Fig. 4) of flexural strength showed that Cention N was significantly higher followed by Ziconomer improved and GC Gold Label Type IX extra
Fig. 4.

Comparison of mean of flexural strength between different restorative materials at different time intervals
Intergroup analysis (Table 4) showed that group A (Cention N) was slightly higher than group C (Zirconomer improved) and significantly higher (p < 0.001) than group B (GC Gold Label Type IX Extra) on day 1 and 28. Group C (Zirconomer improved) was marginally less than group A (Cention N) but significantly higher (p < 0.001) than group B (GC Gold Label Type IX Extra) on day 1 and day 28, group C (Zirconomer improved) was significantly higher (p < 0.001) than group B (GC Gold Label Type IX Extra) on day 28 in artificial saliva. Group B (GC Gold Mark Type IX Extra) showing the lowest microhardness in artificial saliva on days 1 and 28.
Table 4.
Intergroup analysis for microhardness at different time intervals
| Time interval | Group A | Group B | Group C | p-value* | Post hoc test | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |||
| 1 day | 87.28 | 1.169,797703 | 41.581 | 0.583,675138 | 68.527 | 0.464,878718 | <0.001 | A>C>B |
| 28 day | 79.424 | 1.149,600897 | 32.3307 | 0.645,368981 | 48.65 | 0.530,056601 | <0.001 | A>C>B |
*non-significant
Intragroup analysis (Table 5) showed that there was a substantial reduction (p < 0.001) in the microhardness values of group A (Cention N), group C (Zirconomer improved), and group B (GC Gold Mark Type IX Extra) from day 1 to day 28 in artificial saliva.
Table 5.
Intragroup analysis for microhardness at different time intervals
| Groups | Day | Mean | SD | p-value* |
|---|---|---|---|---|
| Group A | 1 day | 81.6801 | 0.758,067052 | <0.001 |
| 28 days | 72.6101 | 0.690,918945 | ||
| Group B | 1 day | 54.1839 | 7.086,323078 | <0.001 |
| 28 days | 46.26,857 | 4.767,331523 | ||
| Group C | 1 day | 76.67,813 | 0.829,621595 | <0.001 |
| 28 days | 65.58,855 | 0.896,357891 |
*non-significant
Comparative evaluation (Fig. 5) of microhardness showed that Cention N was slightly higher than and Ziconomer improved and significantly higher than GC Gold Label Type IX Extra.
Fig. 5.

Comparison of mean of microhardness between different restorative materials at different time intervals
Discussion
This research was undertaken to assess and compare the flexural strength and microhardness of Cention N with improved Zirconomer and GC Gold Mark Type IX Extra at different time intervals in artificial saliva.
Flexural strength and surface microhardness tests are used in dentistry for laboratory stress simulation, which can result from forces applied clinically to restorative materials. The flexural strength of the material is the maximum stress that it can withstand until failure when exposed to bending load, and the hardness is the resistance of the material to indentation or penetration. It has been used to predict material wear resistance against applied forces such as occlusal loading. Knowledge of flexural strength and hardness is important for understanding the clinical behavior of many restorative materials. The requisite flexural properties are highly dependent on clinical applications. High flexural strength is required for restorations that are subject to great masticatory stress.13
In this study, at both the time intervals on the first day and after 28 days of immersion, the flexural strength of Cention N was significantly greater than that of Zirconomer improved and GC Gold Label Type IX Extra. This was similar to the results of the study done in 2018 by Sadananda V et al.,14 which also found superior flexural strength values of Cention N over GIC and Zirconomer. Mishra A et al.15 conducted a study in 2018 in which they stated that flexural intensity in Cention N was significantly higher than GIC and amalgam.
Cention N had higher strength values may be due to the thick polymer network and the degree of polymerization. The fillers are found in the powder of a material consisting of glass filler barium aluminum silicate, ytterbium trifluoride, isofiller (technology Tetric N-Ceram), glass filler calcium barium aluminum fluorosilicate, and glass filler calcium fluorosilicate and alkaline. These fillers are responsible for providing sufficient strength.16 The current study found that Zirconomer's improved flexural strength was substantially higher than GC Gold Label Type IX Extra, similar to the studies conducted by Vemina P Chalissery17 in 2016 and Vemagiri C et al.18 in 2020, which showed that Zirconomer had better physical properties compared to Ketac molar. Zirconomer (White Amalgam) is designed to exhibit strength, that is, consistency with amalgam, through a rigorous manufacturing technique. The glass portion of this high-strength GI undergoes finely controlled micronization to achieve optimum particle size and characteristics. The homogeneous incorporation of zirconia particles into the glass portion further improves the material's toughness and high occlusal load tolerance. Polyalkenoic acid and glass components have been specially processed to give this high-strength GI superior mechanical and handling characteristics.19
The flexural intensity was found to be the lowest in GC Gold Label Type IX Extra at both time intervals, that is, for 1 and 28 days. Similar studies were conducted by Moshaverinia M et al.20 in 2019 in which they reported that EQUIA Forte Fil is a promising restorative material with superior flexural strength and surface hardness compared to regenerative GICs such as Fuji IX GP and ChemFil Rock which were commonly used in dentistry.
In the present study, Cention N showed marginally higher microhardness values than Zirconomer improved and the microhardness of both Cention N and zirconomer improved significantly higher than GC Gold Label type IX Extra at both time intervals on the first day and after 28 days of immersion. This was similar to the study conducted by Mazumdar P et al.21 in 2018, which reported that Cention N had the highest microhardness value followed by silver amalgam, nanohybrid composite resin, and type II GIC. Possibly their increased microhardness is linked to the inorganic filling nanoparticle size, which makes Cention N a more clinically suitable choice for clinical treatments.
GC Gold Label Type IX Extra displayed the lowest microhardness compared to Cention N and Zirconomer improved on day 1 and 28. In contrast to the present research, Prabhakar et al.22 in 2010 found that the surface hardness of traditional GICs was higher than that of resin-modified materials when stored in deionized for 30 days. In 2017, Asafarlal S19 carried out a comparative assessment of the hardness of three GICs– Zirconomer, Fujii IX Extra GC, and Ketac Molar. The result of the study found that Fuji IX Extra GC showed high durability among the materials tested. According to this research, the explanation for this was that the particle size and matrix vary from one substance to another, and hence the hardness. Therefore each material has a different polishability. To be successful, the cutting particles must be harder than the filler materials. The process of polishing influences the surface hardness of the GIC since it requires polishing the particles of glass.
Artificial saliva was used as a tool for the determination of physical properties to mimic natural oral environmental conditions, although it is difficult to replicate exactly the properties of human saliva due to the inconsistent and fragile existence of natural saliva. A similar medium used in a study conducted by Ong J et al.23 in 2018 suggested that the leaching of restorative constituents was stated to be higher in artificial saliva compared to distilled water. In contrast to the present research, El Mallakh BF and Sarkar NK5 reported that deionized water was favored as a storage medium over artificial saliva due to the high viscosity and presence of ions in the latter. In vitro results may not be directly representative of in vivo results.
Despite this standardization of the experiment, these results indicate variation, as limitations remain. Existing when attempting to extrapolate these findings to the clinical output of the oral content difficulties in the cavity such as saliva, visibility problems, material handling operator, etc. It could play an important role in the curing and setting of the material that will affect the process strength of the material a lot.
The properties measured from specimens submerged in a static medium cannot take into account the complex nature of the conditions present in the oral cavity.
The test was conducted in rectangular moulds, different findings can be obtained within the case of dental preparation.
Further analysis involving the utilization of materials and multiple combinations of polymerization modes and techniques is required.
Conclusion
Based on the findings of this in vitro study, the following conclusions were drawn:
Cention N is a promising restorative material with superior flexural strength and microhardness compared to Zirconomer improved and GC Gold Label Type IX Extra.
Zirconomer improved by providing greater flexural strength and microhardness than GC Gold Label Type IX Extra and less than Cention N.
GC Gold Label Type IX Extra having less flexural strength and microhardness compared to Cention N and Zirconomer improved.
According to present research Cention N and Zirconomer improved were found to be better restorative materials for use in stress-bearing areas.
Orcid
Aditi Singh https://orcid.org/0000-0003-1537-6986
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Nigam AG, Jaiswal J, Murthy R, et al. Estimation of fluoride release from various dental materials in different media—an in vitro study. Int J Clin Pediatr Dent. 2009;2(1):1–8. doi: 10.5005/jp-journals-10005-1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Didem A, Gozde Y, Nurhan O. Comparative mechanical properties of bulk–fill resins. Open J Compos Mater. 2014;4(2):117–121. doi: 10.4236/ojcm.2014.42013. [DOI] [Google Scholar]
- 3.Kavei D. The evolution of contemporary nano–filled composite materials for dentistry clinical applications. http://www.semantic.org/ IJETAE. 2015;8:214–219. Retrieved from. [Google Scholar]
- 4.Curtis AJ, Shortall AC, Marquis PM, et al. Water uptake and strength characteristics of a nanofilled resin based composite. J Dent. 2007;36(3):186–193. doi: 10.1016/j.jdent.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 5.El Mallakh BF, Sarkar NK. Fluoride release from glass ionomer cement in de-ionized water and artificial saliva. Dent Mater. 1990;6(2):118–122. doi: 10.1016/s0109-5641(05)80041-7. [DOI] [PubMed] [Google Scholar]
- 6.Topbasi B, Öveçoglu ML, Türkmen C. Flexural strength and fracture surface characterization of glass-ionomer cements stored in water. http://www.semantic.org/ Oral Health Dent Manag. 2003;2:18–26. Retrieved from. [Google Scholar]
- 7.Ivoclar Vivadent. Scientific Documents: Cention N. :7–58. p. [Google Scholar]
- 8. SHOFU DENTAL GmbH Am Brüll 17, 40878 Ratingen, Germany. [Google Scholar]
- 9.Patel MU, Punia SK, Bhat S, et al. An in vitro evaluation of microleakage of posterior teeth restored with amalgam, composite and zirconomer - a stereomicroscopic study. J Clin Diagn Res. 2015;9(7):ZC65–ZC67. doi: 10.7860/JCDR/2015/13024.6225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Volpato CM, Garbelotto LGAD, Fredel MC, et al. In: Advances in ceramics–electric and magnetic ceramics, bioceramics, ceramics and environment. Sikalidis C, editor. Rijeka: InTech; 2011. “Application of zirconia in dentistry: Biological, mechanical and optical considerations”. pp. 397–404. editor. [Google Scholar]
- 11.Schenck L, Burtscher P, Vogel K, et al. Major breakthrough in the field of direct posterior composite resins - thanks to the combined use of Tetric EvoCeram Bulk Fill and Bluephase Style. Special Feature DZW. 2011;38/11:3–15. [Google Scholar]
- 12. ANSI/ADA Specification No. 66 for Dental Glass Ionomer Cement (1987) [Google Scholar]
- 13.Chung SM, Yap AU, Chandra SP, et al. Flexural strength of dental composite restoratives: comparison of biaxial and three-point bending test. J Biomed Mater Res B Appl Biomater. 2004;71(2):278–283. doi: 10.1002/jbm.b.30103. [DOI] [PubMed] [Google Scholar]
- 14.Sadananda V, Shetty C, Hegde NM, et al. Alkasite restorative material: flexural and compressive strength evaluation. http://journalcra.com Res J Pharm Biol Chem Sci. 2018;9(5):2179. Retrieved from. [Google Scholar]
- 15.Mishra A, Singh G, Singh SK, et al. Comparative evaluation of mechanical properties of Cention N with conventionally used restorative materials—an in vitro study. Int J Prosthodont Restor Dent. 2018;8(4):120–124. doi: 10.5005/jp-journals-10019-1219. [DOI] [Google Scholar]
- 16.Mann JS, Sharma S, Maurya S, et al. Review article Cention N: a review. http://journalcra.com Int J Curr Res. 2018;10(5):69111–69112. Retrieved from. [Google Scholar]
- 17.Chalissery VP, Marwah N, Almuhaiza M, et al. Study of the mechanical properties of the novel Zirconia-reinforced glass ionomer cement. J Contemp Dent Pract. 2016;17(5):394–398. doi: 10.5005/jp-journals-10024-1861. [DOI] [PubMed] [Google Scholar]
- 18.Vemagiri C, Uloopi KS, Chandrappa V, et al. A comparative evaluation of microleakage, compressive strength, flexural strength and fluoride release of Zirconomer and ketac silver: an in vitro study. J of Biomed and Pharm Res. 2020;9(4) doi: 10.32553/jbpr.v9i4.770. [DOI] [Google Scholar]
- 19.Asafarlal S. Comparative evaluation of microleakage, surface roughness and hardness of three glass ionomer cements – Zirconomer, Fujii IX Extra GC and Ketac Molar: an in vitro study. J Dent. 2017;7:427. doi: 10.4172/2161-1122.1000427. [DOI] [Google Scholar]
- 20.Moshaverinia M, Navas A, Jahedmanesh N, et al. Comparative evaluation of the physical properties of a reinforced glass ionomer dental restorative material. J Prosthet Dent. 2019;122(2):154–159. doi: 10.1016/j.prosdent.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 21.Mazumdar P, Das A, Guha C, et al. Comparative evaluation of hardness of different restorative materials (restorative GIC, Cention N, Nanohybrid composite resin and Silver amalgam) – an in vitro study. Int J Approx Reason. 2018;6:826–832. doi: 10.21474/IJAR01/6737. [DOI] [Google Scholar]
- 22.Prabhakar AR, Paul MJ, Basappa N. Comparative evaluation of the remineralizing effects and surface micro hardness of glass ionomer cements containing bioactiv (S53P4): an in vitro study. Int J Clin Pediatr Dent. 2010;3(2):69–77. doi: 10.5005/jp-journals-10005-1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ong J, Yap AU, Hong JY, et al. Viscoelastic properties of contemporary bulk-fill restoratives: a dynamic-mechanical analysis. Oper Dent. 2018;43(3):307–314. doi: 10.2341/16-365-L. [DOI] [PubMed] [Google Scholar]
- 24.www.service-testing.com. www.service-testing.com Calserv Repair, sales, calibration and maintenance of testing machines. Accessed 4th june 2020.
- 25.Gan, Edward. http://www.reserchget.net/ Effects of Conventional and Two–Step Sintering on the Properties of Hydroxyapatite. 2015;10:131–140. Retrieved from. [Google Scholar]


