Abstract
Background
Oral health is an essential component of health throughout life. Two major oral diseases, dental caries and gingival conditions are prevalent in young population. School-based oral health education (OHE) programs with recognized technology and traditional lecturing could be strategic in promotion of oral health behavior in developed and developing countries.
Aim
The aim of the study is to summarize existing evidence in order to evaluate the effectiveness of OHE programs in school children aged 5–16 years in improving their oral health status.
Methodology
Clinical trials with school children between 5 and 16 years were included. Eligible studies were those which had outcomes as caries, plaque and gingival indices, and oral hygiene status. Articles published from 2010 to 2019 in English language from PubMed, Directory of Open Access Journal (DOAJ), and Google Scholar were searched. Forty-one articles were identified and relevance was determined by examining title and full article. Nine articles were included for qualitative synthesis and seven were eligible for meta-analysis. The risk of bias was assessed by Cochrane Handbook. A meta-analysis was done using Review Manager 5.3 software.
Results
After the meta-analysis results for cumulative mean difference was found as 0.05 (–0.17, 0.27), –0.37 (–0.74, 0.00), –0.20 (–0.33, –0.07), and –0.17 (–0.73, 0.38) for plaque status, Oral Hygiene Index-Simplified (OHI-S), debris status, and dental caries, respectively showing a significant difference favoring the experimental group than traditional group.
Conclusion
Interventions given by various aids like lectures, albums, models, flipcharts, leaflets, E-programs, games, drawings, and presentations proved effective in improving oral hygiene status and dental caries, but no reduction in plaque levels and gingival inflammation as compared to oral health talk/counseling by dentists.
How to cite this article
Gurav KM, Shetty V, Vinay V, et al. Effectiveness of Oral Health Educational Methods among School Children Aged 5–16 Years in Improving their Oral Health Status: A Meta-analysis. Int J Clin Pediatr Dent 2022;15(3):338-349.
Keywords: Audio–video presentations, Oral health education, Oral health promotion, Oral health talk, Oral hygiene, School children
Introduction
Oral health to be recognized equally important in relation to general health has come to in recent times.1 Dental caries and gingival diseases are common diseases that affect about 80% of the school going children worldwide.2 The problems of pain and tooth loss adversely affect the appearance, nutritional intake, quality of life, growth, and development of these children.1
The cost of neglect of these diseases is also high due to the personal, financial, and social impacts. Though oral diseases can be preventable in their early stages, the knowledge that these diseases can be prevented by uncomplicated self-controlled oral hygiene procedures is not provided to many of the children and their caregivers like parents and teachers. Also lost in this loop are the policymakers.1 Hence, prevention has become the corner stone of the modern dental practice.3
Health promotion is given with a motto to enable people to manage and to improve their health. OHE is a significant aspect of oral health promotion and is a crucial and basic part of oral health services. The overall purpose is to principally provide information to improve oral health knowledge for adoption of a healthier lifestyle, changed attitudes, and desirable behaviors through educational means.4 Provided the health promotion in schools is conducted in a comprehensive and interesting manner it can improve the oral health status.5 OHE is required for promoting oral health in adolescents. It is during the young years of people that there is a chance to assume responsibility for learning and maintaining health-related attitudes and behaviors that carry over into adulthood.4
Oral health education encompasses publicity campaigns, occasional talks at an elementary school, a showing of dental health films, and an extensive, reinforced program in a school curriculum. Several factors are important for effective OHE such as repetition and reinforcement of oral hygiene instructions. These concepts show significant, positive, short-range, and long-term effects.3
School age is influential in people's lives. It is a time when lifelong sustainable oral health related behaviors, beliefs, and attitudes are being instilled. During this stage, children are more receptive; in addition, earlier establishment of habits produces a longer lasting impact. Therefore, schools can be considered an ideal environment for promoting oral health.4 Favorable health related behaviors are more concretely established in preadolescent and adolescent age group and once established tend to be sustained during adulthood as well. Further, schools provide are always an ideal setting when it comes to deliver OHE in collaboration with preventive services to achieve oral health promotion. Globally, schools have been recognized as an ideal setup to deliver OHE to be effective in improving oral hygiene, oral health knowledge and behavior.6 Moreover, school based approach has been reported to be more cost effective and efficient in delivering preventive and curative services than community based approach.7
Along with engaging young children in the guidelines regarding brushing and role of diet in oral health interventions it is essential to develop their interest toward learning habits for a lifetime of good oral health. In most of these programs, traditional health education aids, such as lectures, demonstration, and models are used which are proven to have a minimal or short-term effect on children.8
For contemporary form of OHE, the use of combined actions is frequent and includes lectures/talks assisted with different tools such as flipcharts, video, slide presentation, and other types of actions such as supervised dental brushing and topical fluoride application.
The aim of this study was to evaluate the effectiveness of OHE methods using flipcharts, slide presentation, audio–video presentations, and models as compared to traditional oral health talk in the school context for enhancing oral hygiene status of school children aged 5–16 years through this systematic review and meta-analysis.
Methodology
Protocol Development
The protocol for this systematic review and meta-analysis was drafted and designed according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement. PROSPERO registration was done a priori under number CRD42020156997. Following the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions version 5.1.09 we conducted this systematic review.
As this is a systematic review ethical approval or the “protection of human subjects and animals in research” and informed consent is not applicable. The focused question posed as “In school children aged 5–16 years are the newer OHE methods as compared to traditional oral health talk effective in improving oral hygiene status, plaque and gingival status, and dental caries status?”
Search Strategy
Various electronic databases were searched bereft restriction of language conducted on PubMed/MEDLINE, DOAJ, Cochrane Central Register of Controlled Trials, and Web of Science until October 2019. Searches in the ClinicalTrials.gov database and in the references of the included studies (cross referencing), were also conducted.
Searches combing the MeSH terms, keywords, and other free terms keeping in mind the focused question were used adducting with Boolean operators (OR, AND). The exact keywords were searched on all platforms according to the syntax rules of different databases. Table 1 depicts the search strategy and population, interventions, comparisons, outcomes, and study design (PICOS) tool.
Table 1.
The search strategy and PICOS tool
| Search strategy | |
|---|---|
| Focused question | In school children aged 5–16 years are the newer oral health educational methods as compared to traditional oral health talk effective in improving oral hygiene status, plaque and gingival status, and dental caries status? |
| Population | (Adolescent [MeSH] OR Teenagers [Text Word] OR Teens [Text Word] OR Kids [Text Word] OR School children [Text Word] OR children [Text Word] OR Youngsters [Text Word] OR Youth [Text Word] |
| Intervention | (School Health Promotions [Text Word] OR Behavioral counseling [Text Word] OR Health education (Mesh) OR Community Health Education [Text Word] OR Dental health education [Text Word] OR Oral health education [Text Word] |
| Comparisons | Oral health talk [Text Word] OR Oral health counseling [Text Word] OR Behavior motivation [Text Word] OR Motivational interviewing [Text Word] |
| Outcomes | Dental caries [Text Word] OR caries [Text Word] OR Tooth decay [Text Word] OR plaque status[Text Word] OR plaque index [Text Word] OR gingival status [Text Word] OR gingival index [Text Word] OR gingival inflammation [Text Word] OR Gingivitis [Text Word] OR oral hygiene index [Text Word] OR oral hygiene status [Text Word] |
| Study design | Prospective cohort, controlled clinical trial, clinical trial, and RCT |
| Search combination | #1 AND #2 AND #3 AND #4 |
| Database search | |
| Language | No restriction |
| Electronic databases | PubMed/MEDLINE, Cochrane Central Register of Controlled Trials, and Web of Science |
| Journals | International Journal of Paediatric Dentistry, International Journal of Clinical Pediatric Dentistry, European Journal of Paediatric Dentistry, Journal of Indian Society of Pedodontics and Preventive Dentistry, and Journal of Pediatric Dentistry and Journal of Indian Association of Public Health Dentistry |
Inclusion Criteria
Population (P): school children (5–16 years) both girls and boys.
Interventions (I): OHE methods including demos/videos/posters/presentations/activities/oral hygiene instructions given by dental professionals only (experimental group).
Comparison (C): traditional OHE method including oral health talk or oral health counseling (control group).
Outcome (O): dental plaque index, gingival index, OHI-S, and decayed, missing, filled teeth (DMFT)/decayed missing filled surface (DMFS) index at different intervals/follow-ups.
Study design (S): experimental, clinical and randomized controlled trial (RCTs) studies, controlled clinical trial, and clinical trials.
Time (T): follow-up term kept at 1 month and 18 months.
Exclusion Criteria
Animal studies, in vitro studies, observational study designs, case reports, and reviews. In addition, studies reporting about a single intervention were excluded.
Selection Criteria
This review included controlled clinical trial, clinical trial, and RCT that evaluated different methods of OHE methods delivered by dental professionals to school children aged 5–16 years. Also only individual studies which followed protection of human subjects and animals in research and which had been ethically approved were included in the review for analysis. Animal studies, in vitro studies, case reports, observational studies, and reviews were excluded.
Screening Process
The search and screening process were conducted independently by two reviewing authors, in context to previously established protocol, primarily analyzing titles and abstracts. In a secondary phase, entire full text articles were selected for careful reading and analyzed as per eligibility criteria (inclusion/exclusion) for subsequent data extraction. Disparity among authors/reviewers were settled through thorough discussion by the third author. Cohen's Kappa (κ) test was applied to assess the inter-reviewer reliability for search agreement. If needed, the authors of the included studies were contacted by e-mail for clarification of any doubts.
Data Extraction
The following data were extracted from the included studies (when available) by two independent reviewing authors: study identification number, authors, study design, follow-up, number of subjects, age, gender, type of OHE for intervention and control groups, mean plaque, gingival, OHI-S index, DMFT score, effect size, and author's conclusions were recorded.
Assessments of the Risk of Bias and Quality
Cochrane Collaboration Tool9 for RCTs was executed for quality assessment of the selected studies by using the random sequence generation, allocation concealment, blinding of participants, incomplete outcome data, selective reporting, and other bias.
Statistical Analysis
Review Manager 5.3 software was used for quantitative analysis. Standardized mean difference and effect size were interpreted as primary summary measures. Graphical representation was done with forest plots and funnel plots to envision the differences between groups and publication bias. The overall estimated results were considered as significant at p < 0.05.
Results
Literature Search
The first hand electronic database search on PubMed/MEDLINE and Cochrane Library resulted in 9,982 titles. Identical articles were 82 in number. After screening the abstracts, 424 relevant titles were selected by two independent reviewers and 383 were excluded for not being related to the context of topic (studies not within required publication period = 100, studies involving other population = 116, other study designs = 80, inappropriate data for extraction as needed = 07, interventions in other settings = 68, and studies with no control group = 12).
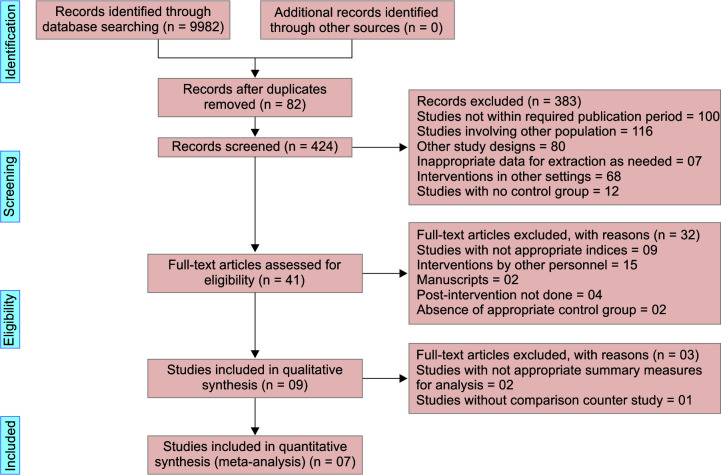
Subsequently after assessment and discussion with reviewers, 41 articles were finalized for full-text article evaluation. Manual searching of the reference of the selected studies did not lead to any additional papers. After prescreening, the inclusion and exclusion criteria were applied and nine studies remained (nine studies with inappropriate indices used for recording outcomes were excluded, 15 studies with interventions given by personnel other than dental professionals were dropped, two excluded were manuscripts, four did not include postinterventions done, and two did not account for appropriate control group). Nine studies were involved for the systematic review which were used for data extraction and statistical analysis. Out of the nine studies, seven studies were eligible and proceeded for the quantitative synthesis. Figure 1 elaborates the PRISMA flowchart.
Fig. 1.
PRISMA 2009 flow diagram
Study Characteristics
There are nine studies included in this review, the general characteristics of which are presented in Table 2. Majority of the studies included, that is, seven are conducted in different parts of India1,2,8,10–13 and one each in Greece6 and Syria.14 The study design of all 11 studies was RCT. The population comprised of 5–16 years old individuals according to the inclusion and exclusion criteria throughout the study term. A total of 1,100 children were included for the studies’ analyses, with equal distribution of participants in intervention and control groups. Notable methodological heterogeneity was found among the experimental OHE methods performed in the included studies. Thus, the interventions described by the studies were categorized such as:
Table 2.
Characteristics of the included studies
| Sl. No. | Study ID | Place of the study | Study design | Sample size at baseline | Total sample at follow-up = N (drop out %) | Age group |
Gender
N (%) |
Method of DHE for intervention group | Method of DHE for control group | Reinforcement period | Follow-up period | Method of outcome assessment | Mean Plaque Index score | Mean Gingival Index score | Mean Oral Hygiene Index Status score | Mean DMFT/DMFS Index score | Authors conclusions |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Chandrashekar et al.2 | Hyderabad, Andhra Pradesh, India | RCT | Group 1: 40 Group 3: 40 |
Group 1: 37 (7.5) Group 3: 40 (0) |
15 years | Group 1: M = 17 (45.9), F = 20 (54.1) Group 3: M = 20 (50), F = 20 (50) |
Group 3: DHE by a qualified dentist at 3 months interval using the audio–visual aids | Group 1: control group with no subsequent DHE after the initial health education offered at the time of screening | At 3 months interval | 6 months | Mean OHI-S, Plaque Index were assessed | Group 1: B = 2.41 (0.5), F = 1.16 (0.34) Group 3: B = 2.22 (0.58), F = 1.2 (0.56) |
− | Group 1: B = 3.59 (0.8), F = 3.21 (0.95) Group 3: B = 3.6 (0.84), F = 2.85 (0.97) |
− | The concept of utilizing the teachers for frequent DHE and screening for any gross deposits of food debris and calculus is feasible. Also frequent DHE by teachers (group 2) was more effective than the infrequent DHE by the professionals |
| 2. | John et al.10 | Tiruchengode, Tamil Nadu, India | RCT | Group A (n = 25) Group C (n = 25) |
− | 4–6 years | − | Group C children were shown a drama enacted by the senior dental residents (trained by the same dentist) disguised as cartoon characters such as Dora, Mickey Mouse, Power Ranger and a devil, for about 20 minutes | Group A: oral health talk was delivered by the dentist | − | 3 months | Mean difference between pre and post-DI-S, a part of the Oral Hygiene Index modified for the primary dentition | − | − | Group A: Pre A-Post A 0.1579 ± 0.2775 Group C: Pre C-Post C 0.4124 ± 0.4815 |
Drama as a method of health education can have a bigger impact on the oral health attitude and practices of the preschoolers. These modes can serve to reinforce as well as improve the oral health practices among preschool children | |
| 3. | Chandrashekar et al.1 | Nalgonda District, Andhra Pradesh, India | RCT | Group 1: 40 Group 2: 40 |
Group 1: 36 (10) Group 2: 35 (12.5) |
15 years | Group 1: M = 16 (44.4), F = 20 (55.6) Group 2: M = 16 (45.7), F = 19 (54.3) |
Group 2: DHE by a qualified dentist at 3 months interval using the audio–visual aids | Group 1: control group with no subsequent DHE after the initial health education offered at the time of screening | At 3 months interval | 6 months | Mean OHI-S, Plaque Index, Gingival Index, and DMFS index were assessed | Group 1: B = 2.46 ± 0.64, F = 2.83 ± 0.41 Group 2: B = 2.34 ± 0.72, F = 2.53 ± 0.78 |
Group 1: B = 1.84 ± 0.5, F = 2.18 ± 0.47 Group 2: B = 1.75 ± 0.68, F = 1.89 ± 0.68 |
Group 1: B = 4.01 ± 1.81, F = 4.67 ± 1.72 Group 2: B = 4.03 ± 1.92, F = 4.28 ± 1.83 |
Group 1: B = 2.03 ± 0.37, F = 2.08 ± 0.43 Group 2: B = 2.40 ± 0.48, F = 2.51 ± 0.52 |
The dramatic reductions in the OHI-S, Plaque Index, and Gingival Index scores in the group supplied with oral hygiene aids call for supplying low cost fluoridated toothpastes along with toothbrushes through the school systems in rural areas |
| 4. | Angelopoulou et al.6 | Greece | Two arm parallel-group prospective clinical trial | Experiential learning (EL) group: 84 Traditional lecturing (TL) group: 100 |
− | 10–11 years | EL group: M = 45 (54), F = 39 (46) TL group: M = 55 (55), F = 45 (45) |
EL group had lecture on oral health issues by a dentist along by their teacher using the program's manual along with extramural visits, for example, to the dentist, to the vet, to the pharmacy or supermarket and which was presented by the students in the classroom using different forms such as theatrical play, posters, songs, crafts, role playing, etc. | TL group had only a lecture on oral health issues by a dentist | − | 18 months | Dental plaque using a modification of Hygiene Index of Lindhe, that does not use a disclosing agent and gingivitis using the GI-S by median (IQR) Mean dental caries (DMFT), according to the diagnostic criteria of the British Association of Community Dentistry |
EL group: B = 64.6 (38.0, 83.3), F = 55.6 (29.2, 79.2) TL group: B = 57.7 (30.6, 80.6), F = 66.7 (37.6, 83.3) |
EL group: B = 31.2 (19.4, 41.7), F = 22.2 (12.5, 43.8) TL group: B = 34.4 (17.7, 48.7), F = 26.0 (8.3, 41.1)* *p < 0.05 |
− | EL group: B = 0.77 (1.13), F = 1.01 (1.45)* TL group: B = 0.55 (1.16), F = 0.87 (1.30)* *p < 0.05 |
EL program was found more successful than TL in oral hygiene improvement. Both oral health education programs improved the oral health knowledge, attitude and behavior of children |
| 5. | Kumar et al.11 | Tamil Nadu, India | RCT | Group A: 30 Group B: 30 |
Group A: 27 (10) Group B: 28 (6.5) |
7–10 years | − | Group B: educated with both flash card and game based (connect the dots) method | Group A: educated with conventional method | Once daily for a period of 1 week | 1 and 3 months | Mean DI-S | − | − | Group A: B = 1.26 (0.37), F = 0.94 (0.34) Group B: B = 1.30 (0.35), F = 0.73 (0.25) |
− | The connect the dots game that includes oral health guidelines including good dental hygiene and dietary habits can thus be an effective intervention aid for teaching the basic oral health concepts among school going children |
| 6. | Malik et al.8 | Lucknow, Uttar Pradesh, India | RCT | Group I: 75 Group II: 75 |
Group I: 75 (0) Group II: 75 (0) |
8– 12 years | − | Group I: dental examiners gave a 15 minutes lecture on oral health, brushing, and diet using PowerPoint presentation | Group II: dental examiners instructed using the game-based teaching method (crosswords and quizzes) combined with PowerPoint | Once a day for 7 days | 1 and 3 months | Mean dental plaque scores by Turesky, Gilmore, Glickman modification of the Quigley–Hein index | Group I: B = 3.04 (0.79), F = 1.55 (0.35)* Group II: B = 3.07 (0.58), F = 1.26 (0.51)* *p < 0.05, significant |
− | − | − | Implementation of crossword game-based oral health education program is an easy and effective aid for teaching oral health instructions and preventing oral diseases in children as the knowledge scores of children increased considerably when the game-based teaching intervention was used |
| 7. | Sadana et al.12 | Amritsar City, India | Double-blind randomized controlled field trial | Group I: 50 Group II: 50 Group III: 50 |
− | 10–12 years | − | Group II: verbal communication but along with self-educational pamphlets Group III: oral health education through verbal communication along with audiovisual method shown in the schools |
Group I: oral health education was verbal communication | − | 6 weeks | Mean plaque score was recorded using Silness and Lӧe Plaque Index | Group I: B = 1.158 (0.39), F = 0.845 (0.18) Group II: B = 1.623 (0.52), F = 1.023 (0.27) Group III: B = 1.453 (0.46), F = 0.728 (0.20) |
− | − | − | The mean plaque scores of children decreased in the experimental group after the intervention. When used along with oral lectures, oral health education was found to be most effective when used with audio–visual aids as well as with self-educational pamphlets. Hence, both these methods when used along with oral lectures are equally effective in improving the knowledge and plaque scores in children |
| 8. | Umamaheswari et al.13 | Tamil Nadu, India | Randomized controlled pilot trial | Group A: 30 Group B: 30 |
Group A: 30 (0) Group B: 30 (0) |
5–7 years | − | Group B: the Good Behavior Game group | Group A: the conventional health education group | Once daily for 7 days | 3 months | Mean difference of DI-S proposed by Greene and Vermillion and modified by Greene | − | − | Group A: baseline-post-3 months 0.168 (0.329) Group B: baseline-post-3 months 0.96 (0.375) |
− | The present study was undertaken to advance the area of behavioral vaccine as an alternative for teaching basic oral health concepts in children. In this study, the GBG was found to be an effective intervention aid for educating children |
| 9. | Al Bardaweel et al.14 | Damascus City, Syria | Clustered RCT | Leaflet cluster (LC): 110 E-learning cluster (EC): 110 |
LC: 100 (9.1) EC: 100 (9.1) |
10–11 years | LC: M = 43 (43), F = 57 (57) EC: M = 48 (48), F = 52 (52) |
LC who received oral health education through leaflets | EC who received oral health education through an E-learning program | 3 months | Mean Plaque Index and Gingival Index scores | LC: B = 2.25 ± 0.43, F = 0.85 ± 0.35* EC: B = 2.33 ± 0.38, F = 1.21 ± 0.40* p < 0.001* |
LC: B = 1.76 ± 0.36, F = 0.74 ± 0.22* EC: B = 1.83 ± 0.34, F = 1 ± 0.25* p < 0.001* |
− | − | Traditional educational leaflets are an effective tool in the improvement of both oral health knowledge as well as clinical indices of oral hygiene and care among Syrian children. Leaflets can be used in school-based oral health education for a positive outcome |
DHE, dental health education; GBG, gingival bleeding grade; IQR, inter quartile range
1 Interventions: OHE, oral health education; activities with lectures, albums, slides, leaflets, counseling, games, drawings, theater, and dieting guidance
2 OHI, oral health instruction
3 Outcomes assessed: PI, plaque index; GI, gingival index; DMFS, decayed dissed filled permanent tooth surface; DMFS, decayed missed filled primary tooth surface; DMFT, decayed missed filled permanent tooth
*Excluded from meta-analysis
Oral health education activities with lectures, albums, slides, leaflets, counseling, games, drawings, theater, and dieting guidance.
Oral health instruction (OHI) reported as additional delivery of information directed particularly to toothbrushing methods.
Therefore, OHIs in control group involved for this review were considered as traditional OHE activities and compared with various types of interventions provided to the school children as mentioned above in (ii) as the experimental group. The overall loss to follow-up ranged from 0 to 12.5%. The intervention study timing ranged from 1 month to 1.5 years.
Varying forms of OHE were given in all the studies at start of the study with different follow-ups of reinforcement depending on the entire time of study (Table 2).
Similarly, the variety of outcome parameters were assessed postintervention across the studies. Oral Hygiene Index-Simplified by two studies,1,2 Simplified Debris Index by three studies,10,11,13 Plaque Index by four studies,1,2,12,14 Tuskegy Modification of Quigley–Hein Plaque Index by one study,8 Gingival Index by three studies,1,6,14 Modification of Hygiene Index of Lindhe Index by one study,1 and DMFT/DMFS Index by two studies.1,6 Overall, postintervention results were showing an inclination toward the intervention groups among the assessed outcome parameters.1,2,6,8,10–13
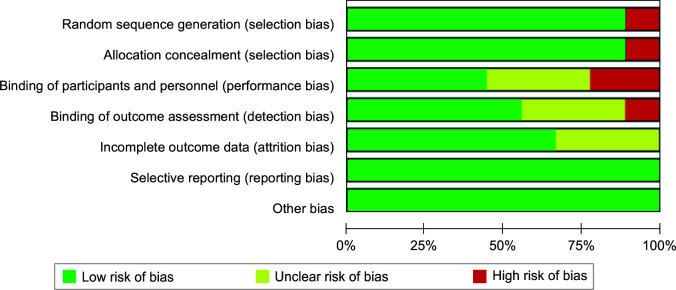
Quality of the Studies
Quality assessment showed a spectrum of variety across the included studies. Quality assessment of the 11 RCTs was executed according to Cochrane Risk of Bias Tool (Table 3). Three studies showed a low potential risk of bias,1,2,13 four studies a moderate risk of bias,8,10–12 and two studies a high potential risk of bias6,14 (Figs 2 and 3).
Fig. 2.
Risk of bias graph
Fig. 3.
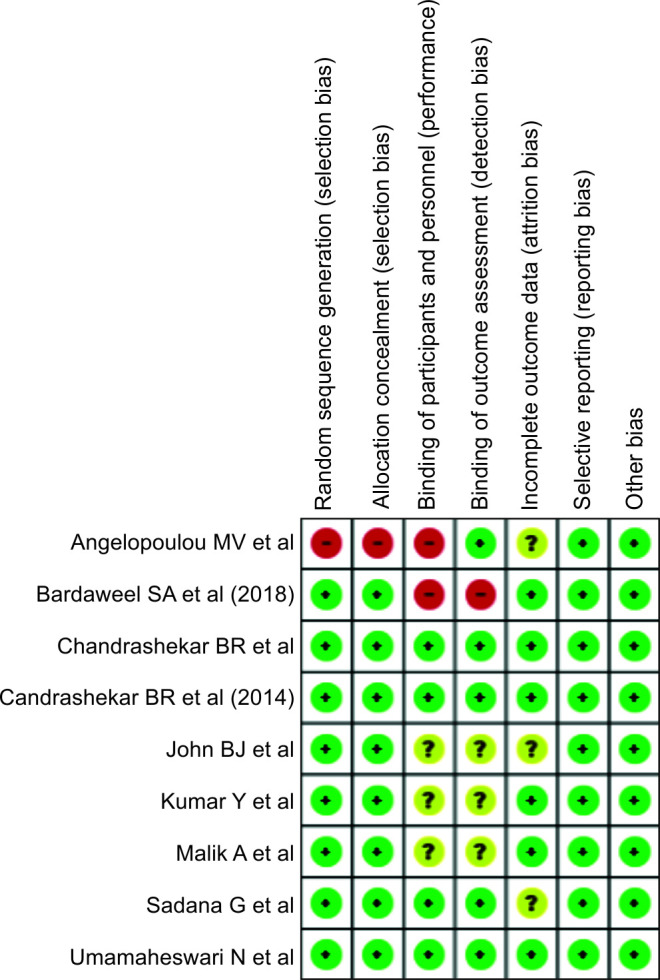
Risk of bias summary
Quantitative Results
A quantitative synthesis (meta-analysis) was done on the selected seven studies.
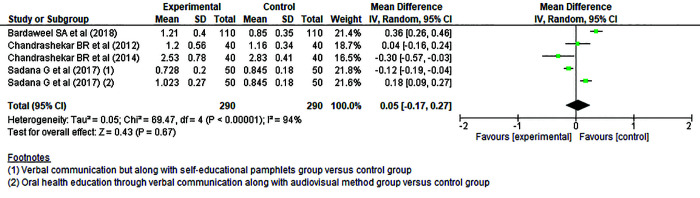
The studies with groups that compared OHE intervention vs controls concerning the plaque outcome (Silness and Lӧe Plaque Index) were evaluated. In these comparisons random-effects model analysis,1,2,12,14 the mean cumulative difference showed no significant finding in the change of the Plaque Index favoring neither the intervention groups nor the control groups [0.05 (–0.17, 0.27)] (Fig. 4). The funnel plot for Silness and Lӧe Plaque Index meta-analysis is presented in Figure 5.
Fig. 4.
Forest plot Silness and Lӧe Plaque Index
Fig. 5.
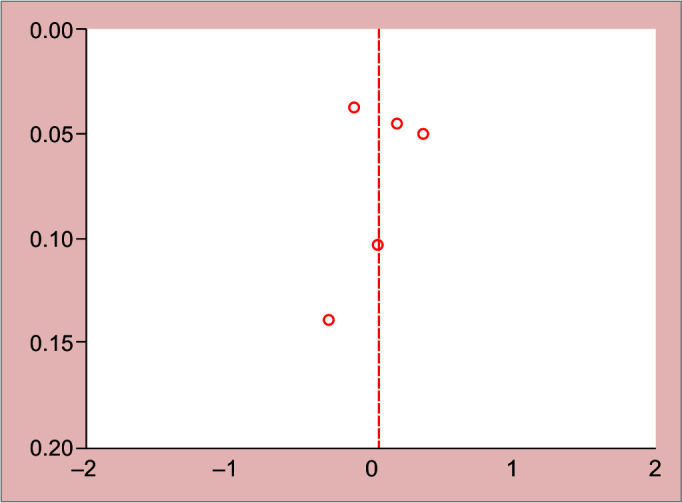
Funnel plot Silness and Lӧe Plaque Index
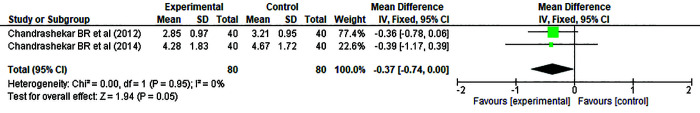
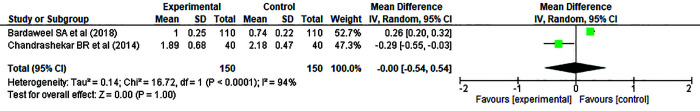
Two studies1,2 in which there were OHE intervention groups vs control groups analyzing oral hygiene status outcome (OHI-S). On deducing the forest plot we found that the cumulative mean difference was –0.37 (–0.74, 0.00) with fixed effect model based on the heterogeneity value of I indicating the newer methods (audio–visual aids) of OHE was more effective over traditional oral health interventions when improving oral hygiene status (Fig. 6).
Fig. 6.
Forest plot OHI-S Index
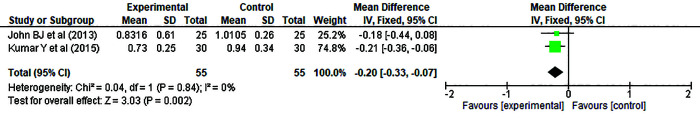
In the random-effects model analysis, two studies10,11 were Simplified Debris Index was analyzed, showed a significant difference oral hygiene status between the two groups, with reduced mean debris score showed that interventions (drama/plays and games based OHE) being more effective group than the controls with cumulative mean difference as –0.20 (–0.33, –0.07) (Fig. 7). The study conducted by Umamaheswari et al.14 used ordinal scale for outcome of interest so was not included in the meta-analysis.
Fig. 7.
Forest plot Debris-S Index
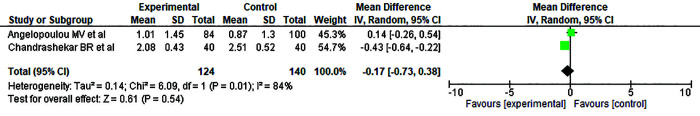
Two studies1,14 in which gingivitis outcome (Silness and Lӧe) were analyzed using random-effects model, showed a significant difference in improving and reducing gingivitis between the groups with mean difference of –0.00 (–0.54, 0.54), thus favoring neither the interventional nor the control group (Fig. 8).
Fig. 8.
Forest plot Gingival Index
Angelopoulou et al.6 assessed gingival status by using Simplified Gingival Index (GI-S) of which the meta-analysis could not be conducted. Whereas, Malik et al.8 did not have any counter study for comparison for Tuskegy–Gilmore Index to measure Plaque Index, hence it was not possible to include them in the meta-analysis.
The DMFT/DMFS Index was assessed by two studies1,6 using random-effects model, showed a significant difference in the change in gingivitis between the groups with mean difference of –0.17 (–0.73, 0.38). In the study by Chandrashekar et al.,1 DMFS Index by Klein et al. was measured but it was found that there was also no significant difference between baseline (p = 0.65) and postintervention (p = 0.56) DMFS scores in the intervention and control group. Similarly, in the study conducted by Angelopoulou et al.6 the intervention was experimental learning through poster, charts, etc. and mean dental caries (DMFT) score was measured according to the diagnostic criteria of the British Association of Community Dentistry, which did not show a significant difference (p = 0.601) in both the groups at the end of 18 months (Fig. 9). Table 2 depicts these results of study and the set of measurement for caries condition, preceding its involvement in the meta-analysis (Fig. 9).
Fig. 9.
Forest plot DMFT Index
Publication bias was not assessed for OHI-S, gingival, debris, and dental caries outcomes because more than five studies are required to detect funnel plot asymmetry.
Discussion
Education, in general, is one of the imperative factors responsible for behavioral change in children.15 Particularly, OHE is the key to prevent oral diseases, and it is always healthier to educate school age children because schools are the best environment to teach preventive dental health practices and have a long-term impact in future.16
This systematic review and meta-analysis showed that the distinct kinds of school oriented programs, which were mainly short-term interventions and only one study6 was found to extend for one and half year. This review, selected interventions that were carried out, only by dental professionals. With the exception of three studies,1,2,13 none of the other studies had rigorous and classic study design, impeding as to blinding of the participants and outcome accessors which was not implemented. Without a doubt, all the included studies1,2,6,8,10–14 have successfully accomplished their study objectives.
For the plaque outcome, four studies,1,2,12,14 were assessed in the quantitative meta-analysis, which checked on plaque scores using Silness and Lӧe Plaque Index, indicating no significant difference between the two types of OHE. The intervention time frame for these studies changed from 6 weeks to 6 months, furthermore there were no indications of regular follow-up visits done.
For OHI-S, the two studies conducted by Chandrashekar et al.1,2 were included in meta-analysis, showed a significant difference in the OHI-S scores favoring the experimental group which had used audio-visual aids as method of intervention. Similarly, for Debris Index-Simplified (DI-S), the two studies11,12 appended in meta-analysis showed a significant difference in the DI-S scores inclining toward the experimental group (drama/plays, games, and flashcards) indicating that OHE by the professionals might have definitely improved the oral health knowledge and practices of the students with a significant short-term improvement in the oral hygiene behavior reflecting in their OHI-S and DI-S scores.
For the gingivitis outcome in meta-analysis, the two studies1,14 showed that there was no significant difference between the experimental and control group ultimately revealing that there was no significant change in the gingival scores suggestive of no reduction in gingival inflammation.
Just two studies assessed caries as the outcome were included in this review.1,6 In general, their findings are colluding to the findings of debris and oral hygiene status results, that these two studies also showed significant difference between intervention and control groups, indicating an inclination toward the OHE intervention group. There is still a need for further investigation and research in dental caries status as attributed to the fact that caries is a chronic disease affecting the hard tissue of teeth. To bring a noticeable change in dental caries, studies need to have a longer evaluation as well as intervention period. The findings of this research may show their benefit in caries prevention in the long run and ultimately leading to improved oral health status.
In this systematic review and meta-analysis, we efforted to bring in new knowledge and information regarding the OHE interventions which could be designed and executed in a learning and influential school environment. In order to reach the masses at young and early age, to make an impact on a large group of school children (5–16 years) and to use the 21st century digitalization and technology boon to our benefit in betterment of oral health for our future generations, we need to revolutionize our methods. The conclusions drawn from this study could be helpful for the developed and developing countries to design school OHE model suiting their needs with interventions which are feasible and acceptable. Previous studies inspired us to conduct this meta-analysis which we contributed to, by involving dental caries as an assessment outcome, articulating and following a stringent selection criterion to reduce any infiltration of bias, keeping the age group of children specific to 5–16 years (common school age across the globe), and conducting subgroup analyses for all the selected outcomes as a variety of indices were used for recording, added up to help us in achieving our destined aim.
We recommend that future studies to be conducted involving assessment of dental caries outcome and plaque status with accord to meticulous methodology. More studies need to be planned for improving OHE with frequent reinforcement periods, regular follow-up visits, and standard methods for measurement of outcome.
The major limitation observed in most of the included studies1,2,8,10–14 is the short-term duration of the studies with lack of continuous reinforcement periods. Also, the mere presence of the dentist in the school and the chances of having a better guidance and supervision provided to the students is consequentially evident in influencing and motivating them to better self-care leading to Hawthorne effect. The ripple effect, personal home oral hygiene practices, and education status of the parents were not considered in the studies evaluated. Our limited access to databases was one of the factors that could not override. Loss to follow-up is also one of the major lacunae observed in majority of the studies. Also, a variability existed in the follow-up period considered for the studies included in the meta-analysis. The differences in the abilities between the dentists in their abilities to disseminate study messages and the ability of the students to assimilate could affect the study outcomes.
Inspiration can be drawn from previous studies17,18 to design an amalgamated school health education program (involving the newer interventions and fractionally the perks of traditional oral health counseling) which can aid to directly improve the oral health status and advertently evolving and upgrading education, awareness and significance of oral health at early age in a healthy learning environment. The OHE methods which are new and state of the art used in the included studies showed a variation only in regard to the deployed educational objects; however, the various intervention, as they were deployed, were based mainly on information transfer, active learning, and in order to produce a positive impact on oral health status.19 The consistency of these effects can only be acquired through a long-term program inculcating educational activities in the school routine, proving that health education is a process that informs, motivates, and helps people adopt and maintain good health practices and healthy lifestyles.20
Conclusion
Health education plays a vital role in oral health promotion among school children. Developing an oral health model in school-based setting or directly in school curriculum with an active amalgamation of the newer interventions along with oral health counseling or talk may be considered an effective tool. This systematic review and meta-analysis highlights that the recent and state of the art OHE methods can teach children to be motivated and trained in order to maintain oral health care, improve oral hygiene status, and inevitably their oral health status by reducing debris and dental caries. The short-term advantage is awareness and hence, for health, making school-based health program more effective and consistent, involving dentists, teachers, parents, and children with regular reinforcement.
Author Contributions
We certify that we have participated sufficiently in the intellectual content (GK, SV and VV), conception (VV and BK), and design (GK and BK) of this work. Search strategy, screening process, and data extraction (GK and BK), discrepancies solved by VV or the analysis (GK, JC, and DP), and interpretation of the data (GK, BK, and JC) (when applicable), as well as the writing of the manuscript (GK, BK, and VV).
(GK—Gurav Kashmira, SV—Shetty Vittaldas, VV—Vinay Vineet, BK—Bhor Ketaki, JC—Jain Chirayu, and DP—Divekar Pallavi).
Orcid
Kashmira M Gurav https://orcid.org/0000-0002-4616-3716
Vineet Vinay https://orcid.org/0000-0002-3354-2186
Ketaki Bhor https://orcid.org/0000-0003-3847-4319
Pallavi Divekar https://orcid.org/0000-0001-9801-8628
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Chandrashekar BR, Suma S, Sukhabogi JR, et al. Oral health promotion among rural school children through teachers: an interventional study. Indian J Public Health. 2014;58(4):235–240. doi: 10.4103/0019-557X.146278. [DOI] [PubMed] [Google Scholar]
- 2.Chandrashekar BR, Suma S, Kiran K, et al. The use of school teachers to promote oral hygiene in some secondary school students at Hyderabad, Andhra Pradesh, India: a short term prospective pilot study. J Fam Community Med. 2012;19(3):184–189. doi: 10.4103/2230-8229.102319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shenoy RP, Sequeira PS. Effectiveness of a school dental education program in improving oral health knowledge and oral hygiene practices and status of 12- to 13-year-old school children. Indian J Dent Res. 2010;21(2):253–259. doi: 10.4103/0970-9290.66652. [DOI] [PubMed] [Google Scholar]
- 4.D'Cruz AM, Aradhya S. Impact of oral health education on oral hygiene knowledge, practices, plaque control and gingival health of 13–15 year old school children in Bangalore city. Int J Dent Hygiene. 2012;11(2):126–133. doi: 10.1111/j.1601-5037.2012.00563.x. [DOI] [PubMed] [Google Scholar]
- 5.Ganesh M, Shah S, Parikh D, et al. The effectiveness of a musical toothbrush for dental plaque removal: a comparative study. J Indian Soc Pedod Prev Dent. 2012;30(2):139–155. doi: 10.4103/0970-4388.99988. [DOI] [PubMed] [Google Scholar]
- 6.Angelopoulou MV, Kavvadia K, Taoufik K, et al. Comparative clinical study testing the effectiveness of school based oral health education using experiential learning or traditional lecturing in 10 year-old children. BMC Oral Health. 2015;15:51. doi: 10.1186/s12903-015-0036-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gauba A, Bal IS, Jain A, et al. School based oral health promotional intervention: effect on knowledge, practices and clinical oral health related parameters. Contemp Clin Dent. 2013;4(4):493–499. doi: 10.4103/0976-237X.123056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malik A, Sabharwal S, Kumar A, et al. Implementation of game-based oral health education vs conventional oral health education on children's oral health-related knowledge and oral hygiene status. Int J Clin Pediatr Dent. 2017;10(3):257–260. doi: 10.5005/jp-journals-10005-1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higgings JPT, Thompson SG. Cochrane Handbook for Systematic Reviews of Interventions. Wiley; 2008. Available from: Accessed on 12th Feb 2020. [Google Scholar]
- 10.John BJ, Asokan S, Shankar S. Evaluation of different health education interventions among preschoolers: a randomized controlled pilot trial. J Indian Soc Pedod Prev Dent. 2013;31(2):96–99. doi: 10.4103/0970-4388.115705. [DOI] [PubMed] [Google Scholar]
- 11.Kumar Y, Asokan S, John B, et al. Effect of conventional and game-based teaching on oral health status of children: a randomized controlled trial. Int J Paediatr Dent. 2015;8(2):123–126. doi: 10.5005/jp-journals-10005-1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sadana G, Gupta T, Aggarwal N, et al. Evaluation of the impact of oral health education on oral hygiene knowledge and plaque control of school-going children in the city of Amritsar. J Int Soc Prev Community Dent. 2017;7(5):259–263. doi: 10.4103/jispcd.JISPCD_251_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Umamaheswari N, Asokan S, Thangakumaran S. Effectiveness of behavioral vaccine on the oral health of children in Komarapalayam, South India: a randomized controlled pilot trial. Contem Clin Dent. 2017;8(3):352–356. doi: 10.4103/ccd.ccd_152_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al Bardaweel S, Dashash M. E-learning or educational leaflet: does it make a difference in oral health promotion? A clustered randomized trial. BMC Oral Health. 2018;18(1):81. doi: 10.1186/s12903-018-0540-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Christensen GJ. Special oral hygiene and preventive care for special needs. J Am Dent Assoc. 2005;136(8):1141–1143. doi: 10.14219/jada.archive.2005.0319. [DOI] [PubMed] [Google Scholar]
- 16.Flanders RA. Effectiveness of dental health educational programs in schools. J Am Dent Assoc. 1987;114(2):239–242. doi: 10.14219/jada.archive.1987.0033. [DOI] [PubMed] [Google Scholar]
- 17.Monse B, Benzian H, Naliponguit E, et al. The Fit for School Health Outcome Study – a longitudinal survey to assess health impacts of an integrated school health programme in the Philippines. BMC Public Health. 2013;13:256. doi: 10.1186/1471-2458-13-256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duijster D, Monse B, Dimaisip-Nabuab J, et al. ‘Fit for school’ – a school-based water, sanitation and hygiene programme to improve child health: results from a longitudinal study in Cambodia, Indonesia and Lao PDR. BMC Public Health. 2017;17(1):302. doi: 10.1186/s12889-017-4203-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stein C, Santos N, Hilgert JB, et al. Effectiveness of oral health education on oral hygiene and dental caries in schoolchildren: systematic review and meta-analysis. Community Dent Oral Epidemiol. 2017;46(1):30–37. doi: 10.1111/cdoe.12325. [DOI] [PubMed] [Google Scholar]
- 20.De Farias IA, de Araujo Souza GC, Ferreira MÂ. A health education program for Brazilian public schoolchildren: the effects on dental health practice and oral health awareness. J Public Health Dent. 2009;9(4):225–230. doi: 10.1111/j.1752-7325.2009.00127.x. [DOI] [PubMed] [Google Scholar]