Abstract
Aim
To study the effect of combination of chlorhexidine and Fluoride on the growth and colonization of cariogenic bacteria (Streptococcus mutans) in children with mixed dentition.
Materials and methods
Sixty children of age 6–14 years with mixed dentition and S. mutans count > 1 × 105 CFU/mL of saliva were divided: group I–chlorhexidine varnish; group II–Fluoride varnish; group III–Combination of chlorhexidine and Fluoride varnish. chlorhexidine and Fluoride varnishes were applied to teeth once every week for four consecutive weeks in respective groups. Salivary S. mutans count was estimated and evaluated at baseline, 1, 3, and 6 months.
Results
No significant difference was seen in group I and II at the end of 1, 3, and 6 months (p > 0.001) but the reduction in S. mutans count was statistically more significant in group III after a period of 6 months (p < 0.001). Maximum reduction in count was noted in group III at all intervals of varnish application.
Conclusion
The concomitant use of chlorhexidine and fluoride varnish would prove to be more effective than individual components over a longer period of time and especially in high caries risk children.
How to cite this article
More VP, Hugar SM, Sogi S, et al. Comparative Evaluation of the Efficacy of Chlorhexidine, Fluoride and the Combined Use of Chlorhexidine and Fluoride Varnishes on Salivary Streptococcus mutans Count in Children with Mixed Dentition: An In Vivo Study. Int J Clin Pediatr Dent 2022;15(3):267-272.
Keywords: Chlorhexidine varnish, Fluoride varnish, Mixed dentition, S. mutans
Introduction
Oral cavity by being the mirror of our body serves as an integral part of general and systematic health. With more holistic approach the expectancy of life have increased. Seemingly oral health also plays a key role in improving the quality of life.1,2 Till date Streptococcus mutans is the known etiological factor in the formation of dental caries. These S. mutans are among the best adapted organisms to the cariogenic environment; hence the treatment of dental caries should be directed toward reduction of S. mutans.3
A number of preventive programs focusing primarily on encouraging the twice daily use of fluoridated toothpaste in the initial years of age and Community water fluoridation to reduce dental caries4 have been carried out but the practicality is a big question in developing countries where there is no centralized water supply system, which makes the initial cost of implementation very high.2
C.G. Emilson5 states that though the use fluoride has proven as the most effective and successful agents in the prevention of tooth decay, only meager antimicrobial activity has been cited and in patients with fluorosis and patients with kidney disorders it is contraindicated. Hence the next most effective antimicrobial agent is chlorhexidine which was introduced 20 years ago by Loe et al.6 Chlorhexidine mouth rinses have proven to be very effective in maintenance of plaque control which is essential in caries reduction as well as gingivitis7 but with some side effects like brown stains, bitter taste, minimal taste sensation and epithelial. desquamation8 Therefore a way to overcome the side effects Cervitec, a varnish containing 1% chlorhexidine and 1% thymol has been introduced.6 To control plaque formation and caries progression, some authors have recommended the concomitant use of chlorhexidine and fluoride.9,10
Hence a research was planned to evaluate the effect of combination of chlorhexidine and fluoride on the growth and colonization of cariogenic bacteria (S. mutans) in children with 6–14 years of age. The required data for the study was collected from 60 children free of any systemic diseases and DMFT/deft 3–5 with mixed dentition aged 6–14 years from the Department of Pediatrics and Preventive Dentistry. While handicap or mentally challenged or children using antibiotics or antiseptic mouthwashes for a period of 3 months prior to the study or with any intraoral appliances or any congenital abnormalities like cleft palate, ectodermal dysplasia, amelogenesisimperfecta, dentinogenesisimperfecta, etc. were excluded from the study.
Materials and Method
The necessary treatment was provided at the beginning of the study. Patients were given a fluoridated tooth paste to brush the teeth twice daily. A wash out period of 10 days was followed before the start of the study which is started on 11th day.11
A total of 100 selected children (one at a time) were made to sit comfortably on the chair. Children were made to rinse the mouth with water to remove any debris and to swallow the preexisting saliva. Subjects were asked to chew a standard piece of paraffin wax block and collect the saliva in mouth for 1 minute. Stimulated saliva was sucked from the floor of mouth of subjects using disposable syringes to avoid any possible contamination and 1 mL of this saliva was injected into containers containing 1 mL Thioglycollate transport media (Fig. 1). The saliva samples were identified by the code numbers given during the period of sample collection and processing. Same code numbers wereused for the particular patient during subsequent saliva sample collection.
Fig. 1.

Photograph showing collection of saliva sample from floor of mouth
The samples were transported to the laboratory immediately after collection and cultured on the same day in Department of Oral Pathology and Microbiology. Sixty patients were selected for the study that had S. mutans count > 1 × 105 CFU/mL and assigned to three different groups: group I- Fluoride varnish (n = 20), group II- chlorhexidine varnish (n = 20), group III- Combination of fluoride and chlorhexidine varnish (applied alternately) (n = 20).
A baseline count of S. mutans was recorded for 60 children and then oral prophylaxis was done for all. Varnish application was performed quadrant wise sequentially starting from mandibular teeth and then continued to the maxillary teeth (Fig. 2). Each subject was instructed to rinse their mouth with plain water followed by drying of teeth with the help of air syringe before varnish application. Varnish was applied to the teeth with the help of applicator tips which are then allowed to dry for 1 minute. Subjects were instructed not to eat or rinse their mouth for 1 hour after the procedure and not to brush till the next morning. Same procedure was repeated once in every week for four consecutive weeks. In group III chlorhexidine and fluoride varnishes were applied alternately every week.
Fig. 2.

Photograph showing application of varnish on teeth under complete isolation
Saliva samples were collected subsequently after 1 month, again after 3 months, and lastly 6 months after the application of varnish for microbiological assessment. The data obtained from the study was compiled, tabulated, and subjected to statistical analysis using ANOVA test and Bonferroni multiple comparison test. p value (<0.001) was considered to be statistically significant.
Results
The difference between the age groups in all three groups was not statistically significant with a p value of 0.104 (p value > 0.001). All 60 children accepted the varnishes (100% in all the three groups) and showed no pain or discomfort after varnish application. Mean DMFT for chlorhexidine varnish group [group I] was 4.10 with a standard deviation (SD) of 0.79; while for Fluoride varnish group [group II] the mean DMFT was 4.15 with standard deviation of 0.75 and chlorhexidine + fluoride varnish group [group III] showed mean of 4.20 with a standard deviation of 0.84 (Table 1, Fig. 3).
Table 1.
Mean, standard deviation (SD), and standard error of mean (SE) of dental caries experience (dmft) according to different varnish groups
| Group | Mean | SD | SE |
|---|---|---|---|
| I | 4.10 | 0.7881 | 0.1762 |
| II | 4.15 | 0.7452 | 0.1666 |
| III | 4.20 | 0.8335 | 0.1864 |
| Total | 4.15 | 0.7770 | 0.1000 |
Fig. 3.
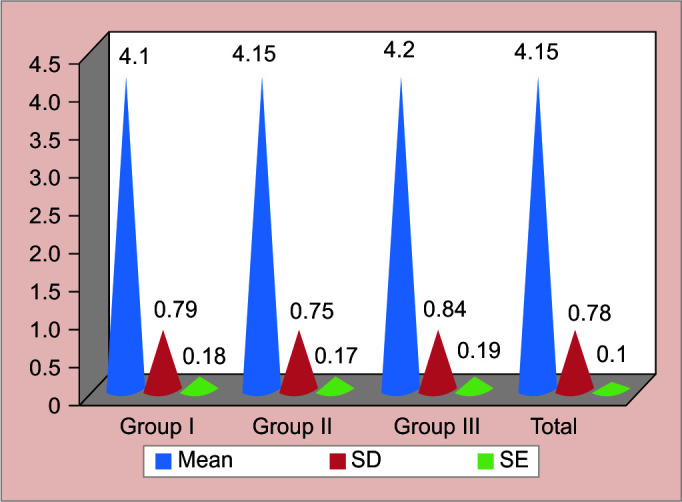
Mean, standard deviation (SD), and standard error of mean (SE) of dental caries experience (DMFT) according to different varnish groups
In group I at baseline a maximum of 120 × 105 CFU/mL of saliva while a minimum of 60 × 105 CFU/mL of saliva was recorded with a mean of 88.85 × 105. The results showed statistically significant reduction in CFU/mL in first month than after 6 months in all three groups (Table 2, Fig. 4). Intergroup comparison (Bonferroni Test) showed significant decrease in S. mutans count in all the three groupsat 1 month, 3 months, and 6 months after the application of varnishes. The reduction in chlorhexidine varnish group [group I] was statistically more significant than Fluoride varnish group [group II] at all intervals with p value 0.00 at 1 month, p value 0.00 at 3 months and p value 0.002 at 6 months (Table 3).
Table 2.
Difference between the mean of Streptococcus mutans colony-forming unit per mL of saliva (x105 CFU/mL) in group I, group II, group III at baseline, 1 month, 3 months, and 6 months after the application of chlorhexidine and fluoride varnishes, respectively in each group
| Duration | n | Mean | Minimum | Maximum |
|---|---|---|---|---|
| Chlorhexidine varnish group [group I] | ||||
| Baseline | 20 | 88.85 | 60 | 120 |
| 1 month | 20 | 0.7 | 0 | 2 |
| 3 months | 20 | 1.5 | 0 | 8 |
| 6 months | 20 | 3.3 | 0 | 8 |
| Fluoride varnish group [group II] | ||||
| Baseline | 20 | 93.2 | 80 | 110 |
| 1 month | 20 | 2.9 | 0 | 6 |
| 3 months | 20 | 5.6 | 0 | 10 |
| 6 months | 20 | 6.6 | 0 | 20 |
| Chlorhexidine + Fluoride varnish group [group III] | ||||
| Baseline | 20 | 87.65 | 65 | 120 |
| 1 month | 20 | 0.3 | 0 | 2 |
| 3 months | 20 | 0.4 | 0 | 2 |
| 6 months | 20 | 0.8 | 0 | 4 |
Fig. 4.
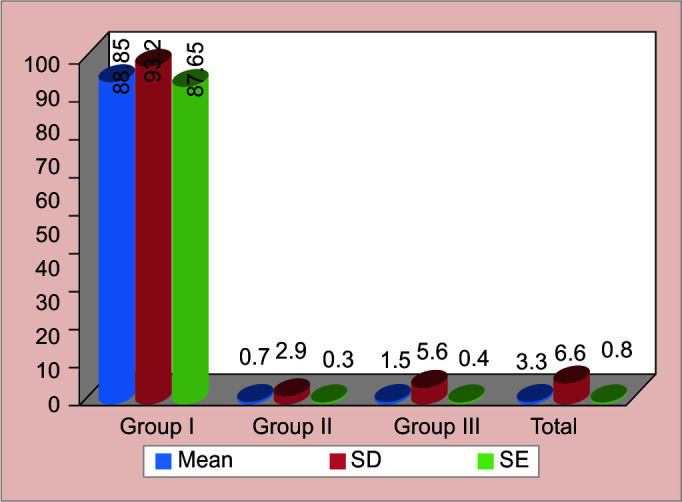
Comparison between the mean of Streptococcus mutans colony-forming unit per mL of saliva (x 105 CFU/mL) in chlorhexidine varnish group [group I], fluoride varnish group [group II], chlorhexidine + fluoride varnish group [group III] at baseline, 1 month, 3 months, and 6 months after the application of varnishes
Table 3.
The comparison of probability values based on Bonferroni multiple comparison test at various intervals of the study. (Intergroup comparison)
| p-value | 1 month | 3 months | 6 months |
|---|---|---|---|
| Group I with group II | 0.00 | 0.00 | 0.002 |
| Group I with group III | 1.00 | 0.239 | 0.008 |
| Group II with group III | 0.00 | 0.00 | 0.00 |
Group III showed statistically more significant reduction in S. mutans owing to a p value of count than group I. Maximum reduction for a longer period was recorded in chlorhexidine + fluoride varnish group [group III] and was statistically significant (Fig. 5).
Fig. 5.
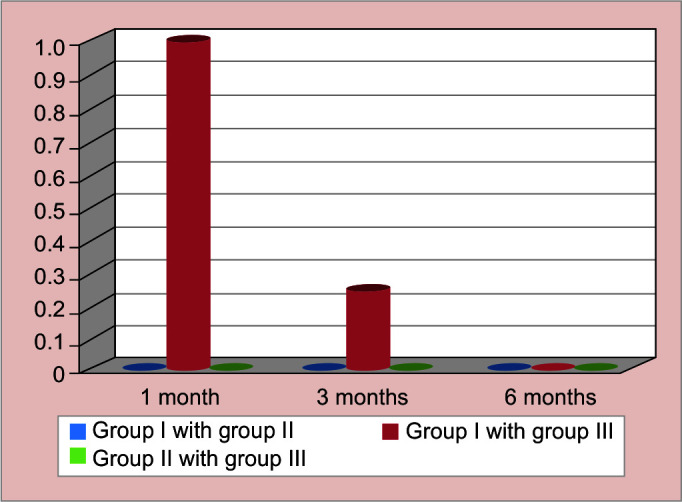
The comparison of probability values based on Bonferroni multiple comparison test at various intervals of the study. (Intergroup comparison)
Discussion
Prevention of dental caries and Minimal Intervention Dentistry plays a vital role in pediatric dental practice. In the present century, great emphasis is placed on caries risk assessment, early diagnosis, and caries control. Thus, the focus has been shifted to preventive strategies and minimal intervention to eliminate the most prevalent disease “dental caries”1 which is a multifactorial disease that will not occur without the presence of the microorganisms; S. mutans playing a major role.12,13 A variety of chemotherapeutic agents have been examined for their ability to control oral microorganisms and to affect plaque formation. The main classes which have been tested are antibiotics, metal ions, enzymes, plant extracts, and phenolic compounds.3
Fluoride is the most extensively studied and used for caries prevention.14 In 1985, Balanyk and Sandham15 developed a chlorhexidine containing antibacterial varnish that brought a new concept into preventive dentistry. Over the past few decades, chlorhexidine has evolved as the gold standard among the antimicrobial substances used in dentistry.16 Emilson CG5 and Messer13,17 showed that the best clinical effect of chlorhexidine has been obtained in high risk children. In our study Cervitec varnish and Fluorprotector varnish were used. One of the constituent of Cervitec varnish is chlorhexidine, which is a bisbiguanide with broad antibacterial activity.6 The highly cationic nature of chlorhexidine makes it both bacteriostatic (at low concentration) and bactericidal (at high concentration).
In our study, chlorhexidine varnish group [group I] showed drastic reduction in mean S. mutans CFU/mL of saliva from 88.85 × 105 CFU/mL of saliva to 0.7 × 105 CFU/mL of saliva at 1 month, 1.5 × 105 CFU/mL of saliva during 3 months, and 3.3 × 10 CFU/mL at 6 months interval after application of varnish (Table 2, Fig. 4).
Fluoride has cariostatic effect on the dental hard tissues and prevents or halts the dental decay.18,19 The mechanism of action of fluoride is to reduce demineralization and promote remineralization of tooth structure20 by the uptake of calcium and phosphate ions of saliva.21 Its antimicrobial activity is due to the inhibition of glucose transport, carbohydrate storage, extracellular polysaccharide formation by interfering with enolase enzyme in microorganisms.21–23 In the present study, Fluoride varnish group [group II] showed reduction in mean S. mutans CFU/mL of saliva from 93.20 × 105 CFU/mL of saliva to 2.9 × 105 CFU/mL at 1 month, 5.6 × 105 CFU/mL at 3 months, and 6.6 × 10 CFU/mL at 6 months interval after application of varnish (Table 2).
Zickert et al.24 1987 and Muerman et al.25 1988 showed that fluoride acts additively or even synergistically with chlorhexidine on S. mutans. Hence, we introduced the third group III where chlorhexidine varnish and fluoride varnish were applied to the same individual but alternately to study the combined effect of both agents on S. mutans. In our study, chlorhexidine + fluoride varnish group [group III] showed statistically significant reduction in mean S. mutans CFU/mL of saliva from 87.65 × 105 CFU/mL of saliva to 0.3 × 105 CFU/mL at 1 month, 0.4 × 105 CFU/mL of saliva at 3 months, and 0.7 × 105 CFU/mL of saliva at 6 months interval after application of varnishes (Fig. 4). Brailsford SR et al.26 stated that the combination of Fluor-Protector and chlorhexidine varnish to be more useful in the prevention of tooth decay and it is very simple to apply and nonpainful.
In accordance to other similar studies,9,27,28 the combination preventive agents is thus helpful in reduction of caries to a greater extent than individual component. This is more important especially in patients with radiation caries,29,30 medically compromised patients, or children with special healthcare needs.31 While in patients with orthodontic appliances, the occurrence of white spot lesions is reduced when a combination of fluoride varnish and chlorhexidine varnish is used.30,32,33 However Subramanian et al.12 showed that the combination of both chlorhexidine and fluoride (Tooth Mousse) was less effective on S. mutans count as compared to chlorhexidine alone. The efficacy of chlorhexidine per se is reduced when used along with agents that are highly anionic in nature. Not many studies have been carried out in this front and more research is still required.
Emilson CG5 and Schaeken MJ et al.34 found that the number of colonized tooth surfaces remained significantly below original levels for more than 26 weeks (almost 6 months) following treatment with chlorhexidine. Bretz et al.35 and Emilson CG5 found significant improvement in the gingival health of subjects for up to 6 months. post treatment. Hence reapplication of the chlorhexidine and fluoride varnishes has to be carried out after every 6 months.5,36
The present study showed effective suppression of S. mutans. with the use of both the antimicrobials individually but the suppression was more significant with the combination of varnishes. The use of combination of chlorhexidine and fluoride varnishes is suitable and safe for very young children. The amount used is also lesser than the gels or mouth rinses. The ingestion of the chlorhexidine is significantly reduced when used in the form of the varnish. It also reduces the cost and cause less trauma to the young patients by early prevention of dental caries.13 Prevention is more cost effective as the patient shifts from high-risk level tolow risk level.37 Also, the varnish itself acts as a protective barrier to prevent the teeth from external staining.38
Considering the shorter treatment time, better taste, easier application technique, and safety, a varnish for preventive programs seems justified. But the most important difficulty in implementation of such preventive program is the availability of these varnishes in developing countries. For this more research is mandatory in this field and also consideration for subsidized rates for these products has to be given.
Conclusion
A safe application of chlorhexidine and fluoride in children is possible when its use is in the form of varnishes. Moreover, chlorhexidine and fluoride remains in the oral cavity over extended period of time, thus the suppression and stabilization of S. mutans to nonpathogenic levels are clearly observed over time.
Our study suggests that more research is urgently needed to determine the optimal preventive regimens, including antimicrobial therapies to prevent and modify the course of oral diseases in children. The concomitant use of chlorhexidine and fluoride varnish has proved to be more effective than individual components over a longer period of time, that is, over a period of 6 months. Hence we recommend the use of combination of chlorhexidine and fluoride varnishes for better results especially in children with high caries risk.
Clinical Significance
With the evolving era in dentistry “constriction with conviction” has gained more popularity. Minimally invasive dentistry is one such branch which has evolved tremendously, it is paramount for the dentist to gain knowledge and choose wisely based on clinical evidence which will help them in their practice. Our study aims in providing knowledge established on evidence-based clinical research which will benefit the dentist from all over the globe.
Orcid
Suganya M https://orcid.org/0000-0001-6977-5064
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.National Oral Health Survey and fluoride mapping 2002–2003. 2004 Dental Council of India, New Delhi. [Google Scholar]
- 2.Hardman MC, Davies GM, Duxbury JT, et al. A cluster randomized controlled trial to evaluate the effectiveness of fluoride varnish as a public health measure to reduce caries in children. Caries Res. 2007;41(5):371–376. doi: 10.1159/000104795. [DOI] [PubMed] [Google Scholar]
- 3.Loesche WJ. Role of Streptococcus mutans in human dental decay. Microbiol Rev. 1986;50(4):353–380. doi: 10.1128/mr.50.4.353-380.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nissen LC, Douglass CW. Theoretical considerations in applying cost-benefit and cost effective analyses to preventive dental programs. J Public Health Dent. 1984;44(4):156–168. doi: 10.1111/j.1752-7325.1984.tb03077.x. [DOI] [PubMed] [Google Scholar]
- 5.Emilson CG. Potential efficacy of chlorhexidine against mutans streptococci and human dental caries. J Dent Res. 1994;73:682–691. doi: 10.1177/00220345940730031401. [DOI] [PubMed] [Google Scholar]
- 6.Löe H, Schiott CR. The effect of mouthrinses and topical application of chlorhexidine on the development of dental plaque and gingivitis in man. J Periodontal Res. 5(2):79–83. doi: 10.1111/j.1600-0765.1970.tb00696.x. [DOI] [PubMed] [Google Scholar]
- 7.Bratthall D, Serinirach R, Rapisuwon S, et al. A study into the prevention of fissure caries using an antimicrobial varnish. Int Dent J. 1995;45(4):245–254. [PubMed] [Google Scholar]
- 8.Petersson LG, Magnusson K, Andersson H, et al. Effect of semiannual applications of a chlorhexidine/fluoride varnish mixture on approximal caries incidence in school children. A three year radiographic study. Eur J Oral Sci. 1998;106(2):623–627. doi: 10.1046/j.0909-8836.1998.eos106203.x. [DOI] [PubMed] [Google Scholar]
- 9.Luoma H, Murtomma H, Nuuja T, et al. A simultaneous reduction of caries and gingivitis in a group of schoolchildren receiving chlorhexidine-fluoride applications. Results after 2 years. Caries Res. 1978;12(5):290–298. doi: 10.1159/000260347. [DOI] [PubMed] [Google Scholar]
- 10.Ullsfoss BN, Ogaard B, Arends J, et al. Effect of a combined chlorhexidine and NaF mouthrinse: an in vivo human caries model study. Scan J Dent Res. 1994;102(2):109–111. doi: 10.1111/j.1600-0722.1994.tb01164.x. [DOI] [PubMed] [Google Scholar]
- 11.Kulkarni VV, Damle SG. Comparative evaluation of efficacy of sodium fluoride, chlorhexidine and triclosan mouth rinses in reducing the mutans streptococci count in saliva: an in vivo study. J Indian SocPedoPrev Dent. 2003;12(3):98–104. [PubMed] [Google Scholar]
- 12.Subramaniam P, Naidu P. Effect of Tooth Mousse plus Cervitec gel on S.mutans. J of Minim Interv Dent. 2009;2(3):164–168. [Google Scholar]
- 13.Anna GA, Cristiane TR, Beatriz GN, et al. The use of chlorhexidine varnishes in children: what is out there? Int J Dent. 2010;9(3):142–147. [Google Scholar]
- 14.Beltrán-Aguilar ED, Goldstein JW, Lockwood SA. Fluoride varnishes: a review of their clinical use, cariostatic mechanism, efficacy and safety. J Am Dent Assoc. 2000;131(5):589–596. doi: 10.14219/jada.archive.2000.0232. [DOI] [PubMed] [Google Scholar]
- 15.Balanyk TE, Sandham HJ. Development of sustained release antimicrobial dental varnishes effective against Streptococcus mutans in vitro. J Dent Res. 1985;64(12):1356–1360. doi: 10.1177/00220345850640120501. [DOI] [PubMed] [Google Scholar]
- 16.George AM, Kalangi SK, Vasudevan M, et al. Chlorhexidine varnishes effectively inhibit porphyromonas gingivalis and streptococcus mutans- an in vivo study. J Indian Soc Periodontol. 2010;14(3):178–180. doi: 10.4103/0972-124x.75913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Messer LB. Assessing caries risk in children. Austral Dent J. 2000;45(1):10–16. doi: 10.1111/j.1834-7819.2000.tb00235.x. [DOI] [PubMed] [Google Scholar]
- 18.Van Houte J. Role of micro-organisms in caries etiology. J Dent Res. 1994;73(3):672–681. doi: 10.1177/00220345940730031301. [DOI] [PubMed] [Google Scholar]
- 19.Pienihäkkinen K, Söderling E, Ostela I, et al. Comparison of the efficacy of 40% chlorhexidine varnish and 1% chlorhexidine-fluoride gel in decreasing the level of salivary mutans streptococci. Caries Res. 1995;29(1):62–67. doi: 10.1159/000262042. [DOI] [PubMed] [Google Scholar]
- 20.Johnson G, Almqvist H. Non-invasive management of superficial root caries lesions in disabled and infirm patients. Gerodontology. 2003;20(1):12–14. doi: 10.1111/j.1741-2358.2003.00009.x. [DOI] [PubMed] [Google Scholar]
- 21.Jabbarifar SE, Tabibian SA, Poursina Effect of fluoride mouth rinse and tooth paste on number of streptococcal colony forming units of dental plaque. J Res Medical Sciences. 2005;10(6):363–367. [Google Scholar]
- 22.Nolte WA. 4th edition. Mosby; 1982. Oral Microbiology: With basic microbiology and immunology. [Google Scholar]
- 23.Makarem A, Jahanian F, KhajehKaramodine M. Evaluation of effect of sodium fluoride tablet on level of streptococcal dental plaque. Mashhad Dental Journal 59. 1996:61. [Google Scholar]
- 24.Zickert I, Emilson CG, Ekblom K, et al. Prolonged oral reduction of Streptococcus mutans in humans after chlorhexidine disinfection followed by fluoride treatment. Scand J Dent Res. 1987;95(4):315–319. doi: 10.1111/j.1600-0722.1987.tb01847.x. [DOI] [PubMed] [Google Scholar]
- 25.Muerman JH. Ultrastructure, growth, and adherence of streptococcus mutans after treatment with chlorhexidine and fluoride. Caries Res. 1988;22(5):283–287. doi: 10.1159/000261122. [DOI] [PubMed] [Google Scholar]
- 26.Ekenback SB, Lindver LE, Lonnies H. Effect of four dental varnishes on the colonization of cariogenic bacterias on exposed sound root surfaces. Caries Res. 2000;34(1):70–74. doi: 10.1159/000016572. [DOI] [PubMed] [Google Scholar]
- 27.Spets-Happonen S, Luoma H, Forss H, et al. Effects of a chlorhexidine-fluoride-strontium rinsing program on caries, gingivitis and some salivary bacteria among Finnish school children. Scan J Dent Res. 1991;99(2):130–138. doi: 10.1111/j.1600-0722.1991.tb01875.x. [DOI] [PubMed] [Google Scholar]
- 28.Petersson LG, Magnusson K, Andersson H, et al. Effect of quarterly treatments with a chlorhexidine and a fluoride varnish on approximal caries in caries-susceptible teenagers: a 3 year clinical study. Caries Res. 2000;34(2):140–143. doi: 10.1159/000016581. [DOI] [PubMed] [Google Scholar]
- 29.Katz S. The use of fluoride and chlorhexidine for the prevention of radiation caries. J Am Dent Assoc. 1982;104(2):164–170. doi: 10.14219/jada.archive.1982.0016. [DOI] [PubMed] [Google Scholar]
- 30.Ogaard B, Larsson E, Henriksson T, et al. Effects of combined application of antimicrobial and fluoride varnishes in orthodontic patients. Am J Orthod Dentofacial Orthop. 2001;120(1):28–35. doi: 10.1067/mod.2001.114644. [DOI] [PubMed] [Google Scholar]
- 31.Gary RR. Effectiveness of methods used by dental professionals for the primary prevention of dental caries. J Dent Edu. 2001;65(10):1063–1072. doi: 10.1002/j.0022-0337.2001.65.10.tb03450. [DOI] [PubMed] [Google Scholar]
- 32.Eronat C, Alpoz AR. Effect of Cervitec on the salivary S. mutans levels in patients with fixed orthodontic appliances. J Marmara Univ Dent Fac. 1997;2(4):605–608. [PubMed] [Google Scholar]
- 33.Attin R, Thon C, Schlagenhauf U, et al. Recolonisation of mutans streptococci on teeth with orthodontic appliances after antimicrobial therapy. Eur J Orthodont. 2005;27(5):489–493. doi: 10.1093/ejo/cji018. [DOI] [PubMed] [Google Scholar]
- 34.Schaeken MJ, De Jong Franklin M. Effect of chlorhexidine Iodine on the composition of human dental plaque. Caries Res. 1984;18(5):401–407. doi: 10.1159/000260794. [DOI] [PubMed] [Google Scholar]
- 35.Bretz WA, Valente MI, Djahjah C, et al. Chlorhexidine varnishes prevent gingivitis in adolescents. J Dent Children. 2000;67(6):399–402. 374. [PubMed] [Google Scholar]
- 36.Svanberg M. Contamination of toothpaste and toothbrush by Streptococcus mutans. Scand J Dent Res. 1978;86(5):412–414. doi: 10.1111/j.1600-0722.1978.tb00646.x. [DOI] [PubMed] [Google Scholar]
- 37.Anusavice KJ. Chlorhexidine, fluoride varnish, and xylitol chewing gum: underutilized preventive therapies? Gen Dent. 1998;46(1):34–38. [PubMed] [Google Scholar]
- 38.Achong RA, Briskle DM, Hildebrandt GH, et al. Effect of chlorhexidine varnish mouthguards on the levels of selected oral micro organisms in pediatric patients. Pediatr Dent. 1999;21(3):169–175. [PubMed] [Google Scholar]


